Introduction to the Microbiology of the Gut (Physiology) UNFINISHED
Session summary Gut infections have a major global impact on health. Symptoms range from mild, self-limiting gastroenteritis to severe and fatal diarrhoea. The gut is colonised with commensal organisms that contribute to its function. Pathogens compromise gut function to produce local and systemic disease. This lecture reviews the normal microbiology of the gastrointestinal tract and presents mechanisms by which the normal gut epithelial cell function is compromised by pathogens, and the subsequent patho-physiological consequences. Learning outcomes At the end of this session you will be able to: Define the concepts of the microbiome and microbiota Describe the development and distribution of the normal intestinal microbiota Explain the associations between the gut microbiota and health/disease Evaluate interventions for modulating gut microbiota Explain pathogenic mechanisms of gastrointestinal disease Session resources Teams link: Join Introduction to the microbiology of the gut (Microsoft Teams Meeting)Links to an external site. Lecture slides: Introduction to microbiology of the gut.pptx
-
What is the human microbiome?
The human microbiome refers to the collection of microbiota and their genomes in the human body
-
What is included in the microbiota?

Microbiota include bacteria, archaea, fungi, protozoa, and viruses that colonize our body surfaces
-
Where is the majority of the microbiome found?
Approximately 70% of total microbes are found in the gut
-
What are the dominant microbial phyla in the gut?
Firmicutes, Bacteroidetes, Actinobacteria, and Proteobacteria are the dominant microbial phyla in the gut
-
How many microbial cells are estimated to be present in the human body?
There are approximately 100 trillion (10^14) microbial cells in the human body
-
How does the gene diversity of the microbiome compare to that of the human genome?
The gene diversity of the microbiome is estimated to be 3.3 million genes, compared to approximately 22,000 human genes
-
What factors influence the variability of the human microbiome?
The mode of delivery (e.g., vaginal birth or cesarean section), mode of feeding (e.g., breastfed or formula-fed infants), antibiotic use, age, and diet are all factors that influence the variability of the human microbiome
-
How should we view ourselves according to the concept of holobionts?
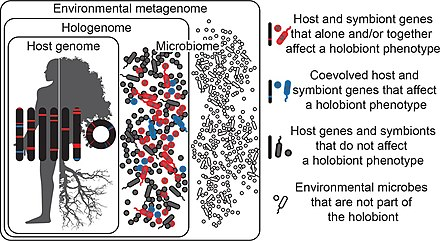
We should view ourselves as a composite of microbial and human cells
-
How should we perceive our genetic landscape according to the concept of holobionts?
Our genetic landscape is a summation of the genes embedded in our genome and the collective genomes (‘microbiome’) of our habitat-associated microbial communities
-
How should we characterize our metabolic features according to the concept of holobionts?
Our metabolic features are an amalgamation of human and microbial attributes
-
What is the significance of the human gastrointestinal (GI) tract?
The GI tract is the largest tube running through the body
-
What structures does the GI tract comprise?
The GI tract comprises the oral cavity, esophagus, stomach, small intestine, and large intestine
-
What is the main function of the GI tract?
The main function of the GI tract is the digestion of food and absorption of nutrients
-
Why is the GI tract a major surface for microbial colonization?
The GI tract provides a large surface area of approximately 200 square meters and is rich in nutrients, making it an ideal environment for microbial colonization
-
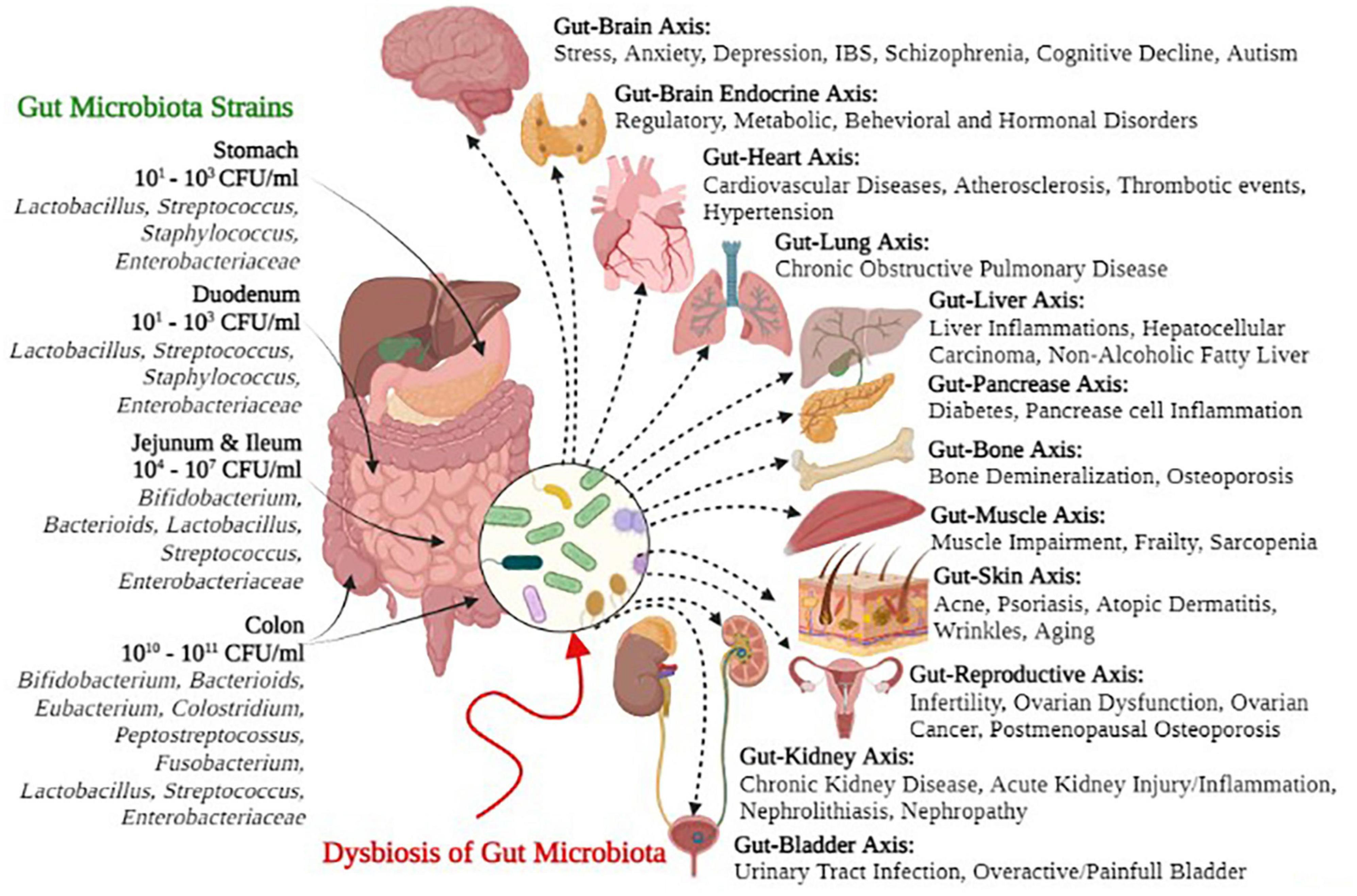
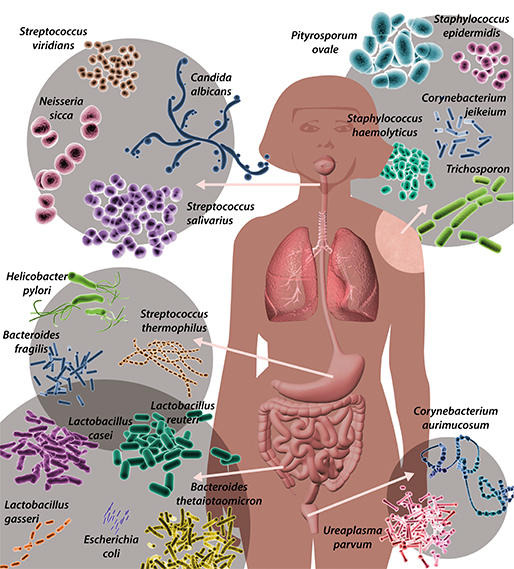
Picture demonstrating the human microbiome
-
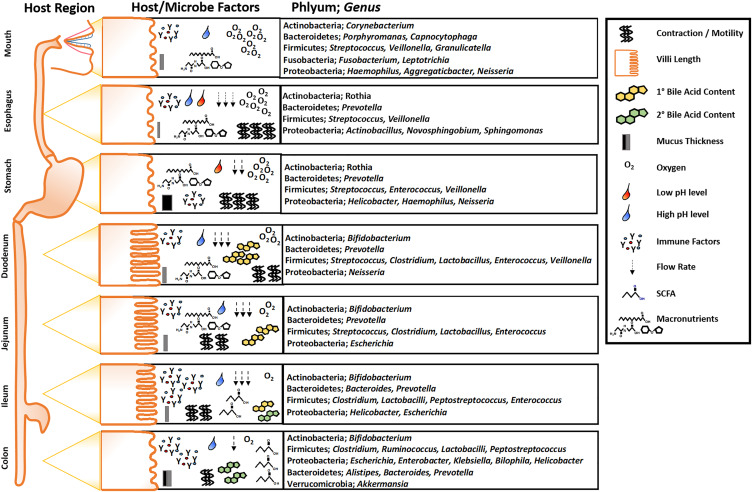
Picture demonstrating the regional diversity of the GI microbiome
-
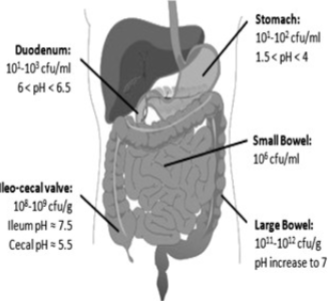
Picture demonstrating the differing pH and bacteria amounts
-
What does the oral cavity consist of?
The oral cavity includes the mouth, nose, and throat
-
What microorganisms are densely populated in the mouth? (7)
♡ Prevotella
♡ Porphyromonas
♡ Desulfovibrio
♡ Bacteroides
♡ Fusobacterium
♡ Eubacterium
♡ Peptostreptococcus
-
What are the characteristics of the stomach?
♡ The stomach is a J-shaped organ that receives food from the esophagus
♡ It aids in both chemical and mechanical digestion
-
What is the microbial environment like in the stomach?
♡ The low pH of the stomach makes it almost sterile, with fewer than 10^3 colony-forming units (cfu) per milliliter of gastric contents
♡ Microorganisms in the stomach are transient rather than resident
-
What are some examples of microorganisms found in the stomach? (3)
♡ Acid-tolerant lactobacilli
♡ Yeasts
♡ Helicobacter pylori
-
What is Helicobacter pylori?

Helicobacter pylori is a gram-negative bacterium.
-
How does Helicobacter pylori colonize the human stomach?
Helicobacter pylori colonizes the human stomach in early life
-
What percentage of the world's population are carriers of H. pylori?
Approximately 50% of the world's population are carriers of H. pylori
-
What are the diseases associated with H. pylori infection?
♡ Disease occurs in about 15% of carriers and may include peptic ulcers, gastric inflammation (gastritis), and gastric cancer
-
What are the main functions of the small intestine?
♡ The small intestine digests and absorbs nutrients.
-
What are the three parts of the small intestine?
♡ The small intestine consists of the duodenum (upper part), jejunum, and ileum (lower parts)
-
Why are there lower numbers of bacteria in the small intestine?
♡ Lower numbers of bacteria (~10^3 per gram) are present due to the secretion of bile and short transit time
-
Where are higher numbers of bacteria found in the small intestine?
♡ Higher bacterial numbers (up to 10^7 per gram) are found in the ileum
-
What are some examples of bacteria found in the small intestine? (5)
♡ Enterococci
♡ Enterobacteria
♡ Lactobacilli
♡ Bacteroides
♡ Clostridia
-
What is the population density of microorganisms in the large intestine (colon)?
There is a rapid increase in population in the large intestine (colon), with approximately 10^12 microorganisms per gram
-
Why is the large intestine (colon) favorable for microbial growth?
♡ The large intestine (colon) provides favorable conditions for microbial growth, including a suitable pH, nutrient availability, and a slow transit time
-
What are some examples of bacteria found in the large intestine? (4)
♡ Bifidobacterium
♡ Bacteroides
♡ Eubacterium
♡ Lactobacillus
-
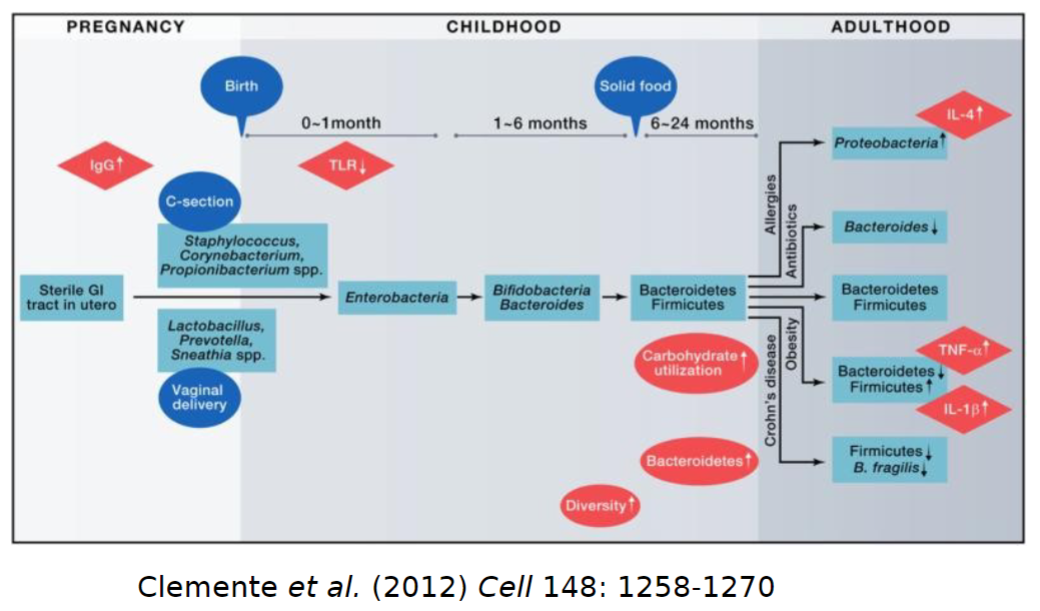
What is the initial state of the gastrointestinal (GI) tract at birth?
The GI tract is sterile at birth.
-
How does colonization of the GI tract occur?
The GI tract is colonized by microorganisms from the mother and the environment
-
What type of microorganisms are the early colonizers of the GI tract?
Early colonizers are aerotolerant as the gut initially contains oxygen; they are later replaced by anaerobes
-
When does the gut microbiota stabilize?
The gut microbiota stabilizes within the first few years of life
-
How many species can be found in the gut microbiota?
As many as 1000 species can be found in the gut microbiota
-
What are some characteristics of the gut microbiota along the length of the GI tract?
The gut microbiota exhibits varying composition and numbers along the length of the GI tract
-
What are some factors that influence gut microbiota composition? (5)
♡ Mode of delivery: vaginal vs. caesarean section
♡ Diet: breastfed vs. formula fed
♡ Antibiotic use
♡ Age
♡ Environment
-
What are some roles of intestinal microbiota in health? (5)
♡ Digestion of food
♡ Development of the gut immune system
♡ Production of short-chain fatty acids
♡ Production of essential vitamins
♡ Resistance to colonization by pathogens
-
How is dysbiosis related to disease?
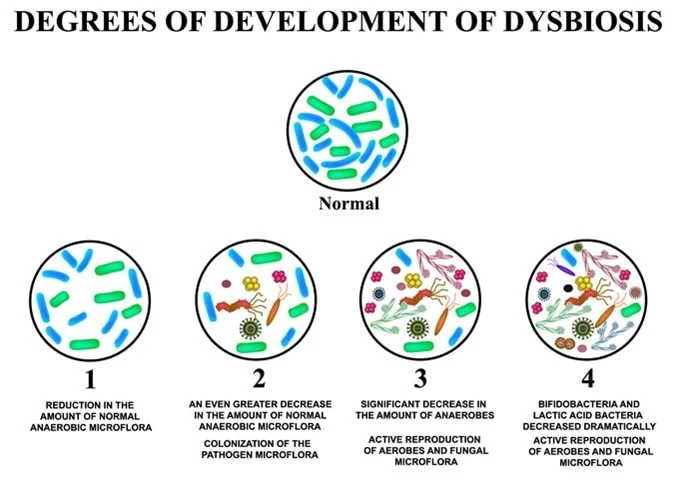
Changes or alterations in microbiota (dysbiosis) are associated with various diseases
-
What changes in microbiota composition are commonly observed in disease states?
A reduction in bifidobacteria and an increase in other microbial groups are commonly seen
-
How are altered community profiles of microbiota related to disease?
Altered community profiles of microbiota may be both a cause and a consequence of disease.
-
What is the relationship between changes in microbiota composition and disease?
While changes in microbiota composition are correlated or associated with disease, it is important to note that correlation does not imply causation
-
What are the characteristics of Bifidobacterium?

Bifidobacterium are anaerobic, non-motile heterofermentative Gram-positive rods
-
Where are Bifidobacterium commonly found?
Bifidobacterium are common inhabitants of the gastrointestinal tract
-
How many species of Bifidobacterium are there?
There are approximately 90 species of Bifidobacterium
-
What are the optimum growth conditions for Bifidobacterium?

The optimum growth conditions for Bifidobacterium are at 37-41°C and pH 6.5-7.0
-
What is the metabolic pathway used by Bifidobacterium for carbohydrate fermentation?
Bifidobacterium ferment carbohydrates using the fructose-6-phosphate phosphoketolase shunt
-
In which population is Bifidobacterium predominant?

Bifidobacterium are predominant in breast-fed infants
-
How does the population of bifidobacteria change with age?
The population of bifidobacteria decreases with age, being highest in infancy, declining and remaining stable in adulthood, and further declining in elderly age
-
How can gut microbiota composition be modulated?
Gut microbiota composition can be modulated through dietary interventions such as probiotics and prebiotics
-
What are some examples of dietary interventions for modulating gut microbiota composition? (2)
♡ Probiotics
♡ Prebiotics
-
What is another method for modulating gut microbiota composition?

Faecal microbiota transplantation
-
What are probiotics?
Probiotics are live microorganisms that can confer a health benefit when administered in adequate amounts.
-
What are common vehicles for delivering probiotics?
Dairy products are the most common vehicles for delivering probiotics.
-
Which microbial strains are the most common probiotics?
The most common probiotic strains are members of Lactobacillus and Bifidobacterium
-
What are some examples of health claims associated with probiotic strains?
Various health claims are associated with probiotic strains
-
Picture demonstrating the presence of bacteria during pregnancy, childhood and adulthood
-
What are some health benefits associated with probiotics? (8)
♡ Prevention of diarrhea
♡ Alleviation of lactose intolerance
♡ Control of inflammatory bowel disease (IBD) and irritable
♡ bowel syndrome (IBS)
♡ Cancer prevention
♡ Cholesterol reduction
♡ Modulation of the immune system
♡ Establishment of healthy microbiota in premature infants
-
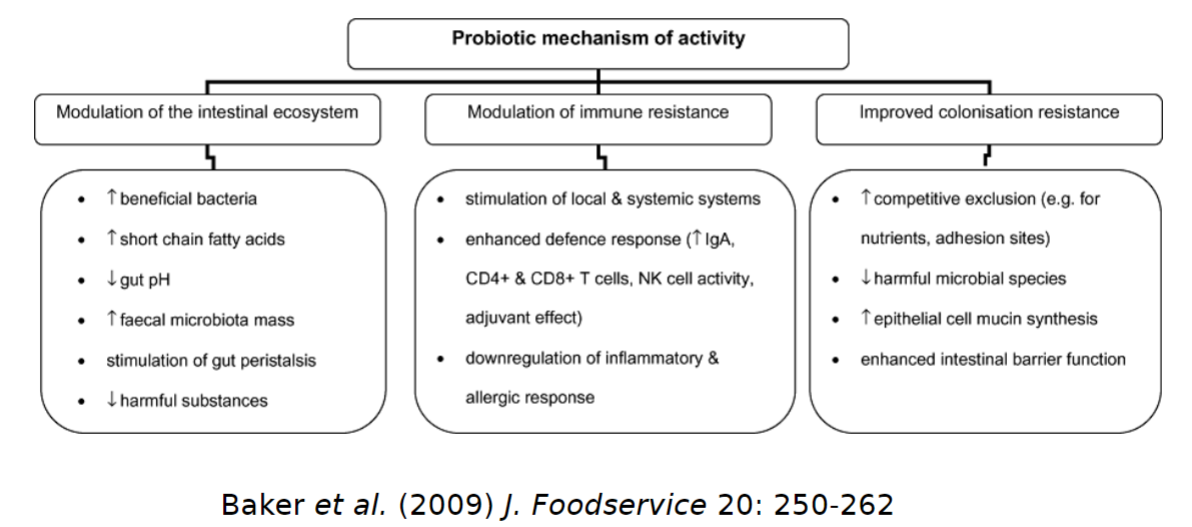
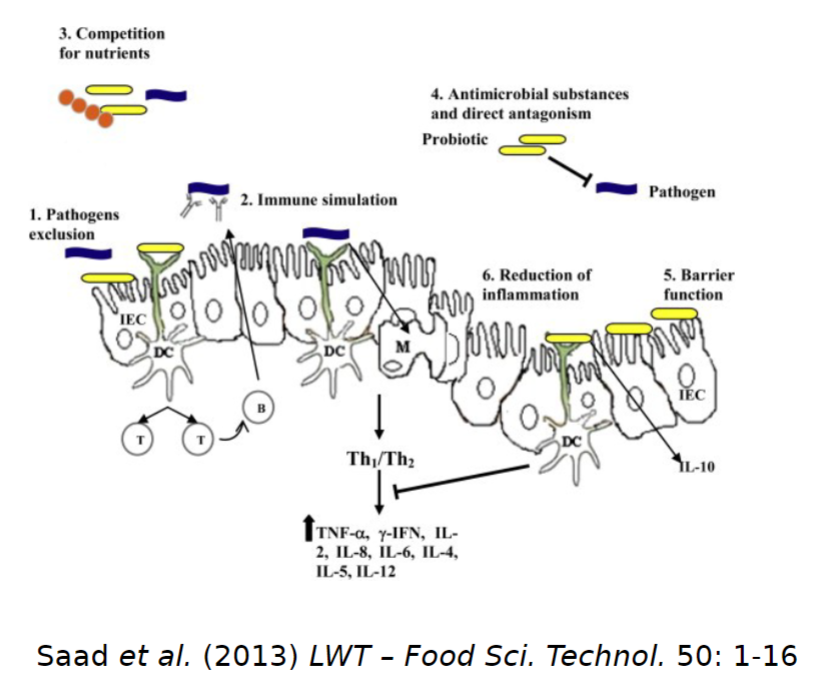
What are some mechanisms of action of probiotics? (3)
Probiotic benefits may occur directly or indirectly through several mechanisms:
♡ Modulation of the intestinal ecosystem
♡ Improved colonization resistance
♡ Modulation of immune response
-
How does modulation of the intestinal ecosystem occur with probiotics?
The consumption of probiotics and the transient colonization that occurs can influence the composition and activity of the natural gut microbiota, helping to maintain a beneficial balance.
-
What are the effects of probiotics on the intestinal ecosystem?
Probiotics increase the population of beneficial bacteria and decrease the population of harmful microorganisms
-
How is the gut made more favorable to beneficial bacteria with probiotics?

Probiotics achieve this by producing organic acids or short-chain fatty acids, which lower the gut pH, and by producing antimicrobial agents such as bacteriocins
-
Which beneficial bacteria are favored by probiotics?
Probiotics make the gut more favourable to beneficial bacteria such as lactobacilli and bifidobacteria, and consequently, less favourable to pathogenic microorganisms
-
How does improved colonization resistance occur with probiotics?
The growth and metabolism of probiotic microorganisms can alter the intestinal environment, leading to improved colonization resistance
-
What are some mechanisms through which probiotics improve colonization resistance?
Probiotics may adhere to epithelial cells, blocking the adhesion of pathogens through competitive exclusion. They may also stimulate mucin production, enhancing intestinal barrier function
-
How do probiotics modulate immune resistance?
Probiotics stimulate mucosal immunity and modulate immune responses by interacting with the gut-associated lymphoid tissue (GALT)
-
What is the gut-associated lymphoid tissue (GALT)?
The GALT is the largest lymphoid tissue in the human body and contains various cells of the immune system that interact with intestinal microorganisms
-
How do host cells recognize probiotic microorganisms?
Metabolites, cell wall components, and DNA of probiotic microorganisms are recognized by host cells sensitive to them, such as toll-like receptors
-
What is the outcome of the activation of toll-like receptors by probiotics?
Activation of toll-like receptors leads to modulation of pro- and anti-inflammatory cytokine expression, resulting in downregulation of inflammatory and allergic responses
-
Why have very few health claims related to probiotics been approved by authorities?
Very few health claims related to probiotics have been approved due to unsatisfactory dossiers of evidence to back such health claims
-
What descriptors are favored by many manufacturers instead of using the term 'probiotic'?
Many manufacturers now favor the use of descriptors such as 'beneficial bacteria', 'live bacteria', and 'good bacteria'.
-
Why is the term 'probiotic' subject to scrutiny?
The term 'probiotic' implies health benefit and is therefore subject to scrutiny
-
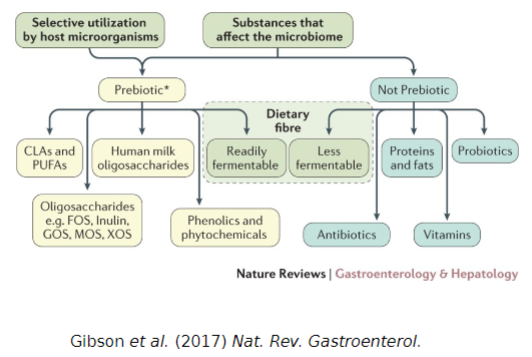
What are prebiotics?
Prebiotics are substrates that are selectively utilized by host microorganisms, conferring a health benefit
-
What are the criteria for a compound to be considered a prebiotic?
The criteria for a compound to be considered a prebiotic include being resistant to gastric acidity, hydrolysis by enzymes, and gastrointestinal absorption, as well as being fermented by intestinal microbiota and selectively stimulating the growth and/or activity of intestinal bacteria associated with health and wellbeing.
-
Can you provide examples of prebiotic compounds?
Examples of prebiotic compounds include inulin, fructooligosaccharides (FOS), galactooligosaccharides (GOS), xylo-oligosaccharides (XOS), isomaltooligosaccharides (IMO), soybean oligosaccharides (SOS), mannanooligosaccharides (MOS), lactosucrose, lactulose, human milk oligosaccharides (HMOs), conjugated linoleic acid (CLA), polyunsaturated fatty acids (PUFAs), and plant polyphenols.
-
What are some natural sources of prebiotics?
Natural sources of prebiotics include agave, banana, garlic, onions, leeks, Jerusalem artichoke, chicory, and wheat
-
Picture demonstrating probiotic mechanism of activity
-
Picture demonstrating bacteria activity in the gut
-
Picture demonstrating prebiotic and not prebiotic bacteria
-
What predominates the microbiota found in breast-fed infants compared to formula-fed infants?
Bifidobacteria predominates the microbiota found in breast-fed infants compared to formula-fed infants.
-
What components in human breast milk have been shown to stimulate the growth of Bifidobacterium?
Human breast milk contains bifidogenic factors such as lactulose, N-acetyl-glucosamine-containing saccharides, and human milk oligosaccharides (HMOs), including short-chain trisaccharides and complex, high-molecular-weight glycans.
-
How do human milk oligosaccharides (HMOs) selectively stimulate the development of bifidobacteria in the gut microbiota?
HMOs, which are only partially digested in the small intestine, reach the colon where they selectively stimulate the development of bifidobacteria in the gut microbiota.
-
What does FMT stand for, and what is its purpose?
FMT stands for Faecal Microbiota Transplantation, and its purpose is to administer a solution of faecal matter from a donor into the intestinal tract of a recipient to directly change the recipient’s microbial composition and confer a health benefit.
-
Name some conditions for which Faecal Microbiota Transplantation (FMT) is used.
♡ Conditions for which FMT is used include:
♡ C. difficile infection
♡ Irritable bowel syndrome (IBS)
♡ Inflammatory bowel disease (IBD)
♡ Ulcerative colitis
♡ Crohn’s disease
-
What are some terms used to describe gastrointestinal tract infections?
Some terms used to describe gastrointestinal tract infections include:
♡ Gastroenteritis
♡ Diarrhoea
♡ Dysentery
♡ Enterocolitis
-
What is gastroenteritis, and what symptoms do it involve?
Gastroenteritis is an acute syndrome characterized by gastrointestinal symptoms such as nausea, vomiting, diarrhoea, and abdominal discomfort, typically caused by an infection.
-
Define diarrhoea and outline its potential consequences.
Diarrhoea is defined as watery or liquid stools, often accompanied by an increase in stool weight above 200 g per day and an increase in daily stool frequency, along with a sense of urgency. It can lead to severe dehydration, excessive fluid and electrolyte loss, organ failure, long-term morbidity, and reduced growth.
-
What is dysentery, and what are its typical characteristics?
Dysentery is an inflammatory disorder of the gastrointestinal tract, typically affecting the large intestine. It is often associated with the presence of blood and pus in the feces, along with symptoms such as pain, fever, and abdominal cramps.
-
Define enterocolitis and describe the areas of the gastrointestinal tract it affects.
Enterocolitis refers to inflammation involving the mucosa of both the small and large intestine.
-
What are some Bacterial Causes of Diarrheal Disease? (8)
Escherichia coli:
♡ ETEC (Enterotoxigenic E. coli)
♡ EPEC (Enteropathogenic E. coli)
♡ EIEC (Enteroinvasive E. coli)
♡ EHEC (Enterohaemorrhagic E. coli)
♡ Salmonella
♡ Campylobacter
♡ Vibrio cholerae
♡ Shigella
-
What are some Viral Causes of Diarrheal Disease? (3)
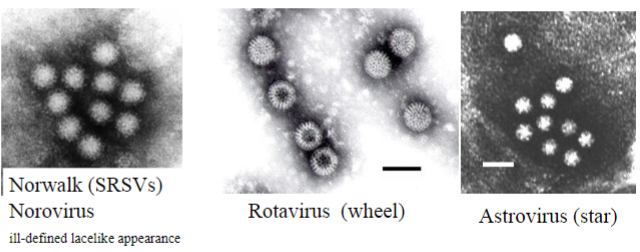
♡ Noroviruses
♡ Rotaviruses
♡ Astroviruses
-
What are the potential consequences of bacterial toxins in the gastrointestinal tract?
Bacterial toxins can exert pharmacological actions locally or at distant sites, as seen in cholera infections.
-
How does the GI tract respond to superficial microbial invasion?
Superficial microbial invasion triggers local inflammation, evident in conditions like Shigella dysentery or Campylobacter food poisoning.
-
What occurs when organisms invade blood and lymphatics in the GI tract?
Deep invasion leads to dissemination of organisms to other body sites, causing conditions such as enteric fevers like Typhoid fever or Hepatitis A
-
What damage can result from perforation or ulceration of the mucosal epithelium in the GI tract post-infection?
Perforation or ulceration may lead to serious conditions like peritonitis or intra-abdominal abscesses, as observed in infections like those caused by Entamoeba
-
How do bacterial toxins contribute to diarrhoea?
Bacterial toxins, such as enterotoxins, affect the gut by altering fluid and electrolyte transport, leading to diarrhoea.

