Capillaries I (Physiology)
Session summary This lecture is about solutes and the movement of solutes in capillaries and tissue fluids. The cell membrane has very important functions and is a protective barrier, but it is also a barrier to solute transport. The lecture will consider the main mechanisms of transporting solutes across the cell membrane. The capillary membrane refers to the capillary wall (endothelial cells and associated structures) and controls solute transport between blood plasma and the interstitial fluid that bathes the cells of the body. Ways in which the capillaries are adapted for transport along with ideas about permeability including Fick’s law of diffusion will be introduced. These processes are essential for delivering oxygen and nutrients to the tissues. Learning outcomes At the end of this session you will be able to: Outline membrane transport mechanisms Describe capillary structure and variations present in different types of capillaries Relate the variables in Fick's law to membrane structure (cell and capillary) and physiological solutes Explain how the concept of permeability incorporates several of the variables in Fick's law Discuss factors at the physiological level that affect the rate of transport by diffusion
-
A H2O solution containing various substances will enter cells from the interstitial fluid, what are these substances?
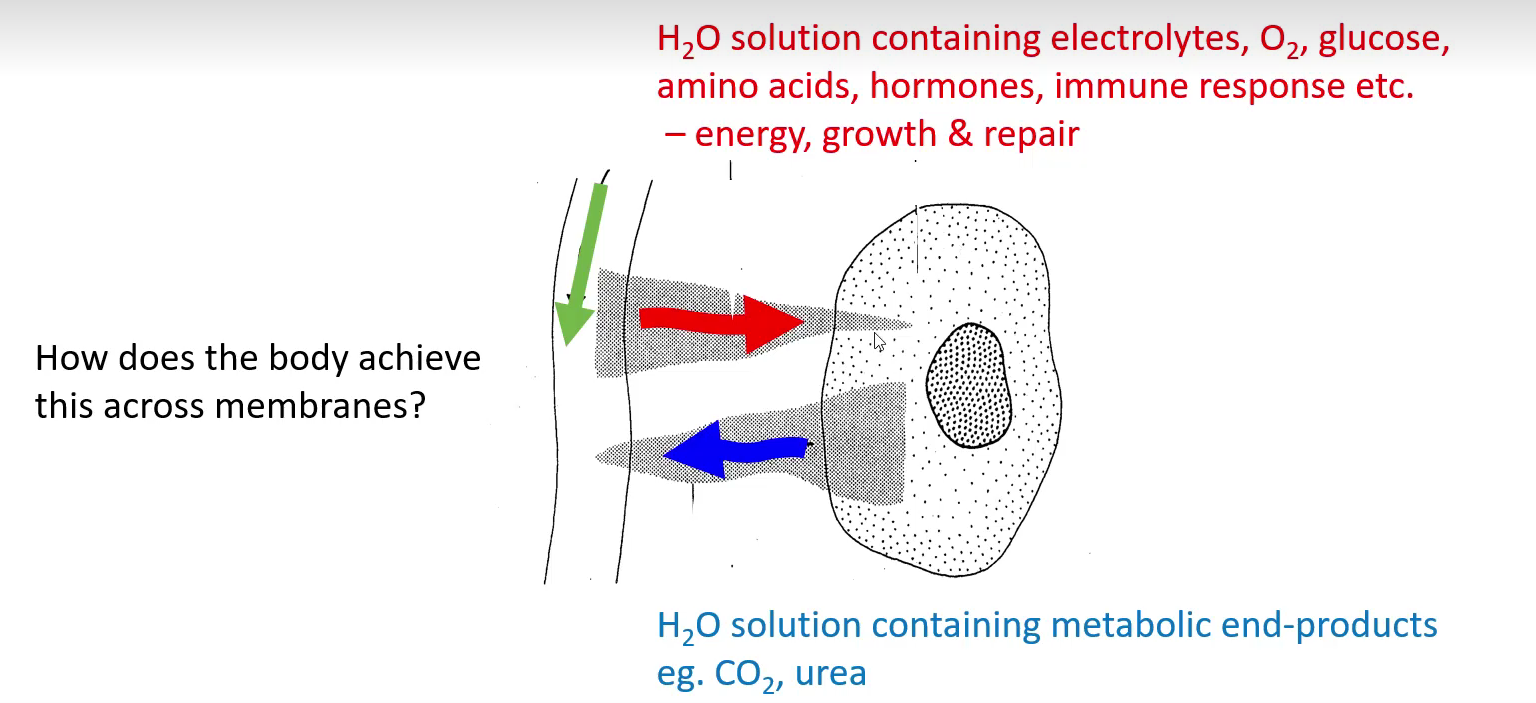
H2O solution containing electrolytes, O2, glucose,amino acids and hormones
-
A H2O solution containing various substances will exit cells into the interstitial fluid, what are these substances?
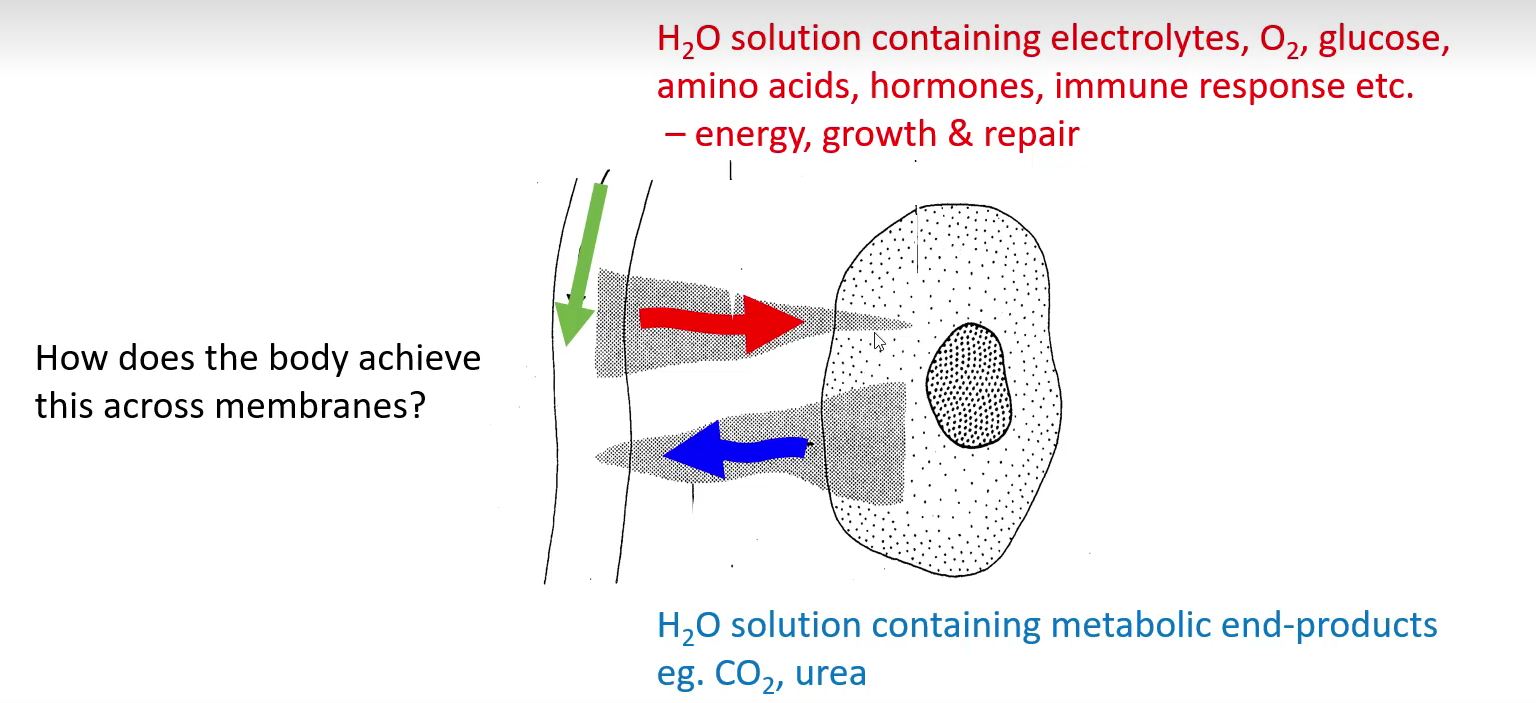
H2O solution containing metabolic end-products e.g. CO2 and Urea
-
State some information about the cell bilayer:
Structure
• Consists of two layers of amphipathic phospholipids• Phosphate head is polar (hydrophilic)• Fatty acid tails is non-polar (hydrophobic)• Form bilayers in solution
Provide support and protectionCell-to-cell recognition – eg. immune systemControls what enters or leaves the cell – e.g. ion movement in nervesRegulates cell function – eg. Insulin-mediated glucose uptake
-
Describe passive transport:
-Movement of molecules DOWN a gradient-Concentration / Pressure / Osmotic / Electrical-Does not require energy-Simple (O2/CO2) or facilitated (ions, glucose)
-
Describe active transport:
-Movement of molecules AGAINST a gradient-Requires energy (uses ATP)-e.g. ATP-dependent pumps, endocytosis, exocytosis
-
State the four passive transport processes and give examples:
Diffusion
Concentration gradient. i.e. O2 uptake from lungs into blood
Convection
Pressure gradient. i.e. blood flow from heart to blood vessels
Osmosis
Osmotic pressure gradient. i.e. Water uptake by cells
Electrochemical flux
Electrical and concentration gradient. i.e. ion flow across cell membranes
-
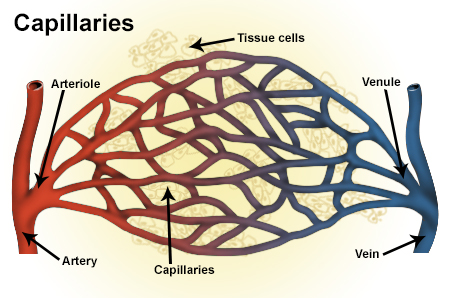
State some information about Solute and fluid exchange occurs at capillaries: (5)
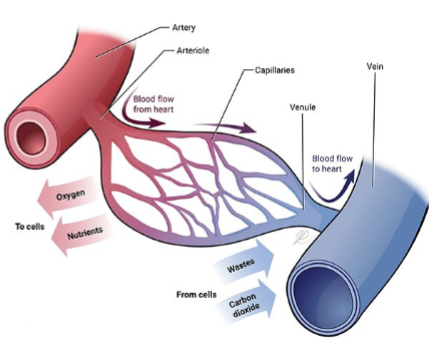
-Connect terminal arterioles to venules - extension of inner lining of arterioles
-Smallest diameter blood vessels endothelium, 1 cell thick, semi-permeable
-Found near every cell in the body but higher density in highly active tissue (muscles, liver, heart, kidney, brain etc)
-Solute exchange (passive diffusion): electrolytes, O2, glucose, amino acids, hormones, drugs
-Fluid exchange along pressure gradients. Regulation of plasma and interstitial fluid volumes
-
What are four properties of passive diffusion?
-Does not require energy (no ATP)
-Molecules move randomly
-Move from area of high to low concentration
-Great for transport of lipid soluble solutes over very short distances, eg. O2, CO2
-
What is the formula for time taken that includes net distance (x)?
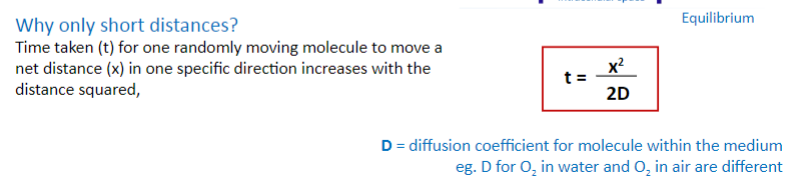
t=x^2/2D
-
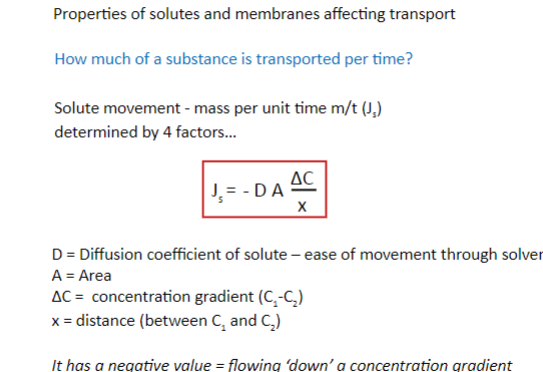
Properties of solutes and membranes affect transport: What are the properties of the solute? (3)
-Concentration gradient-Size of the solute-Lipid solubility of solute (lipophilic, lipophobic nature)
-
Properties of solutes and membranes affect transport: What are the properties of the membrane? (4)
-Membrane thickness/composition-Aqueous pores in the membrane-Carrier-mediated transport-Active transport mechanisms
-
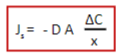
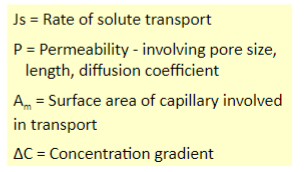
State Ficks law and its formula and what each constant in the formula means
-
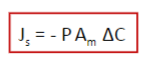
Name some characteristics of the continuous capillaries:
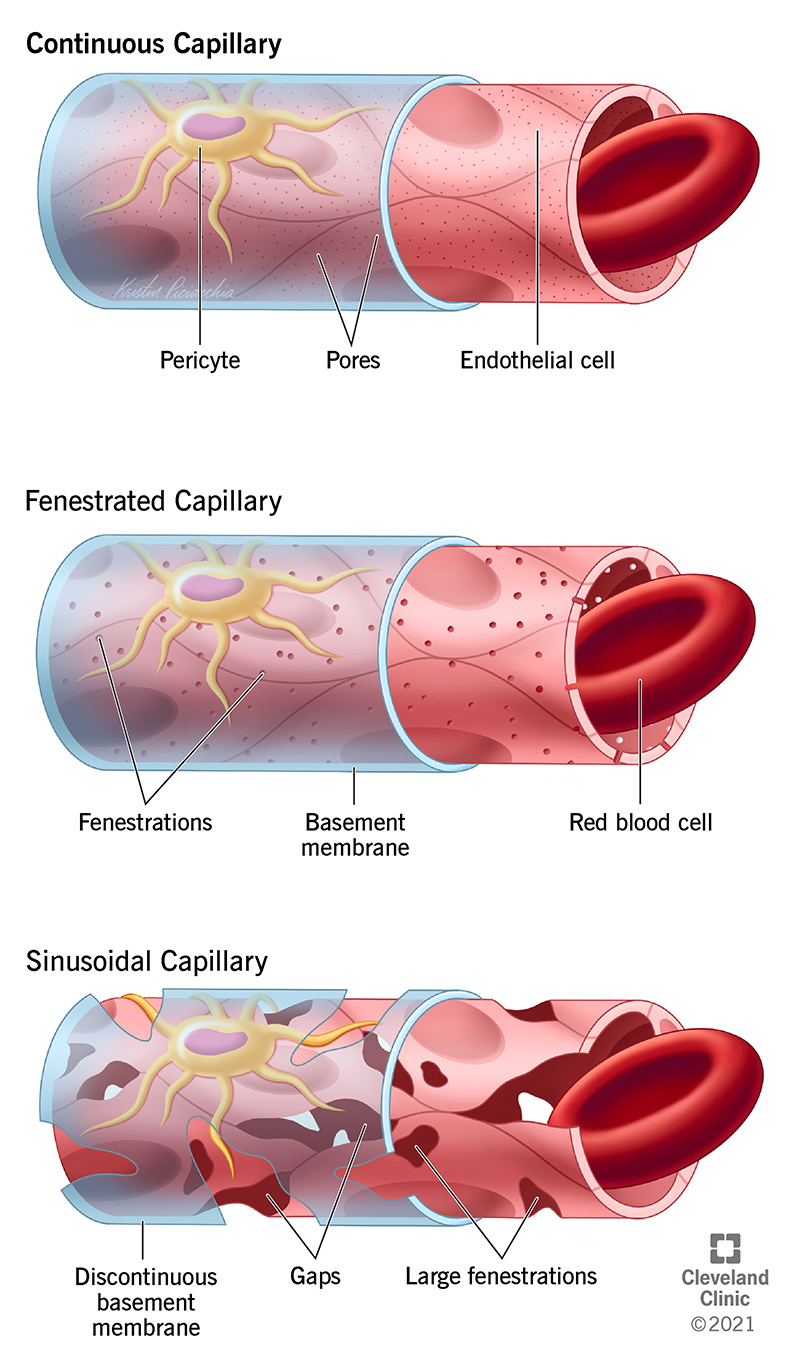
• Moderate permeability; tight gaps between neighbouring cells; constant basement membrane• Blood-brain barrier
• muscle, skin, fat, connective tissue
-
Name some characteristics of the fenestrated capillaries:
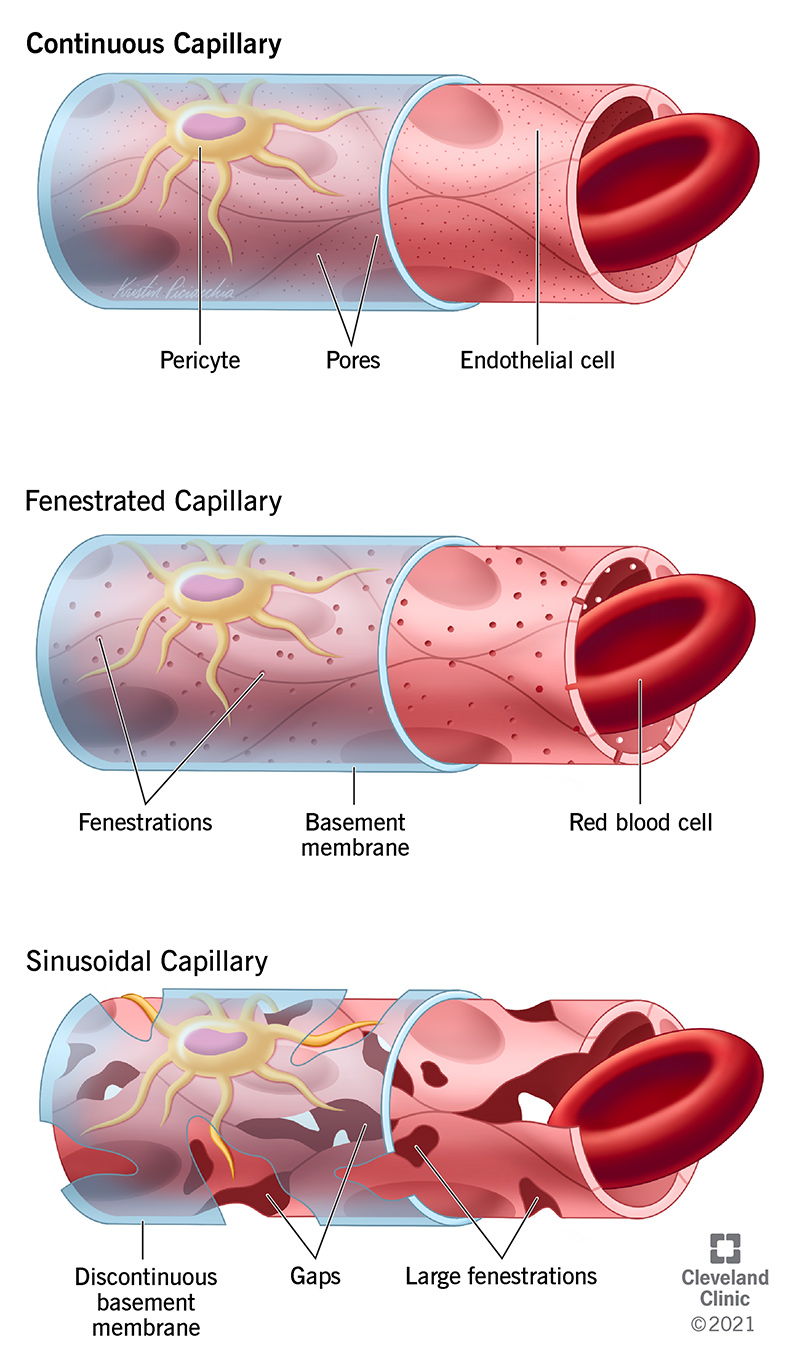
• High water permeability, fenestration structures, modest disruption of membrane
• ‘High water turnover’ tissues e.g. salivary glands, kidney, synovial joints, anterior eye, choroid plexus (cerebrospinal fluid), gut mucosa
-
Name some characteristics of the discontinuous capillaries:
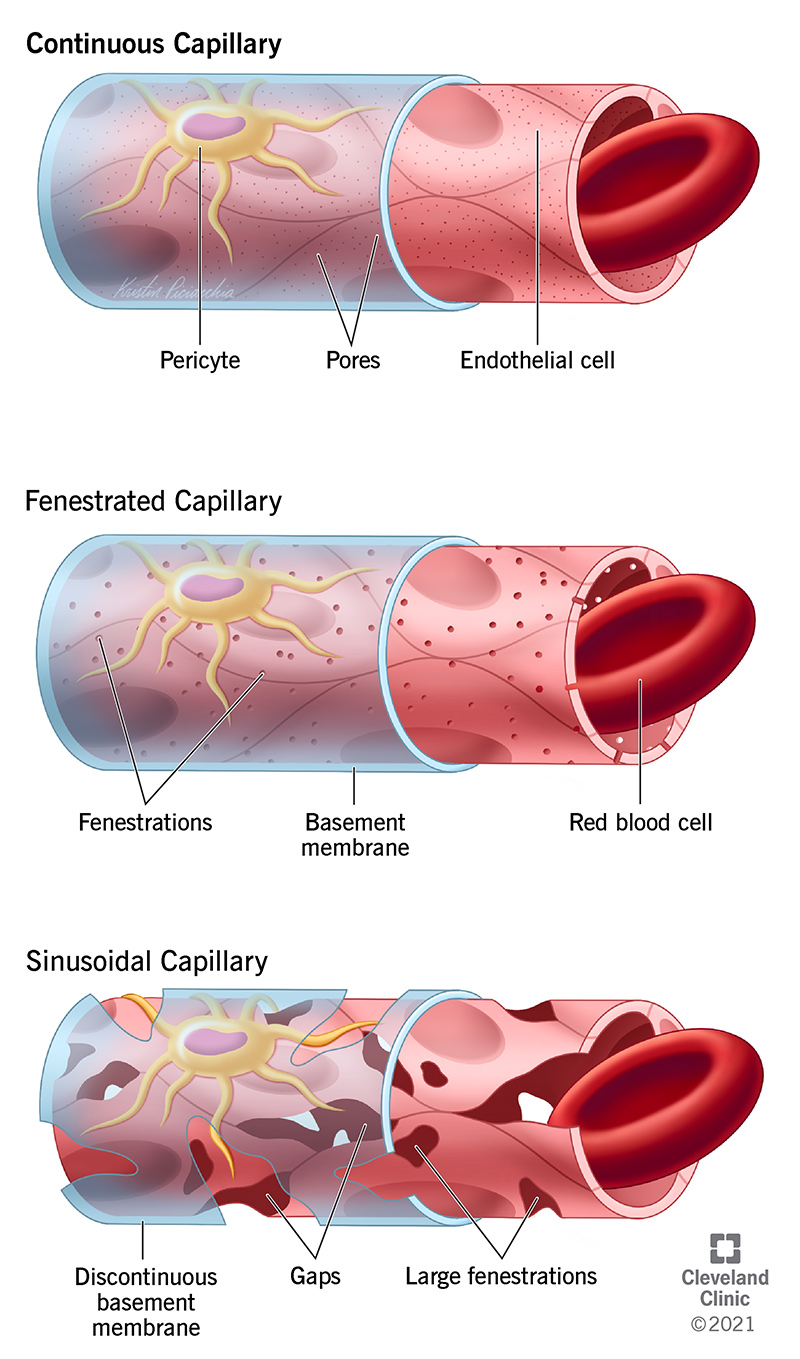
• Very large fenestration structures, disrupted membrane
• When movement of cells is required; RBCs in liver, spleen, bone marrow
-
What are 3 important properties of the capillary
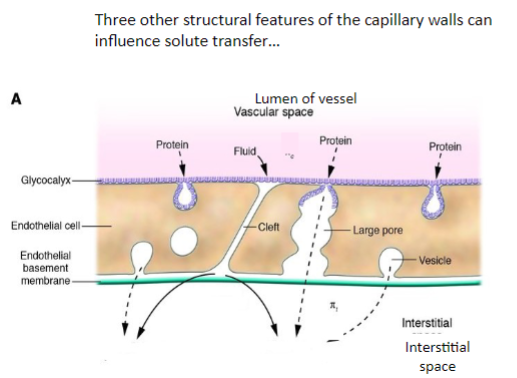
Intercellular cleft
10-20 nm wide
Caveolae & vesicles
Large pore system
Glycocalyx
Covers endothelium, negatively charged material, blocks solute permeation and access to transport mechanisms, highly regulated
-
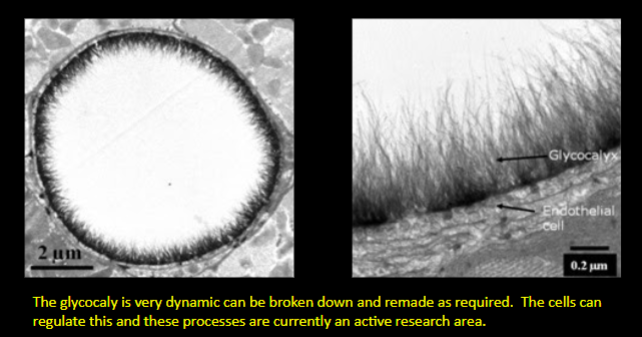
Picture demonstrating real structure of the glycocalyx:
-
What is Permeability?
Is the rate of solute transfer by diffusion across unit area of membrane per unit concentration difference ie. ’how freely a solute crosses a membrane’
-
What is the equation for the rate of solute transport that includes x (increased path length through the membrane)
-
What do the constants in both the modification of ficks law formula and formula for the rate of solute transport that includes x mean?
-
What is the modification of fick's law for a porous membrane?
-
A picture summarising solute transport - diffusion and filtration:
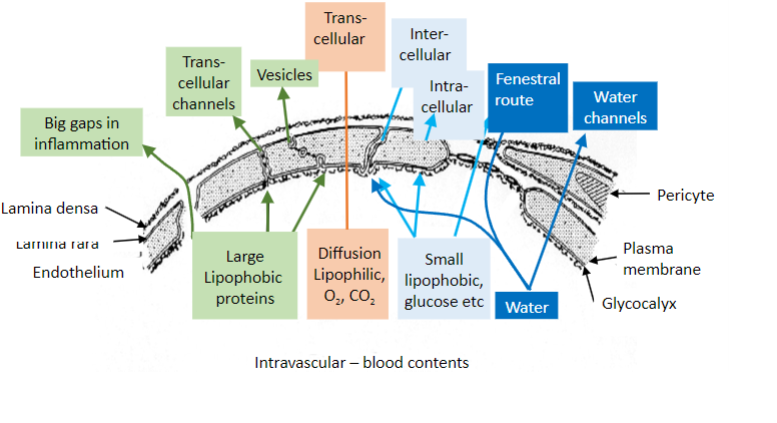
-
Picture outlining how to calculate the dominant route of transport - diffusion or filtration?
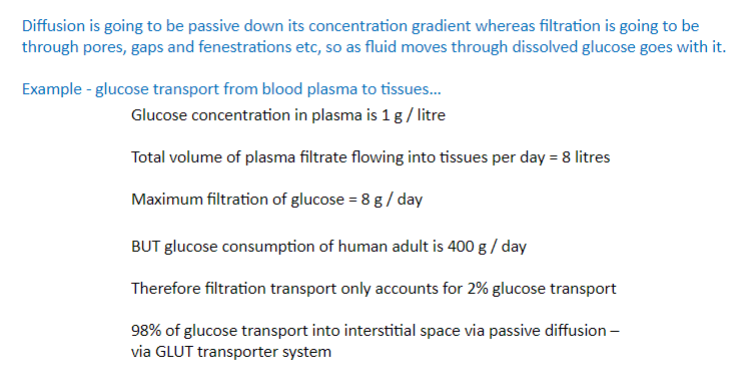
-
State 3 ways on how diffusion rate is controlled physiologically
-Blood Flow
-Falls in interstitial concentration
-Recruitment of capillaries
-
How does blood flow control heart rate? (long answer)
-More blood brings more solutes. Increased bloodvolume means less time for equilibration to occuracross capillaries.-eg. Flow limited diffusion where there is slow flowin a long capillary. O2/CO2 equilibrate over proximalsection and then there is little diffusion over therest of the vessel. Sometimes occurs in sepsiswhere blood pressure and flow are low, can lead toischaemia
-
How does a fall in interstitial concentration of ions control heart rate? (long answer)
During metabolism more solute is used up therebyincreasing the concentration difference.Also, metabolism increases blood flow - increased O2delivery, controlled by the arterioles.
-
How does the Recruitment of capillaries control heart rate? (long answer)
Dilation of arterioles leads to increased number ofcapillaries perfused which increases total surfacearea A for diffusion (Fick’s law). Also this shortensdiffusion distance between capillary and cell.
-
O2 transport from blood to muscle increases over how many times during strenuous exercise?
40x

