-
Spinal cord extends from and to
¾ of an inch in diameter, 16–18 in. long
Extends from foramen magnum to L1 vertebra
function: pathway for sensory and motor impulses
•reflexes
-
conus medullaris
inferior end of spinal cord
-
Cauda equina
•“Horse’s tail”—axons that extend inferiorly from spinal cord’s conus medullaris
-
Filum terminale
•Thin strand of pia mater within cauda equina that attaches conus medullaris to coccyx
-
cervical enlargement location
•the inferior cervical part of the spinal cord and innervates the upper limbs
-
lumbosacral enlargement
•extends through the lumbar and sacral parts of the spinal cord and innervates the lower limbs
-
External surface of cord has two longitudinal depressions
•Posterior median sulcus
•Anterior median fissure
-
The spinal cord is associated with 31 pairs of spinal nerves which are from:
•8 cervical nerves (C1–C8)
•12 thoracic nerves (T1–T12)
•5 lumbar nerves (L1–L5)
•5 sacral nerves (S1–S5)
•1 coccygeal nerve (Co1)
-
Epidural space
between dura and periosteum of vertebra
Epidural anesthesia is given here
-
Dura mater is different to brain because:
single meningeal layer (in contrast to double-layered dura around brain)
•Stabilizes spinal cord
•Fuses with connective tissue around spinal nerves
-
subdural space
potential space separating dura mater from deeper arachnoid mater
-
Subarachnoid space
real space filled with cerebrospinal fluid (CSF)
-
Pia mater
innermost meninx, adheres to the spinal cord
-delicate layer of elastic and collagen fibers
-Has paired, lateral triangular extensions called denticulate ligaments, anchor spinal cord laterally to the dura mater
-
The spinal cord grey and white matter is made up of:
•Gray matter: dendrites and cell bodies of neurons, unmyelinated axons, and glial cells
•White matter: Myelinated axons
-
horns of Gray Matter and what neurons they house?
Anterior horns house somas of somatic motor neurons
Lateral horns contain somas of autonomic motor neurons
-Only in T1–L2
Posterior horns contain axons of sensory neurons and cell bodies of interneurons
Gray commissure contains unmyelinated axons for communication between right and left side
-houses a narrow central canal
-
Within gray matter are functional groups of neuron cell bodies called? different kind?
called nuclei:
•Sensory nuclei in posterior horns contain interneuron cell bodies of somatic sensory nuclei and visceral sensory nuclei
•Motor nuclei in the anterior horns contain somatic motor nuclei
•Autonomic motor nuclei are in the lateral horns
-
White matter into three regions
White matter is external to spinal gray matter
Partitioned into three funiculus:
•Posterior funiculus
•Lateral funiculus
•Anterior funiculus (connected by white commissure)
Axons within each funiculus are organized into smaller structural units called tracts
-
connective tissue wrappings:
•Endoneurium
•Perineurium
•Epineurium
-
anterior roots are form by:
Multiple anterior rootlets arise from the spinal cord
•contain motor axons only
•Motor axons arise from cell bodies in the anterior and lateral horns of the spinal cord
-
posterior roots are form by:
Multiple posterior rootlets
• sensory axons only
•Sensory axons arise from cell bodies in the posterior root ganglion, which is attached to the posterior root
-
spinal nerve is
Each anterior root and its corresponding posterior root unite within the intervertebral foramen
•both motor and sensory axons
-
Nerves are numbered
- spinal nerves (C1–C7) exit the intervertebral foramen above the vertebra of the same number
•spinal nerves (C8) exit above the first thoracic vertebra
•The remaining spinal nerves exit below the vertebra of the same number
•Because the spinal cord is shorter than the vertebral canal, roots of lumbar and sacral spinal nerves travel inferiorly to reach their respective intervertebral foramen
-
rami, 2 kinds, where they innervate?
After leaving intervertebral foramen, spinal nerve splits into rami
•posterior ramus innervates deep muscles and skin of the back
•anterior ramus innervates the anterior and lateral portions of the trunk and the upper and lower limbs
-Each anterior ramus splits into multiple branches
-Many of the anterior rami form nerve plexuses
-rami communicantes, extend between the spinal nerves and the sympathetic trunk ganglia
-
dermatome is? what is not innervated?
segment of skin supplied by a single spinal nerve
•All spinal nerves except C1 innervate a segment of skin
dermatome map: Skin divided into sensory segments
•Anesthesia in a region could indicate specific spinal nerve damage
•Shingles rash -blisters along dermatome
referred visceral pain- pain in one organ is mistakenly referred to a dermatome (potentially nowhere near the organ in pain)
-
nerve plexus
network of interweaving anterior rami of spinal nerves
-The major plexuses: the cervical, brachial, lumbar, and sacral plexuses
-
intercostal nerves
Anterior rami of spinal nerves T1–T11 -spaces between adjacent ribs
Spinal nerve T12 is called a subcostal nerve, because it arises below the ribs
With the exception of spinal nerve T1, the intercostal nerves do not form plexuses
-
T1-T12 individual
-Part of T1 helps form brachial plexus; and another lies in first intercostal space
-T2 innervates intercostal muscles of the second intercostal space and is sensory for axilla and medial surface of arm
-T3–T6 innervate intercostal muscles and are sensory for the anterior chest wall
-T7–T12 innervate intercostal muscles, abdominal muscles, and overlying skin
-
Left and right cervical plexuses
formed by anterior rami of spinal nerves C1–C4
Branches of the plexus innervate anterior neck muscles, skin of the neck, and parts of the head and shoulders
-
phrenic nerve
originated primarily from C4 of C3 and C5
•Travels through the thoracic cavity to innervate the diaphragm
-
left and right brachial plexuses
-nerves that supply the upper limbs
Each plexus is formed by the anterior rami of spinal nerves C5–T1
-innervates the pectoral girdle and the entire upper limb of one side
-
roots of the brachial plexus are form from
Anterior rami of C5–T1
•Superior trunk: Nerves C5 and C6
•Middle trunk: Nerve C7
•Inferior trunk: Nerves C8 and T1
-
Portions of each trunk in brachial plexuse are divide into
anterior division and a posterior division
The anterior and posterior divisions converge to form three cords:
•Posterior cord
•Medial cord
•Lateral cord
-
Five major terminal branches emerge from the three cords: in brachial plexuses
•Axillary nerve
•Median nerve
•Musculocutaneous nerve
•Radial nerve
•Ulnar nerve
-
Axillary Nerve of the Brachial Plexus
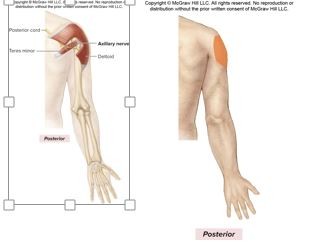
C5, C6
Formed from posterior cord, posterior division of the brachial plexus
motor innervation
Deltoid (arm abductor)
Teres minor (lateral rotator of arm)
Cutaneous Innervation
Superolateral arm
-
Median Nerve of the Brachial Plexus
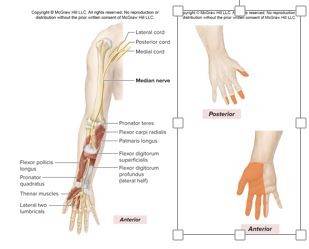
C6-T1
Formed from medial and lateral cords, anterior division of the brachial plexus
motor innervation
-Most anterior forearm muscles (flexor carpi radialis, thumb, later 2 lumbrical)
Cutaneous Innervation
Palmar aspects and dorsal tips of lateral 3-1/2 digits (thumb, index finger, middle finger, and 1/2 of ring finger
-
Musculocutaneous Nerve of the Brachial Plexus
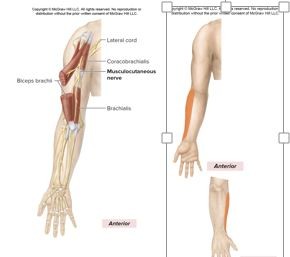
C5-C7
Formed from the lateral cord, anterior division of the brachial plexus
motor innervation
Anterior arm muscles (flex humerus, flex elbow joint, supinate forearm)
Coracobrachialis, Biceps brachii, Brachialis
Cutaneous Innervation
Lateral region of forearm
-
Radial Nerve of the Brachial Plexus
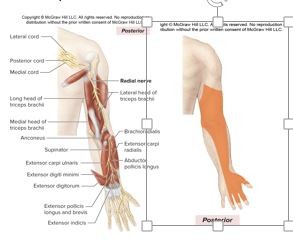
C5-T1
Formed from the posterior cord, posterior division of the brachial plexus
Motor Innervation
Posterior arm muscles
(extend forearm)
Triceps brachii
Posterior forearm muscles
Supinator
Brachioradialis
Cutaneous Innervation
Posterior region of arm
Posterior region of forearm
Dorsal aspect of lateral three digits (except their distal tips)
-
Ulnar Nerve of the Brachial Plexus

C8-T1
Formed from the medial cord, anterior division of the brachial plexus
Motor Innervation
Anterior forearm muscles (flexors of wrist and digits)
Flexor carpi ulnaris
Intrinsic hand muscles
Hypothenar muscles
Cutaneous Innervation
Dorsal and palmar aspects of medial 1-1/2 digits (little finger, medial aspect of ring finger)
-
left and right lumbar plexuses
anterior rami of spinal nerves L1–L4
-The lumbar plexus is subdivided into an anterior division and a posterior division.
-The main nerve of the posterior division is the femoral nerve
-The main nerve of the anterior division is the obturator nerve
-
Femoral Nerve of the Lumbar Plexus
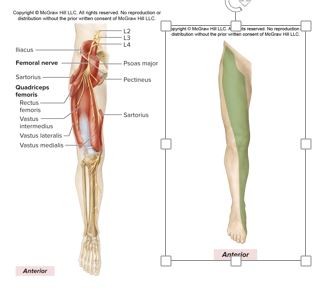
L2-L4
Motor Innervation
Anterior thigh muscles
Quadriceps femoris (knee extensor)
Rectus femoris
Vastus medialis Iliopsoas (hip flexor) Sartorius
Cutaneous Innervation
Anterior thigh
-
Obturator Nerve of the Lumbar Plexus
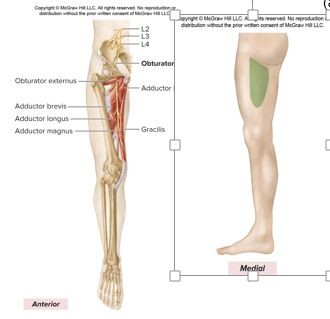
L2-L4
Motor Innervation
Medial thigh muscles (adductors of thigh)
Adductors
Gracilis
Pectineus1
Obturator externus (lateral rotator of thigh)
Cutaneous Innervation
superomedial thigh
-
left and right sacral plexuses
anterior rami of spinal nerves L4–S4
-The lumbar and sacral plexuses are sometimes considered together as the lumbosacral plexus
-The anterior rami are organized into an anterior division and a posterior division
-
sciatic nerve
largest and longest nerve
the tibial division and common fibular division wrapped in a common sheath
-
Sacral Plexuses split into
•Tibial nerve
•Common fibular nerve
-•Along the lateral knee, the common fibular nerve splits into the deep and superficial fibular nerves
-Additional branches from the tibial and common fibular nerves serve the calf, leg, and foot
•Sural, lateral sural cutaneous, and medial sural cutaneous nerves
-
Tibial nerve of the Sacral Plexus
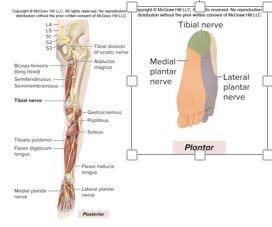
L4-S3
Motor Innervation
Posterior thigh muscles (extend thigh and flex leg)
Long head of biceps femoris
Semimembranosus
Part of adductor magnus
Posterior leg muscles (plantar flexors of foot, flexors of knee)
Flexor hallucis longus
Gastrocnemius
Soleus
Popliteus
Tibialis posterior (inverts foot)
Plantar foot muscles (via medial and lateral plantar nerve branches)
Cutaneous Innervation
heel
-
Common Fibular Nerve of the Sacral Plexus

L4-S2
(Divides into deep fibular and superficial fibular branches)
Motor Innervation
Short head of biceps femoris (knee flexor); see also deep fibular and superficial fibular nerves
-
Deep Fibular Nerve
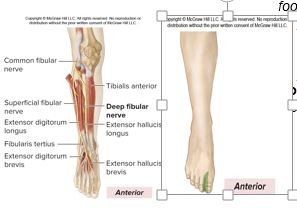
L4-S1
Motor Innervation
Anterior leg muscles (dorsiflex foot, extend toes)
Tibialis anterior (inverts foot)
Extensor hallucis longus
Dorsum foot muscles (extend toes)
Extensor digitorum brevis
Cutaneous Innervation
dorsal interspace between 1st and 2nd toe
-
Superficial Fibular Nerve
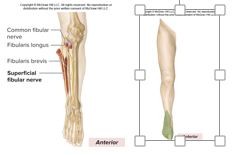
L5-S2
Motor Innervation
Lateral leg muscles (foot evertors and plantar flexors)
Fibularis longus
Fibularis brevis
Cutaneous Innervation
anteroinferior part of leg most of dorsum of foot
-
Reflexes
rapid, preprogrammed, involuntary reactions to a stimulus
Survival mechanism against potentially harmful stimuli
Properties of reflexes:
•A stimulus is required to initiate the reflex
•A rapid response requires that few neurons are involved and synaptic delay is minimal
•A preprogrammed response occurs the same way every time
•An involuntary response ensures no intent or preawareness is required
-
reflex arc, 5 steps
neural circuit of a reflex
•Stimulus activates sensory receptor
•Nerve impulse travels through sensory neuron to the CNS
•Interneurons process information about the stimulus
•Motor neurons send impulses to effector
•Effector (muscle or gland) brings about response
-
Ipsilateral
reflex arc Both the receptor and effector organs are on the same side
-
Monosynaptic
Sensory axons synapse directly on motor neurons, whose axons project to the effector
-
withdrawal (flexor) reflex
polysynaptic reflex arc:
•Initiated by a painful stimulus
•transmitted to the spinal cord
•Interneurons receive the information and stimulate motor neurons to direct flexor muscles to contract in response
•Simultaneously, antagonistic extensor muscles are inhibited so that the traumatized body part may be quickly withdrawn
-
stretch reflex
monosynaptic reflex arc:
•Stretch in a muscle is monitored by stretch receptors called muscle spindles
•The fibers within a spindle are intrafusal muscle fibers (innervated by gamma motor neurons)
•Most muscle fibers in a muscle are not in spindles, and so are extrafusal muscle fibers (innervated by alpha motor neurons)
•When a stimulus stretches a muscle, the muscle reflexively contracts
•Example: knee jerk reflex; the stimulus stretches the quadriceps and it reflexively contracts
-
Tendon reflex aka,
Golgi tendon reflex-
•Golgi tendon organs are nerve endings in tendons near a muscle–tendon junction
•As a muscle contracts, force is exerted on its tendon, resulting in tension in the tendon and activation of the Golgi tendon organ
•Nerve impulses signal interneurons in the spinal cord, which in turn inhibit the actions of the motor neurons
•Muscle relaxes, protecting the muscle and tendon from excessive tension
-
Abnormal reflex responses
Hypoactive reflex: Response is diminished or absent
Hyperactive reflex: Response is abnormally strong
-
Development of the Spinal Cord
CNS develops from neural tube,
cranial and spinal nerves develop from neural crest cells
Neural canal becomes central canal of spinal cord
Basal plates form anterior horns, lateral horns and anterior part of gray commissure
Alar plates form posterior horns and posterior part of gray commissure
-
Contralateral
reflex arc Impulses initiating from a receptor cross the spinal cord to activate effector organs on the opposite limb
-
Polysynaptic
More complex pathways exhibit a number of synapses involving interneurons within the reflex arc

