
Lipid Transport (The Living Cell)
Learning objectives How are fats transported around the body The differences between chylomicrons, VLDL, LDL and HDL How are they targeted to different tissues How lipids are exchanged between lipoproteins and between lipoproteins and cells The importance of cholesterol uptake and how it is regulated What happens if lipid transport goes wrong
-
Lipids are transported by three interlinked systems, what are these systems?
-The exogenous pathway
-The endogenous pathway
-The reverse cholesterol transport pathway
-
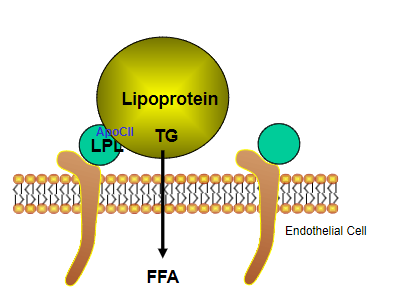
What does the exogenous pathway do?
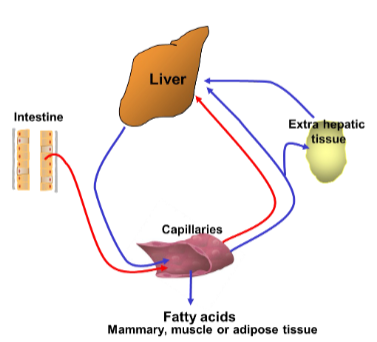
Transports lipid from the gut to the liver
-
What does the endogenous pathway do?
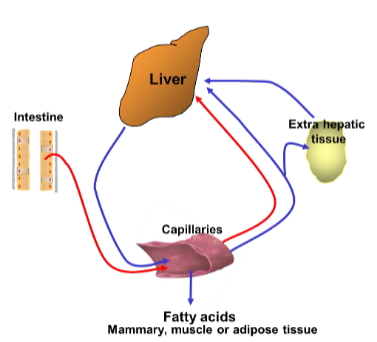
Transports lipids synthesised by the liver to non-hepatic tissue, including adipocytes
-
What does the reverse cholesterol transport pathway do?
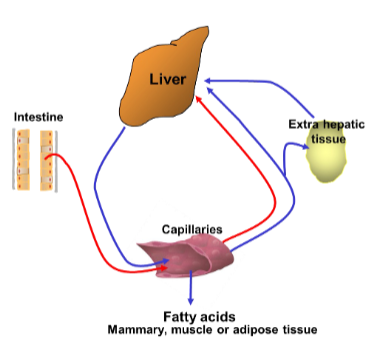
Takes lipid from the circulation and from non-hepatic tissue back to the liver
-
What is hepatic tissue?
Refers to the tissue associated with the liver
-
What are the proportions (%) of the Fatty acids and lipids in the circulation?
Triglycerides (45%)
Phospholipids (35%)
Cholesterol esters Cholesterol (15%)
Free Fatty Acids (5%)
-
State some information about Free Fatty Acids (FFA) (5)
1. Formed from triglycerides stored in adipose tissue
2. Circulates bound to protein as Na+ salt particularly albumin as unbound FA would act as a detergent
3. Saturation occurs at about 2mM FA molecules
4. FA enter cells by simple diffusion
5. Intracellular concentration FFA kept low
-
Lipoproteins are carried in the blood as?
Plasma lipoproteins
-
What are the five types of lipoprotein?
– Chylomicrons
– Very low density lipoproteins (VLDL)
– Intermediate density lipoprotein (IDL)
– Low density lipoproteins (LDL)
– High density lipoproteins (HDL)
-
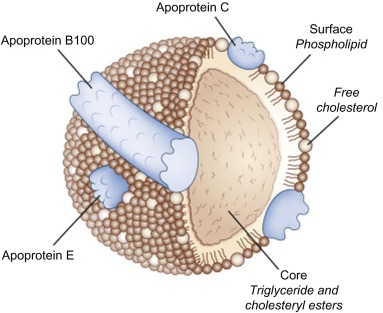
What is a lipoprotein?
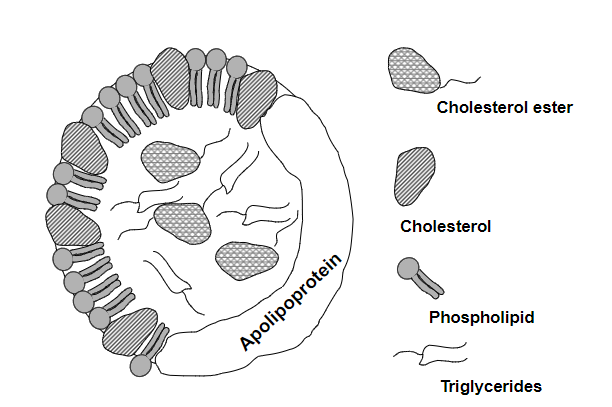
A complex biochemical structure composed of lipids (fats) and proteins
-
What is a Apolipoprotein?
Is a protein component of a lipoprotein
-
What is another name for apolipoprotein?
Apoprotein
-
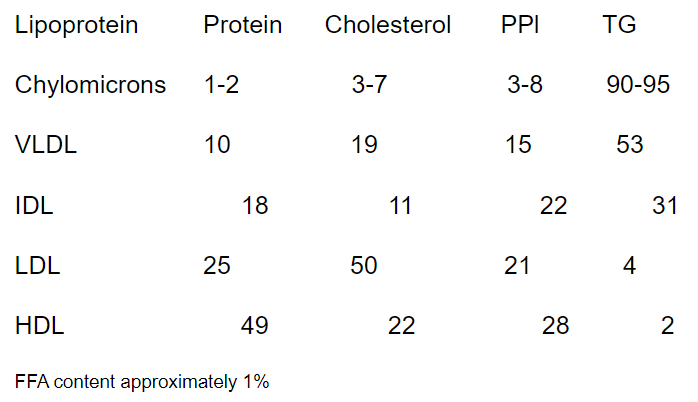
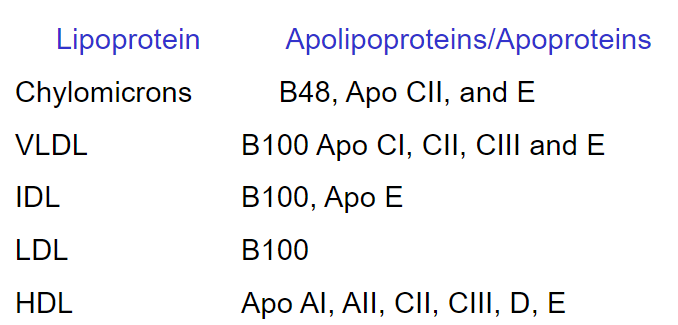
A picture summary of the different lipoprotein compositions (by % weight)
-
A picture summary of the different lipoprotein Apolipoproteins:
-
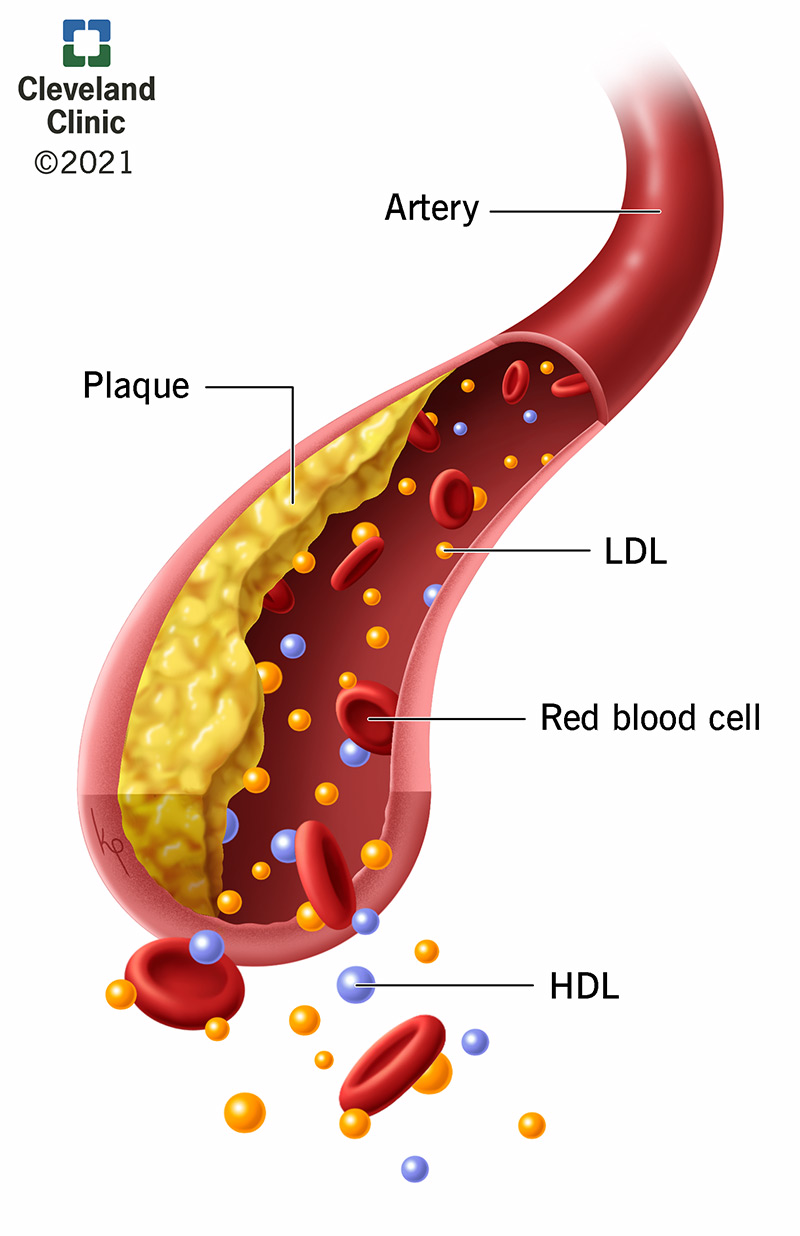
What are the four main functions of Apolipoproteins?
• Structural
• To solubilise lipids
• Act as enzymes or enzyme cofactors
+Apo CII for lipoprotein lipase
+Apo AI for lecithin:cholesterol acyltransferase
• Tissue targeting
+Apo B100 and Apo E bind to the LDL receptor
+Apo E binds to the HDL receptor
-
Chylomicrons, which transport dietary lipids, have low density because...?
They are rich in triglycerides
-
B48 is added to the chylomicrons in the what?
SER
-
Chylomicros are Secreted by Reverse Pinocytosis into the Lymphatics; What is pinocytosis?
-A cellular process by which cells engulf fluids, dissolved solutes, and small particles from their surroundings
-It is a form of endocytosis
-
Apo C2, C3, and E Transferred from HDLs to the what?
Chylomicrons
-
What does LPL stand for?
LipoProtein Lipase
-
LPL on adipocytes is stimulated by what hormone?
Insulin
-
What is Type 1 hyperlipidaemia?
-Deficiency in lipoprotein lipase or Apo C2
-Characterised by high plasma triglyceride
-
What is Type 2 hyperlipidaemia?
-Deficiency in lipoprotein lipase or Apo C2
-Characterised by high LDL
-Most are caused by a genetic defect in the synthesis, processing or function of the LDL receptor
-
What is Type 4 hyperlipidaemia?
-Most common form results in raised VLDL concentrations, often due to obesity or alcohol abuse
-
Where does LPL bind? And what is activated by Apo CII?
-
What is the chylomicron lifetime circulation in the blood?
1 hour
-
Chylomicron remnants are removed by what?
By the liver with the involvement of Apo E
-
Chylomicrons contain Fat-soluble vitamins, what vitamins are they?
A and E
-
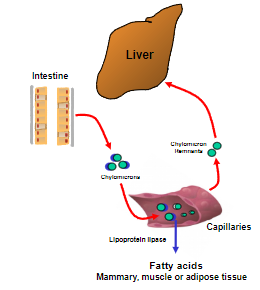
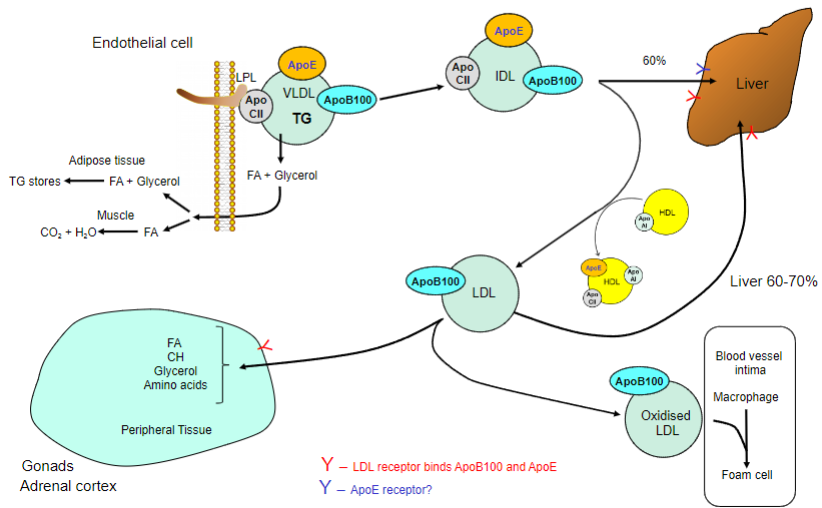
Where is VLDL synthesised?
By the liver when dietary intake of carbohydrates exceeds immediate need
-
Triglycerides that are formed are packaged with what? What is this formation stimulated by? What is it inhibited by?
-Free fatty acids, phospholipids, cholesterol esters and Apo B100 to form nascent VLDL
-Stimulated by Insulin
-Inhibited by glucagon
-
Nascent VLDLs receive what from HDL?
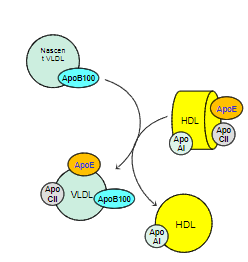
ApoE and ApoCII
-
VLDL remnants are removed by what?
-By the liver by apoE (TG 15-60 mins)
-
Picture outlining the fate of VLDLs
-
What are the major carrier of cholesterol
LDL
-
LDL is metabolised slowly, how long does it take?
3 days
-
LDL carry cholesterol to where? And regulate what?
-Transporting cholesterol from peripheral tissues (such as arterial walls) back to the liver
-Regulate De Novo Synthesis
-
What is De Novo synthesis
Refers to the process by which cells or organisms synthesize complex molecules, such as proteins, nucleic acids, lipids, or other biomolecules, from simple precursor molecules
-
LDL contains what apolipoprotein?
Contain 1 ApoB100 which can bind to a specific receptor on hepatocytes
-
Picture outlining the synthesis VLDL to LDL
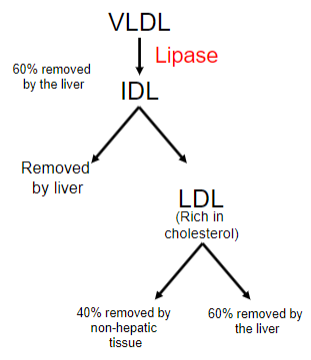
-
How is HDL created? (3 ways)
Nascent Particles by the Liver and Intestine: HDL can be synthesized as nascent particles directly by the liver and intestine, contributing to their initial formation.
Budding of Apolipoproteins from Chylomicrons: Apolipoproteins can bud from chylomicrons, forming HDL particles as part of lipid metabolism.
From Free ApoAI: HDL can also be created from free apolipoprotein A-I (ApoAI), a major apolipoprotein associated with HDL.
-
Nascent HDL acquire what from endothelial cells?
Cholesterol and phospholipids
-
HDL's most important function is reverse cholesterol transport, this involves what?
Transporting excess cholesterol from peripheral tissues, including vascular cells, back to the liver for elimination or recycling
-
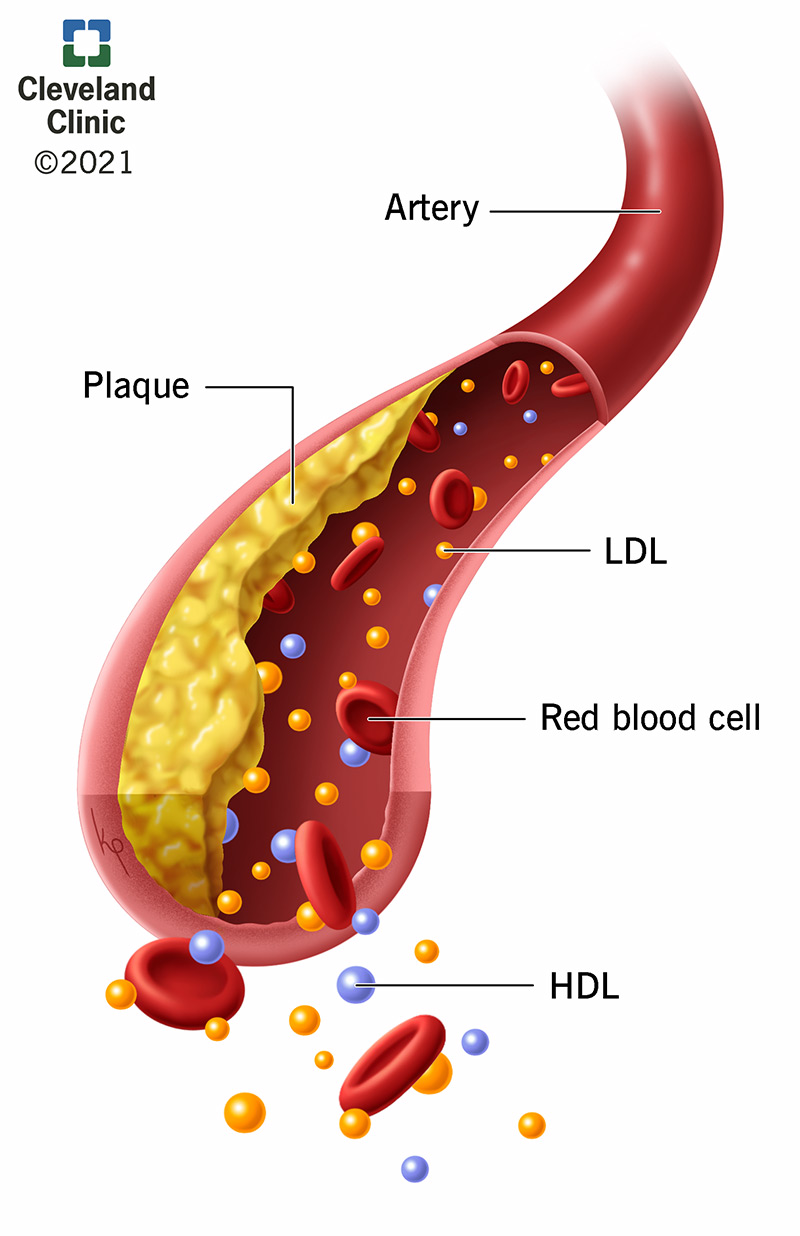
HDL's reverse cholesterol transport function also helps prevent the formation of foam cells. What are foam cells?
Foam cells are lipid-laden macrophages and are a hallmark of atherosclerosis
-
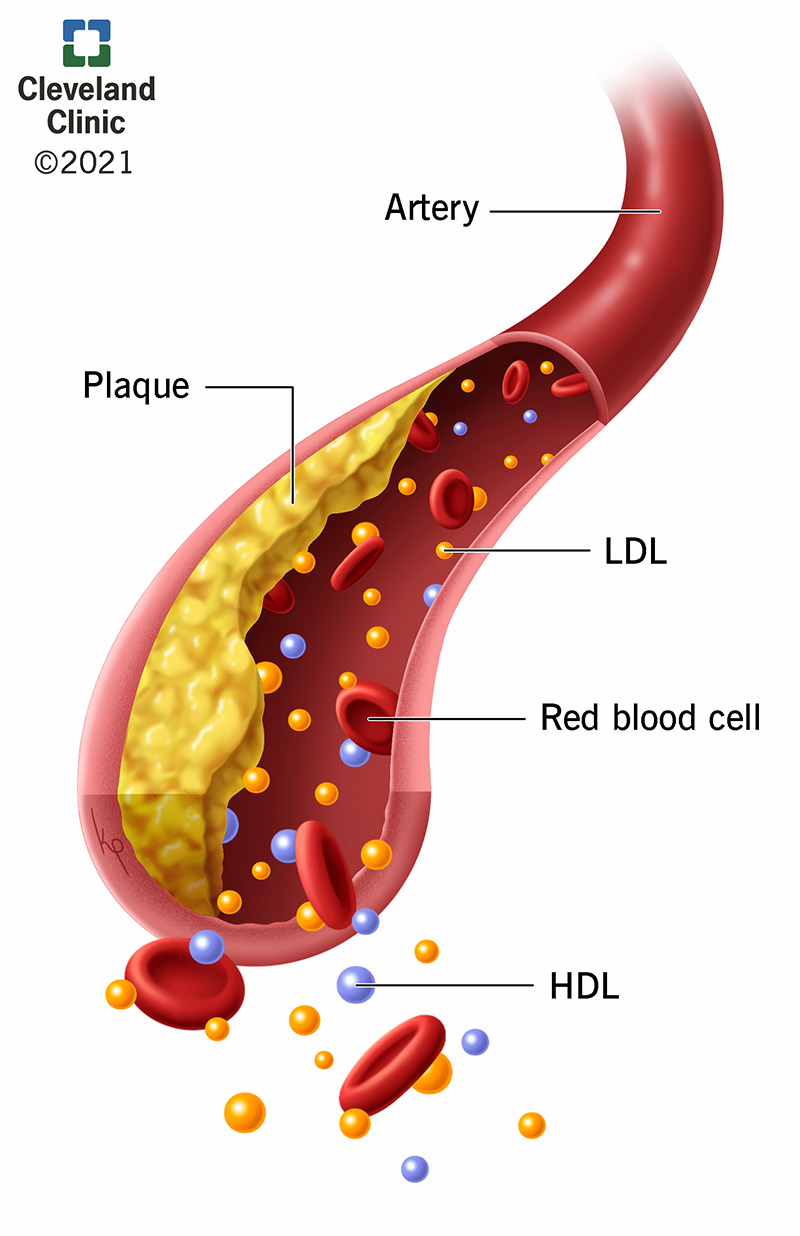
What is atherosclerosis
-A cardiovascular condition characterized by the accumulation of plaques within the walls of arteries
-These plaques are composed of various substances, including lipids (such as cholesterol and triglycerides), fibrous tissue, calcium deposits, and inflammatory cells
-
HDL possesses LCAT, an enzyme that catalyzes what?
-The esterification of cholesterol
-This enzymatic activity helps in the formation of cholesterol esters, preventing the cholesterol from returning to the cell
-
ABC1 is a protein associated with HDL that plays a role in what?
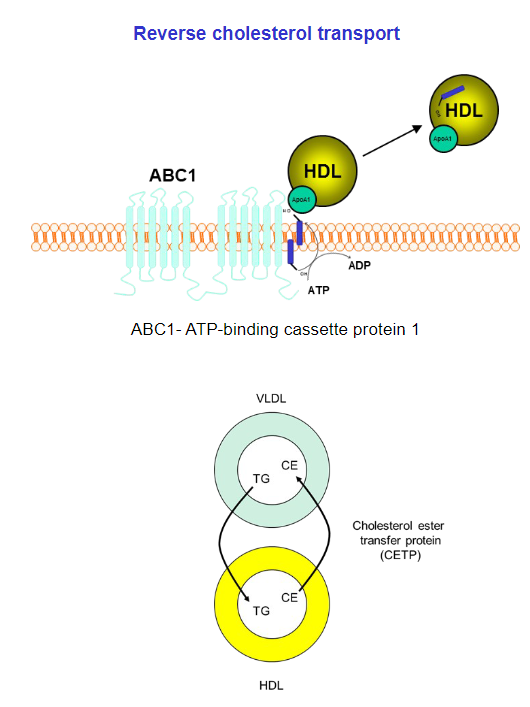
-Cholesterol efflux
-Facilitating the movement of cholesterol from cells to HDL particles.
-
Cholesterol-rich HDL can either deliver cholesterol directly to the liver or exchange it with what?
Other lipoprotein particles, including very low-density lipoproteins (VLDL) and VLDL remnants
-
What is the 'good' cholesterol?
HDL
-
What is the 'bad' cholesterol?
LDL
-
Lipoproteins are removed from the circulation by what mechanism?
Receptor mediated endocytosis
-
What regulates cholesterol uptake and synthesis?
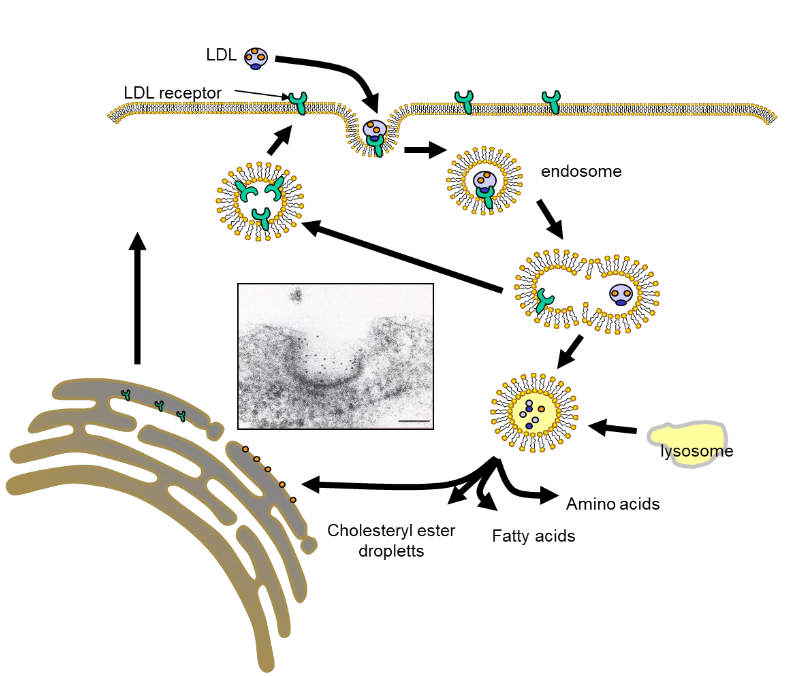
Cholesterol regulates its own uptake and synthesis
-
Increased cholesterol inhibits the enzyme activity of what?
HMG-CoA reductase
-
Decreased cholesterol increases the synthesis and expression of what?
LDL receptors
-
Statement:
HMG-CoA is a target for therapy
Is this true?
YES
-
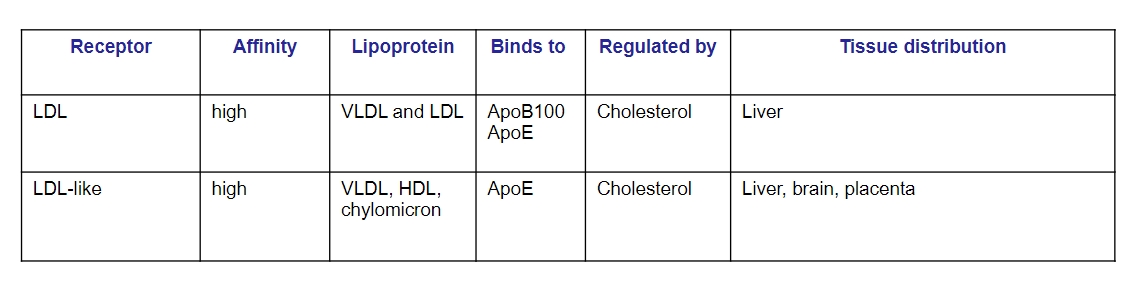
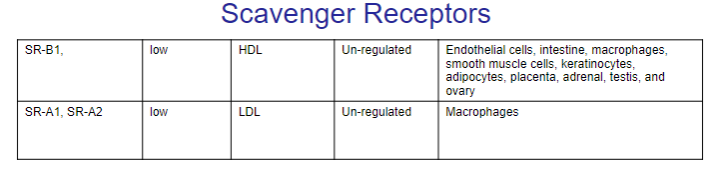
Picture summary of the scavenger receptors
-
Familial Hypercholesterolemia (FH) is a genetic disorder characterized by significantly elevated levels of low-density lipoprotein (LDL) cholesterol in the blood.
What do Homozygous individuals experience: (4)
And why does this happen? (mutation)
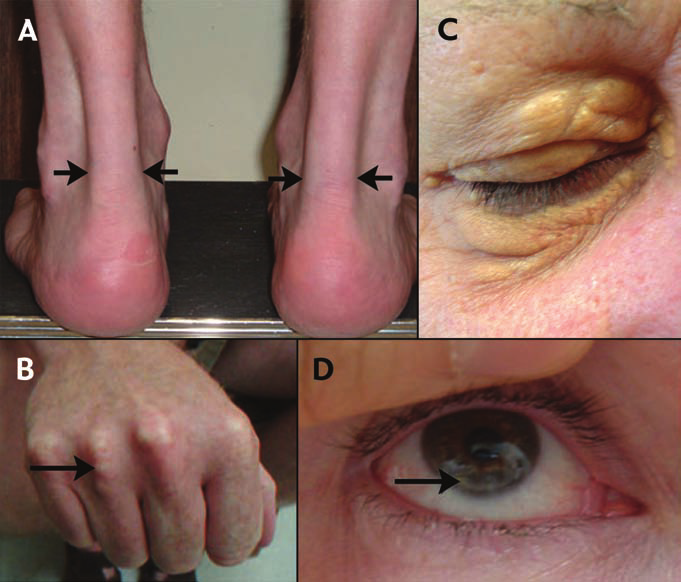
1. High serum cholesterol (800mg/ml, normal is 200mg/ml)
2. Develop blocked arteries (atherosclerosis)
3. Die young from heart attacks
4. De novo synthesis is not regulated by LDL
Single amino acid substitution that prevents localisation of the LDL receptor to the coated pits.
-
What are the Abnormalities of Lipid Transport? And what is it due to?
Diabetes Mellitus: increased FFA mobilisation, decreased Chylomicron and VLDL utilisation
Obesity: hypertension, NIDDM, hyperlipidaemia and hyperglycaemia
Gene defects: apolipoproteins, enzymes or receptors
Leading to: hypercholesterolaemia, atherosclerosis
-
A general summary
-Lipoproteins consist of triglycerides, phospholipids, cholesterol and cholesterol esters associated with proteins called apolipoproteins
-Apolipoproteins act as receptors, enzymes or enzymes co-factors
-Apolipoproteins also help solubilise the lipids and provide structure to the lipoprotein
-Chylomicrons are formed in the gut and transport dietary lipids-VLDLs transport endogenously synthesised lipids from the liver
-LDLs are a made from VLDLs and are a major cholesterol transporter
-HDLs is involved in reverse cholesterol transport back to the liver anddelivers cholesterol to tissues such as the testis and adrenal

