-
Cardiac location
1. heart is located in left-middle of chest (mediastinum).
2. approx the size of your fist. Weights about 1lb.
3. Pumps blood and oxygenates body, nutrients delivery, waste removal.
-
Cardiac structures
1. know route of blood circulation how it goes through heart.
-
Cardiac Chambers
1. right atrium: thin walled, receives unoxygenated venous blood from IVC/SVC.
2. Right ventricle: thin walled (.5cm), low pressure, receives blood from right atrium, pumps blood to the lungs via the pulmonary artery.
3. Left atrium: receives oxygenated blood from the lungs via pulmonary veins and pumps it into the left ventricle.
4. Left ventricle: thick walled (1.5 cm), high pressure, receives blood from the left atrium and sends blood to the body via the aorta.
-
AV Valves
1. mitral valve b/t LA/lv, two cusp valve between left atrium and left ventricle.
2. Tricupsid valve b/t RA/RV three-cusp valve between right atrium and right ventricle.
3. these valves are open during diastole and closing during ventricular contraction (systole) to prevent reflux of blood into atria. Closure creates s1, heart sound "lub".
4. Maintain unidirectional flow of blood (prevents backflow of blood)
5. Open and close due to pressure gradients.
6. Both valves are held by strong filaments, chordae tendinae, arise from papillary muscles of ventricles. these structures help keep the valve closed during systole.
-
Semi lunar valves
1. pulomonary valve: b/t RV and PA
2. Aortic valve b/t LV and aorta.
3. open during systole, closed during diastole, closure creates s2 heart sound 'dub'
4. Closure prevents backward flow into the ventricles.
-
Coronary arteries
1. provides blood to the electrical and mechanical structures of the heart during diastole.
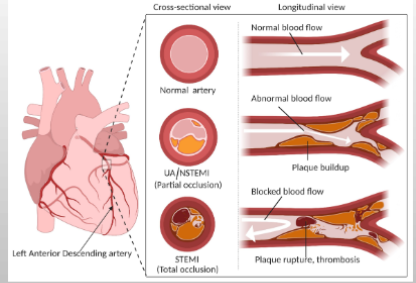
2. LCA = left coronary artery
, LAD- left anterior descending, LCA- left circumflex, RCA- right coronary
-
Cardiac Electrophysiology
1. Automaticity: the ability to initiate an impulse
2. Excitability: ability to respond to a impulse
3. Conductivity: ability to transmit an impulse.
4. Contractility: the ability to respond to the impulse with a pumping action.
5. Refractoriness: time period when the heart cannot respond to a impulse.
-
Absolute vs relative refractory
1. absolute refractory: cannot cause another repolarization no matter what.
2. relative refractory: with enough energy greater than initial amount can cause another repolarization.
-
Cardiac electrophysiology
1. sympathetic - flight or flight: increase HR, force of contraction and impulse conduction (adrenergic)
2. Parasympathetic - feed / breed - decrease heart rate, force of contraction and impulse conduction (vagal)
-
Pace makers of the heart
1. SA node: rate 60-100 bpm "normal pacemaker of the heart"
2. Internodal pathways: connect SA to AV node, located where SVC meets RA, includes Bachman's bundle, Wenckebach's bundle.
3. AV node: 40-60 bpm, located in RA, medially and just above tricuspid valve.
4. Bundle of HIS purkinje/ventricles: 20-40 bpm, passes between mitral and tricuspid valves downward through septum, branches to RBBB, LBBB and then purkinje fibers.
5. SA node -> av node -> bundle of HIS if fails.
6. Any single cell inside heart and generate impulse to beat.
-
Correlation of Electrical and Mechanical Events
1. If you know what is happening in the Mechanical system (blood flow, valve opening and closing, contractions) you can then correlate it to the activities of the ELECTRIAL system of the heart.
-
Cardiac Cycle - Ventricular Diastole
1. T-P interval
2. Isovolumetric relaxation
3. Begins with the closure of aortic and pulmonic valves
4. Period of rapid filling and feeding the coronary arteries
5. Ends with opening of mitral and tricuspid valves.
-
Cardiac cycle - Late ventricular Diastole
1. P wave and PR interval
2. Atrial contraction - atrial contracting SA node is firing
3. Atrial kick (15-25% of C.O.) - Starlings law - if you overstrech a vessel and let it relax, it will force more, atria OVERFILL ventricles, causing increase in Cardiac Output.
4. Atrial kick is lost during A fib, CHB/F.
-
Cardiac cycle - Ventricular Systole
1. Mitral and Tricuspid valves are closed
2. Pulmonary and aortic Valves open
3. Contraction occurs and Stroke volume is ejected
4. ST segment - rapid ejection
5. T wave - reduced ejection
6. Normal ejection fraction is > 60%.
-
Normal ECG
1. P wave - depolarization of the atria in response to SA node firing.
2. PR interval - delay of AV node to allow filing of ventricles.
3. QRS complex - depolarizations of ventricles triggers main pumping contractions.
4. ST segment - beginning of ventricle repolarization, should be flat.
5. T wave - ventricular repolarization.
-
P wave
1. represents atrial depolarization
2. Usually first deflection seen on ECG
-
PR interval
1. normal PRI is 0.12 to 0.20 seconds (3-5 small boxes)
2. Represents the time of transmission of the electrical impulse from the atria to the ventricles.
3. Measured from the beginning of the P wave to the beginning of the QRS.
-
The QRS complex or interval
1. Normal QRS width is 0.06 to 0.12 seconds (1.5 to 3 small boxes)
2. Represents the spread of the electrical impulse through the bundle of HIS and bundle branches to the purkinje fibers resulting in ventricular depolarization.
3. Measured from the beginning of the QRS to end of the QRS.
4. 1st Negative deflection on the ECG (q), then a positive deflection (r), then another negative deflection (s).
-
The ST segment
1. This represents the early phase of repolarization of the ventricles.
2. Measured from the end of the QRS (j point) to the beginning of the T wave.
3. ST segment is usually ISOELETRIC. Elevation or depression of the ST segment may be indicative of MI or ischemia.
-
The QT Interval
1. Length varies with HR.
2. Represents the total time from the onset of ventricular depolarization to the completion of repolarization.
3. Causes of lengthened QT interval: drugs haldol, antibiotics, antiemetics, TCAs, sotol, quinidine, hypokalmeia, hypocalcemia, hypothermia.
4. Normal QT is 0.30 to 0.45
5. QT interval should be 1/2 of the R-to-R interval.
6. measured from beginning of QRS to end of T wave.
-
T wave
1.represents ventricular repolarization
2. Abnormalities may represent MI, ischemia, or electrolyte imbalances.
3. The onset of QRS to mid peak of the T wave represents the absolute refractory period. The midpoint to the end of the T wave represents the relative refractory period.
-
ECG/EKG changes in hyperkalemia
1. Wide qrs
2. Loss of p wave
3. Tented T waves.
4. Sine Wave pattern, V fib.
-
Standard Limb lead
1. RA LA LL RL
2. Lead II default lead (going in direction of heart)
3. The further apart the leads, the better quality picture of ekg.
4. Avoid bone, don't move
-
3 vs 5 vs 12 lead
1. cloud over grass, smoke over fire , chocolate in the middle
2. On 3 lead lose green and brown.
3. The lead placement is same for all three.
4. 5 Lead systems are better than 3 lead systems because they allow for a "true" V lead.
5. 12 lead looks at the heart from 12 different angles and gives the most info for dx dysrhythmias.
6. Flip ekg to right side if right side damage is suspected.
7. Most 5 leads systems will allow you to run two leads simultaneously. Lead 2 has nice upright p waves, qrs, easy to count and diganose atrial ryhtms.
8. V lead- diagnoses vt, bbb, pvcs. in any post MI pt, the V lead should be one of your leads.
-
R to R interval
1. Beginning of QRS to beginning of next QRS
2. Useful for measuring ventricular rate and regularity.
-
Calculating the Heart rate
1. six second strip method
2. six seconds = 30 large boxes
3. Count # of QRS complexes in 6 seconds and multiply by 10 to get the HR in beats per minute.
-
Systematic approach to EKG interp
1. Count the rate (atrial=p waves and ventricular=qrs)
2. Is it regular or irregular? (spacing consistent?)
3. Is there a P wave for each QRS?
4. Is the PRI normal?
5. Is the QRS normal? (normal vs wide)
6. What is the rhythm?
-
Normal sinus rhythm
1. HR 60-100bpm
2. Rhythm: regular
3. P wave: before each qrs, identical
4. PR interval: 0.12-0.20
5. QRS: <12 seconds
-
Sinus bradycardia
1. HR: <60bpm
2. Rhythm: regular
3. P wave: before each qrs, identical
4. PRI: 0.12-0.20
5. QRS: <12
6. causes: slow firing of SA node, increased vagal tone. can be caused by drugs (b-blockers, ca channel block, digoxin) or result of hypothermia or hypothyroid. Normal in athletes.
7. s/s: usually asymptomatic. if pronounced can lead to fatigue or syncope, sob, dizzy, hypoBP, sx of HF.
8. Tx: correct underlying cause. Acutely give atropine and/or pacing. Chronically pacemaker if symptomatic. atropine doesn't work on alcohol.
-
Sinus Tachycardia
1. hr > 100 bpm
2. Rhythm: regular
3. P wave: before each qrs, identical
4. PR interval: 0.12-0.20
5. QRS <0.12 secs
6. Cause: increased stim of SA node due to increased sympath tone (FOF) exercise, caffiene, drugs like Dopamine, epi, albuterol, or patho due to sepsis fever hyperthyroid hypoxemia.
7. S/s: fatigue, CO dec, may have palps, dizzy, may cause ischemia in post MI pts.
8. tx: underlying cause: pain, sepsis, or fever. freq nurse assessments and VS. WATCH TRENDS. possbily beta blockers or Ca channel blockers.
-
Supraventricular Tachycardia (SVT)
1. hr: 140-250 bpm (most start at 160)
2. Rhythm: Regular
3. P wave: abnormal P before each QRS (diff to see)
4. PR interval: <0.20
5. QRS < 0.12 secs
6. Cause: caffeine, eoth, excitement, anxiety
7. Loss of atrial kick, rapid rate, difficult to dx.
8. Tx is LEAST INVASIVE FIRST, vagal maneuvers (valsalva, vagal stim) ice buckets, 1st line drug is adenosine (6mg slam half life of seconds, 12mg second dose, shock), beta blockers, and Ca channel blockers. Synchronized cardioversion if unstable.
-
Atrial Fibrillation
1. HR: A: 350-650 bpm, V: slow to rapid
2. Rhythm: irregular (regularly irregular)
3. P wave: fibrillatory (fine to course)
4. PR interval: n/a
5. QRS<0.12
6. Numerous ectopic foci near pulmonary veins produces an erratic quivering of the atria.
7. Lose atrial kick
8. Cause: age, MI, cardiac surgery, CHF, digoxin tox, HTN, DM
9. S/s: if rapid ventricular response rate, may be dizzy and SOB, lose atrial kick, so CO is dec. May have thrombus formation
10. Tx: chronic vs new onset, control rate (diltiazem, digoxin, b blockers, Ca block), anticoagulate, inr 2-3, synch cardio vert once fully anticoagulated, catheter ablation.
11. Nursing care is to doc strips, assess for s/s of dec CO monitor effect of drugs.
-
Atrial Flutter
1. HR: A: 220-430 bpm, V: <300 bpm
2. Rhythm: regular or variable
3. P wave: sawtoothed appearance, consistent numerous p waves
4. PR interval: n/a
5. QRS <0.12 seconds
6. Cause: one irritable focus in the walls of the atria stimulate atria to contract.
7. Causes: MI, valvular heart disease, cardiac surgery, organic heart disease.
8. S/s: R/T ventricular response. May be SOB, dizzy if rate is fast.
9. Tx: control rate (digoxin, verapamil, b blockers), anticoagulated, inr 2-3, synchronized cardioversion once fully anticoagulated, catheter ablation.
10. Nursing care is to frequently assess, document rhythm changes, prepare for cardioversion.
-
1st Degree AV Block
1. Rhythm: regular, impulse originates in SA node but has a delayed conduction through the AV node resulting in a prolonged PRI.
2. Rate: usually normal
3. P waves: normal
4. PRI > 0.20 seconds
5. QRS: normal
6. Cause: inferior wall MI, digoxin tox, hypo/hyperk, use of b block, Ca block, quinidine.
7. Tx: benign, Correct cause, atropine if symptomatic. Observation.
-
Second Degree AV Block, Type 1: Mobitz 1 or Wenckebach
1. Rhythm: regular, some impulses from the SA node are blocked from passing all the way to ventricles resulting in dropped beats.
2. Rate: usually normal
3. Waves: normal except more P's than QRS's
4. Intervals: PRI increases until a beat is dropped.
5. Causes: IWMI, digoxin tox, CABG surgery
6. Tx: observation, if symptomatic may need atropine, pacing, dopamine.
-
Second Degree AV Block Type II - Mobitz II
1. Rhythm: atrial regular, ventricular irregular.
2. Rate: atrial > ventricular
3. Waves: More P waves than Qrs's
4. Intervals: For each QRS conducted, PRI is identical and normal, then QRS dropped
5. Causes: AWMI, digoxin tox
6. Tx: pacemaker if symptomatic, external pacing pads on stand-by mode, atropine, dopamine ,or epi if symptomatic.
-
Third Degree Heart Block (lethal)
0. P wave: normal but not related to QRS
0. PR interval: none
1.Complete AV dissociation: "no relationship between the P's and QRS's"
2. Heart's electrical activity is divided in two, AV node conducts atria and escape rhythms conduct ventricles.
3. Causes: MI, digoxin tox, chronic degeneration of conduction pathways.
4. Sx: light headedness, syncope
5. Tx: pacemaker, atropine, dopamine or epi if symptomatic
-
Premature Ventricular Contractions (PVCs)
1. Escape foci from ventricle, originates outside the normal conduction pathway. Wide QRS, no P waves seen with QRS. QRS is wide and bizarre.
2. Cause: acute MI, ischemia, electrolyte imbalances (k, mg), acidosis, hypoxemia, stress, stimulants, drugs.
3. Usually asymptomatic
4. Nursing Interv: check o2 sats, check/replace electrolytes, monitor pt and doc occurence, meds: amiodarone?
5. Danger: multifocal- more than one shape of QRS, triplet: occur in groups of three qrses
-
Ventricular Tachycardia (lethal)
1. Single, irritable focus in ventricles
2. Causes: MI, CHF, cardiomyopathy, hypoxia, electrolyte imbalances, acidosis, med tox such as Dig, stimulants like cocaine, amphetamines, mechanical irritation.
3. S/s: stable (pt has pulse, talking, bp ok), pulseless (dead)
4. Tx: if stable, amiodarone and/or electrical cardioversion, If pulseless immediately start CPR and defib in code blue setting. Long term may warrant AICD.
-
Torsade de Pointe
1. Rate: 150-200
2. May quickly become V fib
3. Tx: CODE BLUE, Magnesium as first line drug.
4. Treat like V tach... CPR, DEfib, Epi
-
Ventricular Fibrillation (lethal)
1. HR: 300-600 (never will have a pulse)
2. Rhythm: extremely irregular
3. P wave: absent
4. PR interval: n/a
5. QRS: fibrillatory baseline
6. Chaotic, irregular electrical activity
7. Quivering ventricle from multiple foci
8. No blood flow = no Cardiac output = no pulse
9. Cause: ischemic heart disease, chf, cad, mi , hypoxia, acidosis, electrolytes
10. Tx: CODE BLUE (start cpr, shock, epi)
-
Asystole
1. HR, rhythm, p wave : absent
2. No CO = a lethal rhythm
3. Confirm in 2 leads (is it fine V-fib? has a lead popped off?)
4. Call CODE BLUE, treat per ACLS algorithm.
5. Look for causes (5 H's and T's)
6. If have a rhytm, is it a perfusing BP/hr?
-
Causes of Lethal Rhythms:
1. H: hypoxia, hypothermia, hypovolemia, hypo/hyperk, hydrogen ion acidosis.
2. T: tension pneumothorax, tamponade, tablet OD, thrombus: MI, thrombus PE
3. Hypo/hyperglycemia.
-
Nursing Responsibilities for Cardiac
1. Print measure interpret and post a rhythm strip at the beginning of your shift.
2. Get a 12 lead ECG for any rhythm changes
3. Get a set of vital signs for any rhythm changes.
4. Know your unit standards and when to notify the MD.
-
Cardiac Labs to know
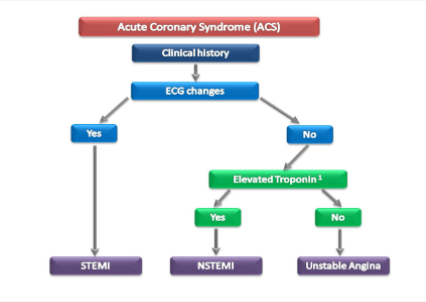
1. Troponin or High Sensitivity to troponin 0.04ng, below 14ng for high sens.
2. Lipid Profile
3. BNP <100 pg/mL
4. INR, PT(11-13.5sec), PTT(25-35), Heparin Xa if anticoagulated
5. Electrolytes
-
Management of Cardiac Arrest
1. CPR: start compressions, maintain patent airway, ventilate with mouth-to-mask device
2. Advanced Cardiac Life Support: defib, cardiovert, meds, advanced airways/interventions
-
Cardioversion - If pulse present
1. Synchronized countershock
2. Used in emergencies for unstable ventricular/supraventricular tachycardia dysrhythmias.
3. Used electively for stable tachydysrhythmias resistant to medical therapies.
4. Must be sedated. (relative)
-
Defibrillation - if no pulse
1. Asynchronous countershock that depolarizes critical mass of myocardium simultaenously to stop re-entry circuit and allows sinus node to regain control.
-
We have pulses, Now what?
1. ROSC
2. Reassess ABCs and intervene appropriately
3. Targeted temp management (TTM): decrease metabolic oxygen demand, decrease core temp to 36 or 32 degrees C.
4. Prevent event from happening again: or be prepared for it to happen again.
-
SVT Case Study
1. IV, Labs, fluid replacement/adenosine 6mg->12mg->cardiovert shock (sedate before).
-
Radiofrequency catheter ablation
Ablate a fib.
2. Surgical procedures: permanent pacemaker, implantable cardioverter/defibrillator.
-
Pacemakers
1. Pacemakers provided a timed electrical stimulation to the heart that then depolarizes the cardiac tissue causing contraction.
2. A spike will show on the ECG rhythm and should be followed by evidence of depolarization or CAPTURE of the cardiac cells. Capture is assessed by the presence of a pulse. Capture = for each spike there is a QRS conducted.
-
Indications for a pacemaker
1. Bradycardic rhythms including Second Degree Heart Block Type II and Third Degree Heart Block.
2. LEFT BBB, Severe HF, Post-op CABG, to override atrial fibrillation.
-
Types of Pacemakers
1. Temporary pacing - noninvasive and invasive. Transcutaneous - with pads, Transvenous - wire in heart.
2. Permanent pacemakers: SQ placed generator with wires that go down into heart.
-
Pacemaker Settings
1. Synchronous - works with the patient's heart and is used only "on demand"
2. Asynchronous - works on a fixed rated no matter what the patient's intrinsic rate is doing.
-
Leadless Pacemaker Device
1. Newest tech, uses a single chamber leadless system pacing only anchored in the right ventricle muscle.
2. Can go through MRI
3. No pocket infections, no lead movement
4. Implant takes 30-40 mins.
-
Nursing Care for Pts w/ Pacemakers
1. Pre-op teach
2. Assess pacemaker settings
3. Assessing capture/sens
4. Assessing Rhythm strip
5. Postop teach: no lift/reach until leads seed. Watch for s/s of infection, BP/pulse. Monitor, carrying pacemaker info card at all times, no MRI, electromagnetic areas.
6. Battery life of 5-15 years.
-
Pacemaker Failure to Sense
1. Pacemaker does not sense underlying rhythm and pacemaker fires during an excitable period.
2. On the QRS or on the T wave.
-
Pacemaker Failure to Capture
1. Pacemaker spikes without "capturing" and depolarizing the ventricles.
2. The energy level of the pacemaker is not set high enough, or has moved so the ventricles do not respond.
3. You see the pacemaker spike, but no pulse accompanies it!
-
Pacemaker/AICD combination
1. Has all the capabilities of a pacing brady rhythms and defib lethal rhythms.
-
Teaching for AICD's
1. Need to stay on antiarrhythmic drugs
2. If you get a shock, sit down and have someone notify their physician.
3. Discomfort with shock
4. Stay away from electromagnetic fields.
5. Family needs to learn CPR
6. No MRI
7. Have your card with you at all times.
-
Life Vest
1. in meantime device for potential pacemaker candidate, will shock lethal rhythms.
-
Aneurysms of Central Arteries
1. Permanent localized dilation of artery, enlarging artery to twice its normal diameter.
2. Classification:
3. By vessel wall involvement: true or psuedo aneurysms
4. By shape: fusiform (entire vessel wall), saccular
5. By location: abdominal aortic, thoracic aortic.
-
Anatomy of Aorta
1. Intima, Media, Adventitia.
2. In aneurysms, failure in wall.
-
Aneurysms of Central Arteries
pic from textbook to know different types of arteries mal.
-
Assessment of Aortic Aneurysms
1. Most patients ASYMPTOMATIC.
2. Physical assessment is NOT considered a strong tool for dx aneurysm. Do not palpate abdomen.
3. Pain in abdomen, flank, back if abdominal.
4. Abdominal mass is pulsatile if >5cm and patient is very thin.
5. Assess for sob, hoarseness, difficulty swallowing, chest pain if thoracic.
6. Tearing sensation going to back = ruptured aneurysm.
-
Dx assessment of Aneurysms
1. CT is GOLD STANDARD
2. Frequent dx imaging to track changes in diameter of aneurysms.
3. UA, quick suspect
4. Aortic arteriography if going to OR.
-
Non-surgical management of Aneurysm
1. Monitor aneurysm growth with frequent CT scans.
2. Maintain BP at normal level to decrease risk of rupture - treat hypertension! Use Beta Block / Ace inhibs.
3. Nurse is responsible for performing frequent assessments of BP, HR, peripheral circulation and pain level.
-
Endovascular Repair of Abdominal Aortic Aneurysm
1. For elective surgeries, patients at high risk for major abdominal surgery.
2. Least complications, quickest recovery.
3. Use a flexible Dacron stent graft.
-
Abdominal Aortic Aneurysm Surgical Resection
1. Preop care depends on if emergent or elective.
2. Bowel prep.
3. Teaching TC+DB.
4. Peripheral pulses assessment
5. IVF
6. Blood
7. Informed consent
-
PostOp Care for Abdominal Aneurysm
1. Hemodynamic monitoring
2. BP management
3. Assess/prevent complications: MI, graft occlusion/rupture, renal failure, hypovolemia, resp distress, paralytic ileus.
4. Avoid flexion of the graft
5. Discharge teaching.
-
Thoracic Aortic Aneurysm repair
1. Preop care
2. Op care
3. Post op care assessment: VS, complications, sensation and motion in extremities, resp distress - on vent, cardiac dysrhythmias.
-
Rupture
1. Pts w/ a ruptured AAA may present in frank shock as evidenced by cyanosis, mottling, AMS, tachycardia, and hypotension.
2. At least 65% of pts w/ ruptured AAA die from sudden cardiovascular collapse before arriving at hospital.
3. Mechanical stress acting on the arterial wall exceeds the strength of the wall issue.
4. Hemorrhagic and hypovolemic shock.
-
Risk of rupture (no memory)
1. Less than 4.0 cm in diameter = less than 0.5%
2. Between 4.0 to 4.9 cm in diameter = 0.5 to 5%
3. Between 5.0 to 5.9 cm in diameter = 3 to 15%.
4. Between 6.0 to 6.9 = 10 to 20%
5. Between 7.0 to 7.9 cm = 20 to 40%
6. Greater than or equal to 8.0 cm in diameter = 30 to 50%
-
Level of consciousness in Aortic aneurysm
1. May be caused by sudden tear in aortic intima, opening way for blood to enter aortic wall.
2. Pain described as tearing, ripping, stabbing
3. Life threatening - usually blood is lost and the patient needs to go to OR immediately.
4. Emergency care goals: reduce BP, decrease velocity of left ventricular ejection, eliminate pain (raises bp/hr).
-
Aortic dissection
1. not a rupture
2. Weakening in the intima and blood can get through and runs the length of the vessel.
3. Separates the intima and tunica of the vessel.
4. Vessel can no longer expand and contract appropriately.
-
Cardiomyopathy
1. enlargement of heart
-
Four types of cardiomyopathy
1. Dilated cardiomyopathy
2. Hypertrophic cardiomyopathy
3. Restrictive cardiomyopathy
4. Arrhythmogenic right Ventricle cardiomyopathy
5. Very high mortality rate - 75% at 8 years post dx.
-
Dilated cardiomyopathy
1. Huge dilated chambers, impaired systolic function, stasis of blood
2. Most common type
3. Pt will be weak, HF, dysrhythmias, decreased CO
4. Tx similar to CHF
-
Dilated cardiomyopathy tx
1. Does not respond well to therapy.
2. Medications to treat HF: decrease preload(nitrates, loop diuretics), reduce afterload (ACEI), control neurohormonal stimulation (betablockers), reduce clot risk (anticoagulants)
3. Control of dysrhythmias
4. Cardiac rehabilitation
5. LVAD - left ventricular assist device
6. Transplant
-
Hypertrophic Cardiomyopathy
1. Left ventricular hypertrophy with small chamber size.
2. Sudden cardiac death in athletes thought to be this type.
3. Patho: stiff left ventricle so the heart can't fill. Genetic disorder
4. Treatment: beta blockers, calcium channel blockers, AV pacing, surgery remove excess muscle.
-
Restrictive cardiomyopathy
1. Impairment of diastolic filling and strech - walls are stiff but not thick.
2. Least common
3. Systolic function remains unaffected.
4. Symptoms and treatment are of the HF and dysrhythmias.
-
Arrhythmogenic Right Ventricular Cardiomyopathy
1. Replacement of myocardial tissue with fatty and fibrous tissue
2. Familial association
3. Affects young adults
4. Asymptomatic.
5. Tx like chf
-
Cardiomyopathy Pt Education
1. Treatment is like CHF
2. Report palpitations, dizziness, fainting
3. Report worsening HF s/sx
4. Avoid strenuous activity
5. Avoid alcohol
6. Avoid toxins
7. Medication teaching
8. Pacemaker and/or implantable cardiac defibrillators.
-
Cardiomyopathy surgical management
1. Ventricular septal myectomy
2. Percutaneous alcohol septal ablation
3. Left ventricular assistive device - aorta to LV, acts as LV pump.
4. Heart transplantation
-
Infective and Inflammatory Disorders of the Heart
1. vegetation growing on heart valves.
-
Infective endocarditis
1. Microbial infection of the endocardium - vegetation on valves
2. RFs:
3. Abnormal heart valves, implanted devices, congenital heart abnormalities.
4. Poor dental hygiene
5. IV drug use or prolonged use of IV catheters.
6. Surgeries/procedures involving the GI system or mouth.
7. Weakened immune system, elderly.
-
Endocarditis CM
1. Recurrent fevers
2. Murmurs
3. Anorexia and weight loss
4. Development of HF
5. Evidence of systemic embolization - fragments of emboli break loose and travel to head (TIA), lungs (PE), distal limbs.
-
Diagnosis of Endocarditis
1. Echo or TEE shows vegetation
2. Increased WBCs
3. Positive blood cultures
4. New murmur
5. Known source
-
Complications of Endocarditis
1. Valve damage
2. CHF
3. Arrthymia
4. Emboli: brain, kidney, lungs
-
Treating Endocarditis
1. IV antibiotics - 2 to 6 weeks minimum course.
2. Treat heart failure from damaged valve
3. Rest
4. Surgical valve replacement
5. Prevention: minimize or correct RFs, good oral hygiene, prophylactic antibiotics for high risk patients with procedures or conditions most likely to result in bacteria in the blood stream.
-
Pericarditis
1. Inflammation of the pericardial sac: causes pleuritic chest pain, sharp and stabbing, may be accompanied by a pleural effusion.
2. Acute: most commonly a viral cause, after a resp infection or dressler's syndrome after an MI.
3. Chronic: caused by fibrous thickening of pericardium from TB, radiation therapy, trauma, metastatic cancer.
-
Is it pericarditis?
1. Chest pain that is relieved by sitting forward. WORSENS = Supine.
2. pericardial friction rub (scratchy heart sound)
3. Fever with elevated WBC count
4. ECG changes - A fib common
5. Pericardial effusion seen on echocardiogram.
-
Pericarditis Treatment
1. Management of pain with NSAIDs.
2. Comfort: maintain HOB elevated
3. Antibiotics if ineffective
4. Pericardiectomy if secondary to malignant disease.
-
Rheumatic Heart Disease
1. Rheumatic fever complication
2. Affects all parts of heart
3. Autoimmune process: triggered by a reaction to the streptococcal bacteria in strep throat.
4. Mitral/aortic valve disease
5. Atrial fibrillation
6. Heart failure can develop
7. Prevention - early dx and tx of strep.
-
Common causes of Chest Pain
1. Cardiac: acute coronary syndrome (life threat), Non-life: stable angina, pericarditis, myocarditis.
2. Pulmonary: life: pulmonary embolus, pneumthorax Nonlife: pneumonia, pleurisy
3. Vascular, life: aortic syndromes
4. GI life: pancreatitis, non life: gastric ulcer, cholecystitis, gerd
5. MS: life: trauma, non life: skeletal muscle pain, chostochondritis, trauma
6. Other: herpes, idiopathic, anxiety
-
RF for CAD and Acute MI
1. Modifiable: Obesity, smoking, sedentary lifestyle, elevated cholesterol, HTN, DM2, excessive alcohol, stress, metabolic syndrome, diet
2. Non-modifiable: age, gender, family hx, ethnicity, dm1
-
Acute Coronary syndrome
-
ACS patho
-
Ischemia vs injury vs infarction in Heart
1. Infarction = death, cells not coming back.
2. Injury = cells in survival mode, energy goes to keeping them alive. ST segment elevation with/ or without loss of R wave.
3. Ischemia causes ST seg depess w/w/o T wave inversion as result of altered repolarization.
4. Goal is to save as much tissue as possible.

