
Haemostasis (Pathology)
Aims: To show how the haemostatic system acts in defence and wound healing and how defensive activation of the haemostatic system can cause tissue damage. Topics covered: Haemostatic response to injury. Defence of the circulating blood volume. Major components involved in in haemostasis. Blood coagulation. Physiological limitation of blood coagulation. Thrombosis. Coagulation tests. The student should be able to: Describe the haemostatic response to injury. Describe the major components involved in the haemostatic system. Explain how the clot participates in wound healing. Describe a mechanism by which the body regulates haemostasis Think of a plausible answer as to why is our haemostatic pathway so complicated. Clots cause much illness and death - what evolutionary advantage can there be in having such a dangerous system?
-
What is Haemostasis?
Haemostasis is a process whereby haemorrhage(bleeding) following vascular injury is arrested
-
Normal haemostatic response to injury depends onwhat? (3)
Normal haemostatic response to injury depends onclosely linked interaction between:
blood vessel wall, circulating platelets coagulation factors
-
FILL IN THE BLANKS:
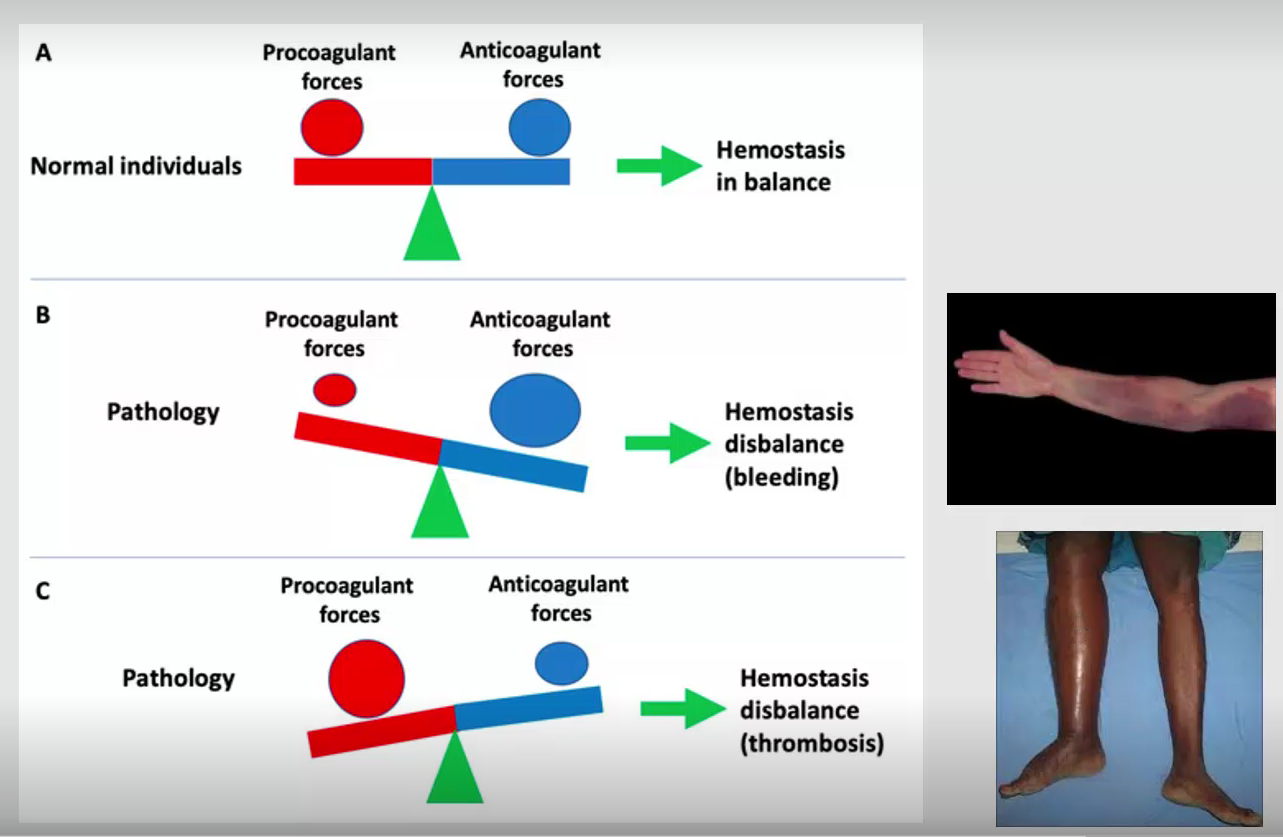
Response needs to be tightly controlled
-To prevent extensive clots developing-To be able to break down such clots once damage is repaired-Thus, there should be a balance between procoagulants and anticoagulants mechanisms
-
What are the Five major components involved in haemostatic system?
-Blood vessels and endothelial cells.-Platelets-Coagulation factors-Coagulation inhibitors-Fibrinolysis
-
The intact blood vessel wall prevents haemostasis.....what do the endothelial cells produce? (3)
-Prostacyclin: - this causes vasodilation and inhibits plateletaggregation (when platelets clump together to form blood clots)
-Antithrombin & Protein C activator: - both inhibit coagulation
-Tissue plasminogen activator: activates fibrinolysis (refers to the normal breakdown of clots)
-
The mechanism of haemostasis can be divided into 4 stages; what are these stages?
1. Constriction of the blood vessel.
2. Formation of a temporary “platelet plug."
3. Activation of the coagulation cascade.
4. Formation of “fibrin plug” or the final clot
-
What does the blood vessel wall do immediately after an injury?
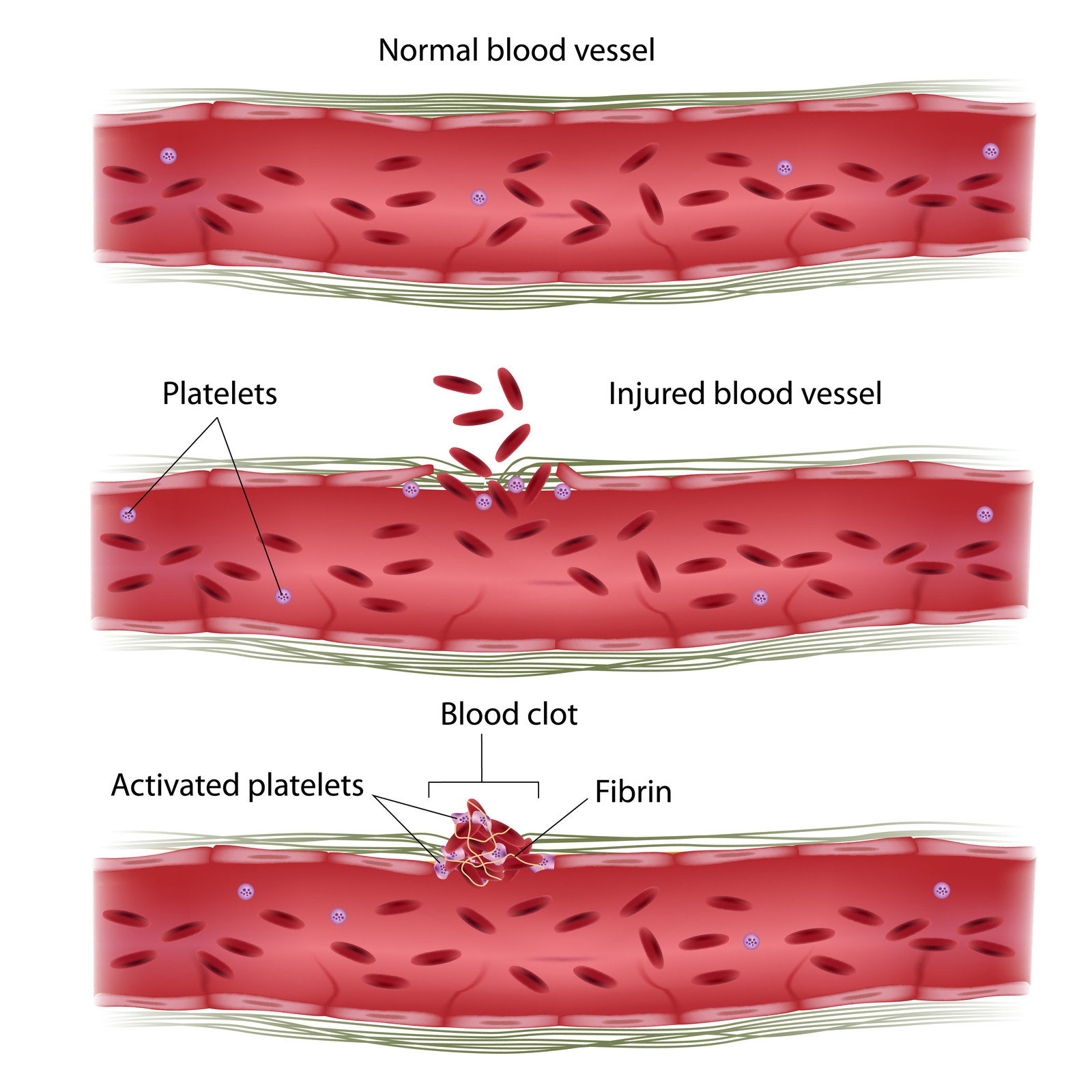
The vessel wall will vasoconstrict (spasm) immediately after, to slow the blood flow to the area of injury (avoids excess blood loss)
+Reduced blood flow allows contact activation of platelets and coagulation factors
-
Thrombin converts fibrinogen into what?
Fibrin
-
What are platelets
They are small disc-shaped with large surface area toabsorb coagulation factors
-
Platelets have membrane receptor agonists such as:
-GPIa/IIb complex & GPVI which are receptors for collagen.
-Glycoproteins (GPIb & IIb/IIIa) allows attachment of plateletsto von Willebrand Factor (vWF), then to endothelium.
-
FILL IN THE BLANKS:
Platelet plug formation
1)Following an injury, subendothelial collagen is__________.
2)__________ is released, causing the platelets to change formand __________to the subendothelial collagen.
3)After platelet adhesion, the subendothelial collagenbinds to __________ on the platelet, which activates theplatelets.
4)Activated platelet releases a number of important__________ and chemical mediators from its __________.
+these include ADP, vWF, thromboxane A2, serotonin andcoagulation factors
Platelet plug formation
1)Following an injury, subendothelial collagen isexposed.
2)vWF is released, causing the platelets to change formand adhere to the subendothelial collagen.
3)After platelet adhesion, the subendothelial collagenbinds to receptors on the platelet, which activates theplatelets.
4)Activated platelet releases a number of importantcytokines and chemical mediators from its granules.
+these include ADP, vWF, thromboxane A2, serotonin andcoagulation factors
-
What does ADP do?
Promotes platelet aggregation to form primary haemostatic plug
-
What does Thromboxane (A2) do?
Also potentiates aggregation
-
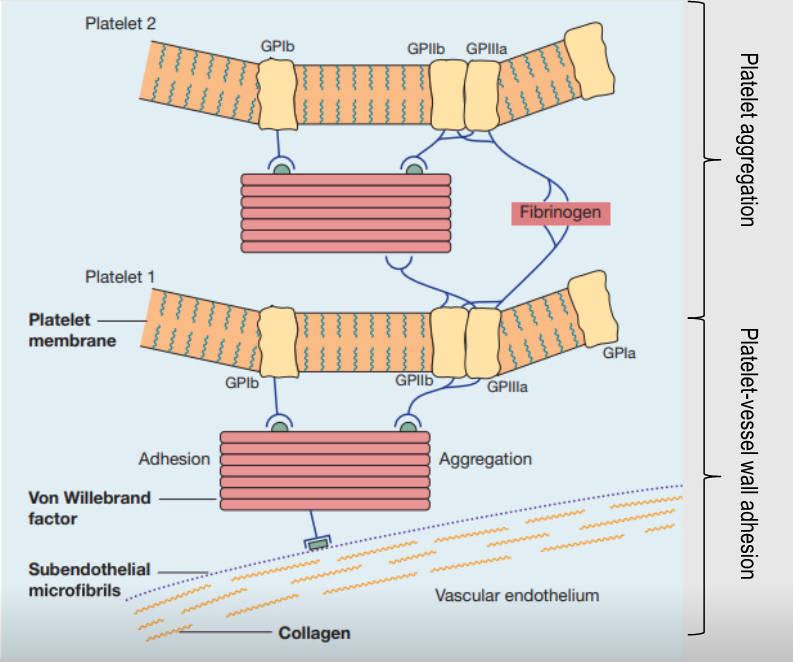
Outline the five steps when it comes to primary haemostatic plug formation
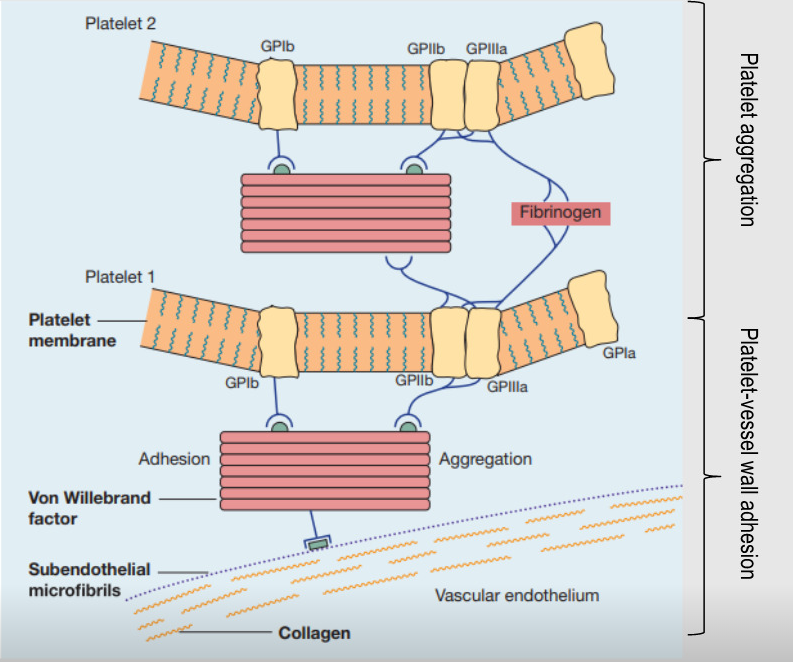
1)Immobilization of platelets at site of injury requiring platelet-vessel wall adhesion.
2)vWF derived from endothelial cells connects platelet tosubendothelial through GPIb receptor.
3)additional platelets from the circulating blood are drawn to the area of injury
4)continuous platelet aggregation promotes the growth of thehaemostatic plug, which soon covers the exposed connectivetissue
5)unstable primary haemostatic plug temporarily controls bleeding
-
Proteins for coagulation cascade are .....?
Proenzymes (serine proteases) and pro factors
-
The coagulation cascade is divided on the basis of what?
Lab test-into intrinsic, extrinsic and common pathways
-
Coagulation begins when...?
When the tissue factor activated on the surface of injured cells binds and activates factor VII
-
How do activated platelets accelerate the coagulation process?
By providing Membrane phospholipid; membrane phospholipid converts factor X to Xa and prothrombin to thrombin
-
What 3 steps does the tissue factor (TF) initiate?
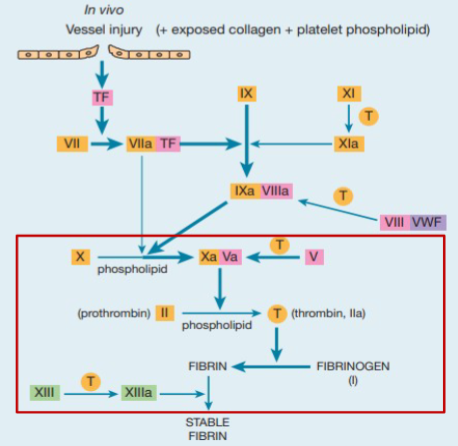
1)When FVII in plasma come in contact to form TF-Vlla
2)TF-Vlla complex activates X and IX
3)Convert soluble fibrinogen into a meshwork of insoluble fibrin
+Tightly regulated; orchestration of coagulation factors, cofactors and inhibitors leads to controlled formation of thrombin then fibrin formation
-
If not checked, blood coagulation could lead to... what?
dangerous occlusion (blockage) of blood vessels (thrombosis)
-
Coagulation is modulated by 3 major inhibitory systems of inactivation of thrombin; what are these 3 systems, and what do they do?
1)Anti-thrombin - an important inhibitor of terminal proteins of cascade, especially FXa and thrombin (Heparin potentiates its action markedly)
2)Protein C and S.- Protein C is vit K-dependent is able to destroy activators factors V and VIII, to prevent thrombin formation.
+Protein S, also vit K-dependent acts as cofactor for C.
3)Tissue Factor pathway inhibitor (TFPI) - inhibits factor Xa and VIIa and TF
-
STATEMENT:Fibrinolysis is the normal haemostatic response to subcellular injury, it is the enzymatic break-down of blood clots
Is this true
FALSE
It is the normal response to vascular injury
-
Fibrin is degraded by what?
Plasmin
-
What are the 2 main general functions of fibrinolysis?
1)Clot limiting mechanism
2)Repair and healing mechanism
-
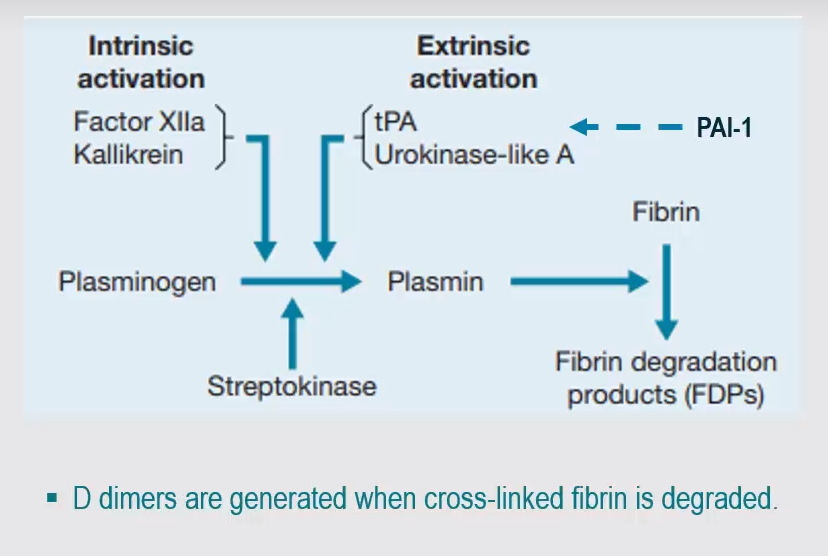
What are the 3 (technically 6) key players of fibrinolysis?
1)Plasminogen
2)Tissue plasminogen activator (t-PA) and urokinase (u-PA)
3)Plasminogen activator inhibitor -1 and -2 (PAI)
-
Activated protein C stimulates fibrinolysis how?
By destroying plasma inhibitors of tPA
-
Picture outlining fibrinolysis (Clot lysis)
-
Picture outlining the importance of haemostatic balance
-
Defective haemostasis with abnormal bleeding may result from what? (3)
-A vascular disorder-Thrombocytopenia or a disorder of platelet function-Defective blood coagulation
-
Simple tests are employed to assess... what?
-Simple tests are employed to assess the platelet, vessel wall and coagulationcomponents of haemostasis
+e.g. Blood count and blood film examination, screening tests of blood coagulation,individual coagulation factor assays, assay of von Willebrand factor
-
FILL IN THE BLANKS:
Clot in wound healing
-Platelets are key to initiating wound healing;
+They stop bleeding with ________ _________ ________ _______
+this followed by _________ ___ ______ ___________ _________ _____
1)_______ _______ _______ _______ blood vessels open up to allow oxygen and nutrients to the site.2)_______ later invade the clot and _______ _______ _______, including _______, to form a structural framework for new tissue.3)Platelets can also form a _______ _______ _______ in their surroundings, in thelater stages of wound healing
Clot in wound healing
-Platelets are key to initiating wound healing;
+They stop bleeding with primary haemostatic plug formation
+this followed by coagulation to form secondary haemostatic plug.
1)When bleeding has stop, blood vessels open up to allow oxygen and nutrients to the site.
2)Fibroblasts later invade the clot and produce vital proteins, including fibronectin, to form a structural framework for new tissue.
3)Platelets can also form a provisional fibronectin matrix in their surroundings, in the later stages of wound healing.
-
There were strong selective pressures on what genes coding for how many factors during vertebrate evolution?
A strong of selective pressures on the 14 genes coding for the 11 factors during vertebrate evolution
-
Positive selection was identified for fibrinogen (FG), FIII, FVIII, FIX, and FX in the mammalian Primates, reptiles and birds. This shows what?
This showed that the coagulation system in vertebrates was under strong selective pressures, toadapt against blood-invading pathogens.
+Positive selection, is less likely to be associated with disease-causing mutations.
-negative selection were more likely to be associated with disease-causing mutations and be destabilizing.
-
A summary:
The haemostatic system represents a delicate balancebetween procoagulant and anticoagulant.
-five major components involved:Platelets,Blood vesselsCoagulation factors,Coagulation inhibitors,Fibrinolytic factors
-Platelets have surface glycoproteins to facilitate direct adherence to subendothelial tissues, vWF.
-Blood coagulation in response to vascular injury commences with TF binding to FVII to initiate cascade
-Clotting is a critical defence mechanism to protect integrity ofthe vascular system after injury.
-Coagulation factor inhibitors include antithrombin, protein C and protein S.
-Dissolution of fibrin clots (fibrinolysis) occurs by activation of plasminogen to plasmin

