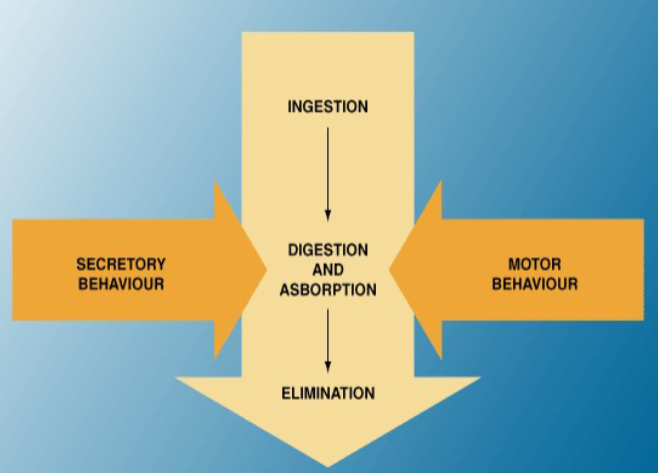
Introduction of the functions that control the GI tract (Physiology)
Session summary This lecture is in two parts. The first part provides a broad overview of the range of functions performed by the digestive (alimentary) tract. The serial and coordinated "processing" of the food as it is transported along the alimentary tract will be described. Note that some of these functions will be discussed in more detail in the subsequent lectures and that this is an introduction to the topic. The second part gives an overview of the ways in which the secretory and motility functions of the gut are regulated by nerves and hormones using selected examples from the stomach and small intestine. The first part of the lecture will describe the general principles of control and introduce the topics of visceral afferents and the second part will introduce examples of control which will be expanded upon in subsequent lectures. Learning outcomes First part of the session: Functions of the alimentary tract. At the end, you will be able to: Describe the function of exocrine secretions in reference to the alimentary tract and give an example Describe the function of motility (including storage) in reference to the alimentary tract and give an example Describe the function of digestion in reference to the alimentary tract and give an example Describe the function of absorption in reference to the alimentary tract and give an example Describe the function of defence in reference to the alimentary tract and give an example Describe the function of endocrine secretions (hormones) in reference to the alimentary tract and give an example Describe the function of excretion in reference to the alimentary tract and give an example
-
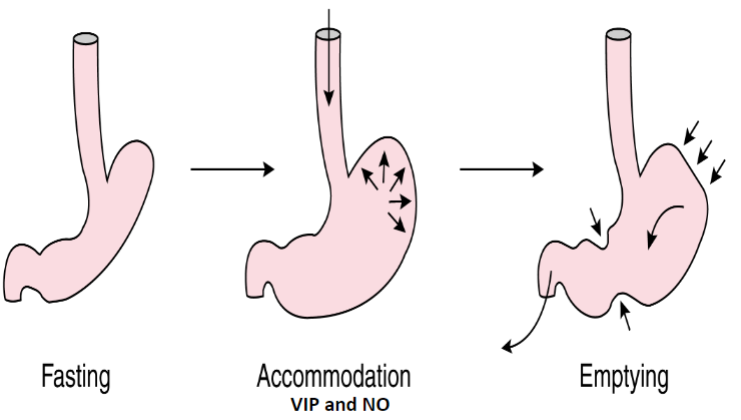
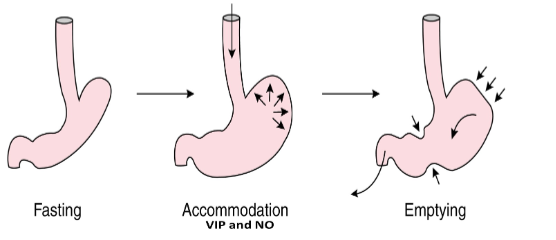
What are VIP and NO important for in the stomach? (1)
☆ They are important in the reflex relaxation of the stomach, promoting the accommodation of food.
-
What is the role of noradrenaline in the stomach? (1)
☆ Released from the sympathetic nervous system; it mediates the relaxation of the proximal stomach, possibly through vasoconstriction.
-
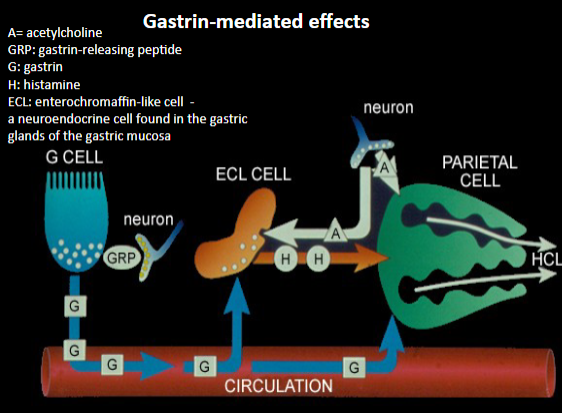
How is gastrin released and what are its effects? (2)
☆ Gastrin is released via the vago-vagal reflex. It stimulates G cells via gastrin-releasing peptide (GRP), leading to the release of gastrin into circulation.
☆ Gastrin stimulates enterochromaffin-like (ECL) cells to release histamine, which in turn stimulates acid (HCl) secretion by binding to H2 receptors on parietal cells.
-
What effect does gastrin have on ECL cells? (1)
☆ Gastrin stimulates enterochromaffin-like (ECL) cells to release histamine.
-
How does histamine contribute to acid secretion in the stomach? (1)
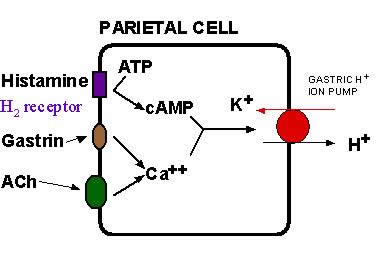
☆ Histamine binds to H2 receptors on parietal cells, stimulating acid (HCl) secretion.
-
What neurotransmitter is released in the vago-vagal reflex, and how does it affect acid secretion? (1)
☆ Acetylcholine (ACh) is released, which stimulates acid (HCl) secretion by acting on ECL cells and muscarinic receptors (M3 receptors) on parietal cells.
-
Name one drug that inhibits the activity of the K+/H+-ATPase pump responsible for acid secretion. (1)
☆ Omeprazole, lanzoprazole, etc. (Proton pump inhibitors)
-
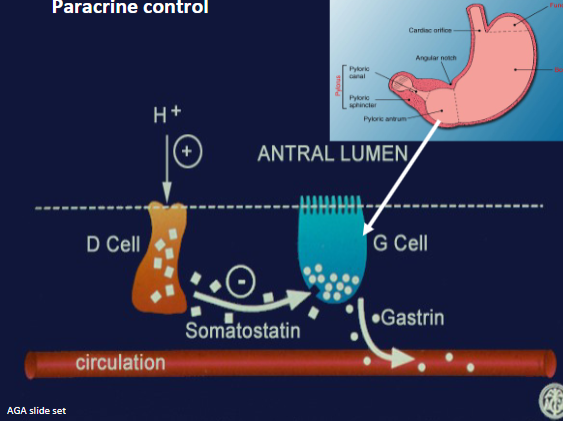
What paracrine hormone inhibits gastrin release and acid secretion in the stomach? (1)
☆ Somatostatin
-
What stimulates the release of somatostatin, and what is its effect on acid secretion? (1)
☆ Somatostatin release is stimulated by hyperacidity of the stomach. It inhibits gastrin release and acid secretion.
-
What is the function of cholecystokinin (CCK) released from the duodenum and jejunum? (1)
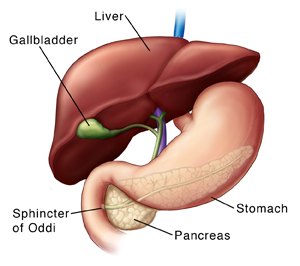
☆ CCK promotes the release of bile into the duodenum by causing contraction of the gallbladder and relaxation of the Sphincter of Oddi.
-
How does CCK exert its effects on gallbladder contraction and Sphincter of Oddi relaxation? (1)
☆ CCK sends afferent signals to the dorsal vagal complex, which releases ACh, NO, and VIP. ACh contracts the gallbladder smooth muscles, while NO and VIP relax the Sphincter of Oddi.
-
What are the effects of cholecystokinin (CCK) on the gallbladder and the sphincter of Oddi? (1)
☆ CCK causes the contraction of the gallbladder and relaxation of the sphincter of Oddi, promoting the flow of bile into the duodenum.
-
Besides promoting the flow of bile, what other effects does CCK have in the gut? (1)
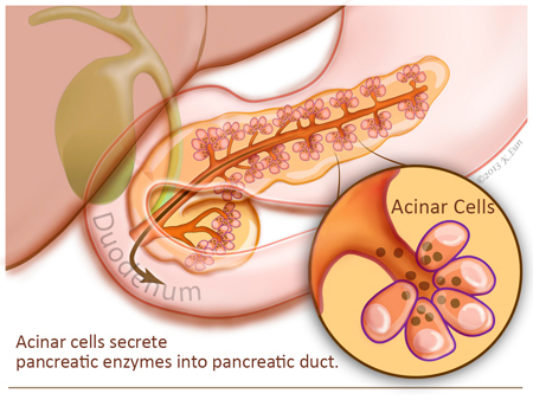
☆ CCK stimulates the secretion of digestive enzymes from pancreatic acinar cells, slows gastric emptying, induces a feeling of fullness (satiety), and stimulates the urge to defecate.
-
What is the role of vasoactive intestinal peptide (VIP) and nitric oxide (NO) in the gastrointestinal tract? (1)
☆ VIP and NO mediate reflex relaxation of the alimentary tract, facilitating receptive relaxation of the fundus and peristalsis by relaxing smooth muscle cells.
-
Describe the functions of secretin in the digestive system. (1)
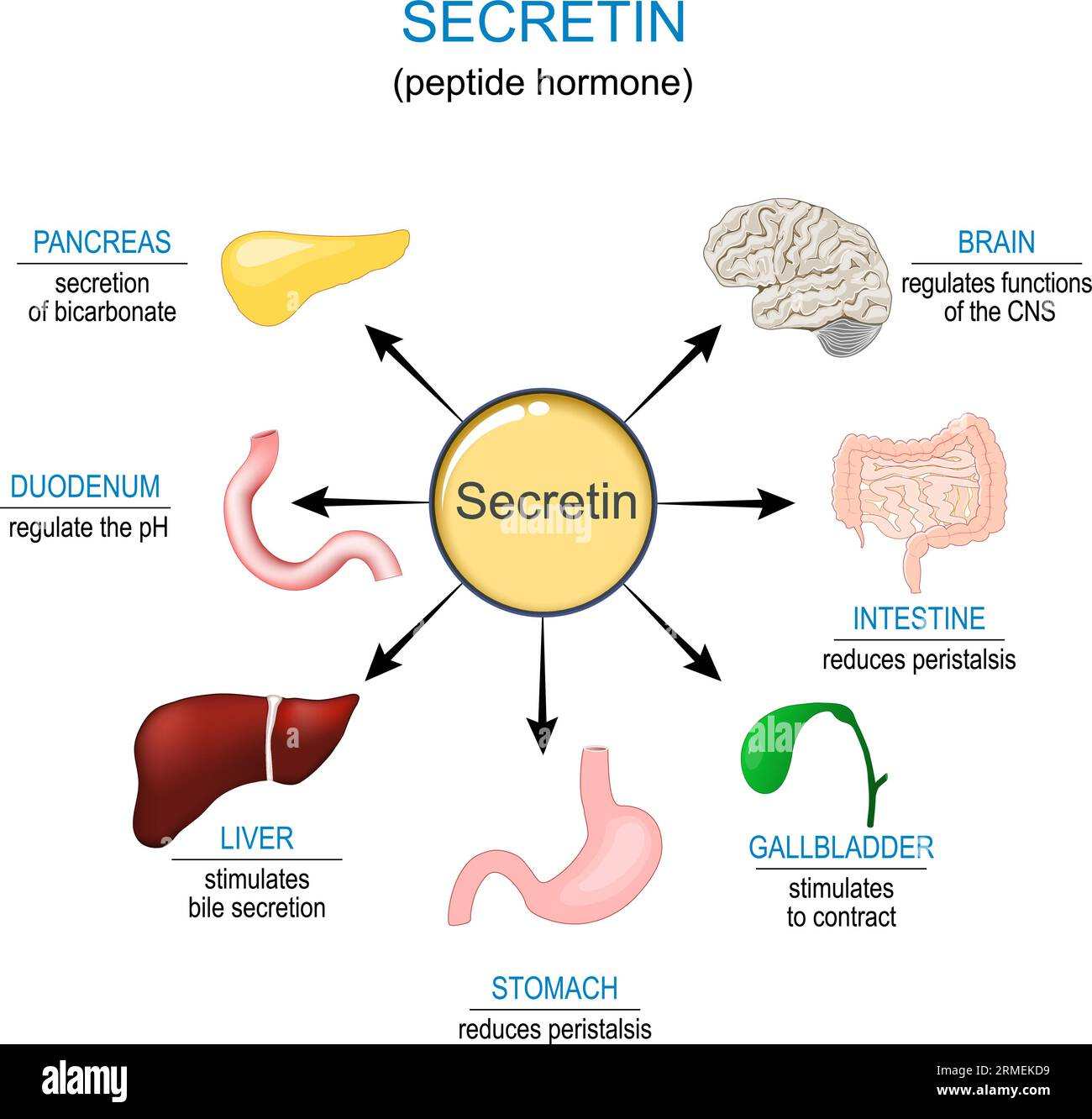
☆ Secretin inhibits gastric contractions, stimulates the secretion of bicarbonate (HCO3-) and water from the gallbladder, and increases bicarbonate secretion from the pancreatic duct cells.
-
What is the function of pepsinogen, and how is it activated? (1)
☆ Pepsinogen, released by gastric Chief cells, is converted to pepsin by hydrochloric acid (HCl) in the gastric lumen. Pepsin mediates the initial digestion of proteins.
-
What is the role of intrinsic factor secreted by parietal cells? (1)
☆ Intrinsic factor is important for the absorption of vitamin B12
-
What stimulates the release of neuropeptide Y, and what is its function? (1)
☆ Neuropeptide Y is stimulated by primary neurons and functions to stimulate appetite.
-
What is the source of leptin secretion and how does its levels correlate with body fat levels? (2)
☆ Leptin is secreted by white adipose tissue, and its levels follow the body's fat levels. It is increased in obesity, suggesting that fat deposition may control appetite via increased leptin levels.
-
What is the function of leptin and how does it relate to appetite regulation? (2)
☆ Leptin acts as a lipostat, informing the brain of the body's energy status based on adipose tissue leptin levels.
☆ It dampens appetite by inhibiting neuropeptide Y (NPY), which stimulates appetite.
-
Does the acuate nucleus (the appetite centre) become leptin-resistant in certain conditions? (1)
☆ Yes, there is evidence suggesting that abnormalities in leptin signaling can lead to leptin resistance in the arcuate nucleus, which correlates with overeating and obesity.
-
What stimulates the release of ghrelin and what effect does it have on appetite? (2)
☆ Ghrelin is released by the stomach and activates NPY-releasing neurons, thereby stimulating appetite.
☆ It is released from the empty stomach but its secretion stops following food intake.
-

What is obestatin, where is it produced, and what is its effect on appetite? (3)
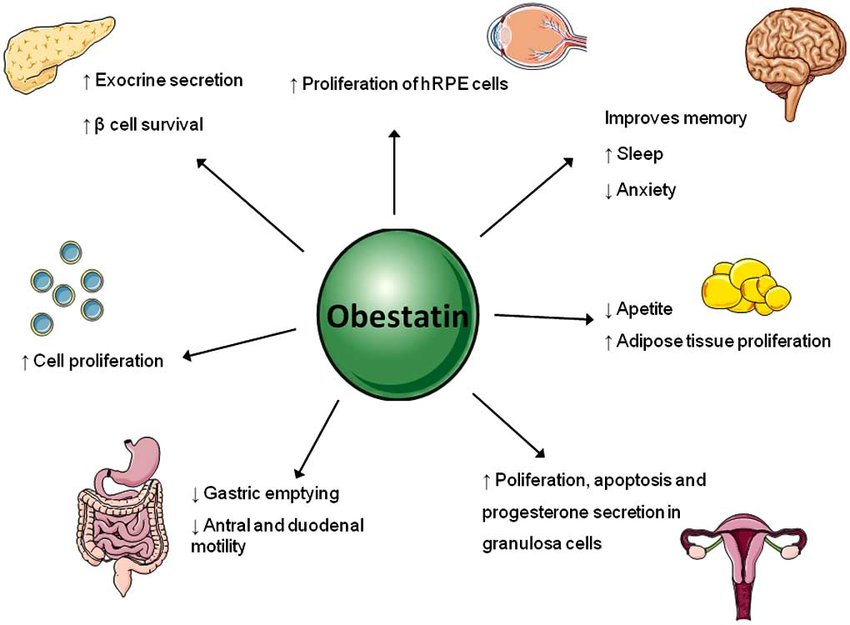
☆ Obestatin is a gene product of ghrelin, produced by epithelial cells of the stomach.
☆ It suppresses appetite and is known to block ghrelin-induced stimulation of food intake
☆ Leading to the suppression of ghrelin-induced weight gain.
-

Define anorexigenic factors and provide examples. (1)

☆ Anorexigenic factors are substances or factors that suppress appetite. Examples include leptin, insulin, peptide YY (PYY), and glucagon-like peptide 1 (GLP-1).
-
Define orexigenic factors and provide examples. (1)

☆ Orexigenic factors are substances or factors that stimulate appetite. Examples include ghrelin, neuropeptide Y (NPY), agouti-related peptide (AgRP), and orexin.
-
What is the role of Angiotensin II in response to hypovolemia? (2)
☆ Angiotensin II promotes aldosterone secretion from the adrenal cortex, which mediates an increase in blood volume and increased blood pressure. It helps maintain blood pressure and fluid balance in the body.
-
Describe the function of Aldosterone and its source in response to hypovolemia. (3)
☆ Aldosterone, secreted from the adrenal cortex, decreases Na+ excretion and promotes the reabsorption of Na+, Cl-, and H2O
☆ Thereby reducing water and Na+ loss while increasing K+ excretion.
☆ This helps raise blood volume and increase blood pressure to correct hypovolemia.
-
What is the role of Vasopressin (antidiuretic hormone) in response to hypovolemia and where is it produced? (3)
☆ Vasopressin, produced by the posterior pituitary, conserves water by inserting water channels in the ducts, promoting water reabsorption by the collecting duct.
☆ It reduces water excretion in the urine, helping to maintain fluid balance in response to hypovolemia.
-
How does Atrial Natriuretic Factor (ANF) contribute to fluid balance during hypovolemia? (3)
☆ ANF, released by the heart in response to stretching of the atrial muscle cells due to increased blood volume, mediates homeostatic control of body water, Na+, and K+.
☆ It increases the excretion of water, Na+, and K+ and decreases blood volume by increasing water loss in the urine.
☆ This is achieved by increasing GFR (Glomerular Filtration Rate), inhibiting sodium reabsorption in the collecting ducts, and inhibiting aldosterone secretion and renin release.
-
Name 2 areas of the digestive tract that have storage functions
☆ Stomach
☆ Colon
-
Name 1 paracrine secretion of the digestive tract and its function
☆ Histamine: Functions to stimulate acid (HCl) secretion by binding to H2 receptors on parietal cells.
-
Name 3 endocrine secretions of the digestive tract
☆ Gastrin
☆ Secretin
☆ Cholecystokinin (CCK)
-
Name 1 lymphoid tissue within the digestive tract
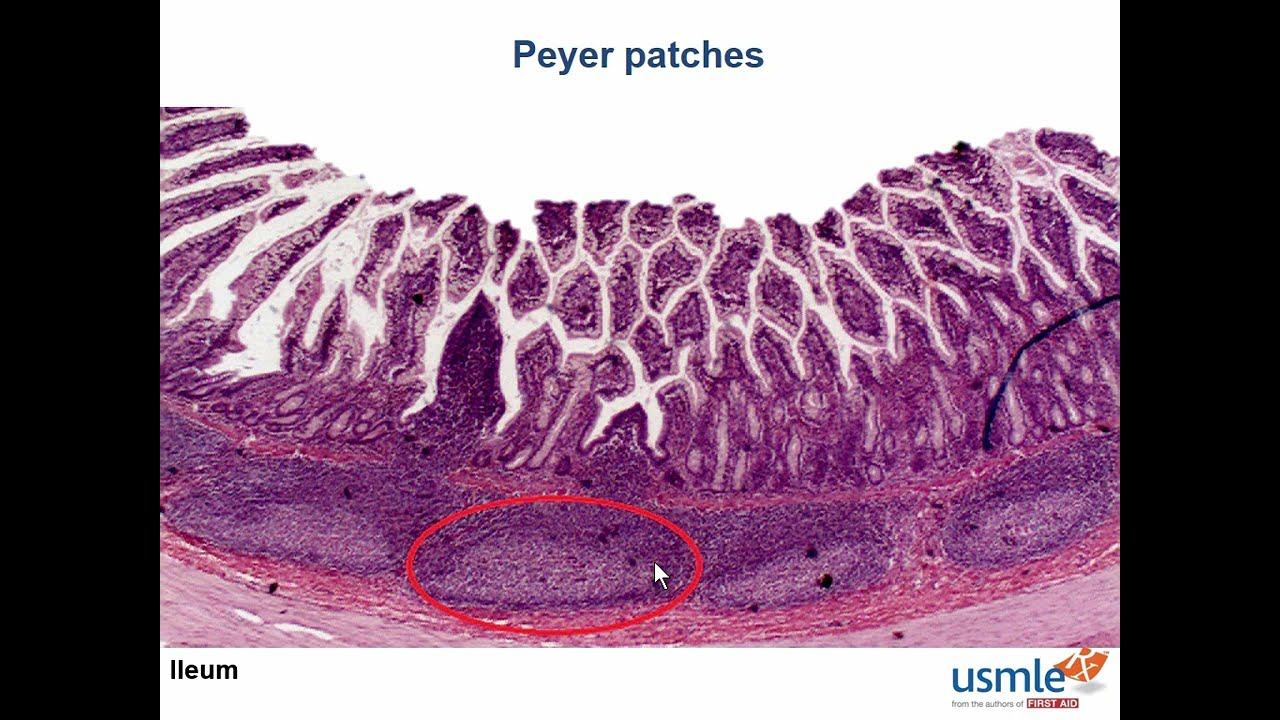
☆ Peyer's patches
-
Name 2 processes by which food is moved along the digestive tract
☆ Peristalsis
☆ Segmentation
-
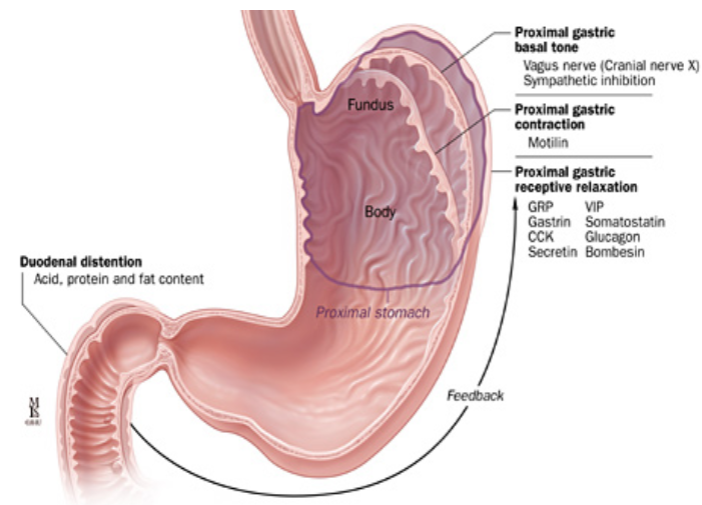
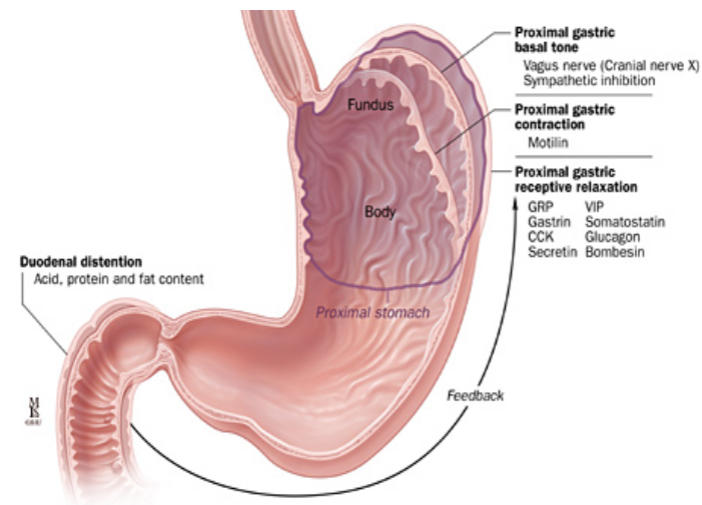
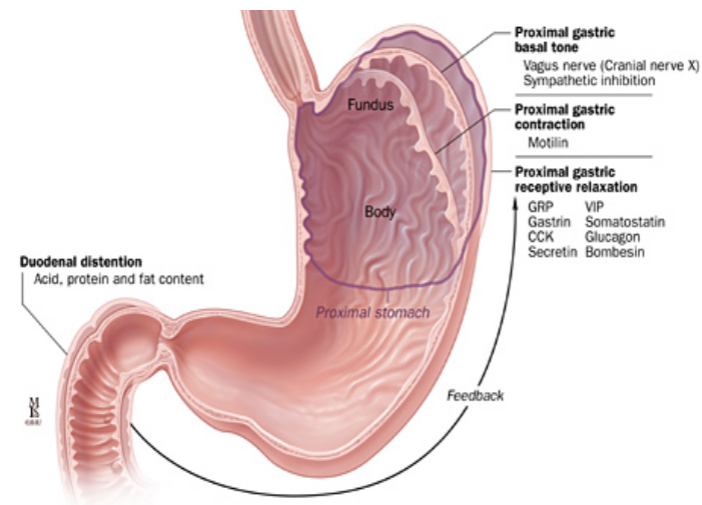
Name 1 process important in the receptive relaxation of the stomach and name 2 substances important in this relaxation
☆ Process: Receptive relaxation of the stomach
☆ Substances: Nitric oxide (NO) and vasoactive intestinal peptide (VIP)
-
List 2 effects of acetylcholine on the gastrointestinal tract
☆ Increased gastrointestinal motility
☆ Increased gastrointestinal secretions
-
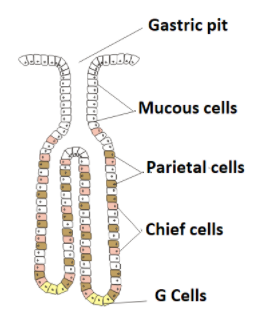
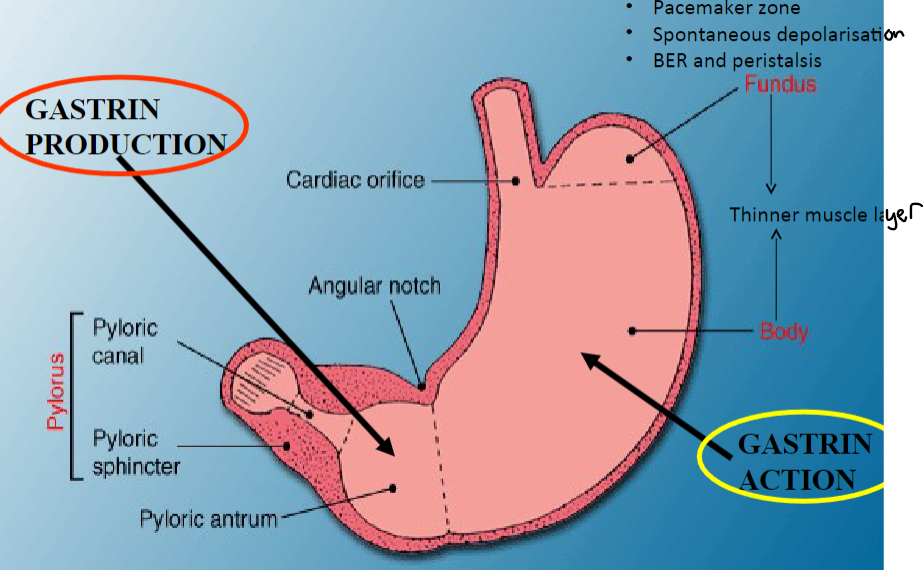
Name the cell type that mediates gastrin release from the antrum
☆ G cells
-
What is the effect of gastrin on parietal cells?
☆ Gastrin stimulates parietal cells to increase acid (HCl) secretion. (1)
-
Name 2 parts of the stomach
☆ Fundus
☆ Antrum
-
Two nerve fibres are important in the local control of the functions of the gastrointestinal tract. Name these and state their functions
☆ Enteric nervous system (ENS): Functions to regulate gastrointestinal motility and secretion locally.
☆ Autonomic nervous system (both sympathetic and parasympathetic branches):
☆ Modulates overall gastrointestinal function and blood flow
-
State how fast/slow the following foods are emptied from the stomach:
Rice:
Rump steak:
Fatty bacon cooked in pure lard:
Rice: Fast
Rump steak: Slow
Fatty bacon cooked in pure lard: Slowest
-
The gastrointestinal tract is often taught to have a “little brain” of its own that can regulate its functions without input from the higher centres. What is the name of this “little brain”?
Enteric nervous system (ENS)
-
What neurotransmitter is primarily involved in the neural mechanism for this relaxation?
Nitric oxide
-
What function does the stomach serve regarding ingested food? (1)
☆ Accommodation & Storage: It acts as a reservoir for food and gradually releases it into the small intestine.
-
What processes occur in the stomach to break down food? (1)
☆ Mechanical and Enzymatic Breakdown: Muscular contractions mix food with gastric juices, and enzymes like pepsin begin protein digestion.
-
What role does the stomach play in the delivery of chyme to the duodenum? (1)
☆ Slow Delivery of Chyme to Duodenum: It controls the release of chyme into the small intestine to prevent overwhelming it with acidic content.
-
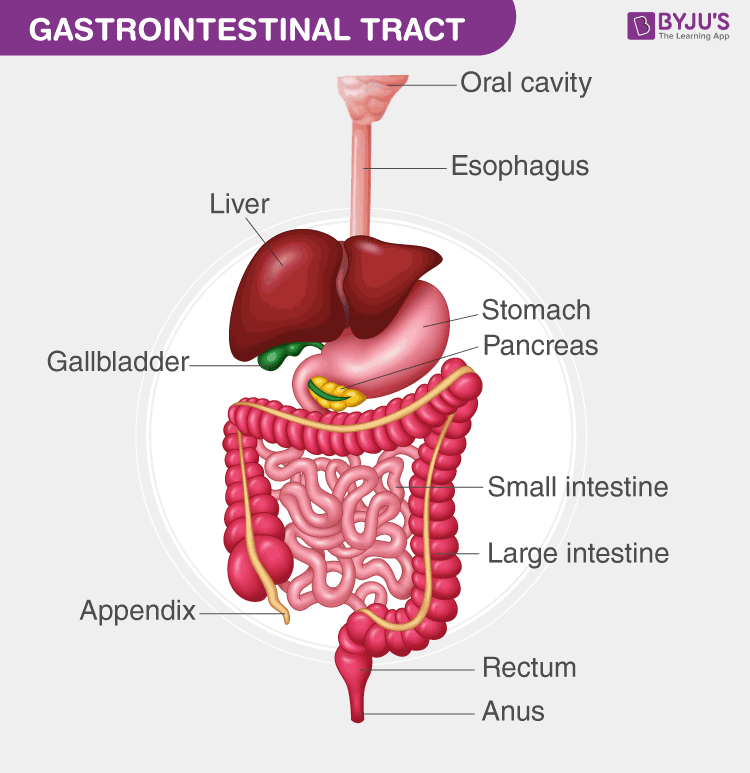
Where is food stored during the first stage of digestion? (4)
☆ Stomach: Acts as a reservoir for food storage.
☆ Fundus and body of the stomach relax to accommodate large volumes of food (~1.5L).
☆ Vagal reflex inhibits smooth muscle tone, allowing for fundic relaxation via mechanoreceptors.
☆ Antral region mixes and grinds food with gastric secretions for digestion.
-
What is the role of the colon/rectum in digestion? (1)
☆ Colon/Rectum: Responsible for the storage of indigestive residues and fecal matter.
-
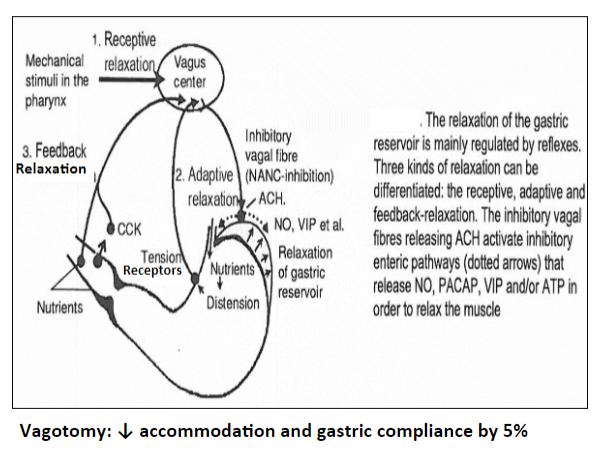
Picture demonstrating how the ANS enables the storage of food into the stomach
-
What are the components of gastric juice stored in the stomach? (5)
Stomach stores 2-3 litres of gastric juice/24hr, containing:
☆ Mucus: Acts as a lubricant and protective barrier, secreted by goblet cells and mucus neck cells.
☆ Lipase: Converts triglycerides to fatty acids and glycerol.
☆ Pepsin: Secreted by chief cells or peptic cells as pepsinogen for protein digestion.
☆ HCl: Secreted by parietal cells, important for defense.
☆ Intrinsic Factor: Secreted by parietal cells, essential for vitamin B12 absorption.
-
What are paracrine secretions commonly referred to as? (4)
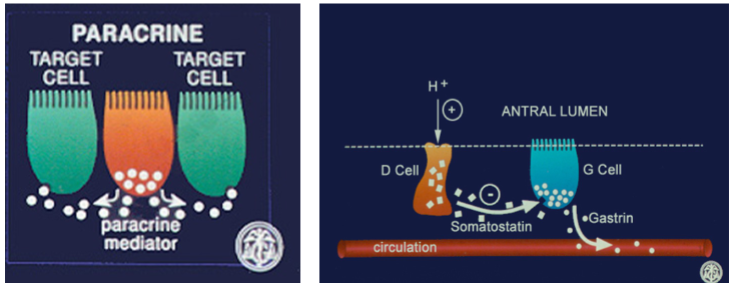
☆ Often called "local hormones".
☆ Secreted from cells in the mucosa.
☆ Act locally on adjacent cells via the interstitial fluid.
☆ Example: Somatostatin inhibits gastrin release in the stomach.
-
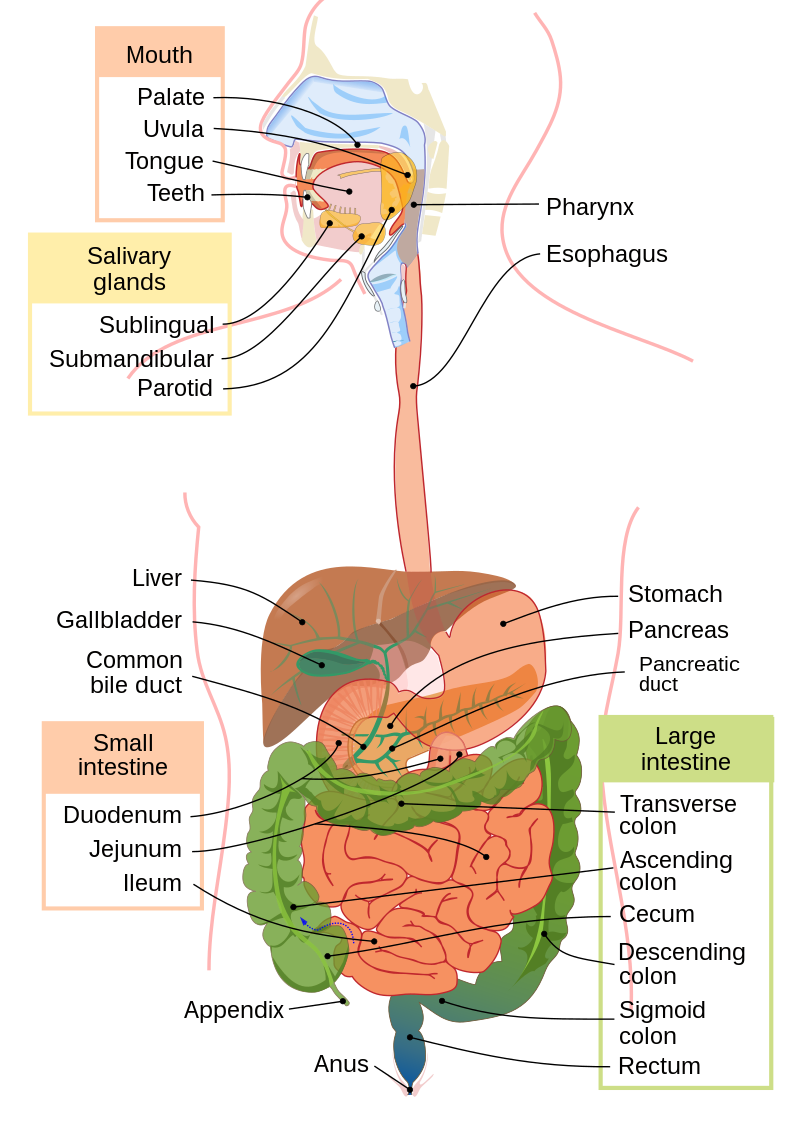
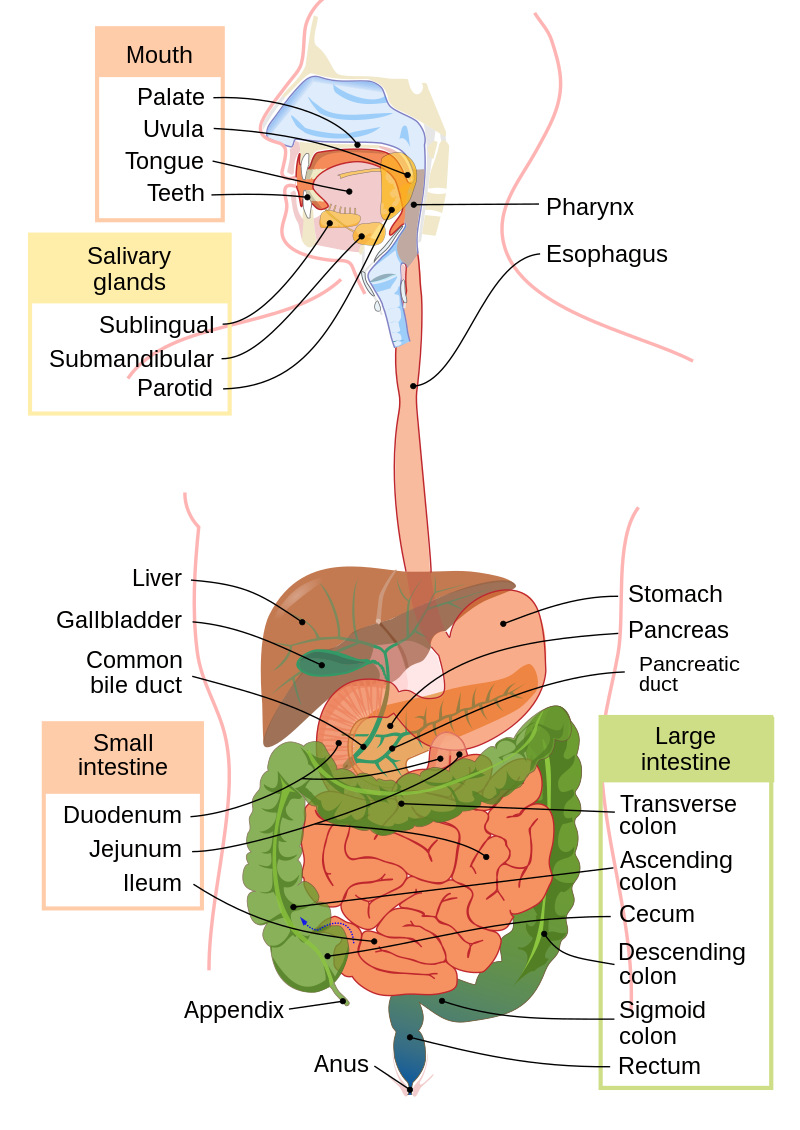
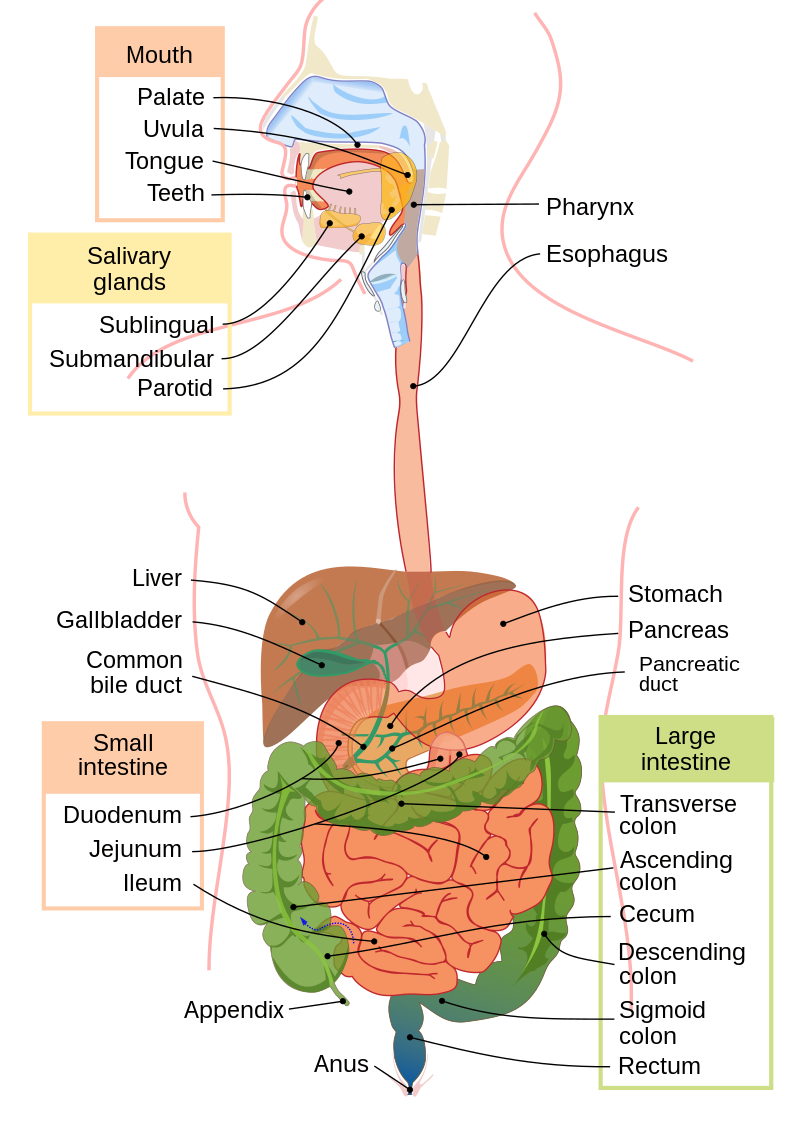
What are the main exocrine secretions involved in digestion? (5)
Salivary Glands: Mucus for lubrication during mastication and speech; lipase.
Gastric Glands: Hydrochloric acid, pepsin, mucus.
Pancreas: Bicarbonate ions, enzymes (e.g., amylase, lipase, carboxypeptidase).
Liver: Bile salts, bile acids.
Secretions from numerous glands with ducts enter the lumen of the gut and are involved in digestion, lubrication, and protection.
-
What are the characteristics and examples of endocrine secretions? (4)
Secretions called 'hormones' synthesized by ductless glands enter the bloodstream.
They travel to their target tissue(s) where they bind to specific receptors to elicit their effects.
Examples include:
Gastrin: Released from G-cells in the stomach antrum.
Secretin: Produced in the duodenal mucosa.
Pancreozymin-cholecystokinin: Also produced in the duodenal mucosa.
Insulin: Produced by pancreatic β-cells.
Exocrine, endocrine, and paracrine secretions regulate active digestion, control gastric motility, and contribute to energy homeostasis.
-
What is the process of absorption and where does it mainly occur? (5)
Absorption is the transportation of nutrients resulting from digestion across the intestinal epithelium into the blood (e.g., glucose, amino acids) or lymph via lacteals for fats/lipids.
Mainly occurs in the small intestine.
Fluid absorption also occurs in the small intestine and colon.
The colon absorbs 90% of water, reducing volume to 200ml of semi-solid fecal matter.
Disorders of fluid secretion and absorption, along with motility, play a crucial role in the pathogenesis of diarrhea.
-
What is the process of absorption and where does it mainly occur? (5)
Absorption is the transportation of nutrients resulting from digestion across the intestinal epithelium into the blood (e.g., glucose, amino acids) or lymph via lacteals for fats/lipids.
Mainly occurs in the small intestine.
Fluid absorption also occurs in the small intestine and colon.
The colon absorbs 90% of water, reducing volume to 200ml of semi-solid fecal matter.
Disorders of fluid secretion and absorption, along with motility, play a crucial role in the pathogenesis of diarrhea.
-
What are the functions of the movements of the muscular wall in the digestive system? (6)
The movements, mostly facilitated by smooth muscle (except extreme ends of the upper esophagus/rectum), allow:
Storage, such as in the proximal stomach and descending colon.
Movement from one region to another (law of gut); mass evacuation.
Mechanical degradation, such as in the gastric antrum.
Mixing of lumen contents, such as in the small intestine.
Transport of nutrients, water, urea, and electrolytes.
Facilitation of digestion and absorption.
-
Where do drugs and some products of normal metabolism leave the body? (4)
Drugs and some products of normal metabolism may leave the body through: i. Saliva ii. Bile, bilirubin iii. Faeces iv. (Vomit)
Indigestible food residues, such as tomato skin, leave the body in the faeces.
-
What are the characteristics of the gut epithelium in terms of defence? (4)
☆ Like the skin and airways, the gut epithelium is an interface with the "contaminated" outside world, exposed to the external environment.
☆ The intestine is the largest mucosal surface in the body and is likely exposed to the heaviest burden of environmental antigens.
☆ Similar to the skin, if there is a breach in the barrier, "toxins" can enter the blood.
☆ Additionally, it is the largest lymphoepithelial organ.
-
What mechanisms protect the gut from harmful substances and pathogens? (1)
Sight, smell, and taste alert us to harmful food substances.
Vomit reflex helps expel potentially harmful substances.
Acid in the stomach (HCl) kills most harmful bacteria.
Mucus secretions provide a protective barrier.
Natural bacterial flora prevents colonization by harmful bacteria.
Aggregation of lymphoid tissue, such as Peyer’s patches, can mount a response to food-borne antigens and analyze/respond to pathogenic microbes.
Peyer’s patches, located in the lamina propria layer of the mucosa and extending into the submucosa of the ileum, contain mucosal-associated lymphatic tissue with white blood cells and lymphocytes, offering protection against infection.
-
What are the metabolic functions of the liver in the abdominal cavity? (1)
The liver, weighing about 1.3 kg in an adult, is a major metabolic organ.
It is involved in carbohydrate, nitrogen, and lipoprotein metabolism.
Additionally, it produces bile from cholesterol.
-
What enables food storage in the stomach? (4)
☆ Empty stomach has a small volume.
☆ Receptive relaxation of the fundus and body of the stomach occurs.
☆ Stomach can accommodate approximately 1.5 liters of food.
☆ Controlled by parasympathetic nerves and vagus inhibitory fibers.
-
What enables food storage in the stomach? (4)
Empty stomach has a small volume.
Receptive relaxation of the fundus and body of the stomach occurs.
Stomach can accommodate approximately 1.5 liters of food.
Controlled by parasympathetic nerves and vagus inhibitory fibers.
-
What are the processes involved in the movement of food into the duodenum? (6)
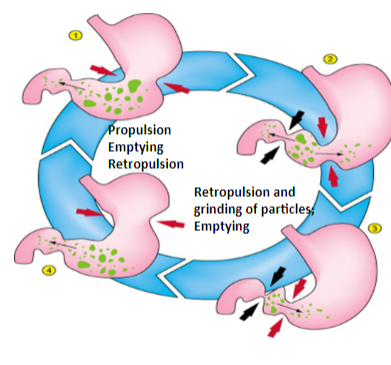
Ripples of contraction move the food towards the antrum, facilitated by a thicker muscle layer.
The pyloric sphincter is often relaxed but closes upon the arrival of a peristaltic wave.
Repulsion of chyme causes the opening of the pyloric sphincter.
Small partially digested material is squirted through the pyloric sphincter into the duodenum.
Repulsion of antral contents backward towards the body allows mixing/grinding, creating a sieving effect where viscous and solid matter are retained in the stomach.
-
Picture demonstrating how the ANS enables food storage in the stomach:
-
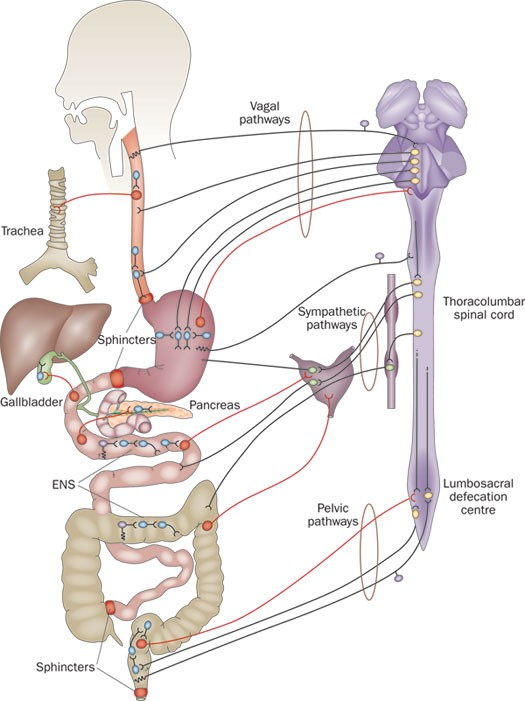
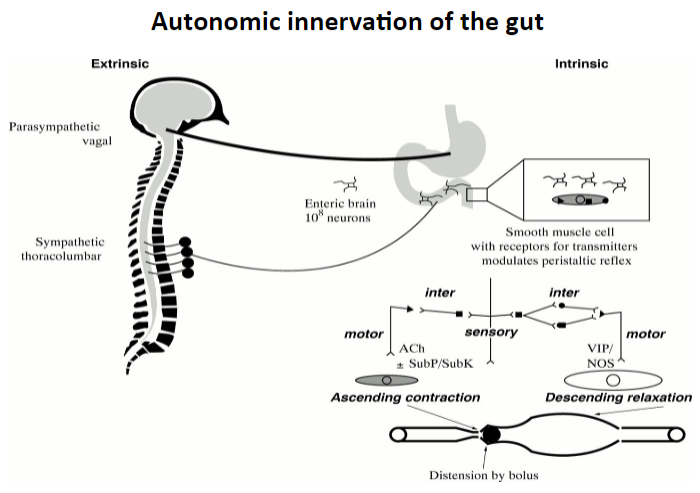
Picture demonstrating the autonomic innervation of the gut (intrinsic and extrinsic):
-
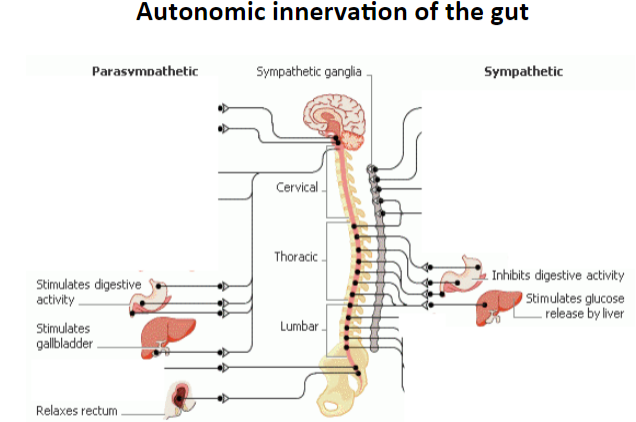
Picture demonstrating the autonomic innervation of the gut:
-
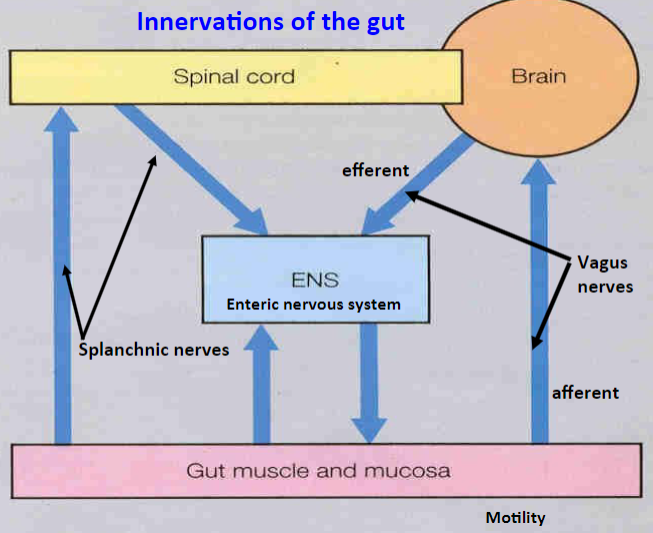
Picture demonstrating the innervations of the gut:
-
Picture demonstrating the guts integrated response to a meal:
-
What are the different types of control in the digestive system? (5)
Endocrine
Paracrine
Neural
Vago-vagal reflex
Enteric or local reflex
Metabolic, influenced by the type of food eaten.
-
What are the characteristics of endocrine control in the digestive system? (2)
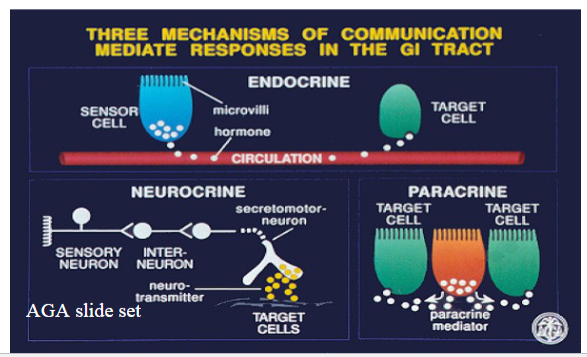
Hormones are carried in the blood from their site of production to their target site.
All hormones produced by the gut are peptides, consisting of a sequence of amino acids.
-
Diagram demonstrating the parts of the stomach:
-
Picture demonstrating gastrin mediated effects:
-
Picture demonstrating paracrine control:
-
What are the characteristics of the enteric nervous system or local reflex in the digestive system? (5)
Two intrinsic nerve fibers are present in the gut:
Myenteric plexus (Auerbach’s plexus) for motor function.
Submucosal plexus (Meissner’s plexus) for intestinal secretions.
They reflexively regulate GI functions entirely within the wall of the gut.
Connected to the central nervous system (CNS) by parasympathetic and sympathetic fibers, but can function autonomously without these connections.
Effects are mediated entirely by the enteric nervous system, the third component of the autonomic nervous system (ANS).
It has a similar number of neurons (100 million) as the spinal cord.
Neurotransmitters involved include acetylcholine (ACh) and nitric oxide (NO).
-
What are the intrinsic neuronal plexuses present in the gut wall? (2)
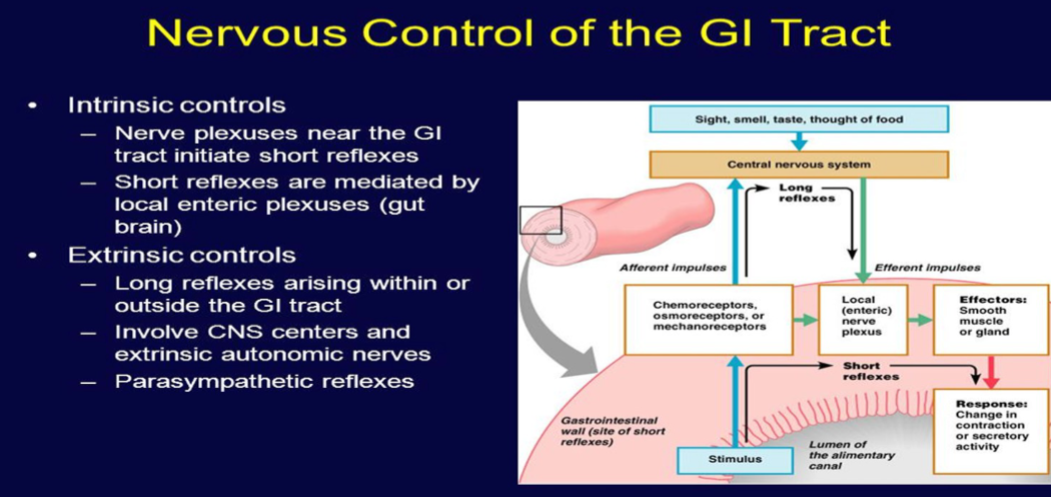
Submucosal Meissner plexus: Regulates the digestive glands.
Myenteric Auerbach plexus: Primarily connected with gut motility.
-
What are the characteristics of Auerbach’s plexus in the gut? (3)
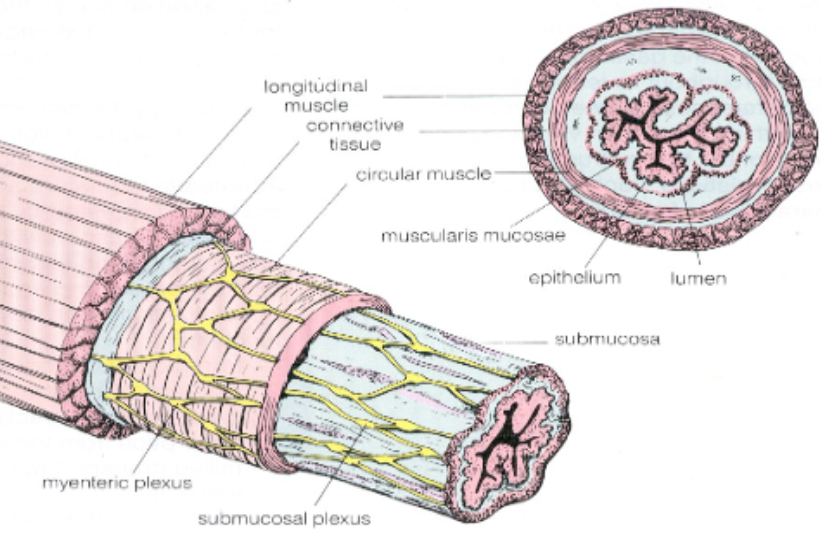
Most prominent plexus.
Cholinergic innervation increases gastric motility and secretion.
Adrenergic stimulation decreases gastric motility and secretion.
-
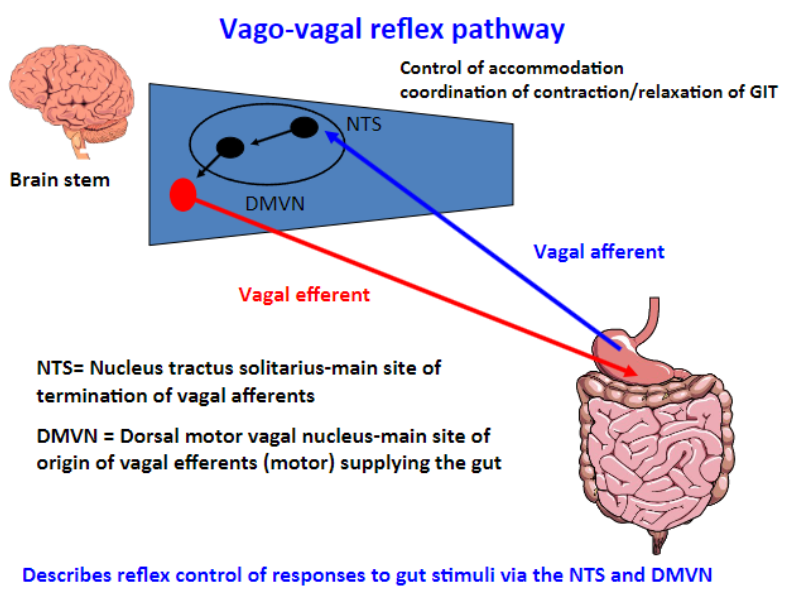
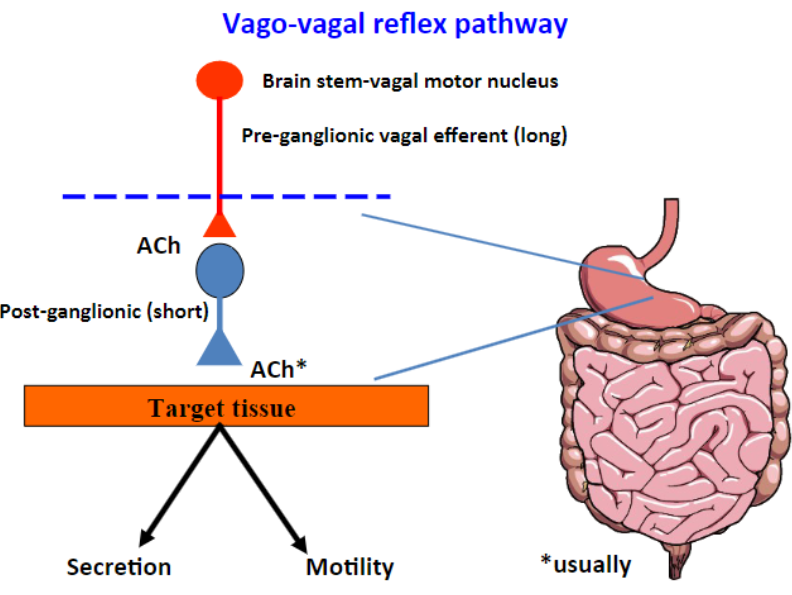
What is the Vago-vagal reflex? (6)
It describes a reflex in which both the afferent (sensory) and efferent (motor) axons are in the vagus nerve trunk.
It is a reflex circuit within the gastrointestinal tract (GIT).
The pathway involves the brain stem, specifically the medulla.
This reflex control of responses to gut stimuli occurs via the Nucleus Tractus Solitarius (NTS) and Dorsal Motor Nucleus of Vagus (DMNV) in the brain, collectively known as the dorsal vagal complex.
The reflex is active during the receptive relaxation of the stomach in response to swallowing, and it involves a loop from the stomach to the brain and then back to the stomach, resulting in active contraction and relaxation of the smooth muscles of the stomach.
It also promotes motility and acid secretion in the stomach.
-
Picture demonstrating the vago-vagal reflex pathway (focus on the NTS and DMVN):
-
Picture demonstrating the vago-vagal reflex pathway (focus on the target tissue):
-
How does the type of food eaten influence metabolic control and gastric emptying? (5)
The rate of emptying from the stomach is dependent upon the material's ability to be absorbed.
Carbohydrates are emptied quickly into the duodenum.
Proteins result in slow emptying from the stomach.
Fatty foods exhibit even slower emptying.
Fatty acids in the duodenum decrease gastric emptying by increasing the contractility of the pyloric sphincter.
-
What are the characteristics of peristalsis in the digestive system? (4)
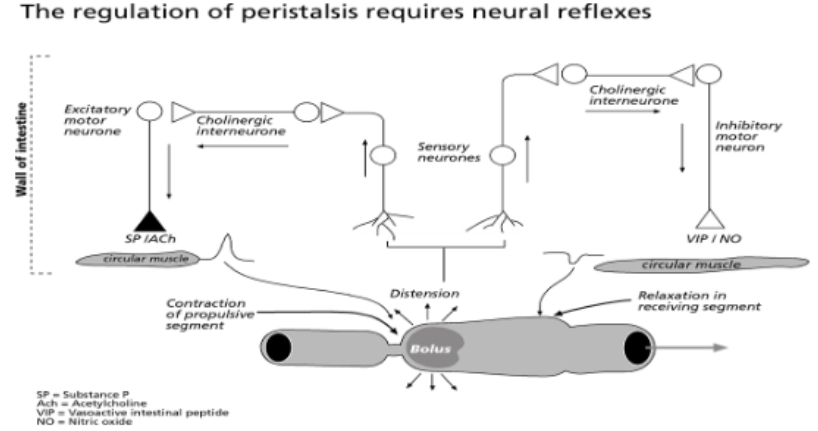
Peristalsis is slower in the large intestine compared to the small intestine.
It involves a wave of propulsive contractions that move the contents of the gut towards the anus.
Contraction is initiated by distension of the gut.
Peristalsis is controlled by vagal inhibitory fibers (VIP, NO) and excitatory fibers (ACh, SP).

