Cellular Structure of Bone (Physiology 2)
Cellular structure of bone - Andrew Marken Lecture Outline The skeleton is a vital part of our physiology, without it we would not have our structure or shape. However, that is not the only purpose of the skeleton. The skeleton actually fulfills several roles in our body. While it may be common to think of the skeleton as a solid fixed, almost lifeless structure, the skeleton that is left behind after death does not reveal the full picture. In fact the bone microenvironment is incredibly dynamic and constantly changing. In this session we will learn about the different functions of bone, what it is made of, how it develops during growth, and how it is maintained in the adult. We will cover the different specialised bone cells, how they interact and are regulated, as well as what happens to bone when something goes wrong causing bone disease. Desired learning outcomes At the end of this lecture unit, students should be able to: Discuss the different functions of the skeleton Describe the different types of bone and why individual bones have different shapes Explain the organic and inorganic components of bone Understand how bones develop via ossification and how this relates to linear growth Explain the role of each specialised bone cell and the process of bone remodelling Identify and explain the function of important paracrine signaling molecules in regulating the differentiation and activity of bone cells Understand the underlying cause of bone disorders including osteopetrosis and osteoporosis Session Resources Lecture Slides The Cellular Structure of Bone 24_5.pptxDownload The Cellular Structure of Bone 24_5.pptx Lecture Recording Introduction Bone Classifications Bone Cells Cellular structure of bone - Andrew Marken Lecture Outline The skeleton is a vital part of our physiology, without it we would not have our structure or shape. However, that is not the only purpose of the skeleton. The skeleton actually fulfills several roles in our body. While it may be common to think of the skeleton as a solid fixed, almost lifeless structure, the skeleton that is left behind after death does not reveal the full picture. In fact the bone microenvironment is incredibly dynamic and constantly changing. In this session we will learn about the different functions of bone, what it is made of, how it develops during growth, and how it is maintained in the adult. We will cover the different specialised bone cells, how they interact and are regulated, as well as what happens to bone when something goes wrong causing bone disease. Desired learning outcomes At the end of this lecture unit, students should be able to: Discuss the different functions of the skeleton Describe the different types of bone and why individual bones have different shapes Explain the organic and inorganic components of bone Understand how bones develop via ossification and how this relates to linear growth Explain the role of each specialised bone cell and the process of bone remodelling Identify and explain the function of important paracrine signaling molecules in regulating the differentiation and activity of bone cells Understand the underlying cause of bone disorders including osteopetrosis and osteoporosis Session Resources Lecture Slides The Cellular Structure of Bone 24_5.pptxDownload The Cellular Structure of Bone 24_5.pptx Lecture Recording Introduction Bone Classifications Bone Cells Bone Formation Old Lecture Version Cellular Structure of Bone slidesDownload Cellular Structure of Bone slides Further Reading Human Physiology (5th Edition) Pocock, Richards and Richards. Chapter 51 Glossary Hydroxyapatite. The principle mineral component of bone, composed of calcium and phosphate (Ca10(PO4)6(OH)2). Responsible for the hardness of bone. Intramembranous ossification. The process by which flat bones develop as osteoblasts differentiate directly from mesenchyme precursors within mesenchymal connective tissue. Endochondral ossification. The process by which long bones develop via the conversion of a cartilage model into bone Chondrocyte. Mature cartilage cell. Produces cartilage matrix. Undergoes hypertrophic differentiation in the growth plate to allow linear growth Growth plate. Specialised cartilage structure found at the metaphysis of long bones between the ossification centers. Allows linear growth. Osteocyte. Terminally differentiated osteoblasts encased within mature bone. They are connected via a network of dendritic processes that allow them to have a mechanosensory role. Thought to be the master regulators of bone remodeling. Osteoblast. Bone cells responsible for secreting osteoid which is then mineralized to become mature bone. Osteoclast. Large, multi-nucleate cells responsible for resorption of bone. Osteoid. The organic matrix of bone, consisting mainly of collagen and other protein. Secreted by osteoblasts, which line the surface of newly-formed bone. Bone remodeling. The skeleton is continually renewed throughout life via the bone remodeling cycle, a process whereby old or damaged bone is removed through osteoclastic bone resorption, and an equal amount of new bone is formed by the osteoblasts Bone Formation Old Lecture Version Cellular Structure of Bone slidesDownload Cellular Structure of Bone slides Further Reading Human Physiology (5th Edition) Pocock, Richards and Richards. Chapter 51 Glossary Hydroxyapatite. The principle mineral component of bone, composed of calcium and phosphate (Ca10(PO4)6(OH)2). Responsible for the hardness of bone. Intramembranous ossification. The process by which flat bones develop as osteoblasts differentiate directly from mesenchyme precursors within mesenchymal connective tissue. Endochondral ossification. The process by which long bones develop via the conversion of a cartilage model into bone Chondrocyte. Mature cartilage cell. Produces cartilage matrix. Undergoes hypertrophic differentiation in the growth plate to allow linear growth Growth plate. Specialised cartilage structure found at the metaphysis of long bones between the ossification centers. Allows linear growth. Osteocyte. Terminally differentiated osteoblasts encased within mature bone. They are connected via a network of dendritic processes that allow them to have a mechanosensory role. Thought to be the master regulators of bone remodeling. Osteoblast. Bone cells responsible for secreting osteoid which is then mineralized to become mature bone. Osteoclast. Large, multi-nucleate cells responsible for resorption of bone. Osteoid. The organic matrix of bone, consisting mainly of collagen and other protein. Secreted by osteoblasts, which line the surface of newly-formed bone. Bone remodeling. The skeleton is continually renewed throughout life via the bone remodeling cycle, a process whereby old or damaged bone is removed through osteoclastic bone resorption, and an equal amount of new bone is formed by the osteoblasts
-
What is the axial skeleton and what does it include? (3)
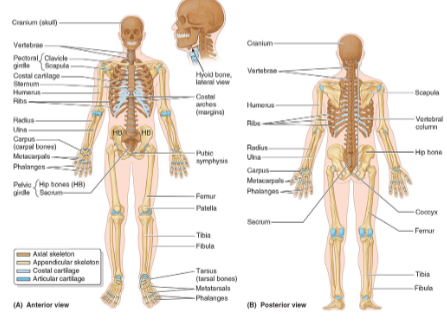
The axial skeleton is the part of the skeleton that includes the central core of the body.
It consists of the skull, neck, vertebral column, and thoracic cage.
It provides support and protection for the brain, heart, and lungs.
-
What is the appendicular skeleton and what does it include? (3)
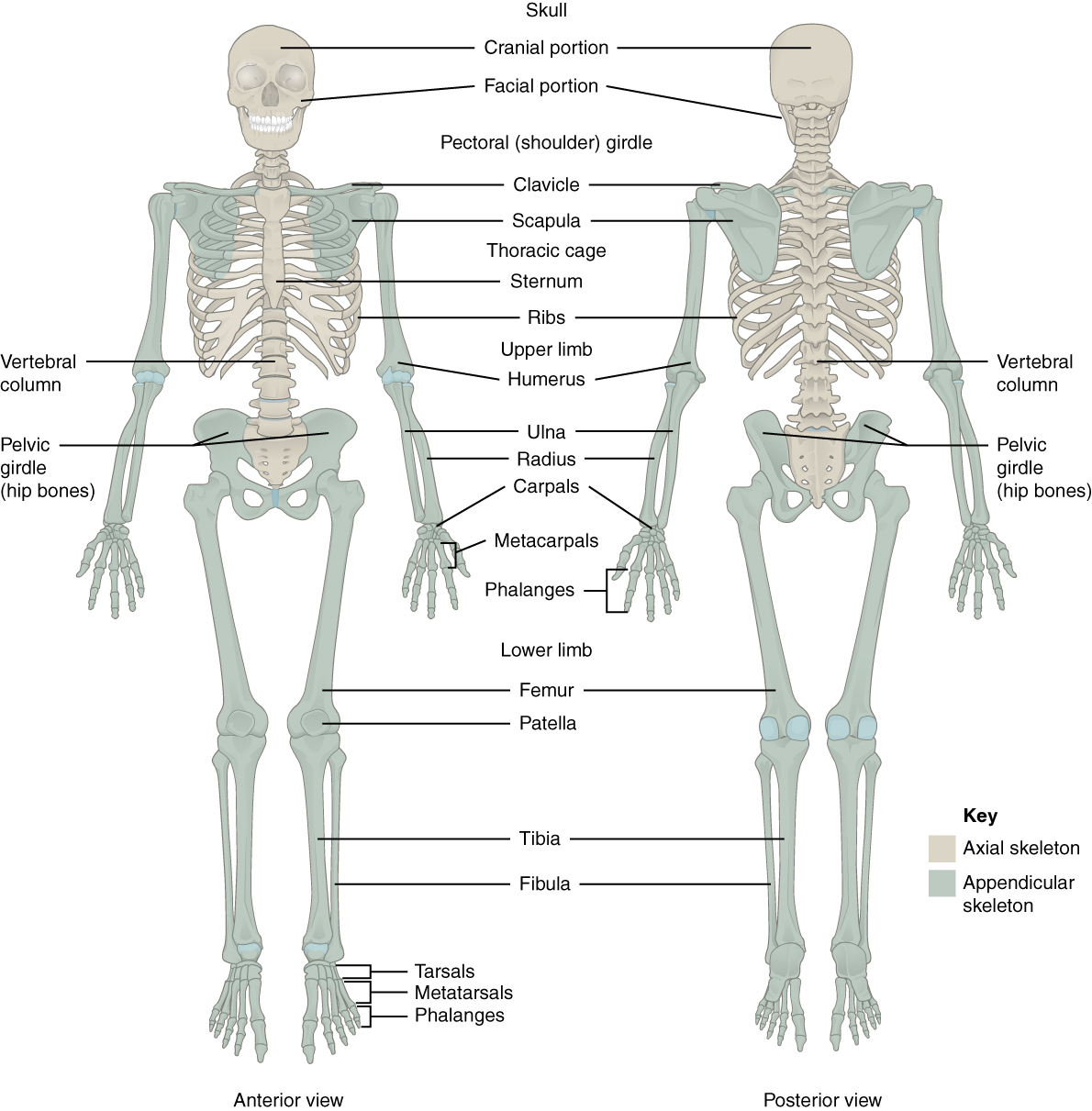
The appendicular skeleton includes the limbs and girdles.
It consists of the upper and lower limbs, as well as the pectoral and pelvic girdles.
It is responsible for movement and interaction with the environment.
-
How are bones articulated in the skeleton? (1)
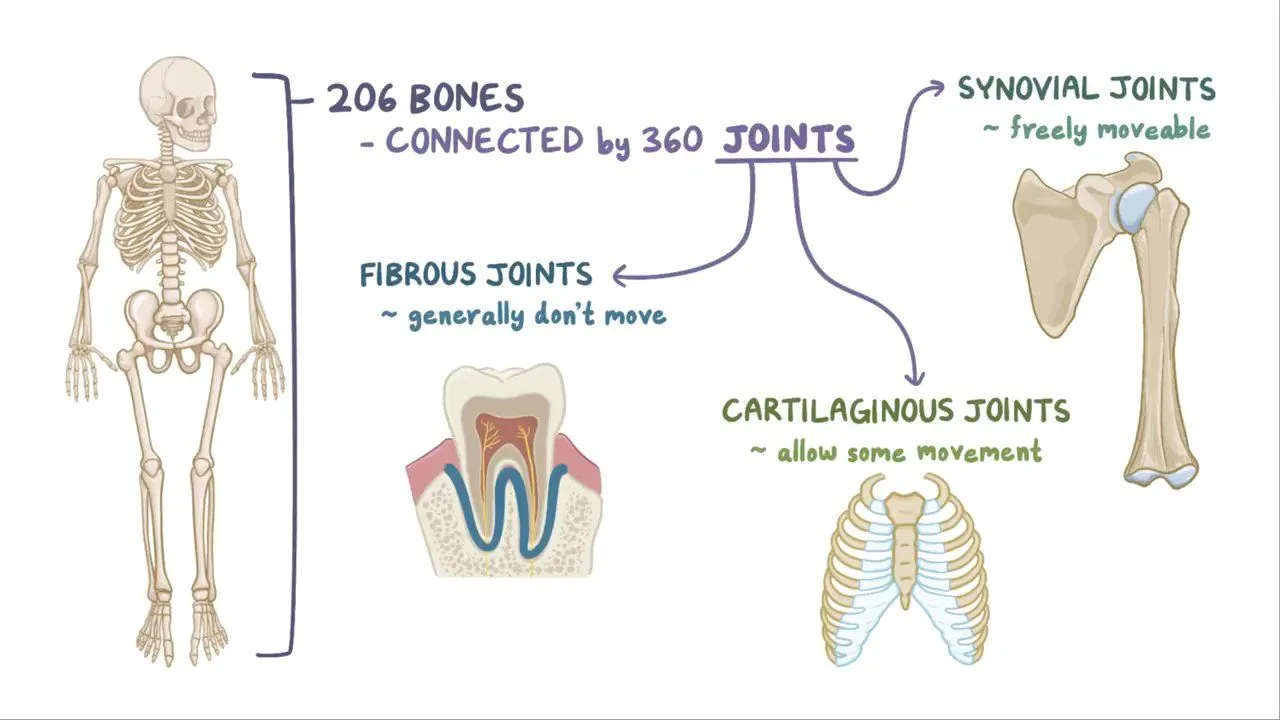
Bones are articulated by cartilaginous/synovial/fibrous joints.
-
What are the main functions of bones? (5)
Physical support: Maintain posture, space, and delineation (define boundaries) of body spaces.
Protection: Protect vital structures such as the brain, heart, and lungs.
Mechanical basis of movement: Provide attachment for muscles and tendons, allowing for leverage.
Storage: Store salts, including calcium, acting as a resource sink.
Haematopoiesis: Bone is the location of red bone marrow, where new blood cells are produced.
-
What is bone? (3)
Bone is a connective tissue covered by hyaline cartilage at joint surfaces and periosteum elsewhere.
It consists of an organic framework layered with inorganic minerals.
Bone combines organic components (collagen fibers, ossein) with inorganic minerals (calcium hydroxyapatite) to provide strength and flexibility.
-
What are the organic components of bone and their function? (2)
The organic components include collagen fibers (ossein) and some ground substance.
They form the bone matrix, contributing to the flexibility and strength of bone.
-
What are the inorganic components of bone and their function? (2)
The inorganic components consist mostly of calcium hydroxyapatite (Ca10(PO4)6(OH)2) crystals.
These crystals calcify the ossein and provide bone with rigidity and strength.
-
What is the primary role of bone in the storage of minerals? (1)
Bone is the main storage site for calcium and phosphorus, releasing or absorbing these minerals as the body needs them.
-
What are the organic components of bone and their functions? (5)
Type 1 collagen (85-90%) provides tensile strength.
Collagen V and collagen III, XI, XIII (5, 3, 11 and 13) are also present in smaller amounts, contributing to bone's structure.
Ground substance consists of non-collagenous proteins that help in bone formation and repair.
These organic components are essential for development, remodeling, growth, and repair of bone.
They also support bone matrix formation and bone mineralization.
-
What are the four major groups of organic components in bone? (4)
Proteoglycan macromolecules: Provide structure and hydration to the bone matrix.
Multiadhesive glycoproteins: Help in cell attachment and interaction with the bone matrix.
Bone-specific, vitamin K-dependent proteins: Involved in bone mineralization.
Growth factors and cytokines: Play a role in bone growth and healing.
-
What are the types of bone classifications based on anatomy? (5)
Flat bones: Thin, flat, and often curved (e.g., skull, sternum).
Long bones: Longer than they are wide, typically found in limbs (e.g., femur, humerus).
Short bones: Cube-shaped, provide support and stability with limited movement (e.g., carpals, tarsals).
Irregular bones: Have complex shapes that don't fit into other categories (e.g., vertebrae, pelvic bones).
Sesamoid bones: Bones embedded in tendons, such as the patella.
-
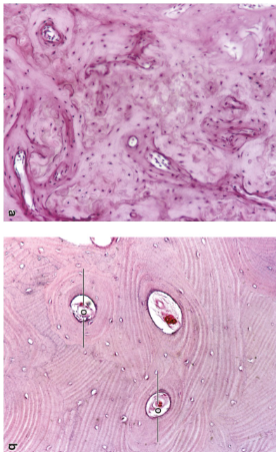
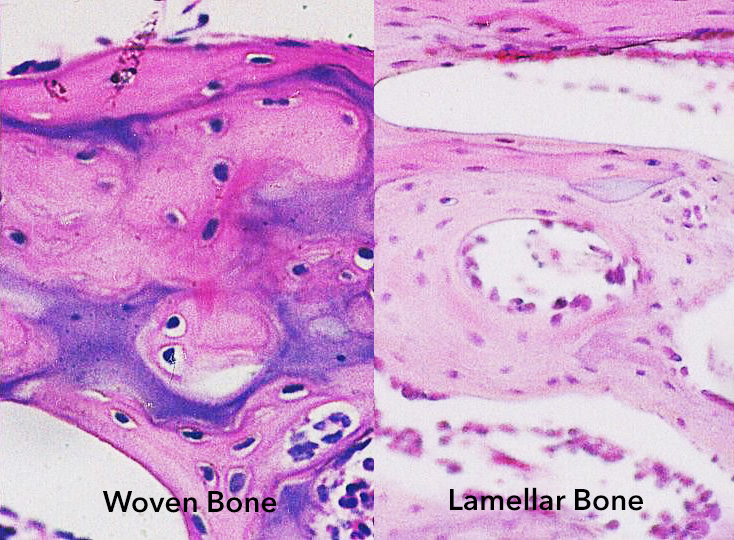
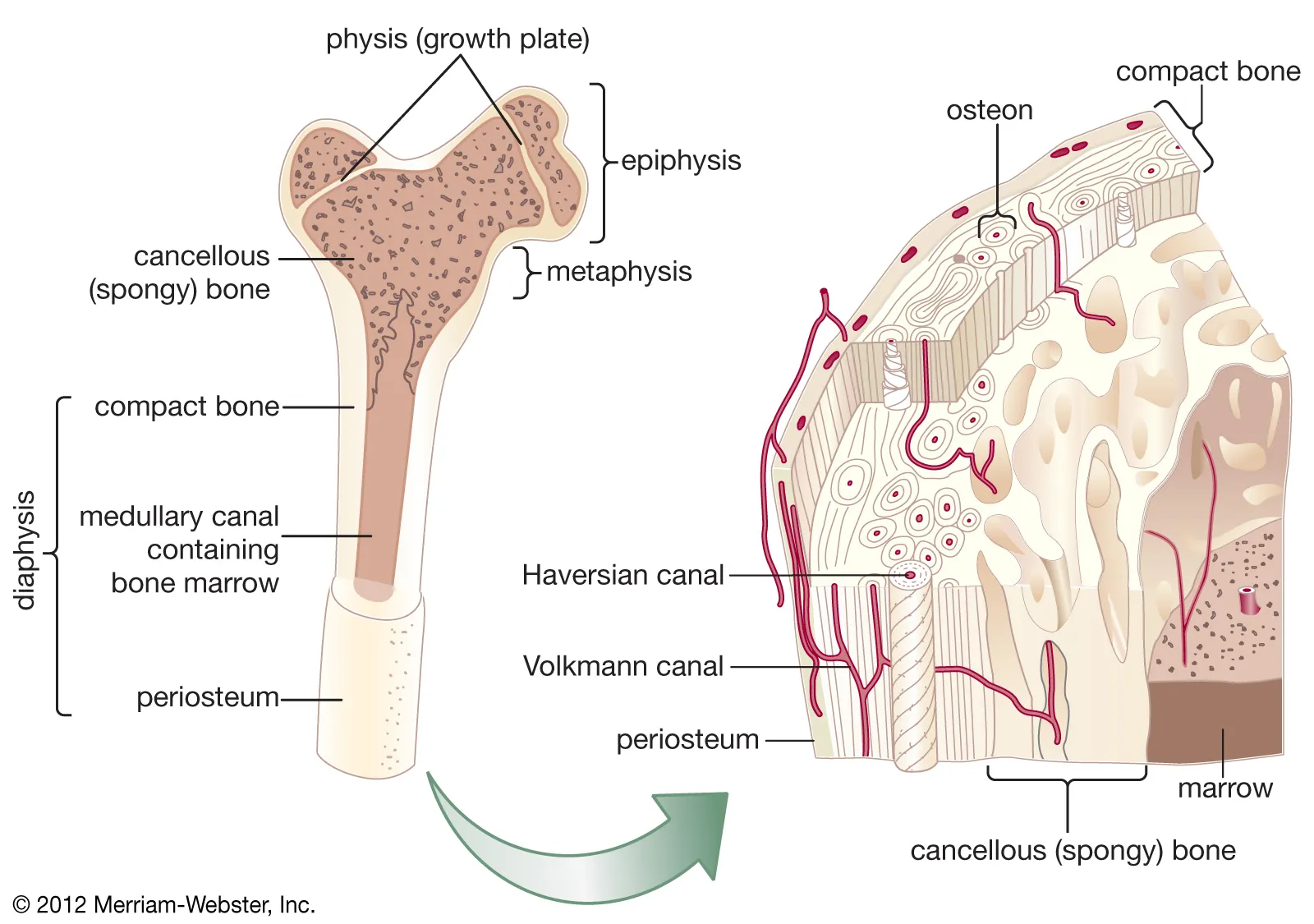
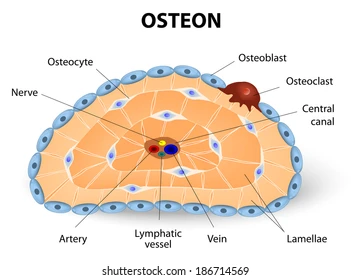
What are the types of bone classifications based on microscopic structure? (2)
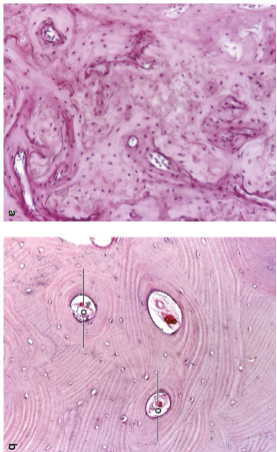
Woven bone (primary, immature): Random arrangement of collagen fibers; found in fetal development and during bone repair.
Lamellar bone (secondary, mature): Organized in concentric layers (lamellae) and osteons; found in mature bone.
-
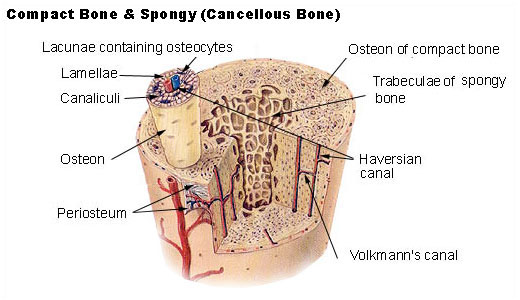
What are the types of bone classifications based on macroscopic structure? (2)
Cancellous (spongy, medullary) bone: Forms the interior of bones, consisting of a network of trabeculae that provide support while minimizing weight.
Cortical (compact) bone: Forms the exterior and is dense, providing most of the bone's strength; makes up 80% of bone mass.
-
What is lamellar bone and what are its characteristics? (4)
Lamellar bone is mature (secondary) bone.
It is organized into concentric layers called lamellae.
These layers are arranged into osteons (functional units of bone).
Lamellar bone is mineralized, with fewer cells and ground substance compared to woven bone.
-
What is woven bone and what are its characteristics? (4)
Woven bone is immature (primary) bone.
The collagen fibers are arranged in a random assortment, interlacing in different directions.
It is temporary, found in fetuses, during bone repair, or where remodeling occurs.
Woven bone is present in tendon attachments and alveolar sockets of teeth.
-
What are the characteristics of cortical (compact) bone? (3)
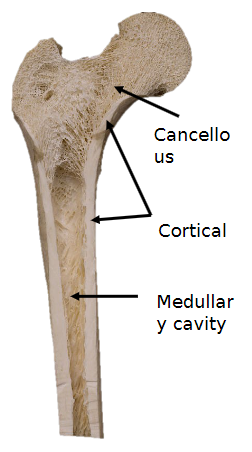
It forms the exterior of bones and is very dense.
It provides strength and is responsible for most of the bone's mechanical support.
It constitutes 80% of bone mass.
-
What are the characteristics of cancellous (spongy) bone? (3)
It is found deep to cortical bone, forming the interior of bones.
It has a network of bony trabeculae that make it lighter but still supportive.
The spaces in cancellous bone are filled with bone marrow.
-
What is the medullary cavity, and where is it found? (2)
The medullary cavity is a central cavity in long bones, where bone marrow is located.
It is lined with cortical bone and plays a role in the storage of marrow and fat.
-
What are the characteristics of cancellous (spongy) bone? (4)
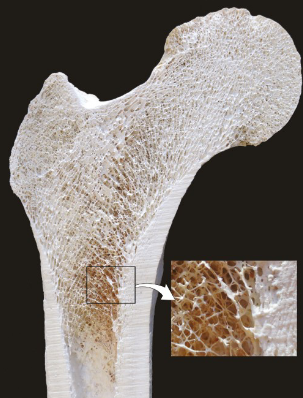
Cancellous bone is lighter, weaker, and more flexible than cortical bone.
It is arranged in trabeculae, which are structures that align with the direction of stress when mature.
It has a higher surface area to volume ratio, making it more suitable for metabolic activity.
The spaces between the trabeculae are filled with bone marrow, which can be either red or yellow.
-
What are the structural features of long bones? (3)
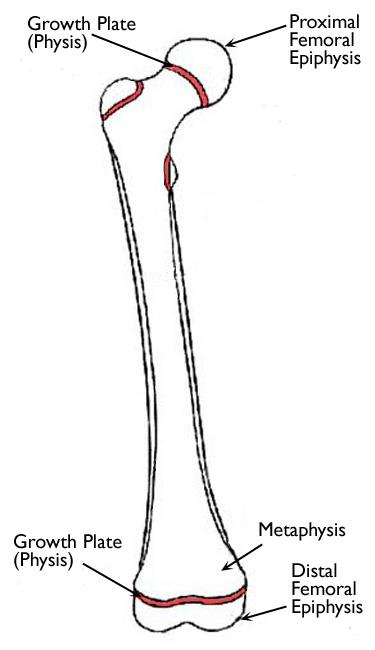
Long bones have a tubular shaft.
They have an epiphysis (head) at each end.
The epiphyses are separated by a growth plate.
-
What are the structural features of short bones? (2)
Short bones are cuboidal in shape.
They consist of cancellous bone surrounded by compact bone.
-
What are the structural features of flat bones? (1)
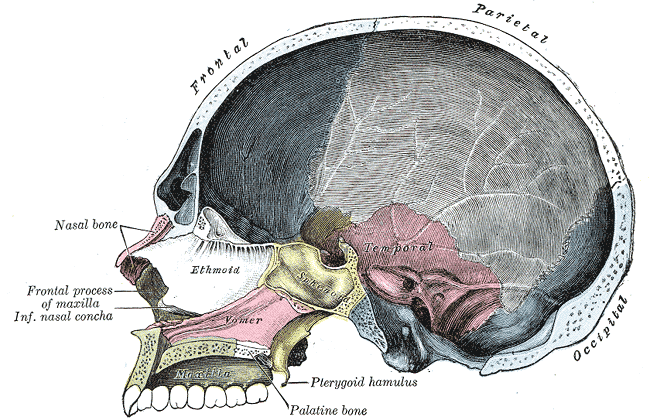
Flat bones generally serve protective functions, such as forming the cranial vault.
-
What are the anatomical classifications of bones and examples of each? (5)
Long bones: Humerus, femur, metacarpals, phalanges.
Short bones: Found only in the wrist and foot.
Flat bones: Ribs, cranial vault, scapulae.
Irregular bones: Pelvis, vertebrae, sphenoid.
Sesamoid bones: Patella.
-
What are the characteristics of sesamoid bones? (2)
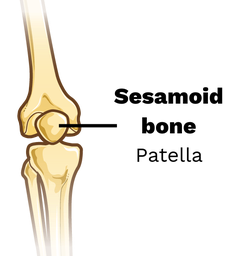
Sesamoid bones are located within tendons where they pass over a joint.
They do not fit into other bone classification groups.
-
What is the periosteum and what are its features? (6)
The periosteum lines the external surface of bones, except at articulating surfaces, where hyaline cartilage is present.
The inner cellular layer contains osteoprogenitor cells (stem cells) when the bone is actively growing or remodeling.
In grown bone, the inner layer contains periosteal cells.
The outer fibrous layer has collagen fibers arranged parallel to the bone surface.
Exception: At ligament and tendon attachments, collagen fibers extend at oblique or right angles and are continuous with those in the ligaments/tendons.
The periosteum supports bone growth, repair, and structural integrity.
-
What are bone cavities and their features? (5)
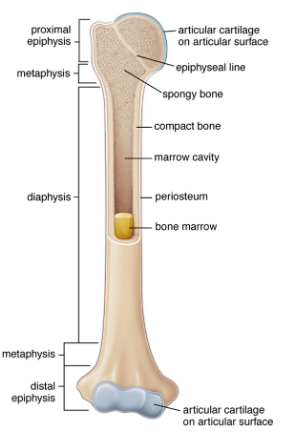
Bone cavities are lined with endosteum, typically a single layer of bone lining cells and osteoprogenitors.
They include the marrow cavity and spaces between spongy bone trabeculae.
Contain red marrow (site of haematopoiesis) and yellow marrow (stores adipose tissue).
In adults, yellow marrow dominates as less new blood cell production is required but can revert to red marrow if needed.
In adults, red marrow is found in limited locations, such as the pelvis, sternum, and vertebrae.
-
What are the types of bone cells and their functions? (4)

Osteoprogenitors:
Stem cells that are the source of new osteoblasts.
Osteoblasts:
Form bone by laying down new organic bone matrix (osteoid).
Osteocytes:
Found within calcified bone, they maintain the bone structure.
Osteoclasts:
Responsible for breaking down bone matrix to allow for remodeling.
-
What are the characteristics and functions of osteoblasts? (6)
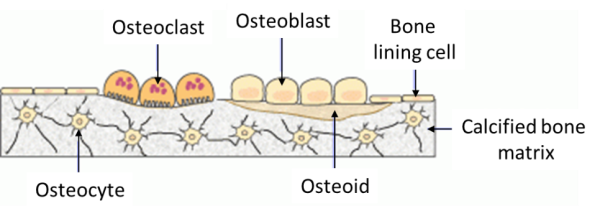
Secretes type I collagen and bone matrix proteins to form the osteoid.
Plays a key role in the calcification process.
Secretes small matrix vesicles involved in bone mineralisation.
Exists as a single layer in contact with forming bone.
Some osteoblasts become embedded in the forming bone and specialise into osteocytes.
Contributes to the formation and initial mineralisation of bone.
-
What are the characteristics and functions of osteocytes? (7)
Osteocytes are mature bone cells enclosed by the bone matrix they secreted as osteoblasts.
They are smaller than osteoblasts and have more cytoplasmic processes.
After mineralisation, they occupy a lacuna (space) shaped to conform to the osteocyte.
Their cytoplasmic processes extend through canaliculi, small channels in the bone matrix.
Osteocytes communicate with other osteocytes and bone cells via gap junctions.
They are metabolically active, maintaining bone and responding to mechanical forces.
Flexing of the bone moves interstitial fluid through canaliculi, aiding in mechanical signal detection.
-
What are the characteristics and functions of bone lining cells? (7)
Bone lining cells are osteoblast-derived.
They are flat cells with few organelles.
Found in areas where no bone remodeling is occurring, covering the bone surface.
Periosteal cells: Located on the external surface of bones.
Endosteal cells: Found on the internal surface of bones.
Maintain and provide nutritional support to embedded osteocytes.
Regulate the flow of calcium and phosphate between the bone and surrounding tissues.
-
What are osteons and their structural features? (6)
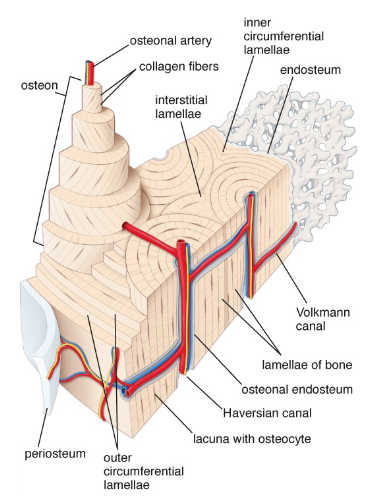
Osteons consist of lamellae arranged in concentric circles around a central canal containing arteries, nerves, and veins (ANV).
Canaliculi diffuse nutrients through interstitial fluid to osteocytes.
Volkmann canals connect adjacent Haversian canals, facilitating communication between osteons.
An osteon includes one central canal and all its surrounding circles of lamellae.
Osteons are arranged in the direction of stress, enhancing strength.
Interstitial lamellae fill the gaps between osteons, representing remnants of old osteons.
-
What are packets in trabecular bone? (3)
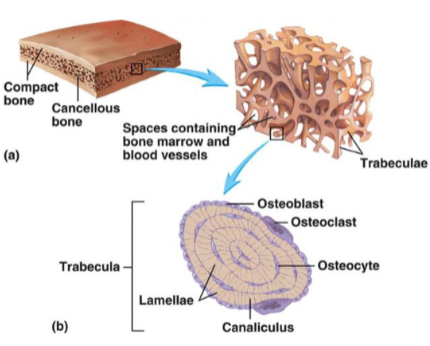
Trabecular osteons are also known as packets.
They rely on diffusion from bone marrow through canaliculi, instead of Haversian canals.
This diffusion system eliminates the need for a central canal in trabecular bone.
-
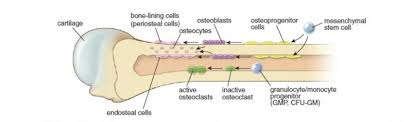
What are the characteristics and functions of osteoclasts? (7)
Found where bone is being resorbed, directly located on the bone in resorption bays.
They are large, multinucleated, and acidophilic cells.
Osteoclasts are not related to osteoblasts and are formed by the fusion of macrophage progenitor cells.
Possess a ruffled border, the site where absorption occurs.
A clear zone forms a sealing ring around the resorption zone.
Use carbonic acid to decalcify the bone and lysosomes to break down bone proteins.
Play a vital role in bone resorption and remodelling.
-
How is osteoclast activation regulated? (6)
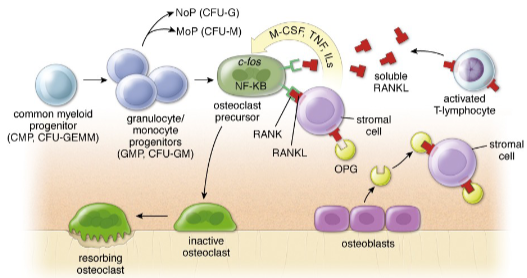
Osteoclast precursors express the RANK receptor molecule.
The RANK receptor interacts with RANK ligand (RANKL), found on stromal cell surfaces or activated T lymphocytes during inflammation.
The RANK-RANKL pathway is blocked by osteoprotegerin (OPG), which is produced by osteoblasts.
The OPG/RANKL system mediates bone resorption and remodeling, balancing osteoclast activity (OPG acts like a decoy, if more RANK-OPG is formed there is less RANK-RANKL) Little osteoclast activity occurs when new bone is being made, due to increased OPG production.
OPG acts as a regulator, preventing excessive bone resorption.
-
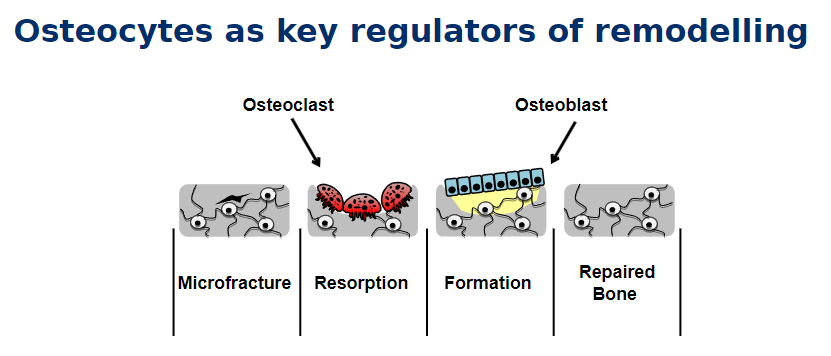
What is bone remodeling and why does it occur? (3)
Bone is a dynamically changing organ, with small portions constantly being remodeled.
The entire skeleton is replaced approximately every 7 years through the process of bone remodeling.
Bone remodeling ensures structural integrity and allows for adaptation to stress and metabolic demands.
-
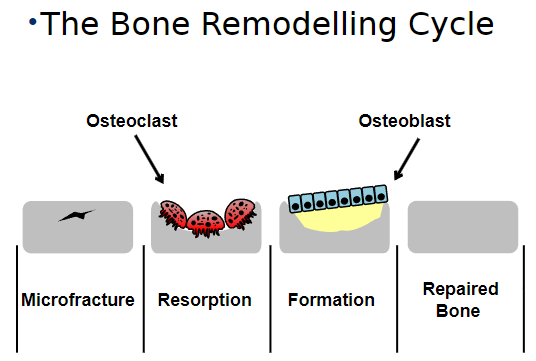
Picture demonstrating The Bone Remodelling Cycle:
-
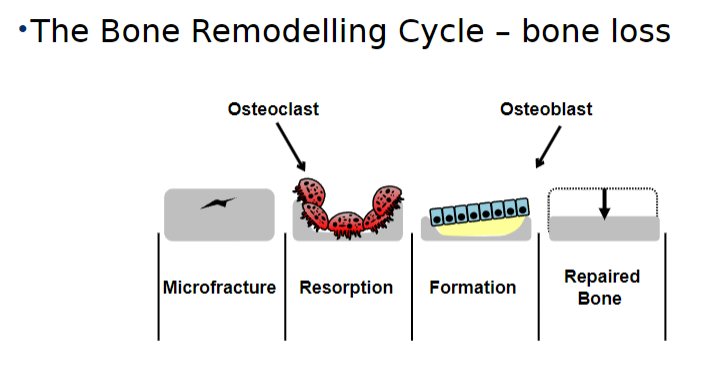
Picture demonstrating The Bone Remodelling Cycle - BONE LOSS:
-
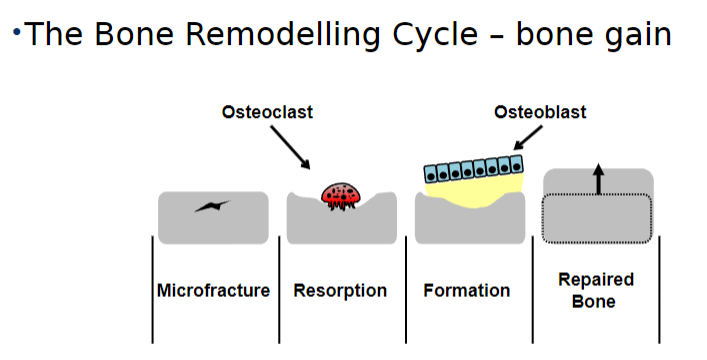
Picture demonstrating The Bone Remodelling Cycle - BONE GAIN:
-
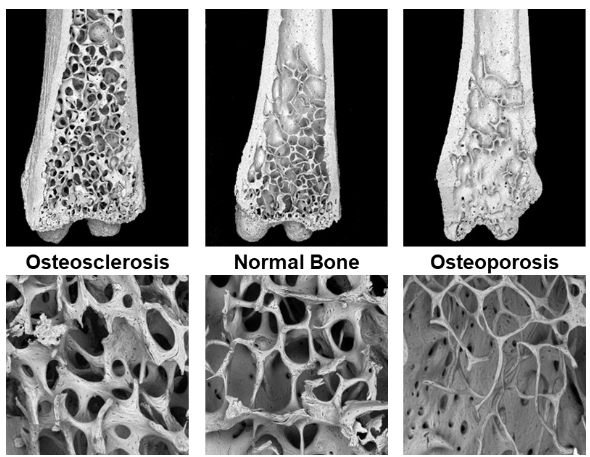
Picture demonstrating the effects of osteosclerosis and osteoporosis compared to normal bone:
-
Picture demonstrating Osteocytes as key regulators of remodelling:
-
What are the two types of bone formation? (6)
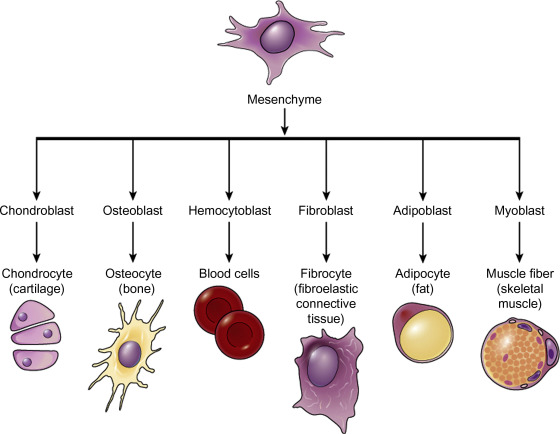
Intramembranous ossification:
A simpler method where bone forms directly from mesenchyme.
Produces flat bones of the skull, face, mandible, and clavicle.
Endochondral ossification:
Uses a cartilage precursor as a framework.
Produces axial and weight-bearing bones.
Refers only to the initial setting down of bone, followed by remodeling via appositional growth.
Long bones also later employ intramembranous ossification.
-
What occurs during intramembranous ossification? (7)
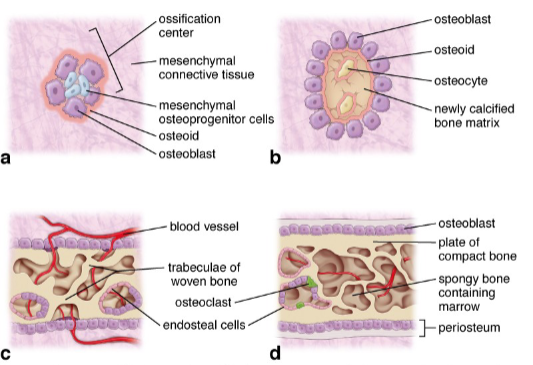
Occurs within embryonic mesenchyme (connective tissue precursor).
An ossification center forms from an aggregation of osteoprogenitors.
Osteoblasts accumulate at the periphery and produce osteoid, trapping osteocytes.
Forms woven bone in two plates (outer and inner) with thick trabeculae.
Spaces are lined with osteoblasts and endothelial cells.
Woven bone is eventually replaced by lamellar bone.
Blood vessels carry bone marrow cells into spaces between trabeculae.
-
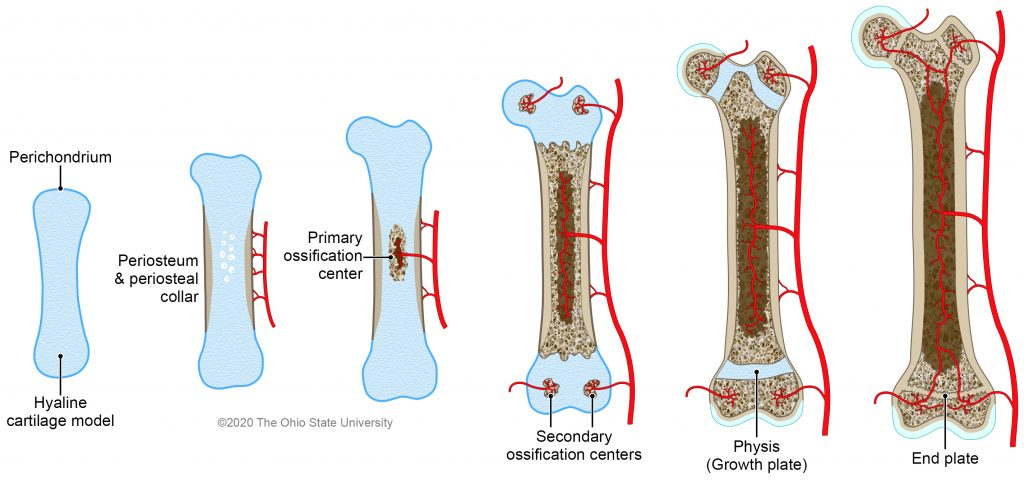
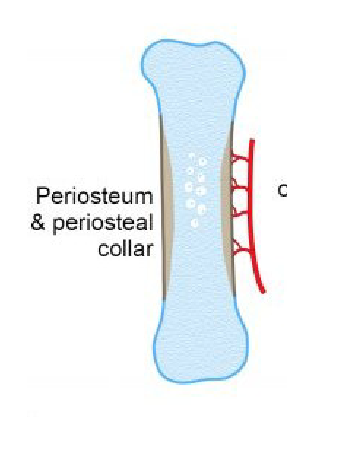
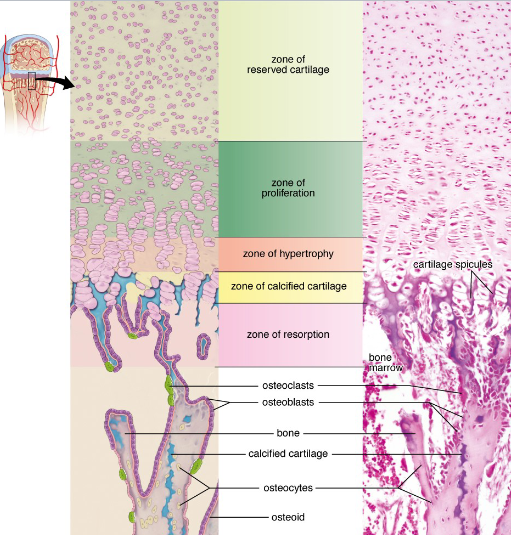
What is endochondral ossification and its initial process? (4)
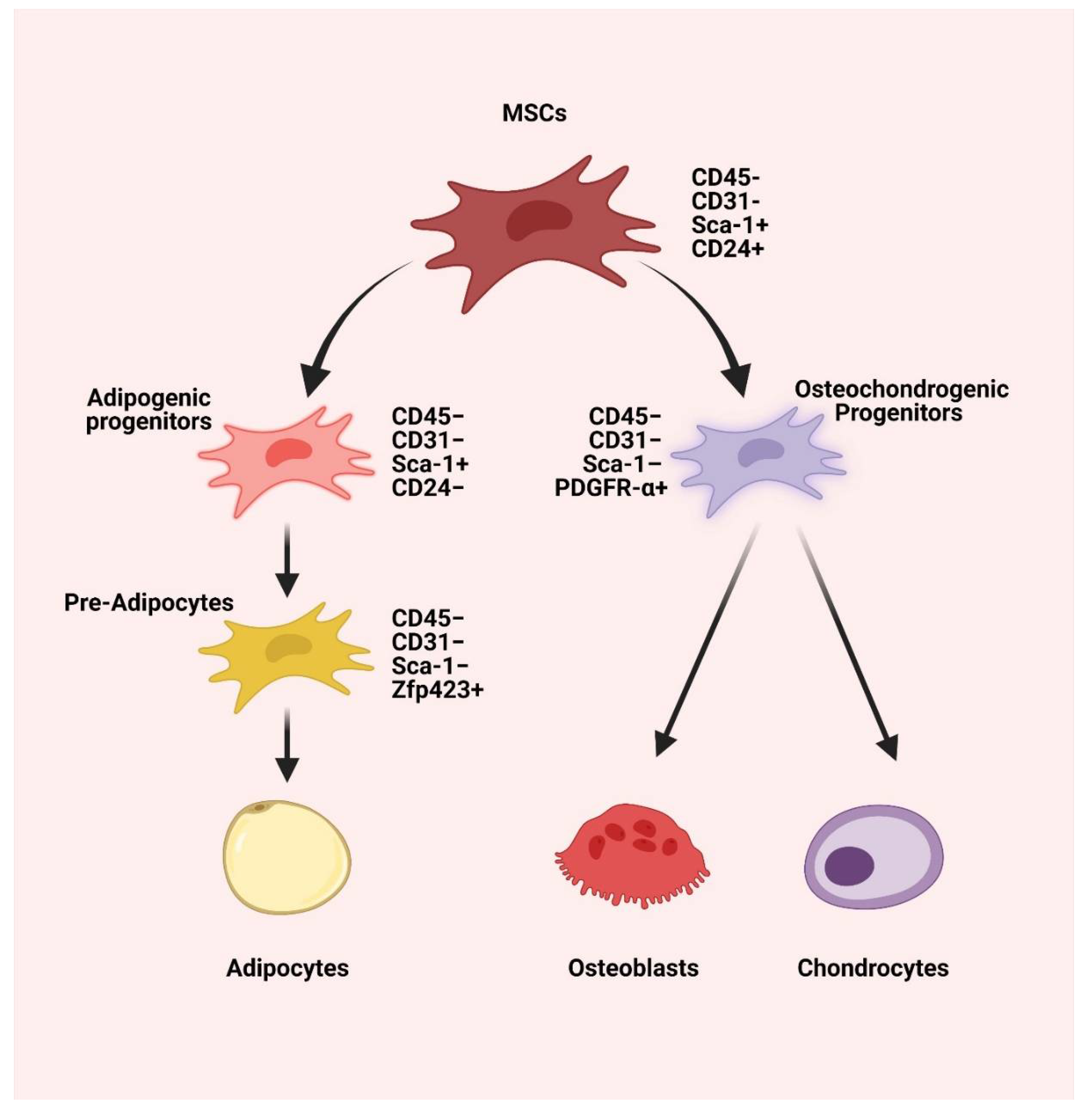
Mesenchymal cells (MSCs) differentiate into chondrocytes.
These cells produce a hyaline cartilage model (its called model because the cartilage is the precursor of initial bone formation) of the future bone.
A cuff of bone forms around the diaphysis (shaft) in long bones.
Chondrocytes grow and mature in the zone of hypertrophy - region in the growth plate (Chondrocytes in this zone increase in size rather than dividing or producing new cartilage matrix).
-
What occurs in the midregion of endochondral ossification? (5)
Chondrocytes in the midregion become hypertrophic.
These cells synthesize TNAP (tissue non-specific alkaline phosphatase).
This triggers calcification (not mineralization) of the cartilage.
Calcified cartilage matrix inhibits nutrient diffusion, causing chondrocyte death.
This forms the zone of calcified cartilage.
Calcification: The deposition of calcium salts, hardening the tissue.
Mineralization: The formation of hydroxyapatite crystals, converting tissue into bone.
-
How does bone formation proceed after chondrocyte death? (4)
Osteoprogenitor cells and blood vessels invade the calcified cartilage matrix from the periosteum.
These cells proliferate and differentiate into osteoblasts.
Osteoblasts begin laying down bone matrix, forming bone in the resorption zone.
The calcified cartilage is gradually replaced by bone tissue.
-
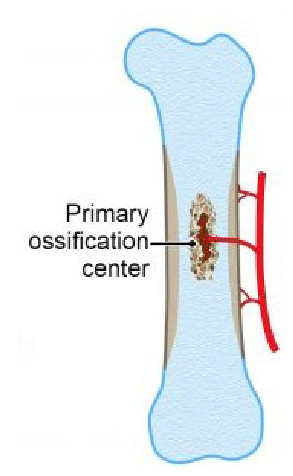
What happens during secondary ossification in endochondral ossification? (5)
Secondary ossification centers form in the epiphysis after birth.
The process continues until only the physis (growth plate) remains of the original cartilage framework.
New cartilage is produced in the zone of proliferation and resorbed in the zone of resorption to elongate the bone.
The growth plate is maintained until maximal growth is achieved.
Finally, epiphyseal closure occurs, fusing the epiphyseal and diaphyseal marrow cavities.
-
Picture Demonstrating a 'conveyor belt' of the formation of bone:
-
What is a physeal fracture and its key characteristics? (4)

The physeal (growth plate) is the weakest point of the bone, especially during growth spurts.
Physeal fractures have rapid healing due to the active growth of the growth plate.
However, there is a risk of growth arrest if the fracture is not properly treated.
Growth arrest can result in shortened bone or deformities.
-
What is hydroxyapatite and its role in bone? (2)
Hydroxyapatite is the principal mineral component of bone, composed of calcium and phosphate (Ca10(PO4)6(OH)2).
It is responsible for the hardness of bone, giving bone its rigid structure.
-
What is intramembranous ossification and how does it occur? (3)
Intramembranous ossification is the process by which flat bones develop directly from mesenchymal precursors.
Osteoblasts differentiate from mesenchymal cells within mesenchymal connective tissue.
It is the primary method for the formation of bones such as the skull and clavicle.
-
What is endochondral ossification and its significance? (3)
Endochondral ossification is the process where long bones form from a cartilage model that gradually converts into bone.
It is crucial for the formation of axial and weight-bearing bones.
This method of ossification is used in the formation of most long bones such as the femur and humerus.
-
What is a chondrocyte and its function in bone growth? (2)
A chondrocyte is a mature cartilage cell responsible for producing the cartilage matrix.
In the growth plate, chondrocytes undergo hypertrophic differentiation to facilitate linear bone growth.
-
What is the growth plate and its role in bone development? (2)
The growth plate is a specialized cartilage structure located at the metaphysis of long bones.
It allows for linear bone growth by producing new cartilage that is later converted into bone.
-
What is an osteocyte and what role does it play in bone? (3)
An osteocyte is a terminally differentiated osteoblast encased within mature bone.
It is connected via dendritic processes that form a network throughout the bone.
Osteocytes have a mechanosensory role and are thought to be the master regulators of bone remodeling.
-
What is an osteoblast and its function in bone formation? (2)
An osteoblast is a bone cell responsible for secreting osteoid, the organic matrix of bone.
Osteoblasts play a key role in forming new bone by mineralizing the osteoid to become mature bone.
-
What is an osteoclast and its role in bone remodeling? (2)
An osteoclast is a large, multinucleated cell responsible for resorption of bone.
It plays a critical role in bone remodeling by breaking down old bone to allow for new bone formation.
-
What is osteoid and its role in bone formation? (2)
Osteoid is the organic matrix of bone, primarily composed of collagen and other proteins.
It is secreted by osteoblasts and later mineralized to form mature bone tissue.
-
What is bone remodeling and its importance? (2)
Bone remodeling is a continuous process where old or damaged bone is removed by osteoclasts and replaced by new bone formed by osteoblasts.
This cycle is essential for maintaining bone health and repairing damage over time.

