Effect of the Environment on the Skin (Physiology 2)
Effect of environment on skin - Azza Shoreim Session introduction The skin is the major interface between the body and the world, conveying sensations and also reacting and adapting to environmental cues like heat, cold and sunlight. It protects us from a wide range of environmental “insults” or stresses such as infections, irritants and physical trauma. Here more detail is presented on these responses and protective functions, and an introduction to what can happen if protection fails – some types of skin disorders and diseases. Learning Outcomes At the end of this resource you will be able to: List the potential types of environmental “insults” upon the skin. List the protective features of the skin. Describe the normal skin adaptations to environmental insults. Describe common abnormal skin conditions that have environmental causes. Session Resources AS Environmental effects on the skin.pptxDownload AS Environmental effects on the skin.pptx Session Recording: Extra Activity: Mind the Gap Skin conditions can have a very different appearance in people of different skin colours. Today’s lecture gave only a short introduction to skin pathology but for anyone interested in this, an amazing student-staff collaboration at St George’s has recently resulted in an online resource: https://www.blackandbrownskin.co.uk/mindthegapLinks to an external site. with an online handbook Mind the GapLinks to an external site., showing the appearances of skin conditions on black and brown skin. Optional resources Human Physiology (5th Edition) Pocock, Richards and Richards. Chapter 42 Glossary Thermoregulation – regulation of body temperature Waveband – a band of wavelengths (of radiation) Ultraviolet (UV) A, B and C – the three wavebands of UV light. Band UVA comprises the longest and UVC the shortest wavelengths. All shorter than visible light. Solar elastosis – loss of skin elasticity (wrinkles) Naevus (pl. naevi) – a skin mole Melanoma – cancer of melanocytes Non-melanoma skin cancer – as it sounds, but nearly always from keratinocytes Dermatitis – skin inflammation Allergen – something that can cause allergy Papilloma – a wart
-
What is the skin's role as an interface? (2)
Acts as a boundary between the body and the external environment.
Protects the body from a wide range of insults (stresses).
-
What complications can arise from extensive epidermal or epidermal + dermal damage, such as severe burns or drug reactions? (5)
Dehydration and shock
Infection
Heat loss and hypothermia (or hyperthermia due to impaired thermoregulation)
Protein loss and electrolyte imbalance
High-output cardiac failure and renal failure
-
What is toxic epidermal necrolysis (TEN)? (2)
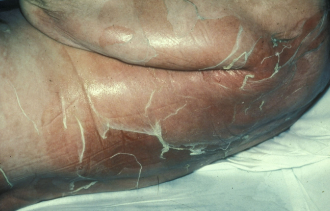
A rare adverse drug reaction causing detachment of the epidermis.
Often fatal.
-
What are the initial symptoms of toxic epidermal necrolysis? (1)

Flu-like illness.
-
What symptoms follow the initial flu-like illness in toxic epidermal necrolysis? (3)

Rapid appearance of a painful erythematous rash.
Desquamation (shedding) of skin.
Mucous membrane involvement.
-
What are some environmental insults that the skin faces? (3)
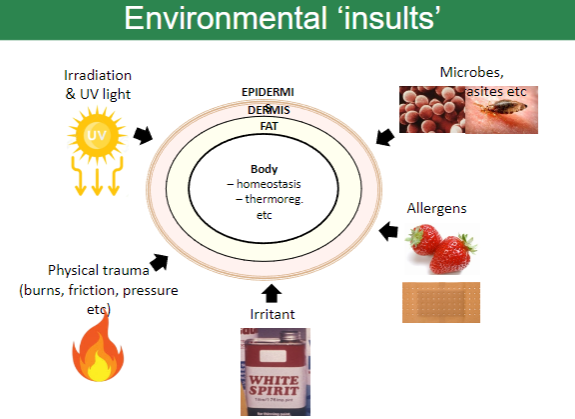
Irradiation (e.g., UV light exposure).
Microbes and parasites.
Physical trauma (e.g., burns, friction, pressure).
-
What roles does the skin play in the body? (2)
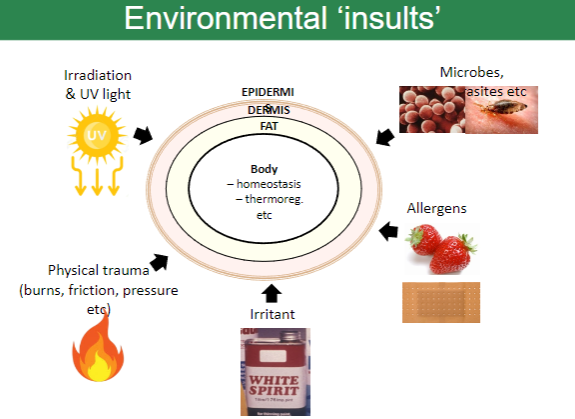
Maintaining homeostasis.
Thermoregulation (temperature control).
-
What are some irritants that can affect the skin? (2)
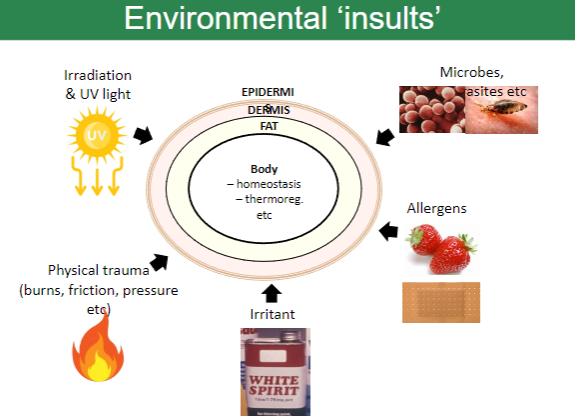
Chemicals such as white spirit.
Allergens, leading to reactions.
-
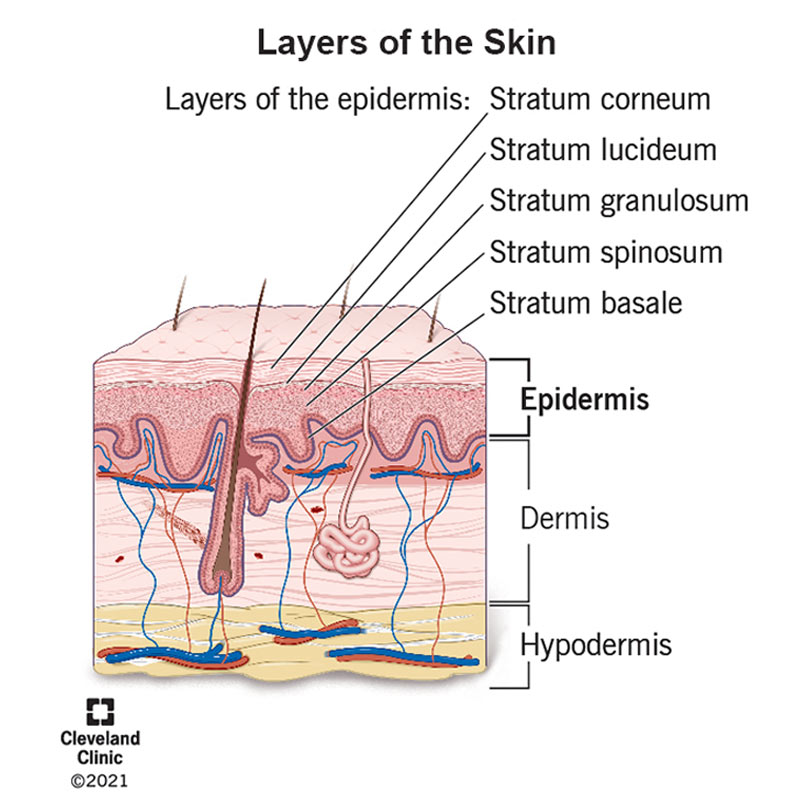
What are the three primary layers of the skin? (3)

Epidermis.
Dermis.
Fat layer (subcutaneous tissue).
-
What protective features of the skin prevent drying? (2)
Waterproof epidermis due to lipids produced from keratinocytes.
Oil from sebaceous glands.
-
How does the skin protect against friction and impact? (5)
Thick, regenerating epidermis.
Keratin in the epidermis.
Nails for additional protection.
Basement membrane anchors the epidermis to the dermis with a wavy border against shear forces.
Collagen fibres in the dermis, which are strong and multidirectional.
-
How does the skin regulate heat? (2)
Sweating to cool the body.
Vasodilation to release heat.
-
How does the skin provide protection against the cold? (3)
Subcutaneous fat for insulation.
Adaptable blood supply.
Hair on the head for additional warmth.
-
How does the skin protect against burns and injury? (1)
Thick, regenerating epidermis.
-
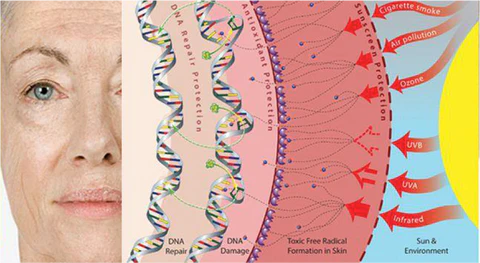
What features of the skin protect against radiation and sunlight? (2)
Thick epidermis.
Melanin to absorb UV radiation.
-
How does the skin protect against infections? (2)
Impervious epidermis acts as a barrier.
Resident immune cells in the skin
-
What protective features of the skin prevent drying? (2)
Waterproof epidermis.
Oil from sebaceous glands.
-
How does the skin protect against friction and impact? (5)
Thick, regenerating epidermis.
Keratin in the epidermis.
Nails for additional protection.
Basement membrane anchors the epidermis to the dermis with a wavy border against shear forces.
Collagen fibres in the dermis, which are strong and multidirectional.
-
How does the skin regulate heat? (2)
Sweating to cool the body.
Vasodilation to release heat.
-
How does the skin protect against cold? (3)
Subcutaneous fat.
Adaptable blood supply (vasoconstriction).
Hair, particularly on the head
-
What are the skin’s defenses against burns and injury? (1)
Thick, regenerating epidermis.
-
How does the skin protect against radiation/sunlight? (2)
Thick epidermis.
Melanin.
-
What are the protective features of the skin against infections? (2)
Impervious epidermis.
Resident immune cells within the skin.
-
What are the skin’s adaptations to heat? (2)
Sweating.
Vasodilatation
-
What are the skin’s adaptations to cold? (1)
Vasoconstriction
-
What is hyperkeratosis, and how does it develop? (2)
Thickening of the stratum corneum in response to rubbing or pressure (e.g., feet, guitarist fingers, lifting weights).
Can also occur (slightly) after ultraviolet exposure.
-
What is tanning, and how does it develop? (1)
Melanocyte response to ultraviolet exposure, leading to skin darkening over several days.
-
What are arteriovenous (AV) shunts, and where are they found? (2)
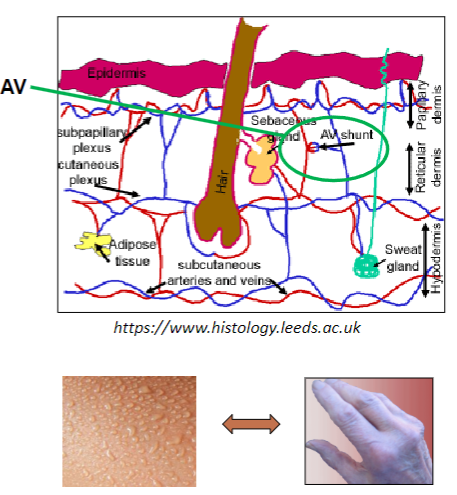
Anastomoses (Connections) between arterioles and venules.
Found in the dermis and numerous in this layer.
-
How do AV shunts respond to thermoreceptors in the skin? (3)
Shunts open in response to heat, increasing blood flow to the superficial vascular plexus for heat loss.
Shunts close in response to cold, reducing blood flow to retain heat.
These changes occur in the papillary dermis, just below the epidermis.
-
How does the skin's appearance change during thermoregulation by AV shunts? (2)
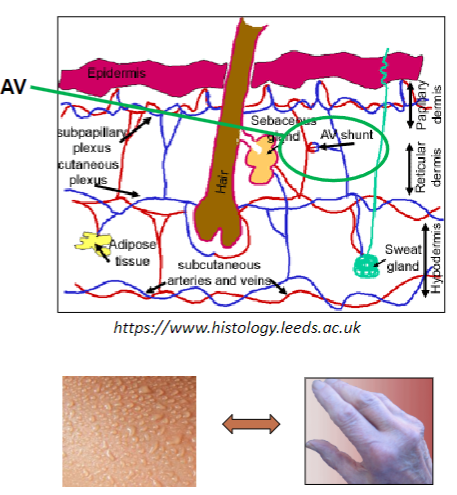
Redder skin with increased blood flow for heat loss.
Bluer skin with reduced blood flow to retain heat.
-
How do AV shunts in the face differ from other areas? (1)
They can also respond to emotions or the sympathetic nervous system, causing blushing.
-
What is a potential danger of AV shunts being shut off for too long? (1)
Can lead to tissue damage, such as frostbite.
-
What is the superficial vascular plexus, and where is it located? (2)
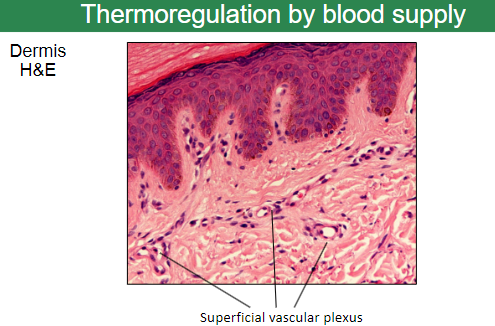
A network of blood vessels in the papillary layer of the dermis.
Plays a key role in thermoregulation by controlling blood flow near the skin's surface.
-
How does thermoregulation occur through the superficial vascular plexus? (2)
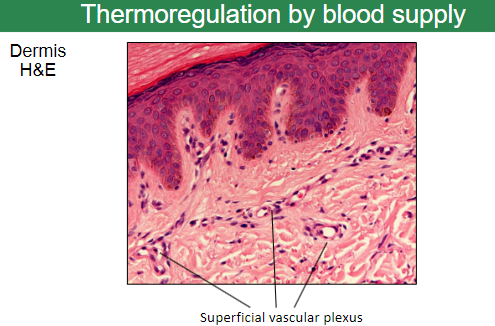
Increased blood flow to the plexus results in heat loss.
Decreased blood flow conserves heat by reducing heat loss.
-
What histological staining technique is used to visualize the dermis? (1)
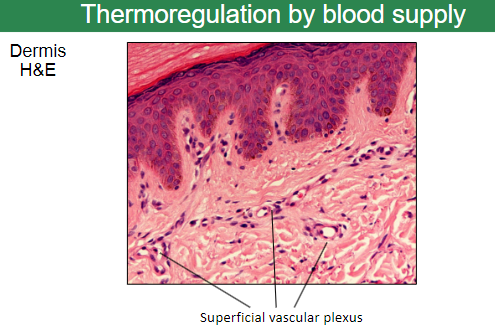
Hematoxylin and Eosin (H&E) staining is commonly used.
-
What are the main contributors to the color of human skin? (2)
Melanin (mainly dark skin).
Hemoglobin (mainly light skin).
-
What genetic factors contribute to skin color? (1)
There is normal genetic variation in the amount of melanin, with over 12 known genes influencing melanin production.
-
How does melanin provide protection against UV radiation? (2)
Melanin protects against DNA damage, which can lead to skin cancer.
Dark skin (e.g., black and Asiatic) has lower incidence of skin cancer, approximately 8-10% of the rate in white people.
-
Where are melanocytes located and what do they do? (2)
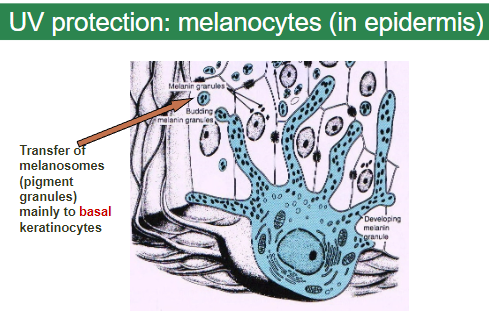
Melanocytes are located in the epidermis.
They transfer melanosomes (pigment granules) mainly to basal keratinocytes.
-
How does tanning provide UV protection? (3)

Melanocytes increase activity, producing and transmitting more melanin.
This increase in melanin offers some protection against UV.
Skin thickens in response to UV exposure, providing additional protection.
-
What is the basic process of suntanning at the cellular level? (5)
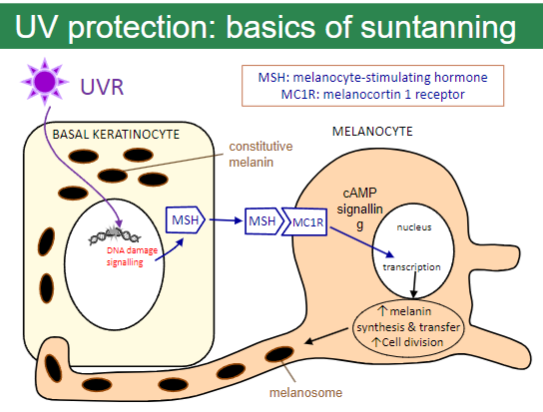
MC1R (melanocortin 1 receptor) and MSH (melanocyte-stimulating hormone) play key roles in the process.
UV radiation causes DNA damage, which triggers a signalling pathway.
This pathway stimulates an increase in melanin synthesis and its transfer to basal keratinocytes.
Cell division increases in response to UV exposure, contributing to skin thickening.
cAMP signaling helps activate the process by affecting melanosomes (pigment granules).
-
What are the key steps and molecules involved in the synthesis of melanin during suntanning? (5)
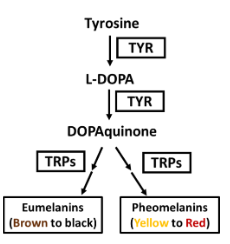
Tyrosine (TYR) serves as the starting molecule for melanin production.
Tyrosine is converted into L-DOPA by the enzyme tyrosinase (TYR).
L-DOPA is further oxidized into DOPAquinone by tyrosinase.
Enzymes like Tyrosinase-Related Proteins (TRPs) influence the downstream processing of DOPAquinone.
DOPAquinone is a precursor for two types of melanin:
Eumelanin (brown to black pigment).
Pheomelanin (yellow to red pigment).
-
How does the skin protect against microorganisms? (4)
Small cells in non-basal layers of skin, including dendritic cells, play a key role.
These cells function as antigen-presenting cells (similar to macrophages).
Langerhans cells are specialized dendritic cells in the epidermis that help recognize pathogens.
Langerhans cells, along with the rest of the immune system, form a network in the epidermis to provide protection against microorganisms.
-
What are some abnormal effects of the environment on the skin? (6)
Friction/scratching can damage the skin.
Ultraviolet irradiation causes skin damage and increases the risk of skin cancer.
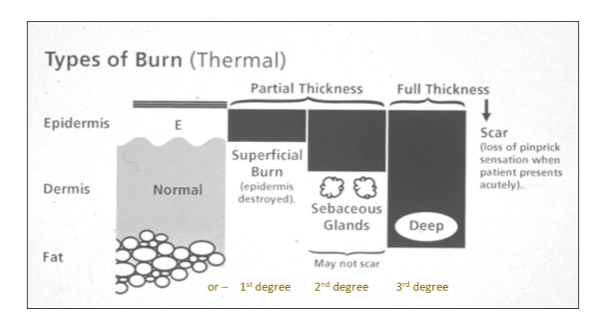
Burns lead to tissue damage and potential loss of skin function.
Irritants can cause inflammation or damage to the skin.
Allergens trigger allergic reactions and skin sensitivities.
Microbes (bacteria, viruses, fungi) can cause infections or skin diseases.
-
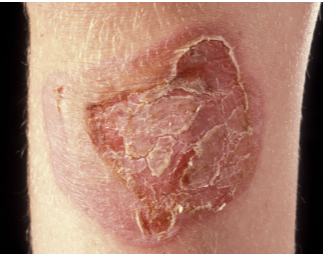
What is lichenification and what causes it? (2)

Lichenification is an extreme form of hyperkeratosis, characterized by thickened, leathery skin.
It is caused by excessive rubbing, scratching, or prolonged skin conditions that trigger repeated irritation.
-
What are the effects of sunburn and its relation to skin cancer? (4)
Sunburn is caused by UV irradiation, which acts as a radiation burn to the skin.
It results in blisters, inflammation, and cell death due to severe DNA damage.
Having been sunburnt increases the risk of developing skin cancer.
Using UV sunbeds before age 35 increases the risk of skin cancer by 75%.
-
What is Polymorphic Light Eruption and its relation to UV irradiation? (2)

Polymorphic light eruption is a skin condition triggered by UV irradiation.
It results in a rash that appears after sun exposure, particularly in individuals with sensitive skin.
-
What is solar elastosis and how does it relate to wrinkles? (2)

Solar elastosis refers to the loss of skin elasticity caused by long-term sun exposure.
It leads to the formation of wrinkles due to the degradation of collagen and elastin fibers in the skin.
-
What are naevi (moles) and their relationship with UV irradiation? (3)

Naevi (or moles) are benign proliferations of melanocytes in the skin.
They can be caused or exacerbated by UV irradiation.
Having many or large naevi increases the risk of developing melanoma skin cancer.
-
What are freckles (ephelides) and their relationship with UV irradiation? (3)

Freckles (ephelides) have a genetic component and are often linked to individuals with red/fair hair.
They are associated with MC1R gene variants.
Freckles typically appear in sun-exposed areas of the skin.
-
What are solar lentigos (liver spots, age spots) and their association with UV irradiation? (2)

Solar lentigos (also known as liver spots or age spots) are pigmented spots that appear on the skin due to UV irradiation.
These spots are commonly found in areas that have been repeatedly exposed to the sun over time.
-
What are solar keratoses and their association with UV irradiation? (2)
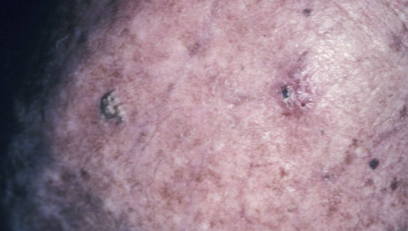
Solar keratoses (also known as actinic keratoses) are dysplastic growths of keratinocytes that result from UV irradiation.
They are often considered precancerous lesions that can potentially develop into skin cancer if left untreated.
-
What is the difference between melanoma and non-melanoma skin cancers? (2)
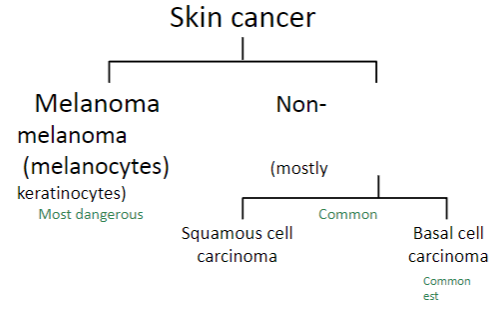
Melanoma is a skin cancer that originates from melanocytes and is considered the most dangerous form of skin cancer.
Non-melanoma skin cancers (e.g., squamous cell carcinoma and basal cell carcinoma) originate from keratinocytes and are generally more common but less dangerous compared to melanoma.
-
What is Basal Cell Carcinoma (BCC) and how is it treated? (2)
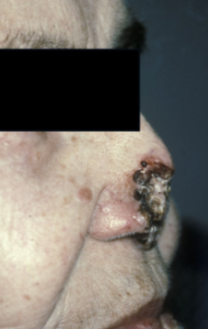
Basal cell carcinoma (BCC), also known as ‘rodent ulcer’, is a type of non-melanoma skin cancer often caused by UV irradiation.
It is often curable by surgery, particularly if reported early.
-
What is Melanoma and how is it related to UV irradiation? (3)
Melanoma is a type of skin cancer that can be thin, but still dangerous due to its rapid spread.
UV irradiation, including both UVA and UVB, can cause melanoma, even in pigmented mice.
This information is relevant to sunscreen design and tanning salons, as both types of UV radiation contribute to the risk of developing melanoma.
-
What are the benefits of UV radiation for the skin? (2)
UV radiation is needed for vitamin D3 production in the skin. 15 minutes of summer sun on the face and arms per day is enough for white skin, and longer exposure is required for dark skin. Alternatively, vitamin D supplements can be taken.
Ultraviolet radiotherapy is used for treating certain skin conditions, such as vitiligo and psoriasis.
-
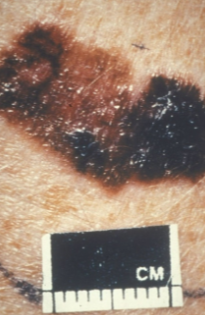
Picture demonstrating the types of burns (degrees):
-
What is irritant contact dermatitis and what are its symptoms? (4)
Irritant contact dermatitis occurs when there is too much exposure to a substance.
It can still be used, but the amount of exposure should be reduced.
People vary in sensitivity to the irritant.
Symptoms can include redness, itching, swelling, blistering, and/or scaling.
-
What is allergen contact dermatitis and what are its symptoms? (5)

Allergen contact dermatitis occurs due to an allergy to something that contacts the skin, involving the immune system.
A tiny amount of the allergen may be sufficient to trigger a reaction.
It can vary greatly between people and may develop after long or short exposure.
Symptoms include redness, itching, swelling, blistering, and/or weeping.
Avoiding the allergen in the future is essential to prevent further reactions.
-
What is the difference between irritant contact dermatitis and allergen contact dermatitis, and how does sensitization occur? (4)
Irritant contact dermatitis is common, while allergen contact dermatitis is relatively uncommon (e.g., nickel).
Sensitization occurs first when Langerhans cells process the antigen and present it to lymphocytes.
Upon subsequent exposure, delayed hypersensitivity occurs due to the presence of memory T-cells, which recognize the antigen.
-
What is Paronychia and how is it caused? (2)

Paronychia is a nail fold infection, which can be caused by either fungal or bacterial infections.
-
What is Tinea capitis and what does it affect? (2)

Tinea capitis is a fungal infection commonly known as scalp ringworm.
It primarily affects the scalp and can cause hair loss, itching, and scaly patches.
-
What is Impetigo and what causes it? (2)
Impetigo is a bacterial skin infection.
It is commonly caused by Staphylococcus aureus or Streptococcus pyogenes and results in blisters, red sores, and crusting.
-
What is Human Papilloma Virus (HPV) and how does it affect the skin? (2)
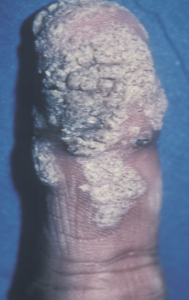
Human Papilloma Virus (HPV) causes warts on the skin, which can be raised, rough, or flat.
It is a viral infection that spreads through direct contact or contaminated surfaces.
-
How can infections enter the body through the skin and what factors predispose individuals to infection? (3)
Portal of entry: Microbes can enter through breaches in the epidermis, such as cuts or abrasions. For example, Streptococcus can cause cellulitis.
Impaired immunity: Conditions like HIV and viral warts can increase susceptibility to infections.
Pre-existing skin conditions: For example, eczema herpeticum occurs when the herpes virus infects areas of skin affected by eczema.
-
What are the normal adaptive mechanisms of the skin, and what environmental insults can cause skin damage? (8)
Normal adaptive mechanisms:
Temperature changes: Sweating, vasodilation, and vasoconstriction.
Friction: Hyperkeratosis (thickening of the skin).
UV radiation: Melanin production.
Environmental insults causing skin damage:
Friction and scratching.
UV radiation.
Burns.
Irritants.
Allergens and microbes (bacteria, viruses, fungi).

