Control of Cardiac Output (Physiology)
Session Summary This lecture is about two important parameters that control cardiac output, preload and afterload. These parameters are summarized by Starling’s law and Laplace’s law. Changing preload and afterload are fundamental in treating cardiac diseases and this is the theoretical underpinning of these ideas. Learning outcomes At the end of this session you will be able to: • Outline of mechanisms involved in controlling stroke volume & cardiac output • Describe energy of contraction • Understand preload - Starling’s Law • Understand afterload - Laplace’s Law • Consider effect of arterial blood pressure on stroke volume • Consider effect of venous return and systemic blood pressure changes on ventricular pressure-volume loop curves
-
What is Hypertrophic Cardiomyopathy?
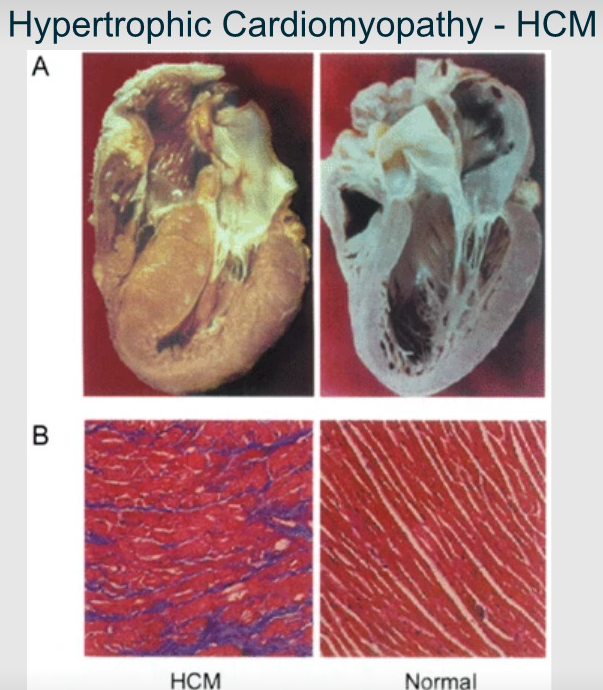
Is a genetic heart condition where the heart muscle becomes abnormally thick (hypertrophied), making it harder for the heart to pump blood effectively
-
What does BP stand for?
Blood Pressure
-
What does TPR stand for?
Total Peripheral Resistance
-
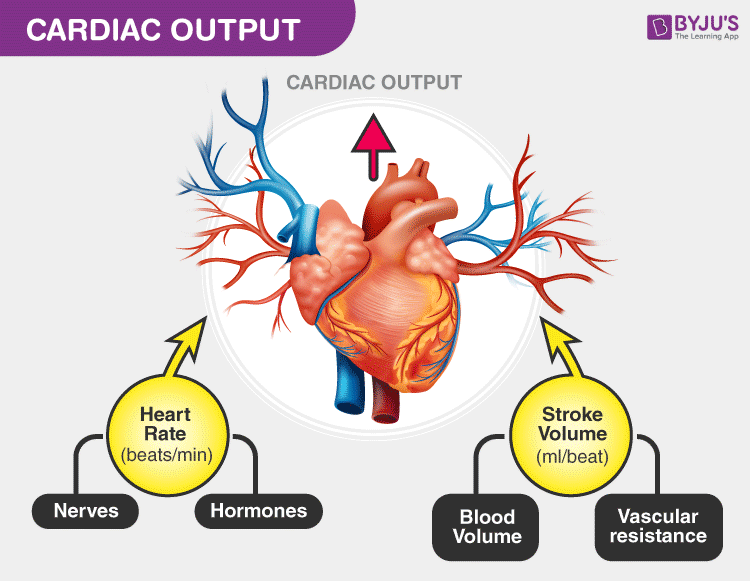
What is cardiac output (CO) defined as?
The amount of blood ejected from the heart per minute
-
What is the equation for Cardiac output?
CO = HR x SV
-
What is the equation for BP?
BP = CO x TPR
-
The strength of heart contraction is due to what type of nerves? And circulation of a specific neurotransmitter which increases intracellular calcium
-Sympathetic nerves
-Circulating adrenaline
-
What is preload?
-Stretching of the heart at rest
-Increases stroke volume due to Starling's Law
-
What is Afterload?
-Opposes ejection
-Reduces stroke volume due to Laplace's Law
-
Afterload tends to be associated with what?
Arterial pressure
-
Energy of contraction of cardiac muscle is relative to....
The muscle fibre length at rest
-
A Greater stretch of ventricle in diastole (blood entering) allows for....
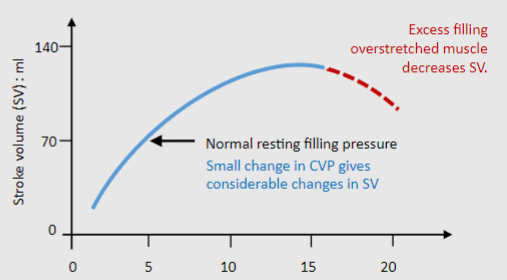
A greater energy of contraction and greater stroke volume achieved in systole
-
more blood in = more blood out
is not an intrinsic property of the cardiac muscle
Is this true?
FALSE
It is an intrinsic property of the cardiac muscle
-
What are 3 characteristics of an un-stretched fibre?
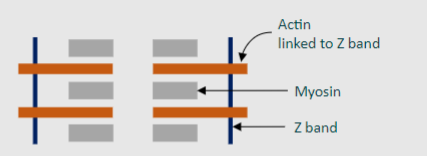
-Overlapping actin/myosin-Mechanical interference-Less cross-bridge formation available for contraction
-
What are 4 characteristics of a stretched fibre?
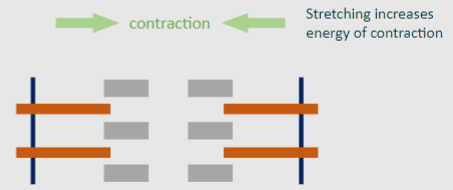
-Less overlapping actin/myosin-Less mechanical interference-Potential for more cross-bridge formation-Increased sensitivity to Ca2+ ions
-
What are 5 reasons why Preload is important (roles and effects of Starling's Law)
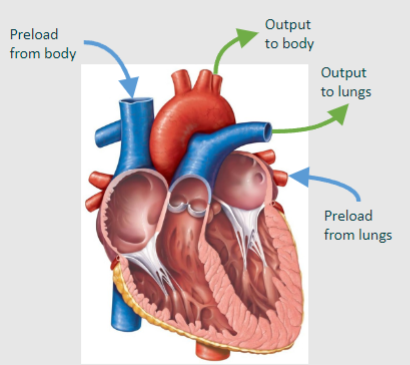
•Balances outputs of the right ventricle and left ventricle – important
• Responsible for fall in cardiac output during a drop in blood volume or vasodilation (e.g. haemorrhage, sepsis)
• Restores cardiac output in response to intravenous fluid transfusions
• Responsible for fall in cardiac output during orthostasis (standing for a long time) leading to postural hypotension & dizziness as blood pools in legs.
• Contributes to increased stroke volume & cardiac output during upright exercise
-
Afterload opposes the contraction that ejects blood from the heart and is determined by....?
Wall stress
-

More energy of contraction is need to overcome this wall stress to produce cell shortening and ejection.
Laplace’s law describes parameters that determine afterload through the equation:
What does T, P and r mean?
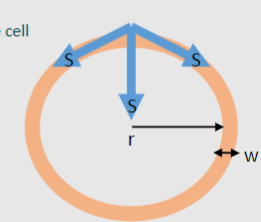
Wall tension (T), pressure (P), and radius (r) in a chamber (ventricle)
-

Wall stress (S) is made up of Tension (T) over wall thickness (w)
Is there another equation where we can calculate wall stress?

-
Afterload is increased by what? (2)
-Increasing pressure
-Increasing radius
-
Afterload is reduced by what? (1)
-Increasing wall thickness
-
How does a small ventricle radius affect wall stress/afterload?

• Greater wall curvature
• More wall stress directed towards centre of chamber
• Less afterload
• Better ejection
-
How does a Large ventricle radius affect wall stress/afterload?
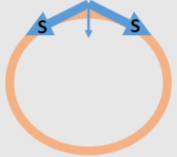
• Less wall curvature
• More wall stress directed through heart wall
• More afterload
• Less ejection
-
How does a huge theoretical radius affect wall stress/afterload?

• Negligible wall curvature
• Virtually all stress directed through wall
-
One of the reasons why Laplace's law is important is because it Opposes Starling’s law at rest
Elaborate on why? (3)
-Increased preload gives increased stretch of chamber (Starling’s law)
-This increases chamber radius (decreases curvature) therefore increasing afterload-In a healthy heart, Starling’s Law overcomes Laplace’s therefore ejection is OK
-
One of the reasons why Laplace's law is important is because it Facilitates ejection during contraction
Elaborate on why? (2)
-Contraction reduces chamber radius so less afterload as the chamber empties
-This aids expulsion of last portion of blood and increases stroke volume
-
One of the reasons why Laplace's law is important is because it Contributes to a failing heart at rest and during contraction
Elaborate on why? (2)
-In a failing heart the chambers are often dilated and radius is large
-So increased afterload opposing ejection
-
Laplace’s Law essentially means what?
Means good ejection with small radius, bad with large radius.
-
What does Laplace's law actually state?
States that increased blood pressure (P) will increase wall stress which will increase afterload & reduce ejection
-
Acute rises in blood pressure is offset by....?
-Starling’s law
- increased stretch give increased contraction and increased stroke volume
-Local positive inotropes (noradrenaline)
-Baroreflex
-decreased sympathetic tone which decreases blood pressure
-
Chronic increase in arterial blood pressure:
Increased energy expenditure attempts to maintain stroke volume but ultimately stroke volume will......?
gradually decrease
-
A decrease in blood pressure would decrease or increase efficiency of the heart?
DECREASE
-
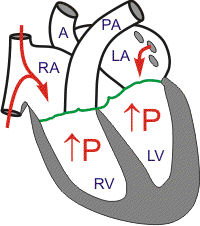
Laplace’s law & hypertrophy in heart failure
Why is increased radius (r) important in relation to this?
-eg. Heart failure where heart does not contract properly(myocardial infarction, cardiomyopathies, mitral valve re-gurgitation)
-The blood left in ventricle leading to eventual volume overload
-
Laplace’s law & hypertrophy in heart failure
Why is increased pressure (P) important in relation to this?
eg. Pressure-overload heart failure do to increasedpressure/afterload in chamber (hypertension, aortic stenosis)
-
What is ventricular hypertrophy?
A thickening of the wall of the heart's main pumping chamber
-
Increases in either radius or pressure will increase wall stress(afterload) which opposes ejection
How will the heart compensate?
What is a flaw of this compensation?
-The heart compensates with ventricular hypertrophy (greater myocyte size and more sarcomeres), increasing wall thickness
-This decreases wall stress per sarcomere and therefore afterload, so maintains SV and CO
-But this requires more energy (more sarcomeres used) and therefore greater O2
-The amount of energy required continues to increase, so ultimately contractility will decrease and produce more heart failure...it is a vicious circle
-
Stroke work carries out two functions:
State these functions
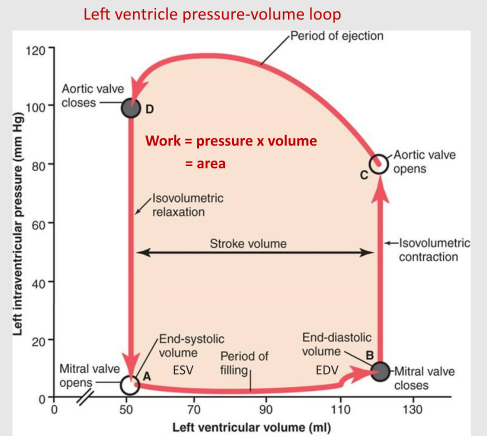
1. Contracts until chamber pressure > aortic pressure (isovolumetric contraction)
2. Ejection from ventricle
-
Preload increases the __________ _________ and afterload opposes the __________ __________
What are the missing terms?
'Stroke volume' twice
-
What does isovolumetric contraction mean?
The phase of systole when both valves are closed (and, as a result, the productive flow is zero)
-
Higher energy used in isovolumetric contraction reduces energy available for........?
Ejection
-
During exercise, there is increased preload;
Elaborate on how this is caused (relate to the ventricle)
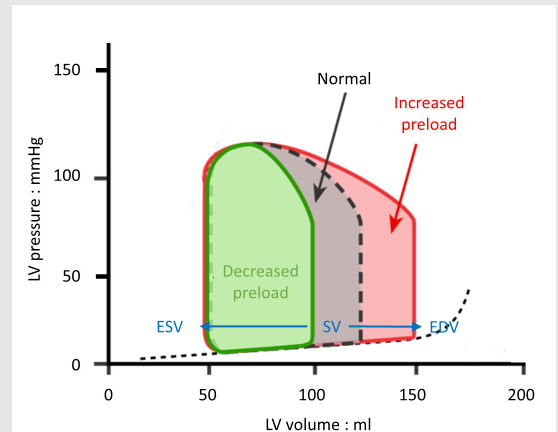
-During exercise, increased venous return leads to increased preload and higher end diastolic volume (EDV)
-The ventricle will eject blood to the same end systolic volume (ESV) so there is an increase in stroke volume, shown by an increase in the width of the PV loop
-
During hypertension, there is increased afterload;
Elaborate on how this is caused (relate to the ventricle)
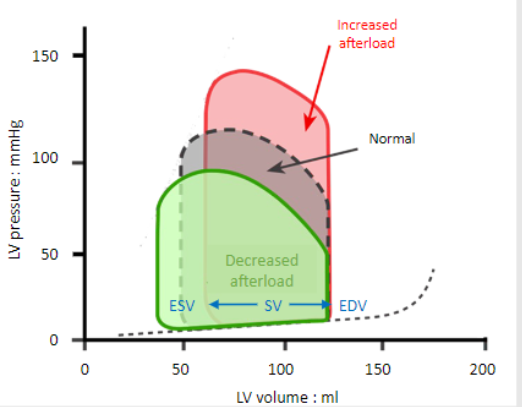
-There is a longer time spent in isovolumetric contraction to increase pressure in the chamber above that in the aorta to open the valve
-This uses more energy and lowers the force of contraction, reducing stroke volume and an increasing end-systolic volume (ESV)

