-
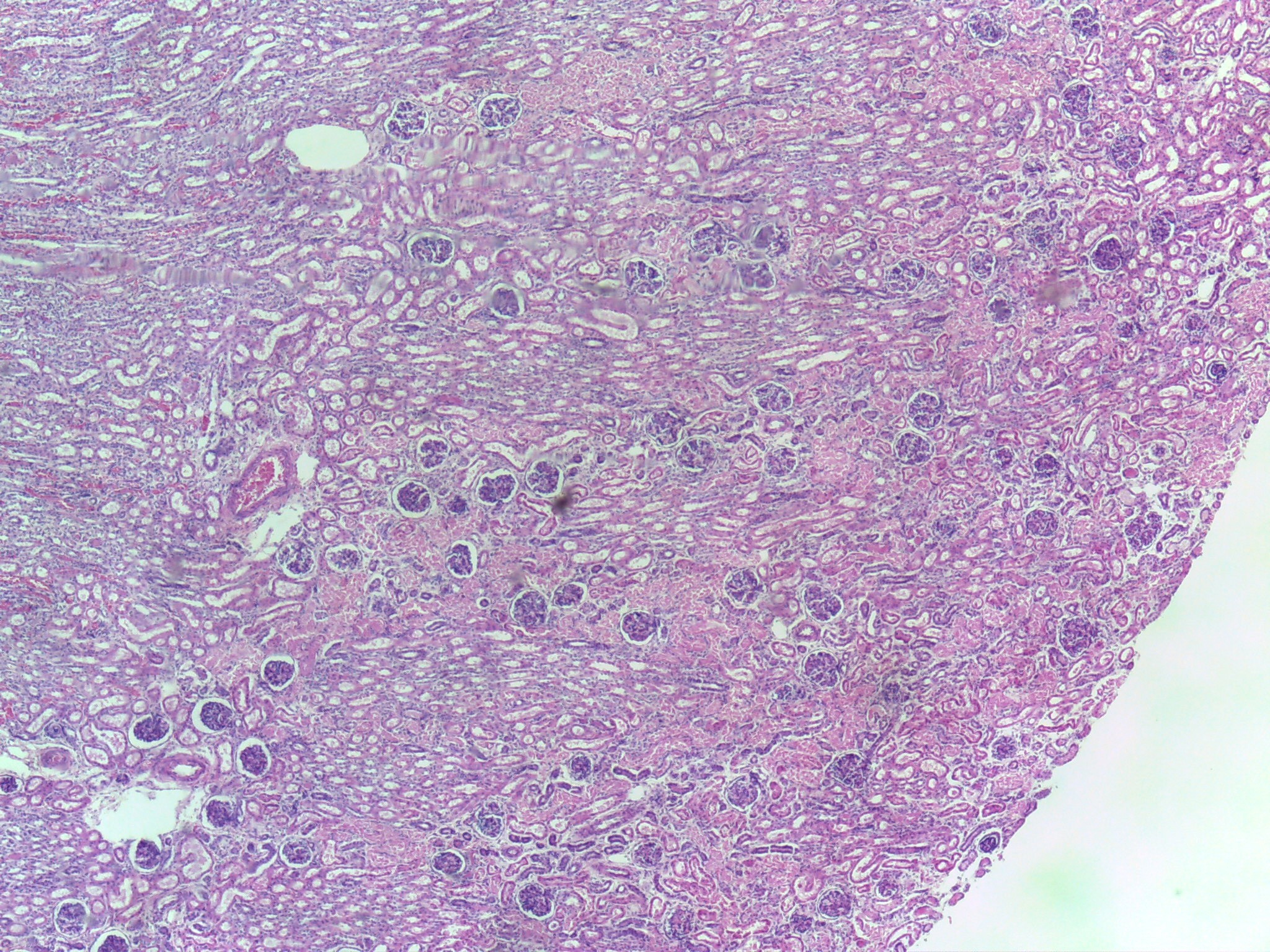
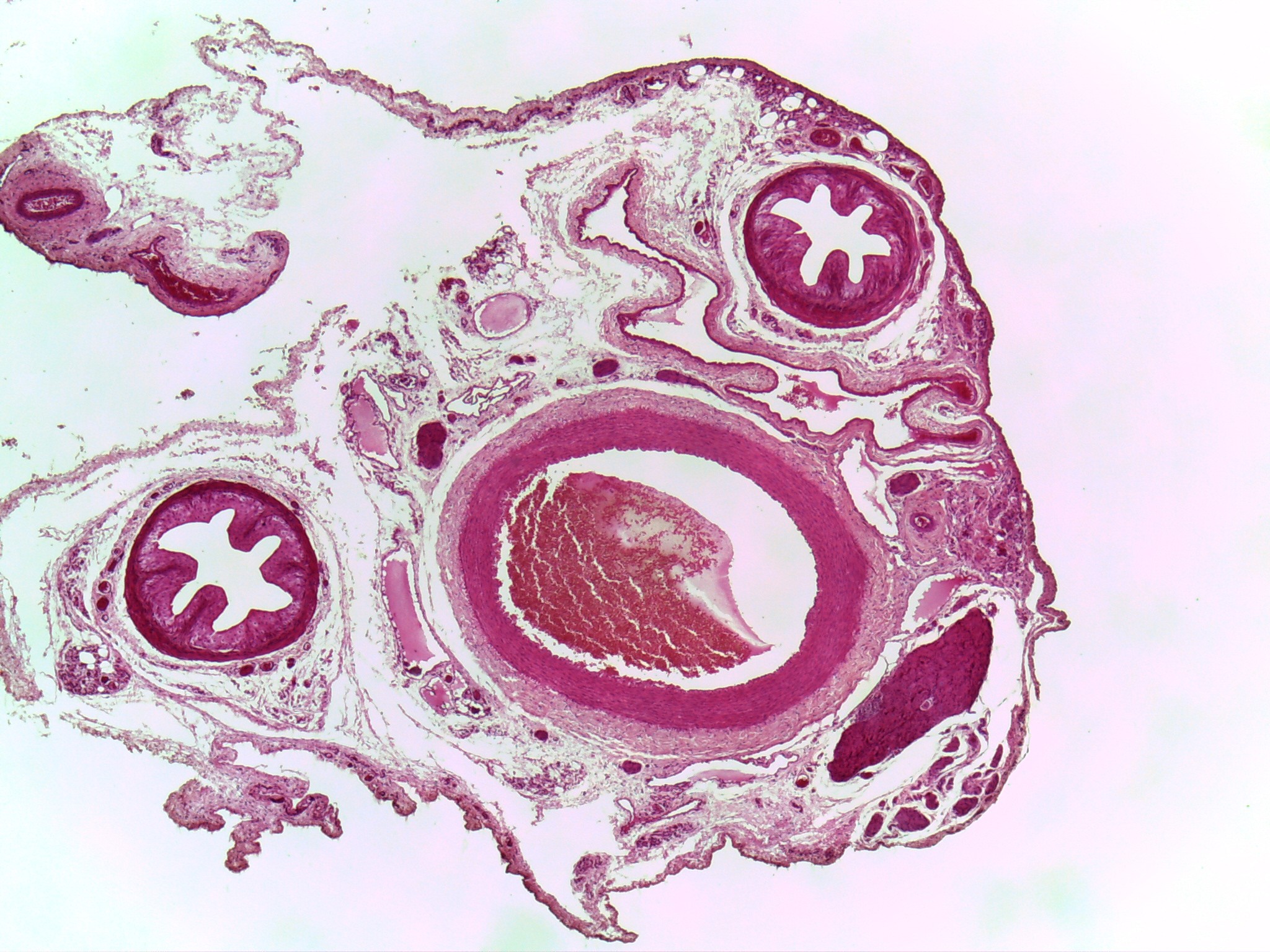
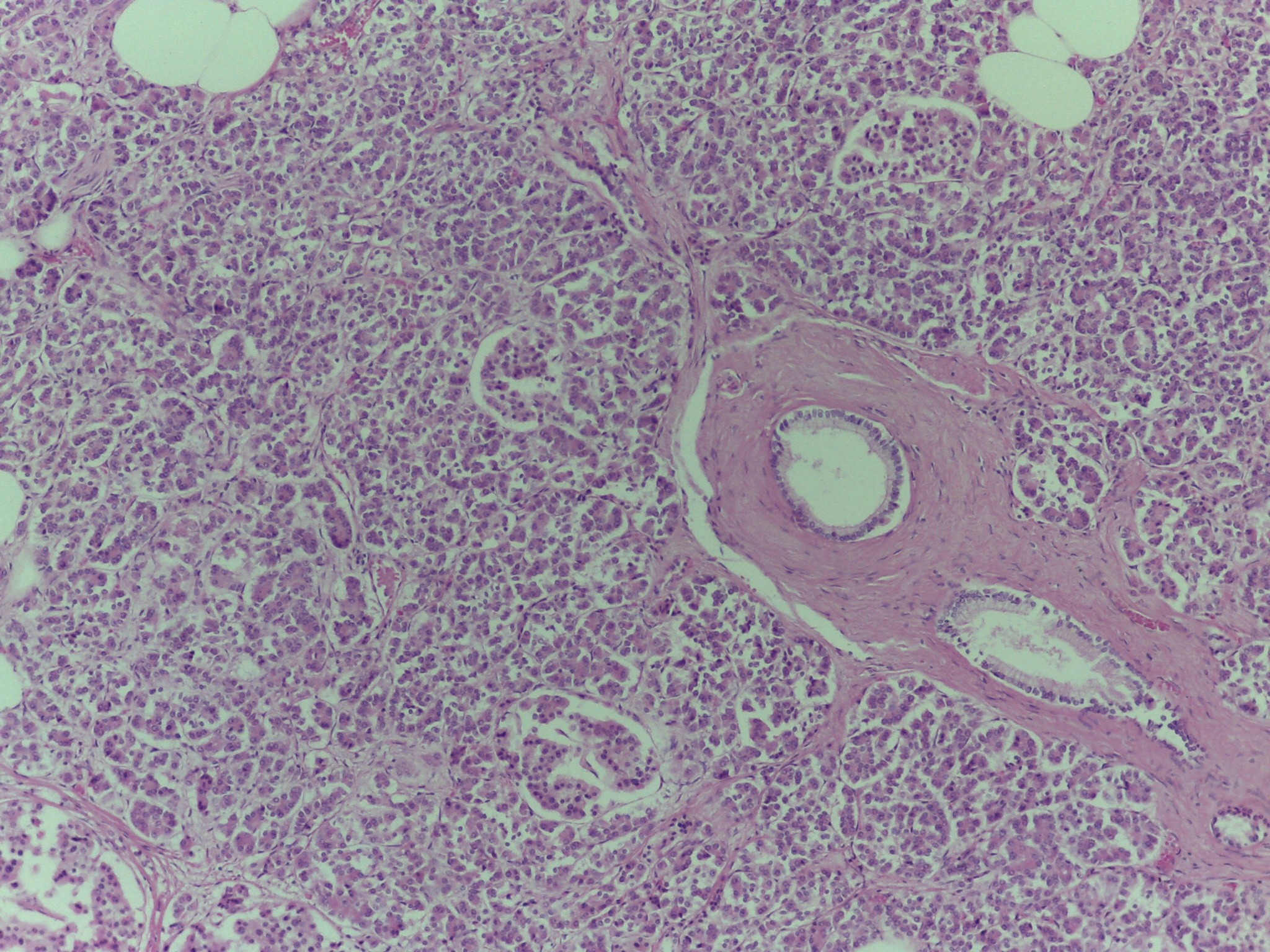
Kidney - (Low mag.)
Tissue: Simple Squamous Epithelial Tissue
Simple Cuboidal Epithelial Tissue
Presence of renal corpuscles along renal tubules allows one to identify this organ as the kidney.
-
Kidney
Tissue: Simple Squamous Epithelial Tissue
Simple Cuboidal Epithelial Tissue
Low magnification slide image of the kidney.
Presence of renal corpuscles along renal tubules allows one to identify this organ as the kidney.
Often lower power allows initial identification of the organ.
-
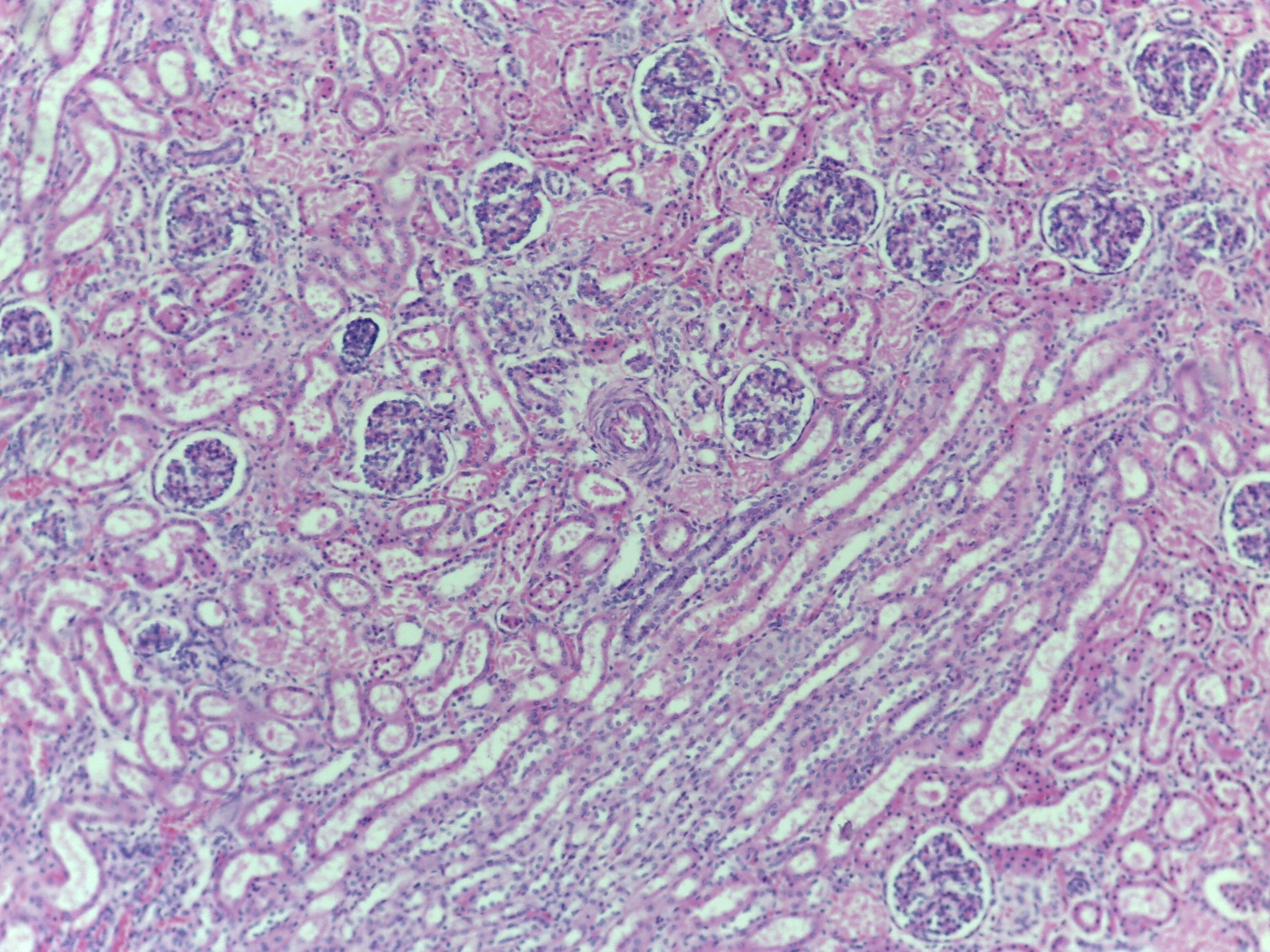
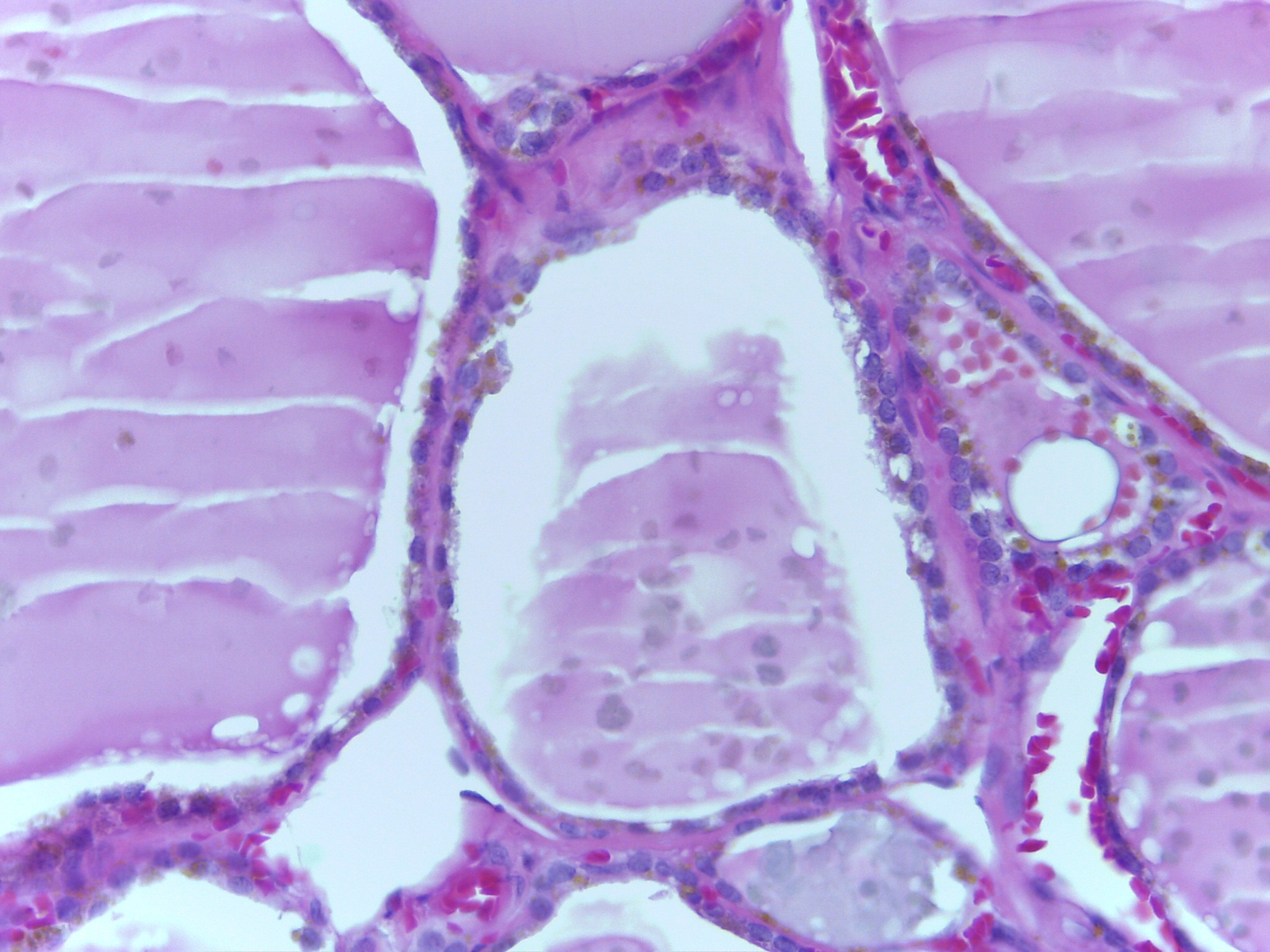
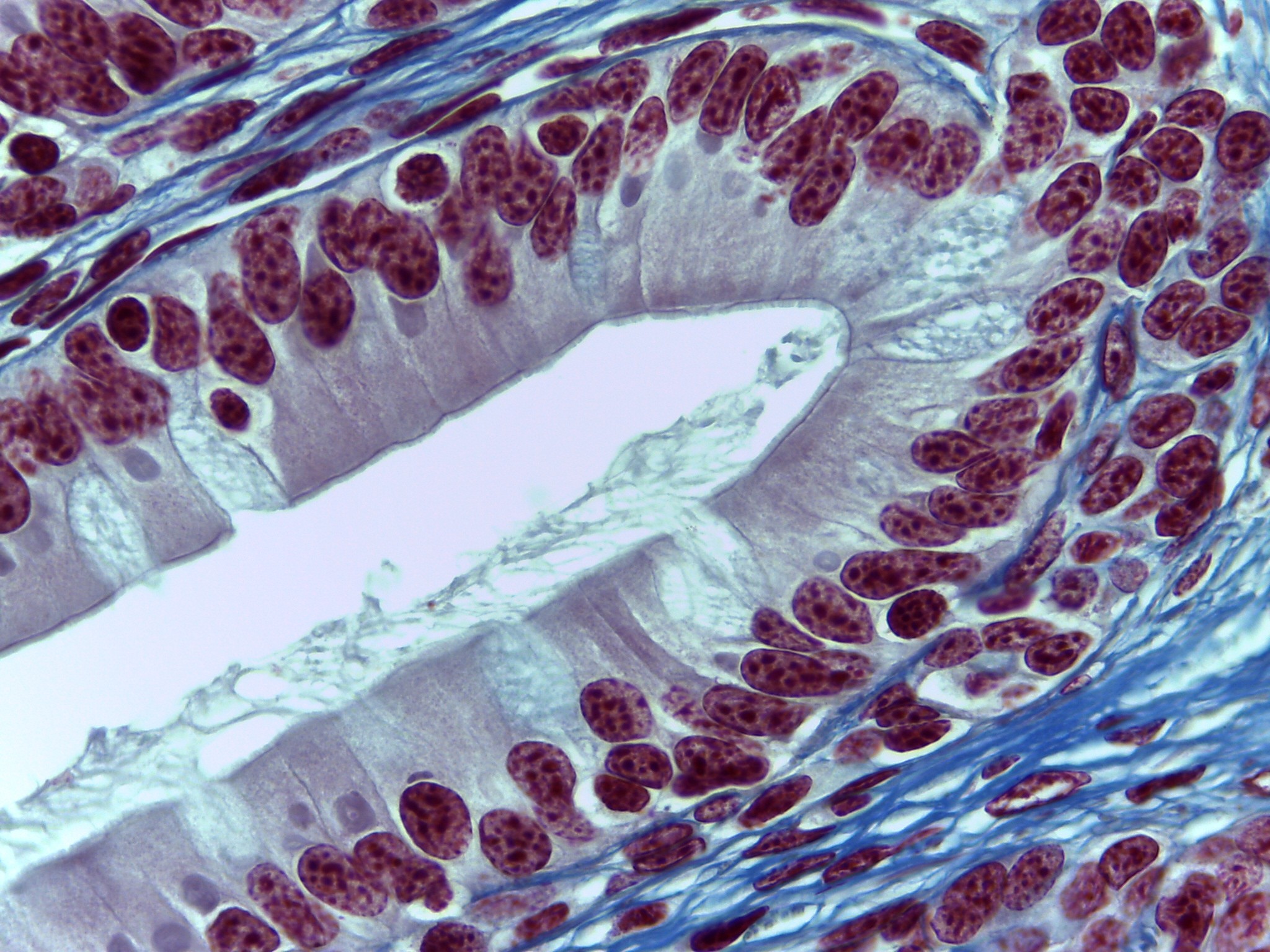
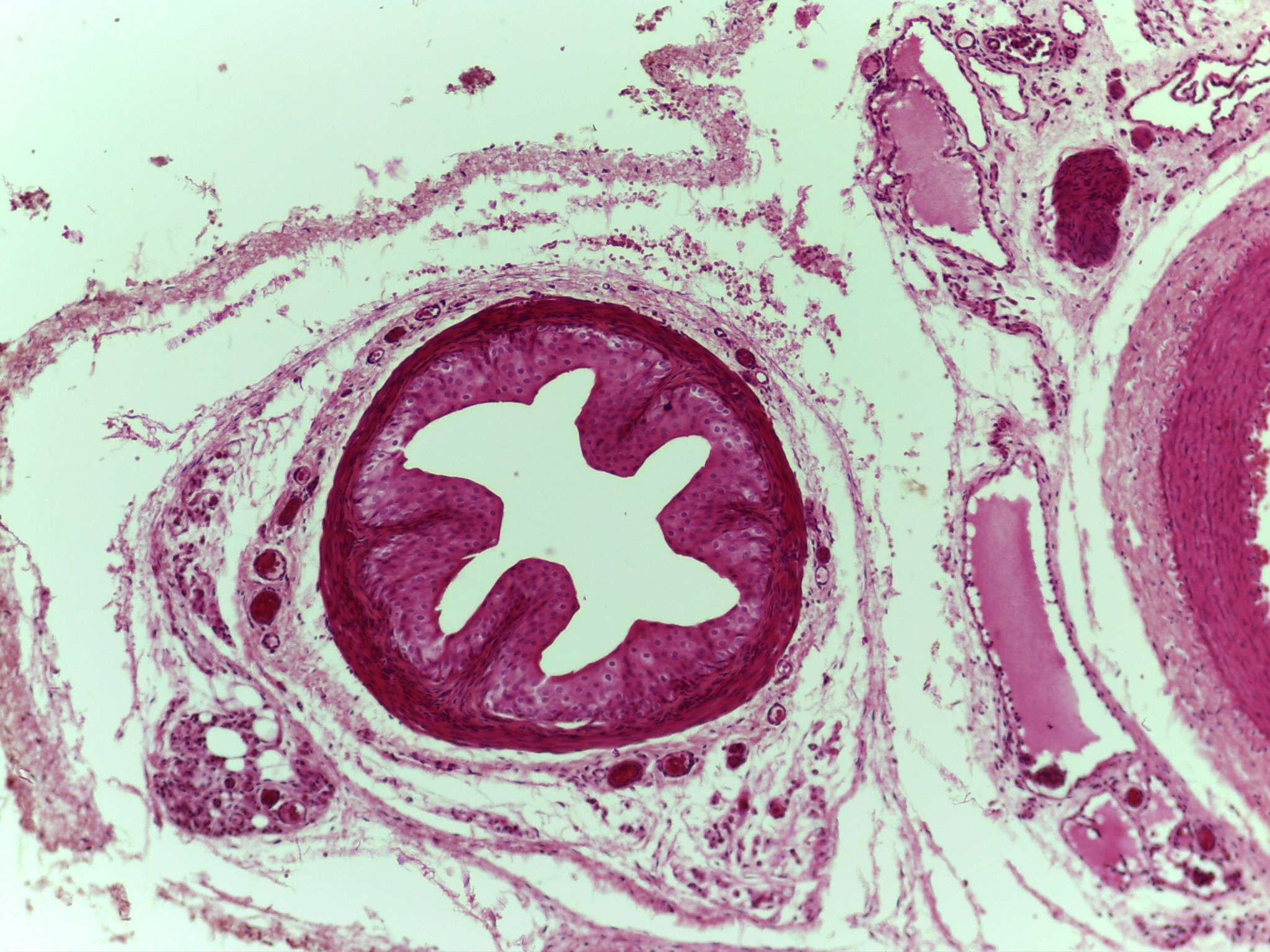
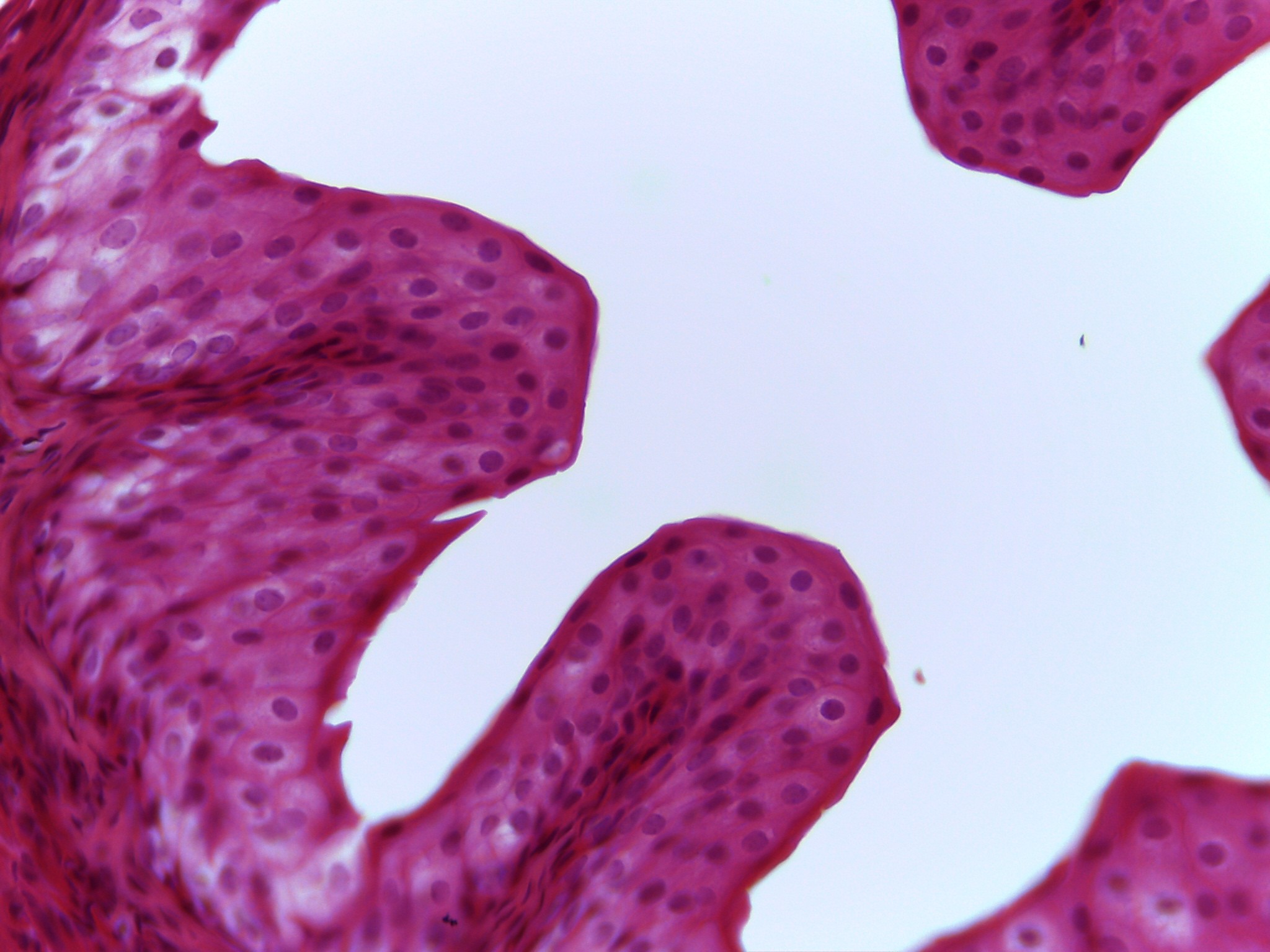
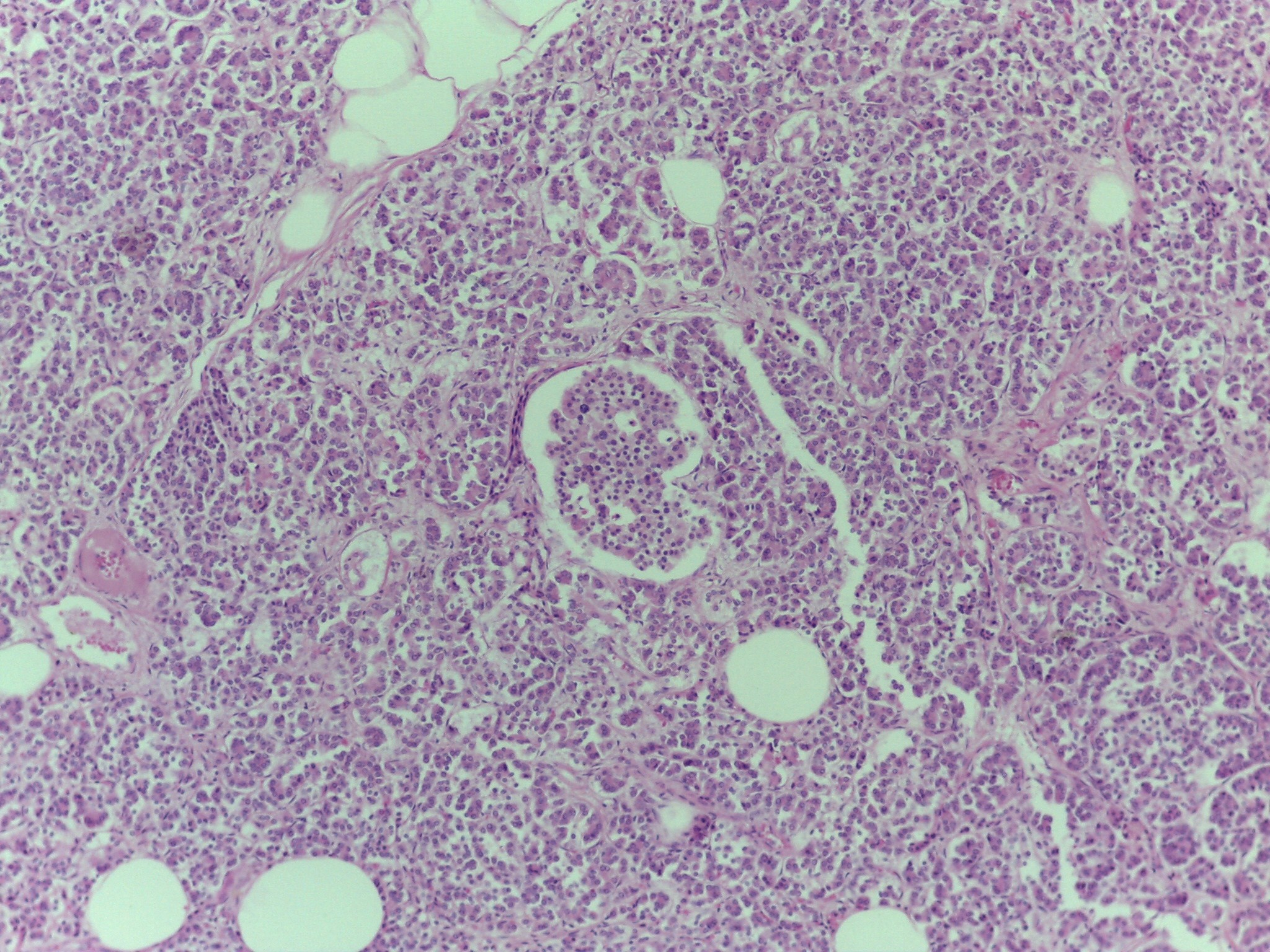
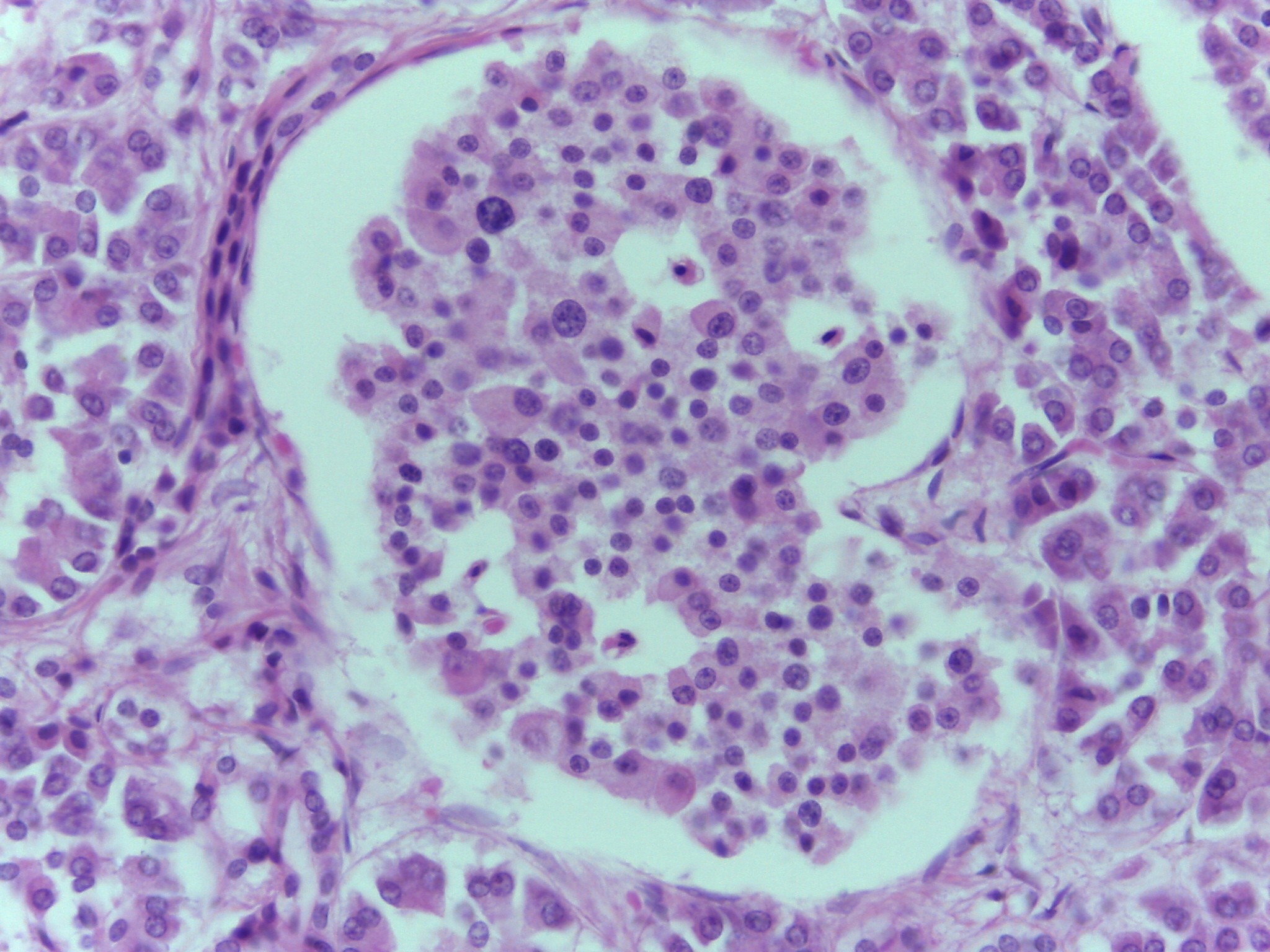
Renal Corpuscles - (High mag. of two renal corpuscles)
Tissue: Simple Squamous ET
This magnification allows you to identify the outer Bowman’s capsule and the inner glomerulus.
Function of glomerulus is diffusion.
Function of Bowman’s capsule is filtration.
Consist of a glomerulus which is surrounded by the Bowman’s capsule
-
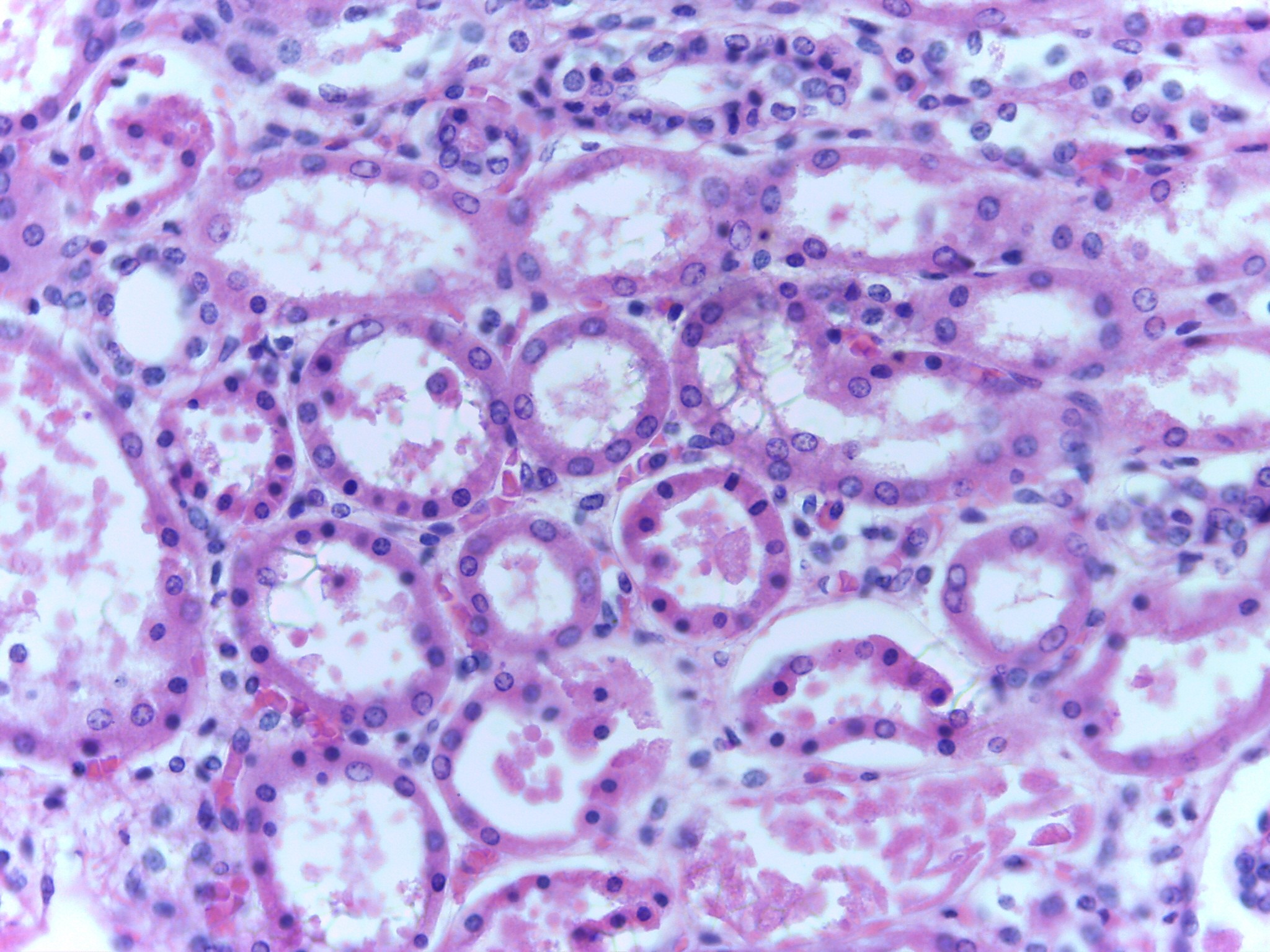
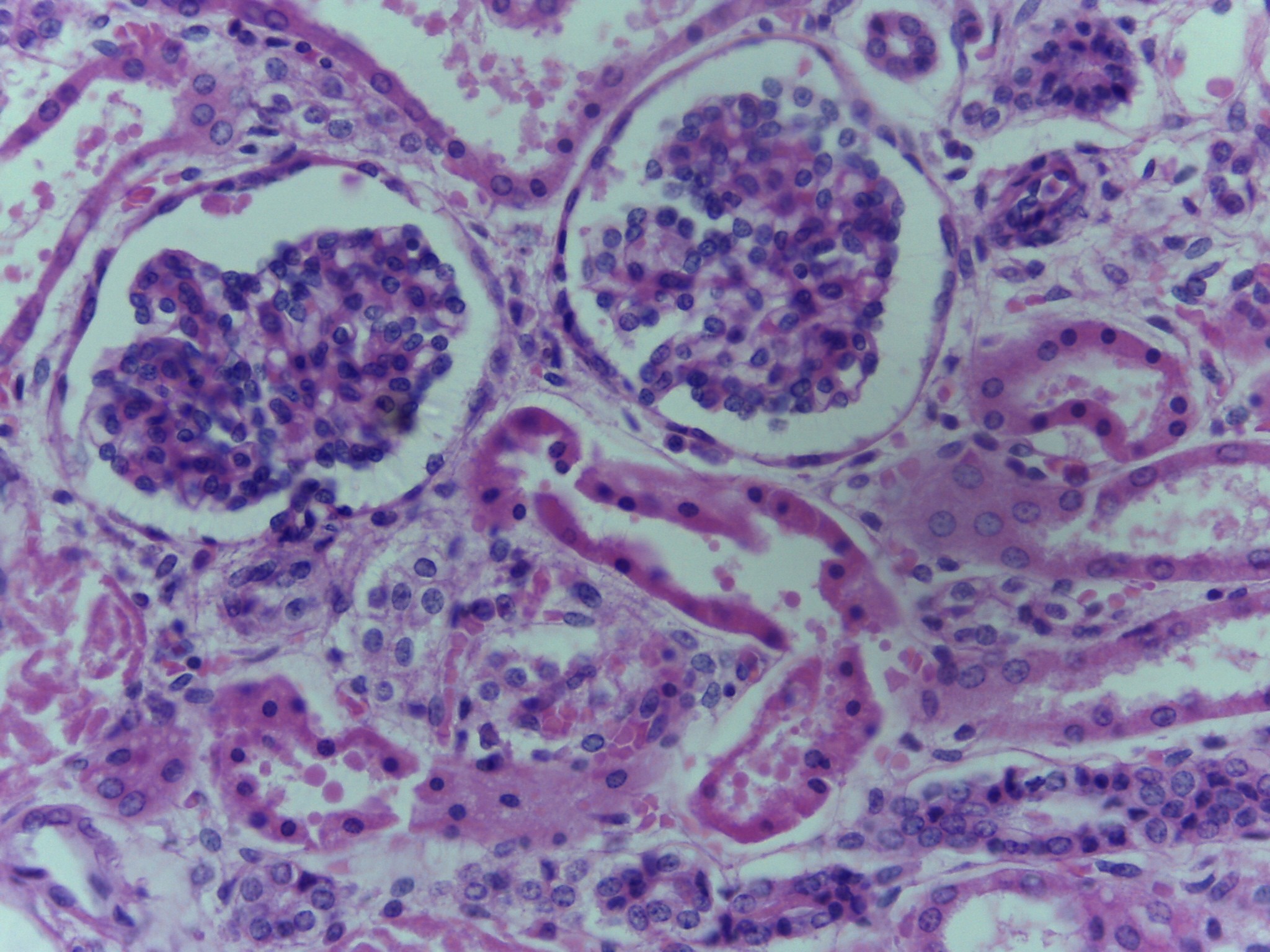
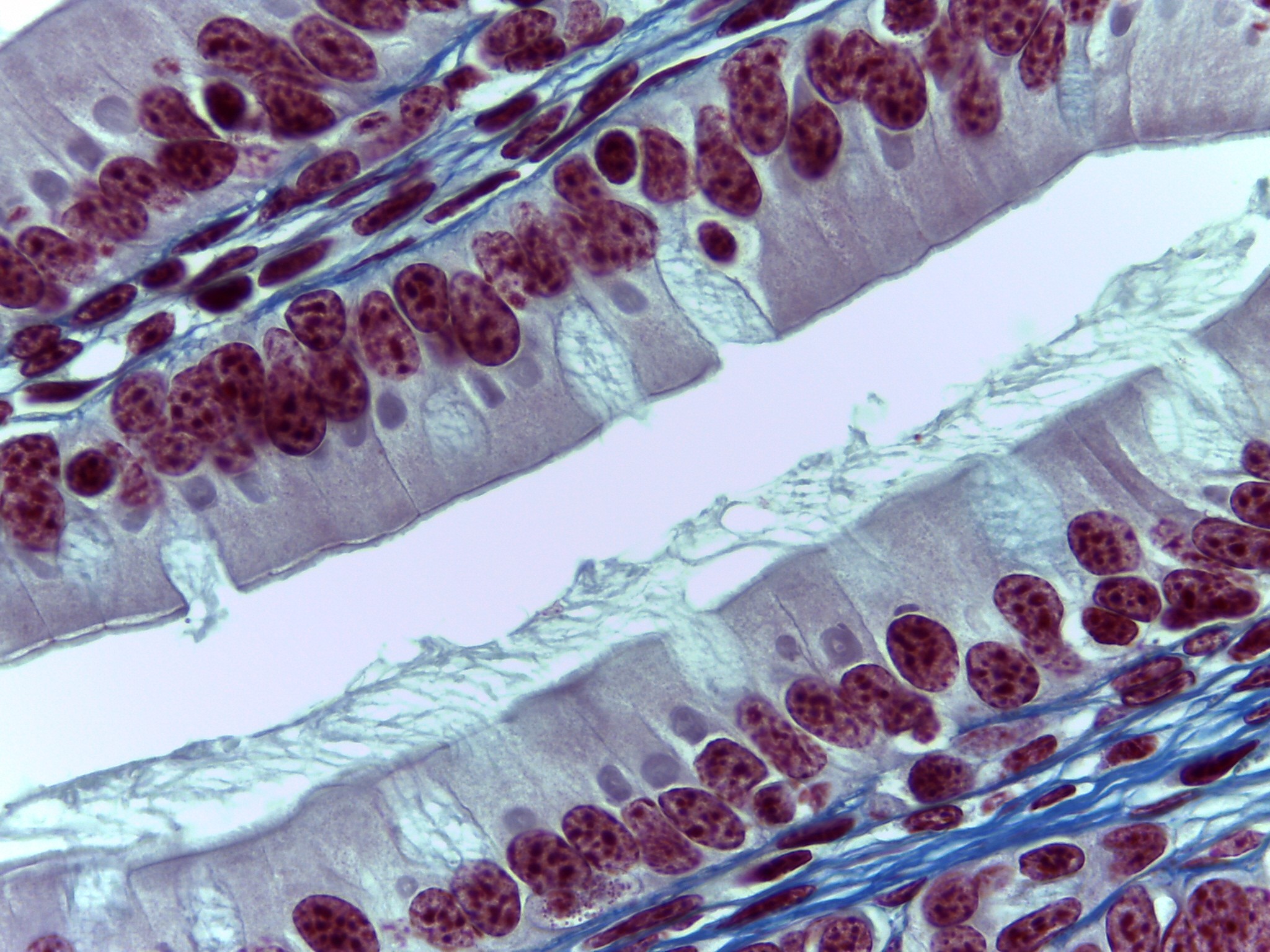
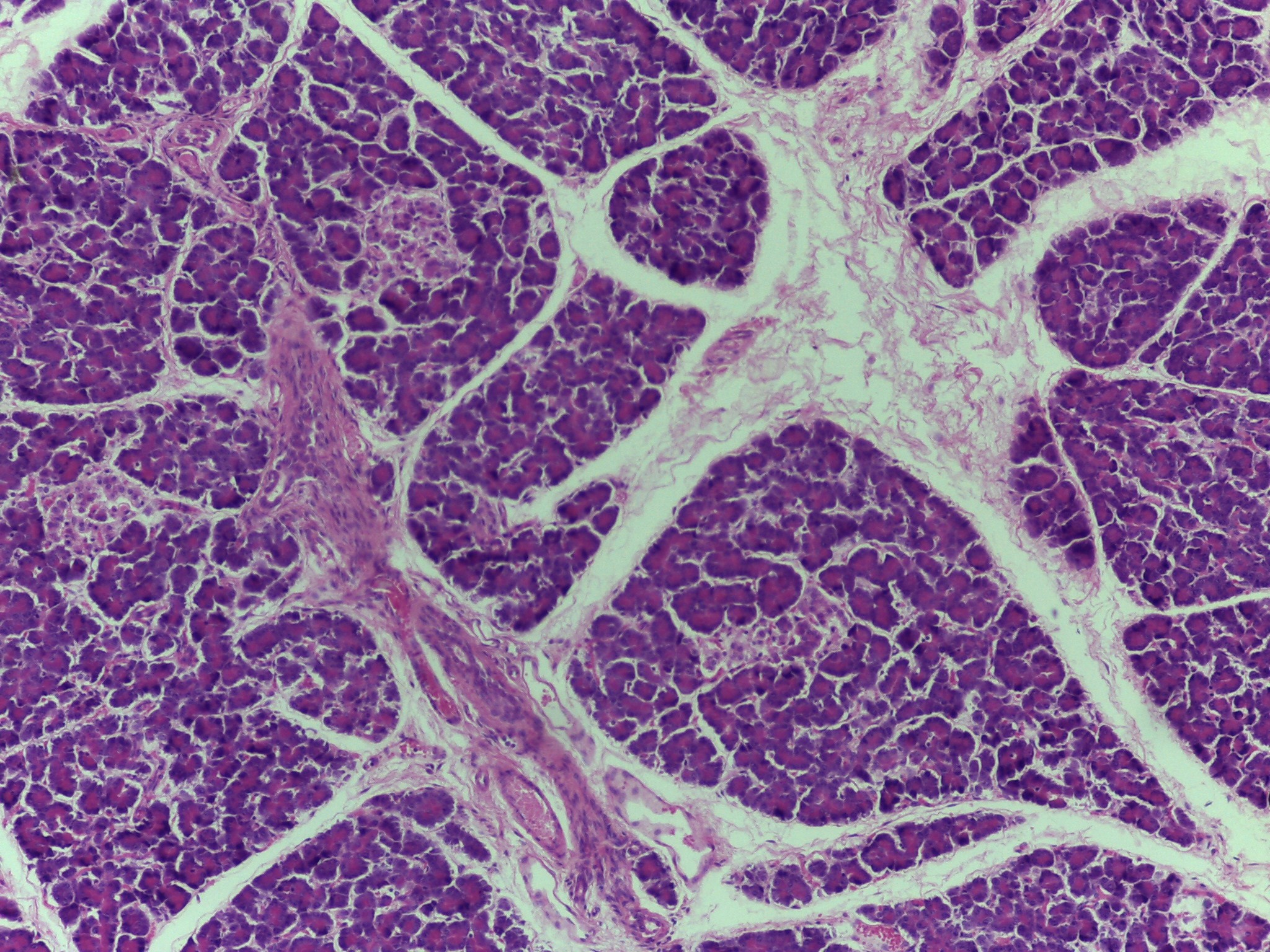
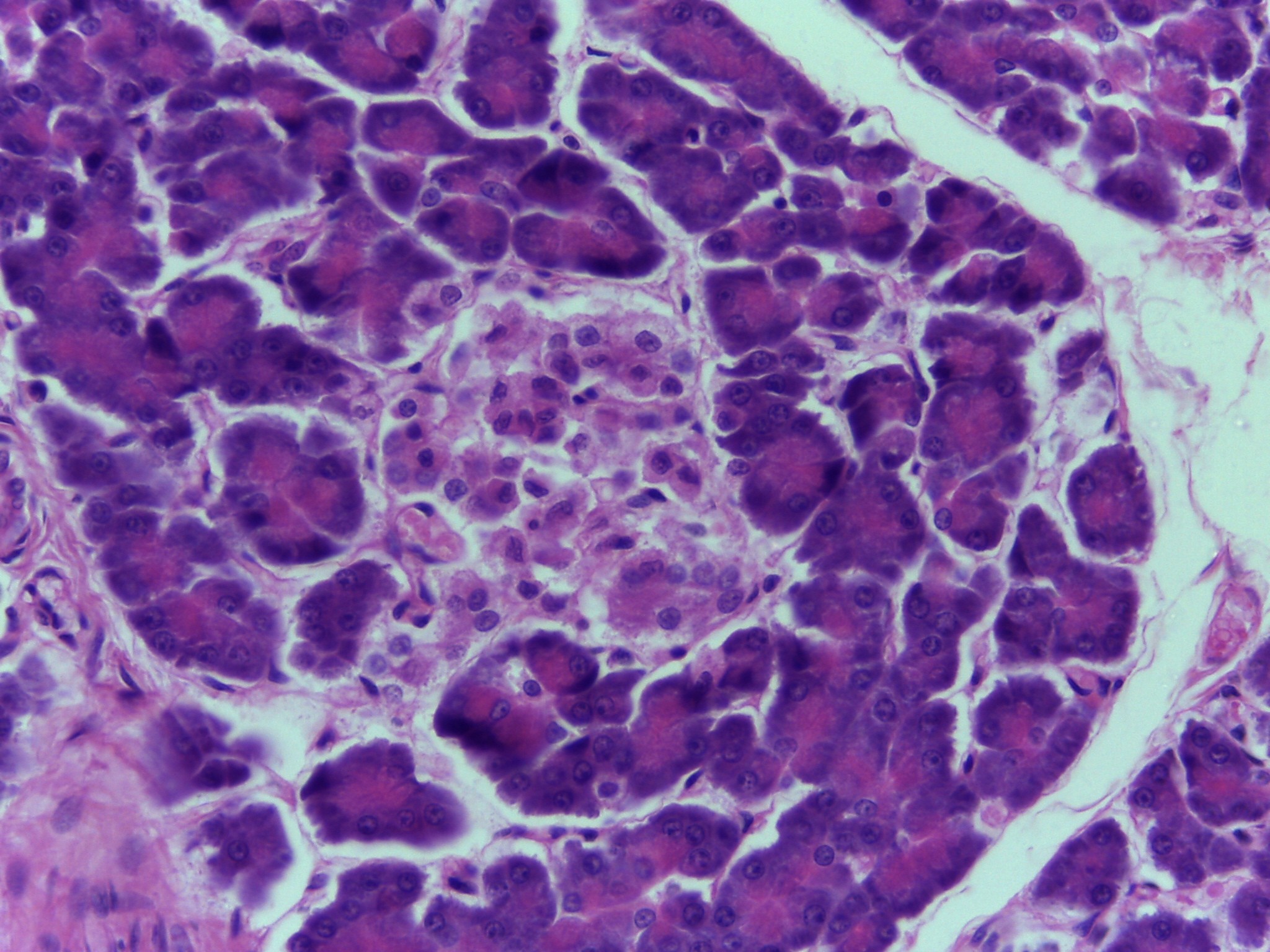
Kidney Tubules
Tissue: Simple Cuboidal ET
Function: selective reabsorption
Near perfect cross-sections at high magnification of renal tubules
Things reabsorbed must leave the tubules, tubules must be permeable to substance for reabsorption to occur.
Examples of materials reabsorbed are glucose and amino acids.
Anything not permeable can’t be reabsorbed and these substances are lost as urine.
Ex: Urea (waste).
Consist of a lumen and wall
-
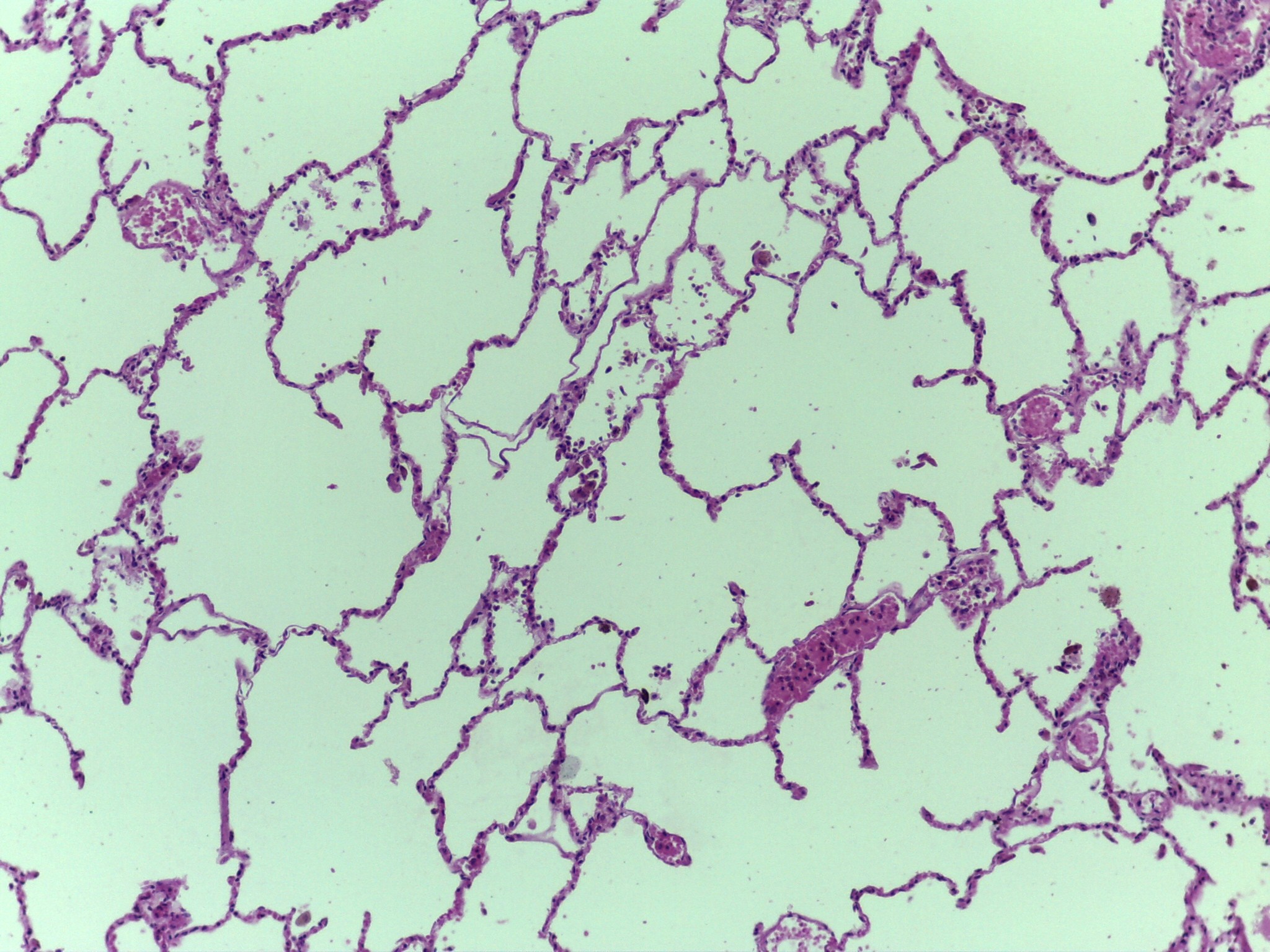
Lung (Low mag.)
Tissue: Simple Squamous ET (alveoli)
Function: gas exchange; diffusion of gasses
Functional units of lungs = alveoli
Blood passes through lungs inspired oxygen passes from alveoli into blood where it binds hemoglobin and is transported to all of the body’s tissues.
Carbon dioxide moves from blood to alveoli to be expired.
-
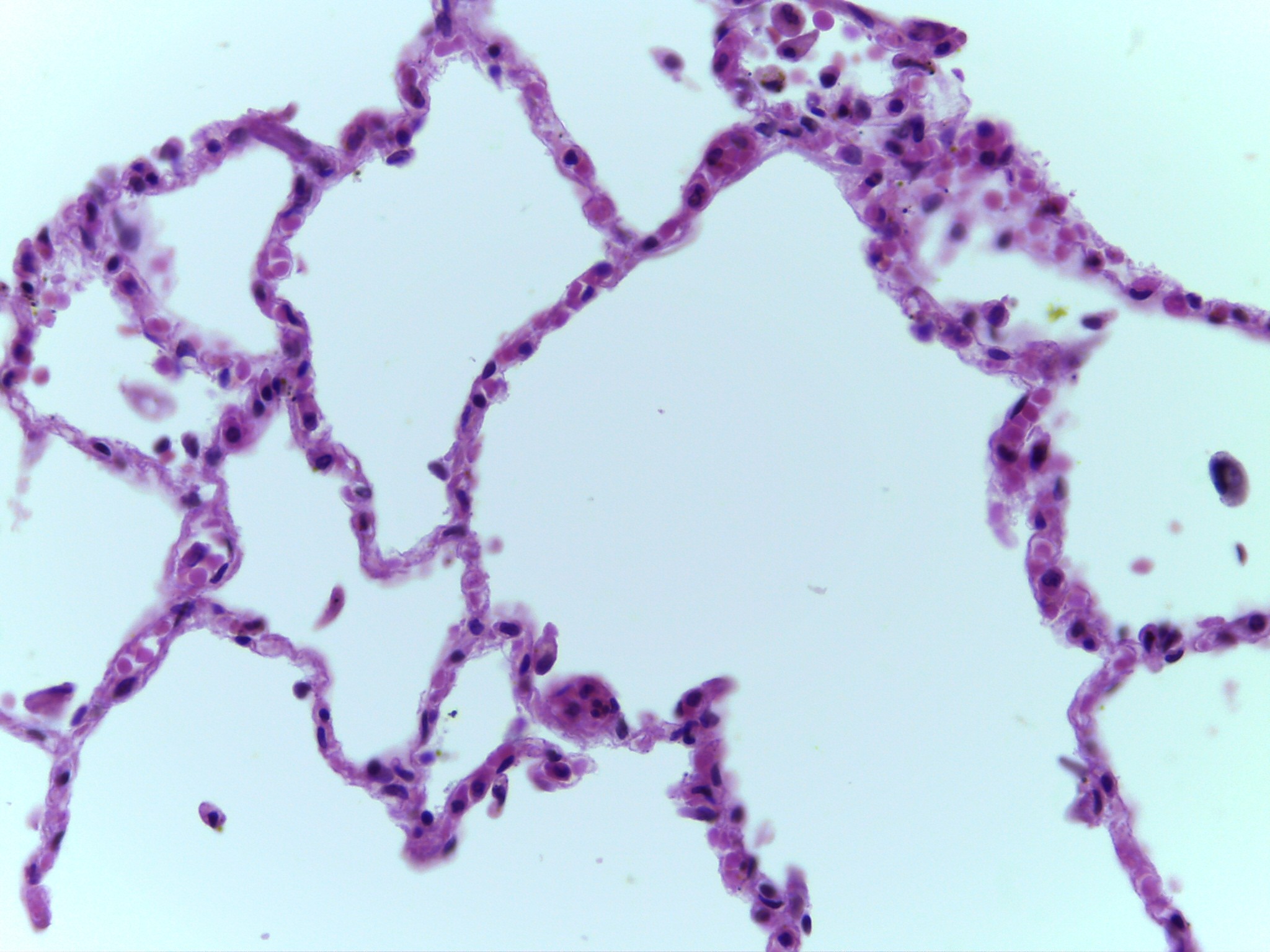
Lung (High mag.)
Tissue: Simple Squamous ET (alveoli)
Function: gas exchange; diffusion of gasses
When looking at alveolar wall you can tell that it is cellular and can initially pick out alveoli.
There are two alveolar walls; each belonging to their own alveolus: 2 cell layers thick; one layer corresponding to one alveoli.
-
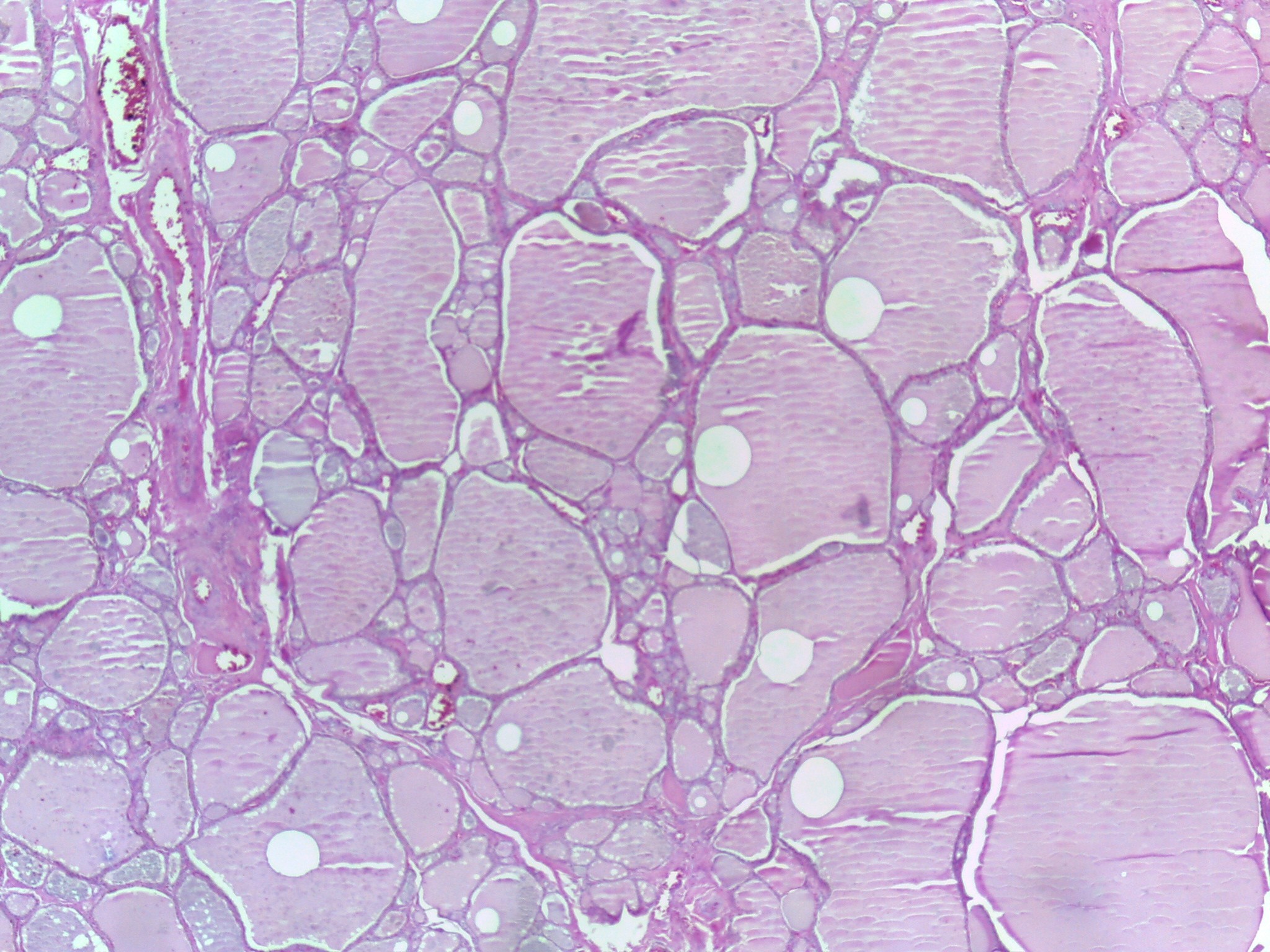
Thyroid (Low mag.)
Tissue: Simple Cuboidal ET
Function: follicular cells produce thyroxine (T3/T4)
Structures visible are thyroid follicles
Material in center of follicle is a mixture called colloid.
When cells are actively producing thyroxine they are thicker and appear cuboidal.
When cells are less active than they are not as thick and appear more squamous.
Call the tissue simple cuboidal epithelial tissue but differentiate between low and high cuboidal.
-
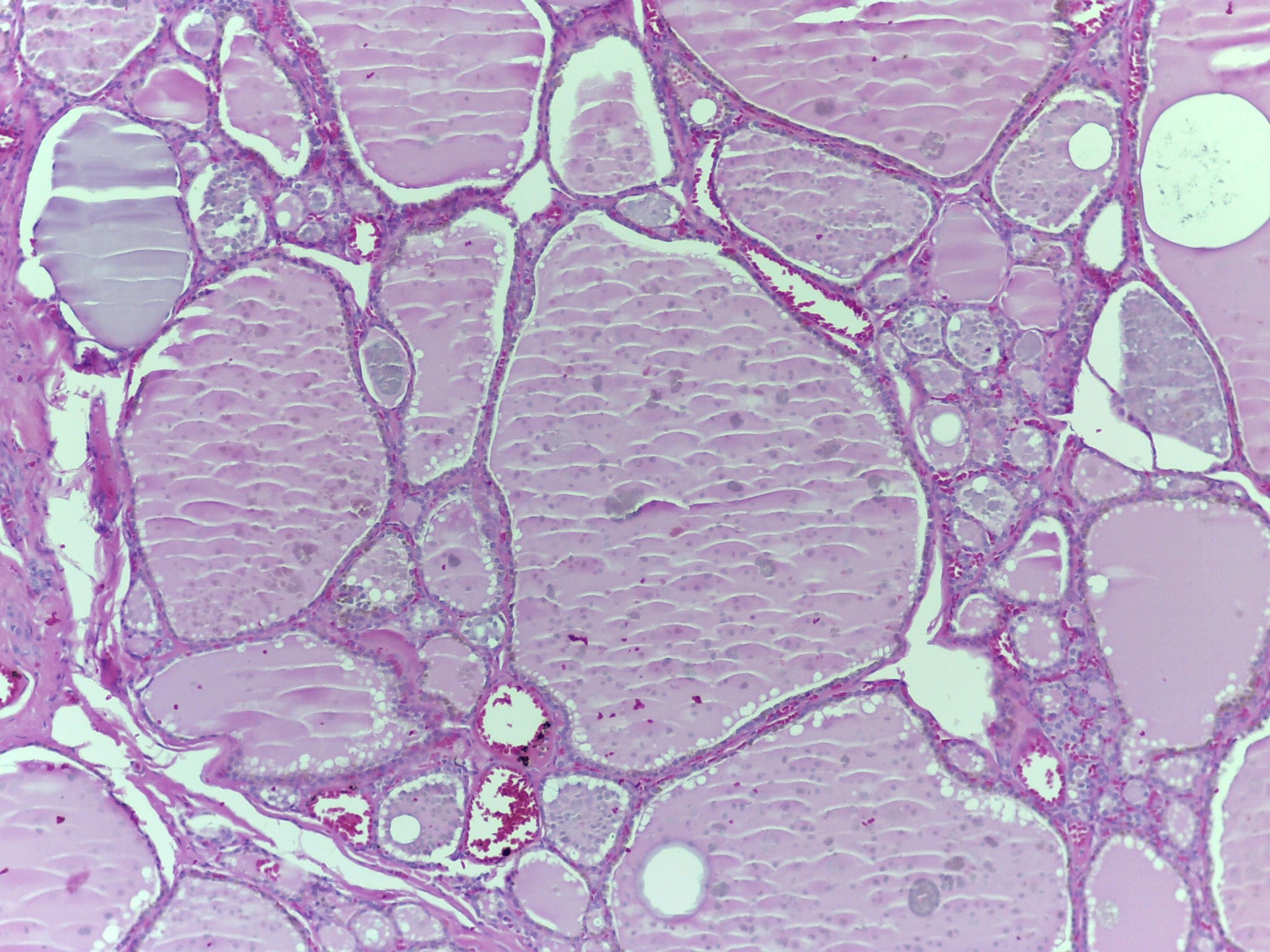
Thyroid (Med mag.)
Tissue: Simple Cuboidal ET
Function: follicular cells produce thyroxine (T3/T4)
Structures visible are thyroid follicles
Material in center of follicle is a mixture called colloid.
When cells are actively producing thyroxine they are thicker and appear cuboidal.
When cells are less active than they are not as thick and appear more squamous.
Call the tissue simple cuboidal epithelial tissue but differentiate between low and high cuboidal.
-
Thyroid (High mag.)
Tissue: Simple Cuboidal ET
Function: follicular cells produce thyroxine (T3/T4)
Structures visible are thyroid follicles
Material in center of follicle is a mixture called colloid.
When cells are actively producing thyroxine they are thicker and appear cuboidal.
When cells are less active than they are not as thick and appear more squamous.
Call the tissue simple cuboidal epithelial tissue but differentiate between low and high cuboidal.
-

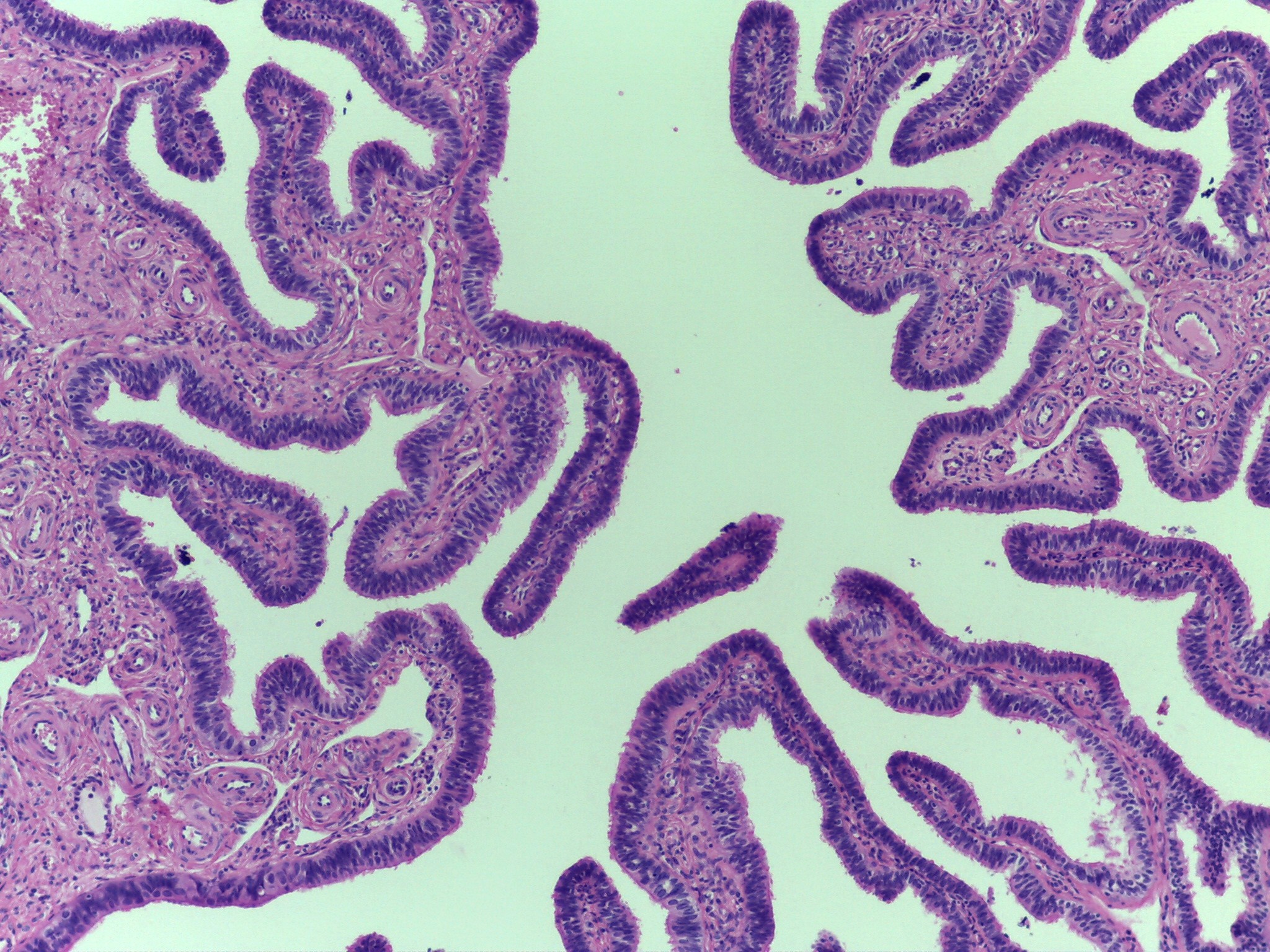
Small Intestine
Tissue: Simple columnar ET
Function: absorbs nutrients and water
Cross-sections at low magnification of the small intestine.
Identifiable because it is convoluted into villi.
Contain a villus, villi, lumen.
Villi: finger-like projections
Lining of stomach convoluted into villi to increase the surface area
-
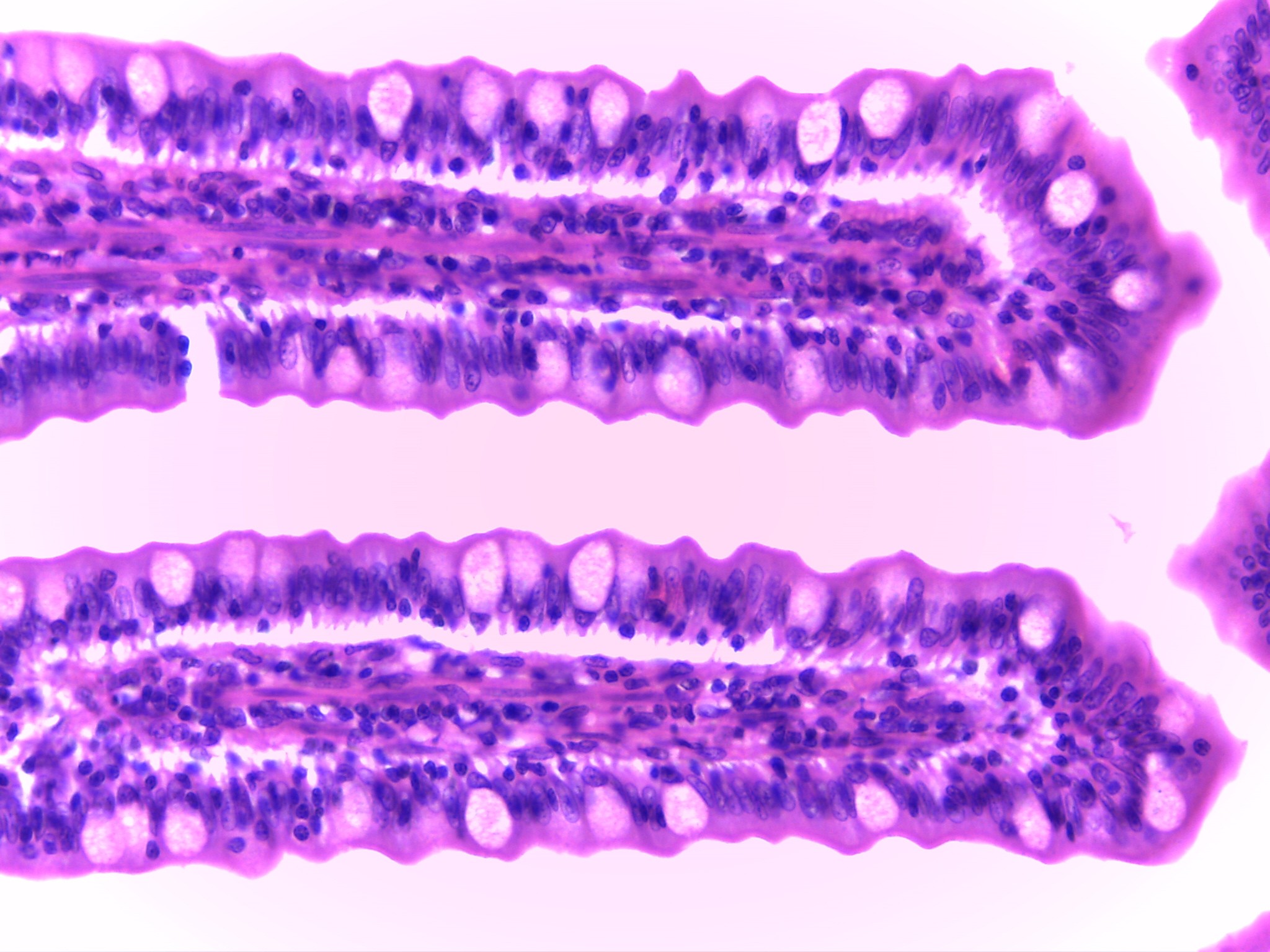
Small Intestine (intermediate mag.)
Tissue: Simple columnar ET
Function: absorbs nutrients and water
Villi more prominent.
Goblet cell visible.
Goblet cells secrete mucin that combines with water to form mucous.
-
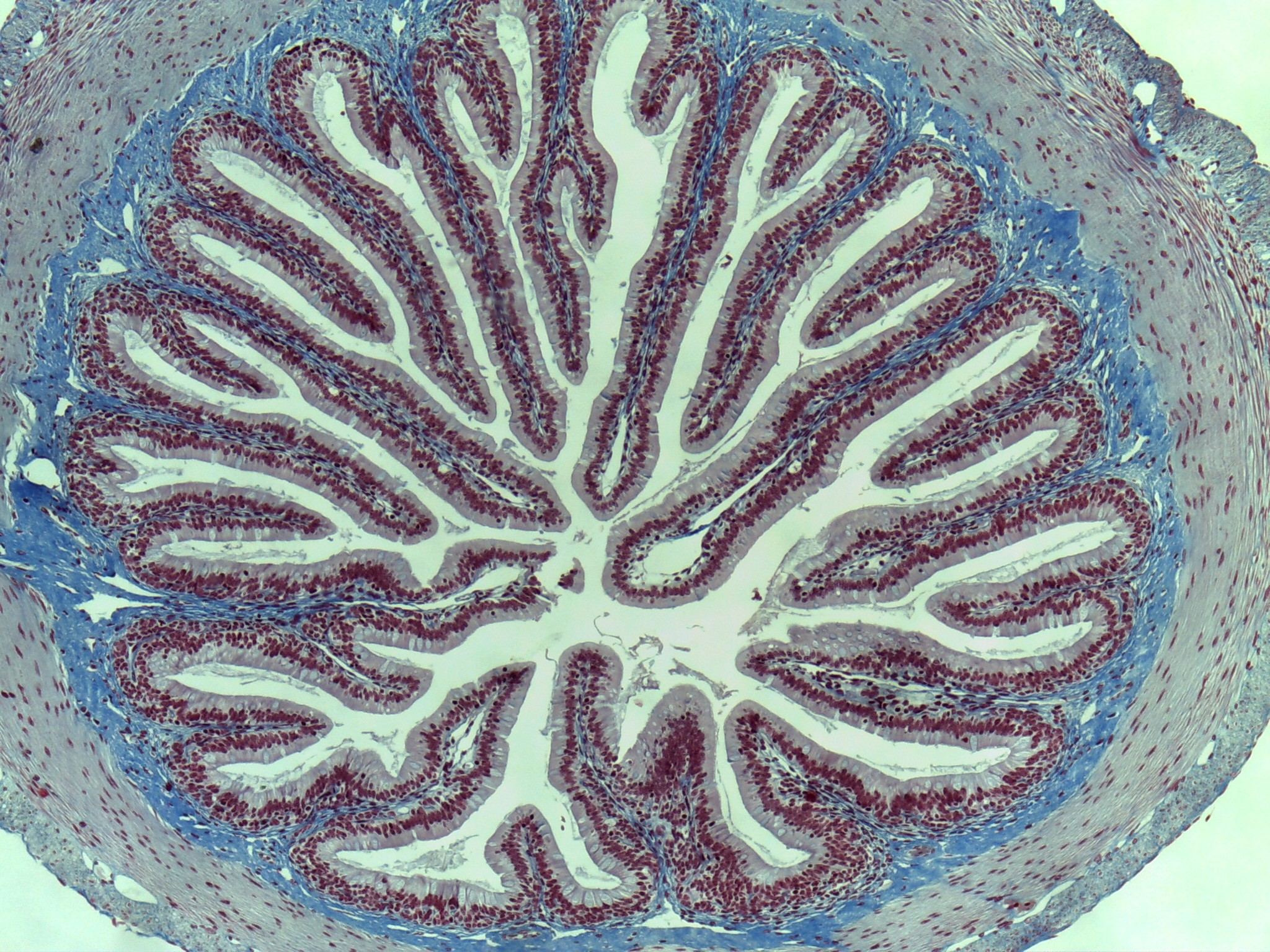
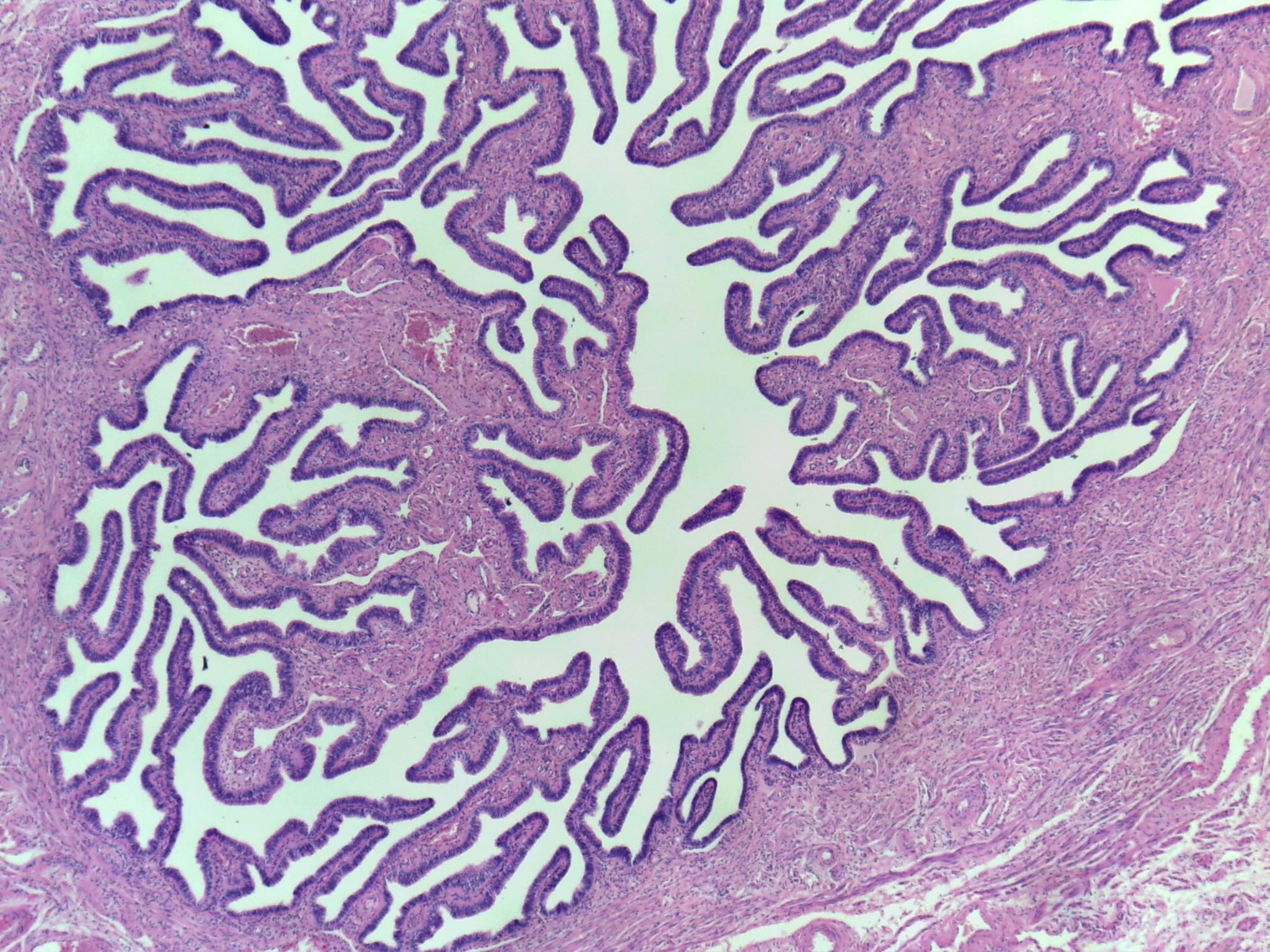
Small Intestine (Low mag.)
Tissue: Simple columnar ET
Function: absorbs nutrients and water
Cross-section at low magnification of small intestine.
Identifiable because it is convoluted into villi.
-

Small Intestine (Med mag.)
Tissue: Simple columnar ET
Function: absorbs nutrients and water
Villi more prominent
Goblet cells visible
Goblet cells secrete mucin that combines with water to form mucous.
-
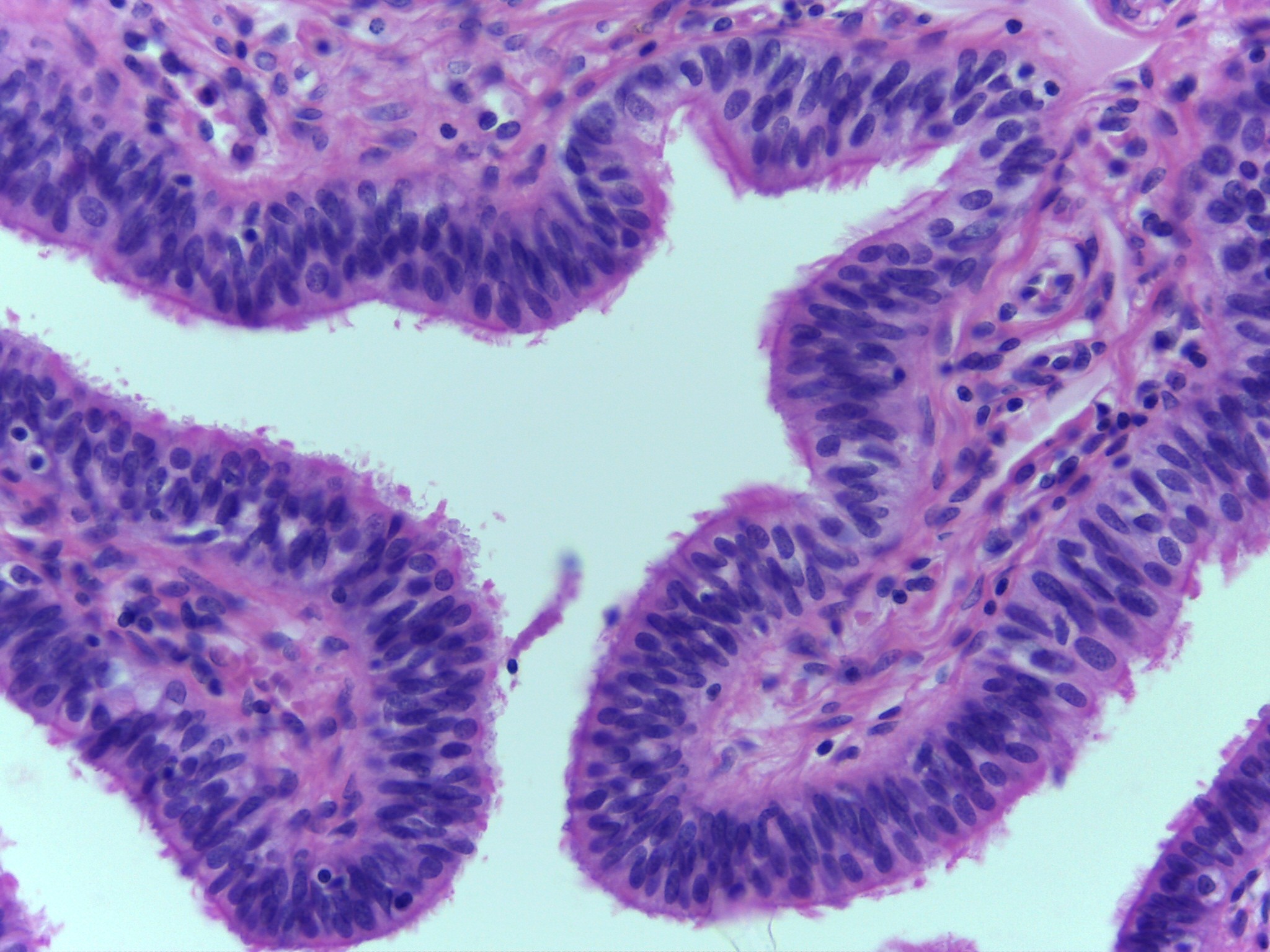
Small Intestine (High mag.)
Tissue: Simple columnar ET
Function: absorbs nutrients and water
Cells lining the villi are columnar in shape.
Layer called the mucosa.
Three types of cells in mucosa:
Columnar cells: function in absorption of nutrients (monomers)
Goblet cells: secrete mucin
Enteric cells: AKA brush border cells line digestive tract
-
Small Intestine (High mag.)
Tissue: Simple columnar ET
Function: absorbs nutrients and water
Layer of mucous also visible along the free surface of cells.
Cells lining the villi are columnar in shape
Layer called the mucosa
Three types of cells in mucosa:
Columnar cells: function in absorption of nutrients (monomers)
Enteric cells: AKA brush border cells
Lines digestive tract
Forms mucosa lining of villi in small intestine
Goblet cells: that secrete mucin
-
Small Intestine (High mag.)
Tissue: Simple columnar ET
Function: absorbs nutrients and water
Goblet cells clearly visible.
Layer of mucous also visible along the free surface of cells.
Cells lining the villi are columnar in shape.
Layer called the mucosa
Three types of cells in mucosa:
Columnar cells: function in absorption of nutrients (monomers)
Goblet cells: secrete mucin
Enteric cells: AKA brush border cells line digestive tract
-
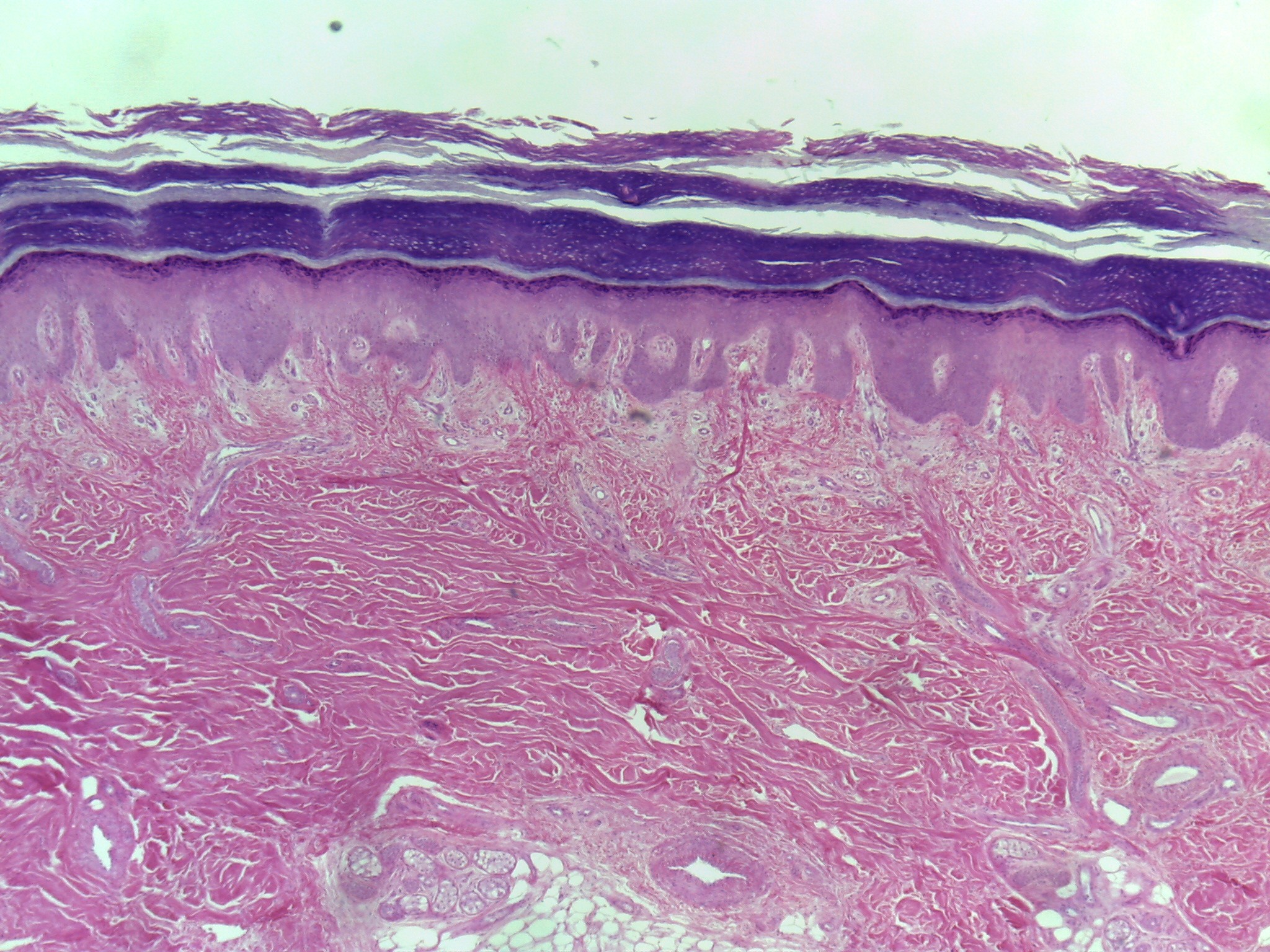
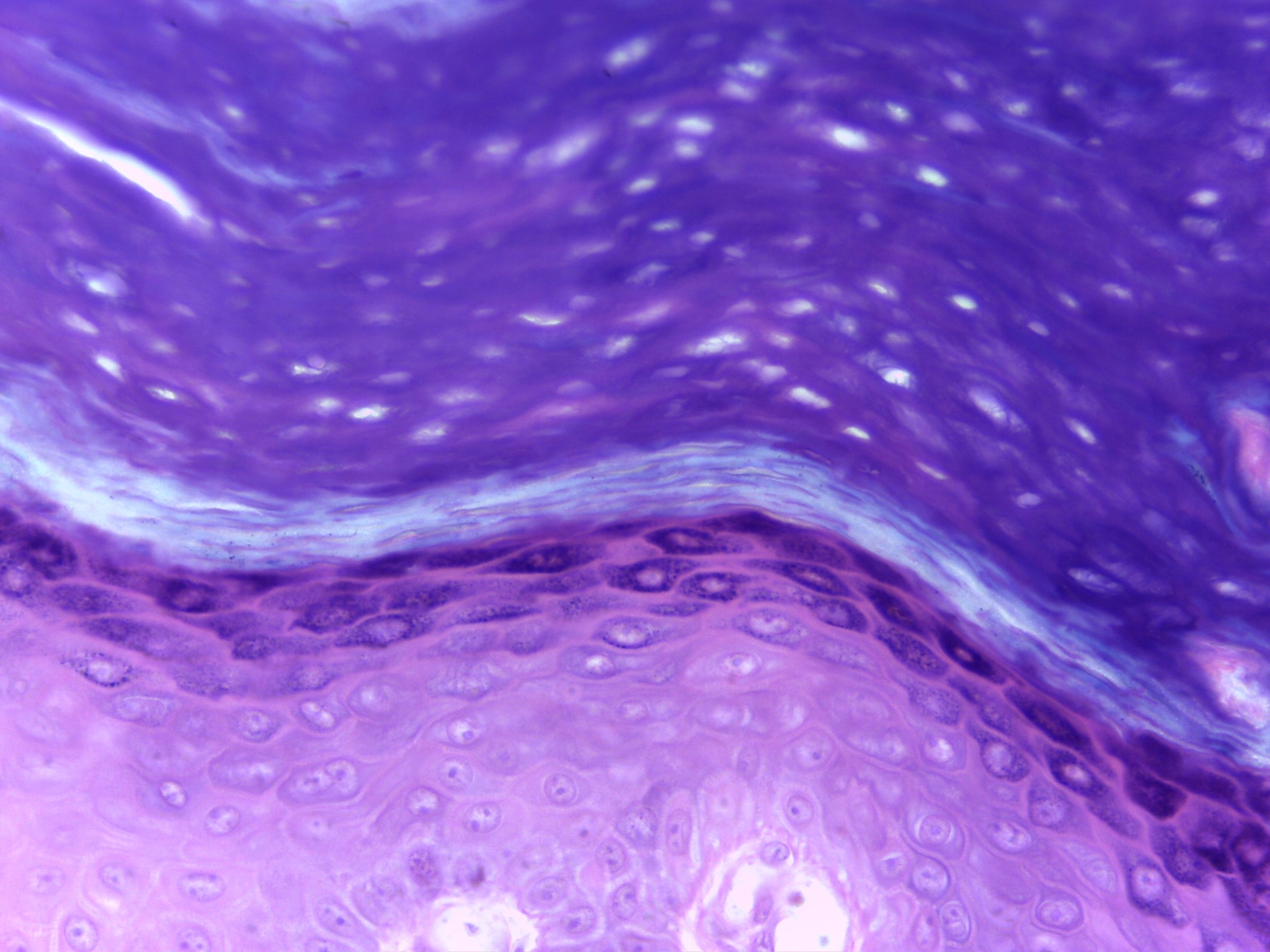
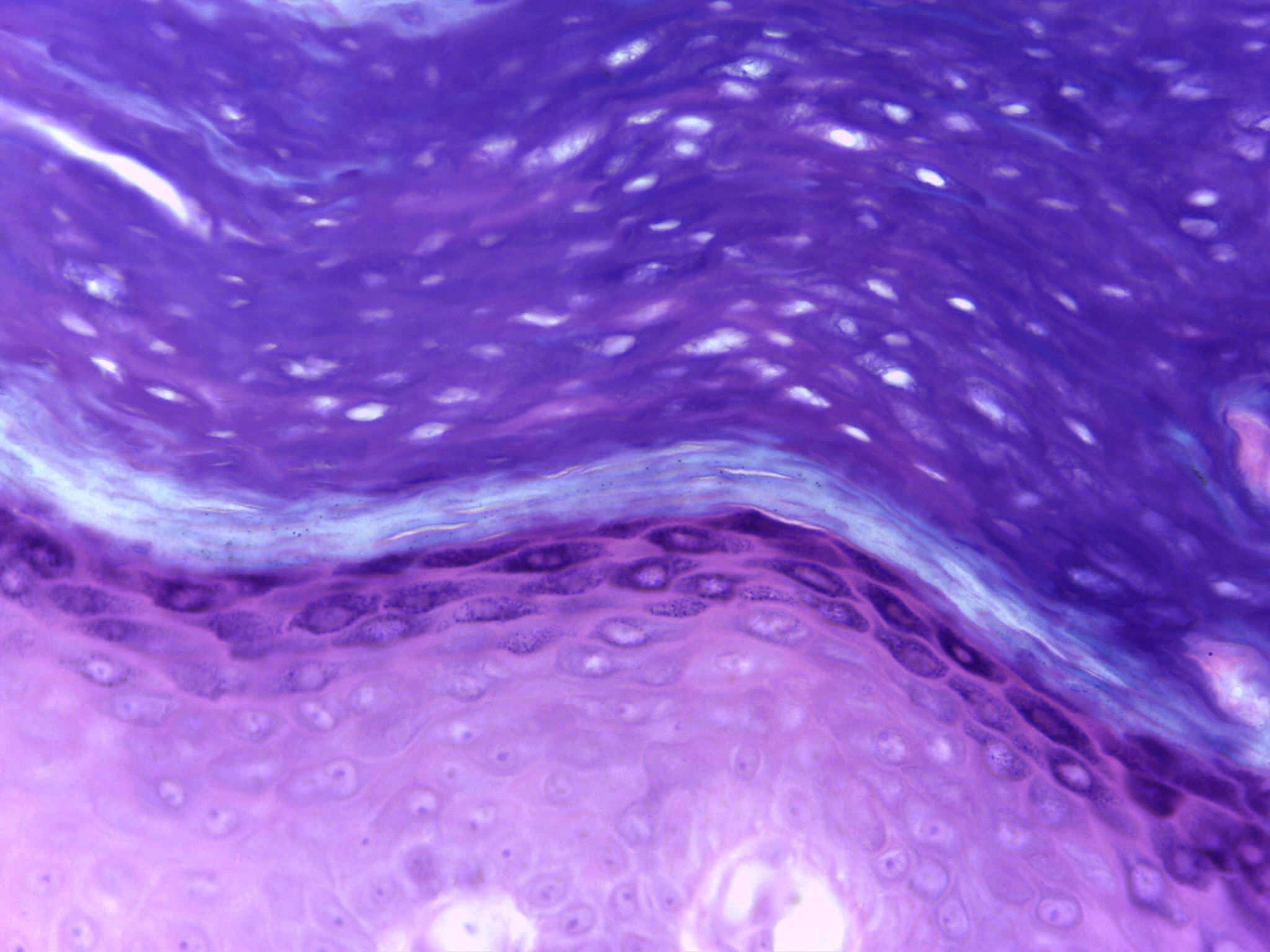
Low skin- keratinized (low mag.)
Tissue: Keratinized stratified squamous ET
Functions: strength and waterproofing
At this magnification can see overlying epidermis made of keratinized stratified squamous epithelial tissue .
Epidermis of skin
Underlying dermis made of dense irregular connective tissue.
Dermis becomes denser as you look deeper.
-
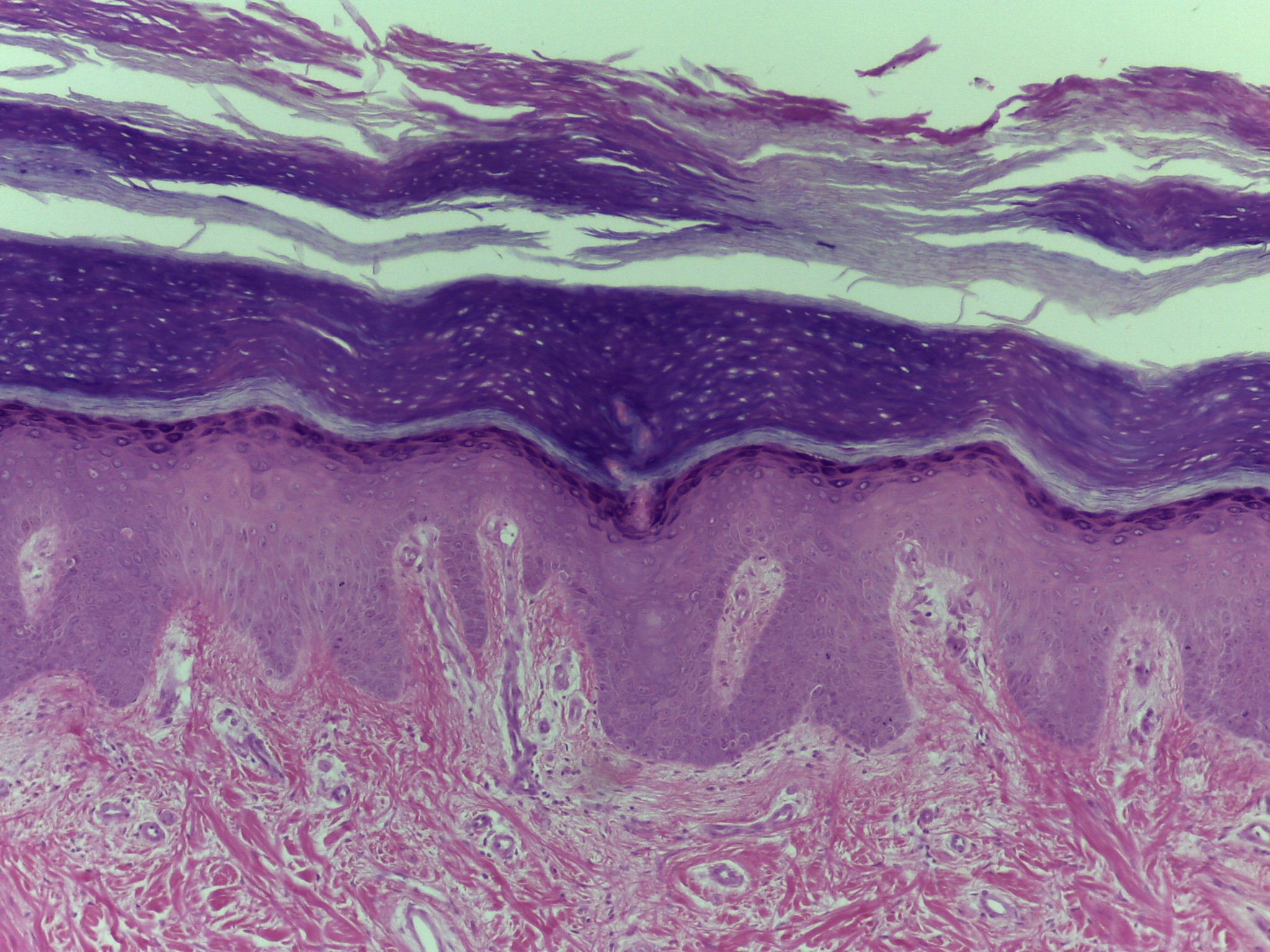
Low skin- keratinized (low mag.)
Tissue: Keratinized stratified squamous ET
Functions: strength and waterproofing
At this magnification can see overlying epidermis made of keratinized stratified squamous epithelial tissue .
Epidermis of skin
Underlying dermis made of dense irregular connective tissue.
Dermis becomes denser as you look deeper.
-
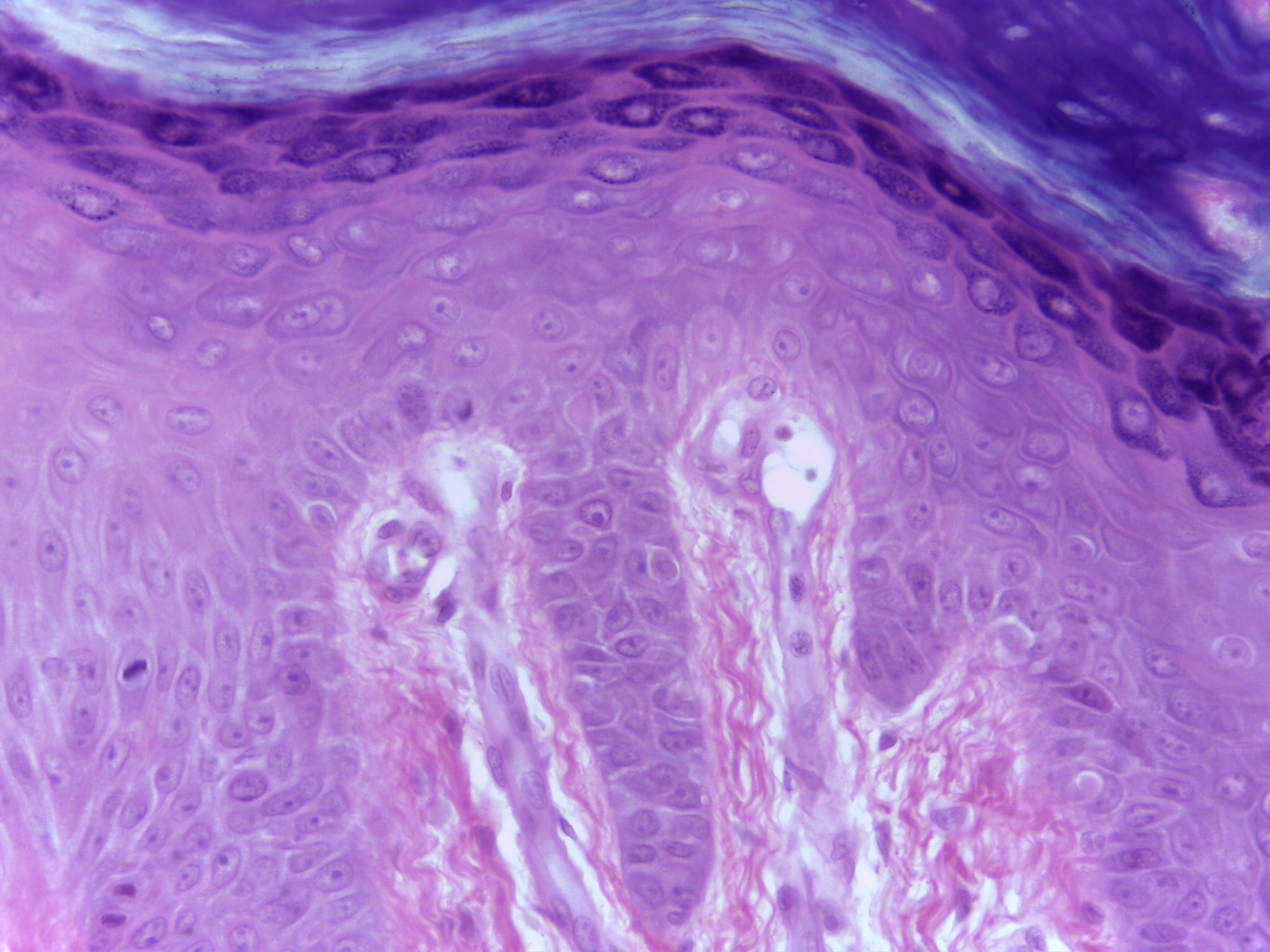
Epidermis (high mag.)
Tissue: Stratified Squamous ET
Function: acts as a barrier that protects the body.
High magnification of the deepest part of the epidermis, where it meets the dermis (interface).
5 layers of the epidermis of thick skin
-
Epidermis (high mag.)
Tissue: Stratified Squamous ET
Function: acts as a barrier that protects the body.
High magnification of the deepest part of the epidermis, where it meets the dermis (interface).
5 layers of the epidermis of thick skin
-
Epidermis (high mag.)
Tissue: Stratified Squamous ET
Function: acts as a barrier that protects the body.
High magnification of the deepest part of the epidermis, where it meets the dermis (interface).
5 layers of the epidermis of thick skin
-
Stratum Corneum
Tissue: Stratified Squamous ET
Function: acts as barrier that protects body.
High magnification of the most superficial aspect of epidermis, stratum corneum.
Cells don’t look like cells because they are extremely flat, anucleated, keratinized, and dead.
-
Esophagus (low mag.)
Tissue: Stratified Squamous ET
Function: carry food and liquid from your mouth to your stomach.
Cross-section of non-keratinized stratified squamous tissue at low magnification
Makes identification of organ easy
Non-keratinized stratified squamous epithelial tissue
-
Esophagus
Tissue: Stratified Squamous ET
Function: carry food and liquid from your mouth to your stomach.
Cross-section of non-keratinized stratified squamous tissue at low magnification
Makes identification of organ easy
Non-keratinized stratified squamous epithelial tissue
Shows nature of the tissue.
-
Esophagus (High mag.)
Tissue: Stratified Squamous ET
Function: carry food and liquid from your mouth to your stomach.
Only most superficial cells are squamous, deeper cells are thicker.
Non-keratinized squamous epithelial tissue found in esophagus
Because tissue is non-keratinized cells are not dead.
Can see nuclei in even most superficial cells
-
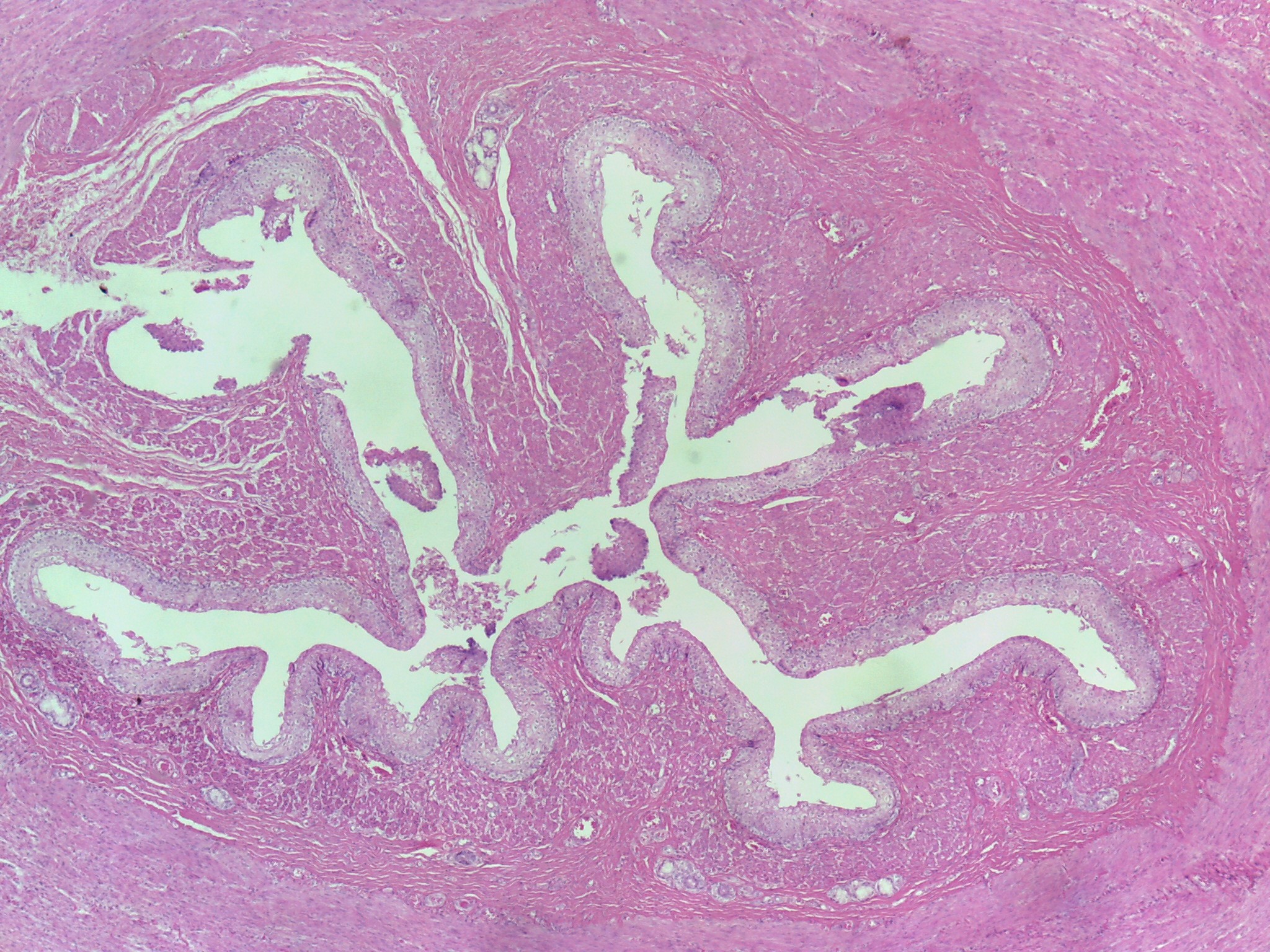
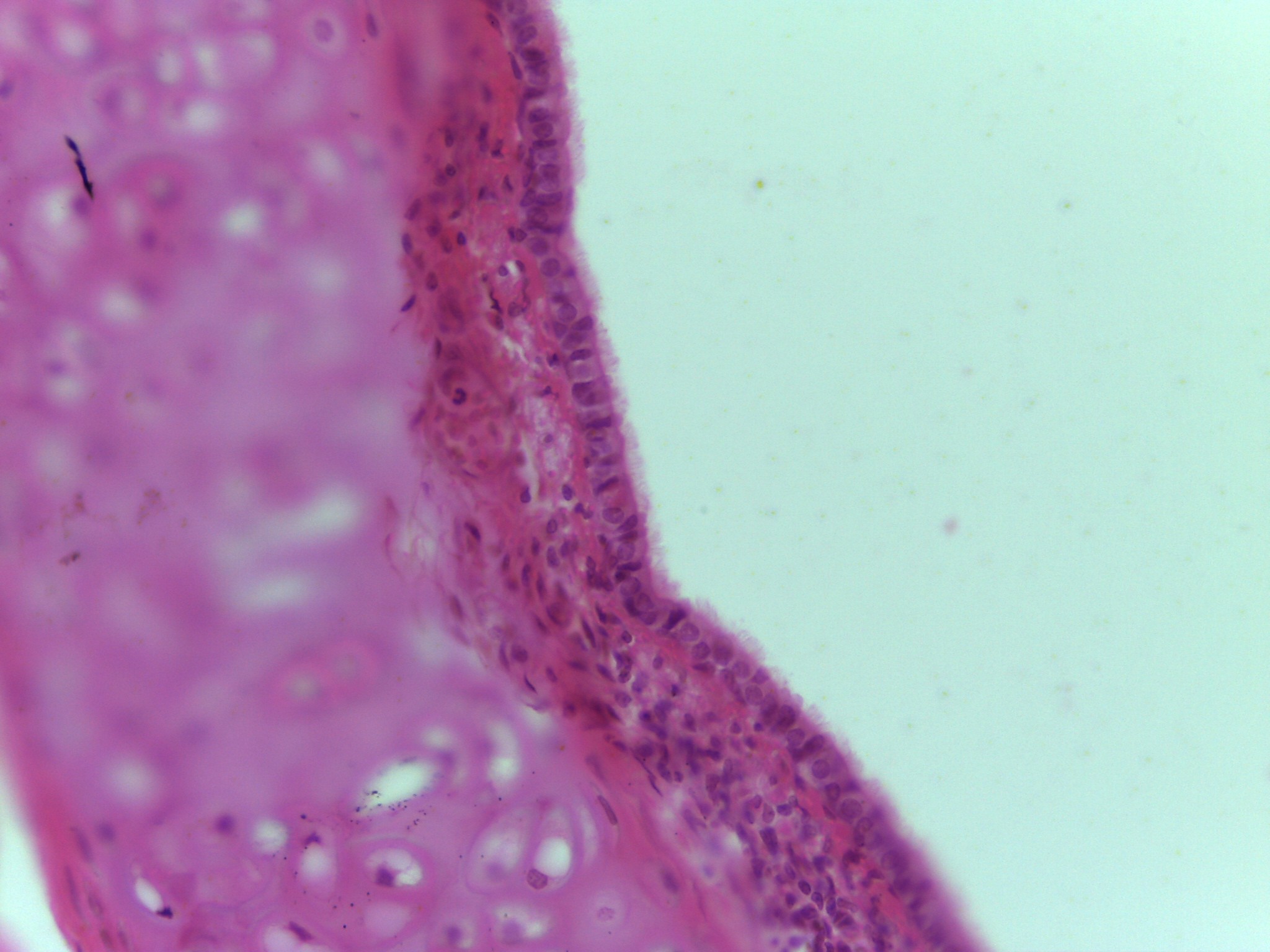
Fallopian tube (low mag.)
Tissue: simple ciliated columnar ET
Function: transport the ova from the ovary to the uterus each month.
Are convoluted but convolutions are irregular when compared to the small intestine.
Small intestine is convoluted into villi and villi are very regular.
Cilia are on the free surface of tissue, creating currents that propel the oocyte and embryo toward the uterus.
Forms mucosa.
Contains goblet cells that secrete mucin.
Mucous protective and lubricating.
-
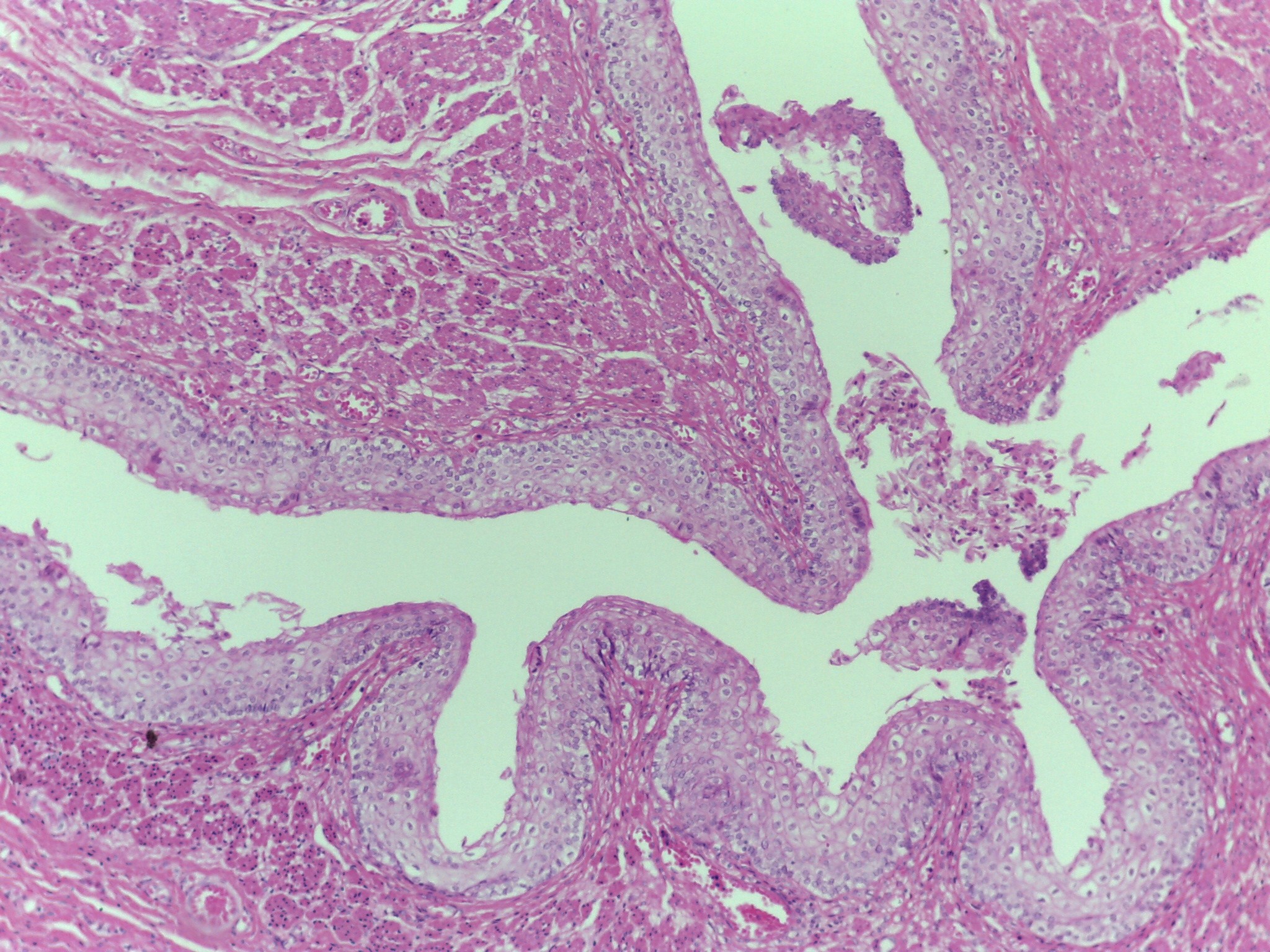
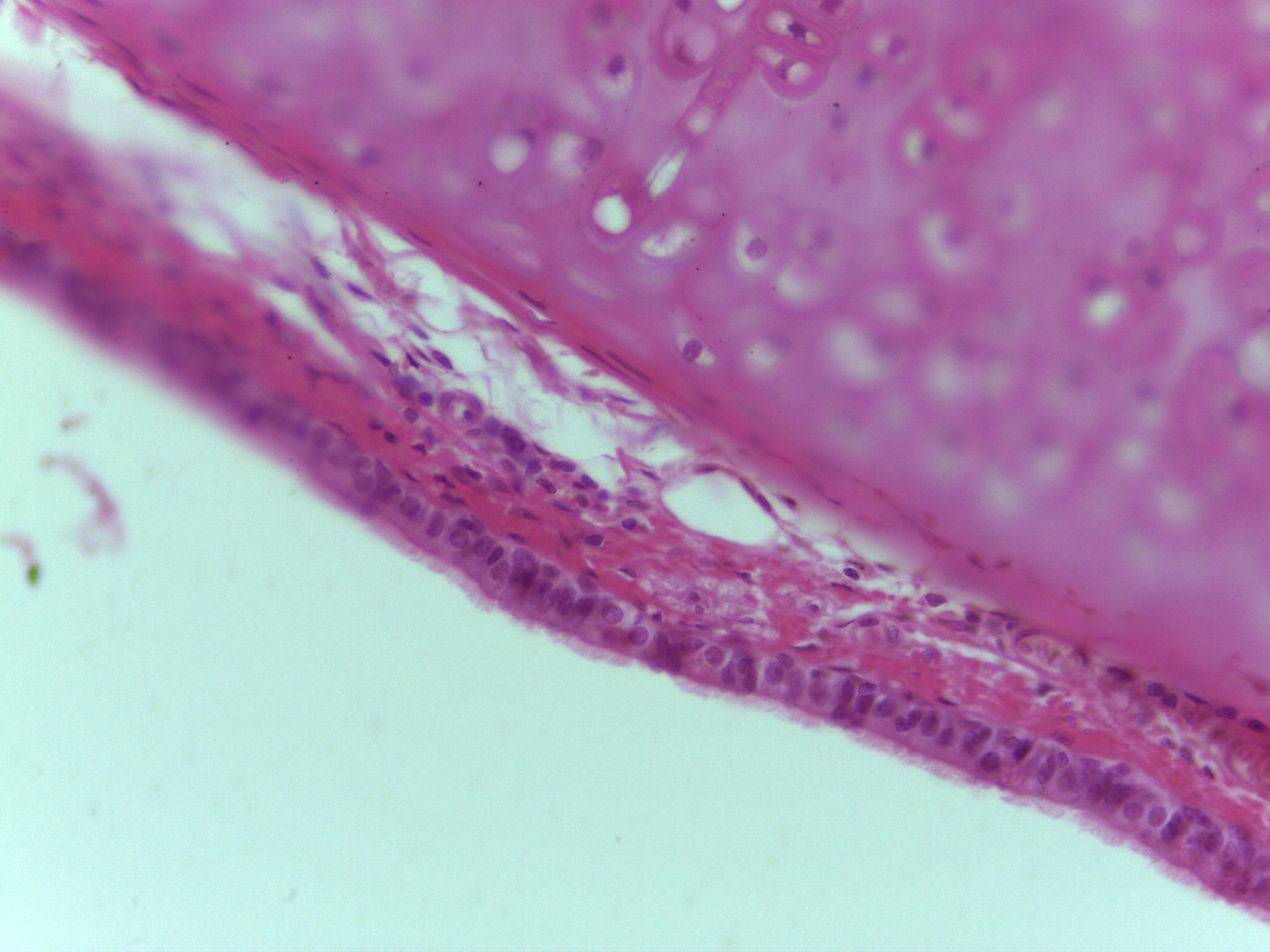
Fallopian tube (med mag.)
Tissue: simple ciliated columnar ET
Function: transport the ova from the ovary to the uterus each month.
Are convoluted but convolutions are irregular when compared to the small intestine.
Small intestine is convoluted into villi and villi are very regular.
Cilia are on the free surface of tissue, creating currents that propel the oocyte and embryo toward the uterus.
Forms mucosa.
Contains goblet cells that secrete mucin.
Mucous protective and lubricating.
-
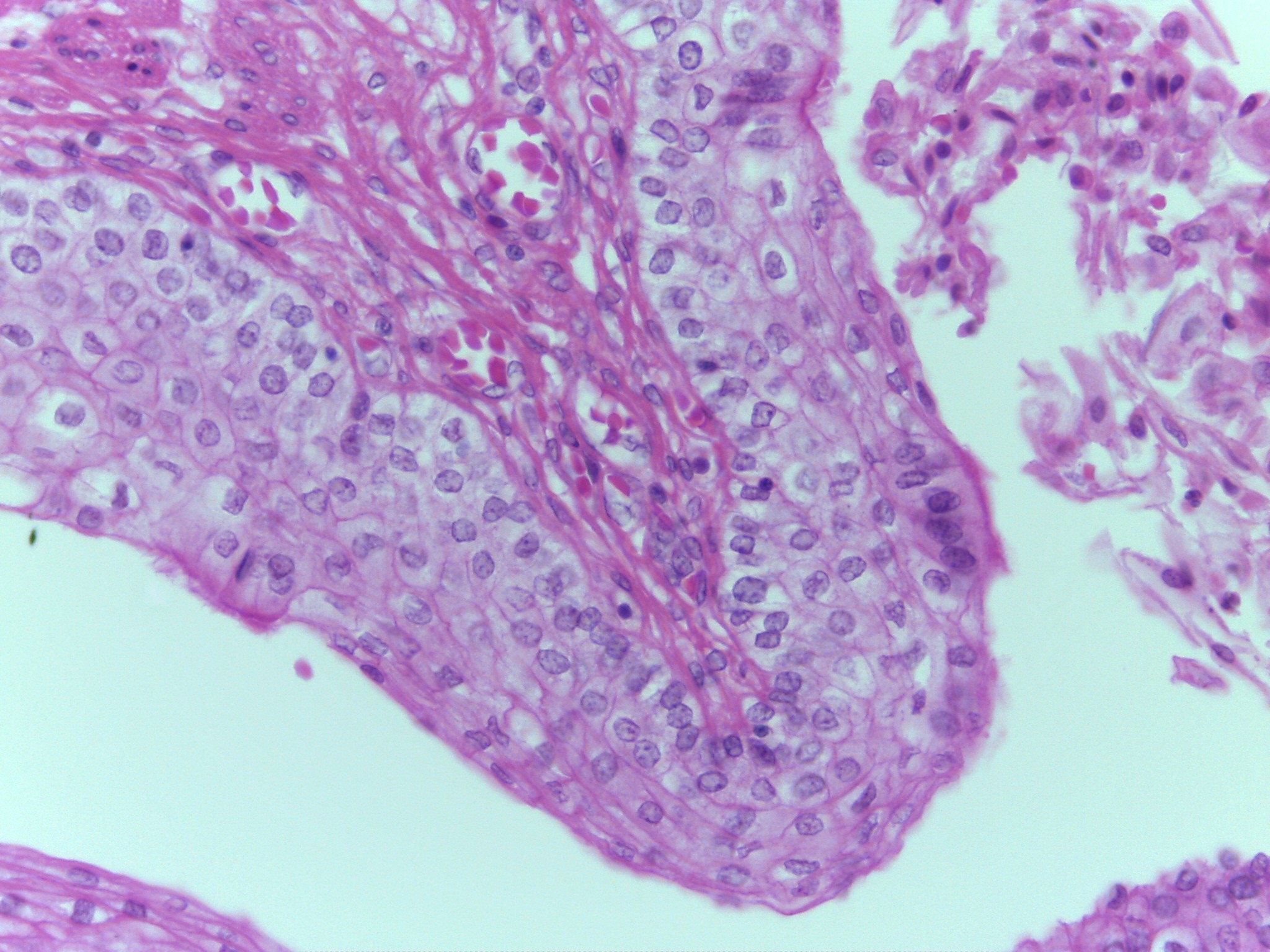
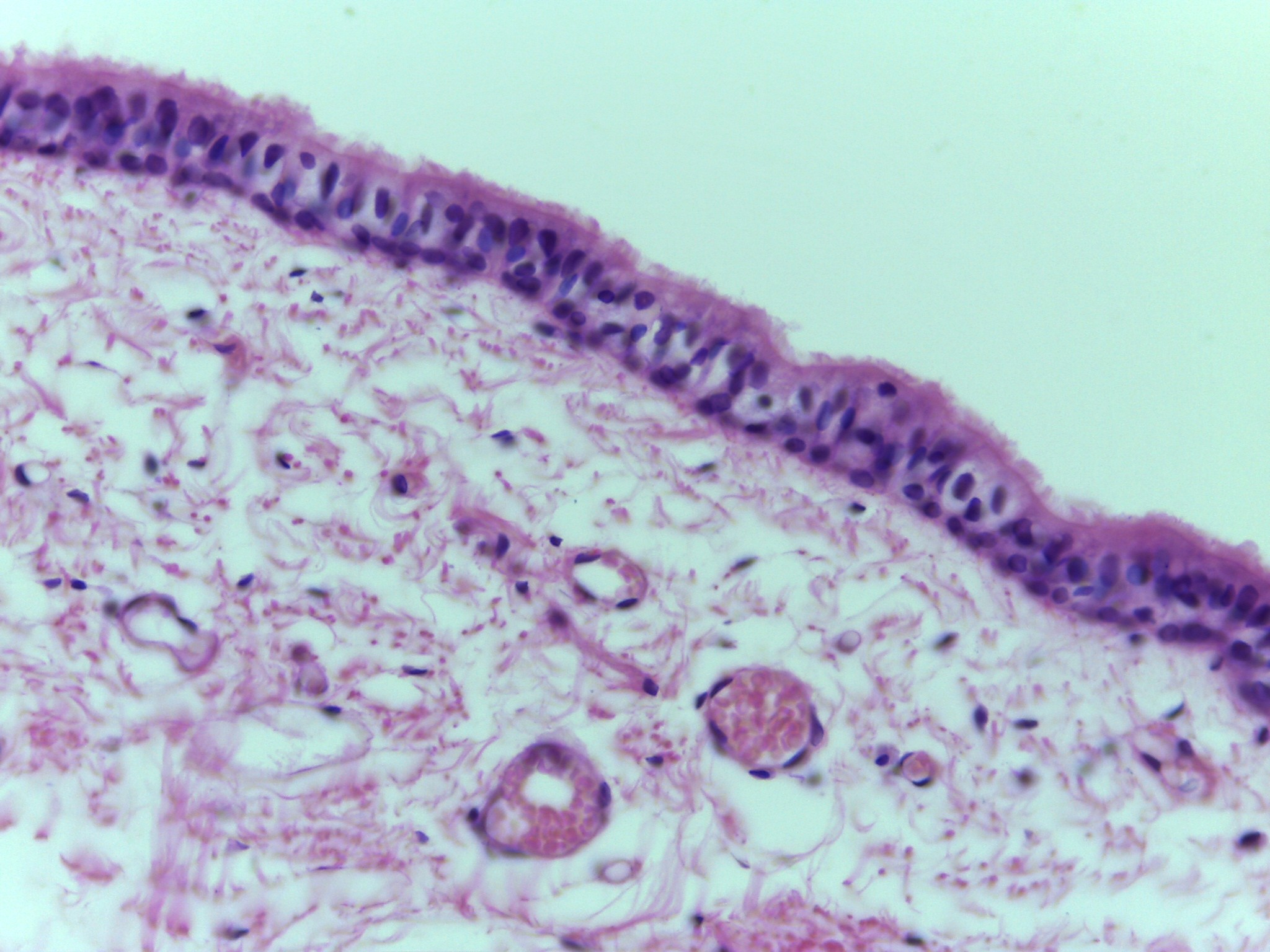
Fallopian tube (high mag.)
Tissue: simple ciliated columnar ET
Function: transport the ova from the ovary to the uterus each month.
Are convoluted but convolutions are irregular when compared to the small intestine.
Small intestine is convoluted into villi and villi are very regular.
Cilia are on the free surface of tissue, creating currents that propel the oocyte and embryo toward the uterus.
Forms mucosa.
Contains goblet cells that secrete mucin.
Mucous protective and lubricating.
-
Neck of mouse– Trachea and Esophagus
Purpose is to study trachea.
Trachea lined with pseudostratified ciliated columnar epithelial tissue (PSCCE).
Also contains hyaline cartilage: form C-shaped rings that prevent trachea from collapsing.
Presence of these two different types of tissue in trachea reminds us that organs are composed of two or more types of tissue.
Lines trachea and bronchi
Function: to remove foreign material and bacteria; form lower respiratory tract
-
Trachea
Trachea lined with pseudostratified ciliated columnar epithelial tissue (PSCCE).
Also contains hyaline cartilage
This is an intermediate magnification of the trachea showing the PSCCE and the hyaline cartilage.
-
Trachea
Trachea lined with pseudostratified ciliated columnar epithelial tissue (PSCCE).
Also contains hyaline cartilage
High magnification image of trachea
Cilia are visible
PSCCE appear stratified because different types of cells found here are different heights and have nuclei at different heights
PSCCE is not stratified because every cell does contact basement membrane.
Nuclei at different heights create the illusion there are multiple layers of cells.
-
Trachea
Trachea lined with pseudostratified ciliated columnar epithelial tissue (PSCCE).
Also contains hyaline cartilage
Three types of cells found here:
Ciliated columnar cells
Goblet cells
Basal cells
-
Trachea
Trachea lined with pseudostratified ciliated columnar epithelial tissue (PSCCE).
Also contains hyaline cartilage
Particulate matter is trapped in mucous layer
Cilia move causing mucous layer to move.
Constant movement of the mucous layer across the free surface brings up debris from the respiratory tract.
Basal cells mitotically active (stem cells) replacing the other cells
-
Trachea
Trachea lined with pseudostratified ciliated columnar epithelial tissue (PSCCE).
Also contains hyaline cartilage
Lines trachea and bronchi
Function: to remove foreign material and bacteria; form lower respiratory tract
-
Ureter (low mag. through abdominopelvic region)
Tissue: Transitional ET
Both ureters visible
Can see abdominal aorta and inferior vena cava
Aorta: round cross-section
Vena cava: collapsed tube above and to right of aorta
Transitional epithelial tissue
Lines ureters and bladder
Function: distension
-
Ureter (Higher magnification of one ureter, nature of transitional epithelial tissue begins here)
Tissue: Transitional ET
Both ureters visible
Can see abdominal aorta and inferior vena cava
Aorta: round cross-section
Vena cava: collapsed tube above and to right of aorta
Transitional epithelial tissue
Lines ureters and bladder
Function: distension
-
Ureter (high mag.)
Tissue: Transitional ET
Tissue is stratified, cells are somewhat oval/egg-shaped.
Unique tissue because tissue undergoes transition (hence name) when the urinary bladder or ureters change from being empty to full.
When organs full with urine they are able to distend and cells become wider and thinner
-
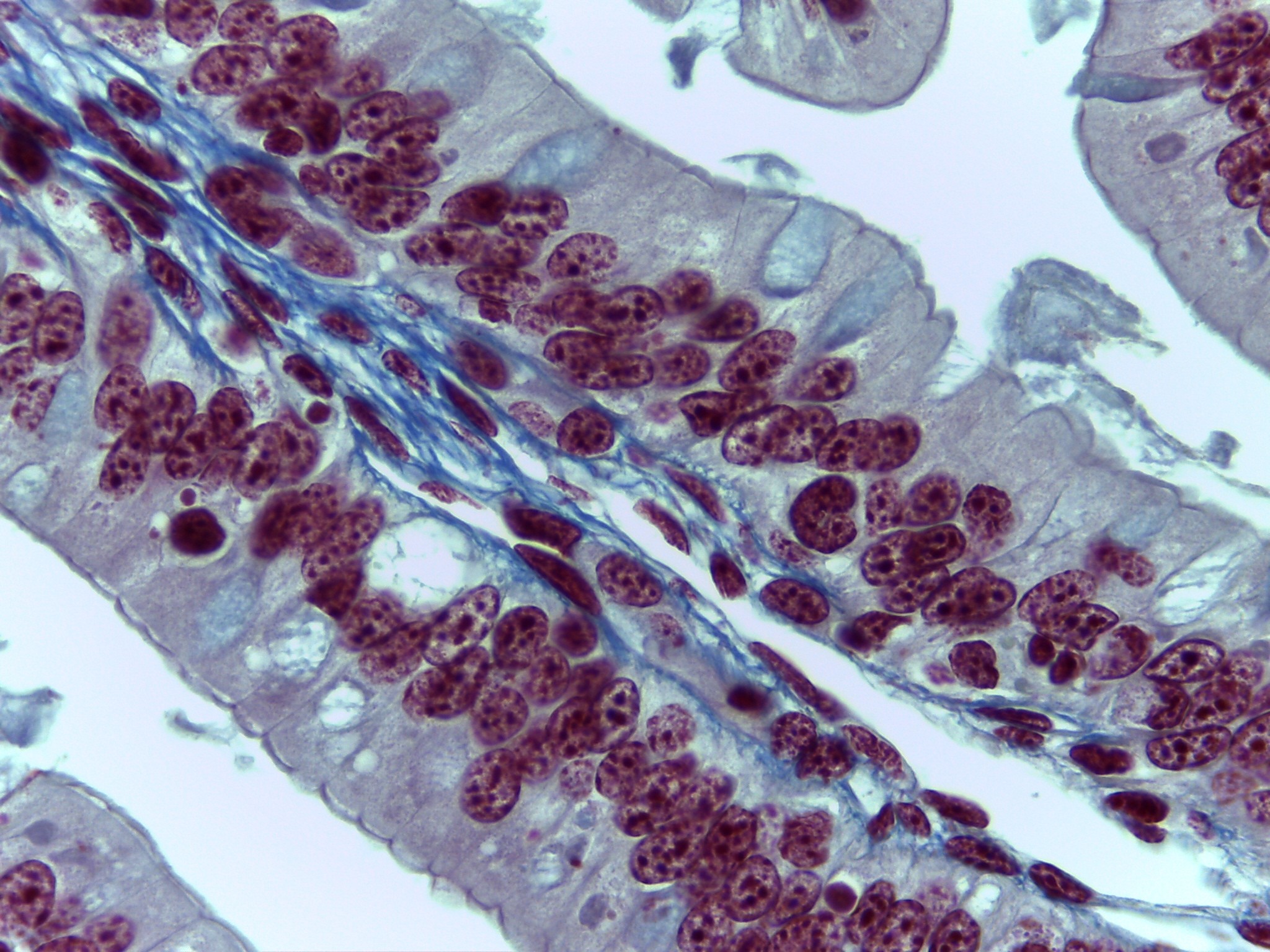
Pancreas (differential stain)
Tissue : Glandular ET
easy to pick out Islets of Langerhans versus acinar cells
Function in two different systems:
Endocrine
Islets of Langerhans: endocrine system cells
Alpha cells: secrete glucagon in response to low blood sugar.
Glucagon stimulate hydrolysis of glycogen (glycogenolysis). Also stimulates hydrolysis of fat (lipolysis) when glycogen stores are low.
Ex: fasting or prolonged exercise
Digestive: an exocrine system
Pancreatic acinar cells produce pancreatic enzymes.
Enzymes travel through pancreatic duct to duodenum of small intestine
-
Pancreas (differential stain)
Tissue : Glandular ET
easy to pick out Islets of Langerhans versus acinar cells
Function in two different systems:
Endocrine
Islets of Langerhans: endocrine system cells
Alpha cells: secrete glucagon in response to low blood sugar.
Glucagon stimulate hydrolysis of glycogen (glycogenolysis). Also stimulates hydrolysis of fat (lipolysis) when glycogen stores are low.
Ex: fasting or prolonged exercise
Digestive: an exocrine system
Pancreatic acinar cells produce pancreatic enzymes.
Enzymes travel through pancreatic duct to duodenum of small intestine
-
Pancreas (non differential stain)
Tissue : Glandular ET
Function in two different systems:
Endocrine
Islets of Langerhans: endocrine system cells
Alpha cells: secrete glucagon in response to low blood sugar.
Beta cells secrete insulin in response to high blood sugar. Insulin stimulates the uptake of glucose. Glucose may be oxidized for ATP or may be used to synthesize glycogen (glycogenesis)
-
Pancreas (non differential stain)
Tissue : Glandular ET
Function in two different systems:
Endocrine
Islets of Langerhans: endocrine system cells
Alpha cells: secrete glucagon in response to low blood sugar.
Beta cells secrete insulin in response to high blood sugar. Insulin stimulates the uptake of glucose. Glucose may be oxidized for ATP or may be used to synthesize glycogen (glycogenesis)
-
Pancreas (non differential stain)
Tissue : Glandular ET
Function in two different systems:
Endocrine
Islets of Langerhans: endocrine system cells
Alpha cells: secrete glucagon in response to low blood sugar.
Beta cells secrete insulin in response to high blood sugar. Insulin stimulates the uptake of glucose. Glucose may be oxidized for ATP or may be used to synthesize glycogen (glycogenesis)
-
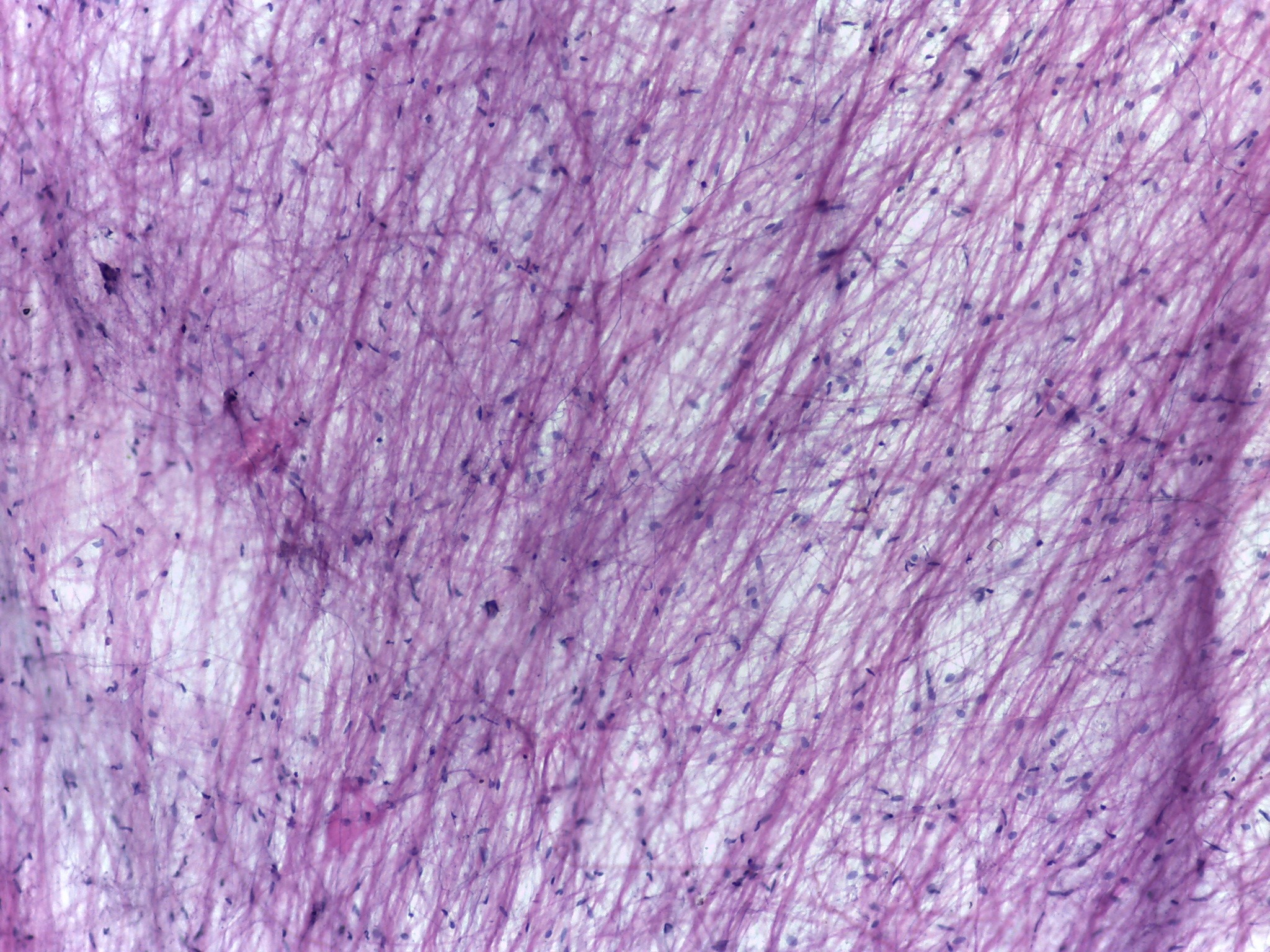
Loose connective tissue (Med mag.)
Thicker (wider) fibers: collagen fibers
Thinner (narrower) fibers: elastic fibers
Dark spots are nuclei of fibroblast cells: cells that produce collagen and elastic fibers
Surrounds blood vessels and nerves. Fluid matrix which facilitates diffusion.
Forms->
Superficial fascia - binds skin to muscles
Deep fascia - binds groups of muscles together
-
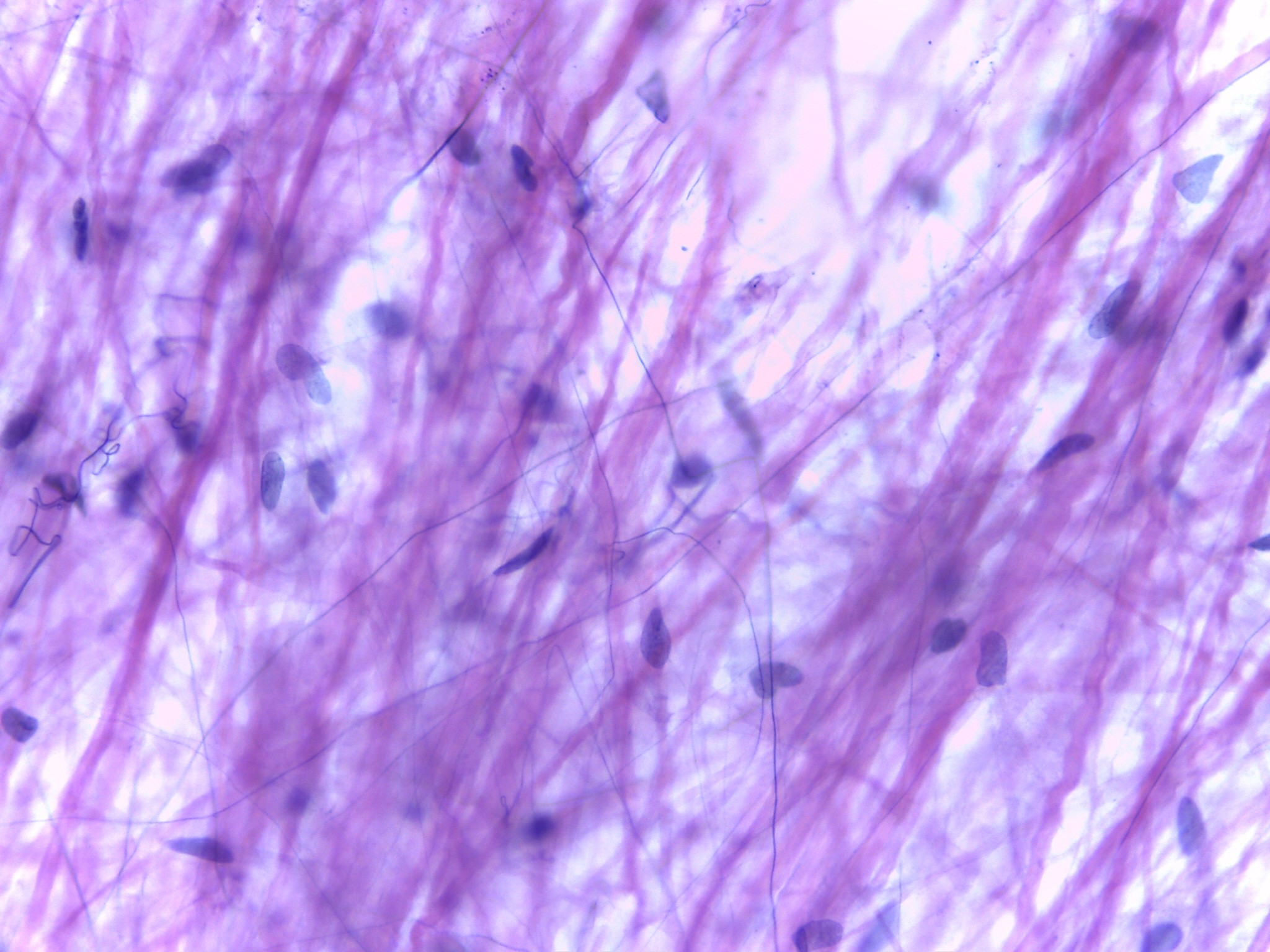
Loose connective tissue (High mag.)
Thicker (wider) fibers: collagen fibers
Thinner (narrower) fibers: elastic fibers
Dark spots are nuclei of fibroblast cells: cells that produce collagen and elastic fibers
Surrounds blood vessels and nerves. Fluid matrix which facilitates diffusion.
Forms->
Superficial fascia - binds skin to muscles
Deep fascia - binds groups of muscles together
-
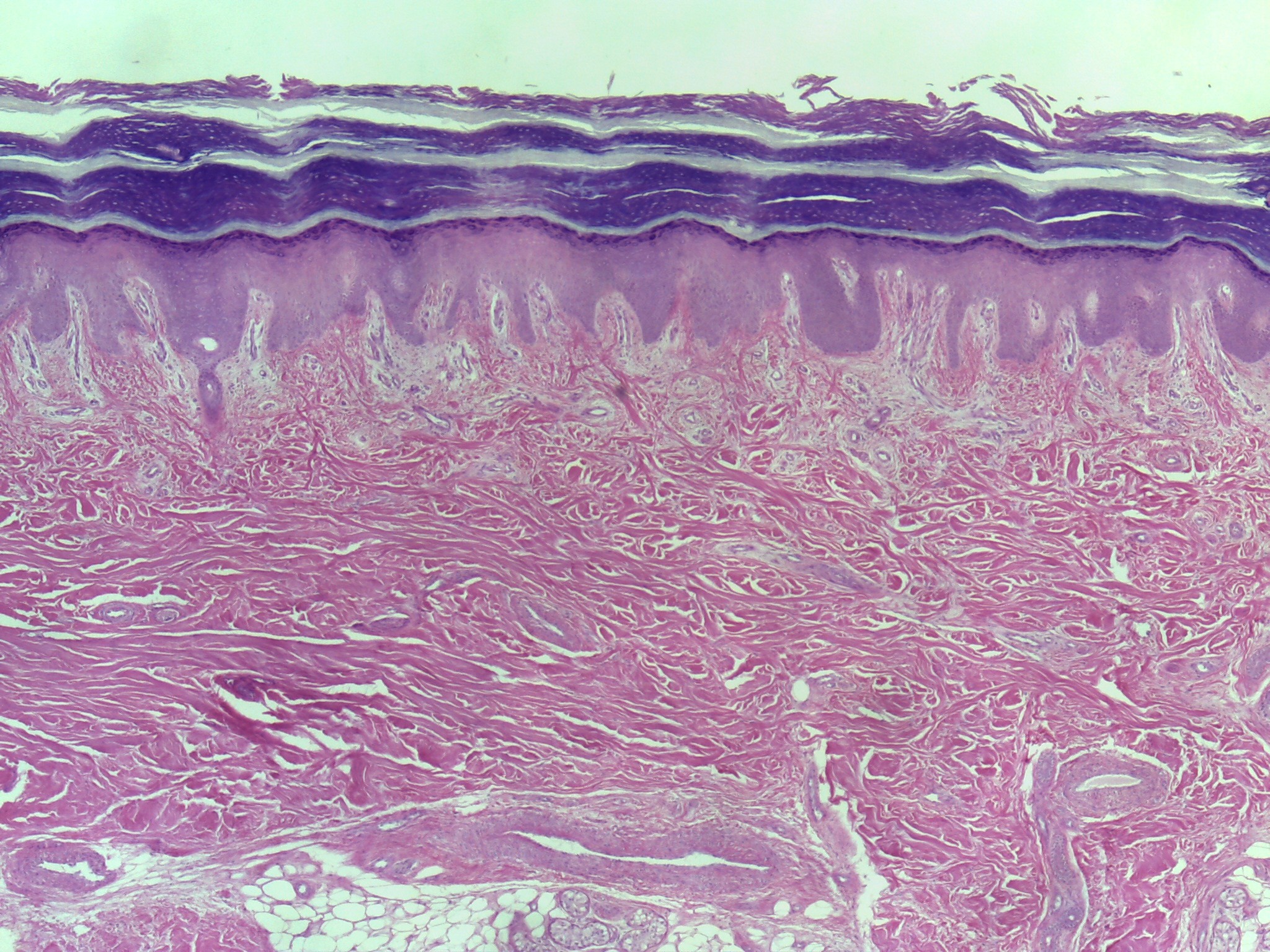
Skin– Dense Irregular Connective Tissue
Similar to slides 32 &33
Focus on dermis
Can see interface between epidermis (keratinized stratified squamous epithelial tissue) and dermis, dense irregular connective tissue.
Superficial aspect of dermis (papillary region) more of a loose connective tissue and deeper you go, into reticular region, denser dermis becomes, dense irregular connective tissue
Dense irregular connective tissue
Densely packed collagen fibers, interwoven in all directions, and contains fibroblast
Forms reticular region of dermis (lower ¾ and ⅘ ), fibrous capsules of organs, joints, and periosteum of bone
-
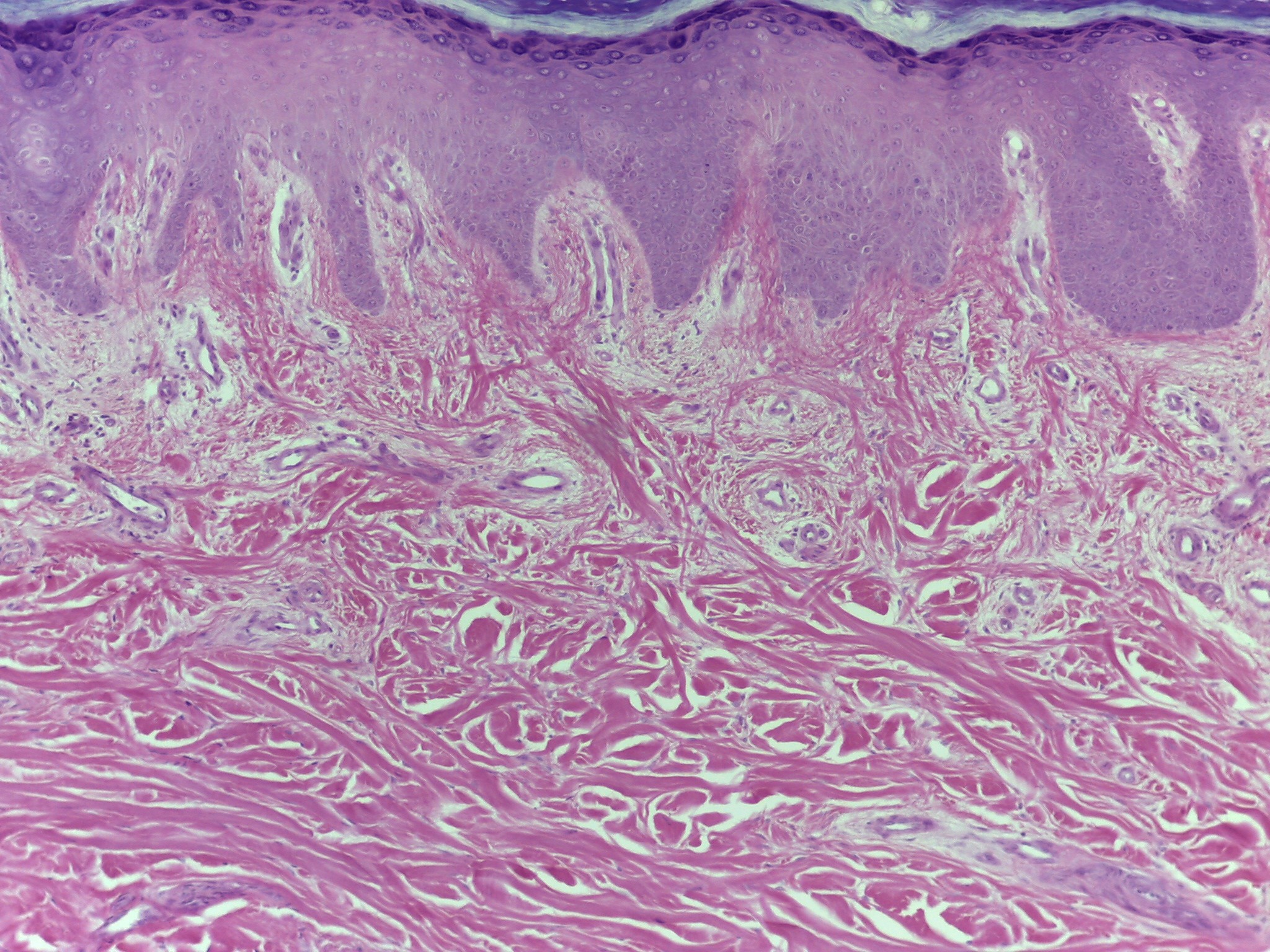
Skin– Dense Irregular Connective Tissue
Similar to slides 32 &33
Focus on dermis
Can see interface between epidermis (keratinized stratified squamous epithelial tissue) and dermis, dense irregular connective tissue.
Superficial aspect of dermis (papillary region) more of a loose connective tissue and deeper you go, into reticular region, denser dermis becomes, dense irregular connective tissue
Dense irregular connective tissue
Densely packed collagen fibers, interwoven in all directions, and contains fibroblast
Forms reticular region of dermis (lower ¾ and ⅘ ), fibrous capsules of organs, joints, and periosteum of bone
-
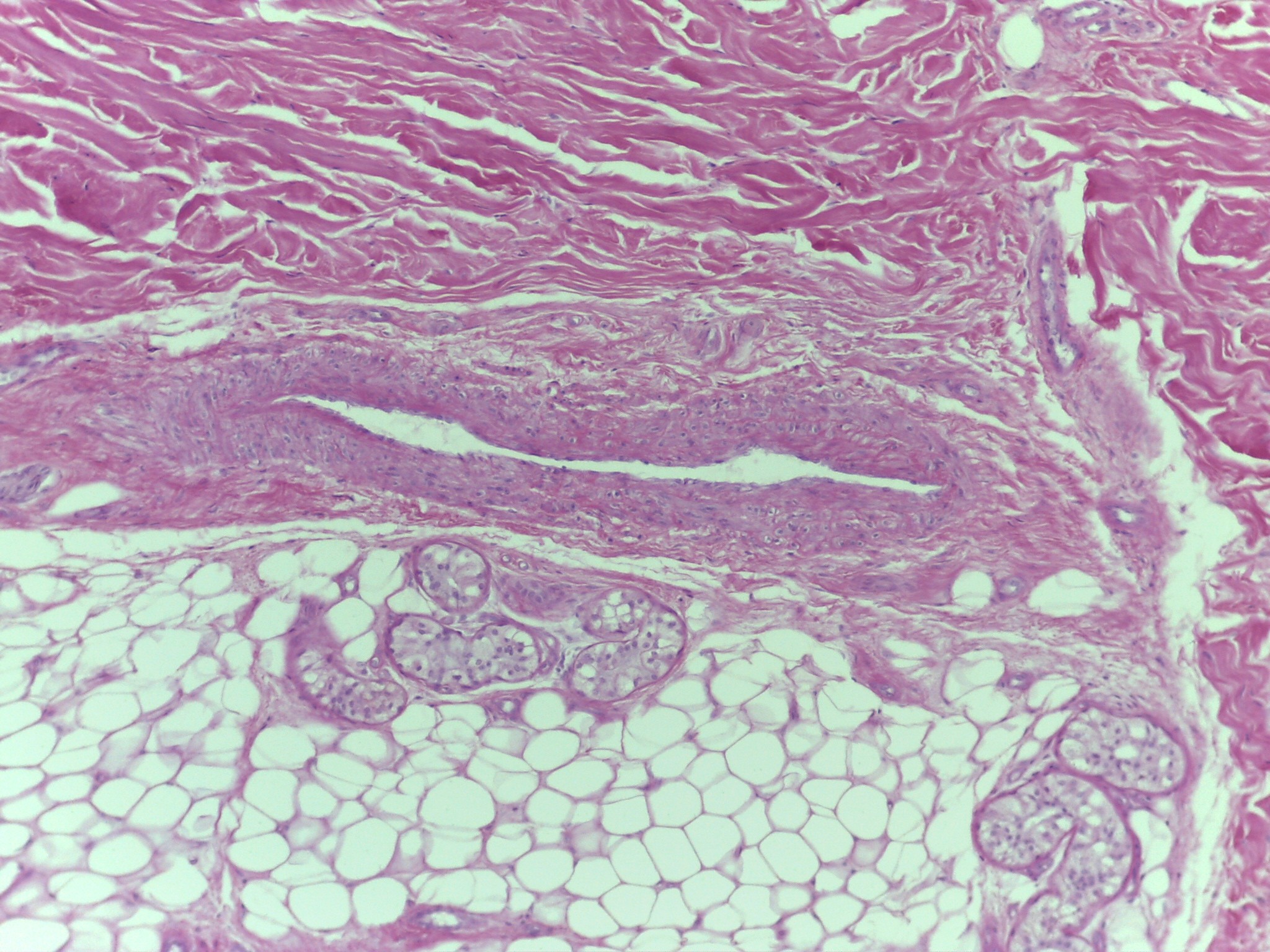
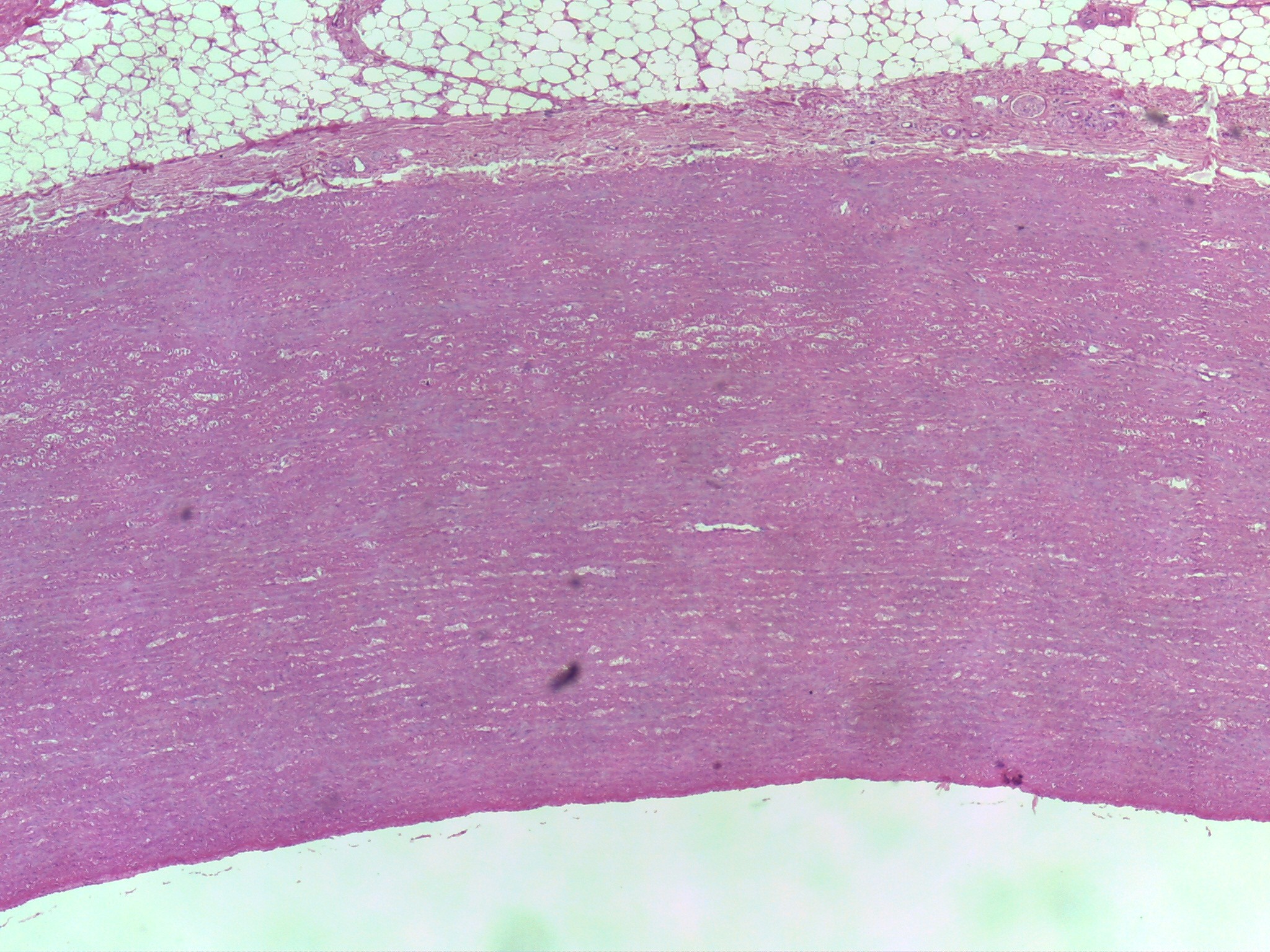
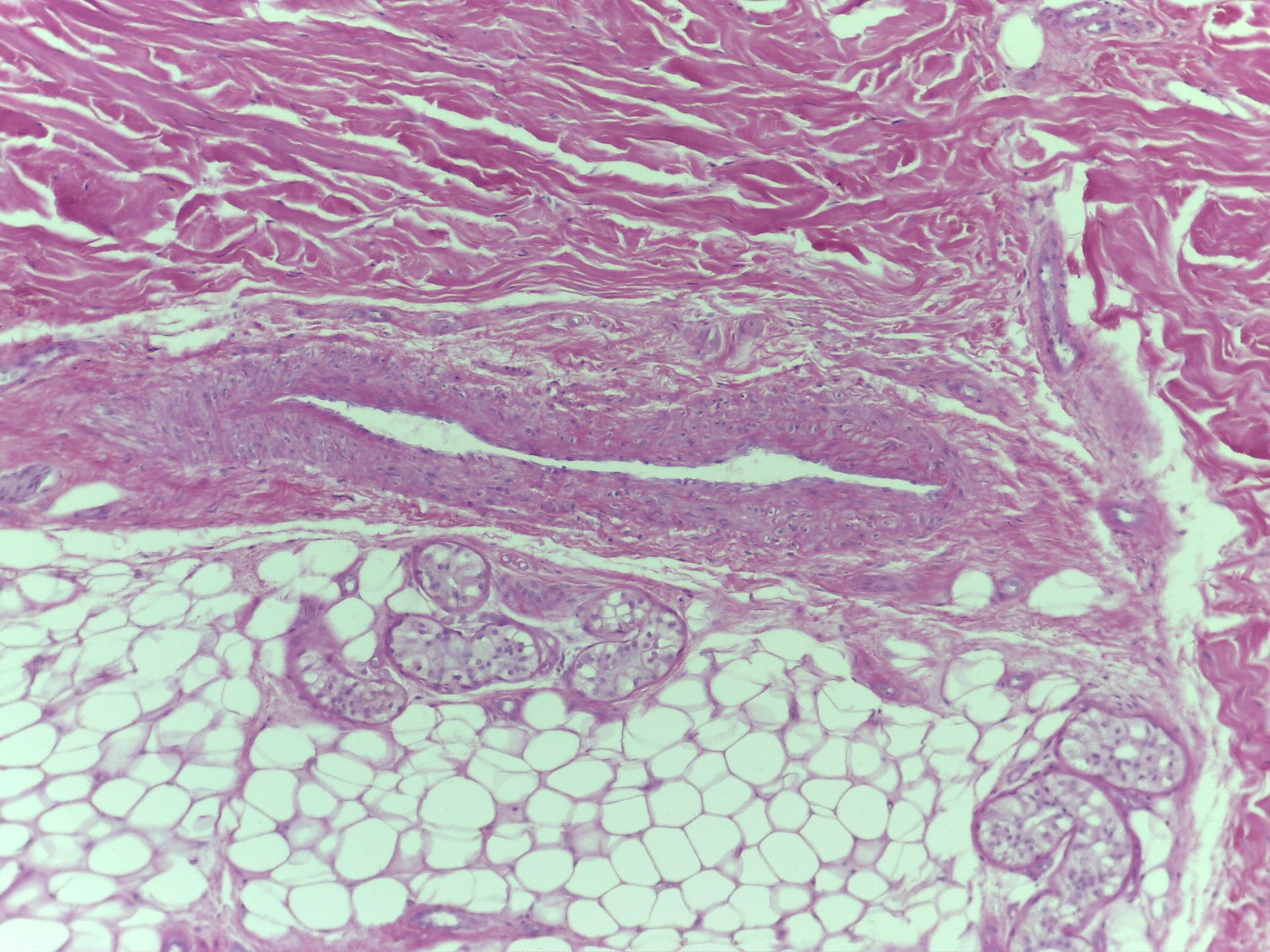
Intermediate of dermis and hypodermis (adipose connective tissue)
Hypodermis is one’s largest aggregation of adipose connective tissue
Adipose Connective Tissue
Located throughout body but mainly in hypodermis
Covers surface of:
Heart
Omentum
Around kidneys
Back of eye
Surrounds joints
Adipose:
Protects
Pads
Stores fat (energy)
Insulates
-
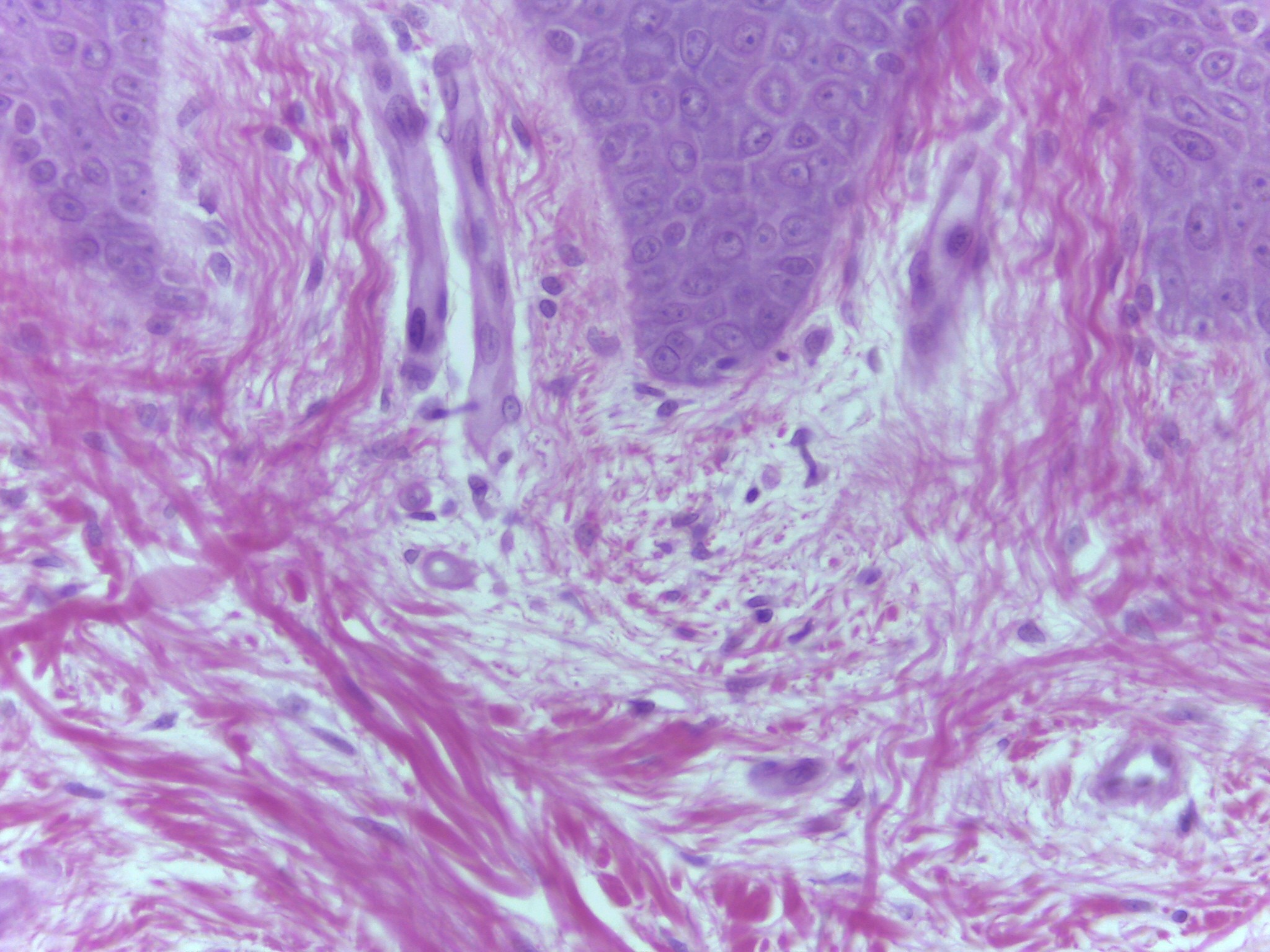
Epidermis– Dermis Interface
High magnification showing interface between epidermis and dermis.
Epidermal components that project inferiorly are called epidermal parallel pegs, dermal components that project superiorly are called dermal papilae
-
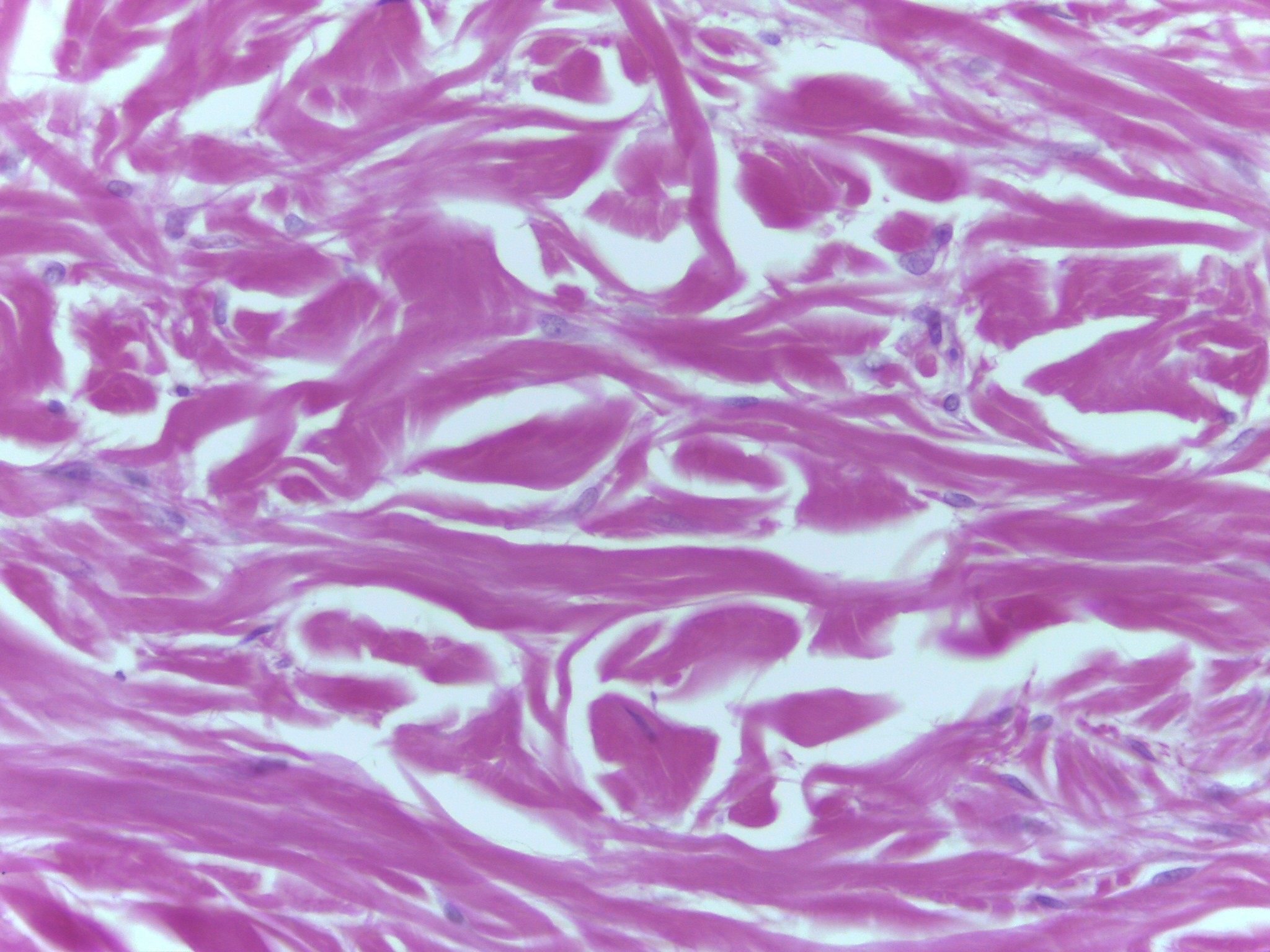
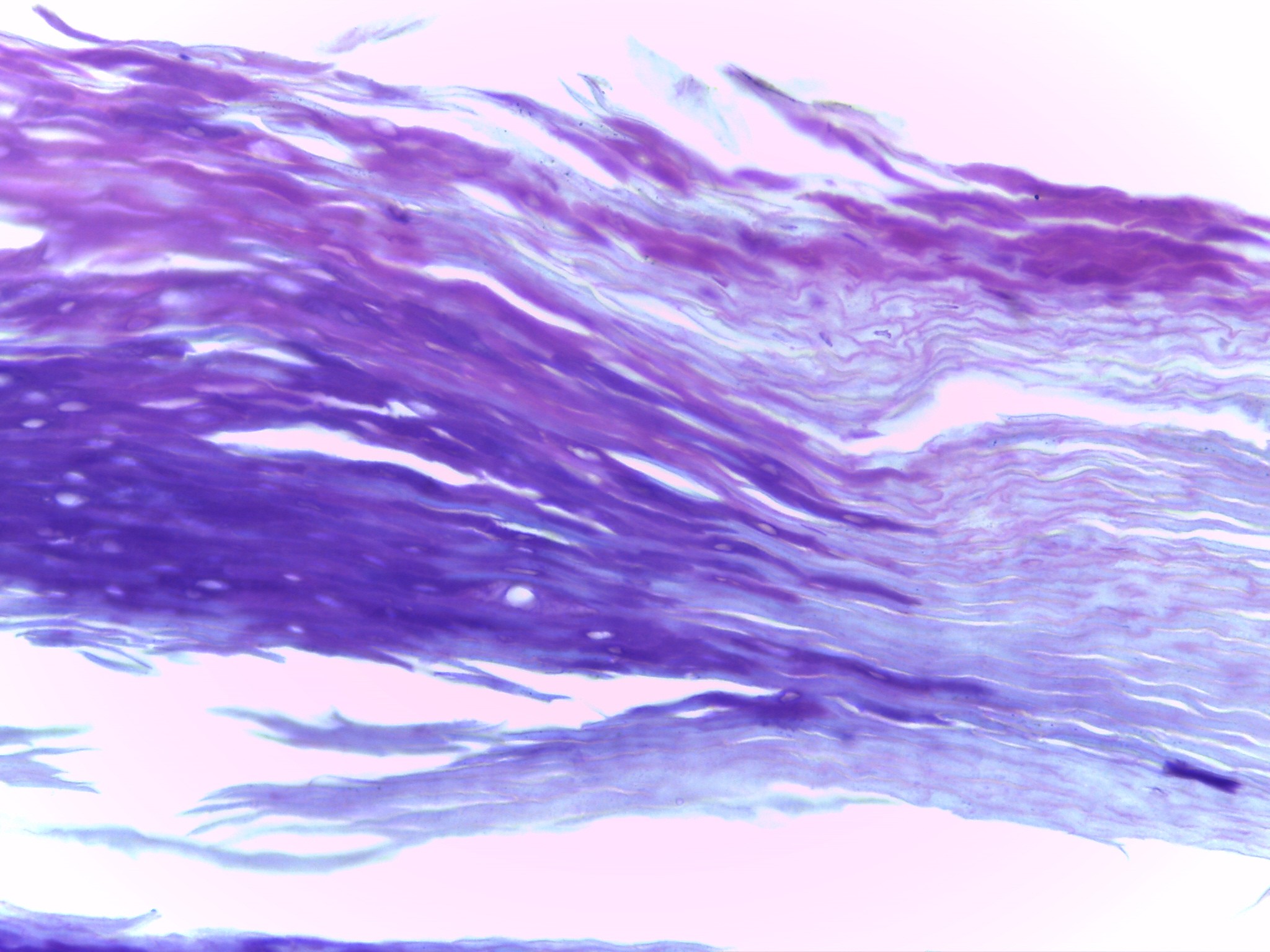
Dermis– Dense Irregular
High magnification deep in dermis (reticular region) of integument where connective tissue is true dense irregular connective tissue
Fibers are collagen fibers and are arranged irregularly
Fibers interwoven and interlocking
Part of an animal’s skin from which leather is made
-
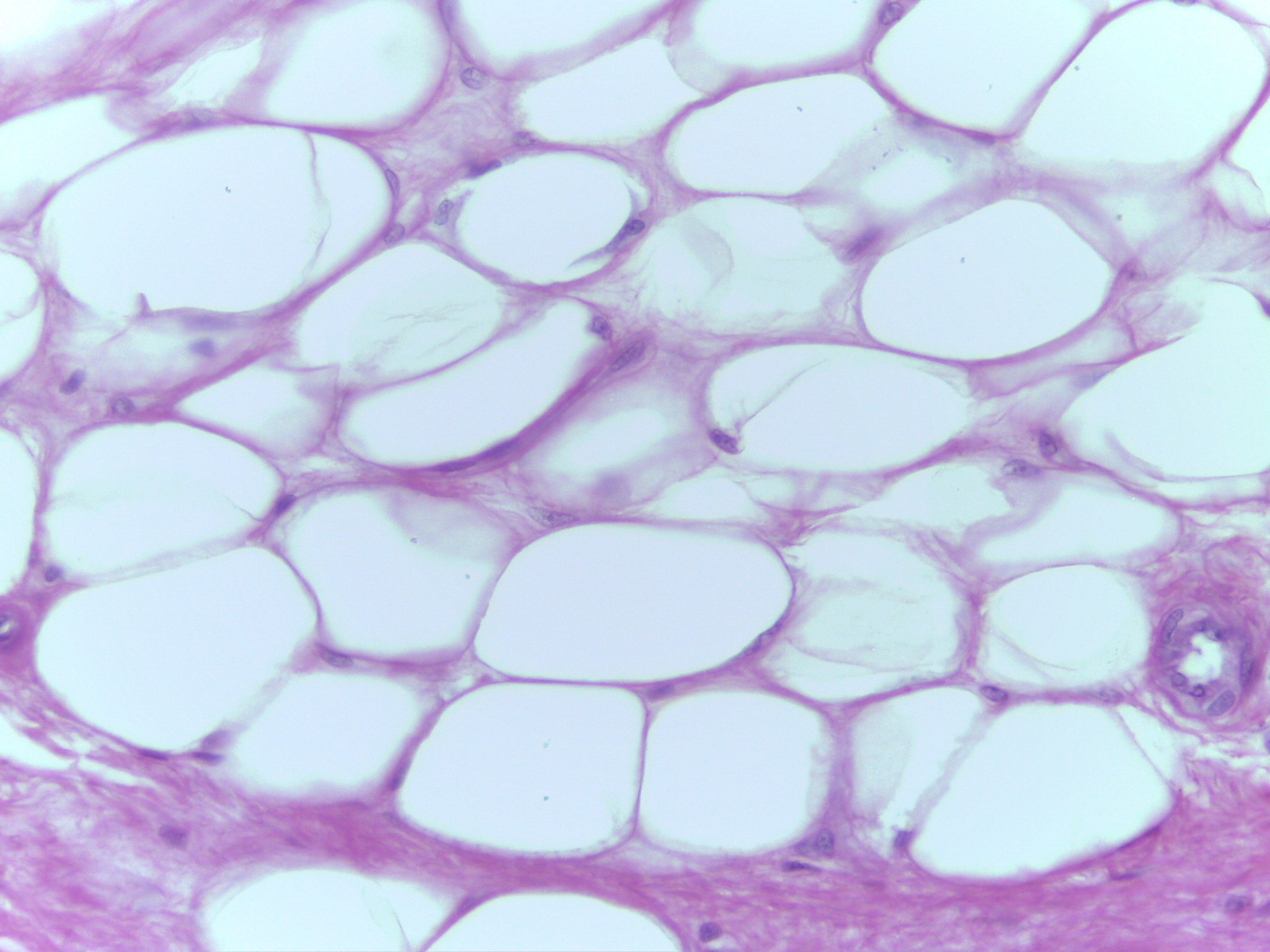
Hypodermis– Adipose
High magnification of adipose connective tissue in hypodermis or subcutaneous of integument
Structure (cells) are adipocytes: store triglycerides
Cells nuclei located at periphery rather than near the center
When cells were living they were filled with triglycerides and all the organelles were forced to the periphery.
-
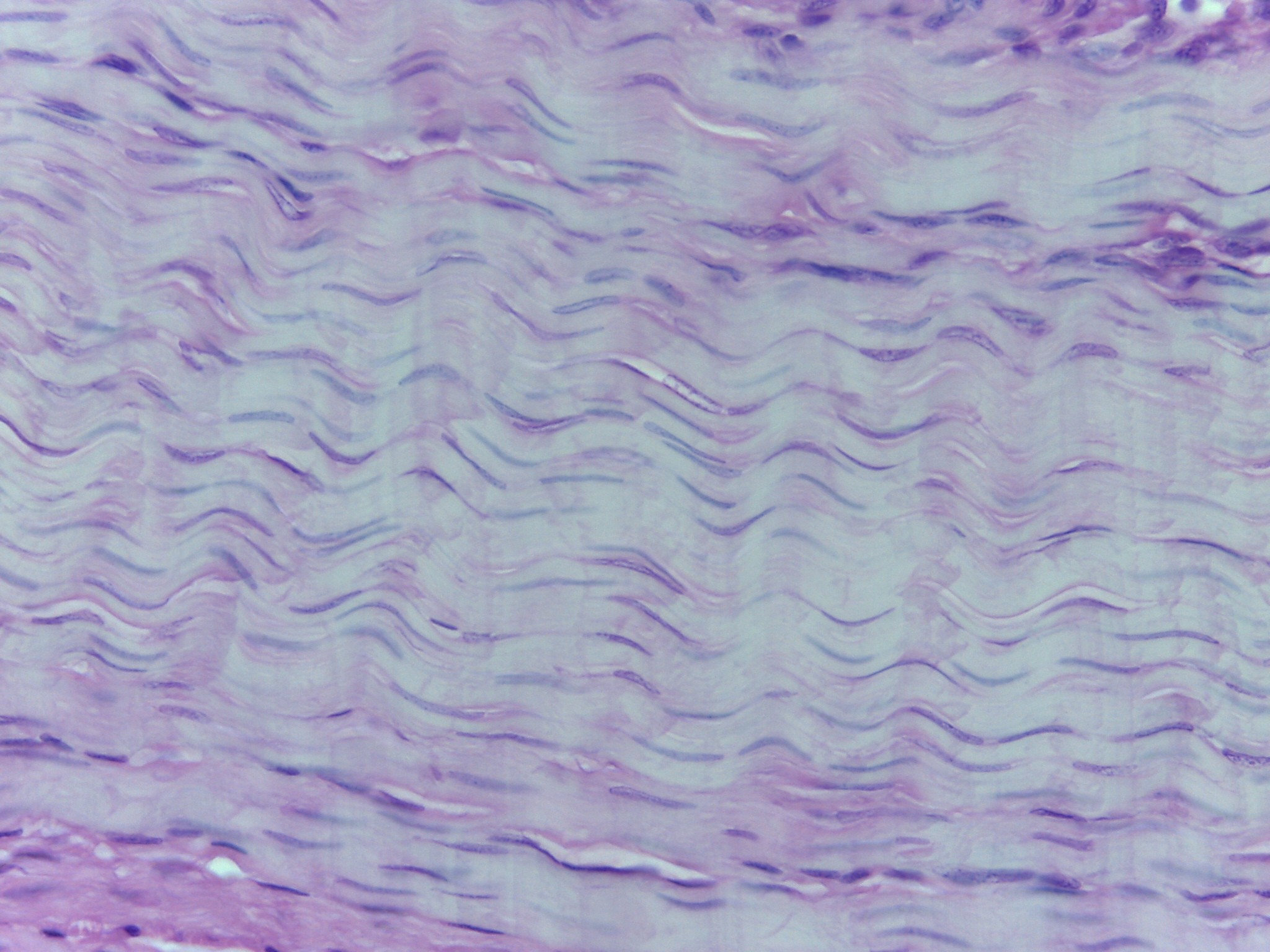
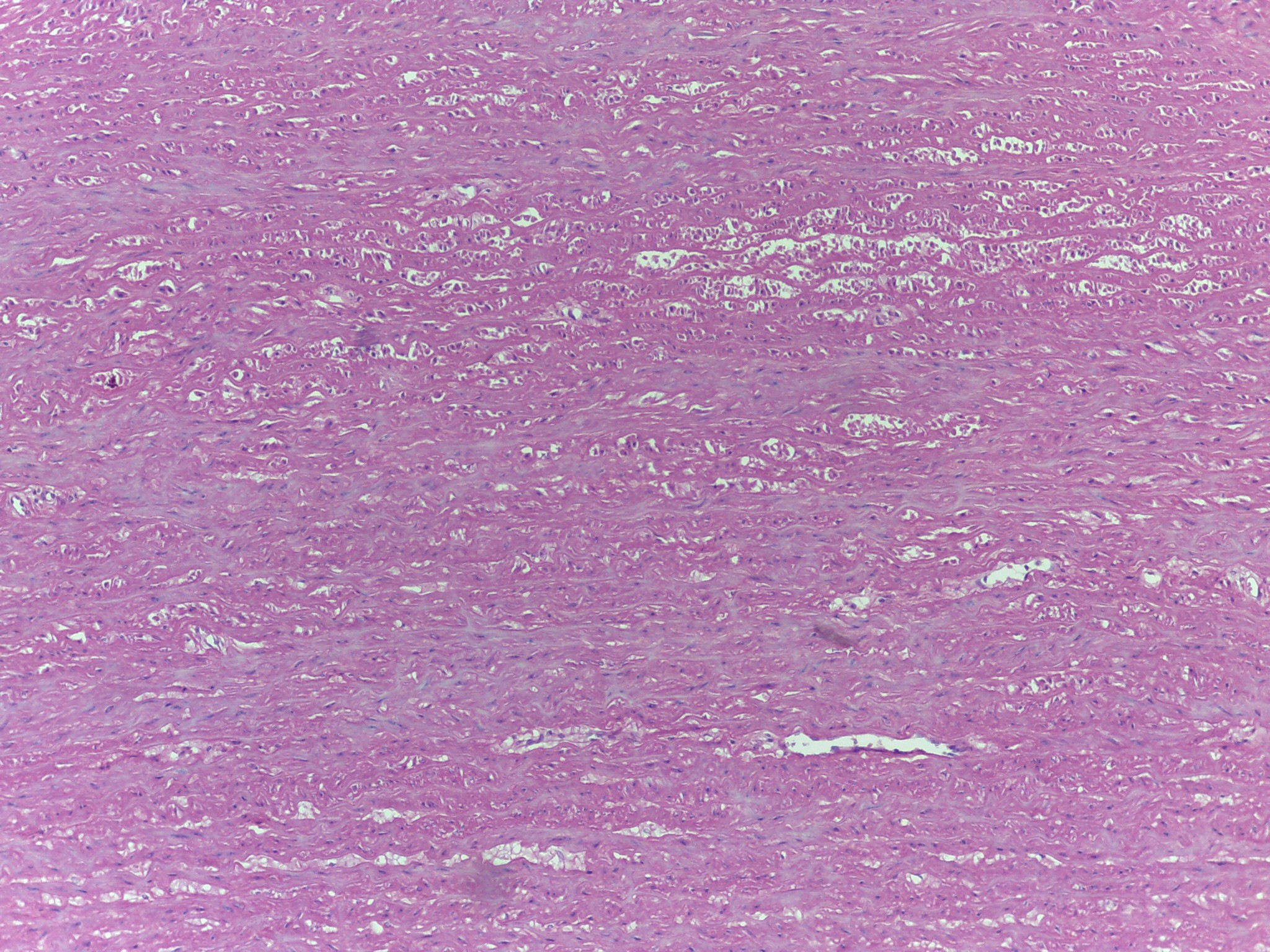
Intermediate magnification of dense regular connective tissue
Dense regular connective tissue collage fibers are predominant type of fiber, just as in dense irregular connective tissue
Difference is dense regular connective tissue the collagen fibers are arranged in parallel fashion
Collagen fibers are parallel to each other and run parallel to long axis of tendon or ligament
Dense regular connective tissue (white fibrous connective tissue)
Densely packed collagen fibers, parallel to long axis of tendon or ligament. Form tendons or ligaments
Collagen: strong, not flexible
-
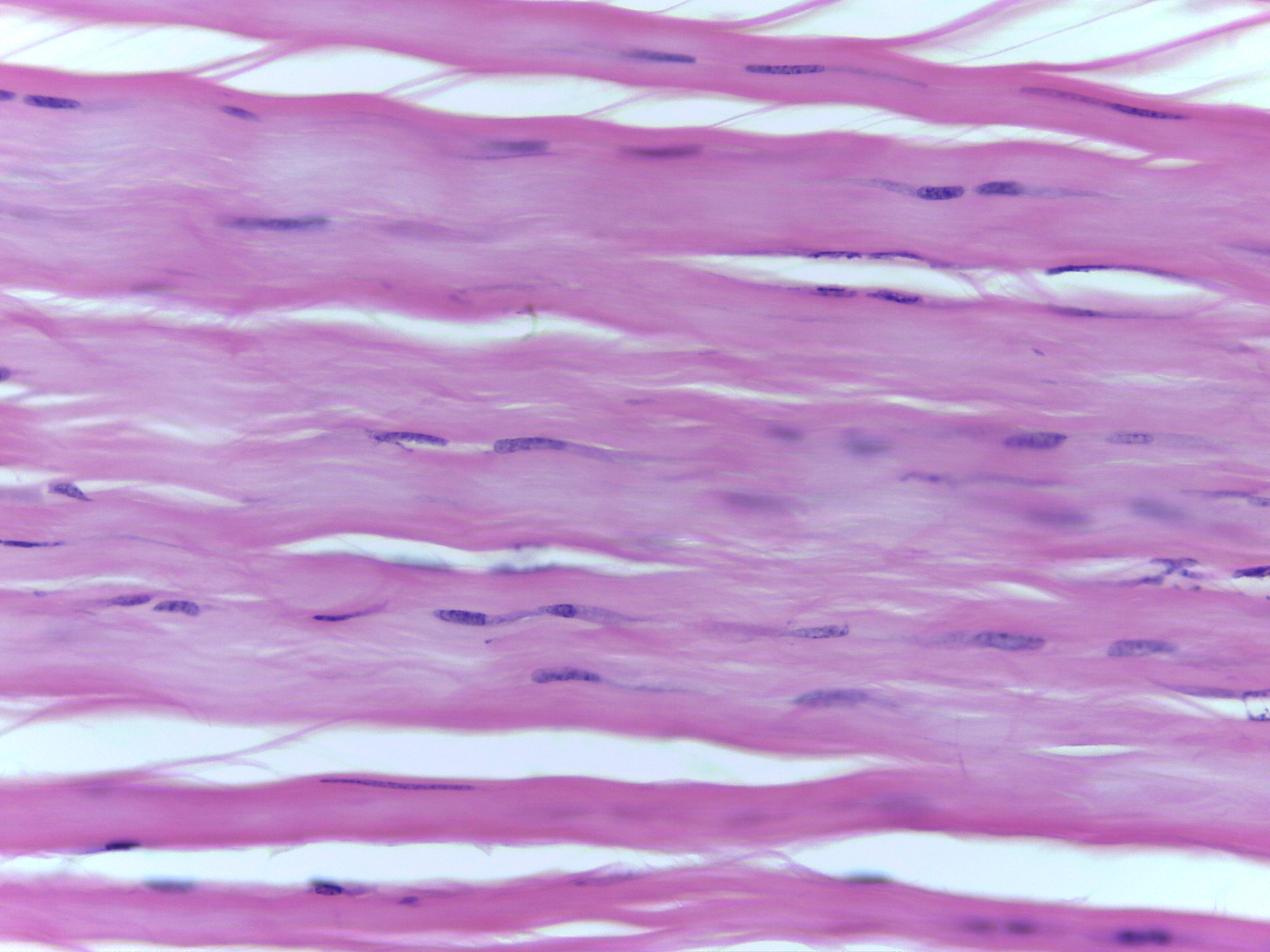
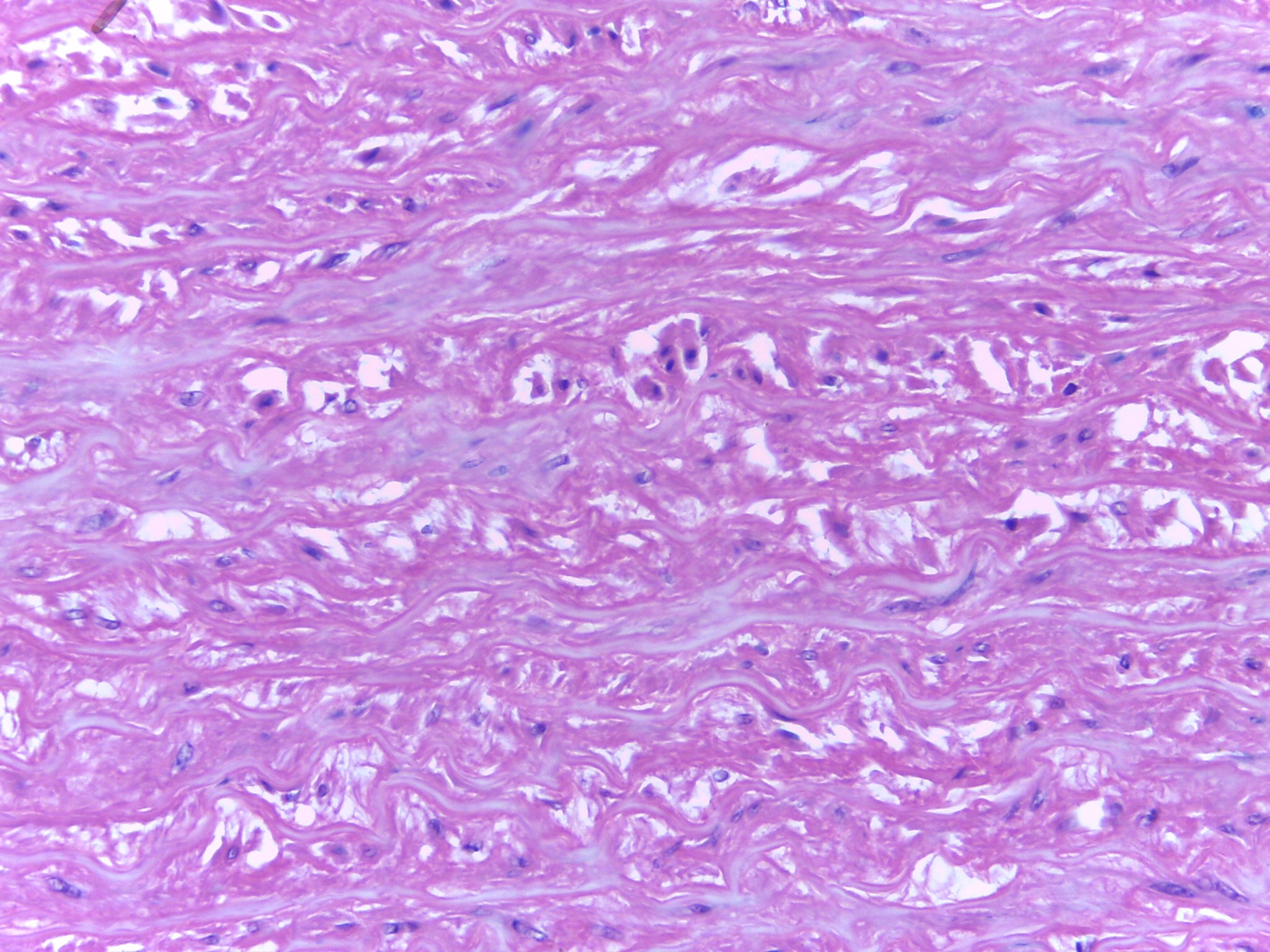
High magnification of dense regular connective tissue
Dense regular connective tissue collage fibers are predominant type of fiber, just as in dense irregular connective tissue
Difference is dense regular connective tissue the collagen fibers are arranged in parallel fashion
Collagen fibers are parallel to each other and run parallel to long axis of tendon or ligament
Dense regular connective tissue (white fibrous connective tissue)
Densely packed collagen fibers, parallel to the long axis of tendon or ligament. Form tendons or ligaments
Collagen: strong, not flexible
-
Dense regular– AKA white fibrous connective tissue
Densely packed collagen fibers, parallel to long axis of tendon or ligament
Form tendons and ligaments
-
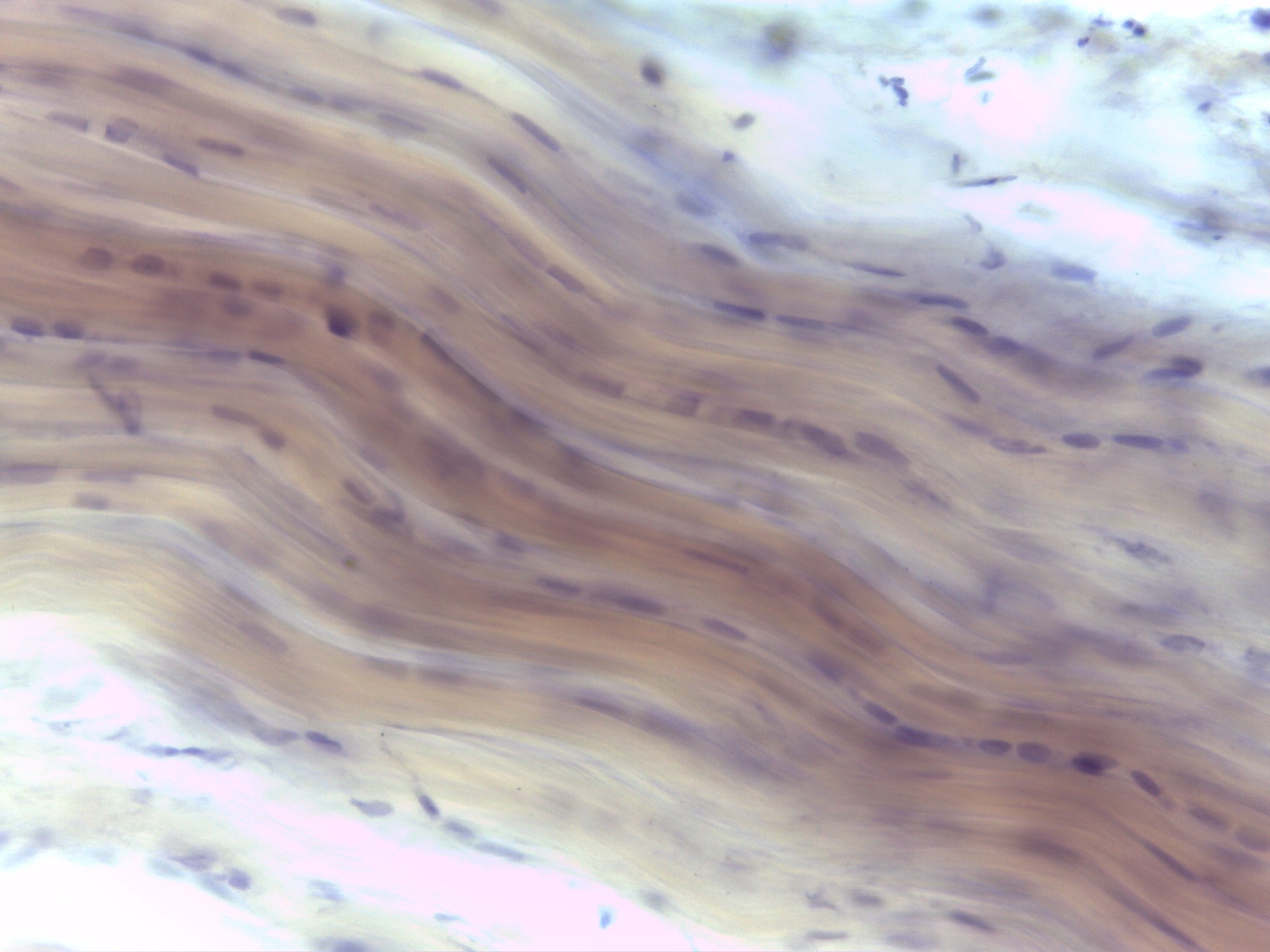
Wall of artery– elastic connective tissue
Elastic connective tissue in wall of aorta
Low magnification
At bottom of image is lumen of the aorta
Elastic connective tissue in arteries in sheets which run perpendicular to wall of vessel.
Arteries rich in elastic connective tissue, compared to veins, because blood pressure is much higher in arteries than in veins
Elastic fibers interwoven into sheets. Found in walls of arteries and lower respiratory tract; contain fibroblast.
Extensible- stretch
Elastic - recoils
-
Wall of artery– elastic connective tissue
Elastic connective tissue in wall of aorta
Low magnification
At bottom of image is lumen of the aorta
Elastic connective tissue in arteries in sheets which run perpendicular to wall of vessel.
Arteries rich in elastic connective tissue, compared to veins, because blood pressure is much higher in arteries than in veins
Elastic fibers interwoven into sheets. Found in walls of arteries and lower respiratory tract; contain fibroblast.
-
Wall of artery– elastic connective tissue
Elastic connective tissue in wall of aorta
Low magnification
At bottom of image is lumen of the aorta
Elastic connective tissue in arteries in sheets which run perpendicular to wall of vessel.
Arteries rich in elastic connective tissue, compared to veins, because blood pressure is much higher in arteries than in veins
Elastic fibers interwoven into sheets. Found in walls of arteries and lower respiratory tract; contain fibroblast.
-
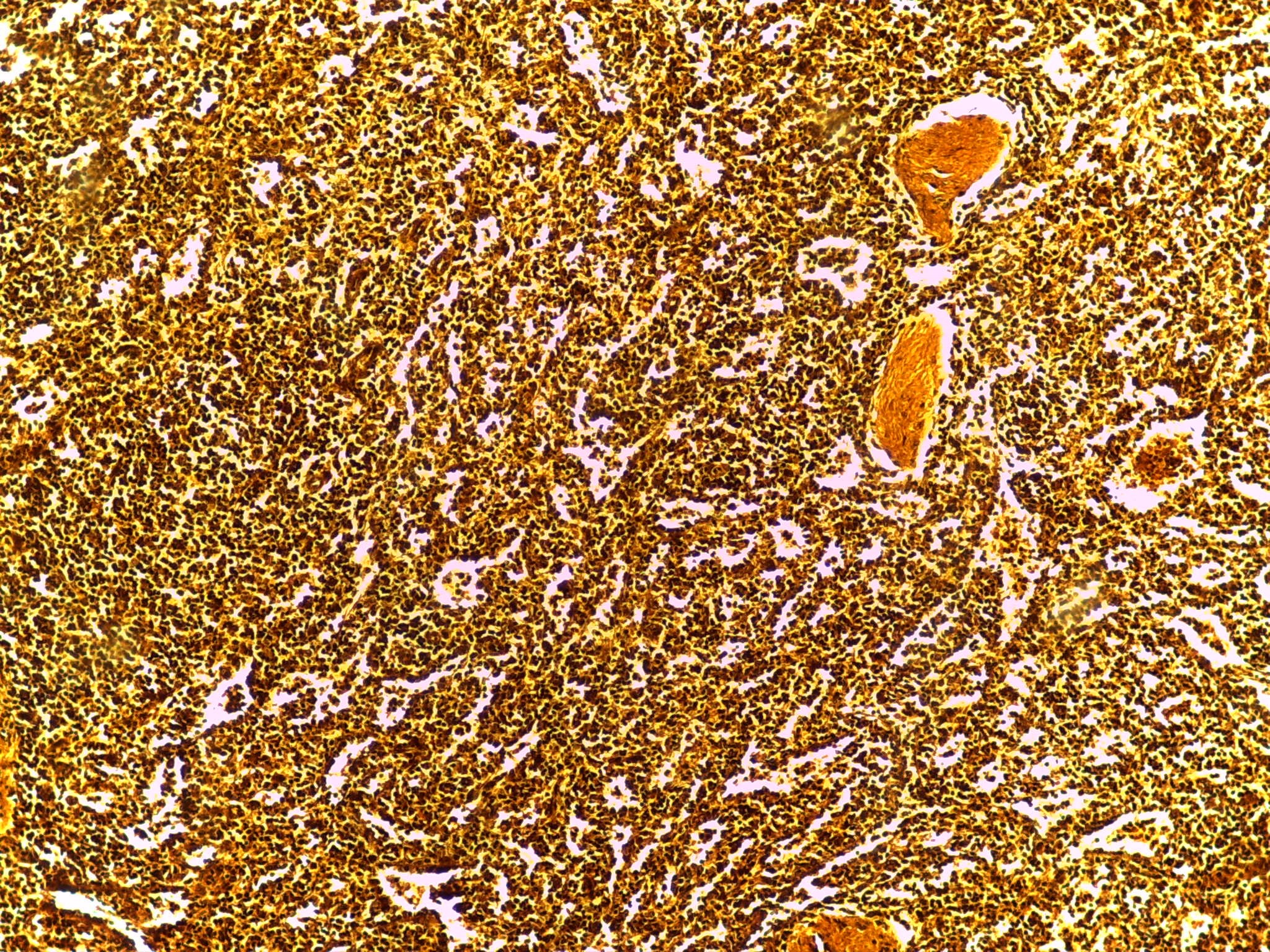
Reticular connective tissue
Reticular connective tissue taken from spleen
Predominate fibers are reticular fibers and spots are reticulocytes or reticuloblast: cells that produce reticular fibers
Reticulocyte refers not only to cells which produce reticular fibers but also to an immature erythrocyte.
Large space that is copper colored is called a sinusoid: cavity or space filled with blood
Actually see erythrocytes in sinusoid because make up 94% of blood cells.
-
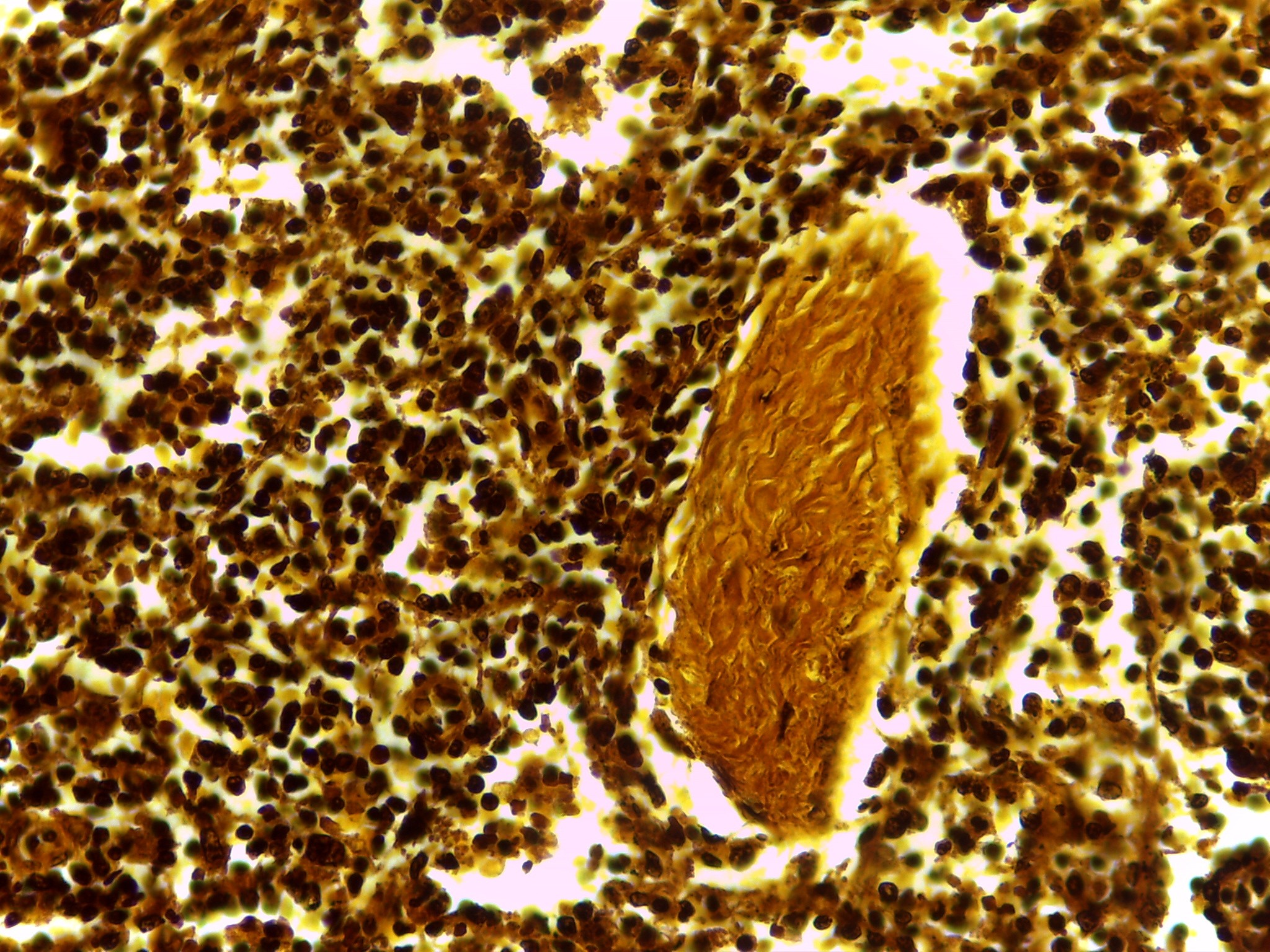
Reticular connective tissue
Reticular fibers are irregularly arranged.
Found in:
Liver
Spleen
Lymph Nodes
Thymus
Bone Marrow
Contains:
Reticuloblast
Mast cells
Macrophages
Reticulocyte/Reticuloblast: produces reticular fibers
-
Adipose connective tissue
Located throughout body but mainly in hypodermis
Covers surface of:
Heart
Omentum
Around kidneys
Back of eye
Surrounds joints
Adipose
Protects
Pads
Stores fat (energy)
Insulates
-
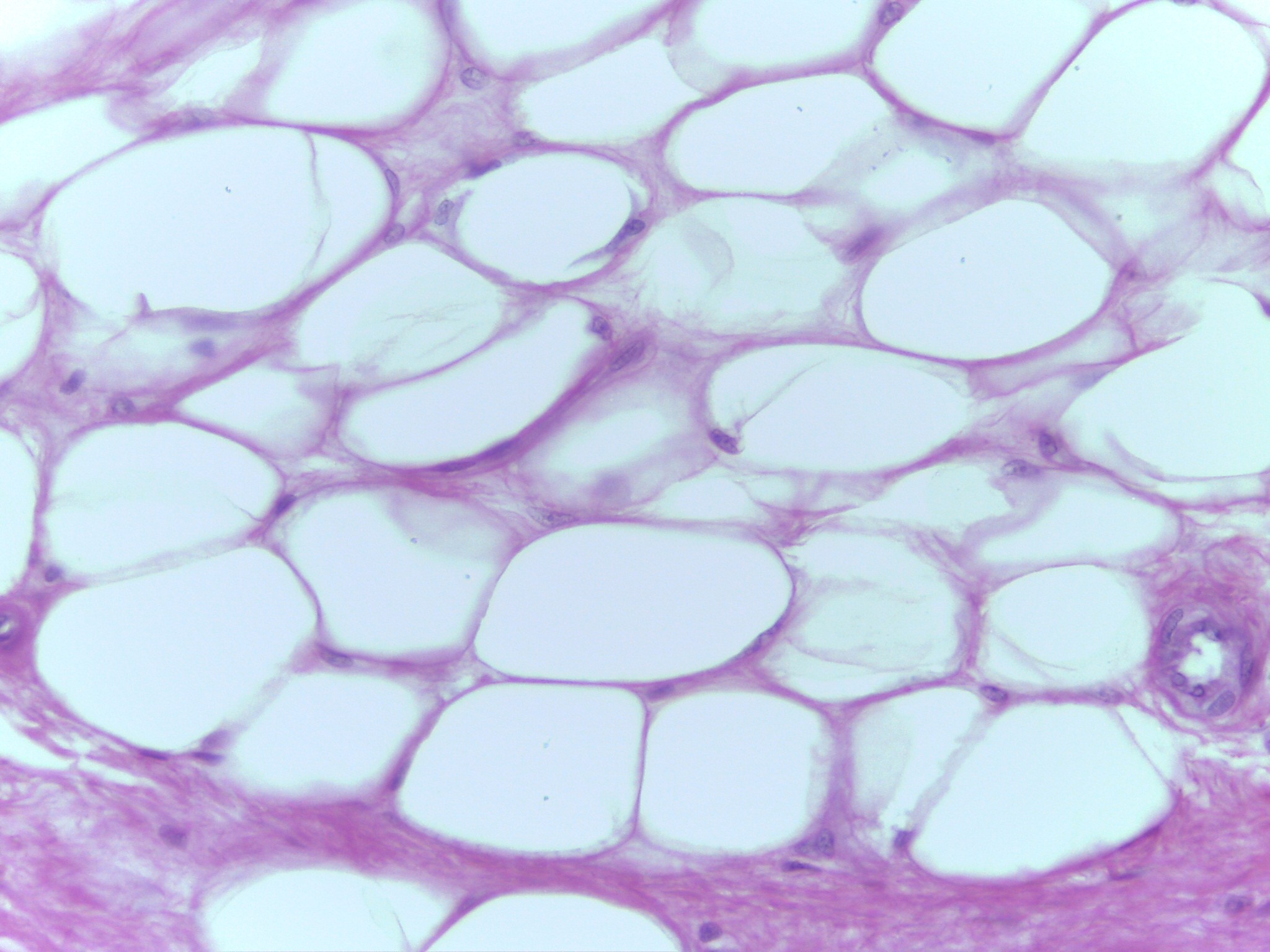
Adipose connective tissue
Located throughout body but mainly in hypodermis
Covers surface of:
Heart
Omentum
Around kidneys
Back of eye
Surrounds joints
Adipose
Protects
Pads
Stores fat (energy)
Insulates
-
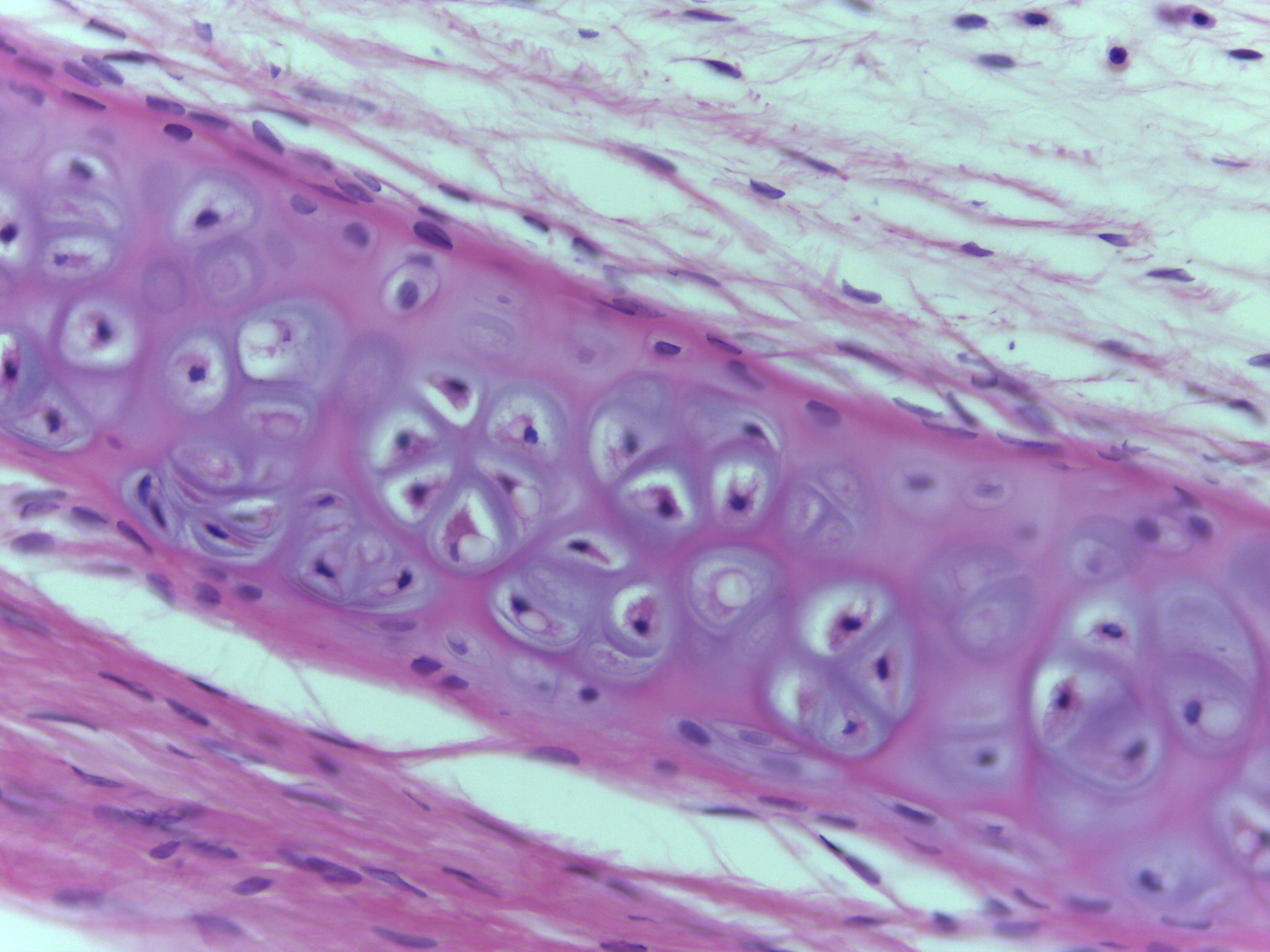
Same images as slides 52 and 58; taken from the trachea
C-shaped rings of the trachea are made of hyaline cartilage connective tissue to prevent it from collapsing
Connective tissue provides support, physical and metabolic, for epithelial tissue
Epithelial tissue is avascular and connective is vascular, mature cartilage is avascular, why it is very difficult for torn cartilage to heal
Cartilage tissue
Composed of chondrocytes contained within elastic matrix
Chondrocytes contained within spaces called lacunae. Lacunae may contain one of many chondrocytes.
Mature cartilage avascular so very slow to heal after injury
-
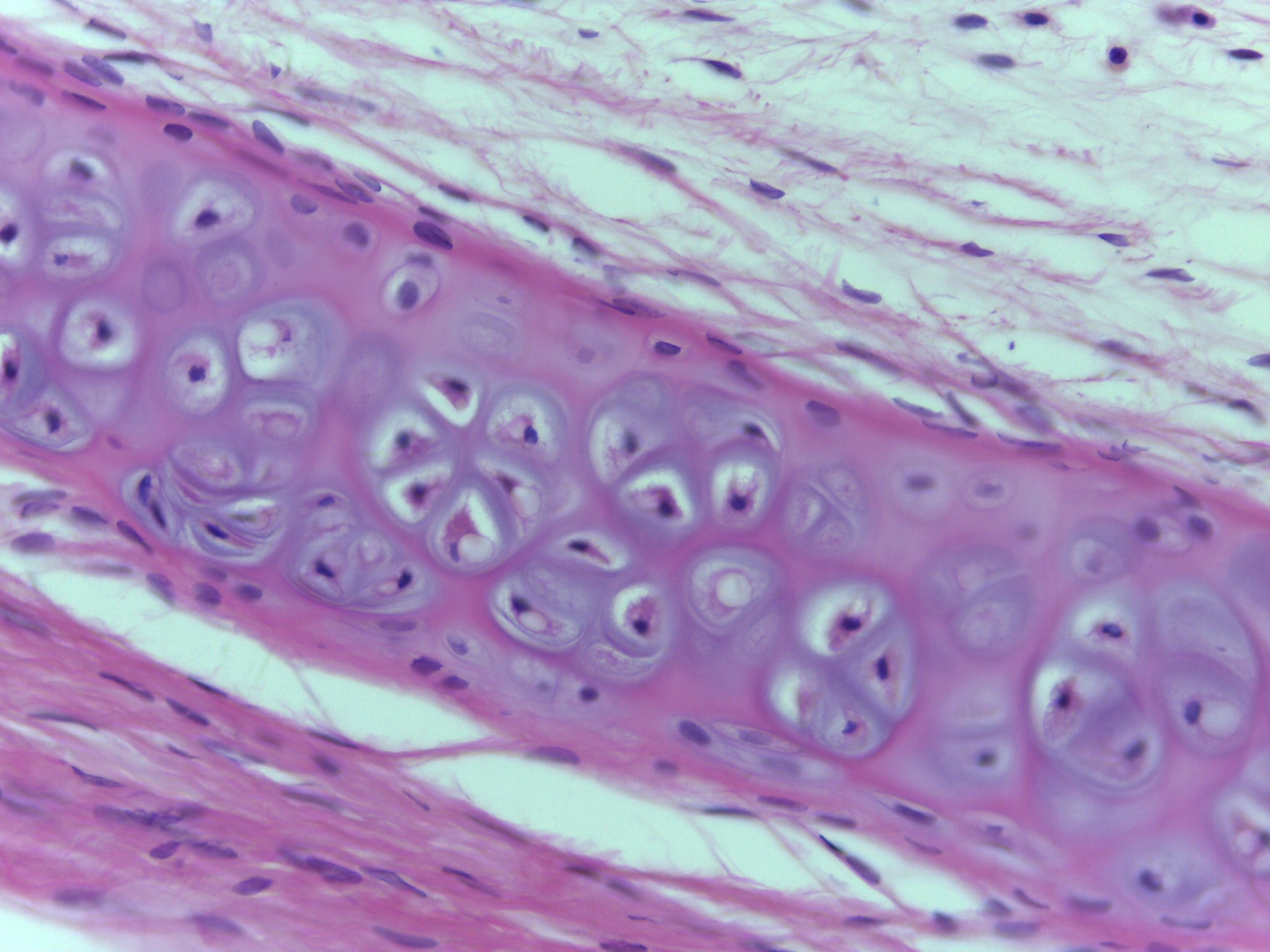
Same images as slides 52 and 58; taken from the trachea
Hyaline Cartilage
Most common in the body
Known as gristle in meat
Forms:
Articular surfaces of bones (articular cartilage)
Rings in trachea and upper respiratory tract
Nasal septum
Costal cartilage between ribs and sternum (sternocostal joints)
Fetal skeleton
High power of hyaline cartilage, can discern spaces called lacunae that contain chondrocytes
-
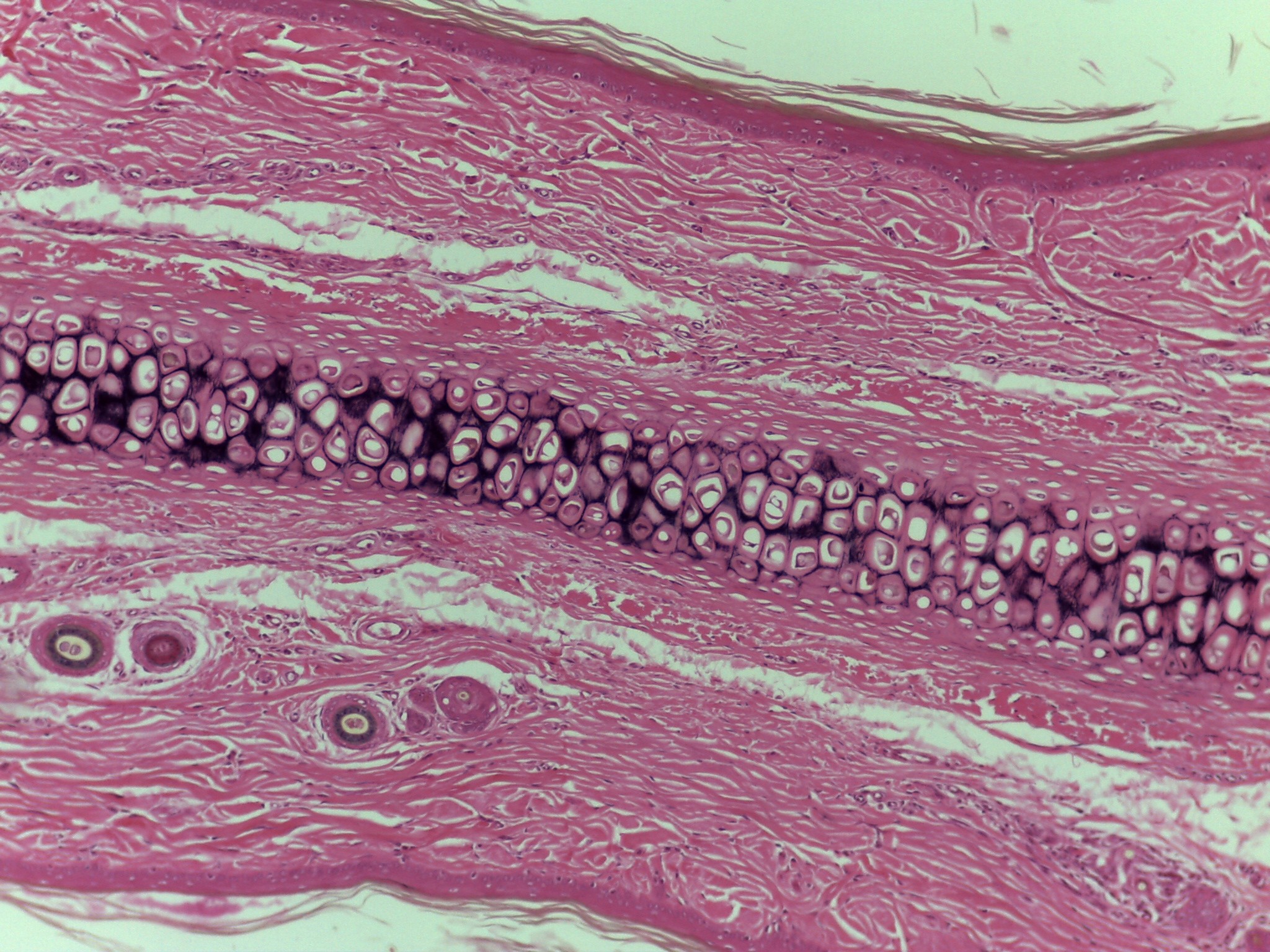
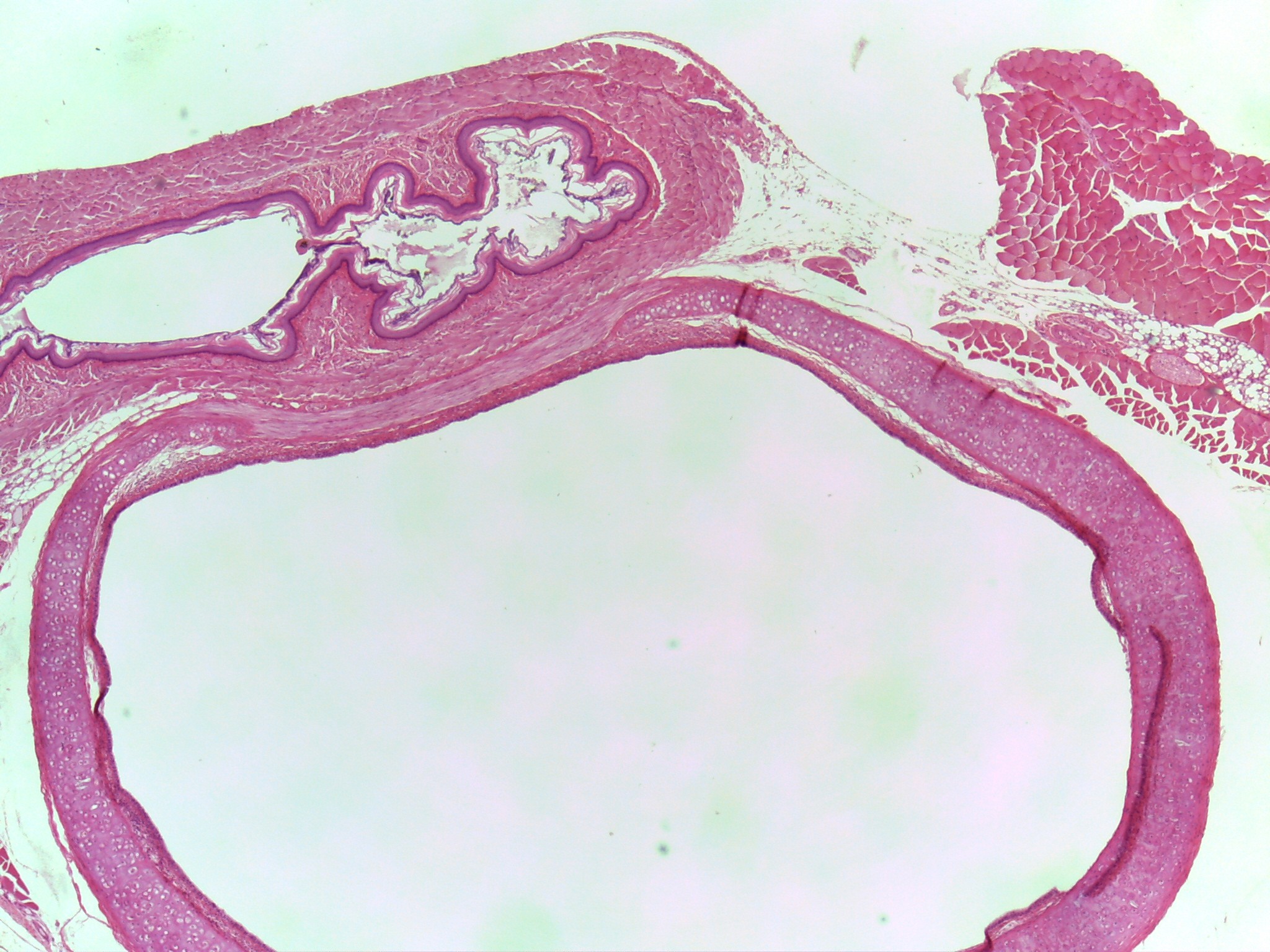
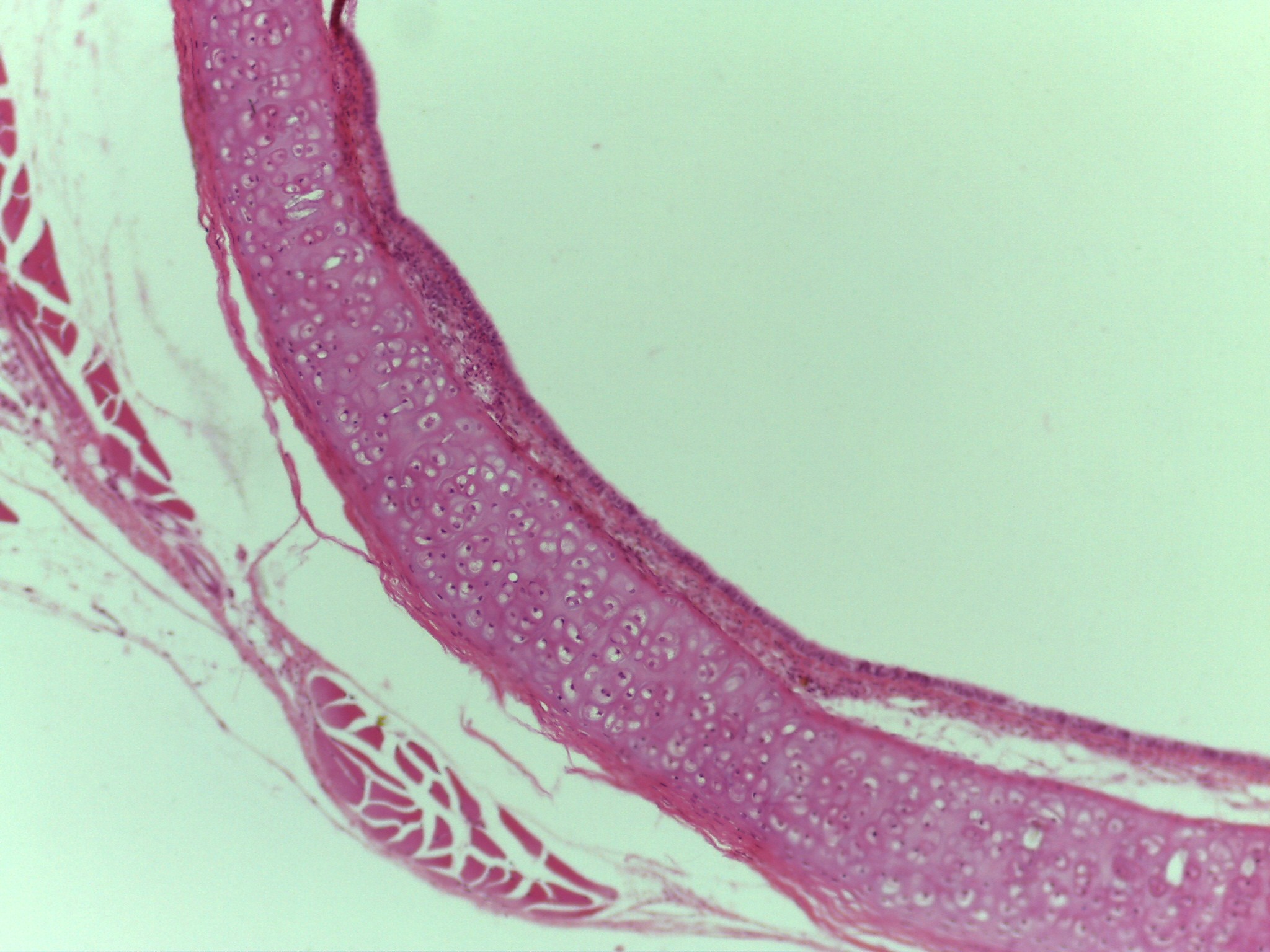
Elastic cartilage connective tissue
Intermediate magnification of external ear of Mus musculus: common mouse
Intermediate aspect of external ear is composed of elastic cartilage connective tissue
There is skin of either side of the elastic cartilage
On each side of the elastic cartilage is dense irregular connective tissue (dermis) and keratinized stratified squamous epithelial tissue (epidermis)
Elastic cartilage connective tissue:
Very flexible cartilage containing elastic fibers that are found in:
External ear
Epiglottis
Larynx
Auditory canal
-
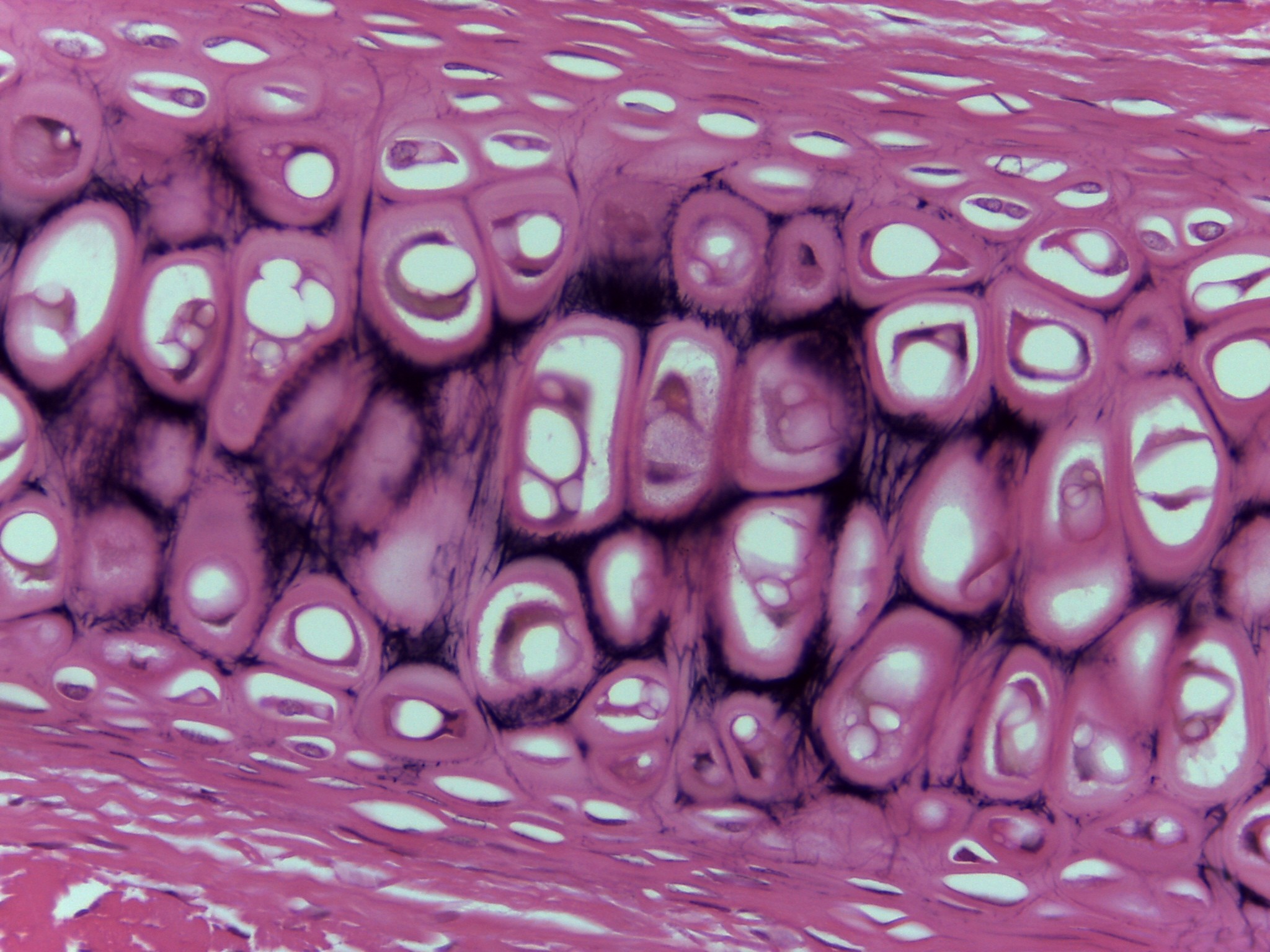
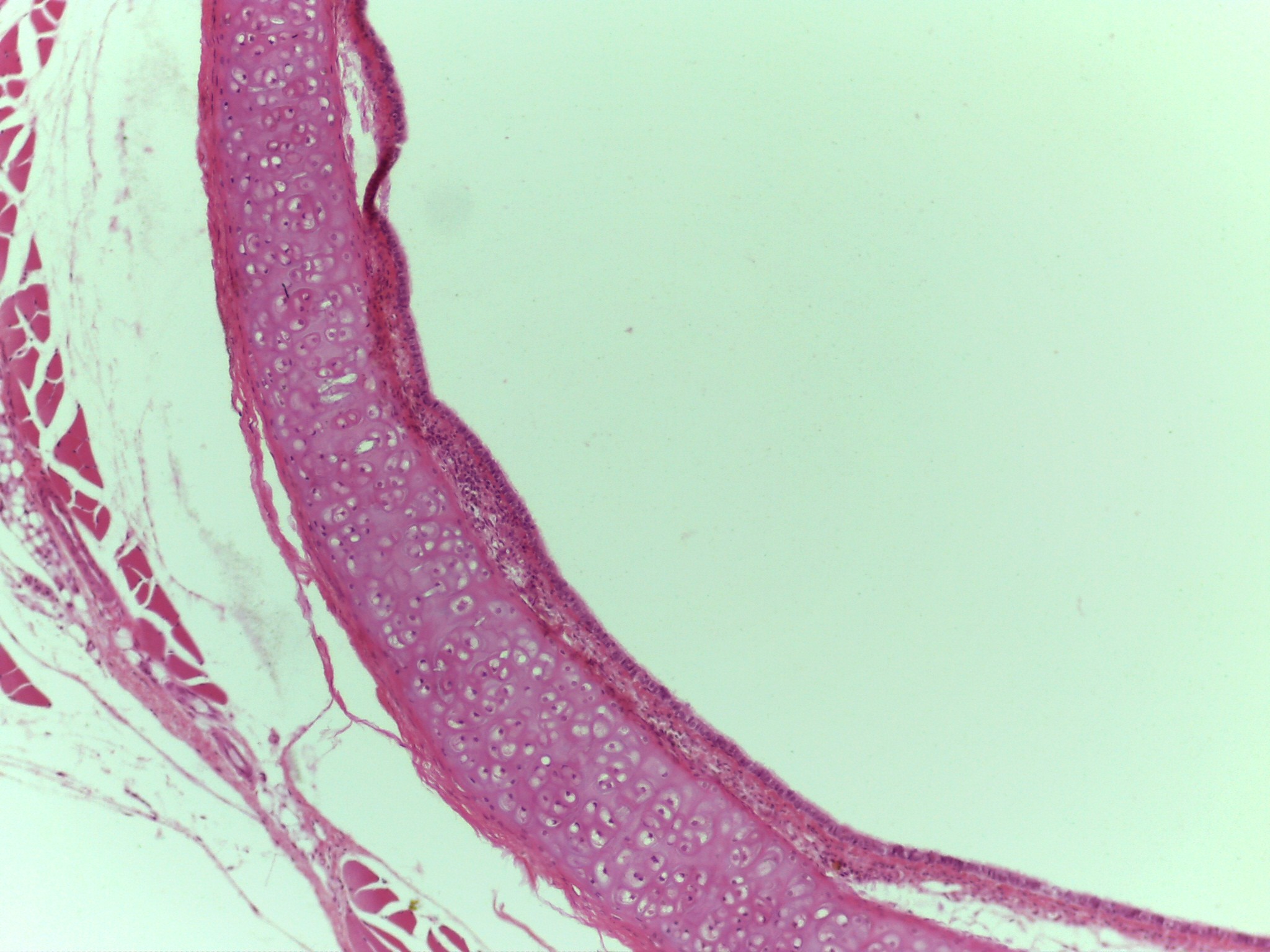
Elastic cartilage connective tissue
High power magnification of external ear of Mus musculus: common mouse
Intermediate aspect of external ear is composed of elastic cartilage connective tissue
Same ultrastructure as discussed in hyaline cartilage, lacunae and chondrocytes.
Very easy to see elastic fibers.
Elastic cartilage connective tissue:
Very flexible cartilage containing elastic fibers that are found in:
External ear
Epiglottis
Larynx
Auditory canal
-
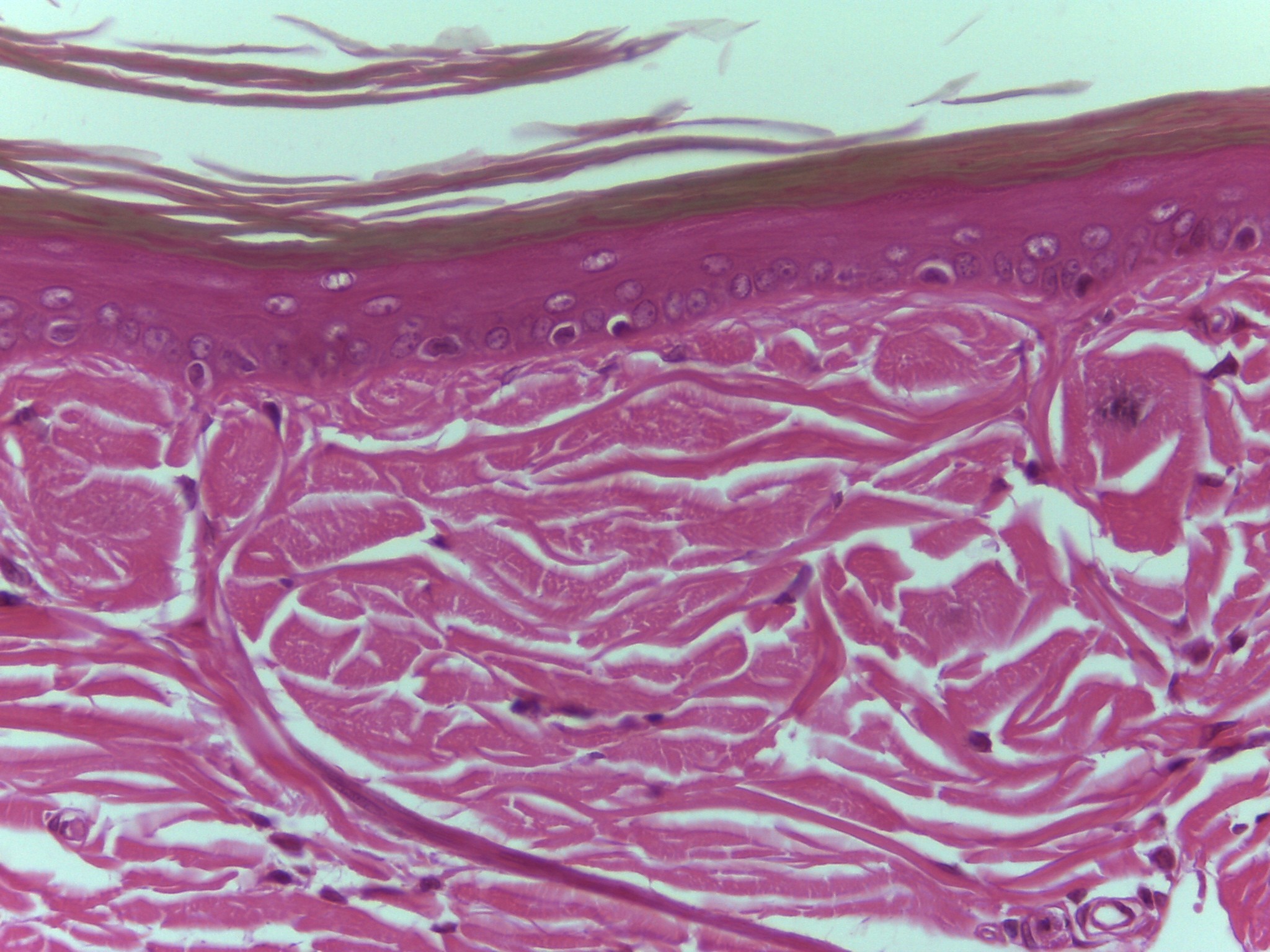
Elastic cartilage connective tissue (skin of ear)
High power magnification view of area above (not anatomical) elastic cartilage
Easy to see this is skin
Elastic cartilage connective tissue:
Very flexible cartilage containing elastic fibers that are found in:
External ear
Epiglottis
Larynx
Auditory canal
-
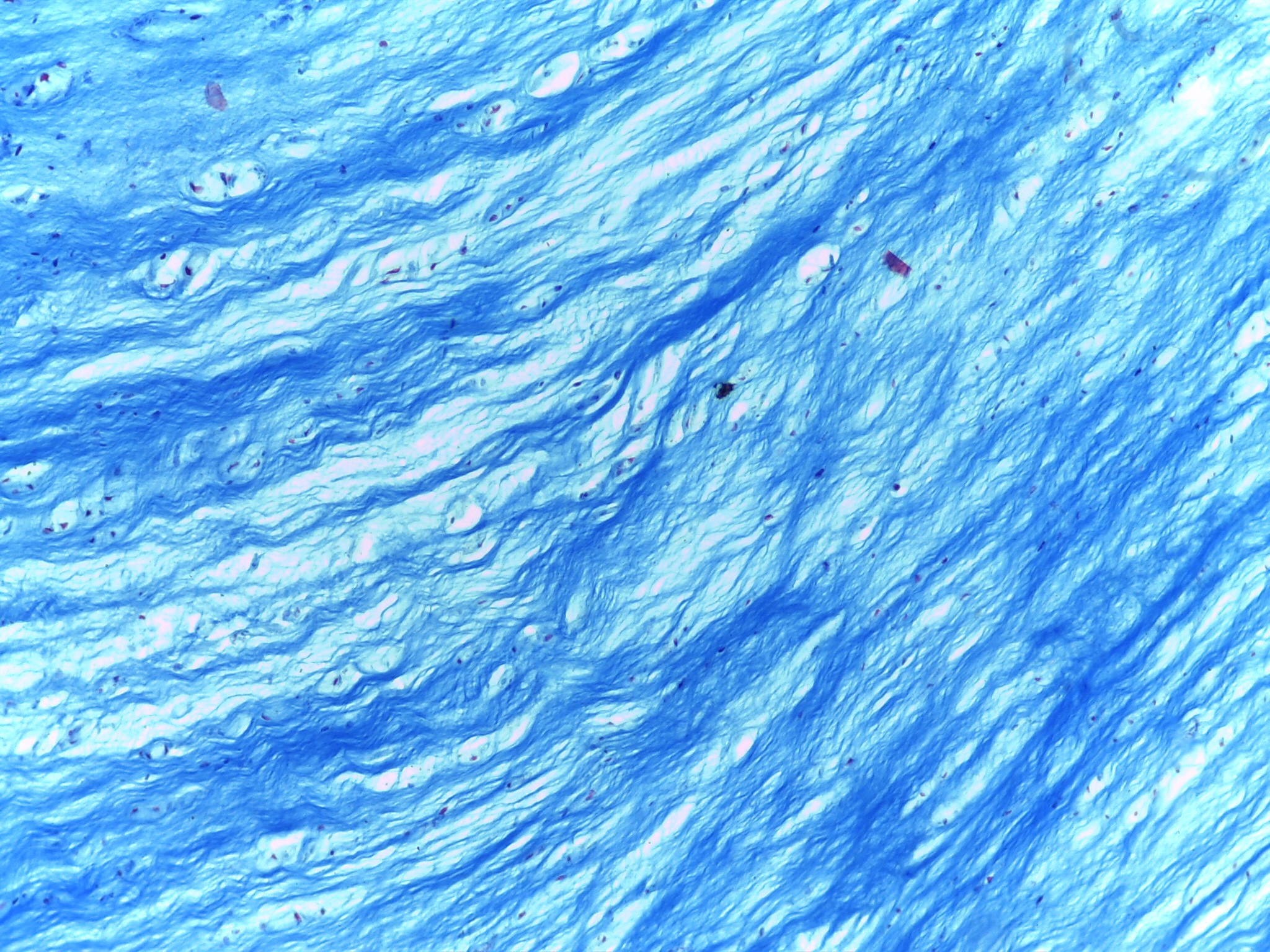
Fibrocartilage connective tissue
Intermediate magnification
Fibrocartilage: strong,built to withstand compression; well suited for menisci of knees, intervertebral joints, symphysis pubis.
Blue fibers: collagen fibers; characteristic of fibrocartilage
Red spots: chondrocytes within their lacunae, same ultrastructure as discussed in hyaline cartilage
-
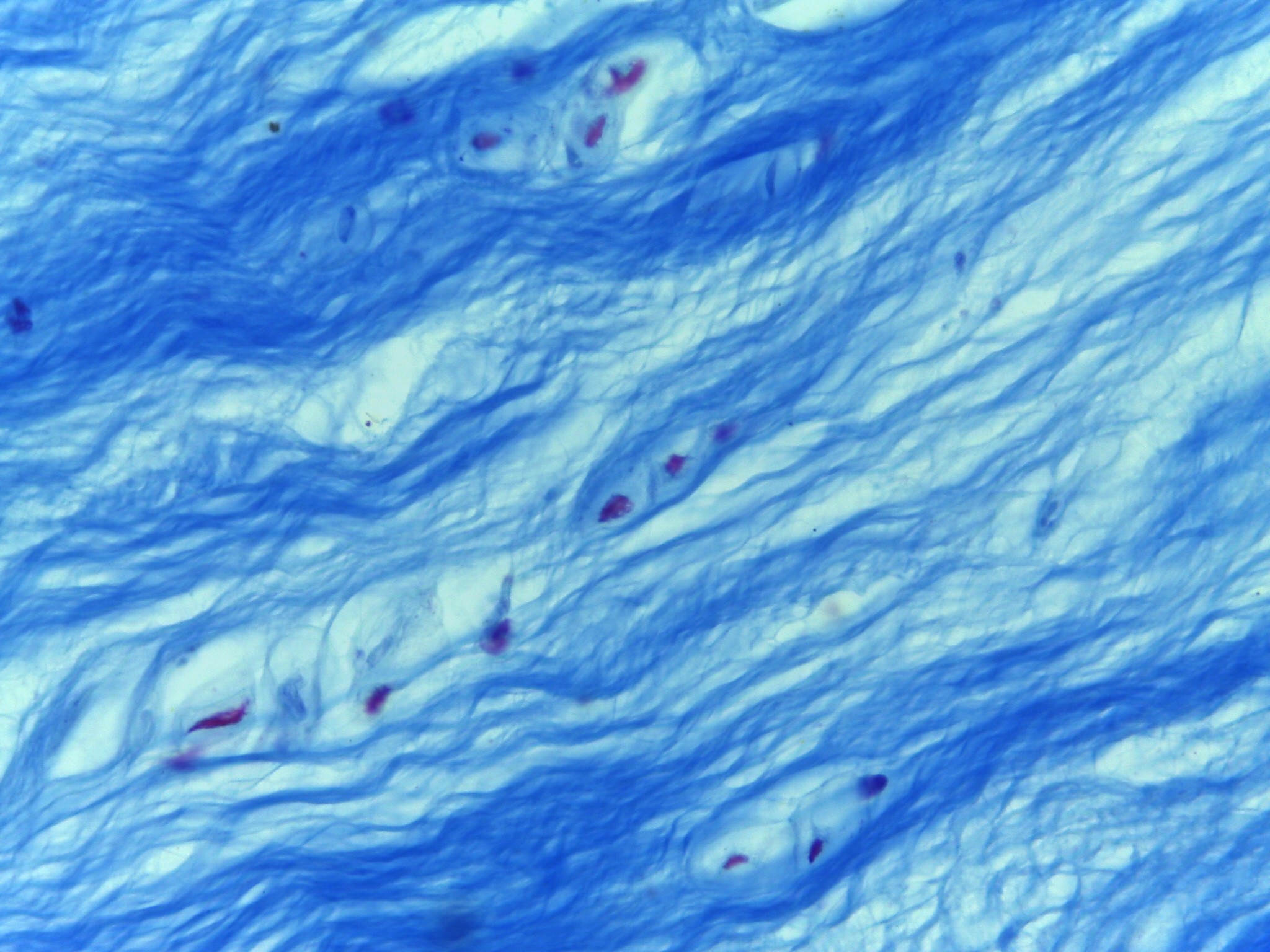
Fibrocartilage connective tissue
Intermediate magnification
Fibrocartilage: strong, built to withstand compression; well suited for menisci of knees, intervertebral joints, symphysis pubis.
Blue fibers: collagen fibers; characteristic of fibrocartilage
Red spots: chondrocytes within their lacunae, same ultrastructure as discussed in hyaline cartilage
-
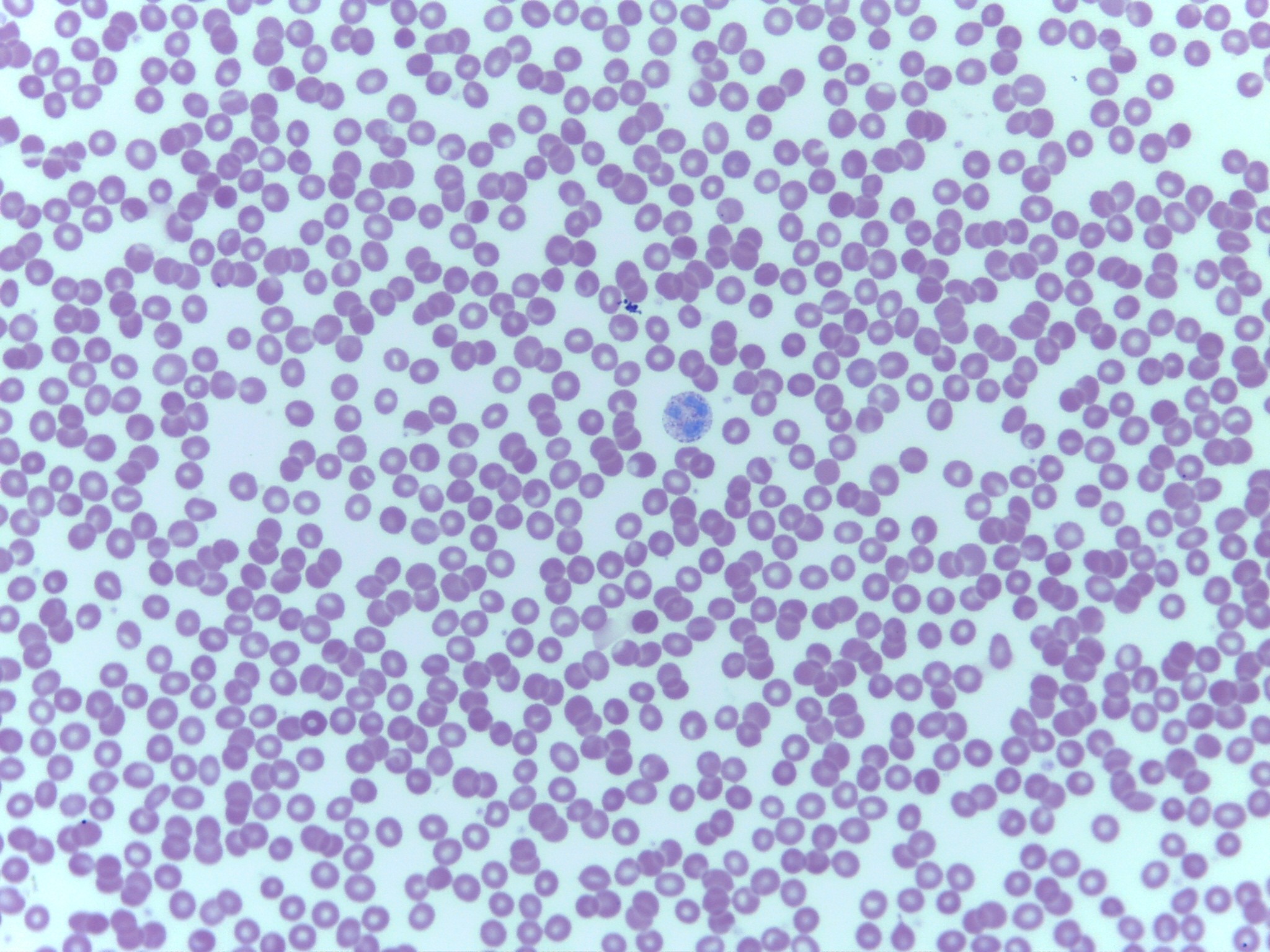
Blood connective tissue– AKA whole blood
Shows two of three basic types of blood cells: erythrocytes and leukocytes; thrombocytes not seen
Most cells erythrocytes: comprise 94% of blood cells
One large cell in center is a leukocyte, specifically a neutrophil
There are few leukocytes seen because they only make up 0.14% of blood cells.
Some erythrocytes are lighter in center and presents like a nucleus
Blood: about 45% cells (formed elements) and 55% plasma
Erythrocytes (RBC): 94% of formed elements
Function: carry oxygen
Mature blood cells: anucleated and packed with hemoglobin
Hemoglobin: protein that binds oxygen
-
Lung alveoli function
diffusion of gasses (simple squamous et)
-
bowman's capsule function
filtration (simple squamous et)
-
glomerulus function
diffusion (simple squamous et)
-
endothelium function
line blood vessels to provide smooth surface (simple squamous et)
-
mesothelium function
cover organs, support (simple squamous et)
-
capillaries function
diffusion of gasses (simple squamous et)
-
kidney tubules function
selective reabsorption (simple cuboidal et)
-
ducts of salivary glands function
secretion (simple cuboidal et)
-
ducts of pancreas
secretion (simple cuboidal et)
-
follicles of thyroid gland function
produce hormones:
thyroxine (t3, t4) - increase metabolic rate.
calcitonin-inhibit osteoclasts, stop decrease in bone mass
parathyroid hrmone (pth)- stimulates osteoclasts, increase bone Ca, decrease bone mass
-
Simple columnar et function
Lines the digestive tract. Forms the mucosa lining of the villi in the small intestine. Contains goblet cells which secrete mucin. Mucin and water combine to form mucous. Mucous is protective and lubricating. The function is absorption of nutrients.
-
Keratinized Stratified Squamous ET function
Epidermis of skin. Functions are strength and waterproofing
-
Non-keratinized Stratified Squamous ET function
Lines oral cavity, nasal cavity, pharynx, esophagus, vagina, anal canal. Functions are to protect against abrasion and maintain moisture.
-
Stratified Columnar ET function
(AKA stratified cuboidal) ducts of sweat glands and mammary glands. The function is to provide structural support.
parts of the epiglottis, pharynx, anus, urethra, and excretory ducts function is to provide protection.
-
Simple Ciliated Columnar ET function
Lines uterine tubes (fallopian tubes) function is to transport material through lumen.
-
Pseudostratified Ciliated Columnar ET function
Lines trachea and bronchi. Function is to remove foreign material and bacteria and form lower respiratory tract.
-
Transitional ET function
Lines ureters and urinary bladder. Function is distension.
-
Glandular ET function
pancreas functions in two different systems: endocrine and digestive
-
Islets of Langerhans
(endocrine system cells)
-
Alpha Cells
secrete glucagon in response to LOW blood sugar.
Glucagon stimulates hydrolysis of glycogen. (glycogenolysis).
Glucagon stimulates hydrolysis of fat (liposis) WHEN glycogen stores are low. (fasting or prolonged exercise)
-
Beta Cells
secrete insulin in response to HIGH blood sugar.
Insulin stimulates uptake of glucose.
Glucose may be oxidized for ATP or may be used to synthesize glycogen (glycogenesis).
-
Pancreas digestive system function
acinar cells produce pancreatic enzymes.
These enzymes travel through pancreatic duct to the duodenum of the small intestine.
-
Fibroblast
produce collagen and elastic fibers
-
Reticulocyte or Reticuloblast
Produce reticular fibers
-
Chondrocyte
cartilage cell
-
Osteocyte
Bone cell
-
Adipocyte
fat cell
-
Mast Cell
produces heparin and histamine
-
Monocyte
Phagocytic WBC in the vasculature
-
Macrophage
A monocyte that is in the interstitial space
-
Plasma cell
produces antibodies
-
Collagen
strong, not flexible

