
Depression (Physiology 2)
Depression - Dr Alexis Bailey Lecture Outline Major depression and bipolar depressive are affective mental health disorders or disorders of mood. There are several theories concerning the biological basis for depression including the monoamine and the neuroendocrine (diathesis-stress hypothesis) theories. Several treatment methods are available for the management of depression including electroconvulsive therapy (ECT), psychotherapy and antidepressant. Antidepressants include tricyclic antidepressants, SSRIs, noradrenaline/5HT reuptake inhibitors and monoamine oxidase inhibitors. For bipolar depression, lithium and sodium valproate is the usual means of treatment. Desired Learning Outcomes By the end of this lecture, students should be able to: 1. Outline the symptoms and the diagnostic criteria for depression 2. Explain the existing theories describing the biological basis of depression 3. Describe the pharmacotherapy available for the treatment of depression 4. Discuss the pharmacological action (mechanism of action) of common antidepressants 5.Future in depression treatment Session Resources Introduction to mental Illness slides (see below for precorded 6min min video of these slides)Download Introduction to mental Illness slides (see below for precorded 6min min video of these slides) Depression lecture slidesDownload Depression lecture slides Session Activities Before we start discussing the neurobiology of depression i just wanted to do a short (6 min) introduction on the neuroscience of mental illness which you can view below. Panopto recording available after the session Quiz time Quiz time. Test your knowledge by carrying out this QUIZLinks to an external site. and this QUIZLinks to an external site. Further Reading 'Neuroscience: Exploring the Brain' by Bear, Connors, Paradiso Chapter 22 'Pharmacology Condensed' by Dale and Haylett Chapter 40 Rang & Dale’s Pharmacology, 8th Edition (Elsevier): Chapters 47 Glossary Affective disorders – They are a set of psychiatric disorders, also called mood disorders. The main types of affective disorders are depression and bipolar disorders Major depression – Major depressive disorder (MDD), is a mental disorder characterized by at least two weeks of low mood that is present across most situations. It is often accompanied by low self-esteem, loss of interest in normally enjoyable activities, low energy, and pain without a clear cause. Monoamine hypothesis of affective disorders – Predicts that the underlying pathophysiologic basis of depression involves deficits of in the levels of serotonin, noradrenaline and/or dopamine in the central nervous system. Diathesis-stress hypothesis of affective disorders – Suggests that exaggerated or hypersensitivity of the hypothalamic-pituitary-adrenal axis is at the centre of the neurobiology of this disorder Electroconvulsive therapy (ECT) – Procedure, done under general anaesthesia, in which small electric currents are passed through the brain, intentionally triggering a brief seizure. ECT seems to cause changes in brain chemistry that can quickly reverse symptoms of certain mental illnesses.
-
What is the major cause of premature death and disability? (1)
Depression
-
What percentage of UK adults reported that their mental health was either bad or the worst it’s ever been in 2024, compared to pre-pandemic levels? (2)
More than 1 in 7 adults reported poor mental health in 2024.
This is an increase from 1 in 10 adults pre-pandemic.
-
What is the difference in mental health struggles between women and men in the UK? (2)
18.5% of women are struggling with poor mental health.
12.5% of men are struggling with poor mental health.
-
How much did the NHS spend on mental health services in England, and what percentage of the total NHS budget did this account for? (2)
The NHS spent £12 billion on mental health services in England.
This accounts for approximately 8% of the total NHS budget.
-
What are affective disorders, and how are they characterized? (2)
Disorders of mood rather than thought or cognition.
The most common affective disorder is depression.
-
What is Unipolar Depression and what are its characteristics? (3)
Mood swings in one direction (depression).
The most common depressive illness.
75% of cases are reactive (induced by environmental factors), and 25% are endogenous (genetic).
-
What is Bipolar Depression and what are its characteristics? (3)
Oscillation between depression and mania.
Mania symptoms include excessive exuberance, enthusiasm, self-confidence, impulsive actions, aggression, irritability, and delusions of grandeur.
-
What are the types of Bipolar Depression? (2)
Type I: More mania episodes, with or without depression (1% of the population).
Type II: Hypomania and always episodes of major depression (0.6% of the population).
-
What is the usual onset of Bipolar Depression and its hereditary tendency? (2)
Onset usually occurs in adult life.
There is a strong hereditary tendency, though no specific genes have been identified yet.
-
What are the key criteria for a Major Depressive Episode according to DSM V? (3)
Five (or more) symptoms must be present during the same 2-week period.
At least one symptom must be either (1) depressed mood or (2) loss of interest or pleasure.
Symptoms must represent a change from previous functioning.
-
What symptoms should not be included when diagnosing Major Depressive Episode? (2)
Symptoms that are clearly due to a general medical condition.
Mood-incongruent delusions or hallucinations.
-
What are the 8 symptoms of Major Depressive Episode as per DSM V? (8)
Depressed mood most of the day, nearly every day (in children, irritable mood).
Markedly diminished interest or pleasure in all, or almost all, activities most of the day.
Significant weight loss when not dieting, weight gain, or decrease/increase in appetite nearly every day.
A slowing down of thought and physical movement (observable by others).
Fatigue or loss of energy nearly every day.
Feelings of worthlessness or excessive/inappropriate guilt nearly every day.
Diminished ability to think or concentrate, or indecisiveness, nearly every day.
Recurrent thoughts of death, recurrent suicidal ideation without a specific plan, or a suicide attempt or specific plan for committing suicide.
-
What are the emotional symptoms of depression according to the ICD-10? (4)
Apathy, pessimism, and negativity.
Low self-esteem and feeling guilty.
Loss of motivation.
Indecisiveness.
-
What are the biological symptoms of depression according to the ICD-10? (4)
Reduced activity.
Loss of libido.
Sleep disturbance.
Loss of appetite.
-
What are some general medical conditions in which depression is often found? (7)
Terminal illness.
Chronic illness (e.g., chronic pain).
Thyroid dysfunction.
Neurological disease.
Stroke.
Drug abuse.
Parkinson’s disease.
-
What is another common co-morbidity with depression? (1)
Anxiety.
-
What is the Monoamine Theory of Depression and who proposed it? (2)

The Monoamine Theory suggests that depression is caused by reduced activity of central noradrenergic and/or serotonergic systems.
Proposed by Schildkraut in 1965.
-
What is the evidence supporting the Monoamine Theory of Depression? (3)
Reduced activity of central noradrenergic and/or serotonergic systems.
Reserpine depletes the brain of norepinephrine (NA) and serotonin (5-HT), inducing depression.
The main antidepressant drugs increase the levels of amines (norepinephrine and serotonin) in the brain.
-
What is the evidence against the Monoamine Theory of Depression? (5)
It is difficult to show consistent deficits in brain levels of norepinephrine (NA) and serotonin (5-HT) in depressed individuals.
Depressed individuals respond better to some antidepressants than others, even if they affect amines differently.
Most antidepressant drugs take several weeks to show therapeutic effects, but they increase amines acutely, suggesting that secondary adaptive changes are more important.
Some antidepressants, like trazodone, have weak or no effect on amine uptake, yet still show antidepressant effects.
Cocaine blocks amine uptake but does not have an antidepressant effect.
-
What is the relationship between serotonin (5-HT) and aggression in bipolar disorder according to the evidence against the Monoamine Theory? (1)
A decrease in serotonin (5-HT) in bipolar disorder is linked to aggression rather than depression.
-
What is the main finding from serotonin research regarding its association with depression? (2)
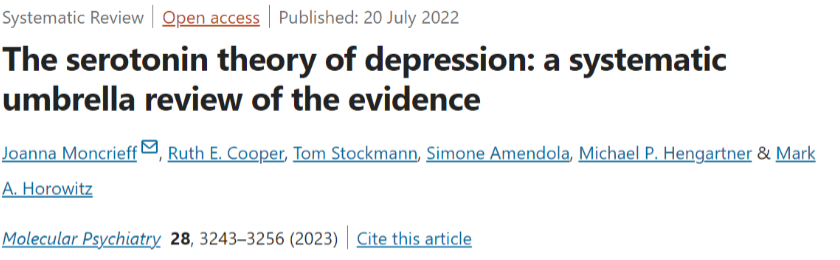
There is no consistent evidence supporting an association between serotonin and depression.
The hypothesis that depression is caused by lowered serotonin activity or concentrations is not supported.
-
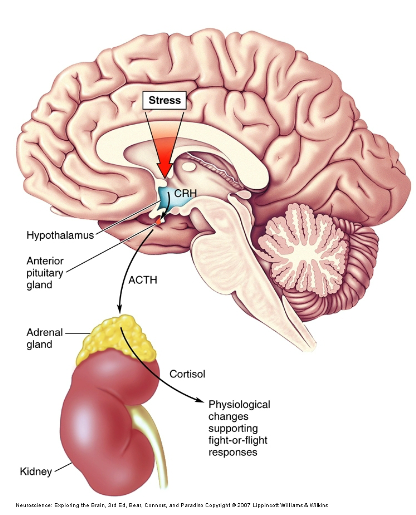
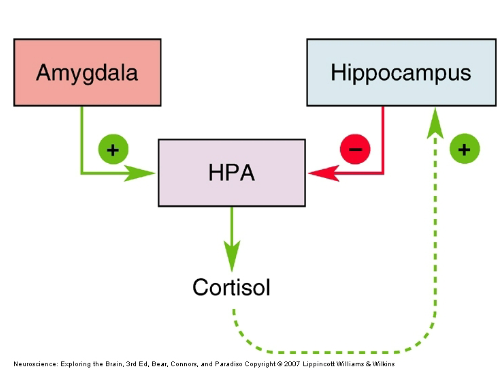
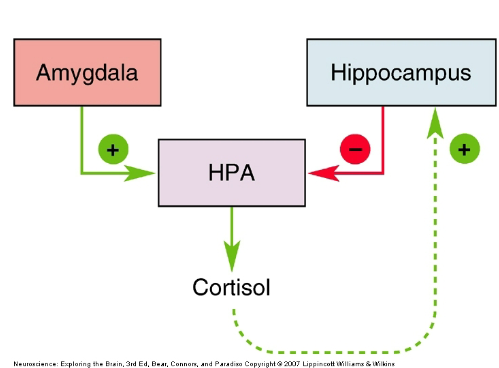
What is the basic mechanism proposed in the Neuroendocrine Theory of Depression? (5)
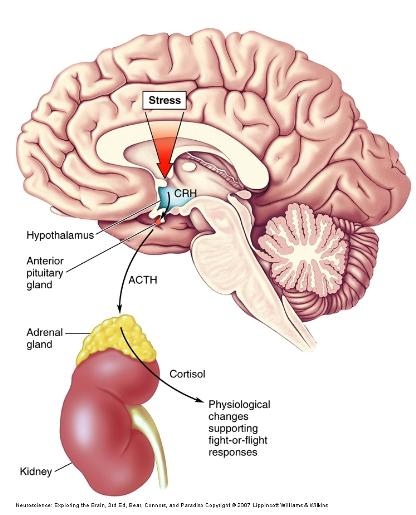
Noreadrenergic (NAergic) and serotonergic (5-HT) neurons input to the hypothalamus.
The hypothalamus releases corticotropin-releasing hormone (CRH).
CRH acts on the pituitary gland to release adrenocorticotrophic hormone (ACTH).
ACTH triggers the release of cortisol from the adrenal cortex.
Cortisol is released in response to increased ACTH in the blood.
-
What would you expect in response to an increase in cortisol? (1)
Increased cortisol can lead to various physiological changes, such as altered stress responses, immune suppression, and potential effects on mood and behavior.
-
What are the key aspects of the Neuroendocrine Theory of Depression? (3)
Corticotropin-releasing hormone (CRH) has behavioral effects that mimic some symptoms of depression.
There is evidence of hyperactivity of the hypothalamic-pituitary-adrenal (HPA) axis in depressed patients.
Increased plasma cortisol and increased CRH levels in cerebrospinal fluid are observed in depressed individuals.
-
How do genes and the environment contribute to hyperactivity in the HPA axis according to the Neuroendocrine Theory? (2)
Both genetic factors and environmental influences can contribute to HPA axis hyperactivity.
This interaction between genes and environment may help explain how certain individuals are predisposed to mental health conditions, also known as the diathesis-stress model.
-
What are the key neuroendocrine changes observed in depression according to the Neuroendocrine Theory? (2)

Reduced hippocampal feedback in depression.
Reduced glucocorticoid receptors (cortisol receptors) in the hippocampus.
-
How is glucocorticoid receptor gene expression regulated according to the Neuroendocrine Theory? (2)
Glucocorticoid receptor gene expression is regulated by early experiences.
Tactile stimulation just after birth activates serotonin (5-HT) pathways to the hippocampus, which then triggers a long-lasting increase in glucocorticoid receptor gene expression.
-
What is the effect of SSRIs on glucocorticoid receptors in the hippocampus? (1)
Selective serotonin reuptake inhibitors (SSRIs) increase the expression of glucocorticoid receptors in the hippocampus.
-
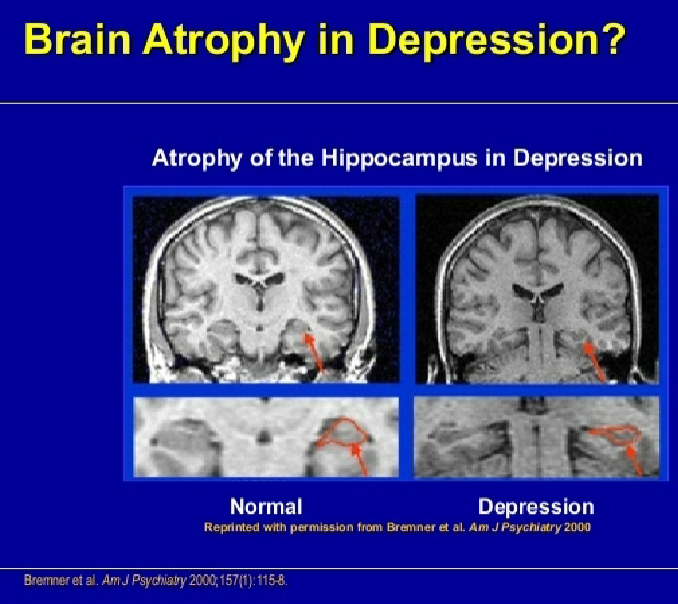
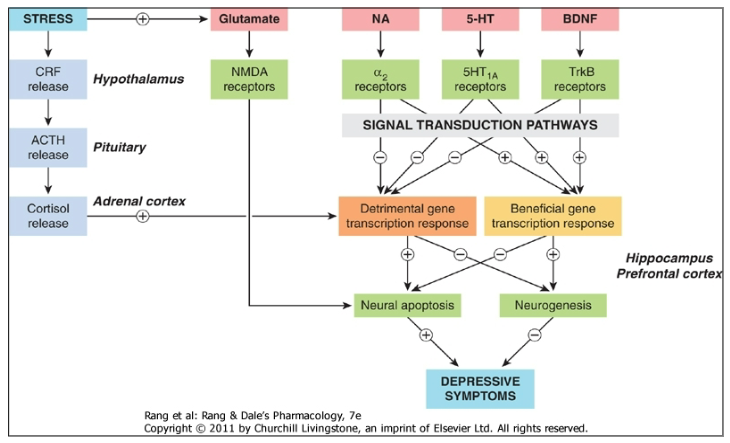
What is the role of neuroplasticity and neurogenesis in depression? (3)
Evidence suggests neuronal loss and reduced neuronal activity in the hippocampus and prefrontal cortex, areas involved in decision-making.
Antidepressants and electroconvulsive therapy (ECT) promote neurogenesis in these regions.
Serotonin (5-HT) promotes neurogenesis during development via brain-derived neurotrophic factor (BDNF).
-
How does glutamate relate to depression according to recent theories? (2)
There is an increase in glutamate in the cortex of depressed individuals.
NMDA antagonists, such as ketamine, show potential for treating depression.
-
What other factors are implicated in depression beyond the neuroplasticity and neurogenesis theories? (2)
Oxidative stress and neuroinflammation.
The gut-brain microbiota axis.
-
How do imbalances in neurotransmitters contribute to depression according to the extended Monoamine Theory? (4)
Imbalances between neurotransmitters (e.g., Monoamines, Dopamine (DA), Acetylcholine (Ach), Corticotropin-releasing factor (CRF), Cortisol (CORT), etc.) lead to long-term alterations in gene expression.
These imbalances cause upregulation of serotonin (5-HT) and norepinephrine (NA) receptors.
The hypothalamic-pituitary-adrenal (HPA) axis becomes hyperfunctional.
Some neuronal loss occurs as a result of these imbalances.
-
Picture demonstrating brain atrophy in depression:
-
Picture demonstrating Pathophysiology of depression:
-
What is the role of Cognitive Behavioral Therapy (CBT) in the treatment of depression? (2)

CBT focuses on changing negative thought patterns and behaviors that contribute to depression.
It aims to improve emotional regulation and develop coping strategies.
-
What are the main pharmacotherapy options for treating depression? (3)

Antidepressants, including SSRIs (Selective Serotonin Reuptake Inhibitors), are commonly prescribed to increase serotonin levels.
Other types of antidepressants include SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors) and TCAs (Tricyclic Antidepressants).
MAOIs (Monoamine Oxidase Inhibitors) are sometimes used but less commonly due to dietary restrictions and side effects.
-
What is the focus of Cognitive Behavioral Therapy (CBT) in treating depression? (2)
CBT helps individuals recognize and change negative cognitive processes.
The goal is to improve mood and counterproductive behaviors by addressing thought patterns.
-
What does Interpersonal Therapy (IPT) emphasize in the treatment of depression? (2)
IPT assumes that depression is multifactorial, with interpersonal difficulties playing a central role.
The therapy aims to address and improve interpersonal relationships, which can help alleviate depressive symptoms.
-
What is the controversy surrounding the effectiveness of SSRIs in treating depression? (2)

Despite millions of prescriptions being written for SSRIs in the UK, a major study found that SSRIs are no more effective than a placebo in treating depression.
This raises questions about the true efficacy of SSRIs for many individuals and the implications for treatment strategies.
-
What are the types of antidepressants and their neurochemical effects? (6)
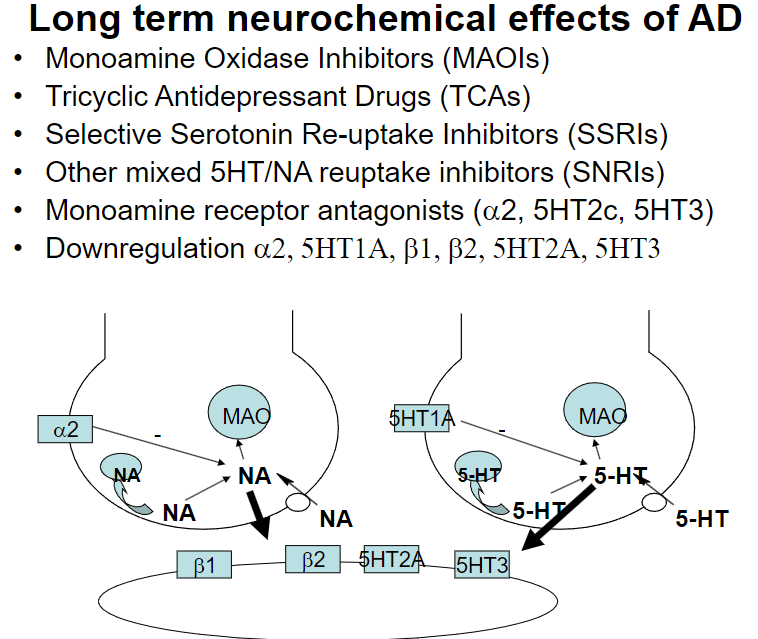
MAOIs: Inhibit breakdown of serotonin, norepinephrine, and dopamine.
TCAs: Block reuptake of serotonin and norepinephrine, increasing their levels.
SSRIs: Inhibit serotonin reuptake, boosting its availability.
SNRIs: Block reuptake of serotonin and norepinephrine.
Monoamine Receptor Antagonists (α2, 5HT2c, 5HT3): Block receptors that regulate neurotransmitter release.
Downregulation: Long-term use leads to reduced sensitivity of receptors like α2, 5HT1A, β1, β2, 5HT2A, and 5HT3.
-
What are the main pharmacological treatments for depression and their effects? (4)
Tricyclic Antidepressants (TCAs): Block reuptake of serotonin and norepinephrine.
Monoamine Oxidase Inhibitors (MAOIs): Inhibit the breakdown of neurotransmitters like serotonin, norepinephrine, and dopamine.
Selective Serotonin Reuptake Inhibitors (SSRIs): Specifically inhibit serotonin reuptake in the synapse, with fewer side effects.
NICE Guidelines: Recommend SSRIs as the first-line pharmacological treatment for depression due to their selectivity and fewer side effects.
-
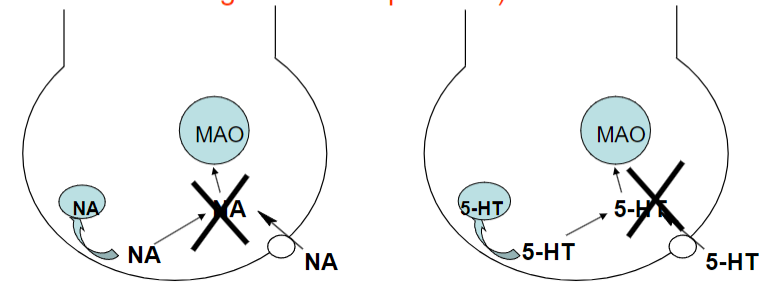
What is the pharmacological effect of Monoamine Oxidase Inhibitors (MAOIs)? (3)
![Increase [NA/5-HT] in cytoplasm: MAOIs prevent the breakdown of norepinephrine (NA) and serotonin (5-HT), increasing their concentration in the cytoplasm.Increase leakage of amines: Elevated cytoplasmic concentrations lead to more amine release.Increase [NA/5-HT] in synaptic cleft: The increased amine release results in higher levels of NA and 5-HT in the synaptic cleft, enhancing neurotransmission.](/flashcards/cardimage2/574fe81c/808/8808627_back.png)
Increase [NA/5-HT] in cytoplasm: MAOIs prevent the breakdown of norepinephrine (NA) and serotonin (5-HT), increasing their concentration in the cytoplasm.
Increase leakage of amines: Elevated cytoplasmic concentrations lead to more amine release.
Increase [NA/5-HT] in synaptic cleft: The increased amine release results in higher levels of NA and 5-HT in the synaptic cleft, enhancing neurotransmission.
-
What are the effects of Monoamine Oxidase Inhibitors (MAOIs)? (5)
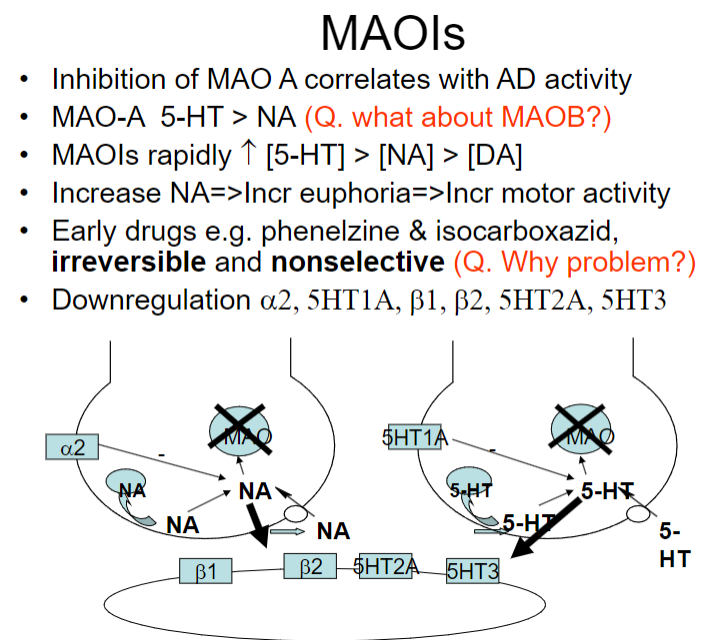
Inhibition of MAO-A: Inhibiting MAO-A is linked to antidepressant (AD) activity, as it affects serotonin (5-HT) more than norepinephrine (NA).
Effect on neurotransmitters: MAOIs rapidly increase 5-HT > NA > dopamine (DA) levels.
Increase in NA: Leads to euphoria and increased motor activity.
Early drugs (e.g., phenelzine, isocarboxazid): Irreversible and nonselective, which can be problematic due to side effects and interactions (e.g., with tyramine).
Downregulation: MAOIs cause downregulation of receptors like α2, 5HT1A, β1, β2, 5HT2A, and 5HT3.
-
What are the food and drug interactions associated with Monoamine Oxidase Inhibitors (MAOIs)? (4)
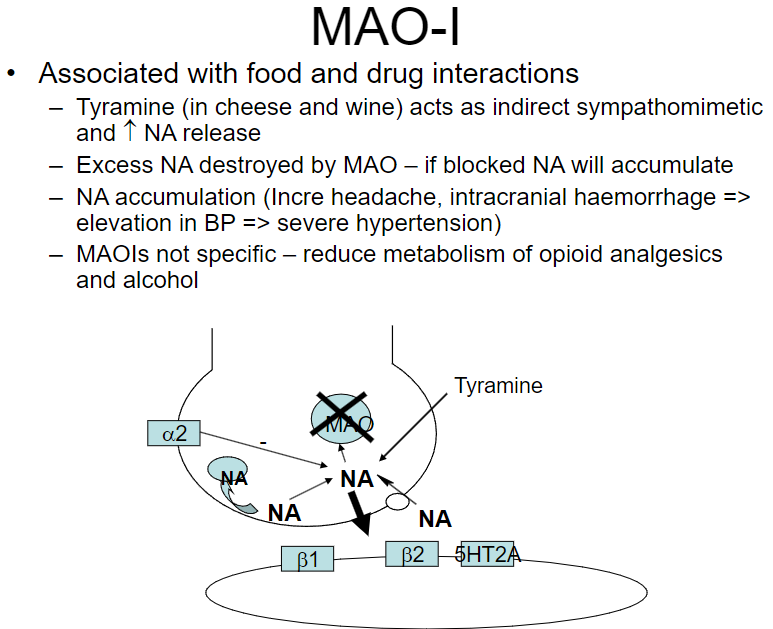
Tyramine (in cheese and wine): Acts as an indirect sympathomimetic, increasing norepinephrine (NA) release.
NA accumulation: When MAO is blocked, excess NA accumulates, potentially leading to severe consequences.
Health risks: Accumulation of NA can result in headaches, intracranial hemorrhages, and severe hypertension.
Other interactions: MAOIs reduce the metabolism of opioid analgesics and alcohol, potentially increasing their effects.
-
What are the features of Reversible MAOIs (RIMAs) such as moclobemide? (3)
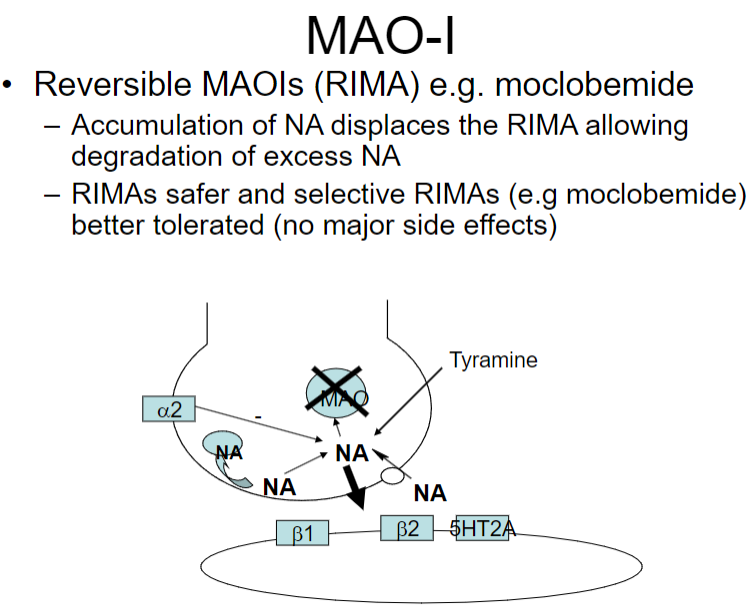
Action: Accumulation of norepinephrine (NA) displaces the RIMA, allowing degradation of excess NA.
Safety: RIMAs are safer compared to irreversible MAOIs due to their selective action.
Tolerance: RIMAs like moclobemide are better tolerated and generally cause no major side effects.
-
What is the 'cheese effect' associated with MAOIs and how does it occur? (4)

MAO inhibition in gut: MAO in the gut is inhibited by MAOIs, preventing the breakdown of dietary amines.
Tyramine accumulation: Tyramine from foods like cheese, yogurt, meat, wine, and yeast products can enter the bloodstream.
Indirect sympathomimetic action: Tyramine acts as an indirect sympathomimetic, displacing norepinephrine from vesicles.
Health risk: The accumulation of norepinephrine can lead to severe hypertension.
-
What are the main therapeutic effects and actions of Tricyclic Antidepressants (TCAs)? (5)
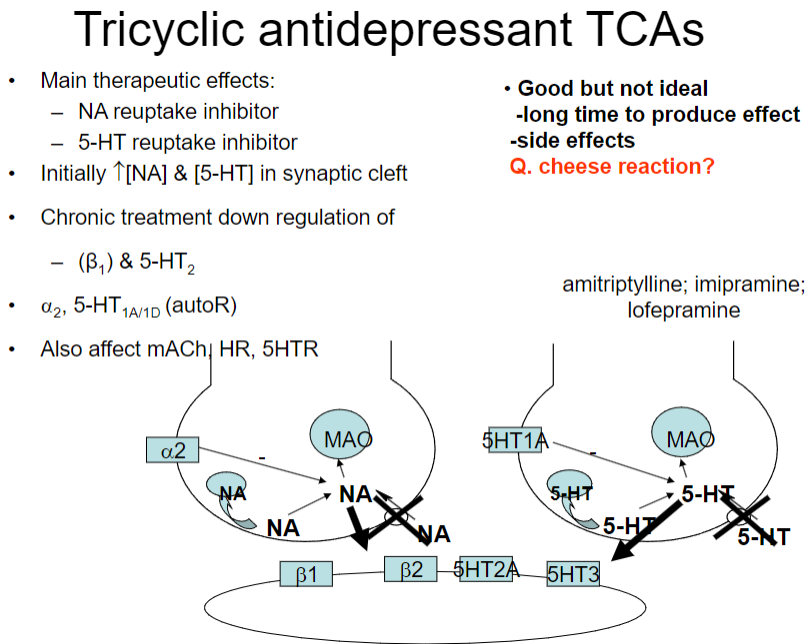
NA reuptake inhibitor: TCAs inhibit the reuptake of norepinephrine (NA).
5-HT reuptake inhibitor: TCAs also inhibit the reuptake of serotonin (5-HT).
Initial effect: Leads to an increase in the concentration of NA and 5-HT in the synaptic cleft.
Chronic treatment: Results in the downregulation of β1 and 5-HT2 receptors.
Additional effects: TCAs also affect α2, 5-HT1A/1D (autoreceptors), muscarinic acetylcholine receptors (mACh), heart rate (HR), and 5-HT receptors.
-
What are the differences between Desipramine and Imipramine? (3)
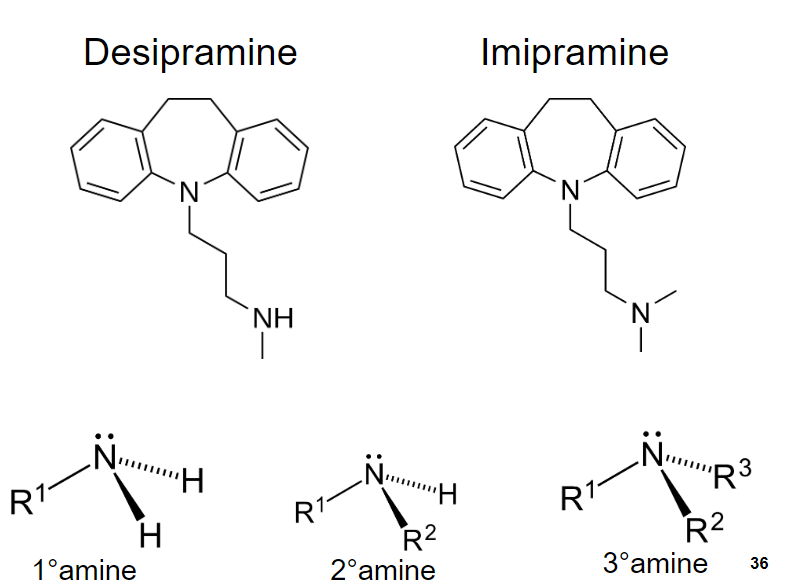
Desipramine: A secondary amine TCA.
Imipramine: A tertiary amine TCA.
Effect on receptors: Desipramine is more selective for norepinephrine (NA) reuptake inhibition, while imipramine has a broader spectrum of action, affecting both serotonin (5-HT) and norepinephrine reuptake.
-
How do TCAs affect neurotransmitter (NT) levels and receptors in the brain? (3)
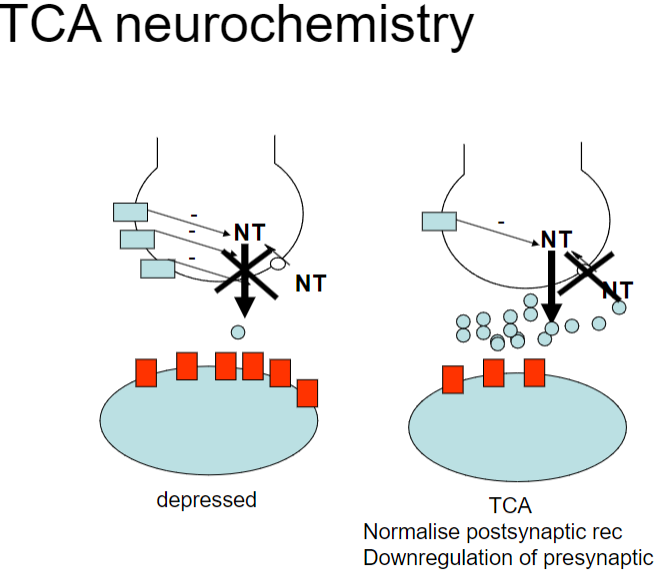
NT in depression: Imbalance in neurotransmitters (e.g., serotonin, norepinephrine) is linked to depression.
TCA action: TCAs inhibit the reuptake of serotonin (5-HT) and norepinephrine (NA), increasing their availability in the synaptic cleft.
Receptor effects: TCAs lead to downregulation of presynaptic receptors (e.g., α2, 5-HT1A) and normalization of postsynaptic receptors, contributing to improved mood and function.
-
What are the main therapeutic effects of SSRIs, and what are their side effects? (3+3)
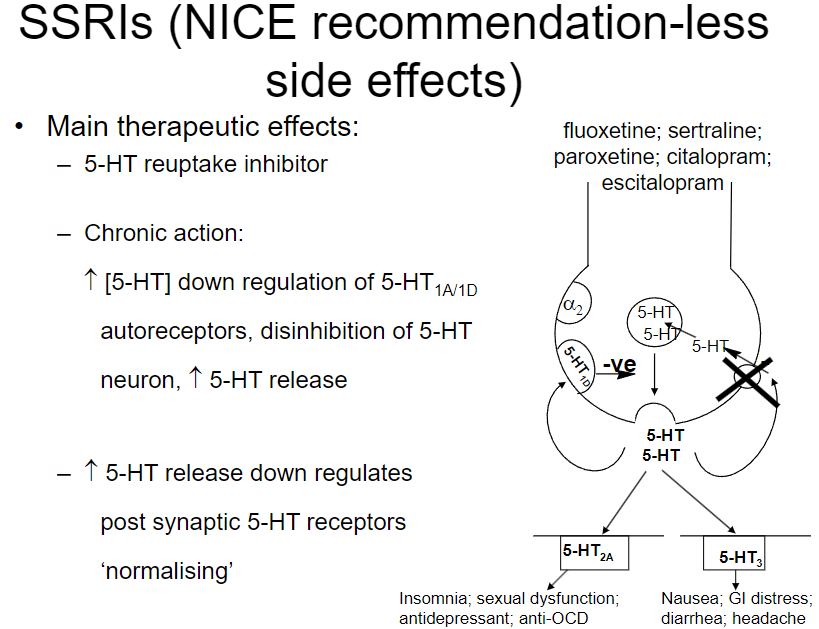
Main effects:
5-HT reuptake inhibition: Increases serotonin (5-HT) levels in the synapse.
Chronic action: Leads to downregulation of 5-HT1A/1D autoreceptors, disinhibiting serotonin neurons and enhancing serotonin release.
Normalization: Chronic increase in serotonin causes the downregulation of postsynaptic 5-HT receptors.
Common SSRIs: Fluoxetine, sertraline, paroxetine, citalopram, escitalopram.
Side effects:
GI distress: Nausea, diarrhea, headache.
Sleep disturbances: Insomnia.
Sexual dysfunction: Common with SSRIs.
-
Explain the neurochemistry of SSRIs and their effects on serotonin receptors. (3)
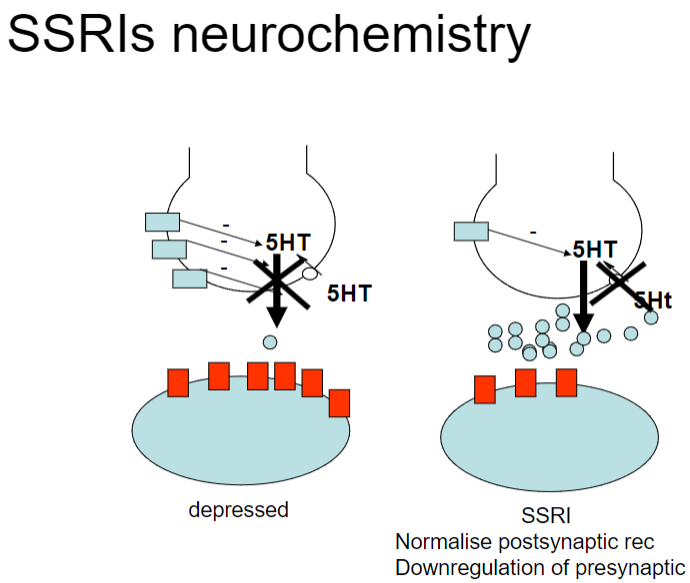
SSRI Mechanism:
Inhibition of serotonin reuptake (5-HT): Increases serotonin (5-HT) concentration in the synapse.
Normalization of postsynaptic receptors: Chronic increase in 5-HT leads to downregulation of presynaptic 5-HT1A/1D autoreceptors.
Disinhibition of serotonin neurons: This downregulation enhances serotonin release, ultimately normalizing postsynaptic receptor activity.
-
Describe the mechanism of action of Mirtazapine (NASSA) and its advantages. (4)
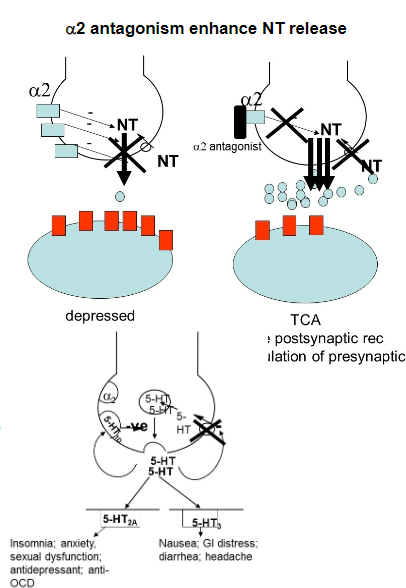
a2 Antagonist:
Increases release of noradrenaline (NA) and serotonin (5-HT).
5-HT Receptor Activity:
Potent antagonist of 5-HT2 and 5-HT3 receptors.
Advantages:
Faster onset than SSRIs.
Lacks side effects associated with 5-HT2 and 5-HT3 receptor antagonism (e.g., nausea, sexual dysfunction).
-
Describe the mechanism, clinical use, and advantages of Ketamine as an antidepressant. (7)
Mechanism of Action:
NMDA receptor antagonist that modulates glutamate signaling.
Promotes synaptic plasticity and rapid neuronal connections, particularly in the prefrontal cortex.
Clinical Use:
Approved for treatment-resistant depression (TRD) in some countries.
Administered via intravenous infusion or intranasal spray.
Onset of Action:
Rapid effect (within hours), much faster than traditional antidepressants that take weeks.
Advantages:
Effective when other treatments fail.
Reduces suicidal ideation quickly.
-
Discuss the problems associated with antidepressants. (6)
Side effects:
Insomnia and other side effects that can lead to relapse.
Toxicity:
Potentially toxic in overdose situations.
Delayed effects:
Most antidepressants take several weeks to show therapeutic effects.
Non-responsiveness:
About 30-40% of patients fail to improve with drug treatment.
Pharmacogenetics:
Variations in P450 enzymes and SERT polymorphisms can affect SSRI effectiveness.
Variable efficacy:
While more efficacious than placebo, some individuals respond better to certain types of antidepressants.
-
What are affective disorders and their main types? (4)
Affective disorders are psychiatric disorders also known as mood disorders.
The main types include:
Depression
Bipolar disorders
-
Describe major depression (MDD). (5)
MDD is characterized by at least two weeks of low mood across most situations.
Often accompanied by:
Low self-esteem
Loss of interest in enjoyable activities
Low energy
Pain without a clear cause
-
Explain the monoamine hypothesis of affective disorders. (4)
The hypothesis predicts that depression results from deficits in serotonin, noradrenaline, and/or dopamine levels in the central nervous system.
-
What is the diathesis-stress hypothesis of affective disorders? (3)
It suggests that hypersensitivity or exaggerated sensitivity of the hypothalamic-pituitary-adrenal (HPA) axis plays a central role in the neurobiology of affective disorders.
-
What is electroconvulsive therapy (ECT)? (3)
ECT involves passing small electric currents through the brain under general anaesthesia.
The procedure causes a brief seizure and seems to induce changes in brain chemistry.
It is used to quickly reverse symptoms of certain mental illnesses.

