What is varicose veins?

♡ Varicose veins are swollen and enlarged veins that usually occur on the legs and feet
♡ They may be blue or dark purple, and are often lumpy, bulging or twisted in appearance
♡ Other symptoms include: aching, heavy and uncomfortable legs. Swollen feet and ankles
What is Deep Vein Thrombosis - DVT?

♡ Deep vein thrombosis (DVT) is a medical condition that occurs when a blood clot forms in a deep vein
♡ These clots usually develop in the lower leg, thigh, or pelvis, but they can also occur in the arm
What is the role of coagulation in haemostasis and thrombosis?
♡ Coagulation plays a crucial role in preventing blood loss by forming clots to stop bleeding
♡ Interestingly, inflammation can activate coagulation, and in turn, coagulation can promote inflammation, making it an inflammatory response
What can an MRI of the brain reveal in cases of ischaemia?
♡ An MRI of the brain can show evidence of ischaemia, such as an infarct in a specific area like the left frontal lobe
♡ Ischaemia of the brain is often caused by an embolic stroke, which can originate from the carotid arteries or the heart
What can be inferred from the presence of an infarct in the left frontal lobe on brain MRI?
♡ The presence of an infarct in the left frontal lobe indicates ischaemia of the brain, likely caused by an embolic stroke
♡ This condition results in a region of neuronal cell death due to inadequate blood supply to the affected area
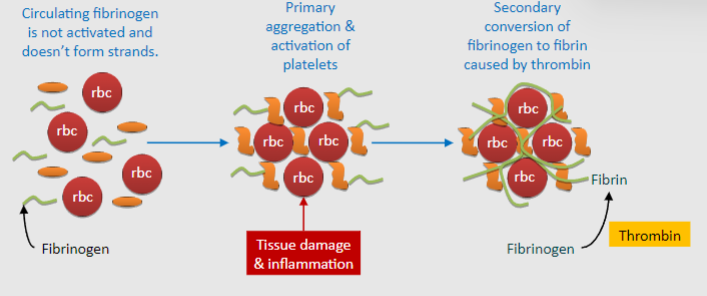
What initiates the clotting cascade in platelets and coagulation
♡ Circulating fibrinogen remains inactive and does not form strands initially
♡ The process begins with primary aggregation and activation of platelets
♡ Secondary conversion of fibrinogen to fibrin is triggered by thrombin
What is the purpose of the clotting cascade?
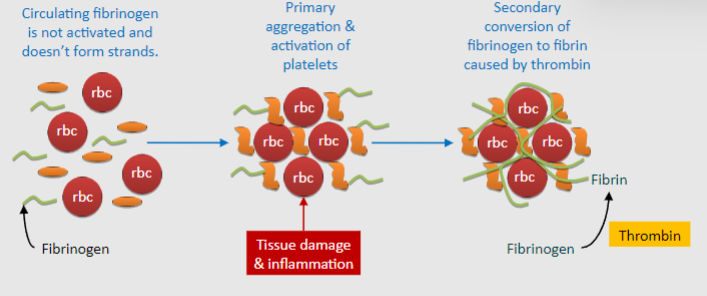
♡ The clotting cascade aims to generate a large amount of thrombin
♡ Thrombin is essential for converting fibrinogen into fibrin, which forms strands crucial for clot formation
How does fibrin contribute to clot formation?
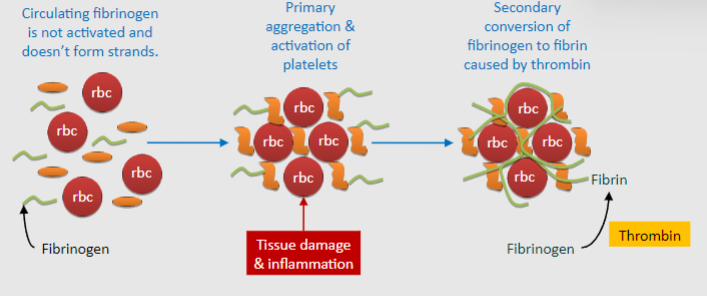
♡ Fibrin, produced through the clotting cascade, solidifies the agglutinated platelets to prevent blood loss
♡ It forms strands that reinforce the platelet plug, leading to the formation of a stable blood clot

What maintains the balance between coagulation and fibrinolysis?

♡ There is a constant balance between coagulation and fibrinolysis in the body.
♡ Anticoagulant and fibrinolytic agents constantly counteract coagulation triggered by tissue damage or inflammation
How do anticoagulants prevent thrombosis? (3)
♡ Anticoagulants prevent thrombosis by inhibiting coagulation
♡ Endothelial cells express various factors that inhibit coagulation, such as nitric oxide and prostaglandin I2
♡ Antithrombin inhibits clotting when bound to heparan
What initiates coagulation when endothelial cells are damaged or inflamed? (3)
♡ When endothelial cells are damaged or inflamed, they may favour coagulation
♡ Subendothelial cells release tissue factor or Von Willebrand factor, which initiates clotting
♡ Von Willebrand factor activates platelets, while tissue factor initiates clotting
How is thrombosis reversed in the body? (2)
♡ Fibrinolysis reverses thrombosis by breaking down the clot
♡ Plasmin, activated from plasminogen by Tissue Plasminogen Activator (tPA), breaks down the clot into smaller fragments.
What are the primary causes and characteristics of arterial thrombosis? (3)
♡ Arterial thrombosis primarily results from atheroma rupture or damage to the endothelium, as seen in conditions like myocardial infarction (MI) and stroke
♡ It typically forms platelet-rich 'white' thrombi and is mostly primary in nature
♡ Arterial thrombi may block downstream arteries, leading to tissue ischaemia or infarction
What are the primary causes and characteristics of venous thrombosis? (3)
♡ Venous thrombosis often results from stasis or a hyper-coagulant state, such as deep vein thrombosis (DVT)
♡ It forms platelet-poor 'red' thrombi and is mostly secondary in nature (arises as a complication)
♡ Venous thrombi are prone to dislodgement and migration, potentially leading to pulmonary embolism when they reach the lungs
What are the 3 parts of Virchow's triad? Elaborate on each:
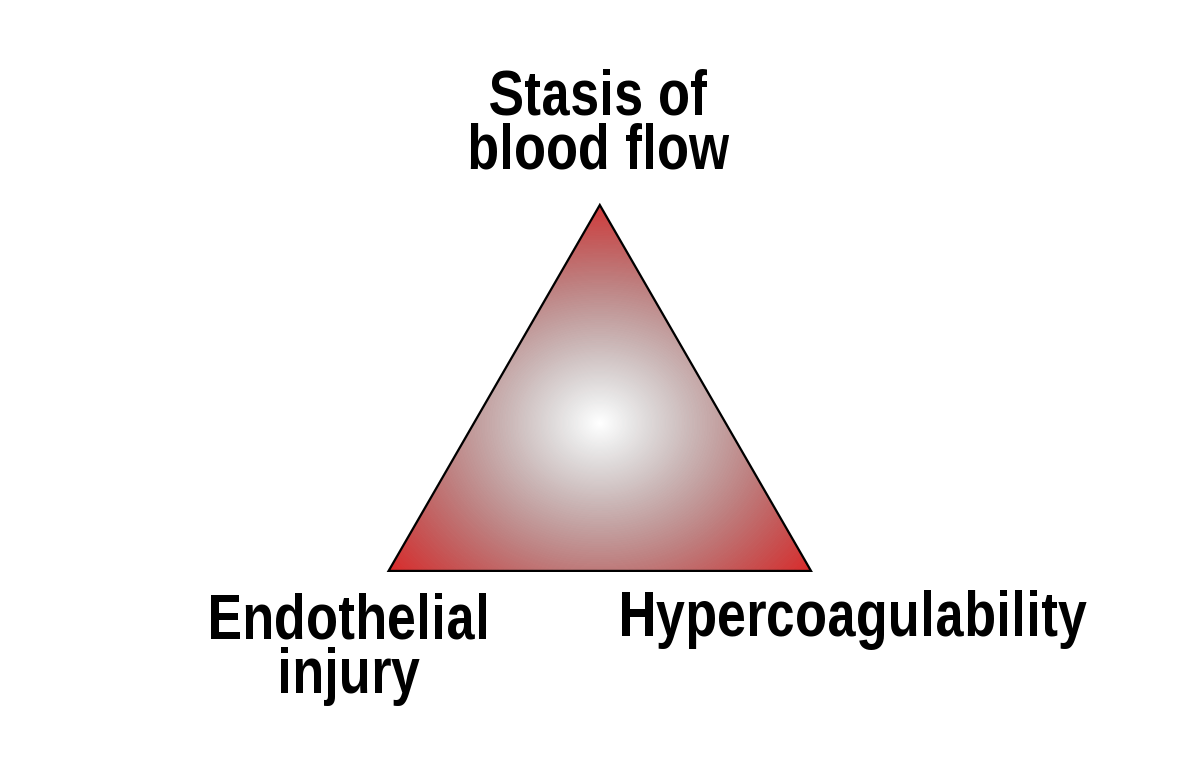
♡ Endothelial injury or dysfunction: Damage or impairment to the inner lining of blood vessels, which can be caused by factors such as inflammation, trauma, or turbulent blood flow
♡ Abnormal blood flow: Conditions that disrupt normal blood flow patterns, such as stasis (sluggish blood flow), turbulence, or changes in vascular anatomy
♡ Hypercoagulability: Increased tendency of the blood to clot, which can result from various factors including genetic predisposition, acquired conditions (e.g., cancer, pregnancy), or certain medications
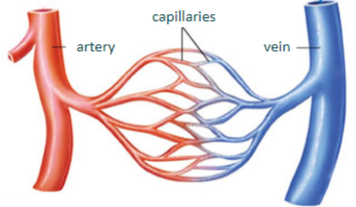
What happens when nearby muscles contract? (2)

♡ Squashes veins
♡ Acts as a pump to return blood to the heart
What can occur if valves are damaged? (3)

♡ Valves may not close successfully
♡ Blood flows in the wrong direction
♡ Blood pools in the legs
What is the function of valves in veins? (1)

♡ Prevent backflow of blood
What is the risk associated with the eddying of blood around valves? (1)

♡ Increases risk of stasis
What happens if venous return is blocked? (2)

♡ The affected organ becomes congested with fluid
♡ Increased pressure leads to more filtration
What is the risk associated with deep vein thrombosis? (1)
♡ The thrombosis might become dislodged and make its way back to the heart
What is the fate of a thrombus if it undergoes resolution? (1)
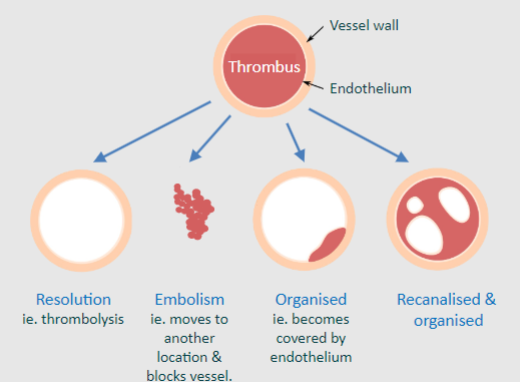
♡ Thrombolysis occurs
What happens if a thrombus causes an embolism? (1)
♡ It moves to another location and blocks a vessel
What occurs when a thrombus becomes organized? (1)
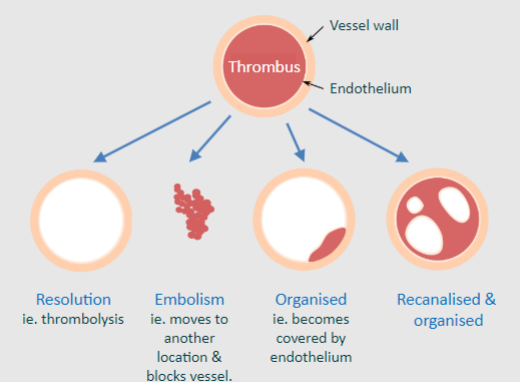
♡ It becomes covered by endothelium
How does a thrombus change during recanalization and organization? (1)
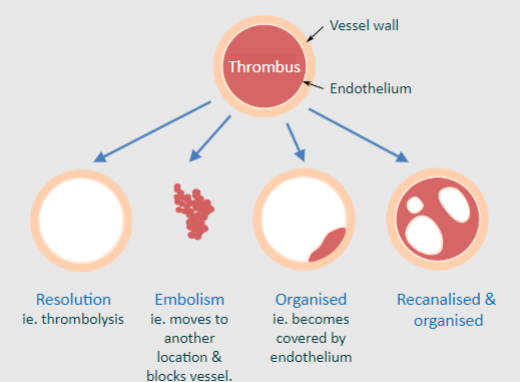
♡ It becomes recanalized and organized
What is recanalisation? (1)
♡ Recanalisation refers to the reopening or restoration of a previously blocked blood vessel, typically after the formation of a thrombus
What are the characteristics of proximal deep vein thrombosis (DVT)? (2)
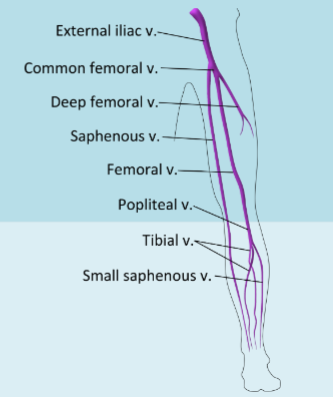
♡ Higher risk of pulmonary embolism
♡ Higher risk of post-thrombotic syndrome (pain, swelling, maybe even ulcers)
What are the characteristics of distal deep vein thrombosis (DVT)? (2)
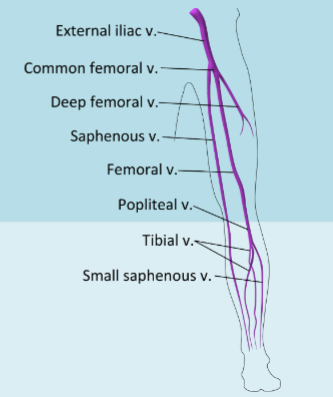
♡ Rarely causes pulmonary embolism
♡ Rarely causes post-thrombotic syndrome
What causes post-thrombotic syndrome? (2), And what are the symptoms? (YUCKY PICTURE)

♡ Inflammation along with damage to the venous valves from the thrombus itself
♡ Valvular incompetence combined with persistent venous obstruction inducing a rupture of small superficial veins, subcutaneous hemorrhage, and an increase of tissue permeability
♡ Symptoms include pain, swelling, discoloration, and even ulceration
Describe the path of a thrombus dislodged from veins leading to pulmonary embolism (3)
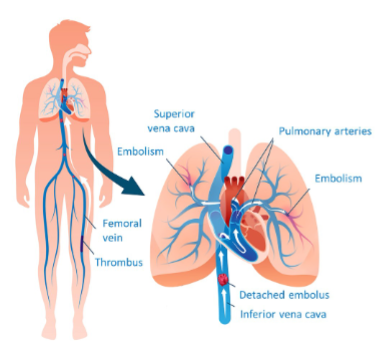
♡ The dislodged thrombus travels back to the right side of the heart
♡ From the right side of the heart, it passes into the pulmonary circulation
♡ Pulmonary embolism occurs when the thrombus blocks one of the pulmonary arteries
What occurs when there is tissue damage in the context of vascular injury?
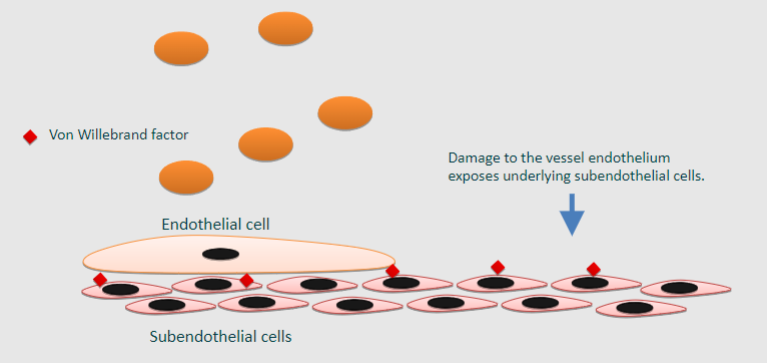
♡ Damage to the vessel endothelium exposes underlying subendothelial cells
How does damaged endothelium contribute to platelet adherence?
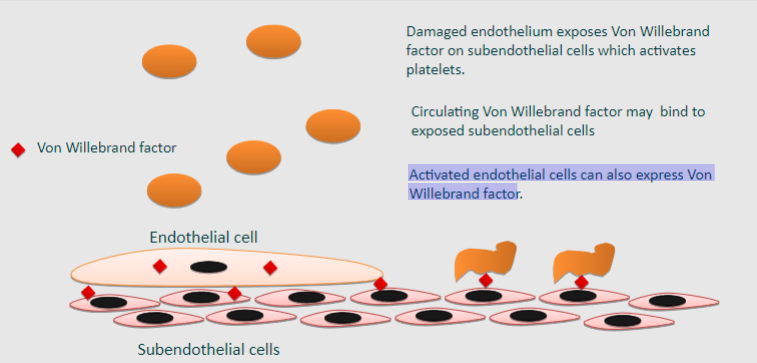
Damaged endothelium exposes Von Willebrand factor on subendothelial cells, which activates platelets
Circulating Von Willebrand factor may bind to exposed subendothelial cells
Activated endothelial cells can also express Von Willebrand factor

What are the factors involved in platelet activation? (5)
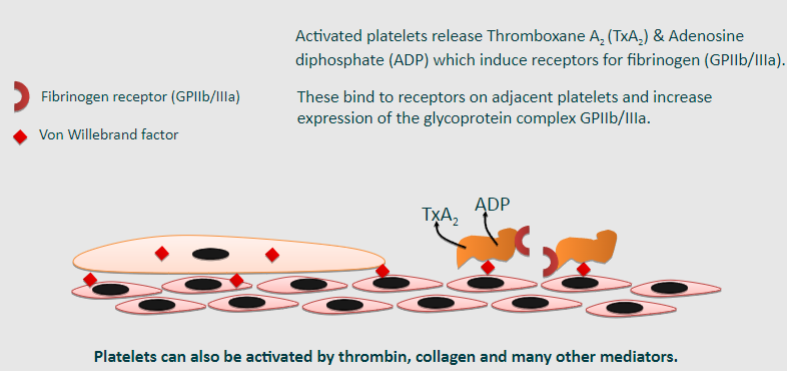
Von Willebrand factor
Fibrinogen receptor (GPIIb/IIIa)
Thromboxane A2 (TxA2)
Adenosine diphosphate (ADP)
Platelets can also be activated by thrombin, collagen, and many other mediators
How do activated platelets further contribute to platelet activation? (3)
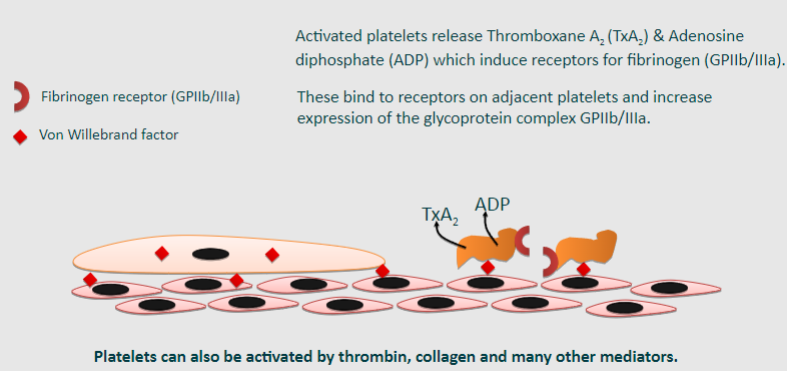
-Activated platelets release Thromboxane A2 (TxA2) and Adenosine diphosphate (ADP).
-TxA2 and ADP induce receptors for fibrinogen (GPIIb/IIIa) on adjacent platelets.
-These receptors bind to receptors on adjacent platelets and increase the expression of the glycoprotein complex GPIIb/IIIa.
What is platelet aggregation and how does it occur? (3)
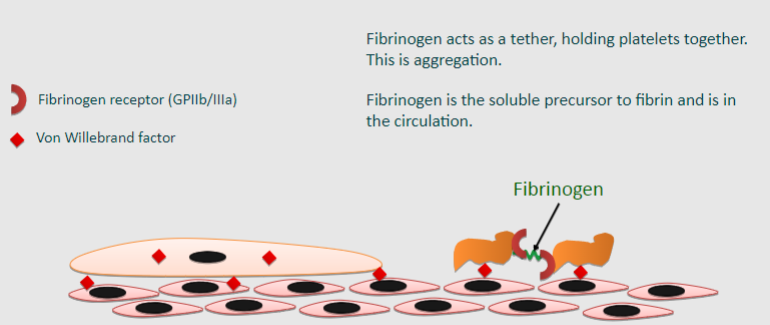
Platelet aggregation is the process by which platelets clump together to form a blood clot.
Fibrinogen acts as a tether, holding platelets together, which is aggregation.
Fibrinogen, the soluble precursor to fibrin, is present in the circulation and facilitates platelet aggregation.
What role do platelets play as a substrate for coagulation? (4)
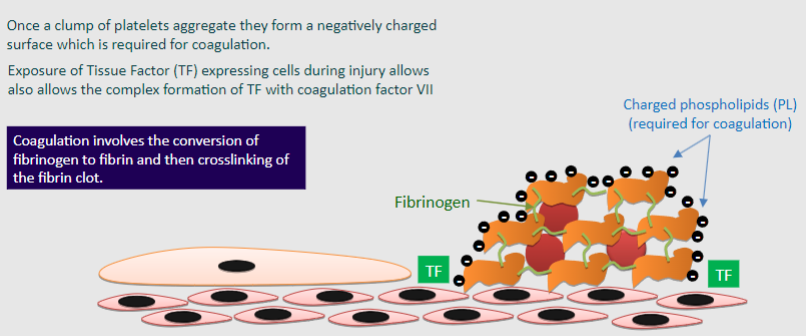
♡ Once a clump of platelets aggregate, they form a negatively charged surface, which is required for coagulation
♡ Coagulation involves the conversion of fibrinogen to fibrin and then crosslinking of the fibrin clot
♡ Exposure of Tissue Factor (TF) expressing cells during injury allows the complex formation of TF with coagulation factor VII
♡ Charged phospholipids (PL) are also required for coagulation
What is the purpose of the common pathway of blood clotting cascades? (1)
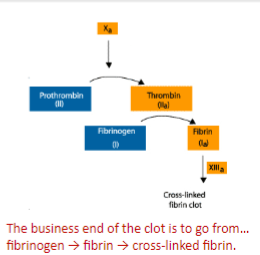
♡ The purpose is to produce activated factor ten (Xa), which is a protease that catalyzes the conversion of prothrombin (II) to thrombin (IIa)
What role does thrombin play in blood clotting? (1)
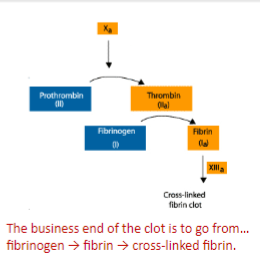
♡ Thrombin (IIa) is a protease that cleaves fibrinogen into fibrin, which is important for blood clot formation

How does fibrinogen promote blood clotting? (1)
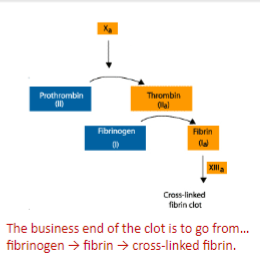
♡ Fibrinogen contributes to blood clotting by binding to the GpIIb/IIIa surface membrane receptor on activated platelets, facilitating platelet aggregation and the formation of bridges between them
What happens once fibrin is formed? (1)
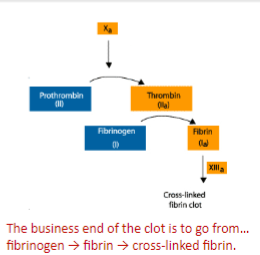
♡ Fibrin forms long polymers that hold activated platelets together in a blood clot
What further stabilizes the blood clot? (1)
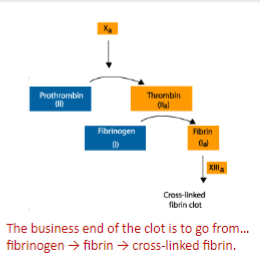
♡ Once there is enough thrombin present, factor thirteen (XIII) is activated and causes cross-linking of fibrin, which further stabilizes the clot
What initiates the extrinsic pathway of blood clotting? (1)
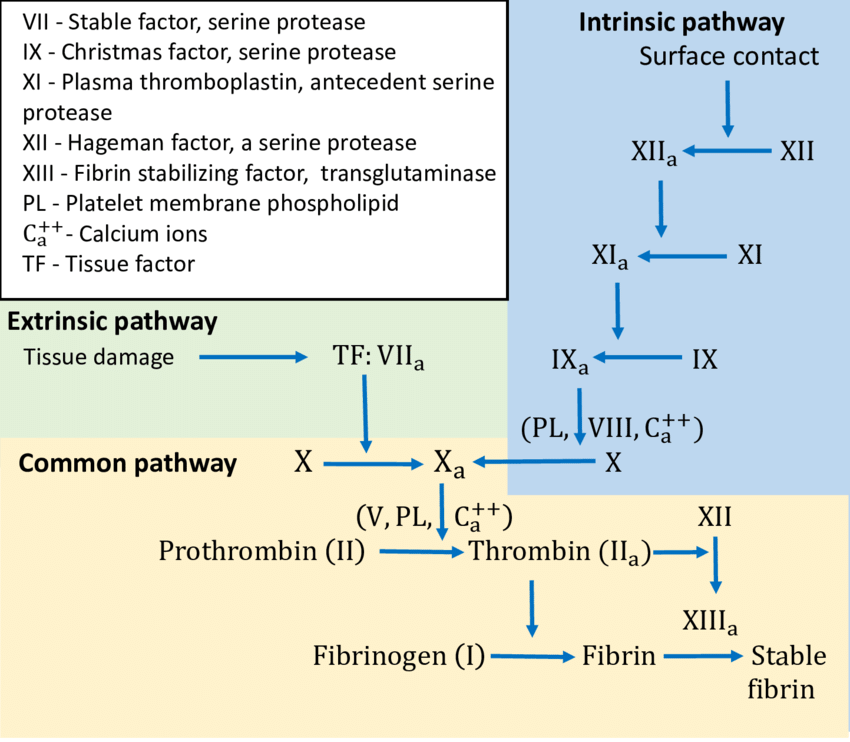
♡ The extrinsic pathway begins in the vessel wall when damaged endothelial cells release Tissue Factor (TF)
How does Tissue Factor (TF) initiate the extrinsic pathway? (1)
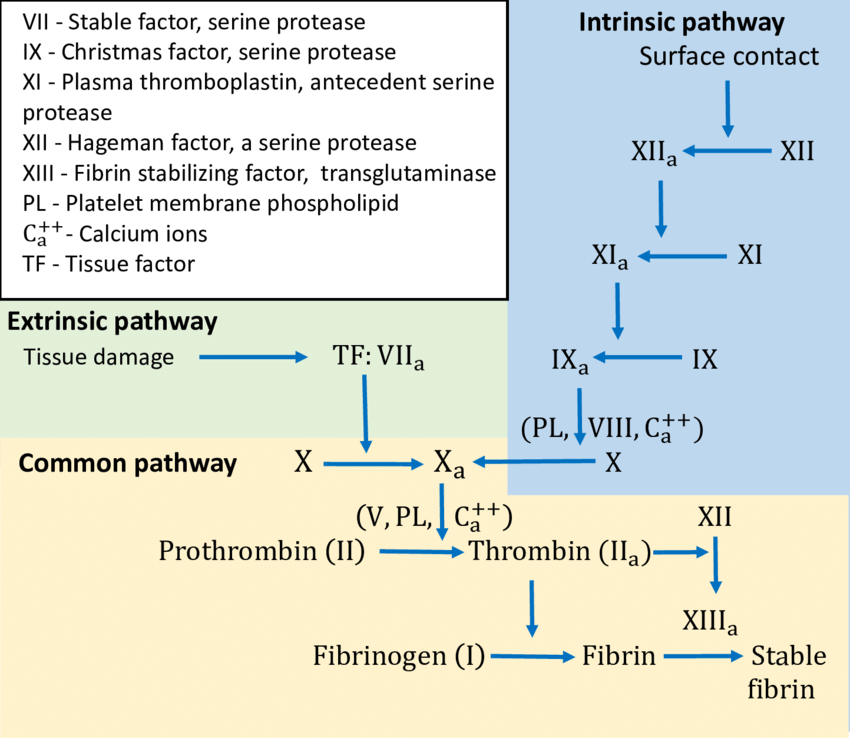
♡ Tissue Factor combines with calcium on the negatively charged platelet surface and activates factor VII
What inactivates the Vlla-tissue factor complex in vivo? (1)
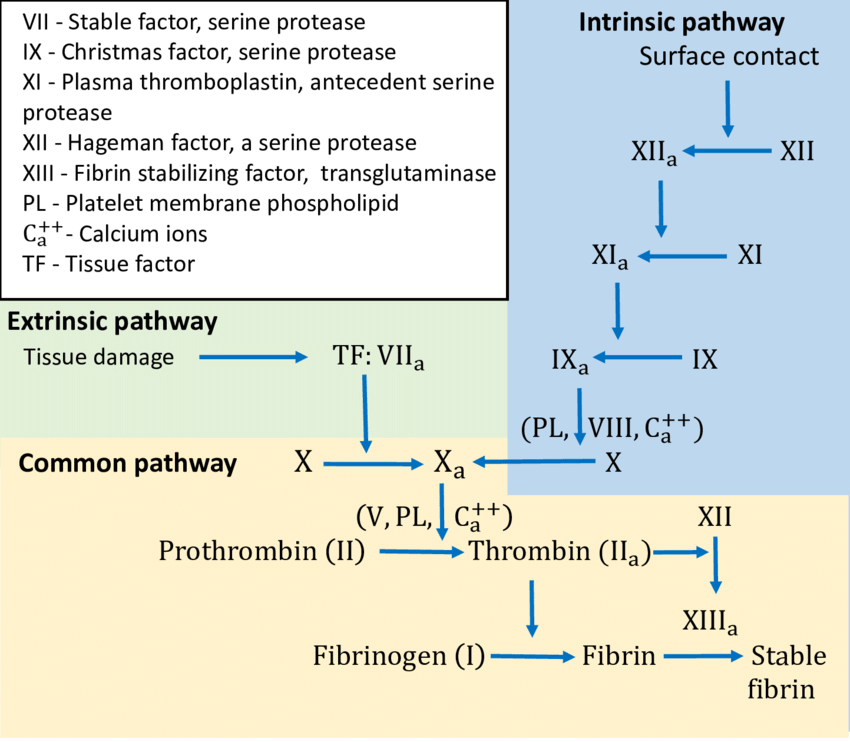
♡ The Vlla-tissue factor complex can be quickly inactivated by antithrombin (AT) in vivo
How does the intrinsic pathway of blood clotting start? (1)
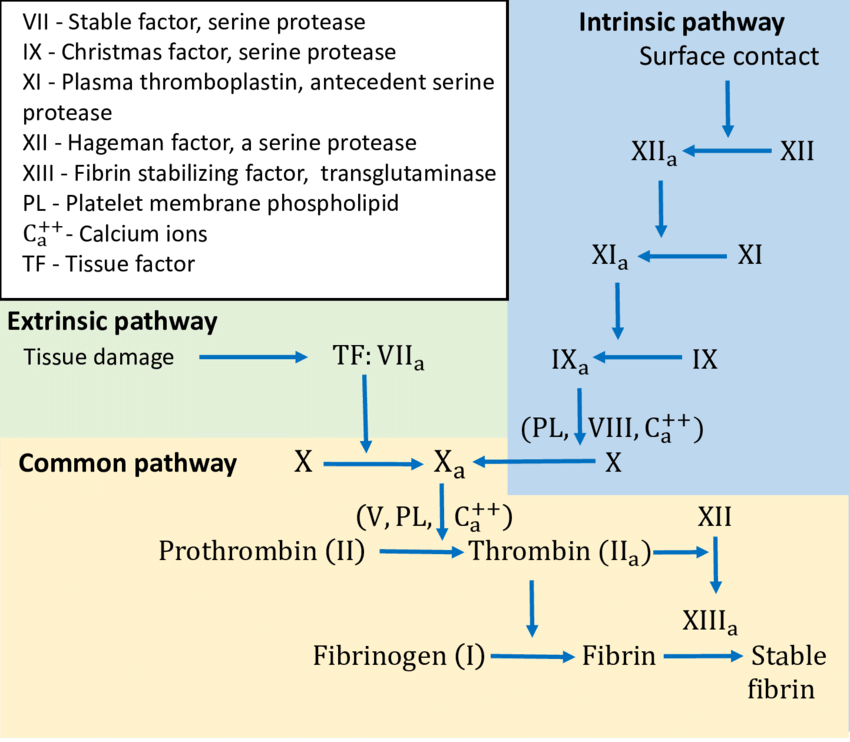
♡ The intrinsic pathway begins in the bloodstream and is activated when blood is exposed to collagen or other damaged surfaces
What activates the intrinsic pathway when blood is put onto a charged surface such as glass? (1)
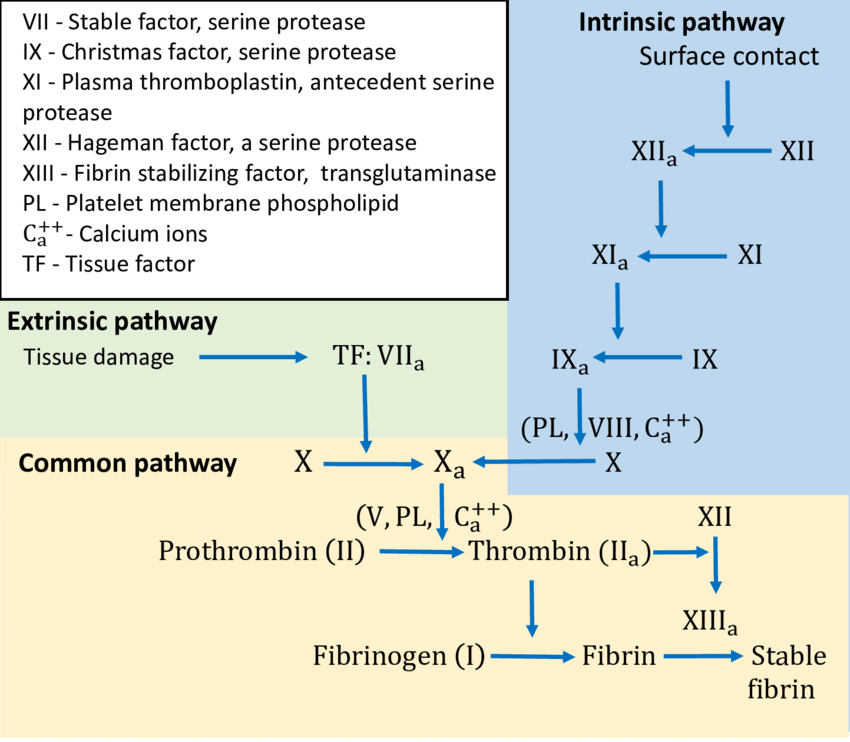
♡ The Activation of factor XII (also known as Hageman factor), which is part of the intrinsic pathway. Factor XII activation initiates a cascade of reactions leading to the formation of a blood clot
What is the difference in physiological effects between defects in the factors of the extrinsic pathway and mutations in the enzymes of the intrinsic pathway? (1)
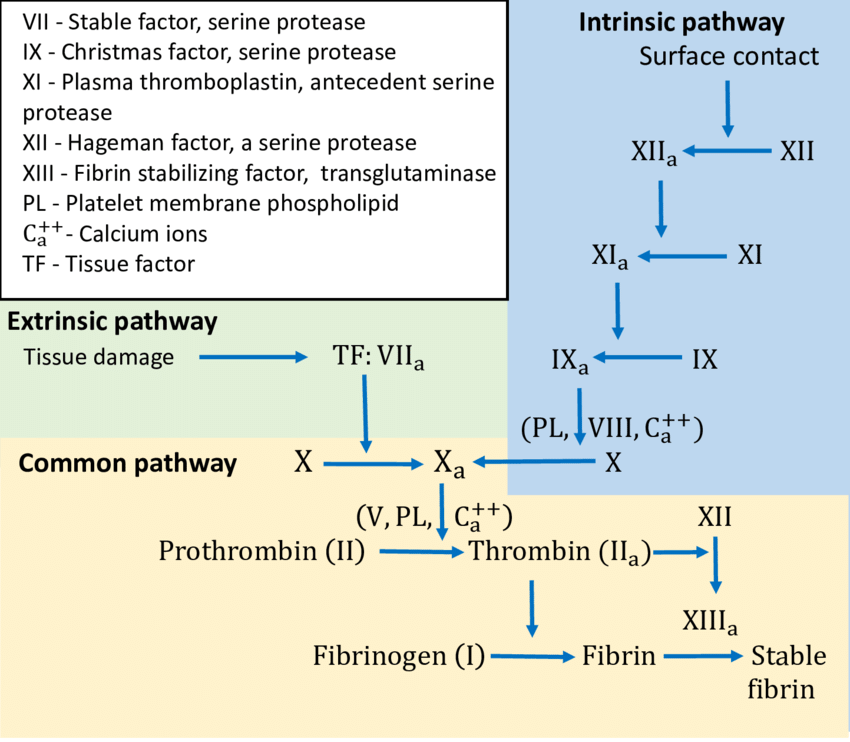
♡ Defects in the factors of the extrinsic pathway have far larger physiological effects than mutations in the enzymes of the intrinsic pathway
What is tissue plasminogen activator (tpA) and what is its function? (2)
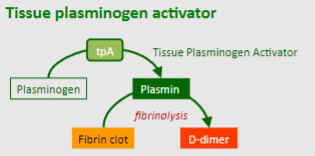
Tissue plasminogen activator (tpA) is a serine protease found on endothelial cells.
It catalyzes the activation of circulating plasminogen into plasmin
What is the function of plasmin in fibrinolysis? (1)
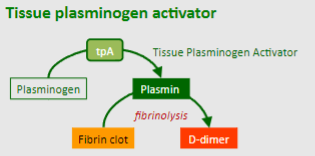
♡ Plasmin catalyzes the breakdown of cross-linked fibrin clot into fragments called D-dimers.
What is the role of antithrombin (AT) in anticoagulation? (3)
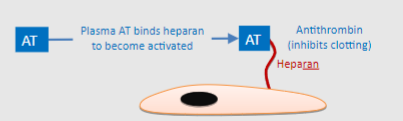
Antithrombin (AT) is a small protein molecule made by the liver that circulates in the plasma.
Heparan expressed by endothelial cells binds to AT, causing a conformational change that activates AT.
The activated AT then inactivates thrombin, factor Xa, factor VII, and other components of the clotting cascade.
How are some thrombolytic agents, such as tissue plasminogen activator, used in clinical practice? (1)
♡ Thrombolytic agents like tissue plasminogen activator and related compounds are used to treat strokes and myocardial infarctions by promoting the breakdown of blood clots