Fertilisation and the Luteal Phase (Physiology 2)
Fertilisation and the luteal phase - Dr David Gillott Session introduction Human fertilisation is arguably the most beautiful event in biology. This lecture examines some of the events that take place just prior to fertilisation, at the moment of fertilisation and during early embryo development. These events take place during the luteal phase of the menstrual cycle which is reviewed. Learning Outcomes At the end of this session, you will be able to: Describe the sperm capacitation and acrosome reaction Understand the physiological changes in the luteal phase of the menstrual cycle Explain the role of the corpus luteum in pregnancy or menstruation Review rescue of the corpus luteum by hCG Describe the structure of the oocyte Describe the molecular events during fertilisation Explain syngamy and early embryo development Session resources Powerpoint slides: Fertilisation and Luteal Phase 2024-25 Dr David Gillott.pptxDownload Fertilisation and Luteal Phase 2024-25 Dr David Gillott.pptx Panopto recording: Some questions to think about... 1. Describe the acrosome reaction and its role in fertilization. 2. Which two important events are triggered by the rise in LH at the end of the follicular phase? 3. What triggers the completion of meiosis II in the oocyte? 4. How does the oocyte prevent polyspermy after a sperm successfully fuses with the egg? 5. What role does human chorionic gonadotropin (hCG) play in rescuing the corpus luteum, and why is this essential for early pregnancy? 6. Outline the roles of the inner cell mass and the trophectoderm in the blastocyst. How does each contribute to early development? 7. What are the key changes in the endometrium during the luteal phase that prepare it for potential implantation? Optional resources Okabe M (2018) Sperm-egg interaction & fertilization - past, present & future.pdfDownload Okabe M (2018) Sperm-egg interaction & fertilization - past, present & future.pdf Glossary Capacitation – molecular changes in sperm to enable the acrosome reaction Acrosome reaction – Reaction in sperm as approaching the egg releasing enzymes Luteal phase – latter phase of the menstrual cycle after ovulation Corpus luteum – a hormone-secreting structure that develops from a follicle after ovulation Cortical reaction – release of cortical granules from the egg at fertilisation, preventing polyspermy Syngamy – the fusion of two cells, or of their nuclei, in reproduction Pronuclei – gametic nucleus after meiosis but before fusion that forms of the nucleus of the zygote Blastocyst – 5 day old embryo with fluid filled cavity
-
What is capacitation, and why is it important? (1)
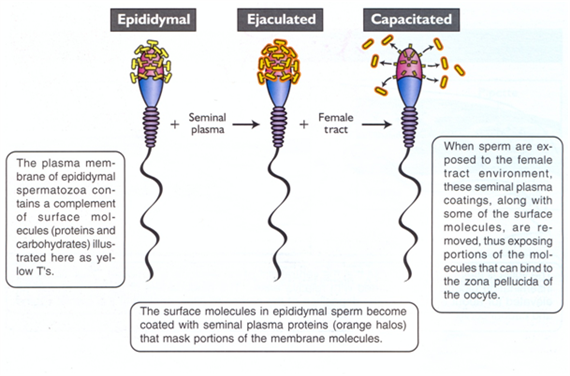
Capacitation refers to molecular changes in sperm that enable the acrosome reaction, preparing the sperm for fertilization.
-
What is the acrosome reaction? (1)
The acrosome reaction is a process in sperm where enzymes are released as it approaches the egg, aiding in penetration.
-
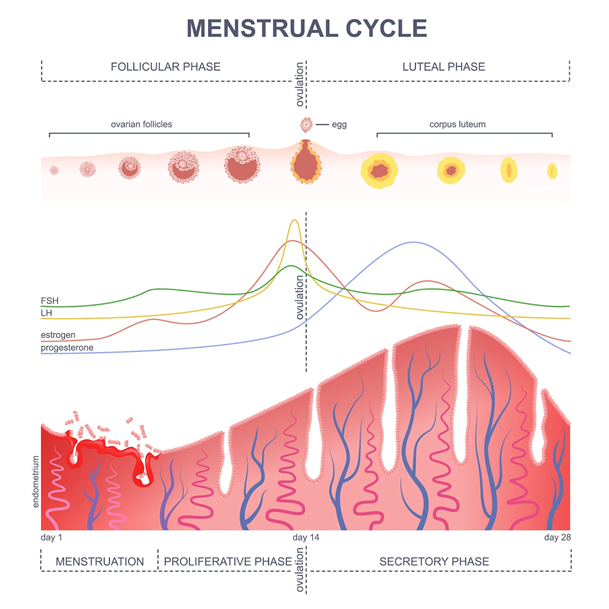
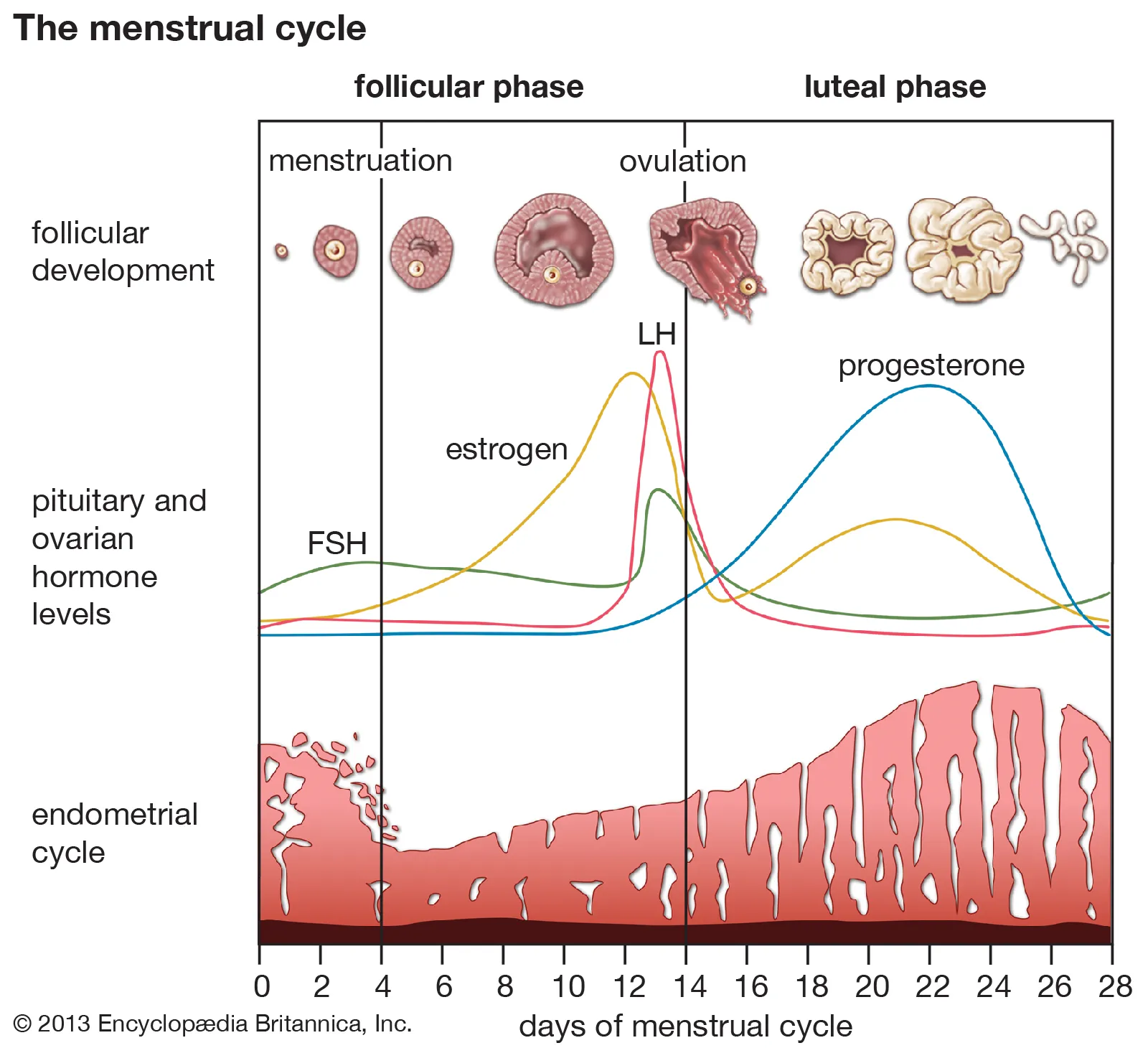
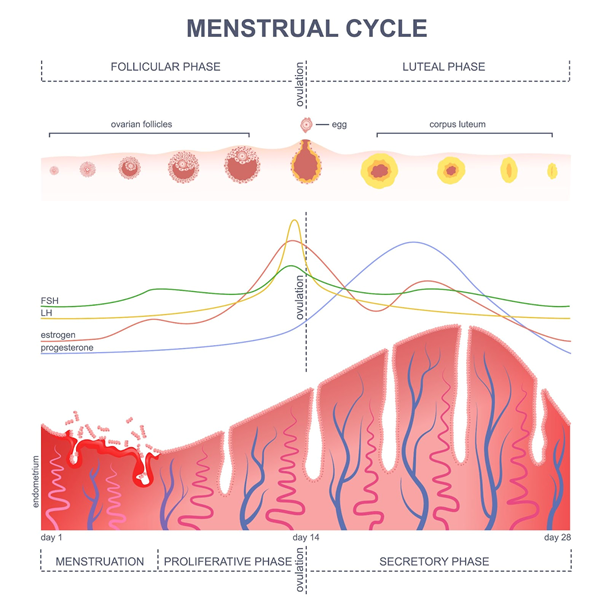
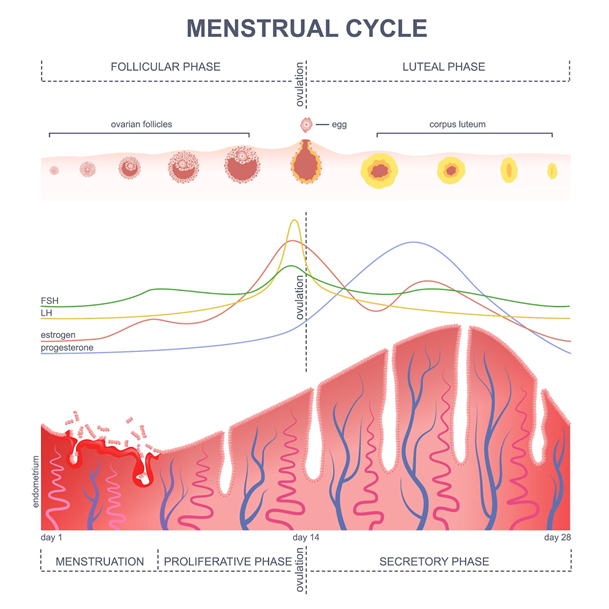
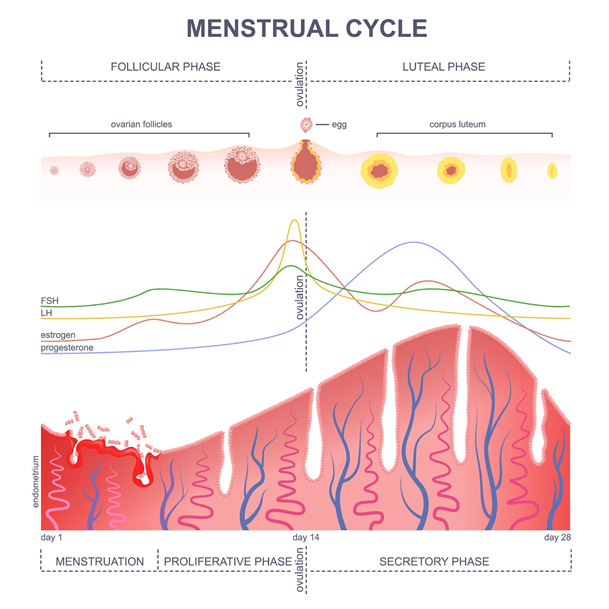
What is the luteal phase? (1)
The luteal phase is the latter phase of the menstrual cycle after ovulation, dominated by progesterone production.
-
What is the corpus luteum? (1)
The corpus luteum is a hormone-secreting structure that develops from a follicle after ovulation and produces progesterone.
-
What is the cortical reaction, and what does it prevent? (1)
The cortical reaction involves the release of cortical granules from the egg during fertilization, preventing polyspermy.
-
What is syngamy? (1)
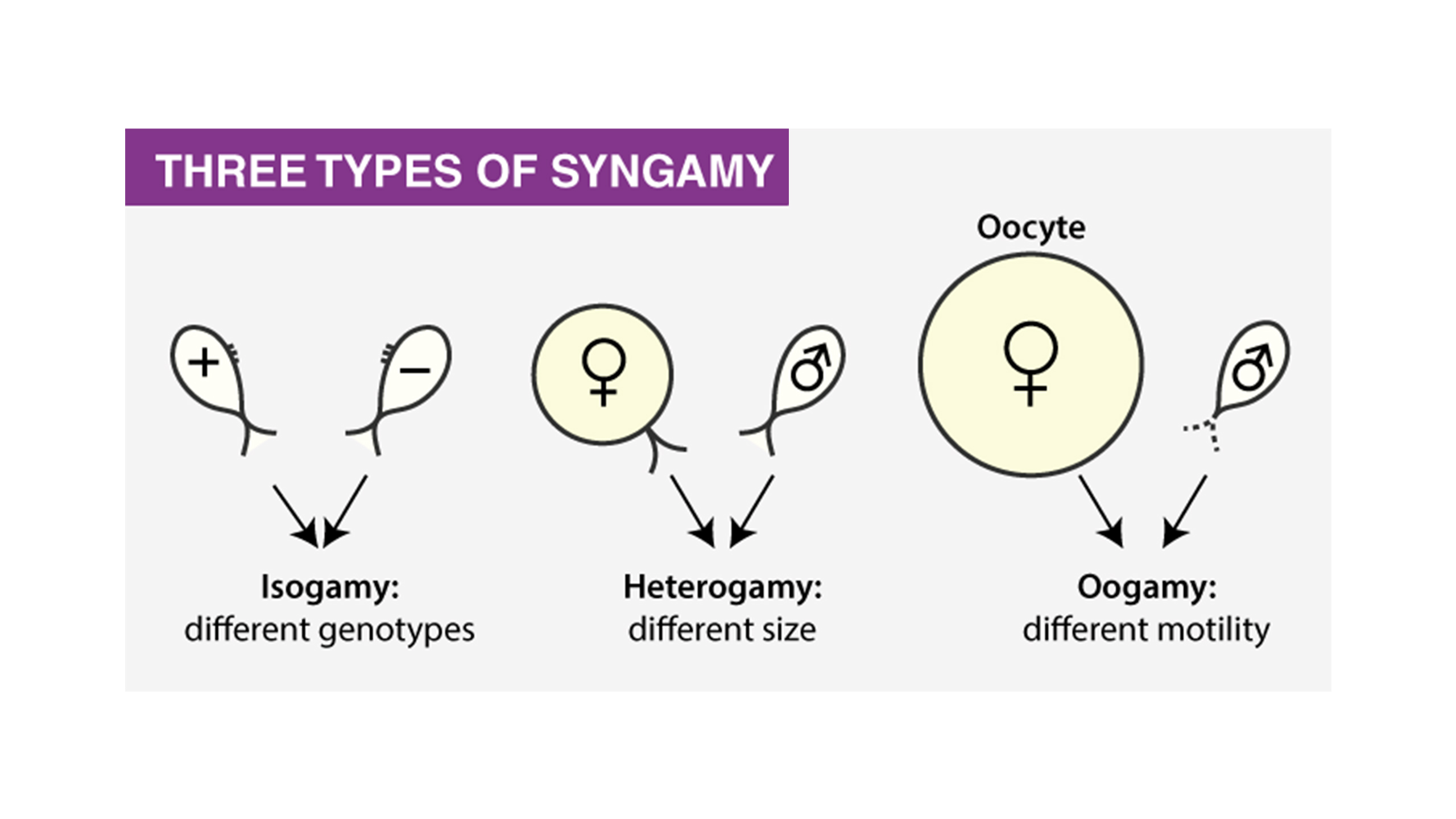
Syngamy is the fusion of two cells, or their nuclei, during reproduction, forming a zygote.
-
What are pronuclei? (1)
Pronuclei are gametic nuclei present after meiosis but before their fusion to form the nucleus of the zygote.
-
What is a blastocyst? (1)
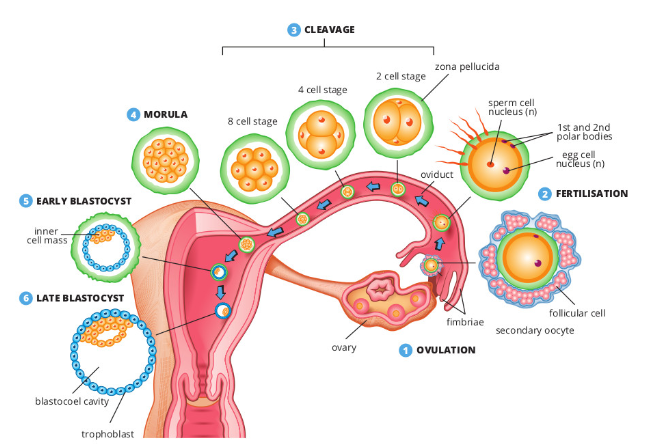
A blastocyst is a 5-day-old embryo with a fluid-filled cavity, essential for implantation and further development.
-
What happens to semen after ejaculation, and why does it coagulate? (3)
Coagulation: After ejaculation, semen coagulates due to proteins and enzymes secreted by the seminal vesicles.
Purpose: Coagulation helps to protect the sperm and allows the semen to stay in place near the cervix, increasing the chances of sperm entry into the reproductive tract.
Enzymes involved: Prostate-specific antigen (PSA), produced by the prostate gland, helps break down the coagulated semen, liquefying it within approximately 15 minutes.
-
What comprises seminal fluid, and how does it behave post-ejaculation? (3)
Composition: Seminal fluid consists of secretions from the prostate and seminal vesicles.
Initial Coagulation: Immediately after ejaculation, seminal fluid coagulates due to the proteins and enzymes it contains, like fibrinogen from the seminal vesicles.
Liquefaction: Around 15 minutes later, the prostate gland’s PSA breaks down the coagulated semen, turning it into a liquid that allows sperm to move.
-
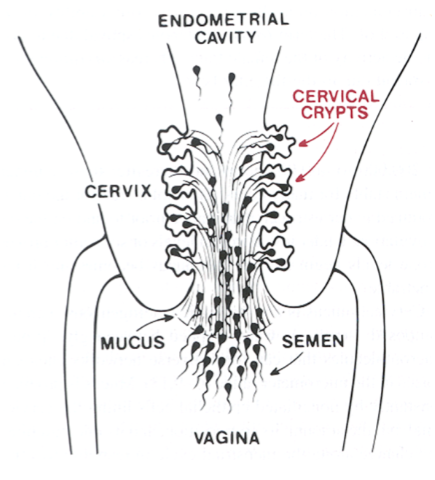
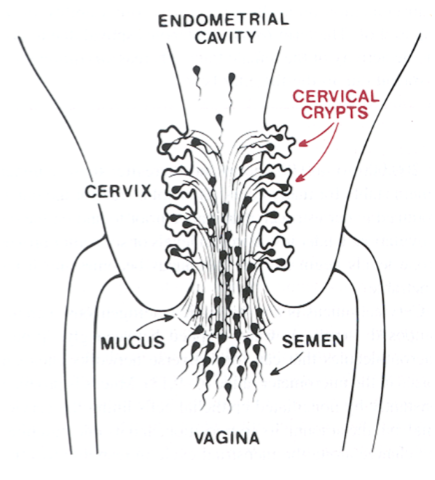
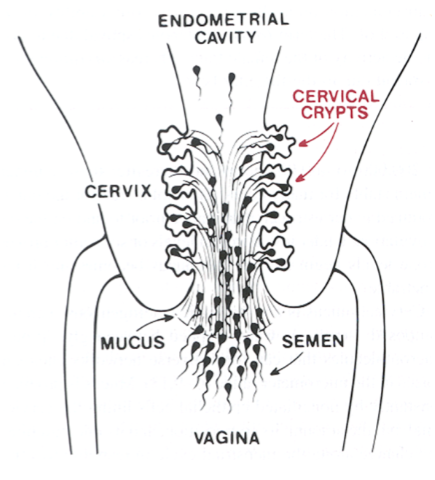
What happens to sperm as they move through cervical mucus? (3)
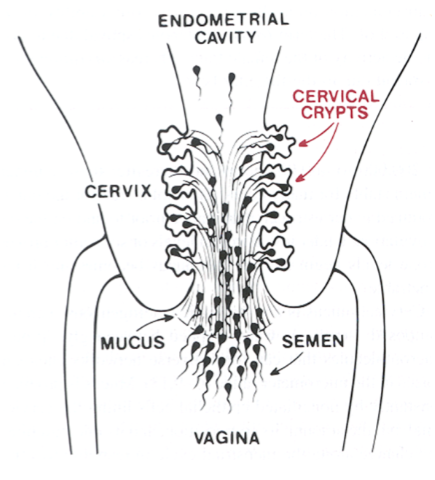
Removal of debris: As sperm move through cervical mucus, they clear away seminal fluid, abnormally shaped sperm, and cellular debris.
Sperm Movement: Sperm swim through the cervical mucus, which can either assist or hinder their progress depending on the mucus’s consistency.
Cervical Mucus Changes: Under the influence of estrogen (and the absence of progesterone), cervical mucus becomes less viscous, which allows sperm to pass through more easily.
-
What role does cervical mucus play in sperm movement? (3)
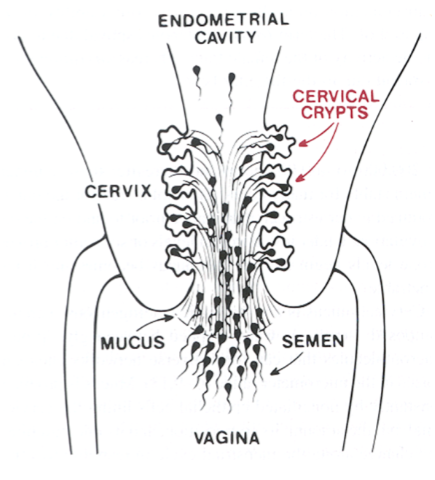
Estrogen Influence: Estrogen decreases the viscosity (thickness) of cervical mucus, making it easier for sperm to move through the cervix.
Reservoir Formation: Sperm can inhabit cervical crypts (small cavities within the cervix), which may act as a reservoir, allowing sperm to survive longer in the female reproductive tract.
Thermotaxis: Some evidence suggests sperm may use thermotaxis (movement towards temperature gradients) to navigate the reproductive tract, although the exact mechanism is not fully understood.
-
How long can sperm survive, and where does fertilization typically occur? (2)
Sperm Longevity: Sperm can survive in the female reproductive tract for up to 5 days, although fertilization typically occurs within 24-48 hours of ejaculation.
Fertilization Location: Fertilization typically occurs in the fallopian tube, where the sperm meets the egg.
-
What is known about sperm's journey through the uterus? (2)
Uterine Passage: The passage of sperm through the uterus is not fully understood.
Role of Cilia: It is believed that currents generated by cilia in the uterus and fallopian tubes may play a role in guiding the sperm toward the egg.
-
What role do chemo-attractants play in sperm movement? (2)
Chemo-attractants: Chemo-attractants released from the oocyte's cumulus complex attract sperm.
Effect: These attractants help guide sperm towards the egg for fertilization.
-

What happens to sperm as they approach the egg? (2)
Hyperactivation: Sperm become hyperactivated (they press q and pop their ults) as they approach the egg.
Increased Tail Movement: Hyperactivation results in more forceful tail beats with increased frequency and amplitude, mediated by calcium (Ca2+) influx through CatSper channels.
-
What is capacitation, and how does it occur? (3)
Definition: Capacitation is the biochemical process that enables sperm to fertilize an egg.
Factors Involved: It is partly achieved by removing the sperm from the seminal fluid. Additionally, uterine or tubal fluid may contain factors that promote capacitation.
Biochemical Changes: Capacitation involves the rearrangement of surface glycoproteins and changes in the membrane composition of the sperm, preparing it for the acrosome reaction.
-
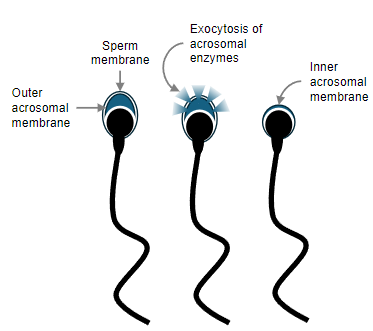
What are the key changes in the sperm membrane during capacitation? (2)
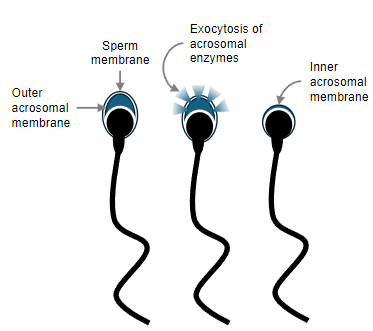
Outer Acrosomal Membrane: The outer acrosomal membrane undergoes biochemical changes.
Inner Acrosomal Membrane: The inner acrosomal membrane also undergoes modifications to prepare for the acrosome reaction, enabling enzyme release.
-
What happens during the acrosome reaction? (4)
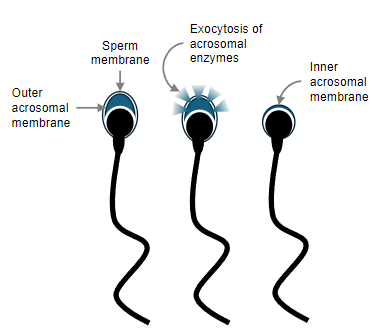
Contact with Zona Pellucida: The acrosome reaction occurs when sperm come into contact with the zona pellucida, a glycoprotein coat surrounding the oocyte.
Fusion of Membranes: The outer membrane of the acrosome fuses with the sperm's plasma membrane, creating pores.
Exocytosis of Enzymes: This fusion releases acrosomal enzymes that help the sperm penetrate the zona pellucida.
Action of Acrosin: Acrosin, bound to the inner acrosomal membrane, further digests the zona pellucida, allowing the sperm to enter the oocyte.
-
What triggers ovulation and how does it affect meiosis? (2)
LH Spike: The spike in Luteinizing Hormone (LH) triggers the resumption of meiosis.
Oocyte Conversion: This leads to the conversion of the primary oocyte into a secondary oocyte, along with the formation of the first polar body.
-

What happens to the follicle during ovulation? (2)
Basement Membrane Breakdown: The basement membrane of the follicle breaks down, causing blood to flow into the middle of the follicle.
Extrusion of Oocyte Cumulus Complex: The oocyte cumulus complex is extruded and caught by the fimbriae of the uterine tube (fallopian tube).
-
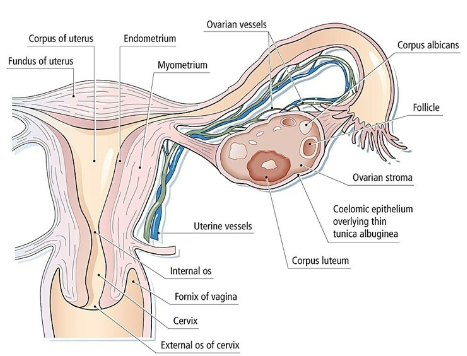
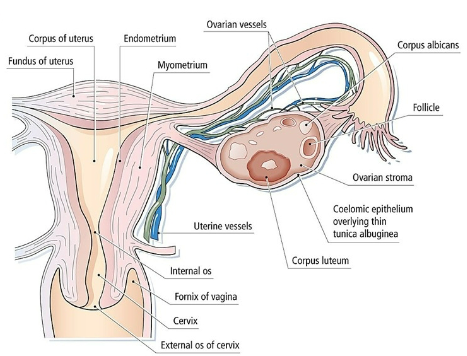
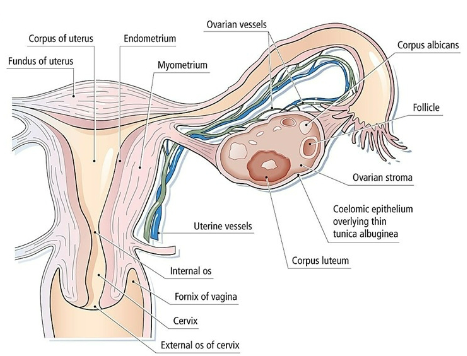
What is the corpus luteum and what does it produce? (2)
Formation of Corpus Luteum: After ovulation, the theca and granulosa cells mix, and the empty follicle transforms into the corpus luteum.
Progesterone Production: The corpus luteum produces progesterone during the luteal phase, preparing the endometrium for potential implantation.
-
What effect does progesterone have on the endometrium? (2)
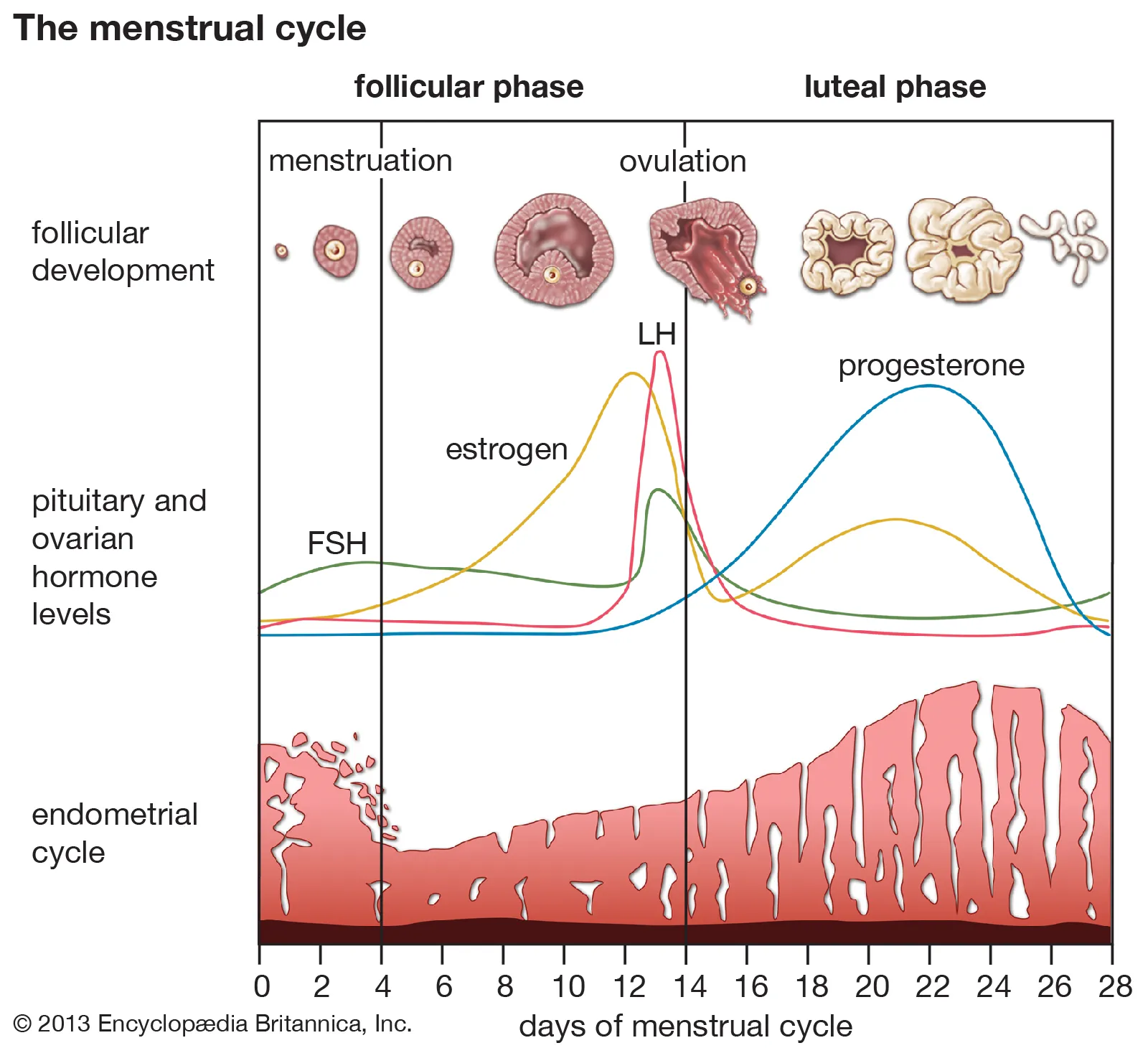
Endometrial Secretions: Progesterone makes the endometrium secretory and receptive to implantation, creating a suitable environment for a fertilized egg.
Cervical Mucus: Progesterone makes cervical mucus more viscous, preventing further sperm penetration after ovulation.
-
What effect does progesterone have on the uterine tubes? (1)
Cilia Suppression: Progesterone suppresses the cilia in the uterine tubes once the oocyte has passed through, preventing further movement of the oocyte.
-
What role does estrogen play in the menstrual cycle? (2)
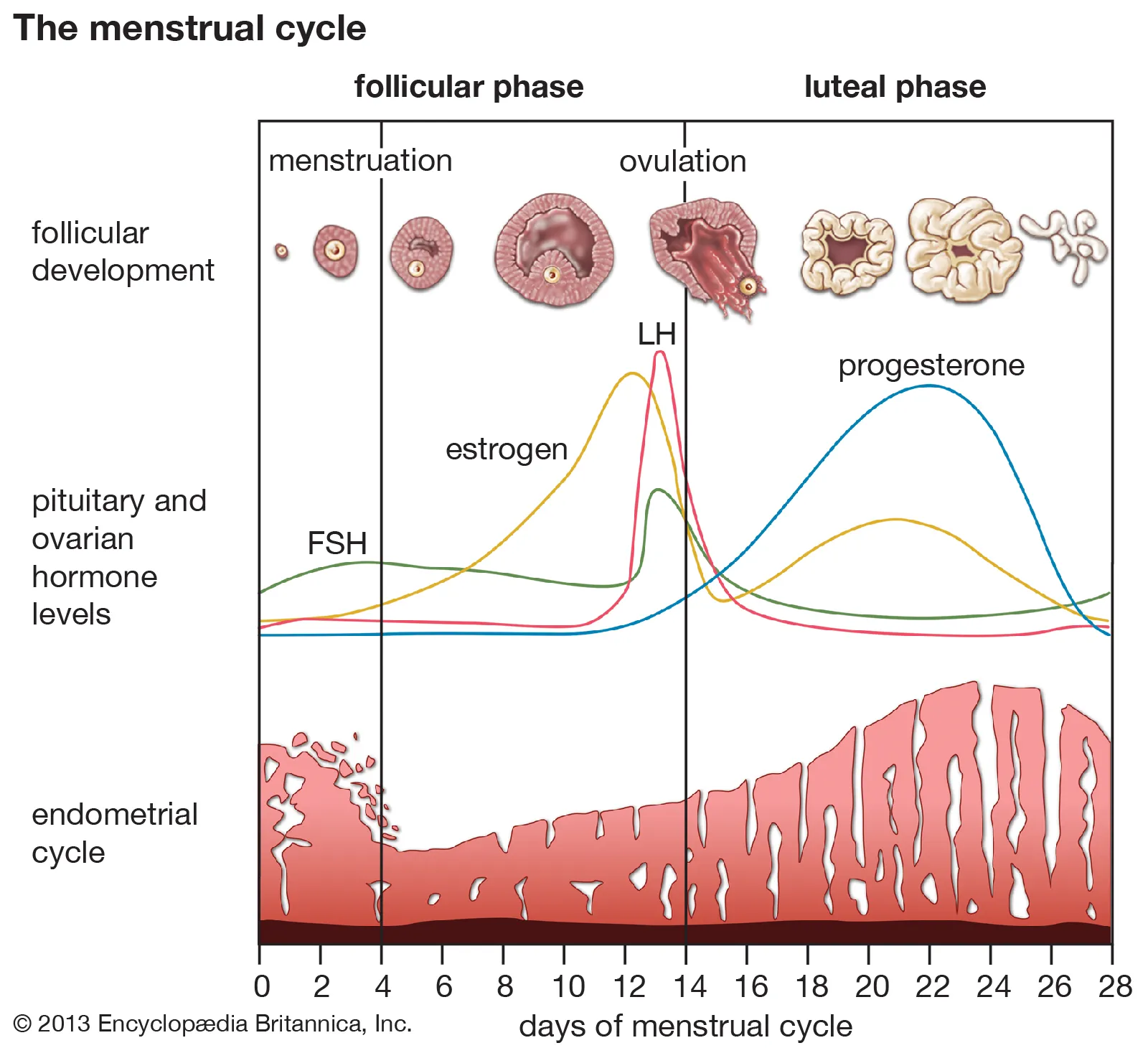
Endometrial Maintenance: Estrogen helps progesterone maintain the endometrium during the luteal phase by supporting its secretory functions.
Follicular Phase Role: During the follicular phase, estrogen promotes the proliferation of the endometrial lining to prepare for a potential pregnancy.
-
What effect does progesterone have on the endometrium? (2)
Endometrial Secretions: Progesterone makes the endometrium secretory and receptive to implantation, creating a suitable environment for a fertilized egg.
Cervical Mucus: Progesterone makes cervical mucus more viscous, preventing further sperm penetration after ovulation.
-
What effect does progesterone have on the uterine tubes? (1)
Cilia Suppression: Progesterone suppresses the cilia in the uterine tubes once the oocyte has passed through, preventing further movement of the oocyte.
-
What role does estrogen play in the menstrual cycle? (2)
Endometrial Maintenance: Estrogen helps progesterone maintain the endometrium during the luteal phase by supporting its secretory functions.
Follicular Phase Role: During the follicular phase, estrogen promotes the proliferation of the endometrial lining to prepare for a potential pregnancy.
-
What does the menstrual cycle achieve? (5)
Menstrual cycle achieves...
-Selection of a single follicle and oocyte.
-Regular spontaneous ovulation.
-Correct haploid number of chromosomes in the oocyte by completing meiosis I and beginning meiosis II.
-Cyclical changes in the cervix and uterine tubes, to enable egg transport and sperm access.
-Preparation of the endometrium of the uterus to receive the fertilised egg.
-Support of the implanting embryo and endometrium by corpus luteum progesterone.
-Initiating a new cycle if fertilisation does not occur.
-
What is the purpose of selecting a single follicle and oocyte during the menstrual cycle? (1)
Selection of Single Follicle and Oocyte: The menstrual cycle ensures that only one follicle and its oocyte are selected to mature and be ovulated, optimizing the chances of successful fertilization.
-
What does regular spontaneous ovulation ensure during the menstrual cycle? (1)
Regular spontaneous ovulation ensures that a mature oocyte is naturally released at the appropriate time in the cycle, optimizing the chances for fertilization and pregnancy.
-
How does the menstrual cycle ensure the correct chromosome number in the oocyte? (2)
Completion of Meiosis I: The menstrual cycle ensures that the oocyte completes meiosis I, resulting in the correct haploid number of chromosomes.
Initiation of Meiosis II: The cycle also ensures that meiosis II is initiated in the oocyte, preparing it for fertilization.
-
What cyclical changes occur in the cervix and uterine tubes during the menstrual cycle? (4)
Cervical Mucus Changes:
During the follicular phase, particularly around ovulation, cervical mucus becomes less viscous (thinner and more stretchy) to facilitate sperm passage.
During the luteal phase, cervical mucus becomes more viscous (thicker) to form a barrier that blocks sperm and protects against infections.
Uterine Tube Changes:
During the follicular phase, increased ciliary activity and muscular contractions in the uterine tubes facilitate egg transport and sperm movement.
During the luteal phase, progesterone suppresses ciliary activity after the oocyte has been transported.
-
How does the menstrual cycle prepare the endometrium? (1)
Endometrial Preparation: The menstrual cycle prepares the endometrium of the uterus to receive and support a fertilized egg, creating an optimal environment for implantation.
-
What role does the corpus luteum play in supporting the embryo? (2)
Progesterone Production: After ovulation, the corpus luteum produces progesterone, which supports the endometrium and prepares it for implantation.
Embryo Support: The progesterone from the corpus luteum also supports the implanting embryo, maintaining the uterine environment until the placenta can take over.
-
What happens if fertilization does not occur at the end of the menstrual cycle? (1)
Cycle Reset: If fertilization does not occur, the corpus luteum regresses, progesterone levels drop, and a new menstrual cycle is initiated.
-
What is the function of the cumulus oophorus at ovulation? (1)
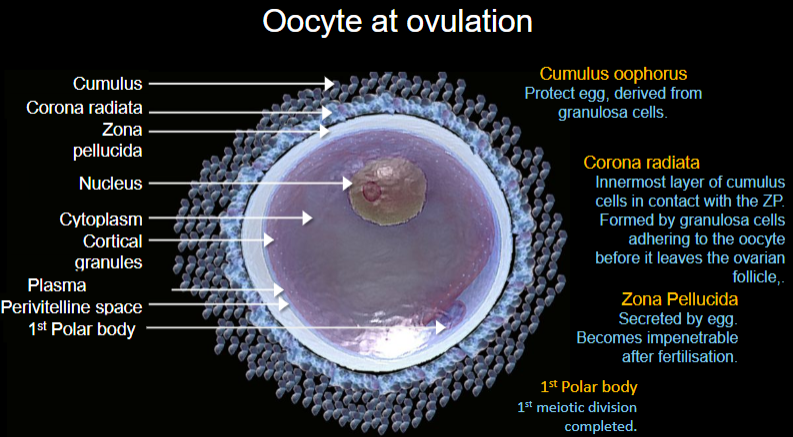
Cumulus Oophorus: The cumulus oophorus, derived from granulosa cells, serves to protect the egg and plays a role in its release during ovulation.
-
What is the corona radiata, and where is it located? (2)
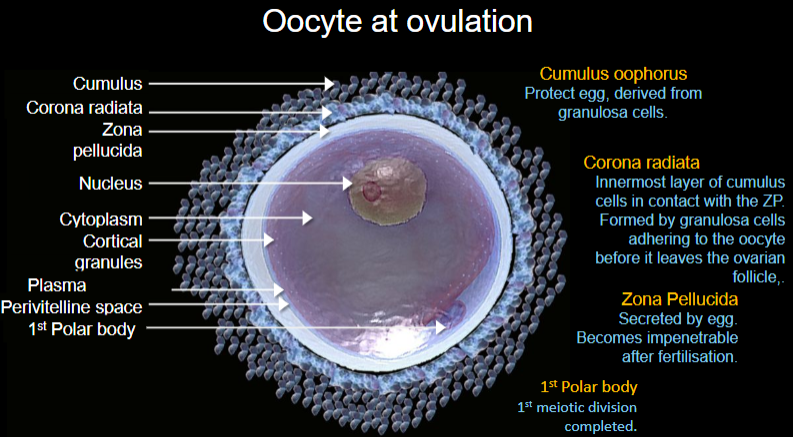
Corona Radiata: The corona radiata is the innermost layer of cumulus cells in contact with the zona pellucida (ZP).
Formation: It is formed by granulosa cells adhering to the oocyte before it leaves the ovarian follicle.
-
What is the role of the zona pellucida during fertilization? (2)
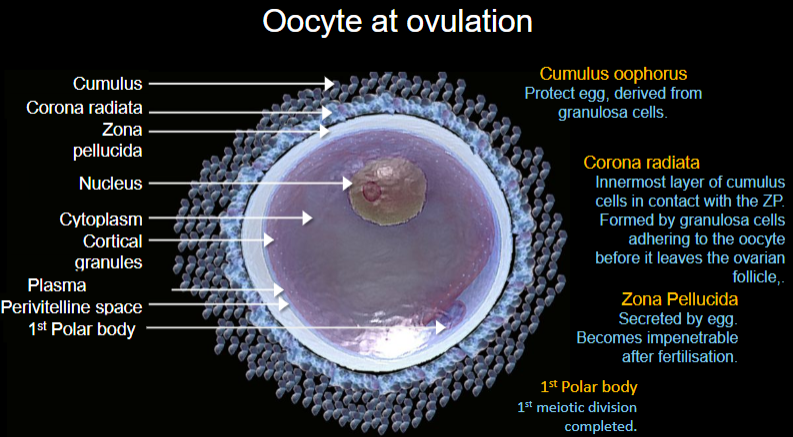
Zona Pellucida: The zona pellucida is a glycoprotein layer secreted by the egg.
Post-fertilization: It becomes impenetrable after fertilization, preventing polyspermy and ensuring that only one sperm fertilizes the egg.
-
What happens to the first polar body during ovulation? (1)
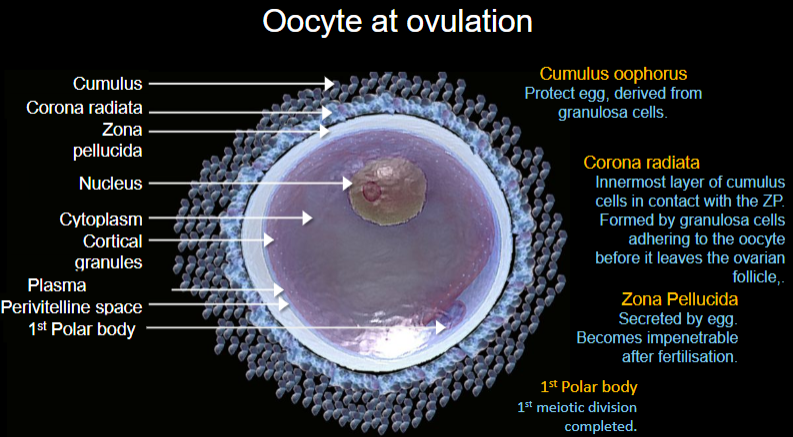
First Polar Body: The first polar body is formed as a result of the completion of the first meiotic division in the oocyte, containing half the chromosomes of the egg.
-
What happens as sperm approaches the cumulus complex during fertilization? (2)
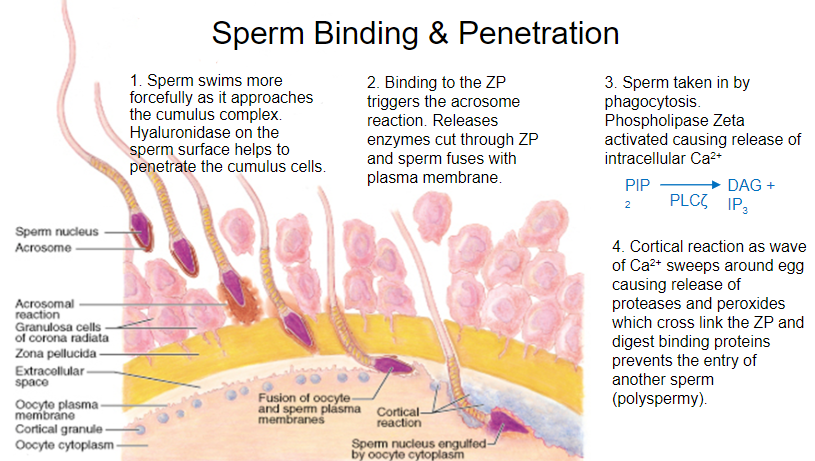
Sperm Movement: As sperm approaches the cumulus complex, it swims more forcefully.
Hyaluronidase: The sperm surface releases hyaluronidase, which helps penetrate the cumulus cells, allowing sperm to move closer to the egg.
-
How is sperm taken in by the egg during fertilization? (1)
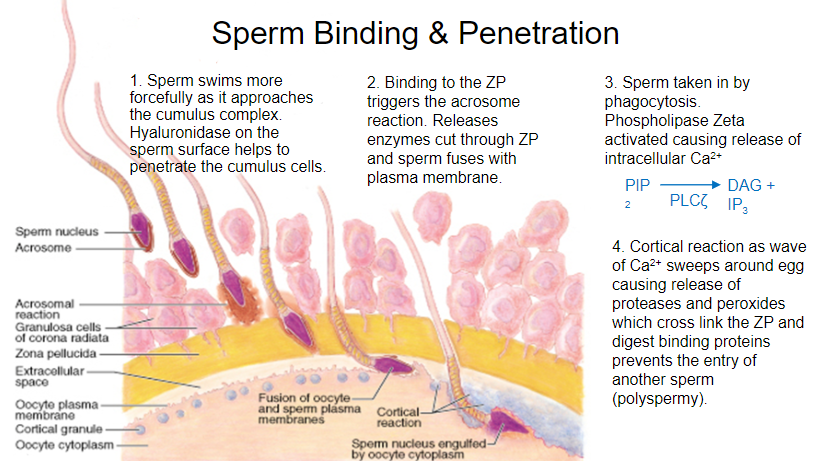
Phagocytosis: The sperm is engulfed by the egg through phagocytosis after it penetrates the cumulus cells and reaches the egg membrane.
-
What role does Phospholipase Zeta play during fertilization? (2)
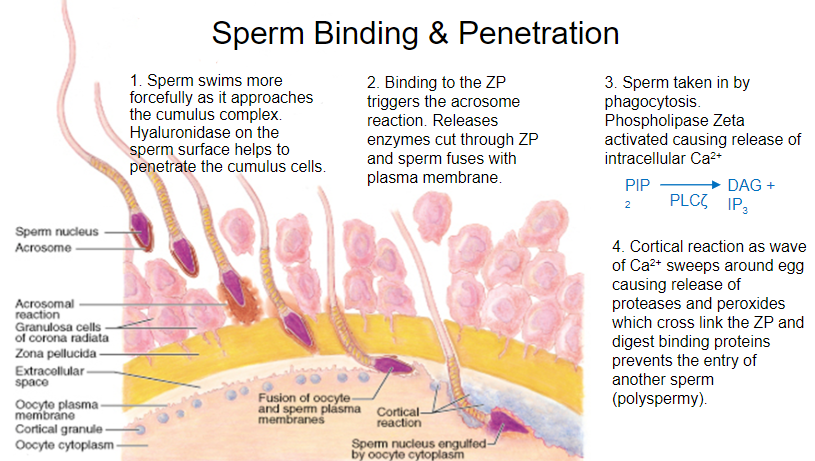
Phospholipase Zeta Activation: Phospholipase Zeta is activated when sperm binds to the egg.
Calcium Release: This activation causes the release of intracellular calcium (Ca2+), which triggers a cascade of events essential for fertilization.
-
What is the cortical reaction, and how does it prevent polyspermy? (3)
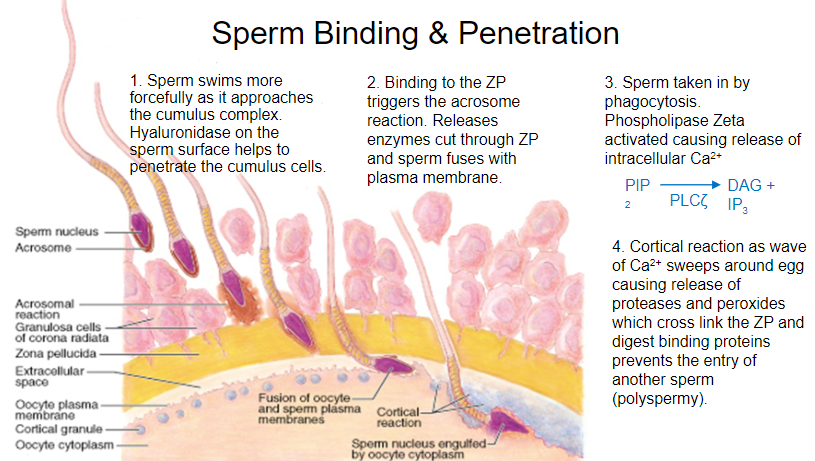
Cortical Reaction: The cortical reaction is triggered by a wave of calcium (Ca2+) sweeping around the egg.
Proteases and Peroxides Release: This wave causes the release of proteases and peroxides, which cross-link the zona pellucida (ZP).
Prevents Polyspermy: The cross-linking of the ZP and digestion of binding proteins prevent the entry of additional sperm, thus preventing polyspermy.
-
What triggers the acrosome reaction, and what does it result in? (2)
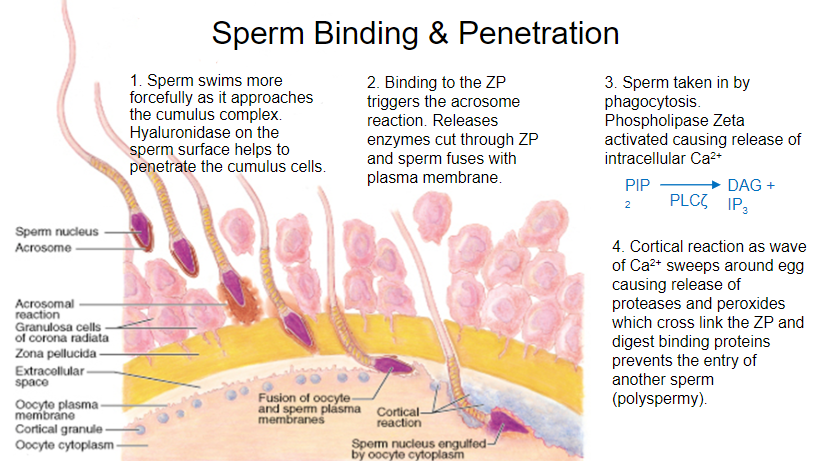
Binding to the Zona Pellucida: Sperm binding to the zona pellucida (ZP) triggers the acrosome reaction.
Enzyme Release: The acrosome reaction results in the release of enzymes that break down the ZP, allowing the sperm to penetrate and fuse with the egg's plasma membrane.
-
What happens to the chromosomes of the ovulated oocyte after meiosis I? (2)
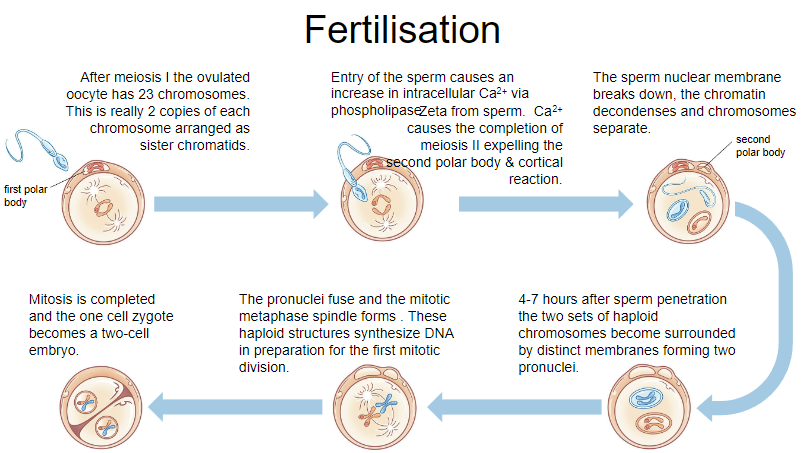
Chromosome Number: After meiosis I, the ovulated oocyte has 23 chromosomes.
Chromosome Structure: Each chromosome exists as two sister chromatids.
-
How does the entry of sperm trigger meiosis II in the oocyte? (2)
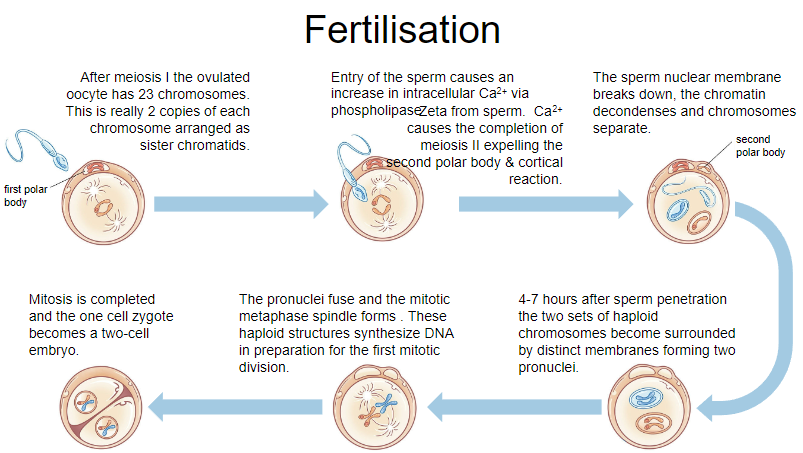
Calcium Release: The entry of sperm causes an increase in intracellular calcium (Ca2+).
Completion of Meiosis II: The rise in Ca2+ triggers the completion of meiosis II, expelling the second polar body and initiating the cortical reaction.
-
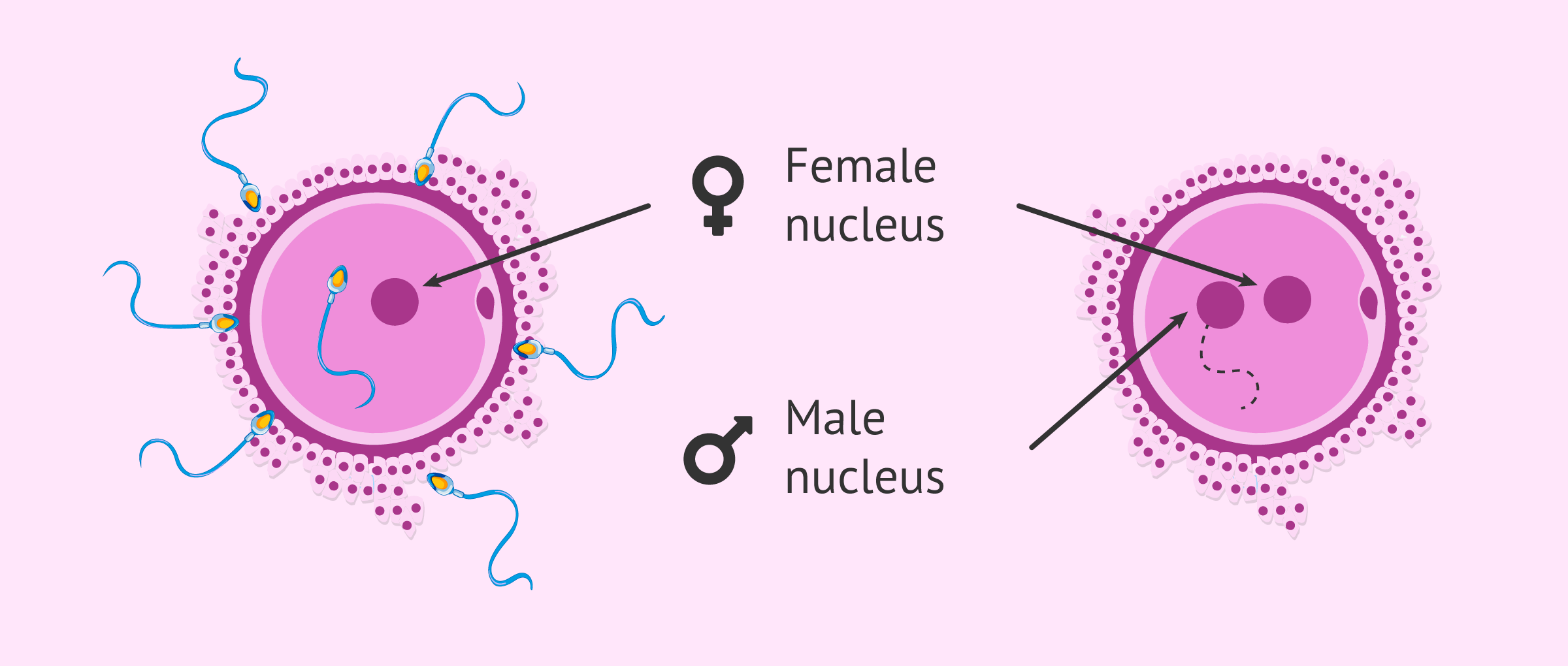
What happens 4-7 hours after sperm penetration during fertilization? (2)
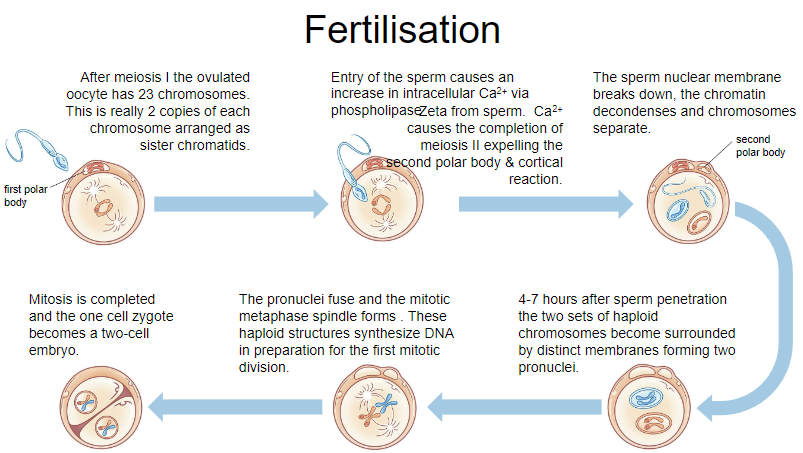
Pronuclei Formation: 4-7 hours after sperm penetration, the two sets of haploid chromosomes become surrounded by distinct membranes, forming two pronuclei.
Sperm and Egg Pronuclei: Each pronucleus contains a haploid set of chromosomes from the sperm and the egg.
-
What happens when the pronuclei fuse during fertilization? (2)
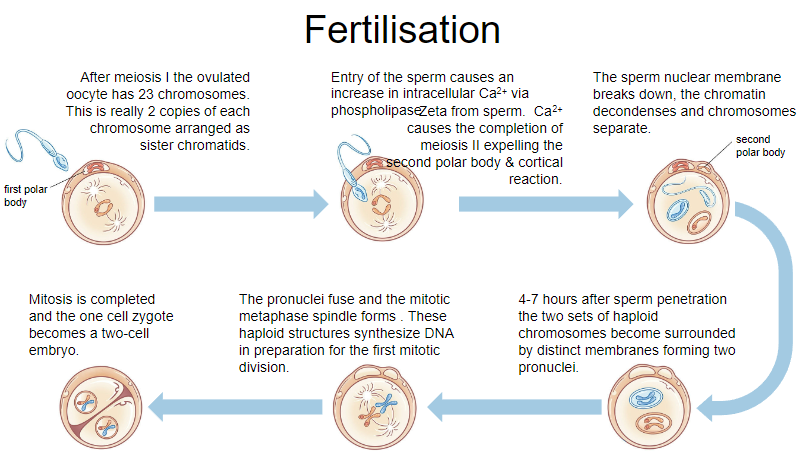
Pronuclei Fusion: The two pronuclei fuse, combining the genetic material from both the sperm and the egg.
Metaphase Spindle Formation: The mitotic spindle forms in preparation for the first mitotic division.
-
What occurs during the first mitotic division after fertilization? (2)
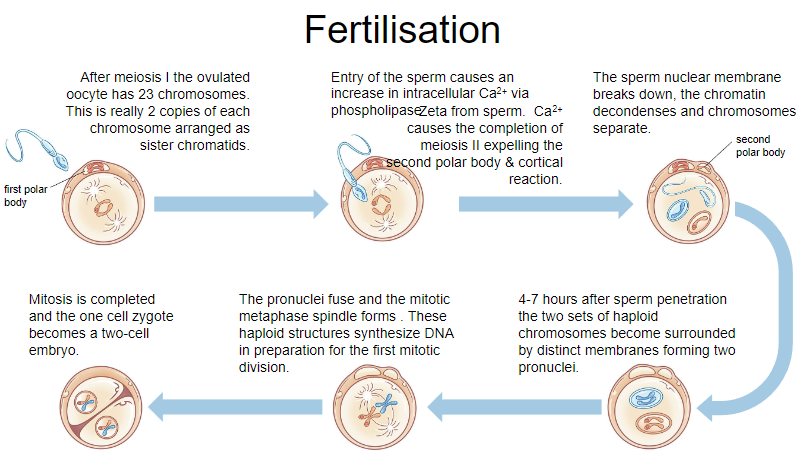
DNA Synthesis: Both haploid structures synthesize DNA in preparation for the first mitotic division.
Zygote to Embryo: Mitosis is completed, and the one-cell zygote becomes a two-cell embryo.
-
What happens to the sperm nucleus after fertilization? (3)
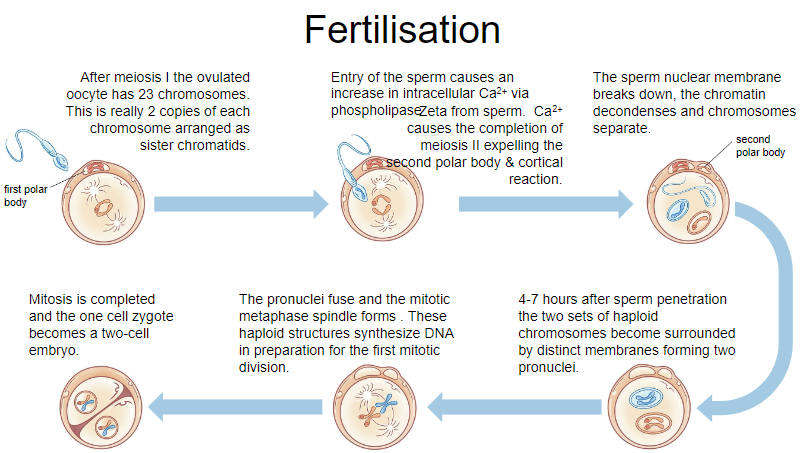
Nuclear Breakdown: The sperm nuclear membrane breaks down.
Chromatin Decondensation: The sperm chromatin decondenses, allowing it to mix with the egg's chromosomes.
Chromosome Separation: The chromosomes separate in preparation for the first mitotic division.
-
What happens when sperm enters the oocyte during fertilization? (2)
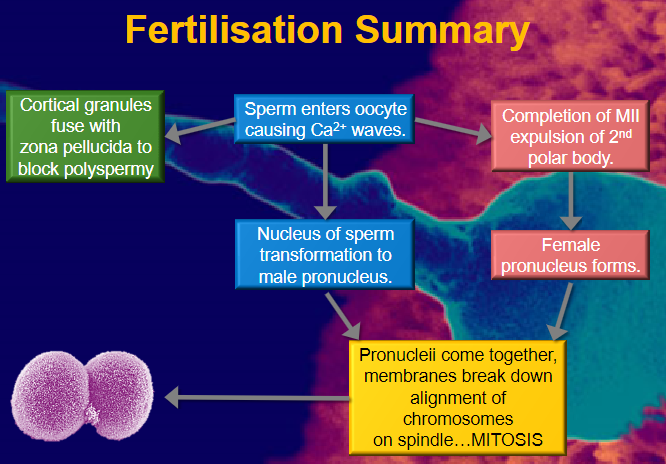
Calcium Waves: Sperm entry triggers waves of calcium (Ca2+) within the oocyte.
Cortical Granules Fusion: Cortical granules fuse with the zona pellucida to block polyspermy, preventing more than one sperm from entering.
-
What happens during the completion of Meiosis II (MII) after sperm entry? (2)
Expulsion of Second Polar Body: The second polar body is expelled as a result of the completion of meiosis II.
Sperm Nucleus Transformation: The sperm’s nucleus undergoes transformation to become the male pronucleus.
-
What occurs after the formation of the male and female pronuclei? (3)
Female Pronucleus Formation: The female pronucleus forms from the oocyte’s nucleus.
Pronuclei Fusion: The male and female pronuclei come together.
Membranes Breakdown: The membranes of the pronuclei break down, allowing chromosomes to align on the spindle for mitosis.
-
What is the first sign of fertilization in early embryo development? (1)
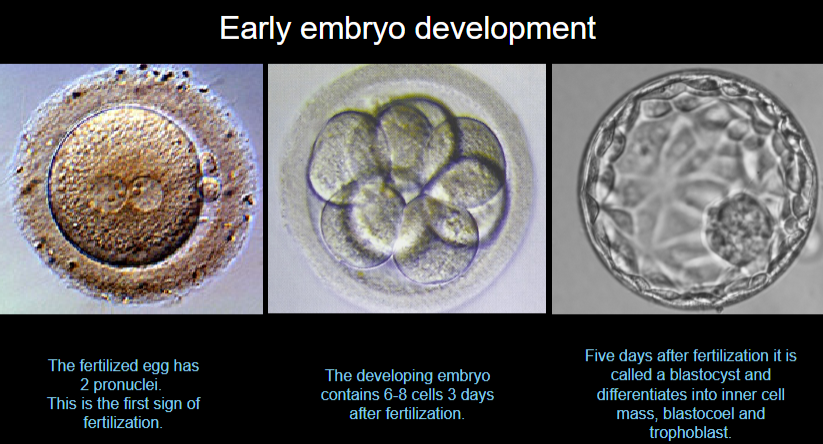
Two Pronuclei: The fertilized egg contains two pronuclei, marking the first sign of fertilization.
-
What is the state of the embryo 3 days after fertilization? (1)
6-8 Cells: The embryo contains 6-8 cells three days after fertilization.
-
What is the embryo called 5 days after fertilization, and what are its components? (3)
Blastocyst: The embryo is called a blastocyst five days after fertilization.
Inner Cell Mass: A group of cells inside the blastocyst that will develop into the embryo.
Blastocoel: A fluid-filled cavity within the blastocyst.
Trophoblast: The outer layer of cells that will form the placenta
-
Picture demonstrating the cycle of the blastocyst:
-
Describe the acrosome reaction and its role in fertilization. (4)
Acrosome Reaction: The acrosome reaction occurs when the sperm comes into contact with the zona pellucida (ZP) surrounding the oocyte.
Fusion of Membranes: The outer acrosomal membrane of the sperm fuses with the plasma membrane, forming pores.
Release of Enzymes: These pores release enzymes that digest the ZP, allowing the sperm to penetrate and fuse with the oocyte.
Role in Fertilization: This reaction is crucial for sperm to reach and fertilize the egg by breaking down the ZP and enabling the sperm to enter the egg.
-
Which two important events are triggered by the rise in LH at the end of the follicular phase? (2)
Completion of Meiosis I: The rise in LH triggers the resumption of meiosis in the oocyte, completing meiosis I.
Ovulation: LH triggers ovulation, causing the mature follicle to rupture and release the secondary oocyte.
-
What triggers the completion of meiosis II in the oocyte? (1)
Entry of Sperm: The entry of the sperm into the oocyte triggers a rise in intracellular calcium, which activates the completion of meiosis II and expels the second polar body.
-
How does the oocyte prevent polyspermy after a sperm successfully fuses with the egg? (3)
Cortical Reaction: The fusion of the sperm with the egg triggers the release of cortical granules from the egg.
Modification of the Zona Pellucida (ZP): The cortical granules modify the ZP by cross-linking proteins and preventing further sperm from binding.
Block to Polyspermy: This prevents additional sperm from entering the egg, ensuring that only one sperm fertilizes the oocyte.
-
What role does human chorionic gonadotropin (hCG) play in rescuing the corpus luteum, and why is this essential for early pregnancy? (3)
Rescue of Corpus Luteum: hCG, secreted by the embryo, binds to the LH receptors on the corpus luteum, preventing its degeneration.
Continued Progesterone Production: By rescuing the corpus luteum, hCG ensures the continued production of progesterone.
Essential for Early Pregnancy: Progesterone is critical for maintaining the endometrium and supporting early pregnancy by preventing menstruation.
-
Outline the roles of the inner cell mass and the trophectoderm in the blastocyst. How does each contribute to early development? (4)
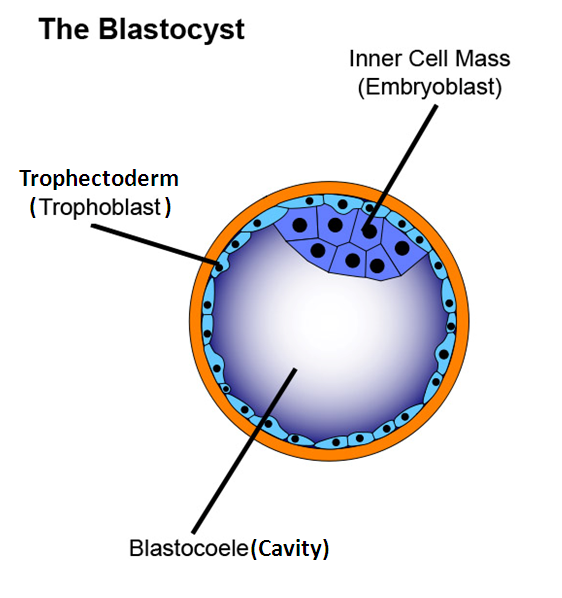
Inner Cell Mass (ICM): The ICM will form the embryo itself, differentiating into the three germ layers that give rise to all the tissues and organs of the body.
Trophectoderm: The trophectoderm forms the placenta, providing the necessary support for the developing embryo.
Early Development: The ICM and trophectoderm work together to initiate early development, with the ICM forming the embryo and the trophectoderm aiding in implantation and nutrient exchange.
Formation of Extra-Embryonic Tissues: The trophectoderm also contributes to forming extra-embryonic tissues essential for embryo survival and growth.
-
What are the key changes in the endometrium during the luteal phase that prepare it for potential implantation? (4)
Endometrial Thickening: Under the influence of progesterone, the endometrium thickens and becomes more vascularized.
Glandular Secretion: The endometrial glands become more active, secreting nutrients to support a potential embryo.
Decidualization: The endometrial cells undergo decidualization, preparing to provide an environment conducive to embryo implantation.
Increased Blood Flow: Blood vessels in the endometrium expand to enhance nutrient and oxygen supply to the developing embryo if implantation occurs.

