Where is the pituitary gland located?
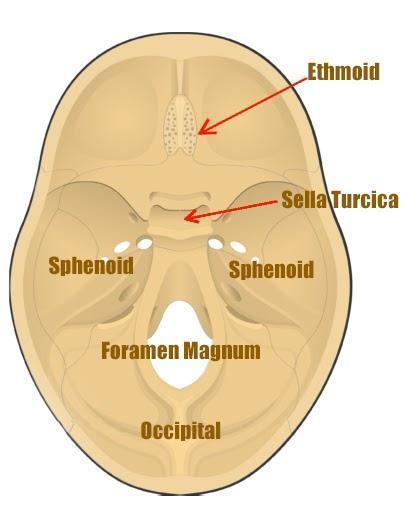
The pituitary gland lies below the brain in the Sella Turcica.
What are the two lobes of the pituitary gland?
The pituitary gland consists of the anterior lobe (adenohypophysis) and the posterior lobe (neurohypophysis).
From where is the anterior lobe (adenohypophysis) of the pituitary gland derived?
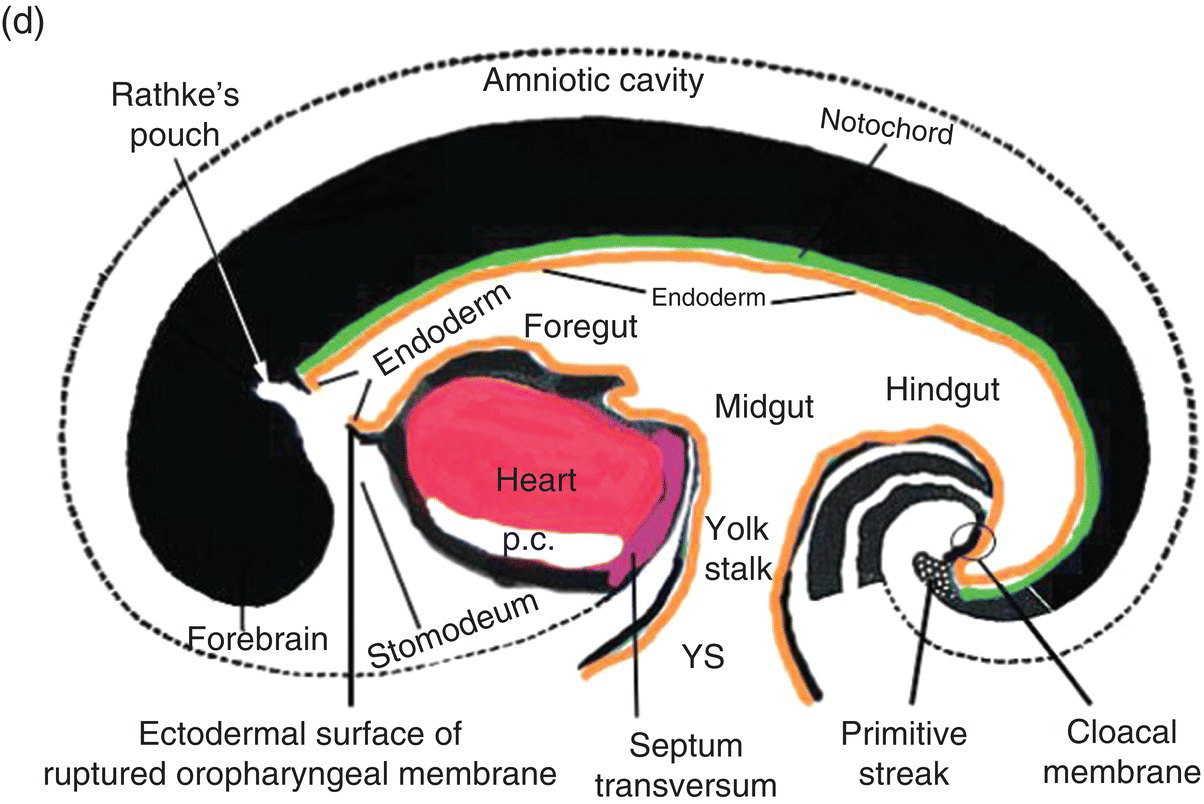
The anterior lobe (adenohypophysis) is derived from an invagination of the roof of the embryonic oropharynx known as Rathke’s pouch.
What forms the pituitary stalk and what is its function?
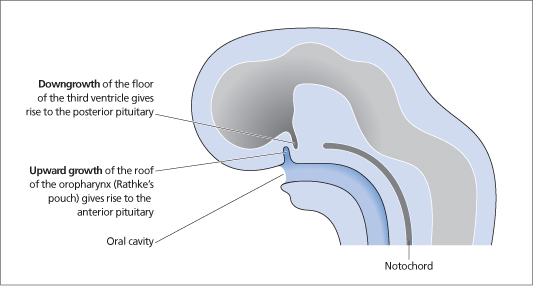
A notochordal projection forms the pituitary stalk, which connects the pituitary gland to the brain and also forms the posterior lobe of the pituitary (neurohypophysis).
What are the two lobes of the pituitary gland?
The anterior lobe (adenohypophysis) and the posterior lobe (neurohypophysis).
Where is the pituitary gland located?
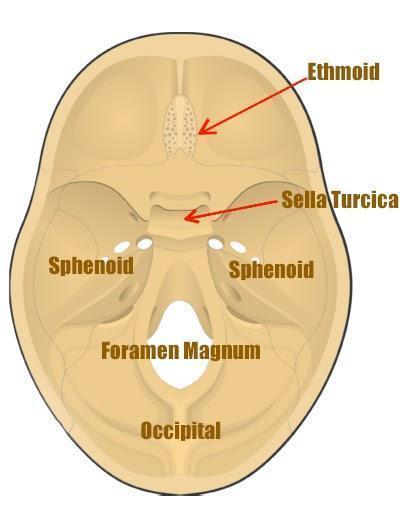
The pituitary gland lies below the brain in the Sella Turcica.
What embryonic structures give rise to the anterior and posterior lobes of the pituitary gland?
The anterior lobe is derived from Rathke’s pouch, an invagination of the roof of the embryonic oropharynx, and the posterior lobe forms from a notochordal projection that forms the pituitary stalk.
What are the two blood supplies to the pituitary gland?
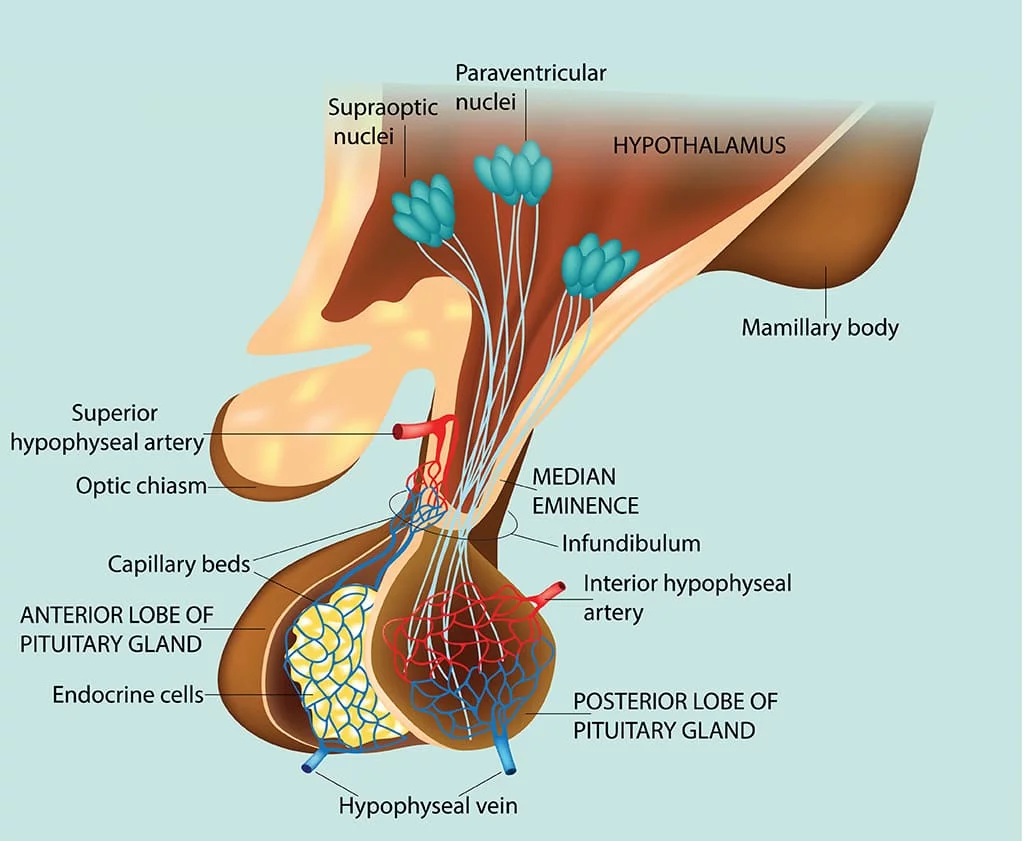
-Long and short pituitary arteries
-Hypophyseal portal circulation, which begins as a capillary plexus around the Arc.
How were pituitary cell types originally classified?

By their staining characteristics with acidic (orange-G) and basic (aldehyde fuscin) dyes.
What hormones are produced by the anterior pituitary gland? (5)
ACTH (Adrenocorticotropic Hormone)
TSH (Thyroid Stimulating Hormone)
GH (Growth Hormone)
LH/FSH (Luteinizing Hormone/Follicle Stimulating Hormone)
PRL (Prolactin)
What is the function of ACTH?
Regulation of adrenal cortex.
What does TSH regulate?
Thyroid hormone regulation.
What is the role of GH?
It promotes growth.
What are LH and FSH responsible for?
Reproductive control.
What is the function of PRL?

It stimulates breast milk production.
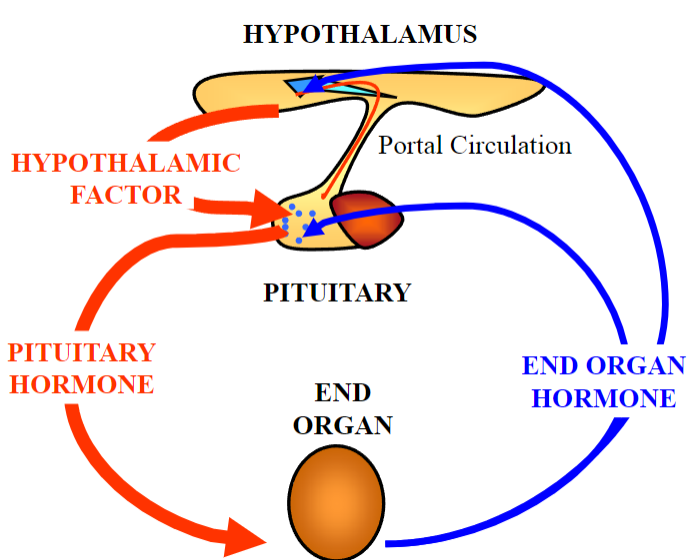
Picture demonstrating portal circulation:
What are the common symptoms of pituitary tumours due to hormone hypersecretion? (6)
Symptoms of hormone hypersecretion include:
Excessive sweating
Rapid heart rate
Weight gain or loss
High blood pressure
Changes in menstrual cycles
Enlargement of body parts like hands or feet
What are the symptoms of pituitary tumors as space-occupying lesions? (3)
Symptoms include:
-Headaches
-Visual disturbances or loss (field defect)
-Invasion of the cavernous sinus, leading to symptoms like eye movement abnormalities or facial numbness
How can hormone deficiency states manifest in pituitary tumor patients?
Hormone deficiency states can result in symptoms such as:
Fatigue
Weakness
Low blood pressure
Loss of libido
Infertility
Mood changes
What is the term used to describe the interference with surrounding normal pituitary tissue caused by pituitary tumors?
It's often referred to as "mass effect" or "compression effect."
What hormone excess syndrome is associated with tumors of the anterior pituitary gland releasing excessive growth hormone (GH)?
Acromegaly is the syndrome characterized by excessive growth hormone (GH) secretion due to tumors of the anterior pituitary.
Which hormone excess syndrome is linked with tumors of the anterior pituitary gland leading to overproduction of adrenocorticotropic hormone (ACTH)?
Cushing's disease results from the overproduction of adrenocorticotropic hormone (ACTH) by tumors of the anterior pituitary gland.
What syndrome of hormone excess arises from tumors of the anterior pituitary gland causing overstimulation of the thyroid gland through excessive thyroid-stimulating hormone (TSH) release?
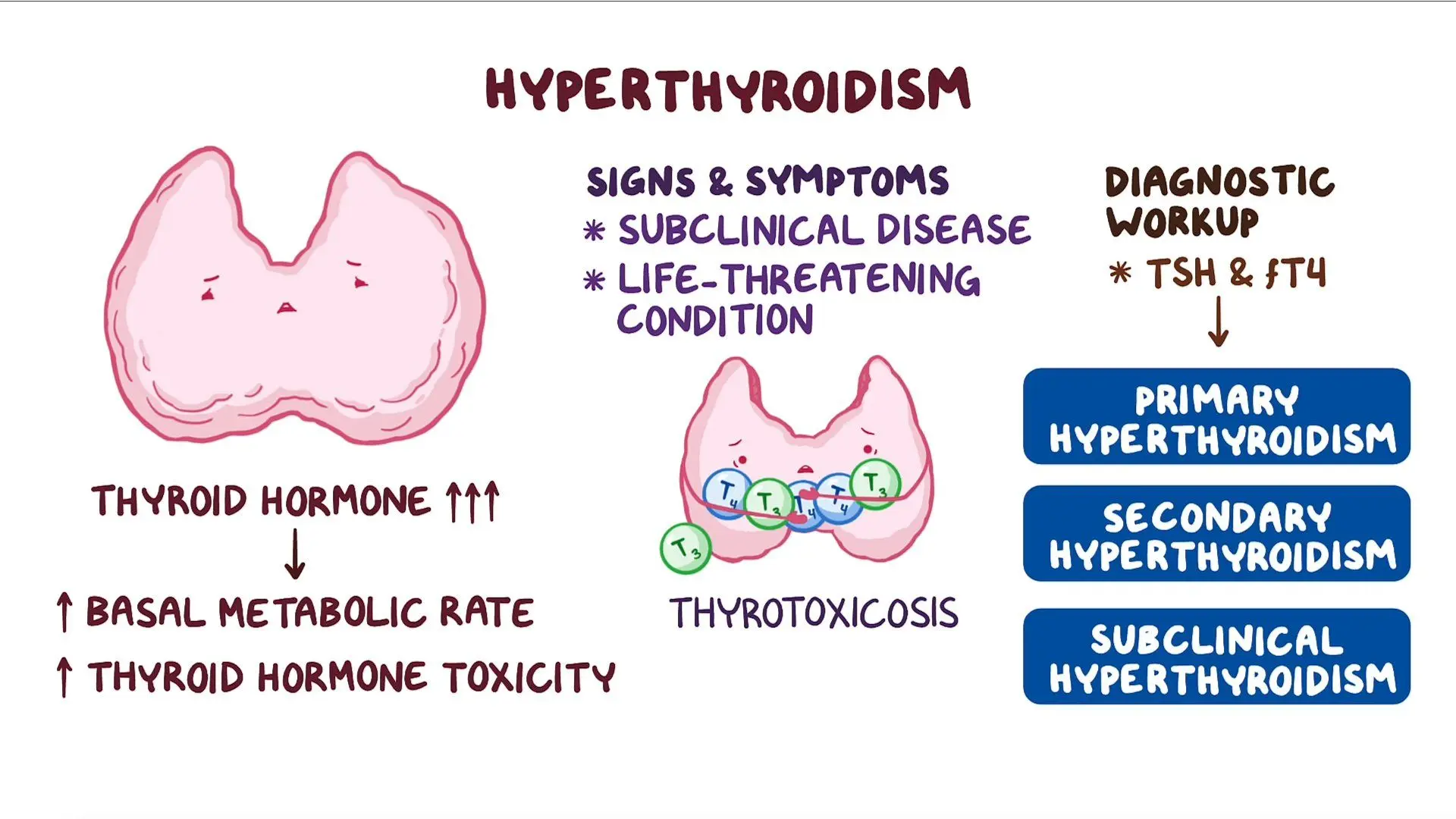
Secondary thyrotoxicosis occurs when tumours of the anterior pituitary gland lead to the overproduction of thyroid-stimulating hormone (TSH), stimulating the thyroid gland excessively.
Which hormone excess syndrome is associated with tumors of the anterior pituitary gland affecting luteinizing hormone (LH) and follicle-stimulating hormone (FSH) secretion?
Non-functioning pituitary tumors may affect luteinizing hormone (LH) and follicle-stimulating hormone (FSH) secretion, leading to various symptoms.
What hormone excess syndrome results from tumors of the anterior pituitary gland causing overproduction of prolactin?
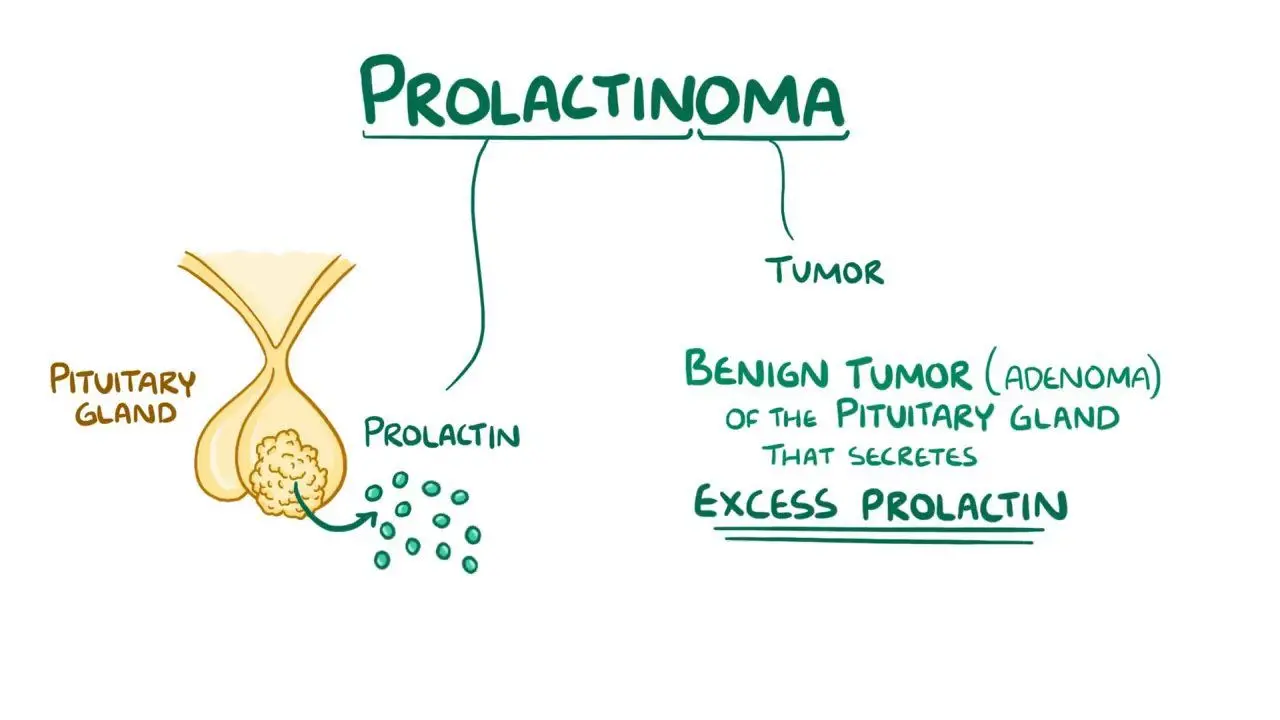
Prolactinoma is the syndrome characterized by the overproduction of prolactin due to tumors of the anterior pituitary gland.
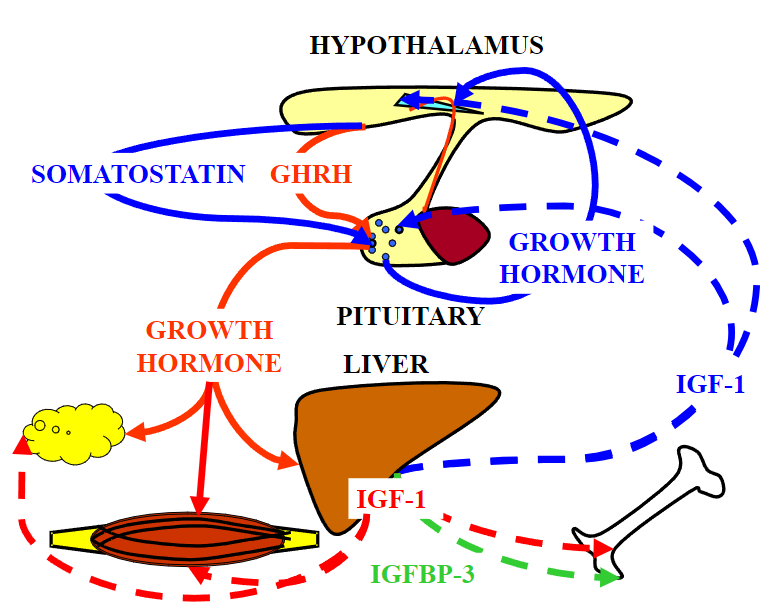
Picture demonstrating IGF secretion:
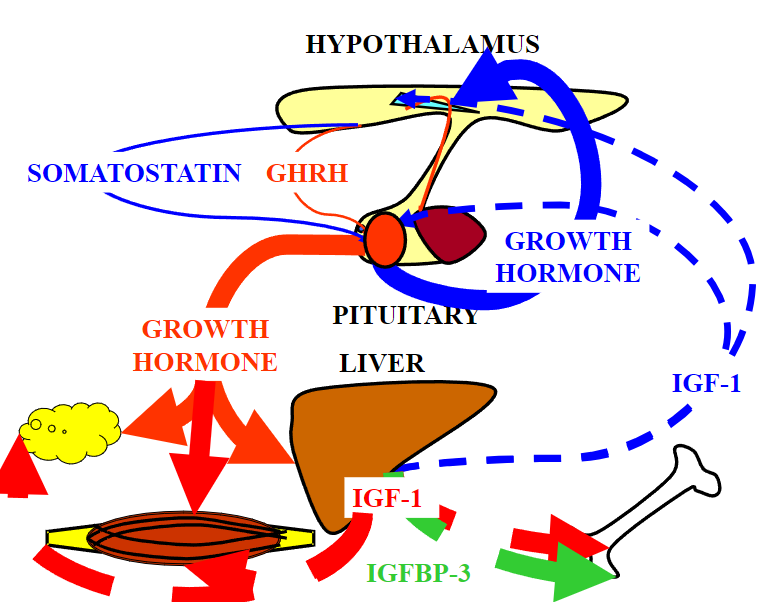
Picture demonstrating the positive feedback mechanism of GH on IGF secretion:
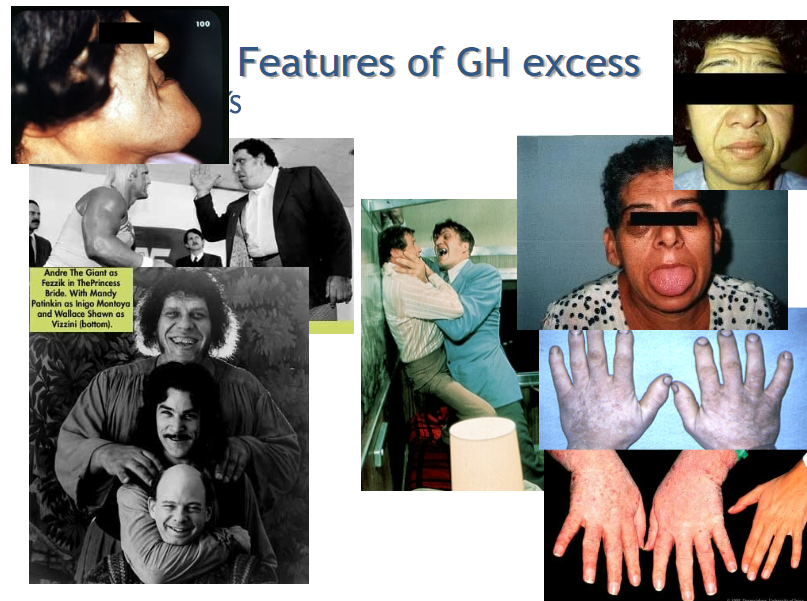
What are some manifestations of acral enlargement associated with excess growth hormone (GH)/insulin-like growth factor-I (IGF-I)?
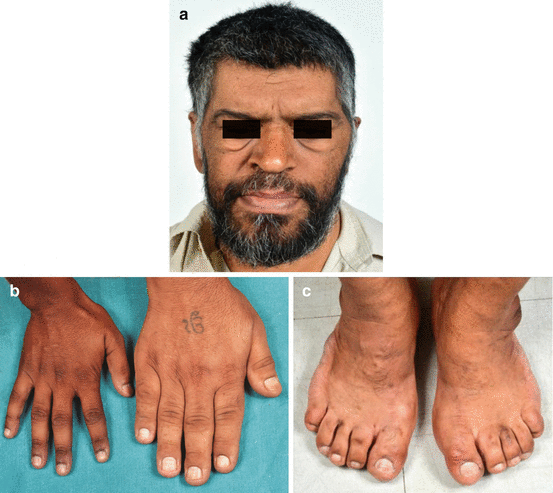
Acral enlargement can lead to spade-like hands, rings becoming too small, increased shoe size, macroglossia (enlarged tongue), and carpal tunnel syndrome in individuals with GH/IGF-I excess.
What changes occur in the skin due to excess GH/IGF-I?

Excess GH/IGF-I can cause increased skin thickness, sweating, and the development of skin tags and acanthosis nigricans (dark patches of skin).
How does excess GH/IGF-I affect appearance?
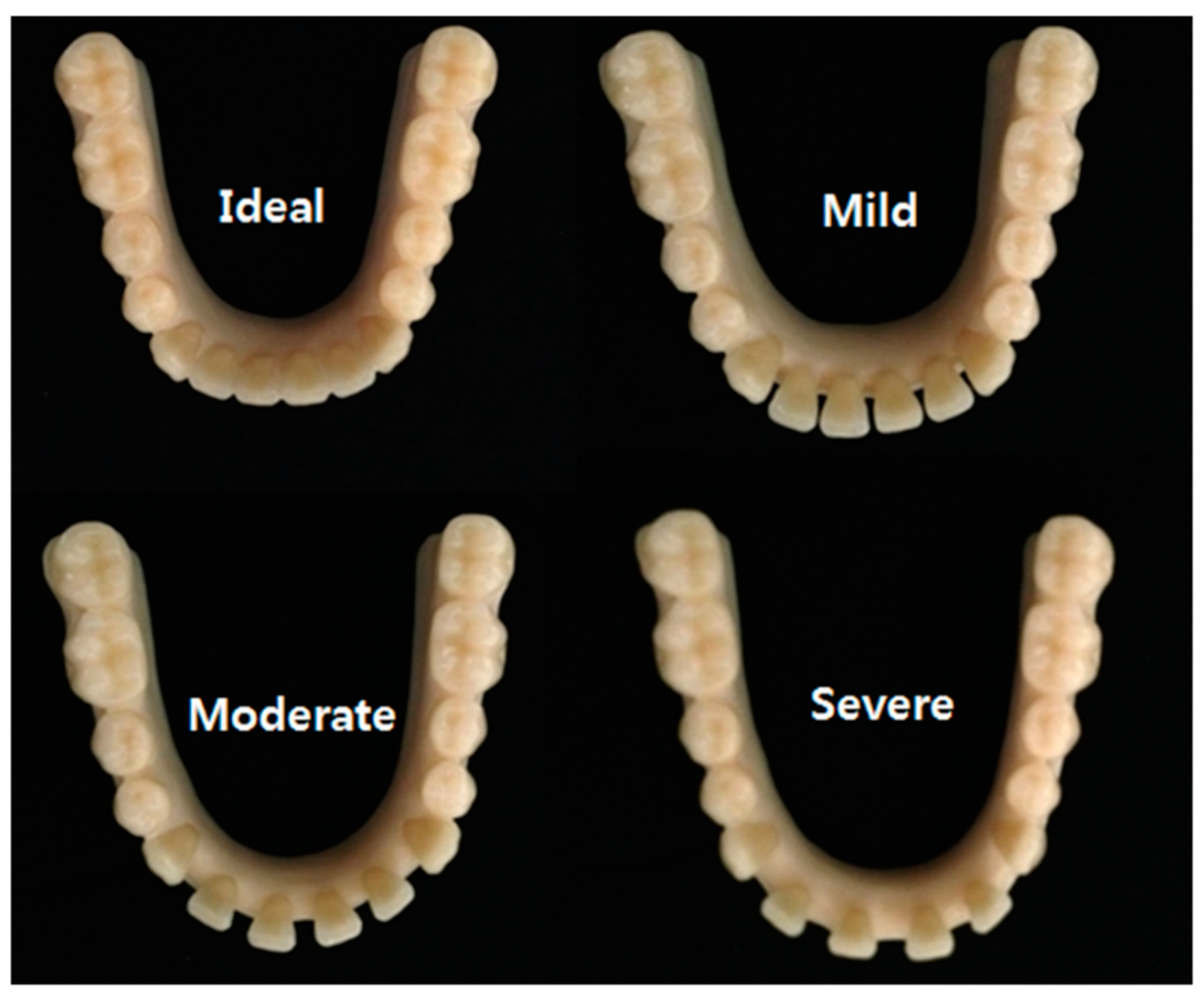
Excessive GH/IGF-I can lead to changes in appearance such as increased inter-dental spacing.
What visceral changes can occur as a result of GH/IGF-I excess?
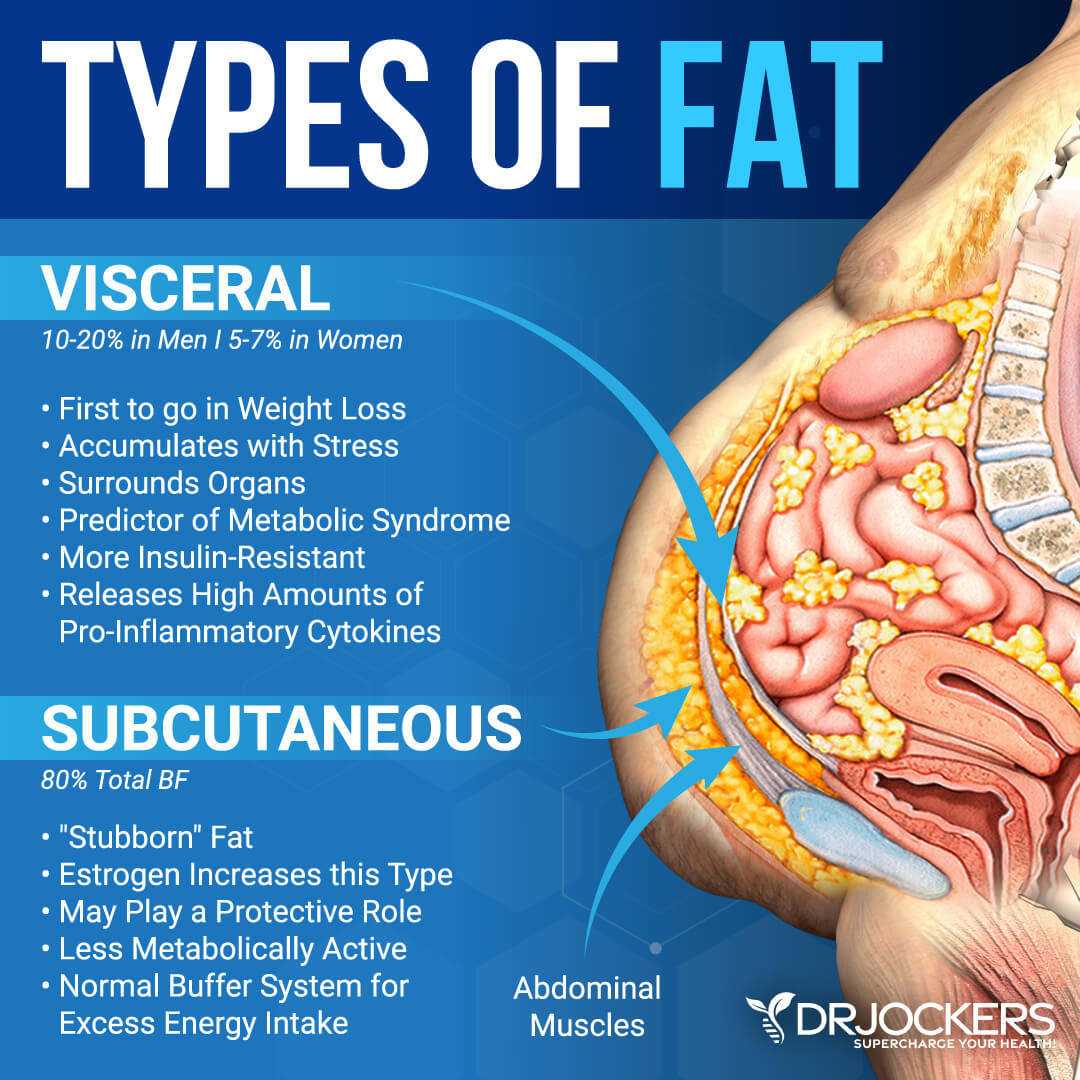
Visceral enlargement may occur in individuals with excess GH/IGF-I.
What metabolic changes are associated with excess GH/IGF-I? (7)
Metabolic changes include impaired fasting glucose, impaired glucose tolerance, diabetes mellitus, insulin resistance, reduced total cholesterol, increased triglycerides, and increased nitrogen retention.
What cardiac complication can result from excess GH/IGF-I?
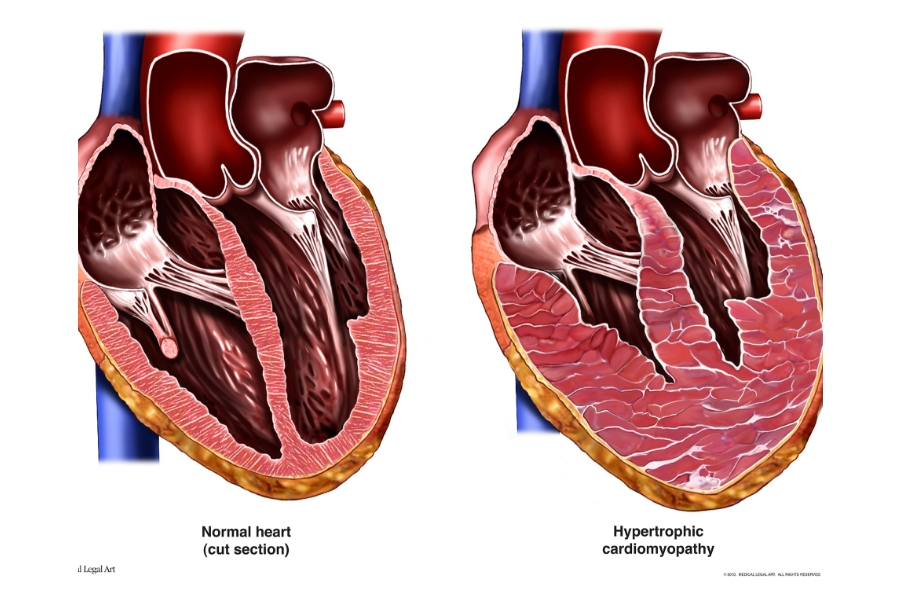
Excess GH/IGF-I can lead to cardiomyopathy, which is a disease of the heart muscle.
What cardiovascular condition may arise due to GH/IGF-I excess?
Hypertension (high blood pressure) can be a consequence of excess GH/IGF-I.
What gastrointestinal manifestations are associated with GH/IGF-I excess?
Bowel polyps and an increased risk of colonic cancer are gastrointestinal consequences of GH/IGF-I excess.
What endocrine disorder can result from excess GH/IGF-I?
Excess GH/IGF-I can lead to multinodular goiter, which is the presence of multiple nodules in the thyroid gland.
What reproductive complication may occur due to GH/IGF-I excess?
Hypogonadism, characterized by reduced function of the gonads, can result from excess GH/IGF-I.
What musculoskeletal issue is associated with GH/IGF-I excess?
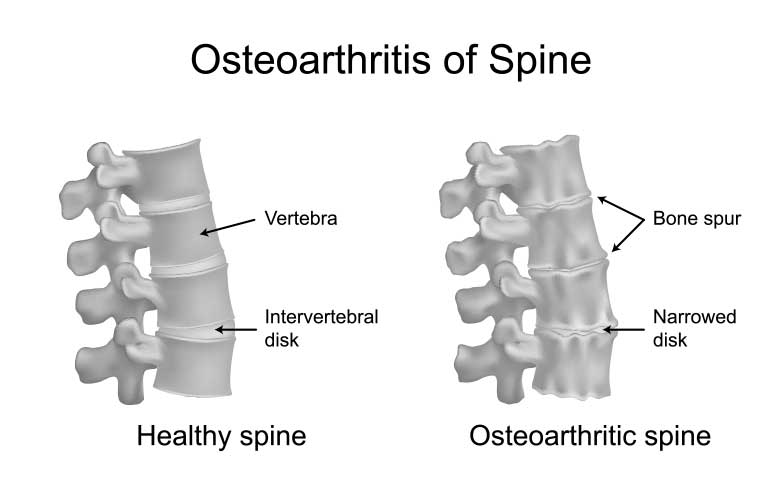
Arthropathy/Osteroathiritis, which is joint disease, can occur as a consequence of excess GH/IGF-I.

What sleep-related condition may arise from GH/IGF-I excess?
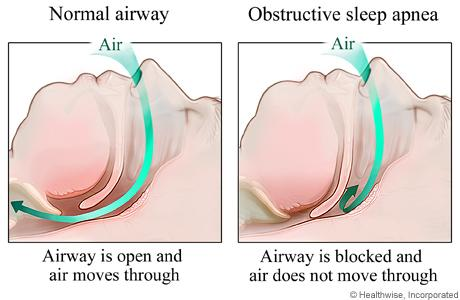
Obstructive sleep apnea (OSA) can be a consequence of excess GH/IGF-I.
Picture demonstrating features of GH excess:
What are the physical symptoms associated with Cushing's syndrome?
Cushing's syndrome is characterized by changes in protein and fat metabolism, leading to central obesity, a moon face, a buffalo hump, thin skin, easy bruising, osteoporosis (brittle bones), and diabetes.
How do changes in sex hormones manifest in Cushing's syndrome?
Changes in sex hormones in Cushing's syndrome can lead to excess hair growth, irregular periods, problems conceiving, and impotence.
What are the consequences of salt and water retention in Cushing's syndrome?
Salt and water retention in Cushing's syndrome can result in high blood pressure and fluid retention.
Picture demonstrating the characteristics of Cushing syndrome:

What characterizes prolactinomas?
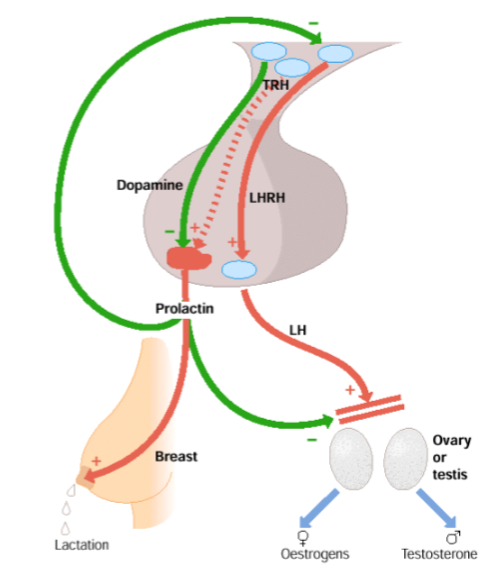
Prolactinomas are common pituitary tumors characterized by their unique regulation compared to other anterior pituitary hormones. They exhibit tonic release of dopamine (DA), which inhibits prolactin (PRL) release, and can lead to positive feedback.
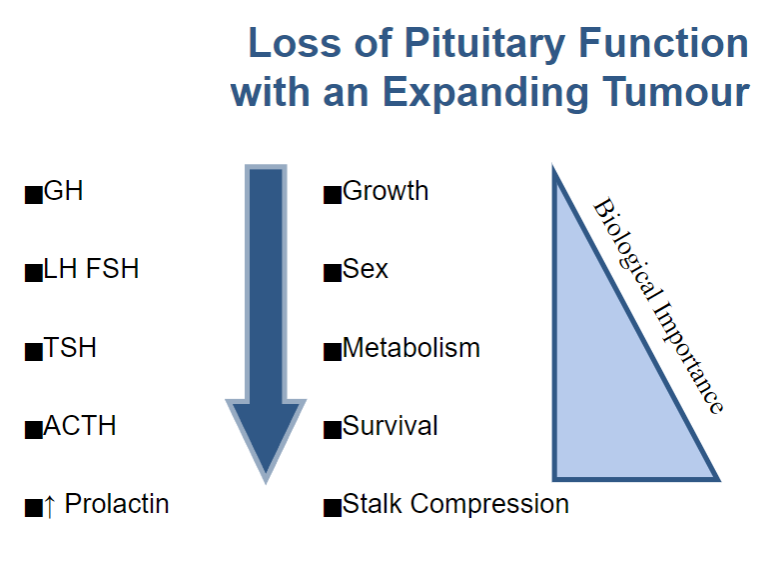
What percentage of all pituitary tumors are non-functioning?
Non-functioning pituitary tumors account for approximately 30% of all pituitary tumors.
What distinguishes non-functioning pituitary tumors from other types of pituitary tumors?
Unlike other pituitary tumors, non-functioning pituitary tumors do not produce a syndrome of hormone excess.
What are the primary symptoms associated with non-functioning pituitary tumors?
Symptoms are primarily due to space occupation and may include headaches, visual field defects, nerve palsies, and interference with the normal function of the pituitary gland, leading to hormone deficiencies.
What are the treatment options for non-functioning pituitary tumors?
Treatment typically involves surgery, often through a transsphenoidal approach, with or without radiotherapy. Currently, there is no highly effective medical therapy for these tumors.
What drugs can interfere with dopamine (DA) and prolactin (PRL) secretion, exacerbating prolactinomas?
Various drugs such as antiemetics, antipsychotics, and oral contraceptives (OCPs) or hormone replacement therapy (HRT) can interfere with DA and PRL secretion.
What are the features of prolactin (PRL) excess (hypogonadism)?
PRL excess can lead to hypogonadism, characterized by symptoms such as infertility, oligoamenorrhea, amenorrhea, galactorrhea, reduced libido, and erectile dysfunction.
What is the primary treatment for prolactinomas?
The primary treatment for prolactinomas is dopamine agonists such as bromocriptine or cabergoline, with surgery typically not being the first-line option.
Picture demonstrating the loss of pituitary function with an expanding tumour:
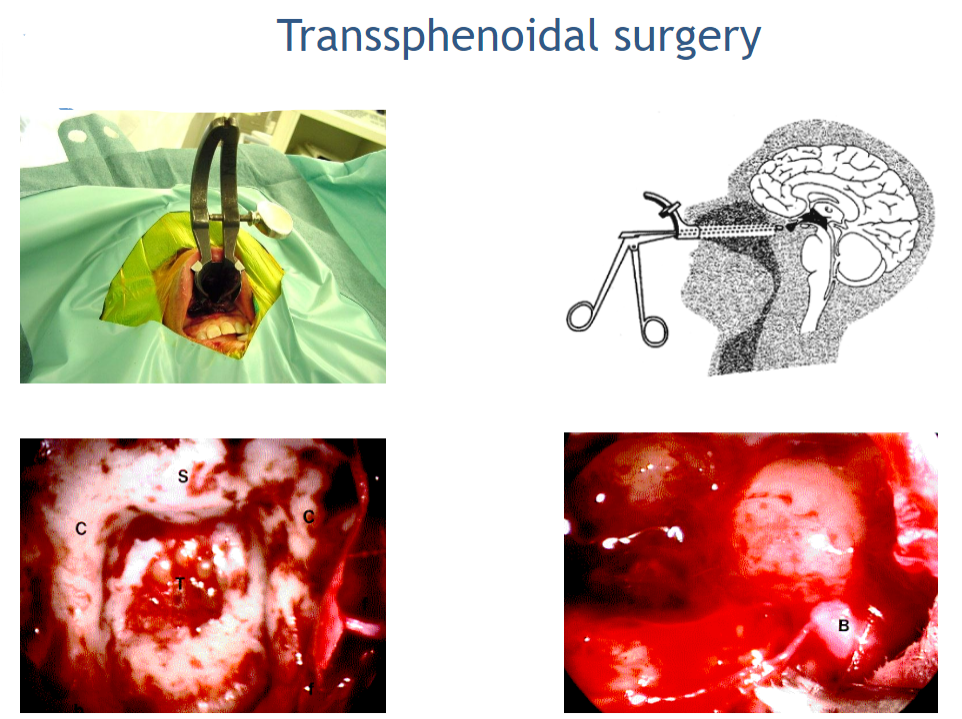
What is Transsphenoidal surgery?
Transsphenoidal surgery is a common pituitary tumor removal process that goes through nasal passages instead of the skull.
Picture demonstrating Transsphenoidal surgery:
What are the primary treatment modalities for pituitary adenomas?
The main treatment options for pituitary adenomas include surgery, radiotherapy, and drugs.
What surgical approach is commonly used for the treatment of pituitary adenomas?
Transsphenoidal surgery is a common surgical approach for removing pituitary adenomas.
In cases of Nelson's syndrome, what additional surgical procedure may be considered?
Adrenalectomy may be considered as part of the treatment for Nelson's syndrome, a condition characterized by the enlargement of the pituitary gland following bilateral adrenalectomy.
What is the role of radiotherapy in the treatment of pituitary adenomas?
Radiotherapy is used to treat pituitary adenomas, although it is a slow process.
How do drugs contribute to the treatment of pituitary adenomas?
Drugs can be used to either block hormone production or stop hormone release from pituitary adenomas, providing an alternative or adjunctive treatment option.
What are the clinical manifestations of hypopituitarism affecting the thyroid?
Clinical manifestations of thyroid hypopituitarism include bradycardia, weight gain, cold intolerance, hypothermia, and constipation.
What symptoms are associated with hypopituitarism affecting sex steroids?
Symptoms include oligomenorrhea, reduced libido, hot flushes, and reduced body hair.
How does hypopituitarism affecting cortisol levels manifest clinically?
Clinical manifestations include tiredness, weakness, anorexia, postural hypotension, and myalgia.
What symptoms are observed in individuals with hypopituitarism affecting growth hormone (GH)?
Symptoms include fatigue and central weight gain.
What are the factors that stimulate vasopressin secretion?
Vasopressin secretion is stimulated by increased plasma osmolality, decreased blood pressure (detected by baroreceptors), and alterations in blood gases such as decreased partial pressure of oxygen (PaO2) and increased partial pressure of carbon dioxide (PaCO2), mediated by hormones like cortisol, sex steroids, and angiotensin II.
What are the actions of vasopressin?
Vasopressin acts on the collecting ducts in the kidney. It increases the permeability of these ducts to water, facilitating the reabsorption of free water. Additionally, vasopressin induces vasoconstriction, contributing to increased blood pressure.
What is Syndrome of Inappropriate Antidiuretic Hormone (SIADH)?
SIADH is a condition characterized by the excessive release of antidiuretic hormone (ADH) from the pituitary gland or other sources, leading to water retention and dilutional hyponatremia.
What are some causes of SIADH?
SIADH can be caused by various factors such as brain injury or infection, lung cancer or infections like pneumonia, asthma, or mechanical ventilation (IPPV), as well as metabolic conditions like hypothyroidism and Addison’s disease.
How is Syndrome of Inappropriate Antidiuretic Hormone (SIADH) diagnosed?
SIADH can be diagnosed based on laboratory findings including decreased plasma sodium levels (<130mmol/l), decreased plasma osmolality (<285mOsm/kg), increased urine osmolality (>100mOsm/kg), and increased urine sodium (>30mmol/l).
What are the treatment options for SIADH?
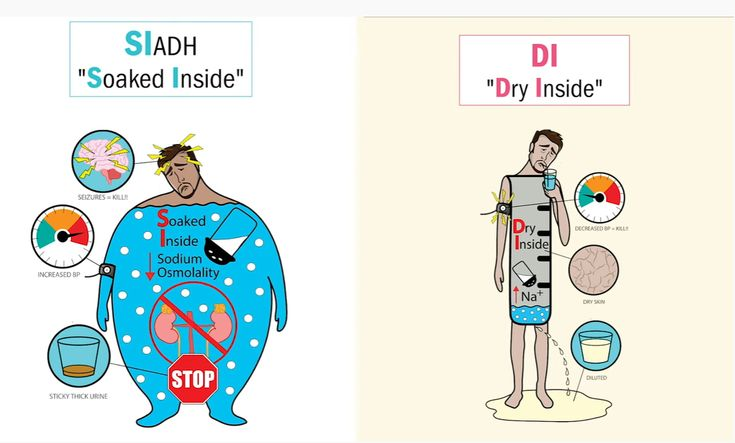
Treatment for SIADH typically involves fluid restriction to prevent further water retention. In some cases, medications like demeclocycline or ADH antagonists such as tolvaptan may be prescribed to counteract the effects of excess ADH.
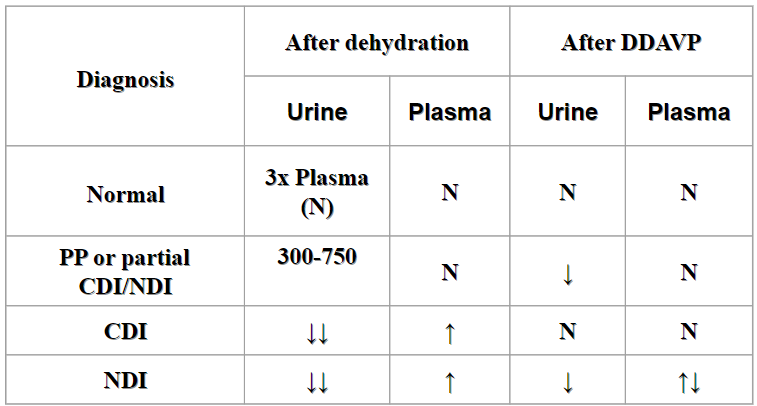
What are the main types of Diabetes Insipidus (DI)?
Diabetes Insipidus (DI) can be categorized into two main types: cranial DI, which results from a lack of production of antidiuretic hormone (ADH) in the hypothalamus or pituitary gland, and nephrogenic DI, which occurs due to the kidneys' inability to respond to ADH, often because of receptor resistance.
How is Diabetes Insipidus diagnosed?
Diabetes Insipidus is diagnosed based on clinical symptoms such as polyuria (excessive urination, often more than 3 liters per day) and polydipsia (excessive thirst), along with laboratory findings including increased plasma sodium levels, increased plasma osmolality (greater than 295 mosmol/kg), decreased urine osmolality (less than 700 mosmol/kg), and decreased urine sodium levels.
Picture demonstrating the Water Deprivation Test:
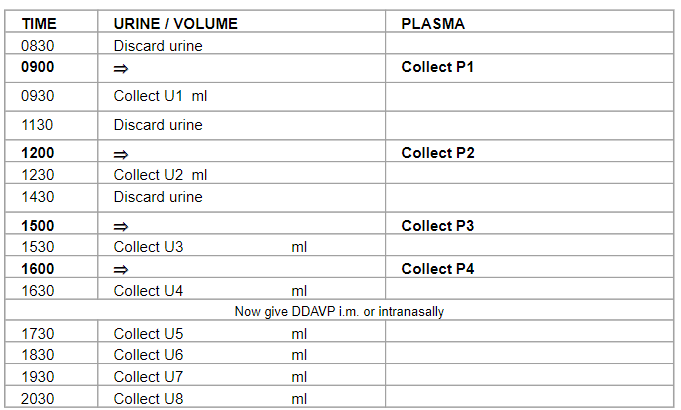
Another picture demonstrating the Water Deprivation Test:
What are the treatment options for Diabetes Insipidus (DI)?
The treatment options for Diabetes Insipidus include:
Fluid rehydration: This involves ensuring adequate fluid intake to prevent dehydration caused by excessive urination.
Desmopressin (DDAVP): Desmopressin is a synthetic form of antidiuretic hormone (ADH) that can be administered orally, intranasally, or intravenously to replace the deficient ADH hormone in individuals with central (cranial) DI.
Receptor sensitizers: In cases of nephrogenic DI, where the kidneys fail to respond to ADH, medications such as chlorpropamide can be used to enhance the sensitivity of the kidneys to ADH, thereby reducing urine output.
What are the key points regarding the pituitary gland?
Answer:
Control Center: The pituitary gland regulates most of the endocrine glands in the body.
Two Lobes: It comprises two lobes - the anterior and posterior lobes, each with distinct functions.
Tumors: Pituitary tumors are typically benign. Considerations include hormone production, impact on normal pituitary function, and effects on surrounding structures.
Treatment: Options include surgery, radiotherapy (DXT), and medical therapy, depending on the nature of the tumor.
Pituitary Failure: Hormone replacement therapy is used to manage pituitary failure, ensuring adequate levels of hormones in the body.