-
Who discovered the first antimicrobial?
Paul Ehrlich and Sahachiro Hata found Salvarsan could treat syphilis
-
Who founded sulfa drugs?
Gerhard Domagk found the red dye Prontosil could treat streptococcal infections in animals
-
What did Alexander Flemming do?
Discovered that Mold Penicillium excreted toxic compounds toxic to Staph Aureus
-
Where are most antimicrobial drugs found?
Microorganisms found in the soil, most are from other bacteria than fungi
-
What are the features of antimicrobial drugs?
-Selective toxicity, measured in Therapeutic Index (larger better)
-Static or cidal, static drugs inhibit growth while cidal kills
-Narrow/Broad spectrum, affect large or small range of microbes
-Combinations, antagonistic drugs interfere with others, synergistic enhances and neither are additive
- Tissue distribution, metabolism, and excretion. Drugs unstable at low pH must be injected, short half life means more doses per day, kidney or liver dysfunction means doses must be adjusted for toxicity
-Adverse effects, for example toxicity, allergic reactions, suppression of normal microbiota
-
What is MIC and MBC?
MIC is lowest concentration of drug needed to prevent growth in vitro
MBC is lowest concentration that kills 99.9% of cells in vitro
-
What are ways you can test for MIC>
-An automated system tests for turbidity in cards
- E test uses strip with drug gradients
- Diffusion bioassay
-
What are the drug targets of bacteria?
Cell wall (peptidoglycan), cell membrane integrity, Nucleic acid synthesis, metabolic pathways, protein synthesis
-
What do B-LACTAM's do?
Inhibit enzymes that catalyze formation of peptide bridges between adjacent glycan strands, IE disrupt peptidoglycan synthesis and weaken cell walls leading to cell lysis.
-
How do bacteria fight against B-lactam?
They synthesize B-lactamase which inactivate it
-
What are Cephalosporins
B-lactam drugs that are resistant to B-lactamases
-
What are the antibiotics that target bacterial ribosomes?
Macrolides prevent continuation of protein synthesis
- Bacteriostatic against gram positives
Tetracyclines black attachment of tRNA to ribosome
- Effective against gram +/- bacteria
- Actively transported in prokaryotic but not animal cells
Aminoglycosides block initiation of translation and cause misreading of mRNA
-enters cells via active transport requiring respiratory metabolism
- Often Toxic due to affect on mitochondria
-
What do fluoroquinolones and Rifamycins do?
fluoroquinolones inhibit topoisomerases and is bactericidal
Rifamycins block prokaryotic RNA polymerase from initiating transcription
-
How do drugs interfere with metabolic pathways?
Through the folate pathway. Bacteria synthesize it, we eat it
-
What are the mechanisms of acquired resistance?
Drug-inactivating enzymes
Alteration of target molecule
Decreased uptake of drug
-
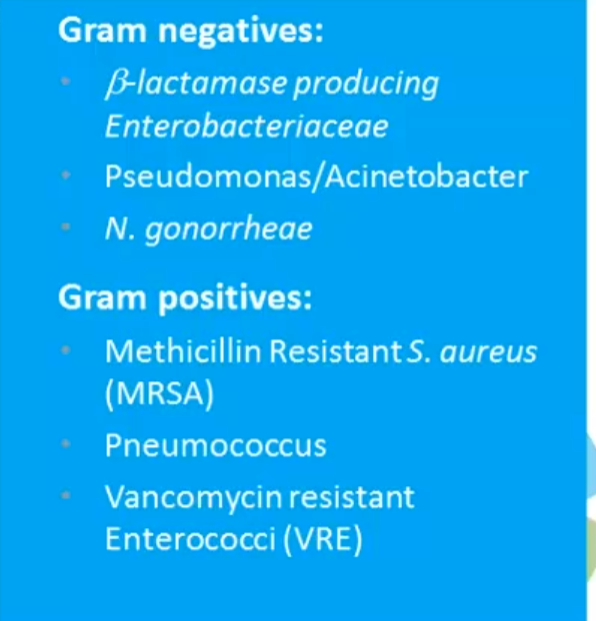
What are the problematic bacteria?