-
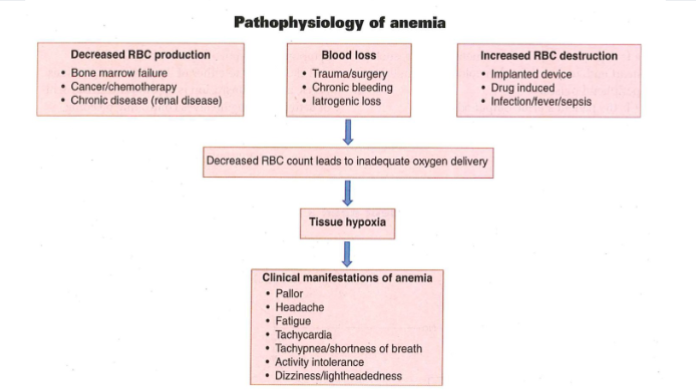
Pathophysiology of anemia
-
Blood values
1. RBC 4.35-5.65 million
2. HCT: 43-49%, 38-44%
3. Hemoglobin: 12.6 - 17.4 g/dL men, females: 11.7-16.1g/dL
4. blood loss of 30% = 1500mL
5. blood loss of 40% = 2000mL
-
Anemia symptoms
1. tiredness, weakness, pale skin, irregular heartbeat, sob, chest pain, dizziness, cold hands and feet, headache
-
Iron deficiency
1. Patho: lacks iron so it makes less hemoglobin and fewer rbcs so delivers less oxygen
2. Risks: hemorrhage; menses; elderly; inadequate dietary intake, GI issues (Crohn's, celiac)
3. CM: pica, glossitis (swelling of tongue), koilonychias (spoon-shaped nails), altered LOC
4. Dx: CBC, ferritin levels
5. NI: Parenteral iron stains the skin (z track method), monitor VS, iron supplements (PO, IM, IV), dietary teaching, Vit. C helps absorb.
-
Vitamin B12 (Cobalamin) Deficiency Anemia
1. B12 = pernicious anemia
2. risks: vegetarians, chronic alcohol abuse, crohn's, elderly
3. CM: peripheral neuropathy, spinal cord dysfunction, AMS, visual disturbances, tinnitus
4. Dx: CBC, serumvit b12
5. NI: Monitor VS, neuro assessment, assess pain, Vit B12 via IM, PO, SL, intranasal, dietary
-
Folic Acid Deficiency Anemia
1. Patho: folate aids in the production of rbc, less folate, less rbc
2. Risks: elderly, chronic disease, alcohol abuse, inadequate dietary intake
3. CM: Pancytopenia (low rbc, wbc, platelets), mood changes, confusion, disorientaiton
4. Dx: CBC, Serum Folate
5. NI: monitor VS, assess b12 deficiency, dietary
-
Blood
1. Blood types: A, B, Rh
2. Blood products: Packed rbc, fresh frozen plasma, whole blood
3. Given when oxygen carrying ability of the blood is compromised, low Hgb
-
Blood Transfusion requirements
1. Patient consent form must be signed
2. Two RNs must verify
3. pt name, mrn, blood bank id, blood type, donor id number, blood exp date, blood product, donor blood product type and rh, results of crossmatch test, special transfusion req if applicable.
4. All blood products must be iniated immediately 20 mins
5. Nurse must stay for 15 mins after start.
6. Each unit of blood must finish within 4 hours.
7. 20 G iv or higher, Y-tubing filter, check for fever, crackles, hives (urticaria) d/c immediately if reaciton.
-
Cancer Early Warning Signs (CAUTION)
1. Change in bowel or bladder habits
2. A sore that does not heal
3. Unusual bleeding or discharge
4. Thickening or lump in breast or scrotum
5. Indigestion or difficulty in swallowing
6. Obvious change in a mole or wart
7. Nagging cough or hoarseness.
-
Cancer Prevention
1. avoid exposure to known carcinogens
2. wear sunscreen
3. prevent/treat infectious diseases
4. maintain a healthy weight
5. engage in regular moderate physical activity
6. eat a healthy, plant based diet, avoid sat. fats, limit red meat
7. limit consumption of alcohol.
-
TNM Staging Classification
1. T = tumor size and penetration:
2. N = cancer spread to nearby lymph nodes
3. M = metastasis (malignant)
-
Cancer External radiation
1. monitor skin changes
2. wash radiation site with water only, no soap
3. do not apply lotions, perfumes, powder to site.
4. Do not wash off the treatment marks
5. protect skin from sun exposure for 1 year.
6. wear loose, soft clothing over treated area.
-
Internal Radiation Cancer tx
1. place pt in private room
2. time, distance, shielding
3. cluster care so minimal time is spent in the room
4. wear lead apron
5. wear a film badge (dosimeter)
-
Antineoplastics
1. drugs to treat cancer
2. Routes: IV (vesicants), PO, IM, topical
3. SE: bone marrow suppression
-
Thrombocytopenia
1. Low platelets
2. Range: 150k-450k
3. CM: easy bruising, superficial bleeding (purple spots), bleeding risk, bleeding from gums or nose, blood in urine or stools, fatigue
-
Neutropenia
1. low wbc count
2. wbc range 4.5k-10k
3. CM: fever, chills, sweating, abd pain
4. NI: filgrastim (neupogen) iv or sq
-
Anemia
1. Erythopoietin stimulating agent = epoetin alfa given IV or SQ
-
Mucositis
1. Lining of digestive system becomes inflamed, complication of cancer, often seen as sores in the mouth.
-
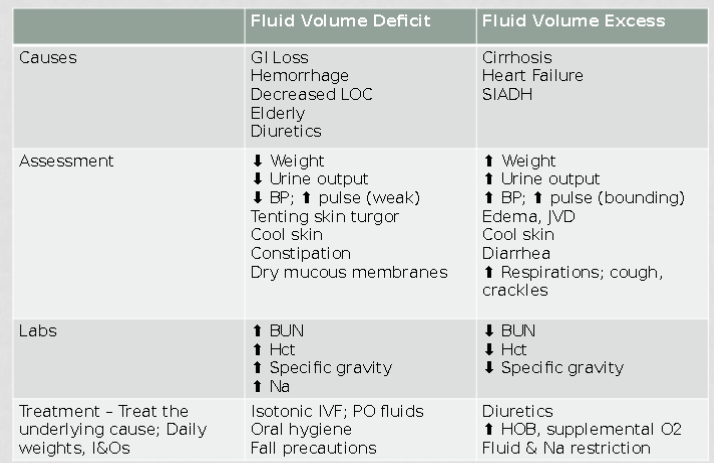
Fluid volume Deficit vs. Fluid Volume Excess
-
Electrolyte Ranges
1. Na = 135-145
2. K = 3.5 - 5
3. Ca = 8.2-10.2
4. Mg = 1.6-2.6
-
Hypocalcemia
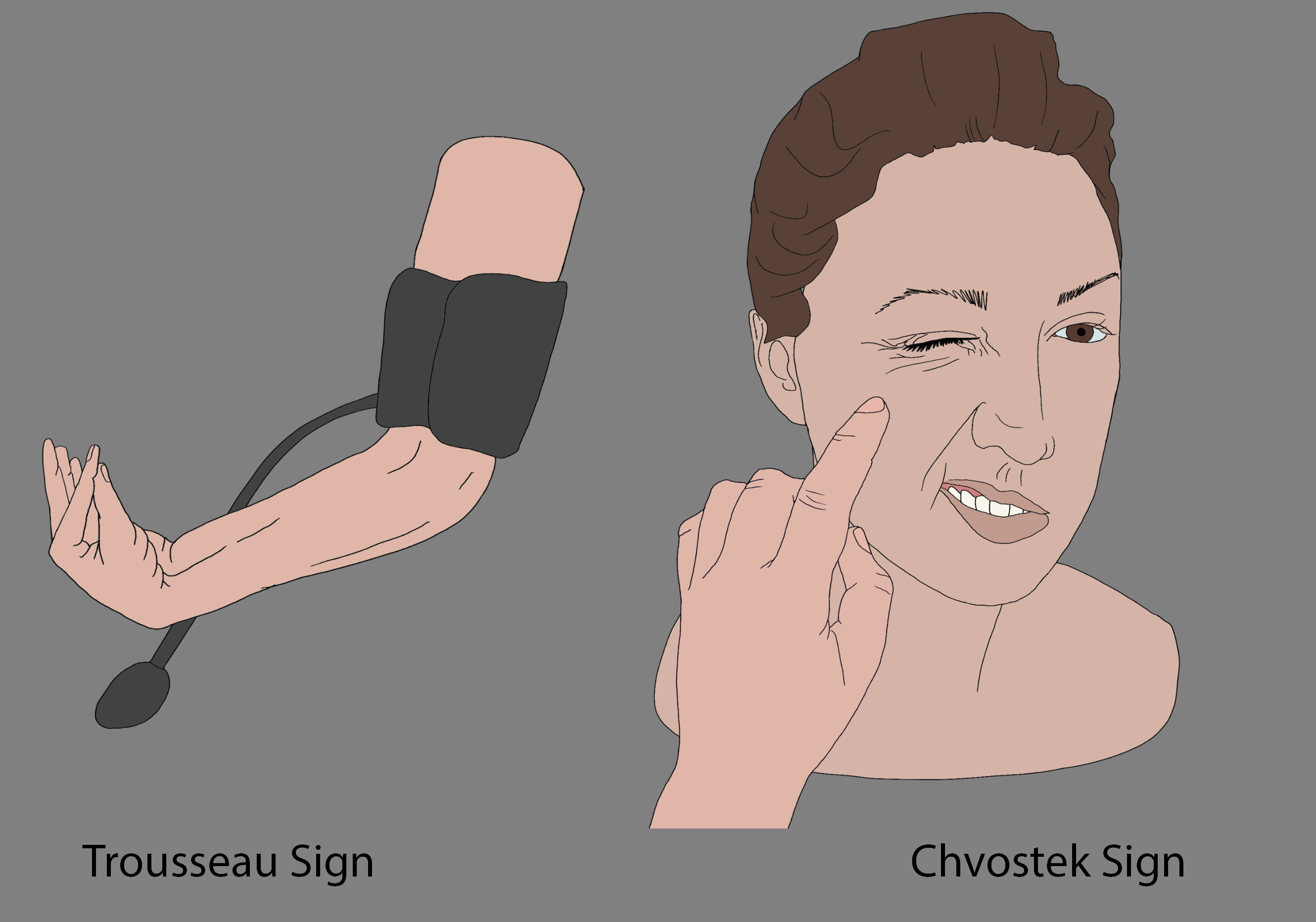
1. Hypocalcemia = hyperexcitable 'al' the alcoholic, alkalotic cow
2. CM: tetany, fractures, diarrhea, Chvostek's and Trousseaus sign, paresthesia's, bronchospasm, Long QT interval
3. Causes: PTH removal, ETOH, malabsorption, alkalosis
4. Priorities: airway, cardiac (ekg), seizures, fracture prevention
5. Tx: dietary, PO, IV
-
Calcium containing foods
1. Cheese, Dairy, Leafy greens, cottage cheese, intake of whole grains, tuna and salmon, milk.
-
Hypercalcemia
1. lots of cows = moving slow/congested, calcium calms
2. Causes: hyper PTH, cancer, sedentariness
3. CM: bradycardia, HTN, blood clots, weak muscles (lots of slow cows), decreased GI motility, lethargy, renal calculi.
4. Priorities: Resp/cardiac monitoring, tissue perfusion, kidney stones (hydration), skeletal fractures.
5. Tx: fluids, dialysis, iv bisphosphates
-
Kidneys excrete
1. Kidneys excrete K and Mg
-
Hypermagnesemia
1. A perm is permanet getting aperm is slow weak, vasodilated, Magnesium mellows
2. Causes: Renal failure
3. CM: resp depression, cardiac arrest (bradycardia), peripheral vasodilation, hypotension, facial flushing, weak muscles, CNS depression drowsy, absent DTRs
4. Priorities: resp arrest, heart block, vasodilation
5. Tx: IVF, dialysis
-
Hypomagnesemia
1. Cheerleaders want to be thin and use pom poms, hyperexcitable
2. Causes: malnutrition, alcoholism
3. CM: tremors/seizures, positive Chvostek's and Trousseau's, HTN, tachycardia
4. Priorities: Airway-spasm, arrhythmias (torsade's de pointes), seizures (tetany), assess DTR
5. Tx: dietary, PO, IV
-
Magnesium containing foods
1. Green leafy vegetables: spinach and broccoli
2. Hailbut
3. peppermint
4. pumpkin, sunflower, and flax seeds
5. Cucumber
6. Cereal, grains
-
Hypokalemia
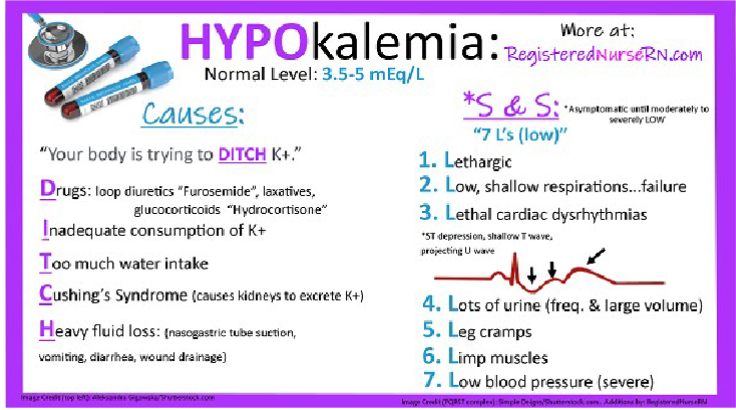
1. Leaky bucket; HyPOKalemia poke holes and cause leak poke someone to wake up slow to wake up.
2. Causes: GI loss, meds (lasix/steroids), surgery, alkalosis
3. CM: weakness/lethargy, n/v, constipation, v-fib, hypotension, muscle cramping
4. Priorities: respiratory, cardiac, fall prevention, iv infusion assessment
-
Potassium foods
1. potatoes
2. oranges
3. tomatoes
4. avocadoes
5. strawberries
6. spinach
7. fish
8. mushrooms
9. melons
-
IV Potassium rules
1. severe tissue irritant
2. never give IM, SC, or IV push
3. Assess IV site hourly
4. Double check concentration
5. Rate is to never exceed 20mEq/hr
6. Dilution is 1mEq of K to 10mL of soln.
7. Use IV pump
8. Use large gauge IV cath for infusion
-
Hyperkalemia
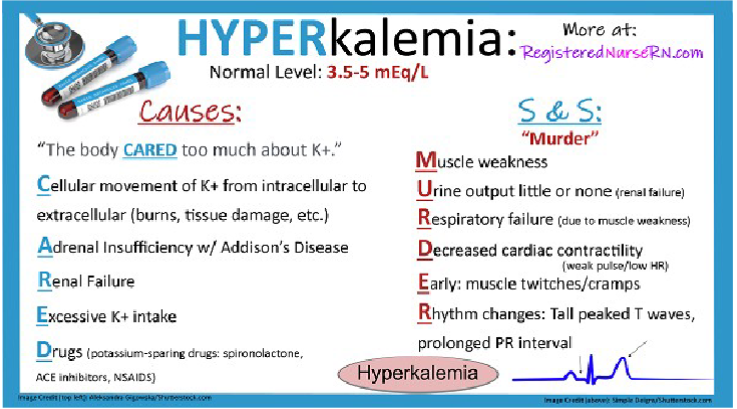
1. All the A's SMART
2. Causes: acidosis, aldactone (htn diuretic), ACEI, addison's, apoptosis(cell death), acute/chronic renal failure
3. SMART = stomach cramps, muscle weakness, asystole, resp fail, tingling (paresthesia)
4. Tx: KIDD, Kayexalate (sodium polystyrene sulfonate), Insulin and glucose, diuretics/dialysis
-
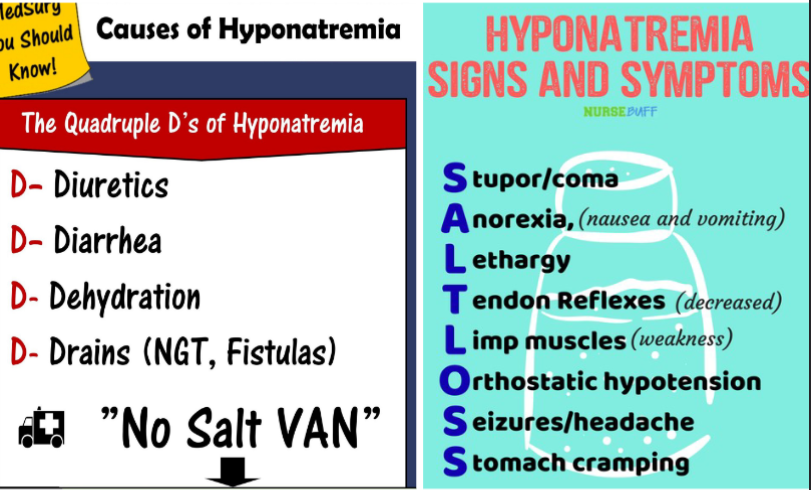
Hyponatermia
-
Hypernatremia
1. SALT, seizure, agitation, low grade fever, thirst
2. Tx: hypotonic fluids given slowly, sodium restriction, seizure precautions, diuretics
-
S/S of malignant hyperthermia
1. Tachycardia
2. muscle rigidity (jaw)
3. dark urine
4. elevated temp
5. cyanosis
6. lactic acidosis
-
Expected Post OP findings
1. Slow return to orientation
2. Electrolyte imbalance
3. Absent bowel sounds
4. Diminished lung sounds in bases
5. Low-grade fever or shivering
6. NG tube drainage
7. Incision drainage and redness
-
Posturing with ICP
1. cause by increase intracranial pressure (ICP)
2. Decortication - abnormal flexion
3. Decerebration - abnormal extension (extend celebrations)
-
Increased ICP
1. Causes: edema, bleeding, neoplasm(cancer tumor)
2. brains response: decreased cerebral blood flow, looses ability to autoregulate, herniation
3. assess for: cushing's, SIADH, perfusion, oxygenation
4. NI: support oxygen, raise HOB, straight body alignment, normal body temp, monitor ICP (5-15), negative fluid balance (get rid of fluids). Avoid coughing and Valsalva maneuver (plug nose)
-
Meningitis
1. Inflammation of the meninges
2. Can be septic or aseptic
3. Lots of different causes of septic meningitis - bacterial, viral ,parasitic, fungal
4. Common symptoms: fever, nuchal rigidity, HA, photophobia, n/v
-
Testing for meningitis
1. lumbar puncture: volume, pressure, specific gravity=1.007, color=clear, glucose=2/3 serum, protein=15-50, blood=none.
2. Kernigs (extend knee, extending head) and Brudzinkis (knee flex, head tilt up)
-
Bacterial vs. Viral Meningitis
1. Bacterial meningitis: deadly, immediate medical attention. Caused by streptococcus pneumoniae. Risk in babies and college dorms. S/s: HA, fever, photophobia, altered LOC, nuchal rigidity, brudzinki/kernig sign
2. Viral Meningitis: less severe, pts get better on their own. Cause: measles, mumps, herpes, non-polio enterovirus. Risks in children and weakened immune system. S/s: fever, HA, photohobias, n/v, , myalgias (muscle aches)
-
Meningitis nursing assessment and interventions
1. neurological assessment
2. vital signs
3. iv fluids
4. antibiotics if bacterial
5. HOB > 30 degrees
6. droplet precautions
7. decrease environmental stimuli
8. prevention: vaccinations
-
Encephalopathy
1. inflammation of the brain
2. high sudden fever, severe HA, photophobia, nuchal rigidity, altered LOC, weakness, motor dysfunction, seizures
3. antivirals
4. seizure precautions, hob 30-45, quiet environment, reposition q2 turns, stool softners, anticonvulsants, similar to meningitis.
-
Is it meningitis or encphalitis?
1. Most frequently caused by bacteria Meningitis2. Is an inflammation of the brain Encephalitis3. May be transmitted by insect vectors Encephalitis4. CSF pressure is increased Meningitis5. Almost always has a viral cause Encephalitis6. Cerebral edema is a major problem Encephalitis7. Inflammation of the meninges Meningitis8. Can start with a blood infection Meningitis
MH
-
Peripheral Neuropathy
1. Damage to the nerves outside the CNS, often in hands and feet
2. caused by: autoimmune disease, diabetes, infection
3. s/s: numbness, pain, weakness, digestion, urination, and circulation issues
4. NI: safety, pain assessment/control, skin assessment, injury prevention, encourage healthy lifestyle
-
Seizure diagnostic tests
1. Neuro exam
2. blood tests: glucose, s/s of infection, genetics, electrolyte imbalances
3. EEG (electrocochleogram): stay awake the night before, detects abnormal brain waives
-
Tonic clonic seizures
1. classic types of generalized seizure that is characterized by muscle rigidity (tonic phase), violent rhythmic muscle contractions (clonic phase) with uncontrolled jerking and loss of consciousness.
-
Nursing care for seizures
1. note the time
2. observe moments
3. airway
4. nothing in mouth
5. safety
6. suction ready
7. call for help
8. do not restrain
9. privacy
10. side lying
11. After the seizure: turn pt on side, suction as needed, allow to rest, assess for injury, document
-
Status epilepticus
1. seizure lasting longer than 30 minutes
2. ABCs
3. intubation
4. iv access
5. lorazepam (ativan) or midazolam (versed)
6. phenytoin (dilantin) or levetiracetam (keppra)
7. ekg and EEG monitoring
8. causes: epilepsy, cerebral damage, brain tumor, electrolyte abnormalities, drug/alcohol overdose or withdraw, encephalitis.
-
Meds given during a seizure
1. Benzos, Carbamazepines, levetiratams, phenytoin, valproic acid.
2. Long acting: maintain therapeutic levels, takes a few weeks
-
Nonsurgical management for seizures
1. antiepileptic drugs (aeds)
2. keto diet
3. importance of compliance
4. seizure dogs
5. wear med id, teach family to help, follow state law driving, avoid alcohol, dont stop meds abruptly, stress reduction
-
Stroke
1. CVA
2. types: hemorrhagic(bleed), ischemic (blood clot), transient ischemic attack (TIA)
3. RF for age >55, women and black
4. 15% hemorrhagic strokes, 85% ischemic strokes
5. Preventable RF: smoking, obesity, meds, heart disease, physicial inactivity, stress, alcohol, high BP, diabetes, high blood cholesterol
6. Nonpreventable RF: race(blacks+asians+hispanics), previous stroke, family history, afib, autoimmune disorders, clotting disorders
-
Diagnosing a stroke
1. FAST: facial droop, arm weakness, slurred speach, time counts
2. NIH Stroke Scale: objectively quantify the impairment.
3. CT scan
-
Acute stroke Management
1. rapid resposne team / met team
2. vs - especially oxygen, blood glucose, iv acess, neuro exam, time last well known, ct, meds
-
Hemorrhagic stroke
1. intracranial hemorrhage: ateriovenous malformation (avm), tumors, aneurysm
2. subdural hemorrhage: trauma, fall car accident ,etc
2. Tx: manage HTN, seizure precautions, stop bleed, surgical management
-
Ischemic stroke
1. origin of blood clots: cardiac from afib, malfunctioning valves, patent foramen ovale, arterial dissection
2. Cholesterol origin cause: damage to blood vessels, cholesterol is nature's band aid, cracked plaques can create a blood clot
3. Ischemic cva tx: fibrinolytics, cerebral angioplasty, carotid endarterectomy
4. medical management use tPa, fibrinolytic, powerful anticoagulant, only for ischemic stroke, must be given in 4 hour window
5. medical management of HTN: betablockers, diuretics, ace inhibitors, angiotensin II receptor blockers, calcium channel blockers, alphafs;lkdf
-
Blood pressure control
1. Ischemic strokes - higher BP: 180/105 after TPA, 200/120 with no TPA
2. hemorrhagic strokes - lower BP, don't lower too fast or too low, aim for normal range
-
Common effects of stroke
1. Left Sided: weak on right side, language/speech impairment, spatial orientation
2. Right sided: weak on left side, vision issues, impulsive, difficulty recognizing impairment
-
Stroke deficit words
1. hemianopsia = blind in half vision
2. agnosia = inability to recognize objects/sounds/people
3. dysarthria = impairment of muscles that control speech
4. apraxia = inability to carry out purposeful movement
-
Common meds after strokes
1. anticoagulants: warfarin
2. antiplatelet: aspirin, clopidogrel
3. drugs to treat underlying risk factors: antihyperlipidemic(cholesterol), drugs to control diabetes, antihypertensives

