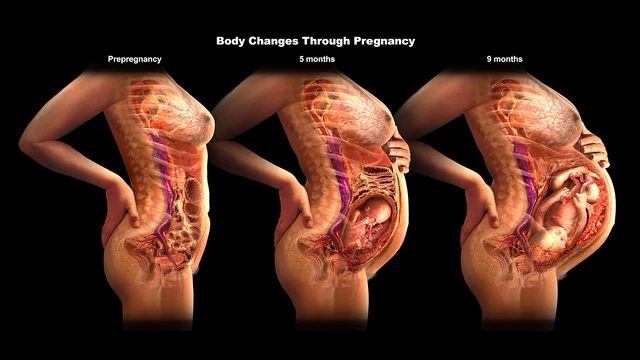
Maternal Changes in Pregnancy (Physiology 2)
Maternal changes in pregnancy - Dr David Gillott Session introduction This lecture will cover the normal physiological changes that occur in human pregnancy from start to finish in multiple body systems. It will describe the hormonal, vascular and physical reasons why the changes take place and what advantages that offers to the mother and foetus. It will also explain why women experience some common symptoms whilst pregnant. The lecture also briefly covers some examples where these physiological changes lead to an abnormal adaptation and disease state. Learning Outcomes At the end of this lecture unit, you will be able to: Describe the normal physiological changes that occur in human pregnancy to the following systems: cardio-vascular, respiratory, haematological, metabolic, uro-genital and renal tract. Explain the hormonal, vascular and physical reasons why these changes occur. Describe the positive effects for mother and foetus for these adaptations and link this to some of the common pregnancy symptoms. Outline abnormal physiological adaption to explain why some women develop gestational diabetes and pre-eclampsia Session resources Powerpoint slides: Maternal changes in pregnancy 2024-25 Dr David Gillott.pptxDownload Maternal changes in pregnancy 2024-25 Dr David Gillott.pptx Panopto recording: Some questions to think about... 1. What changes occur in cardiac output, total peripheral resistance and blood pressure during pregnancy? 2. Why are pregnant women more prone to developing varicose veins and oedema, especially in the lower extremities? 3. What changes occur in respiratory rate and tidal volume during pregnancy, and what is their purpose? 4. What causes the common symptoms of heartburn and acid reflux during pregnancy? 5. What is the role of the placenta in hormone production? 6. How does insulin resistance change during pregnancy, and what role does it play in providing energy to the mother and foetus? 7. What are the key physiological changes in pregnancy that make diagnosing conditions like preeclampsia and gestational diabetes challenging?
-
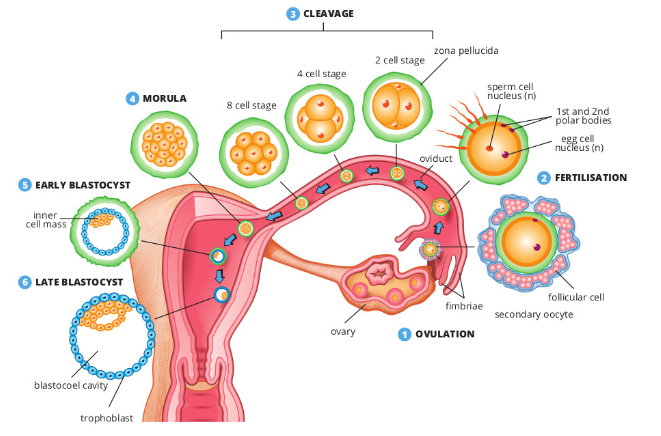
Picture demonstrating the process of egg fertilisation and implantation:
-
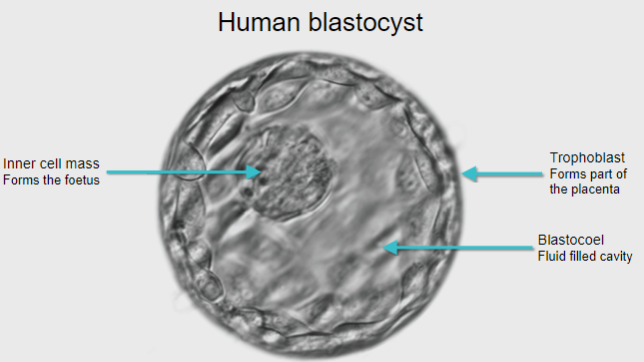
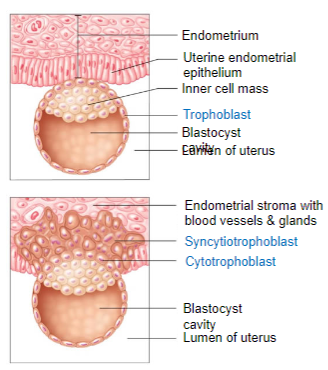
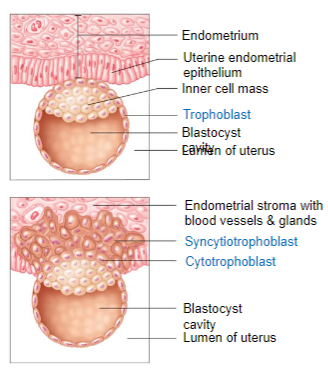
Picture demonstrating a Human blastocyst:
-
What is the implantation window and when does it occur? (1)
The implantation window occurs 6 to 10 days after the LH spike.
-
What is pre-decidualization and what happens to endometrial cells during this phase? (2)
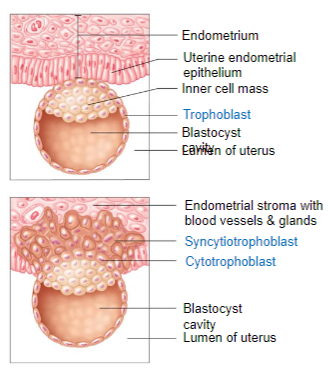
Pre-decidualization occurs during the implantation window.
Endometrial cells become modified, filled with lipids and glycogen, and cover the surface of the uterus.
-
What is the role of these modified endometrial cells if pregnancy occurs? (1)
These modified cells become the maternal contribution to the placenta if pregnancy occurs.
-
What do the glandular secretions of the endometrium contain? (4)
Growth factors
Adhesion molecules
Nutrients
Vitamins, matrix proteins, and hormones
-
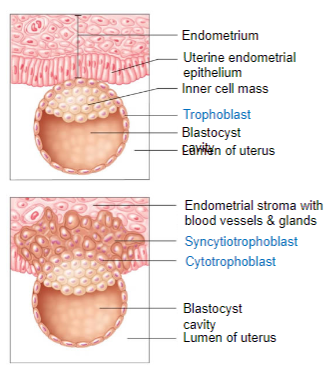
What is the syncytiotrophoblast and how does it form? (2)
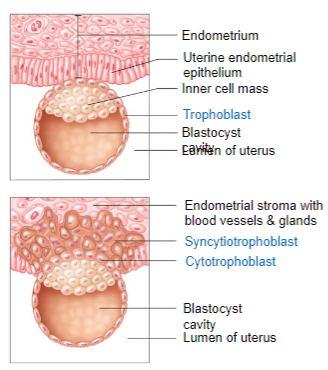
The syncytiotrophoblast is formed by cell fusion, creating a multi-nucleated cytoplasmic mass.
It invades the endometrium.
-
What happens on day 7-8 during implantation? (2)
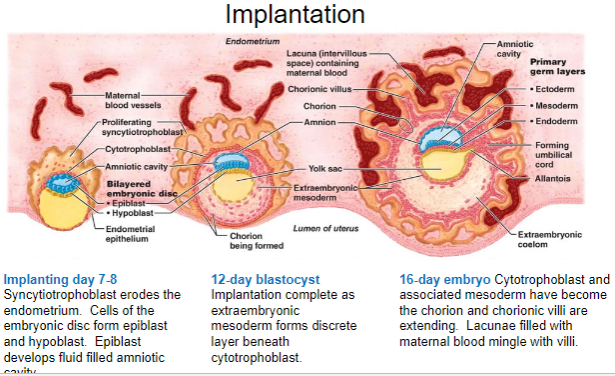
The syncytiotrophoblast erodes the endometrium.
Cells of the embryonic disc form epiblast and hypoblast.
-
What does the epiblast develop into on day 7-8? (1)
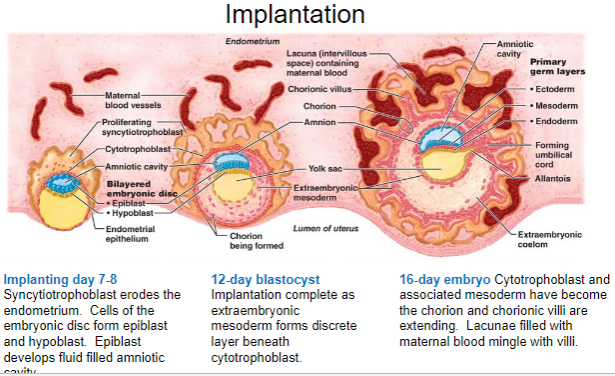
The epiblast develops a fluid-filled amniotic cavity.
-
What happens on day 12 of implantation? (2)
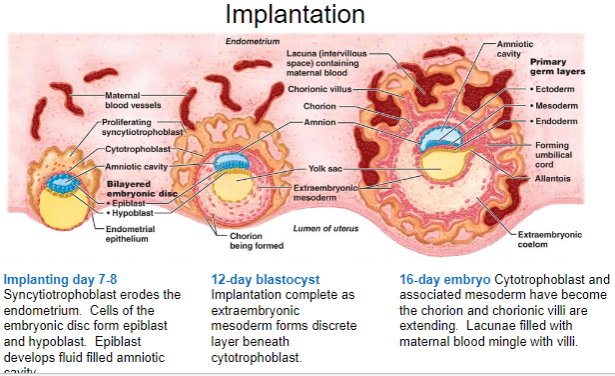
Implantation is complete as the extraembryonic mesoderm forms a discrete layer beneath the cytotrophoblast.
The blastocyst is at the 12-day stage.
-
What occurs on day 16 of embryo development? (3)
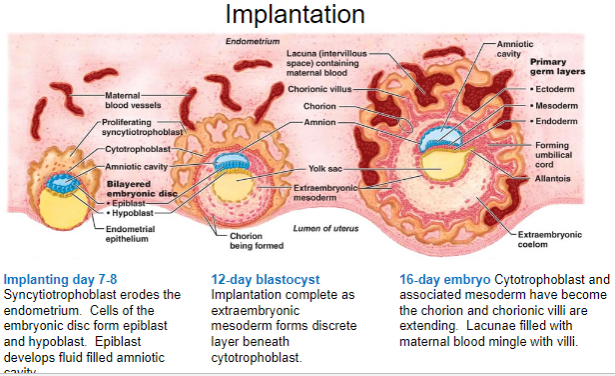
The cytotrophoblast and associated mesoderm form the chorion.
The chorionic villi begin to extend.
Lacunae fill with maternal blood, which mingles with the villi.
-
What is the maternal-fetal interface and its role? (3)
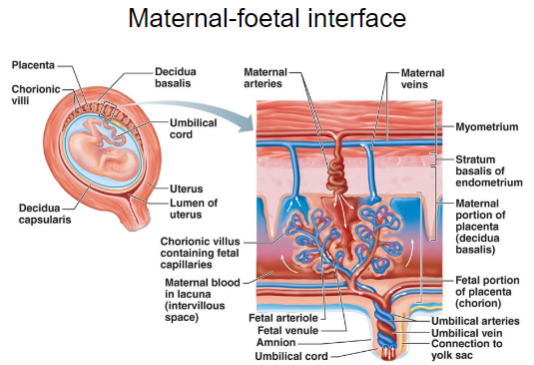
The maternal-fetal interface refers to the area where the maternal and fetal tissues meet, facilitating nutrient and gas exchange.
It consists of the placenta, which serves as a barrier between the mother and fetus.
The interface is responsible for the exchange of oxygen, nutrients, waste, and hormones between the maternal and fetal circulations.
-
What is maternal recognition of pregnancy and how does it occur? (3)
Human chorionic gonadotrophin (hCG) is secreted by the syncytiotrophoblast and increases rapidly during pregnancy.
hCG binds to LH receptors to prevent the death of the corpus luteum, ensuring continued production of estrogen and progesterone.
This hormonal shift triggers rapid changes in maternal systems in response to luteal and later placental steroids.
-
What is the significance of serum hCG levels during pregnancy? (2)
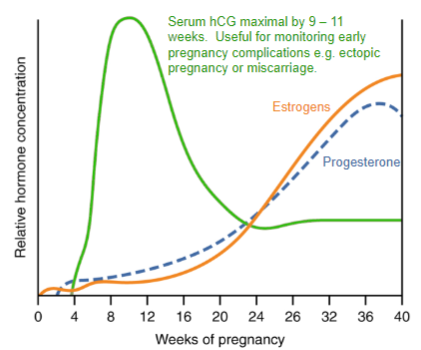
Serum hCG levels are maximal between 9 and 11 weeks of pregnancy.
hCG is useful for monitoring early pregnancy complications, such as ectopic pregnancy or miscarriage.
-
What is placental steroidogenesis and its significance? (5)
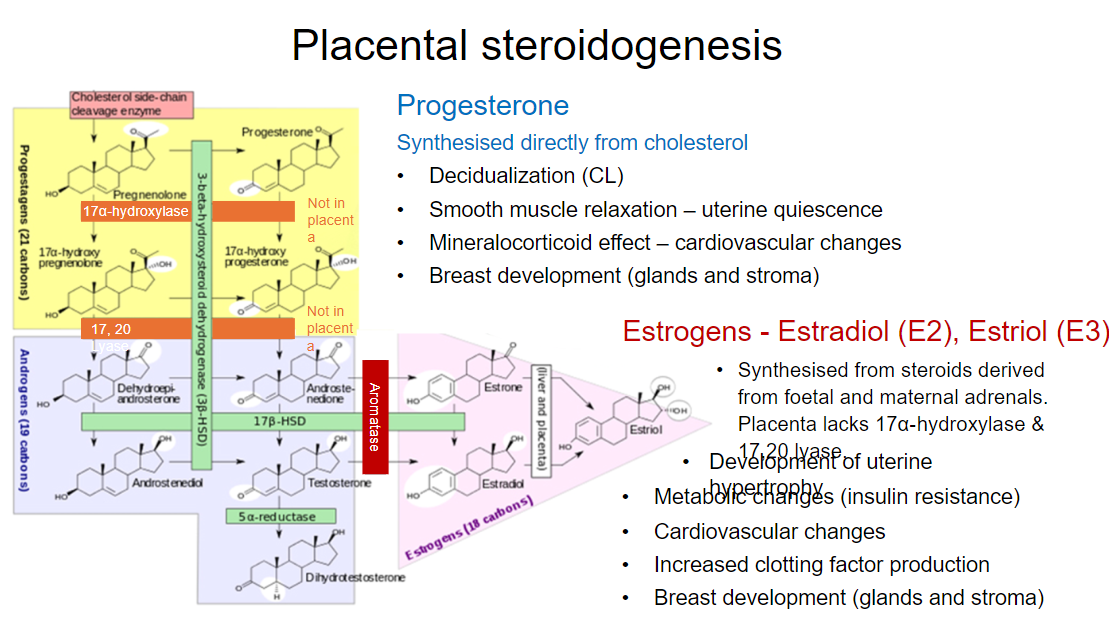
Placental steroidogenesis is the synthesis of steroids derived from fetal and maternal adrenals.
The placenta lacks 17α-hydroxylase and 17,20 lyase enzymes.
Progesterone:
Synthesized directly from cholesterol.
Responsible for decidualization, smooth muscle relaxation, mineralocorticoid effects, and breast development.
Estrogens (Estradiol and Estriol):
Contribute to uterine hypertrophy, metabolic changes, cardiovascular effects, increased clotting factor production, and breast development.
-
What is the average total weight gain during pregnancy and its components? (5)
Total weight gain: 9-13 kg
Foetus and placenta: 5 kg
Fat and protein: 4.5 kg
Body water: 1.5 kg
Breasts: 1 kg
Uterus: 0.5-1 kg
-
How is weight gain distributed during pregnancy? (4)
Approximately 2.0 kg in the first 20 weeks.
Then, weight gain continues at about 0.5 kg per week until full term at 40 weeks.
Total weight gain during pregnancy: 9-13 kg.
Failure to gain or sudden changes in weight should be investigated.
-
What are the psychological considerations regarding weight monitoring during pregnancy? (2)
Constant weight monitoring can cause anxiety.
Weight gain failure or sudden changes require investigation.
-
How does basal metabolic rate (BMR) change during pregnancy? (2)
BMR rises by 350 kcal/day during mid gestation.
BMR rises by 250 kcal/day during late gestation.
-
How is the increased caloric expenditure during pregnancy distributed? (2)
75% of the increased caloric expenditure goes to the foetus and uterus.
25% is used for respiration.
-
How does glucose transfer to the foetus during pregnancy? (2)
Glucose is transported across the placenta to provide foetal energy.
Increased blood glucose levels occur during the 2nd trimester.
-
What happens to maternal glucose regulation during the first trimester? (3)
Maternal reserves are primarily used for energy.
Pancreatic cells increase in number, raising circulating insulin.
Fasting serum glucose decreases as more glucose is taken up into tissues.
-
What happens to maternal glucose regulation during the second trimester? (3)
Foetal reserves are emphasized for energy.
Placental lactogen causes insulin resistance, meaning less glucose is stored.
This leads to an increase in serum glucose in the mother.
-
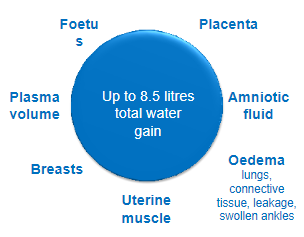
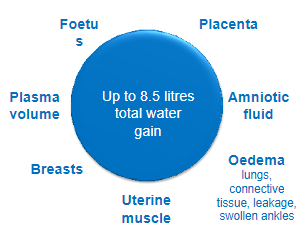
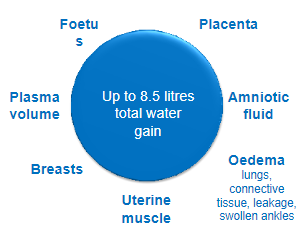
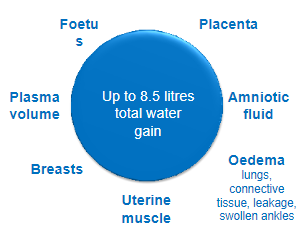
What contributes to total water gain during pregnancy? (7)
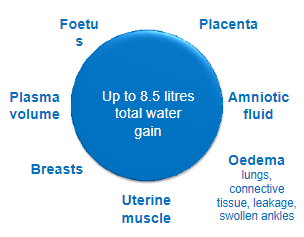
Foetus
Placenta
Amniotic fluid
Oedema (swollen ankles, connective tissue, lungs)
Uterine muscle
Breasts
Plasma volume
-
How do estrogen and progesterone affect water retention during pregnancy? (4)
Estrogen and progesterone act like mineralocorticoids, causing increased sodium retention by the kidneys.
This leads to an increase in blood volume.
RAAS: Placental renin production and angiotensinogen synthesis by the liver increase.
Angiotensin II and aldosterone are elevated.
-
What are the effects of progesterone on vasoconstriction during pregnancy? (2)
Progesterone decreases vaso-sensitivity, leading to resistance to AT2 receptor-mediated vasoconstriction, despite higher levels of angiotensin II.
-
How do connective tissue and ligaments change during pregnancy? (2)
Connective tissue and ligaments take on water, becoming softer.
-
What is the effect of pregnancy on thirst and oncotic pressure? (2)
Resetting of the osmostat decreases the thirst threshold.
Decrease in oncotic pressure (due to lower albumin levels).
-
What is the total water gain during pregnancy? (1)
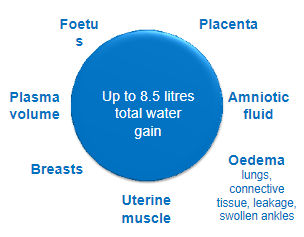
Up to 8.5 liters of total water gain.
-
Picture demonstrating how oxygen consumption has increased:
-
How does pregnancy affect iron absorption and blood volume? (2)
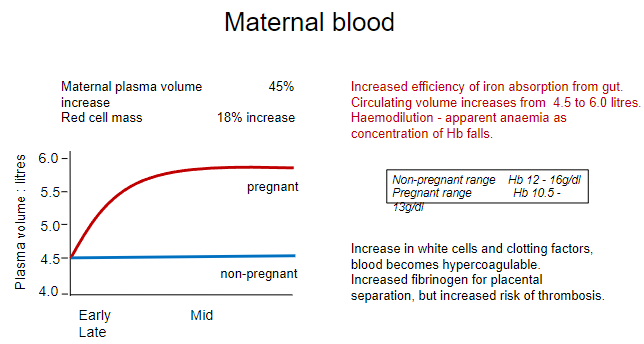
Increased efficiency of iron absorption from the gut to meet maternal and fetal needs.
Circulating blood volume increases from 4.5 to 6.0 liters.
-
What is haemodilution during pregnancy? (2)
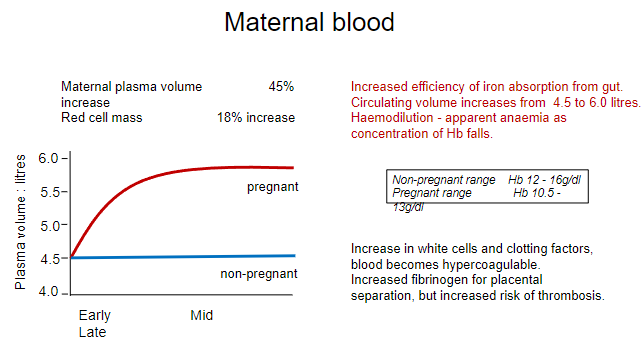
Haemodilution refers to the apparent anaemia that occurs as the concentration of hemoglobin (Hb) falls, due to the increase in plasma volume.
-
What changes occur in the blood during pregnancy? (3)
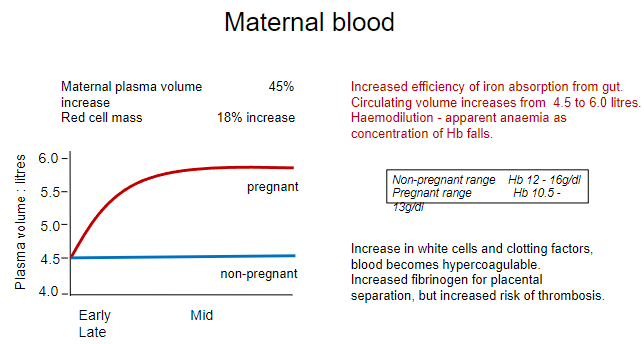
Increase in white blood cells and clotting factors.
Blood becomes hypercoagulable, increasing the risk of clot formation.
Increase in fibrinogen is essential for placental separation, but also raises the risk of thrombosis.
-
How does the expanding uterus affect the cardiovascular system during pregnancy? (2)

The expanding uterus can put pressure on the heart, potentially altering ECG and heart sounds.
Peripheral vasodilation occurs due to progesterone reducing smooth muscle intracellular calcium and estrogen inducing NO synthase in vascular endothelium.
-
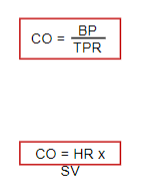
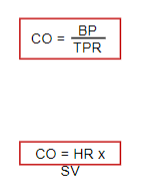
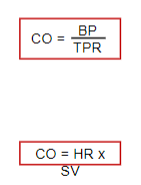
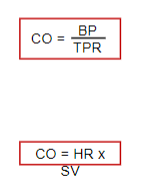
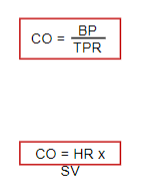
What happens to total peripheral resistance (TPR) and cardiac output (CO) during pregnancy? (2)
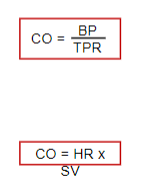
Total peripheral resistance (TPR) falls by 20-30%.
Cardiac output (CO) increases, leading to a slight decrease in blood pressure (BP) during the first two trimesters.
-
What changes occur in cardiac function during pregnancy? (2)
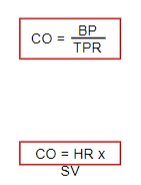
There is an increase in cardiac output, with stroke volume and heart rate rising, reaching a maximum of 40% at 28 weeks.
These changes begin as early as 3 weeks into pregnancy.
-
How can increased cardiac output affect pre-existing conditions during pregnancy? (1)
Increased cardiac output can exacerbate pre-existing conditions, such as aortic valve defects or pulmonary hypertension
-
How does pregnancy affect cardiac output and peripheral resistance in vessels? (2)
Increased cardiac output and vasodilation are induced by steroids.
This leads to reduced peripheral resistance and increased blood flow to key organs.
-
What organs receive increased blood flow during pregnancy? (5)
Uterus
Placenta
Muscle
Kidneys
Skin
-
What is neoangiogenesis and how does it occur in pregnancy? (2)
Neoangiogenesis refers to the formation of new blood vessels.
This includes the development of extra capillaries in the skin, resulting in spider naevi, which assist with heat loss.
-
What characterizes the cardiovascular system during pregnancy? (2)
Pregnancy is characterized by low blood pressure and high blood volume.
-
How does progesterone affect the gastrointestinal (GI) tract during pregnancy? (2)
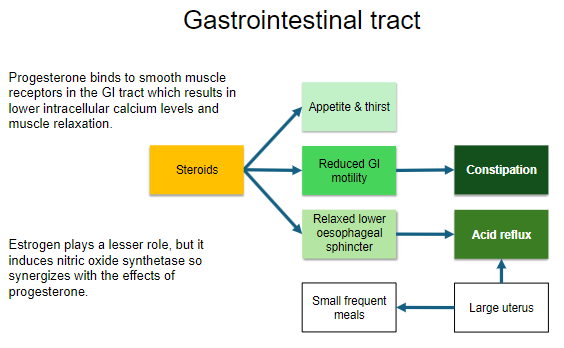
Progesterone binds to smooth muscle receptors in the GI tract, resulting in lower intracellular calcium levels.
This leads to muscle relaxation in the GI tract.
-
What role does estrogen play in the gastrointestinal tract during pregnancy? (2)
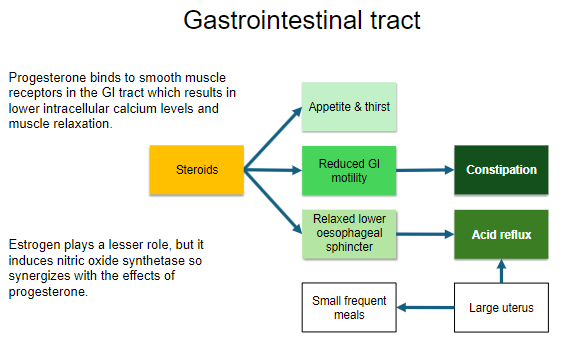
Estrogen plays a lesser role compared to progesterone.
It induces nitric oxide synthetase, which synergizes with progesterone's effects on the GI tract.
-
What is the role of folic acid during pregnancy? (3)
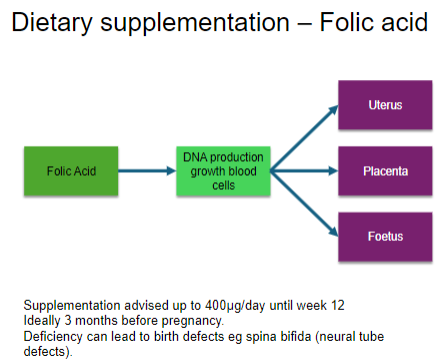
DNA production and growth of blood cells.
Supports the foetus, placenta, and uterus.
Essential for the proper development of the neural tube.
-
When is folic acid supplementation advised and why? (3)
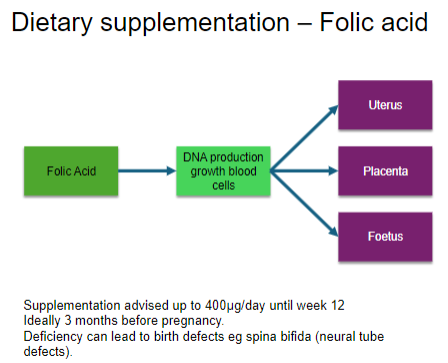
Supplementation is advised up to 400μg/day until week 12 of pregnancy.
Ideally, supplementation should start 3 months before pregnancy.
Deficiency can lead to birth defects, such as spina bifida and other neural tube defects.
-
How does relaxin and progesterone affect the urinary system during pregnancy? (4)
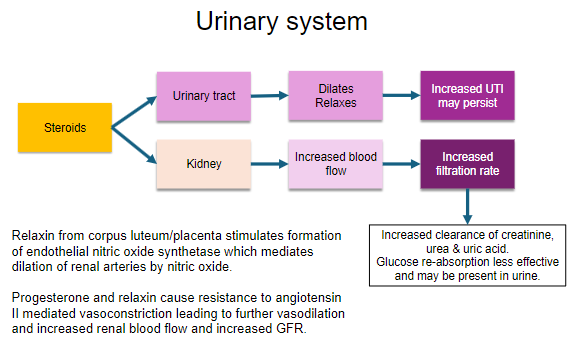
Relaxin from the corpus luteum/placenta stimulates the formation of endothelial nitric oxide synthetase.
This enzyme mediates the dilation of renal arteries through nitric oxide.
Progesterone and relaxin cause resistance to angiotensin II-mediated vasoconstriction, leading to further vasodilation.
These changes increase renal blood flow and glomerular filtration rate (GFR).
-
What is the role of placental CRH in pregnancy? (1)
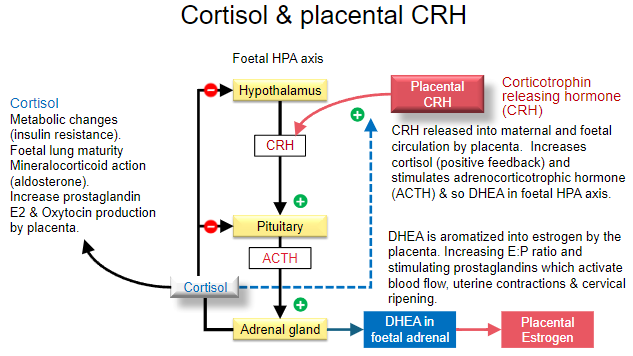
Placental CRH is released into both maternal and foetal circulation.
-
How does placental CRH affect cortisol levels in pregnancy? (1)
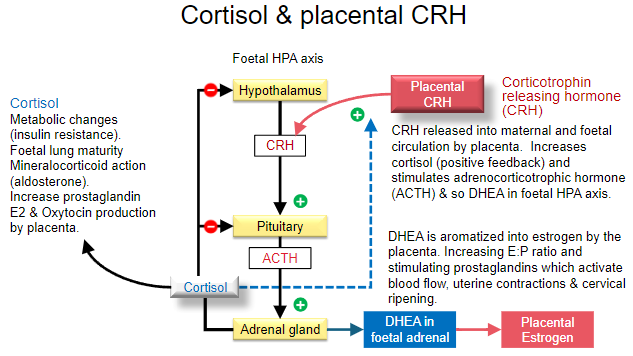
Placental CRH stimulates the release of cortisol through a positive feedback mechanism.
-
What is the role of cortisol in pregnancy? (2)
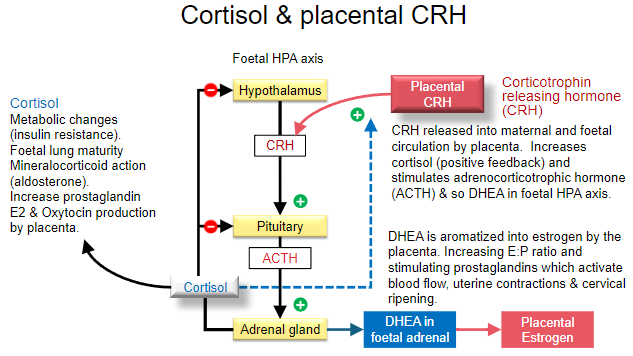
Cortisol causes metabolic changes, such as insulin resistance, in the mother.
Cortisol promotes foetal lung maturity and has mineralocorticoid actions (similar to aldosterone).
-
How does cortisol affect prostaglandin and oxytocin production during pregnancy? (1)
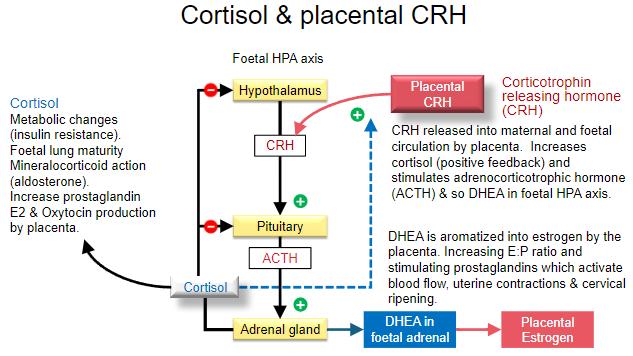
Cortisol increases the production of prostaglandin E2 and oxytocin by the placenta.
-
What is the role of DHEA in pregnancy? (1)
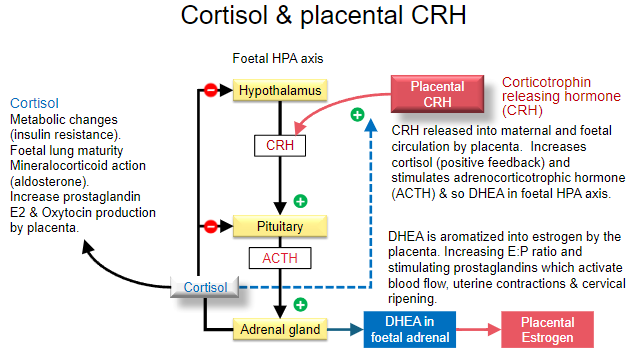
DHEA, produced in the foetal adrenal glands, is aromatized into estrogen by the placenta.
-
How does the estrogen-to-progesterone ratio affect pregnancy? (1)

The increase in the estrogen-to-progesterone (E:P) ratio stimulates the production of prostaglandins, which enhance blood flow, uterine contractions, and cervical ripening.
-
What should be considered if a patient has a history of hyperthyroidism, such as Graves' disease, during pregnancy? (1)
The patient may require endocrine management to maintain normal thyroid function.
-
Why can biochemical tests sometimes indicate hyperthyroidism during pregnancy, and what could it mean? (1)
Biochemical tests may indicate hyperthyroidism, but the patient may actually be normal, particularly in the case of gestational thyrotoxicosis.
-
What symptoms may indicate hyperthyroidism in pregnancy? (6)
Anxiety
Tremor
Heat intolerance
Palpitations
Weight loss or lack of weight gain
Goiter, tachycardia, and hyperreflexia (often associated with hyperemesis gravidarum).
-
What laboratory findings may indicate gestational thyrotoxicosis? (2)
Suppressed TSH and high serum T4.
-
How does pregnancy influence thyroid hormone production? (1)

Increased thyroid hormone production to meet the increased metabolic demand of pregnancy may lead to gestational thyrotoxicosis.
-
How can hCG affect thyroid function during pregnancy? (1)
hCG may act on the TSH receptor, leading to increased thyroid hormone production.
-
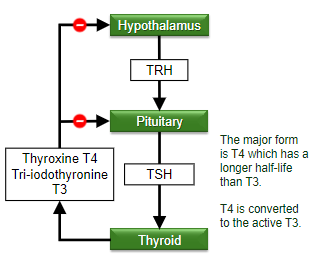
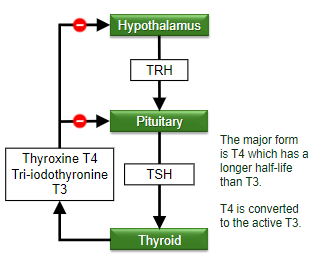
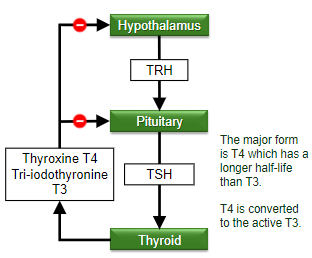
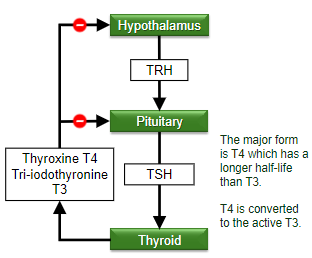
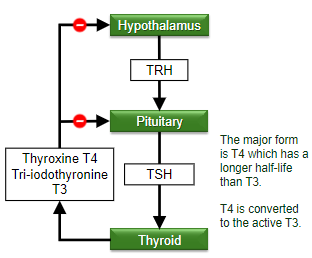
What is the major form of thyroid hormone in the body during pregnancy, and how is it converted? (2)
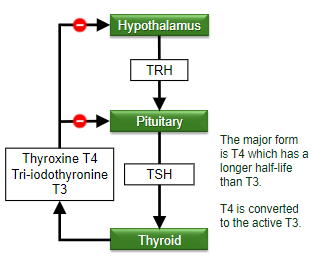
T4 is the major form, and it has a longer half-life than T3.
T4 is converted to the active form, T3.
-
What is the thyroid hormone pathway starting from the hypothalamus? (3)
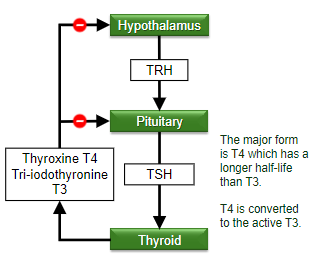
The hypothalamus releases TRH, which stimulates the pituitary to release TSH, leading to the production of T4 and T3 by the thyroid.
-
What is the increase in muscle mass of the uterus during the first 20 weeks of pregnancy? (1)
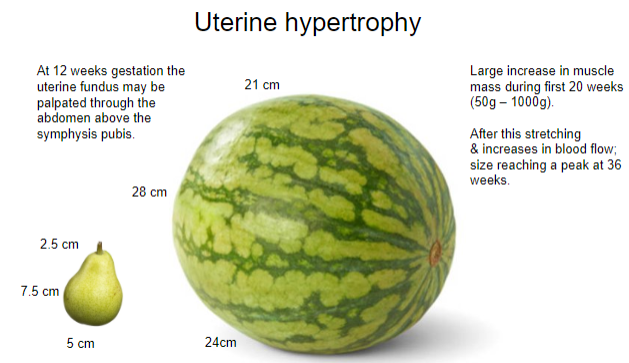
There is a large increase in muscle mass during the first 20 weeks, ranging from 50g to 1000g.
-
What is the size of the uterus at 12 weeks gestation? (1)
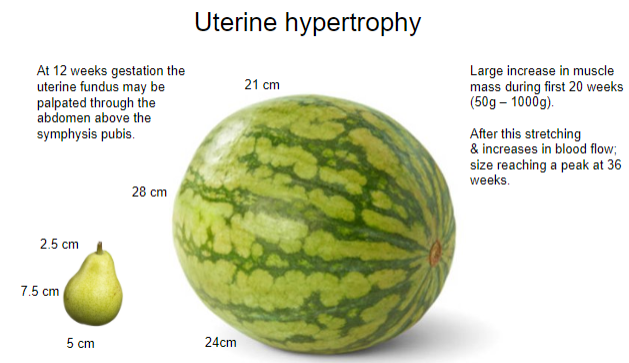
At 12 weeks, the uterine fundus may be palpated through the abdomen above the symphysis pubis.
-
When does the uterus reach its peak size during pregnancy? (1)
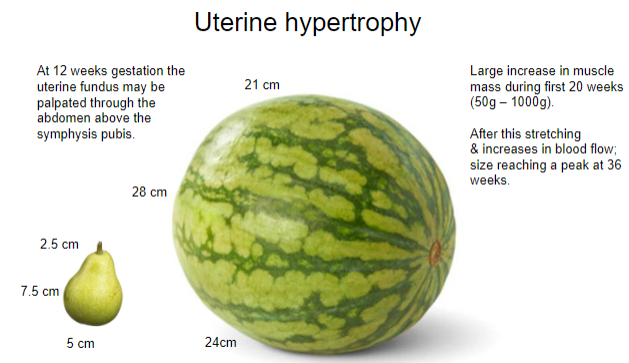
The uterus reaches its peak size at 36 weeks.
-
What are the factors contributing to uterine growth after the first 20 weeks? (2)
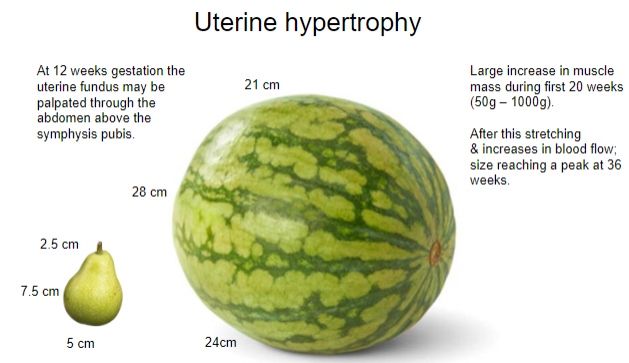
Stretching
Increased blood flow
-
What is the primary function of the cervix during pregnancy? (1)
The primary function of the cervix is to retain the pregnancy.
-
When does tissue softening of the cervix begin during pregnancy? (1)
Tissue softening of the cervix begins at 8 weeks.
-
What changes occur in the cervix's connective tissue during pregnancy? (1)
There are changes in connective tissue that prepare the cervix for expansion.
-
What happens to the cervix's glands during pregnancy? (1)
There is proliferation of glands, and the mucosal layer becomes half of the cervix's mass.
-
What effect does pregnancy have on mucus production in the cervix? (1)
There is a great increase in mucus production, which serves a protective (anti-infective) role.
-
What are the sources of prolactin production during pregnancy? (2)
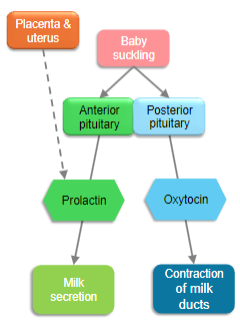
Pituitary
Myometrium
Placenta
-
How do sex steroids affect prolactin's role in milk production during pregnancy? (1)
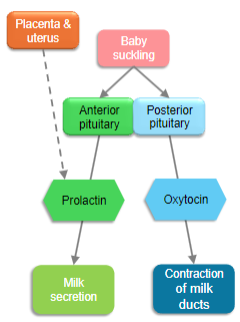
Sex steroids inhibit the stimulatory effects of prolactin on milk production.
-
What causes lactation to begin after birth? (1)
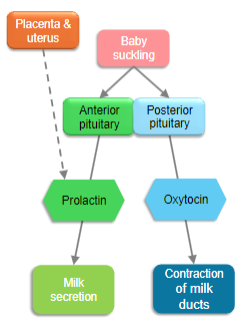
The abrupt drop in steroid levels following placental delivery allows existing prolactin to induce lactation.
-
How does suckling affect prolactin secretion after birth? (1)
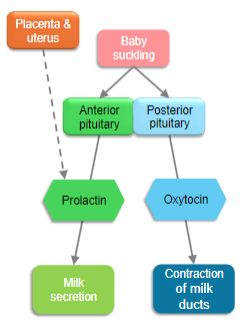
Suckling activates nipple mechanoreceptors, signaling the hypothalamus and causing anterior pituitary prolactin secretion.
-
What causes the release of oxytocin during childbirth? (1)
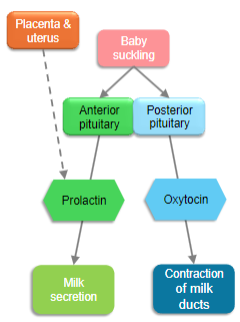
Stretching of the uterus and cervix during childbirth causes the release of oxytocin.
-
How does oxytocin contribute to childbirth and bonding? (2)
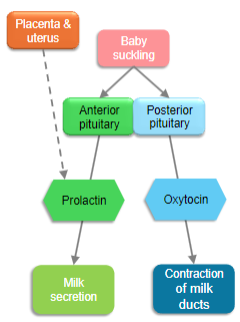
Oxytocin helps with birth and plays a role in emotional bonding with the baby.
-
How is milk ejection triggered after birth? (1)
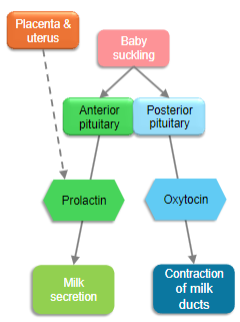
Suckling stimulus triggers the release of oxytocin from the posterior pituitary gland, leading to milk ejection.
-
What is the primary role of prolactin and oxytocin in milk production? (2)
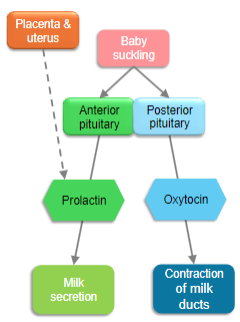
Prolactin controls milk production.
Oxytocin controls the milk-ejection reflex.
-
What happens to steroid levels after the delivery of the placenta? (1)
There is a dramatic and rapid fall in steroids upon delivery of the placenta.
-
How do most endocrine-driven changes return after delivery? (1)
Most endocrine-driven changes return to normal rapidly.
-
What happens to the uterine muscle after delivery? (2)
Uterine muscle rapidly loses oedema but contracts slowly.
However, it does not return to pre-pregnancy size.
-
What effect does the removal of steroids have on prolactin? (1)
The removal of steroids allows the action of raised prolactin on milk production.
-
What changes occur in cardiac output, total peripheral resistance, and blood pressure during pregnancy? (3)
Cardiac output (CO) increases by 30-40% due to increased stroke volume and heart rate.
Total peripheral resistance (TPR) decreases by 20-30% due to vasodilation.
Blood pressure (BP) slightly decreases in the first two trimesters but may return to baseline levels by the third trimester.
-
Why are pregnant women more prone to developing varicose veins and oedema, especially in the lower extremities? (2)
Increased blood volume and pressure from the growing uterus can lead to poor venous return, contributing to varicose veins and oedema, especially in the legs.
Hormonal changes, such as increased progesterone, cause relaxation of smooth muscle in blood vessels, further exacerbating venous pooling.
-
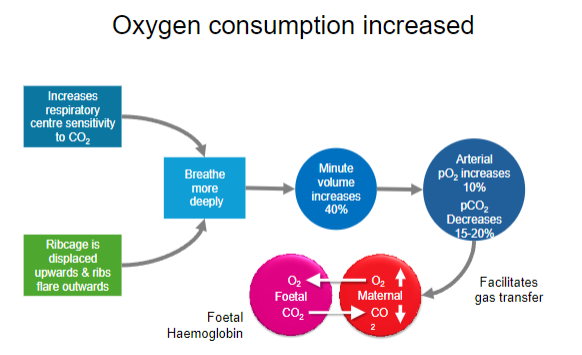
What changes occur in respiratory rate and tidal volume during pregnancy, and what is their purpose? (3)
Tidal volume increases by 30-40%, allowing for greater lung expansion.
Respiratory rate may remain the same or slightly increase.
These changes improve oxygenation for both the mother and foetus and help meet the increased metabolic demands during pregnancy.
-
What causes the common symptoms of heartburn and acid reflux during pregnancy? (2)
Progesterone relaxes the lower oesophageal sphincter, allowing stomach acid to reflux into the oesophagus.
The growing uterus applies pressure on the stomach, further contributing to acid reflux and heartburn.
-
What is the role of the placenta in hormone production? (2)
The placenta produces human chorionic gonadotropin (hCG), progesterone, and estrogen to support pregnancy.
It also plays a role in synthesizing placental lactogen and corticotropin-releasing hormone (CRH), which regulate metabolic and immune responses during pregnancy.
-
How does insulin resistance change during pregnancy, and what role does it play in providing energy to the mother and foetus? (3)
Insulin resistance increases during pregnancy, particularly in the second and third trimesters.
This allows for increased blood glucose levels, providing more energy to the foetus.
The mother's body compensates by producing more insulin, which may lead to gestational diabetes in some cases.
-
What are the key physiological changes in pregnancy that make diagnosing conditions like preeclampsia and gestational diabetes challenging? (3)
Increased blood pressure and protein in the urine can be normal during pregnancy, complicating the diagnosis of preeclampsia.
Elevated blood sugar levels can be seen in normal pregnancy due to insulin resistance, which makes diagnosing gestational diabetes challenging.
Fluid retention and swelling may overlap with symptoms of preeclampsia, further complicating diagnosis.

