Drugs and the Kidney (Physiology)
Session summary Many drugs exert their effects by targeting kidney function. Diuretics are a clinically-important class of such drugs. This session will cover the clinical use of diuretic treatment and physiological mechanisms of diuretic action on the renal tubule. Learning outcomes At the end of this session you will be able to: Outline the main mechanisms for renal excretion of drugs Describe the classes of diuretic drugs and there mode of action Explain the clinical uses and complications of diuretic drugs
-
What is the most important organ for eliminating drugs from the body? (1)
★The kidney is the most important organ for eliminating drugs from the body.
-
What is the general process for drug elimination by the liver and kidney? (1)
★Most drugs are metabolized by the liver to inactive compounds that can be excreted by the kidney.
-
How are polar drugs or metabolites excreted from the body? (1)
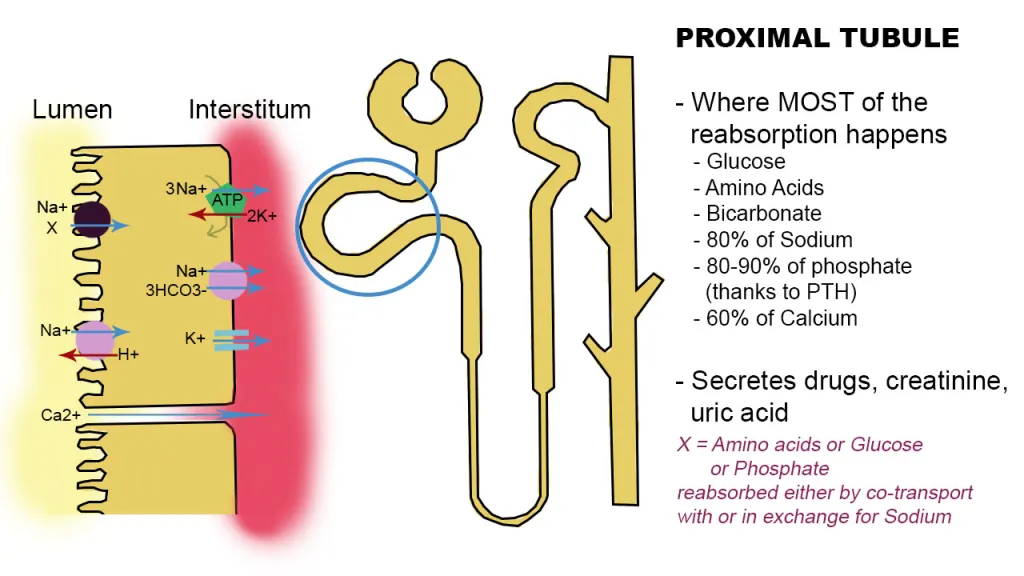
★Polar drugs or metabolites, which are water-soluble and partially ionized, are excreted via specialized transporters, mainly located in the proximal tubule of the kidney.
-
Where does tubular secretion of drugs mainly occur? (1)
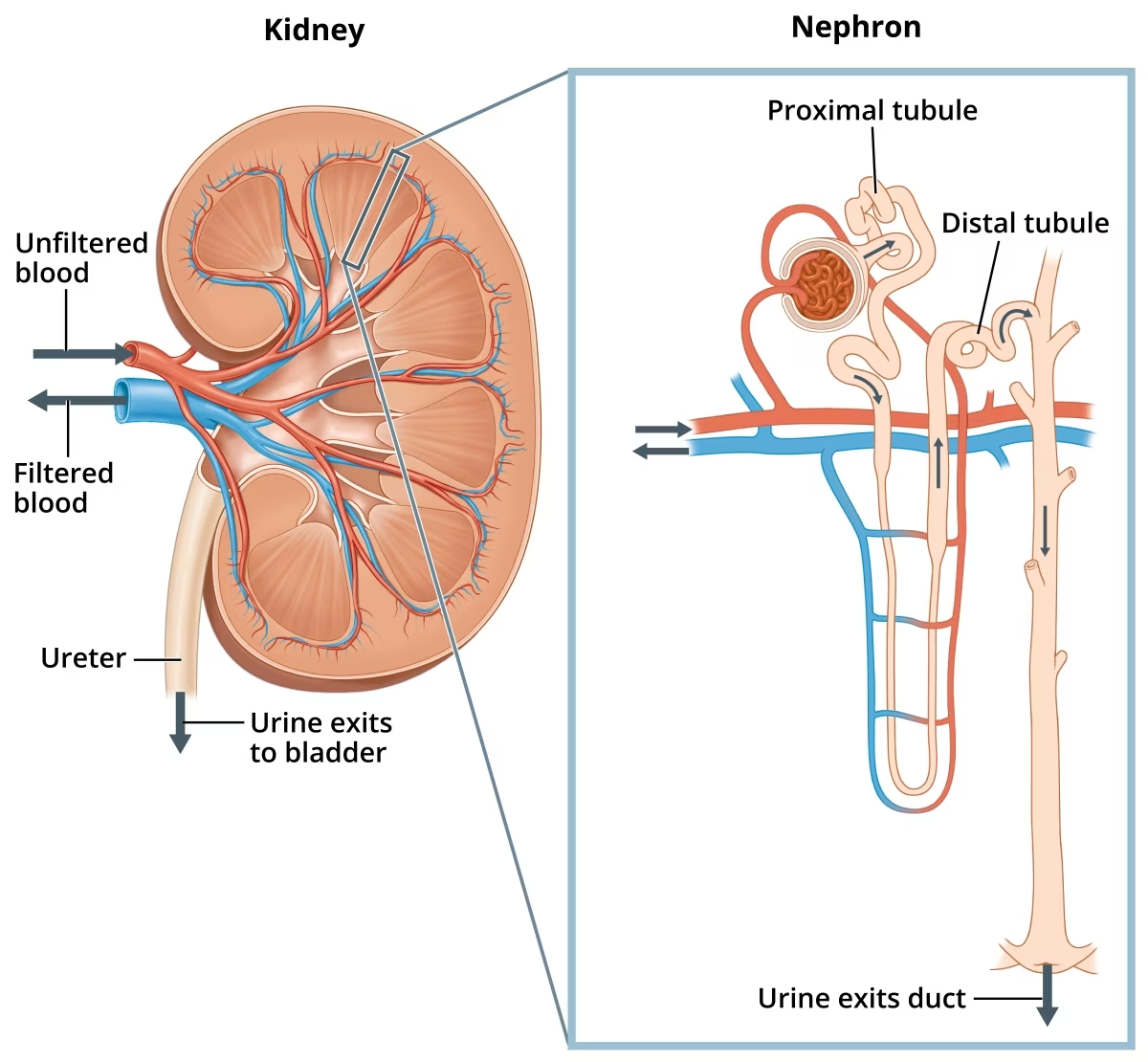
★Tubular secretion of drugs mainly occurs in the proximal tubule (PT) of the kidney.
-
What determines the degree of ionization of drugs in the renal tubules? (1), And give examples (2)
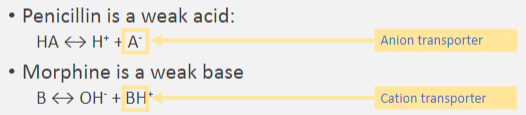
★The degree of ionization of drugs in the renal tubules depends on the drug's pKa and the pH of the environment. For example:
★Penicillin, a weak acid, exists in equilibrium between its protonated (HA) and deprotonated (A-) forms.
★Morphine, a weak base, exists in equilibrium between its protonated (BH+) and deprotonated (B) forms.
-
What types of transporters are involved in tubular secretion of drugs? (1), And give examples (2)
★Tubular secretion of drugs involves a family of non-specific cation and anion transporters, including:
★Anion transporters, which transport negatively charged ions.
★Cation transporters, which transport positively charged ions.
-
What is the primary effect of diuretics? (1)
★Diuretics increase urine output, a process known as diuresis.
-
What additional effect may diuretics have on electrolyte excretion? (1)
★Diuretics may also increase electrolyte excretion, including sodium (natriuresis) and potassium (kaliuresis).
-
What are some important clinical uses of diuretics? (4)
Diuretics are important drugs used in conditions such as:
★Acute pulmonary oedema and heart failure to reduce extracellular fluid (ECF) volume.
★Hypertension to help lower blood pressure.
★Glaucoma due to build up of aqueous humour which diuretic decrease
★Intracranial pressure due to build up of cerebrospinal fluid
-
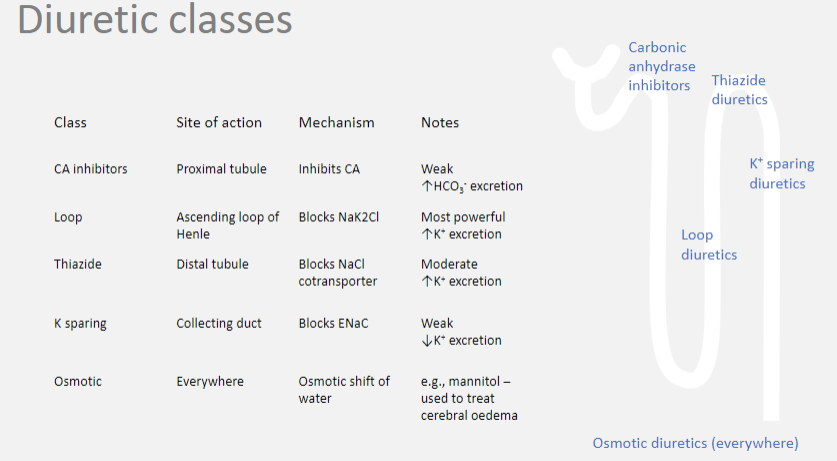
Picture demonstrating the Diuretic classes:
-
What is an example of an osmotic diuretic? (1)
★Mannitol is an example of an osmotic diuretic.
-
How do osmotic diuretics work in the kidney? (1)
★Osmotic diuretics are freely filtered by the glomerulus but are not reabsorbed in the renal tubules. This impairs the dilution of fluid in the distal tubule (DT) and decreases the gradient for water reabsorption, leading to increased urine output.
-
What is a common clinical use of osmotic diuretics? (1)
★Osmotic diuretics, such as mannitol, are commonly used to treat cerebral edema because they do not cross the blood-brain barrier. They create an osmotic gradient that promotes the withdrawal of water from cerebrospinal fluid into the plasma.
-
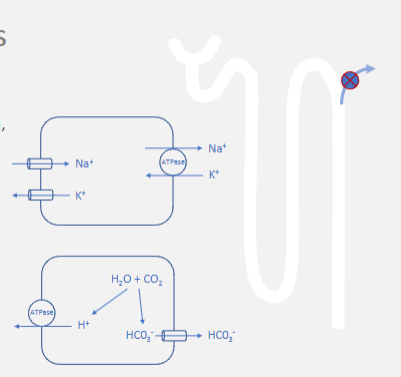
What is an example of a carbonic anhydrase inhibitor? (1)
★Acetazolamide is an example of a carbonic anhydrase inhibitor.
-
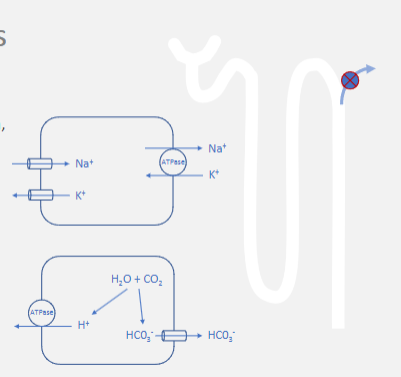
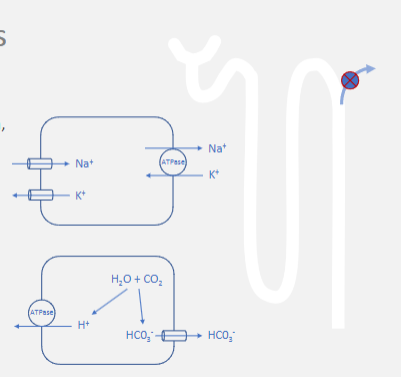
How do carbonic anhydrase inhibitors work in the kidney? (1)
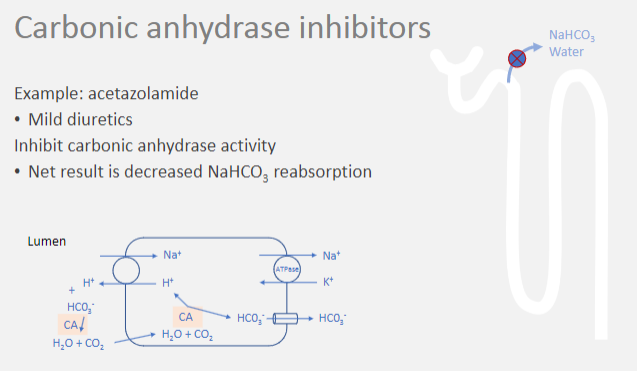
★Carbonic anhydrase inhibitors inhibit the activity of the enzyme carbonic anhydrase in the proximal tubule of the kidney.
-
What is the net result of inhibiting carbonic anhydrase activity? (1)
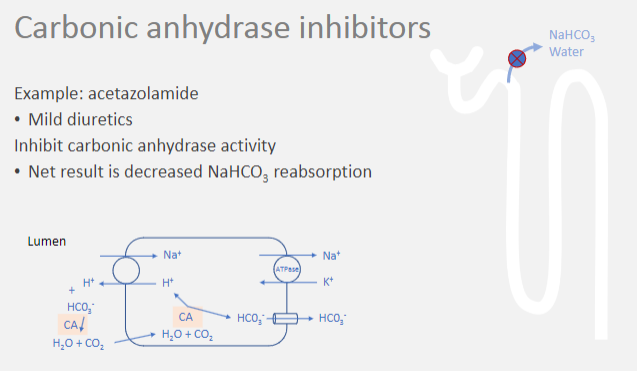
★The net result is decreased reabsorption of bicarbonate ions (HCO3-).
-
Why is decreased reabsorption of bicarbonate ions important? (3)
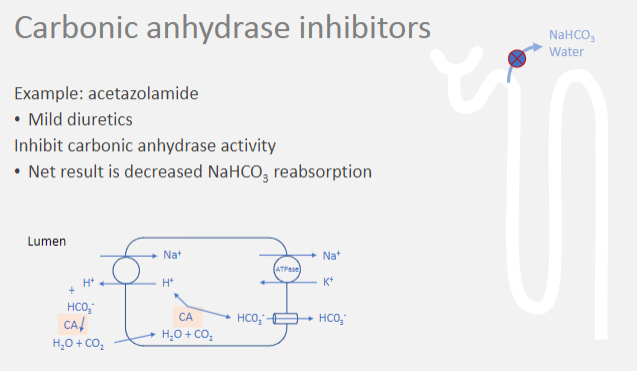
★Decreased reabsorption of bicarbonate ions leads to increased excretion of bicarbonate in the urine.
★Bicarbonate ions play a crucial role in maintaining acid-base balance in the body by acting as a buffer to regulate pH in bodily fluids, including blood.
★Reduced bicarbonate reabsorption can result in metabolic acidosis, an excess of acid in the body fluids.
-
How are carbonic anhydrase inhibitors classified in terms of their diuretic potency? (1)
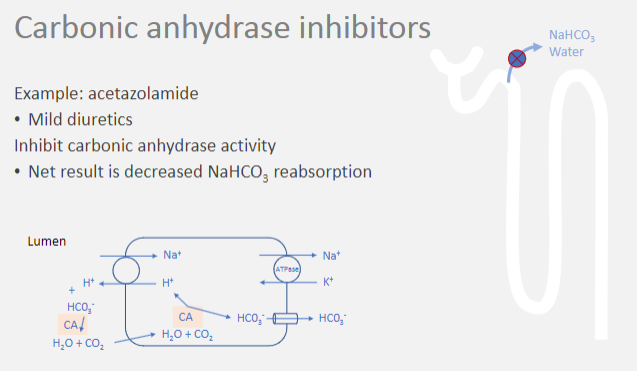
★Carbonic anhydrase inhibitors are classified as mild diuretics.
-
What is an example of a loop diuretic? (1)

★Frusemide is an example of a loop diuretic.
-
How do loop diuretics work in the kidney? (1)
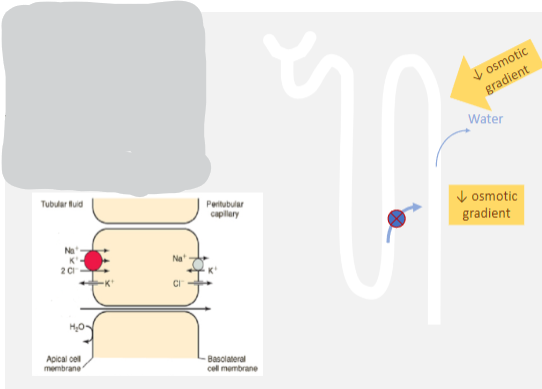
★Loop diuretics inhibit the Na/K/2Cl cotransporter in the thick ascending limb of the loop of Henle.
-
What is the consequence of inhibiting the Na/K/2Cl cotransporter? (1)
★Inhibiting this cotransporter impedes the concentration of medullary interstitial fluid, leading to a reduced osmotic drive for ADH-mediated water reabsorption.
-
What is a common side effect of loop diuretics? (1)
★A significant loss of potassium, resulting in hypokalemia, is a common side effect of loop diuretics.
-
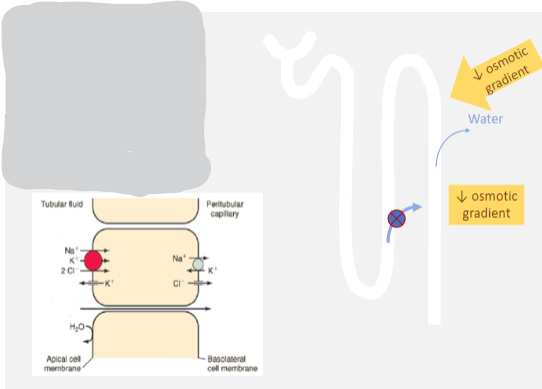
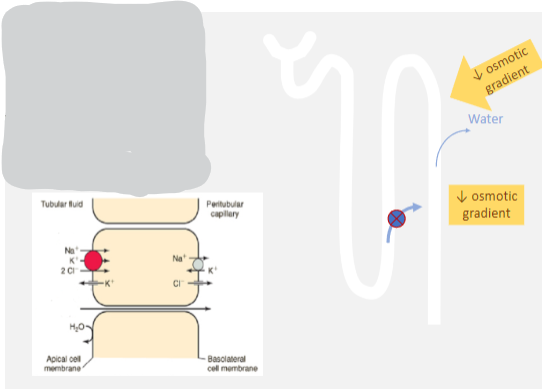
What is the potency of thiazide diuretics? (1)

★Thiazide diuretics are moderately powerful.
-
How do thiazide diuretics work in the kidney? (1)
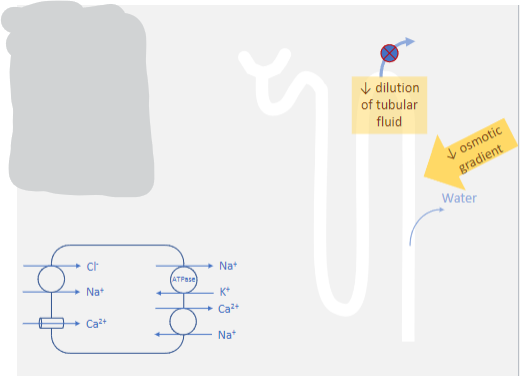
★Thiazide diuretics inhibit the Na/Cl cotransporter in the distal tubule.
-
What is the consequence of inhibiting the Na/Cl cotransporter? (1)
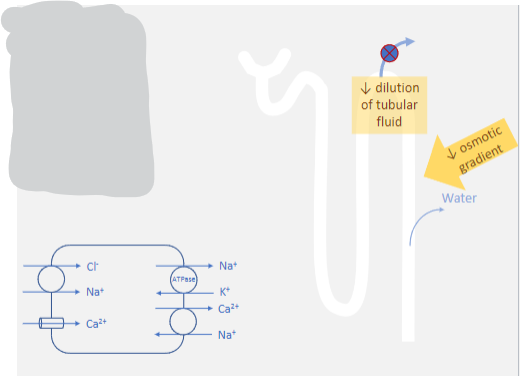
★Inhibiting this cotransporter impedes the dilution of tubular fluid, leading to a reduced osmotic drive for ADH-mediated water reabsorption.
-
What are some common side effects of thiazide diuretics? (2)
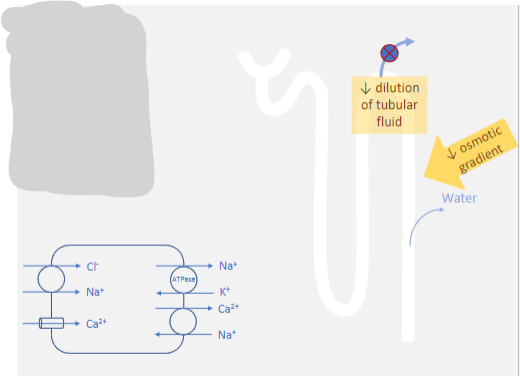
Thiazide diuretics can cause:
★Significant loss of potassium, resulting in hypokalemia.
★Hypercalcemia due to increased Ca/Na exchanger activity.
-
What is the diuretic action of potassium-sparing diuretics? (1)
★Potassium-sparing diuretics have a weak diuretic action.
-
What is the importance of potassium-sparing diuretics? (1)
★They are important because they cause potassium retention, countering the powerful electrolyte secretions of loop diuretics.
-
Where do potassium-sparing diuretics act in the kidney? (1)
★Potassium-sparing diuretics act at the end of the distal convoluted tubule (DCT) and collecting duct.
-
What are examples of potassium-sparing diuretics and how do they work? (2)
★Amiloride blocks the epithelial sodium channel (ENaC).
★Spironolactone is an aldosterone antagonist, preventing the actions of aldosterone.
-
What are the uses of thiazide diuretics? (4)
★Thiazide diuretics have been historically used as first-line treatment for hypertension.
★While no longer first-line treatment according to NHS guidelines, they may still be used as second or third-line options.
★Low doses of thiazides are effective for treating hypertension.
★Higher doses may be used for managing volume overload conditions such as mild to moderate heart failure.
-
What are the uses of loop diuretics? (1)
★Loop diuretics are used for managing severe volume overload conditions such as pulmonary edema due to left ventricular failure.
-
What are the uses of potassium-sparing diuretics? (3)
★Potassium-sparing diuretics may be used to supplement thiazide or loop diuretics to counteract hypokalemia.
★They are also used in the management of heart failure.
★Aldosterone antagonists, a type of potassium-sparing diuretic, may be used to control hyperaldosteronism.
-
What are sodium-glucose cotransporters (SGLTs)? (1)

★Sodium-glucose cotransporters (SGLTs) are proteins involved in secondary active transport.
-
Where are SGLT1 and SGLT2 found, and what are their functions? (1)

★SGLT1 is found in the gut and is responsible for glucose absorption from the gut.
★SGLT1 and SGLT2 are both found in the kidney, particularly in the proximal convoluted tubule (PCT), and are responsible for glucose reabsorption from the kidney filtrate.
-
How do SGLT-2 inhibitors work, and what condition are they used to treat? (2)

★SGLT-2 inhibitors are used to treat hyperglycemia by impairing glucose reabsorption in the kidney.
★By inhibiting SGLT-2, more glucose remains in the tubular fluid, which lowers its concentration in the plasma.
-
What is the result of impaired glucose reabsorption by SGLT-2 inhibitors? (1)

★Impaired glucose reabsorption leads to a mild osmotic diuresis, contributing to their mild diuretic action.

