What are the main functions of the testes? (3)
Produce sperm for reproduction
Secrete hormones to regulate spermatogenesis
Temperature regulation for optimal sperm production
Why are the testes located outside the body? (2)
Maintain a temperature 1.5–2.5°C below body temp
Prevent overheating which reduces sperm count
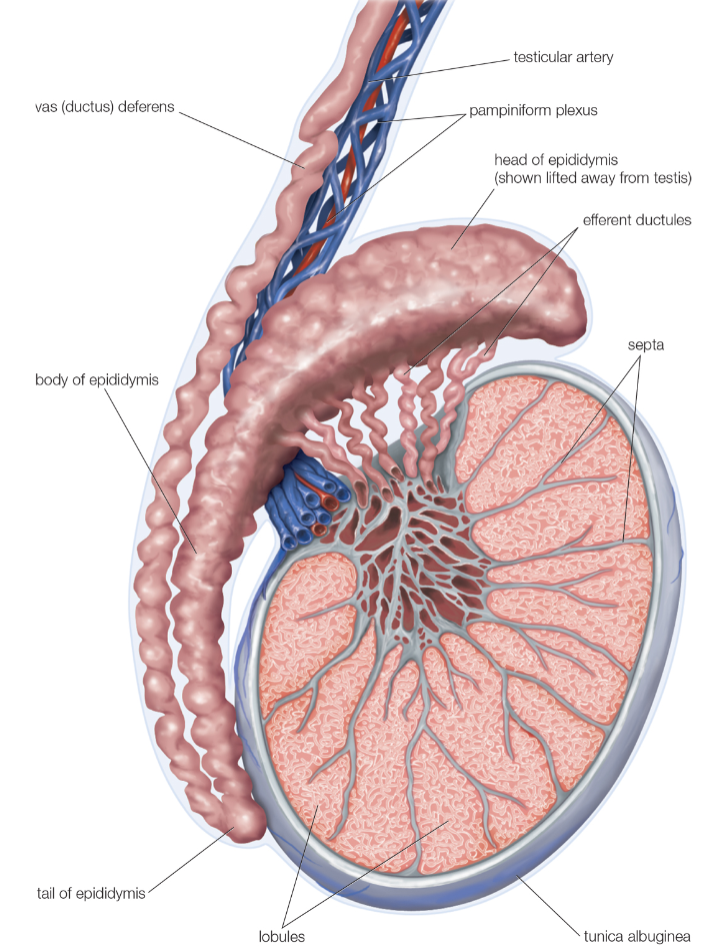
Describe the structure of the testes. (2)
Highly vascularized and innervated
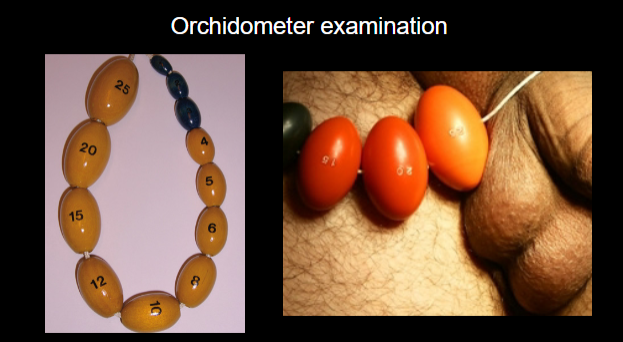
Normal volume of 15–25 ml (measured by orchidometer)
Picture demonstrating an orchidometer:
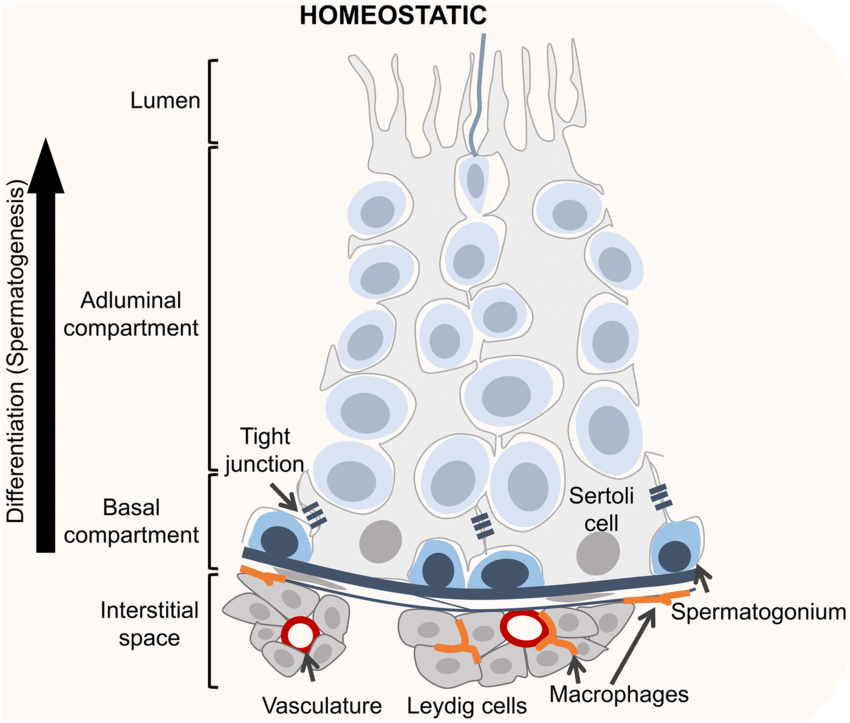
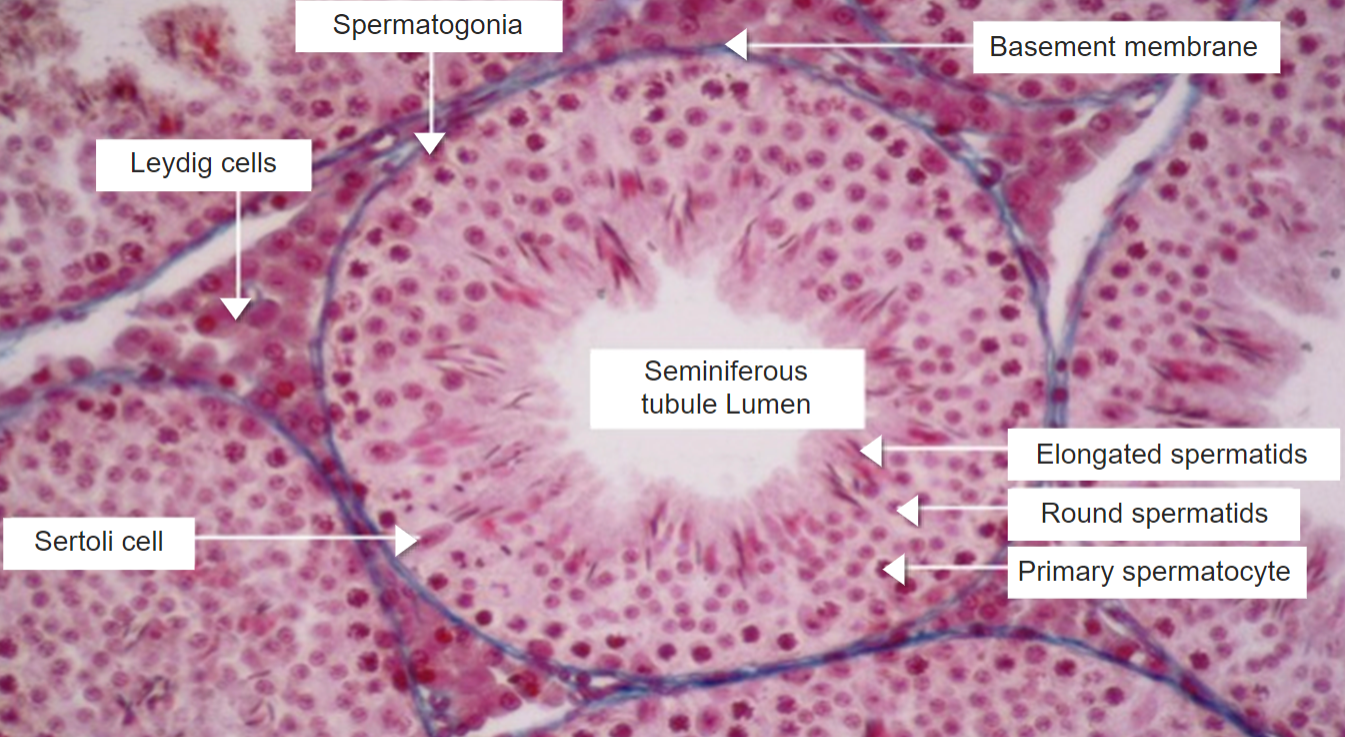
What percentage of the testis is composed of seminiferous tubules, and what is their function? (2)
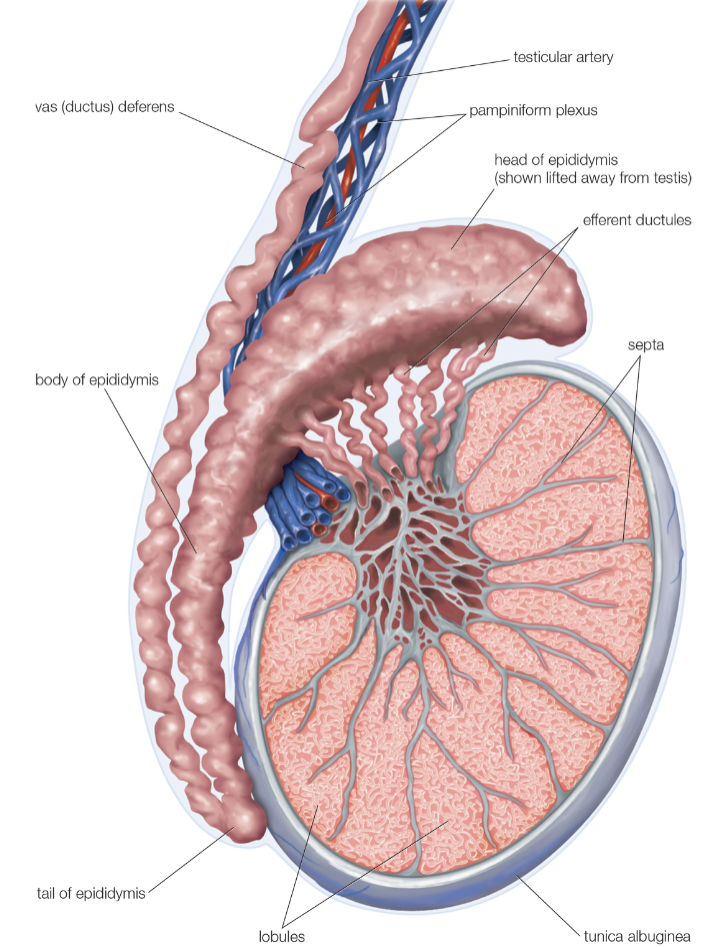
90% of the testis is made up of seminiferous tubules.
These tubules are the site of spermatogenesis.
How long are the seminiferous tubules in each testis, and what is their structure? (2)
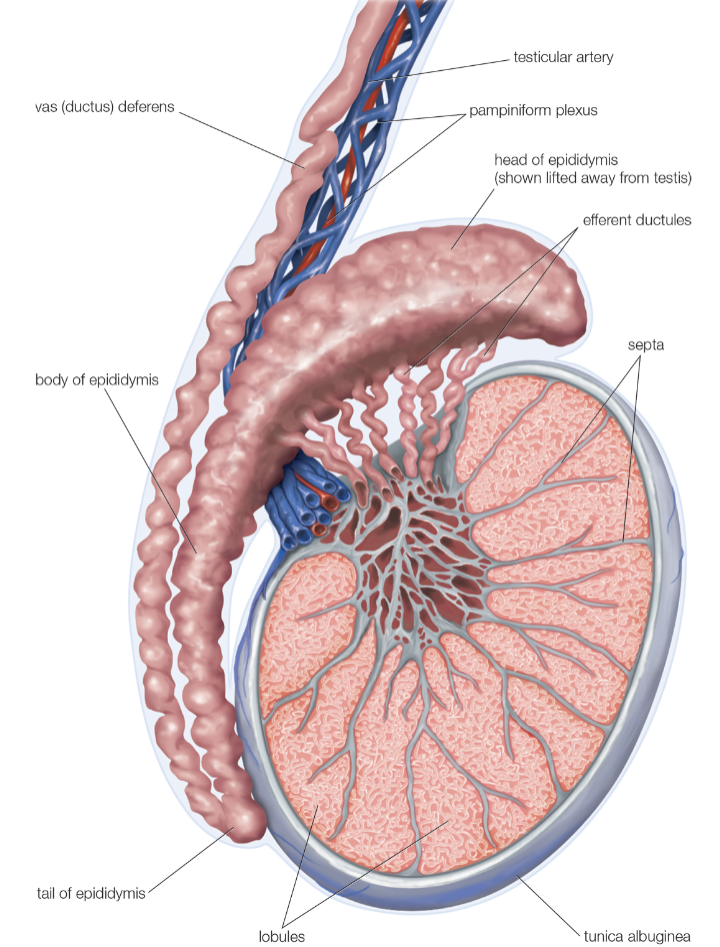
Each testis contains about 600 meters of seminiferous tubules.
The tubules are tightly coiled within the testis.
Where do the seminiferous tubules lead, and what is the pathway of sperm? (2)
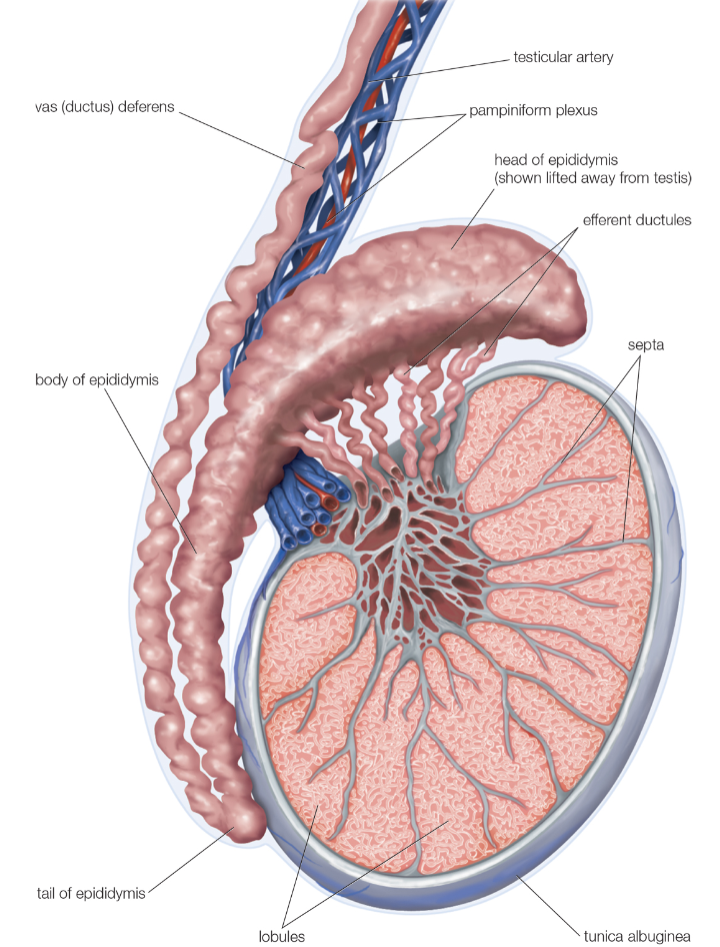
Tubules lead to the epididymis.
From the epididymis, sperm ultimately pass into the vas deferens.
How many sperm are produced per second in the testis, and what is the approximate total during an hour-long lecture? (2)
Approximately 1500 sperm are produced each second.
This amounts to about 5.5 million sperm during an hour-long lecture.
Picture demonstrating the internal structure of the Testis:
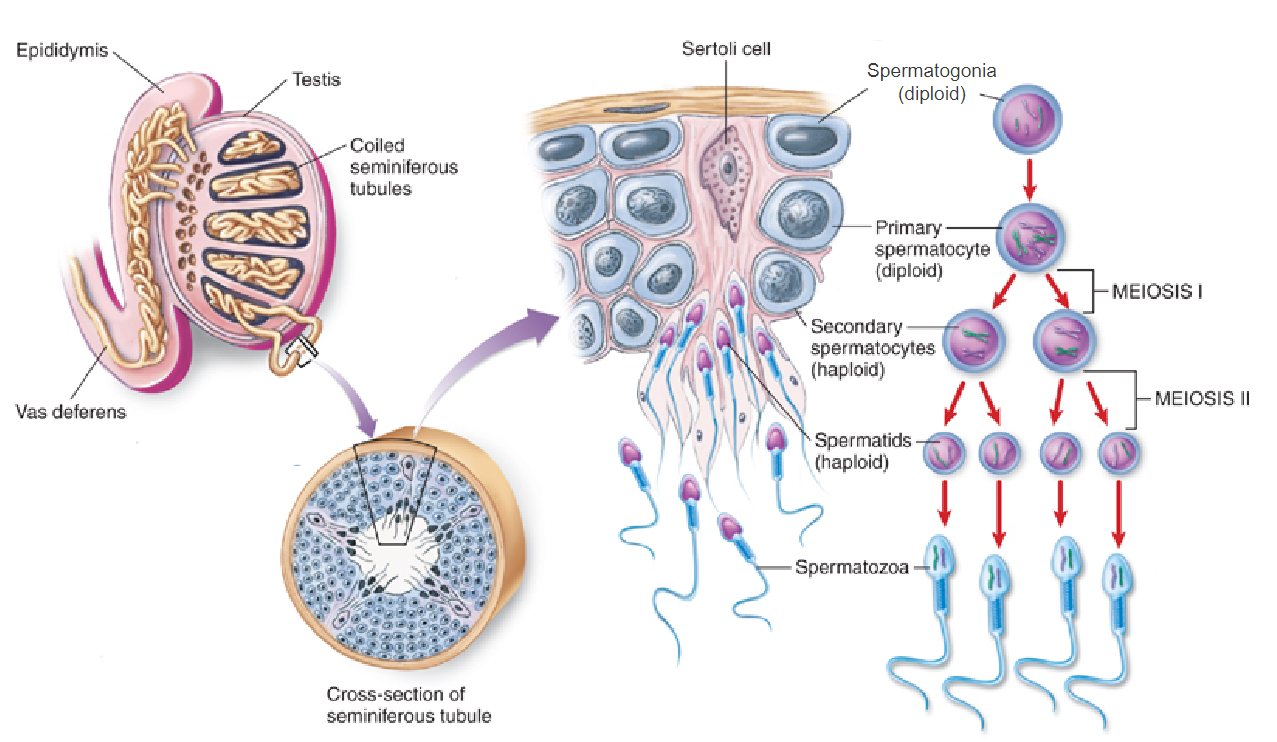
Where are primary germ cells or spermatogonia located within the testis? (1)
They are found on the basement membrane of the seminiferous tubules.
What type of cells make up the walls of the seminiferous tubules, and what is their structure? (2)
The walls are made up of tall columnar endothelial cells known as Sertoli cells.
These cells provide structural and nutritional support for developing sperm.
What is the function of tight junctions between Sertoli cells? (2)
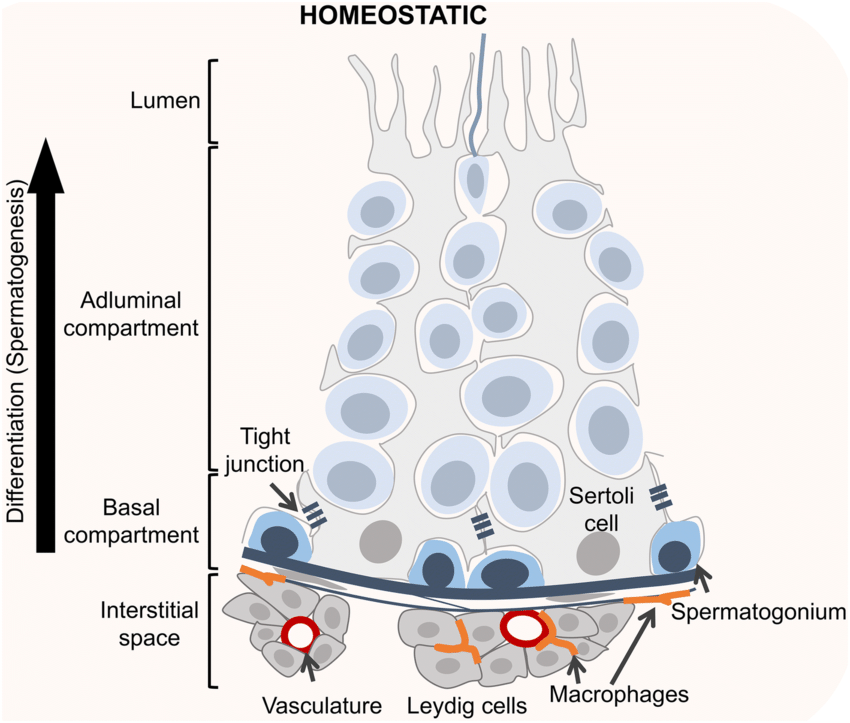
Tight junctions form the adluminal compartment within the tubules.
This compartment creates a specialized environment essential for spermatogenesis.
What fills the adluminal compartment, and what is its role in spermatogenesis? (2)
The adluminal compartment is filled with secretions from Sertoli cells.
These secretions support and nourish the developing sperm cells.
What structures are found in the spaces between the seminiferous tubules? (3)
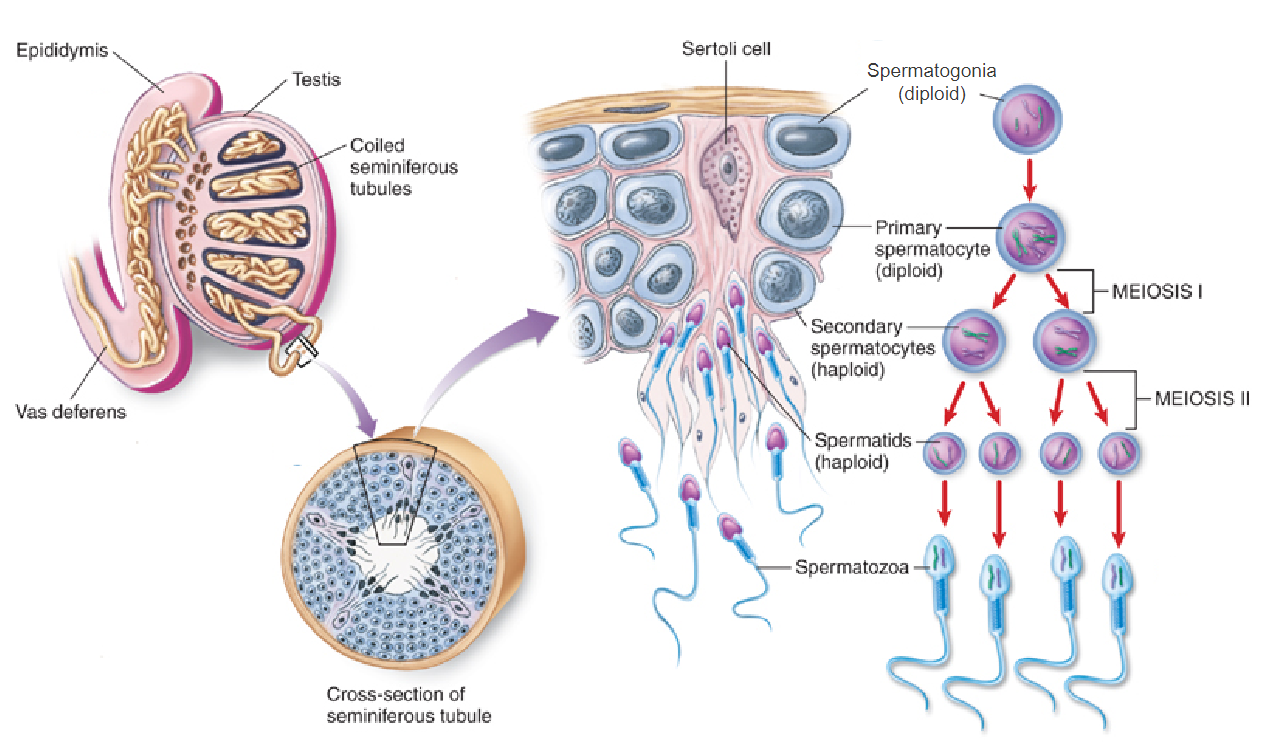
Blood vessels
Lymphatic vessels
Leydig cells and interstitial fluid
Picture demonstrating sertoli cells:
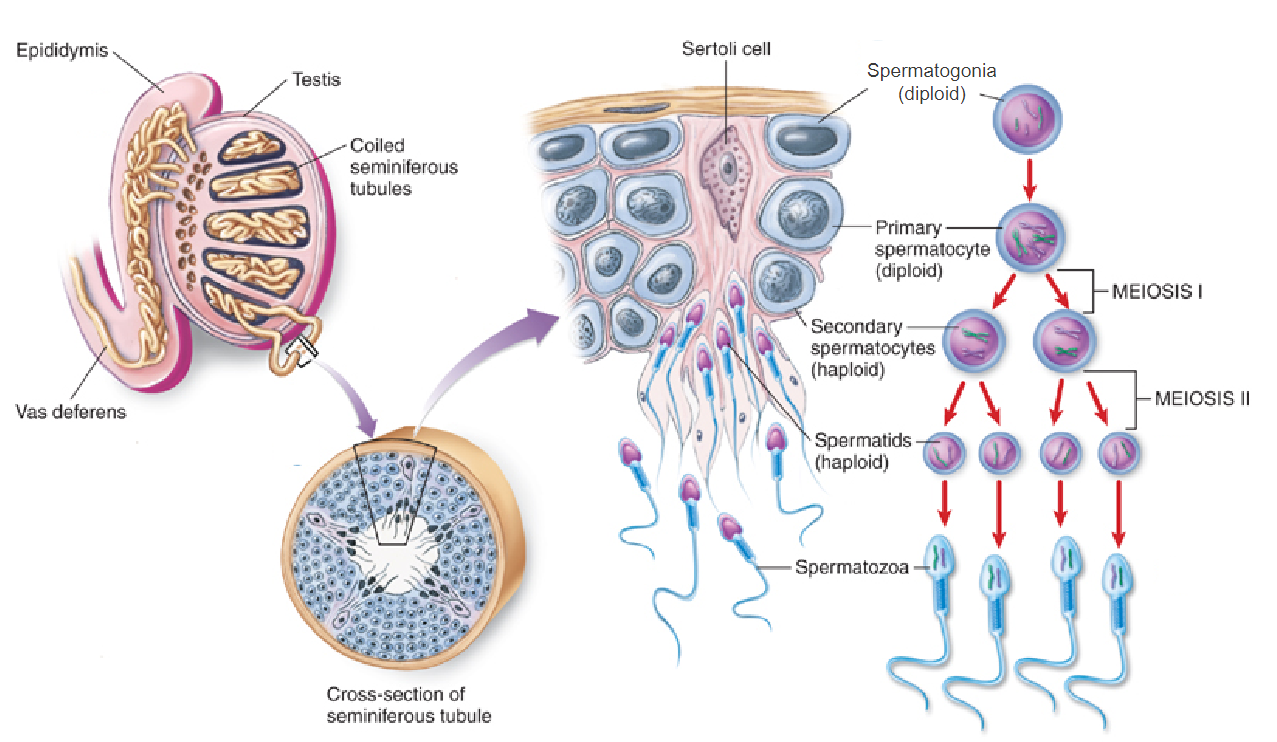
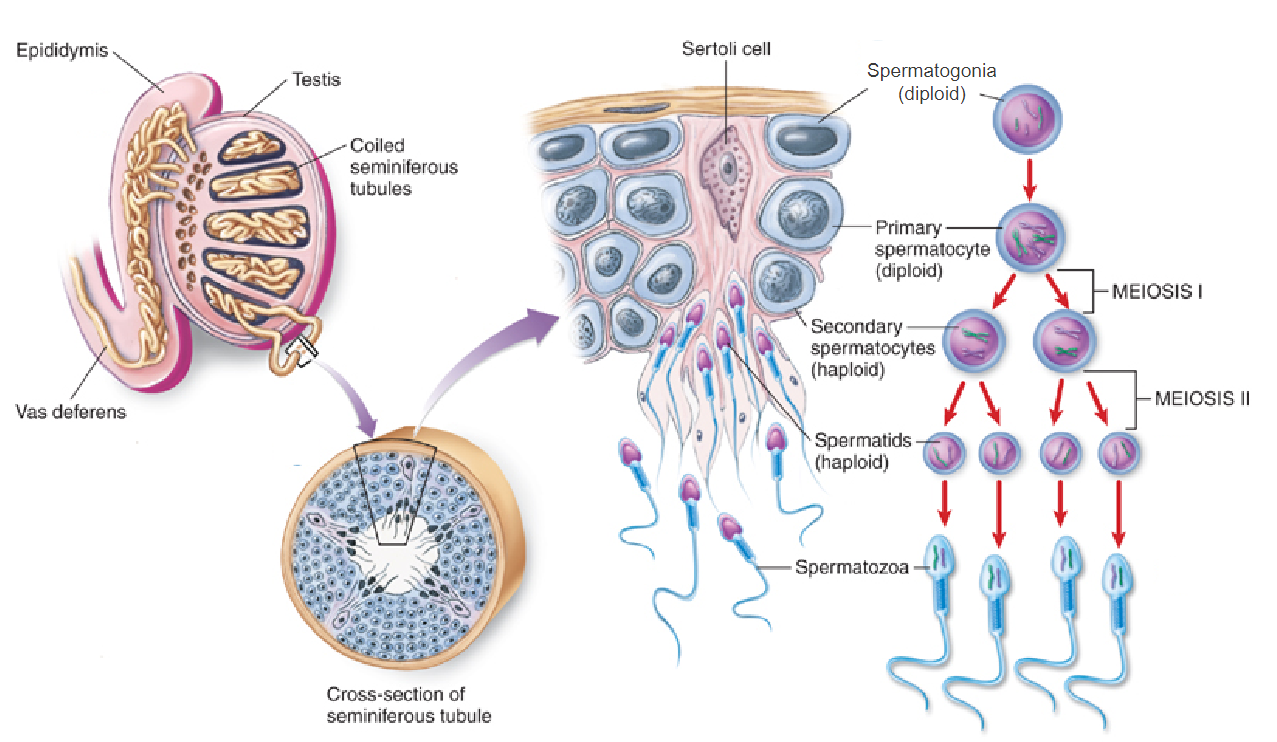
What happens to each chromosome during the interphase (S-phase) of meiosis in males? (1)
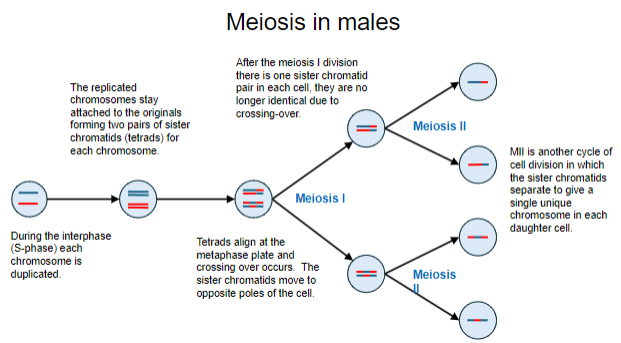
Each chromosome is duplicated, forming two pairs of sister chromatids (tetrads) for each chromosome.
What is a tetrad, and what is its significance in meiosis? (2)
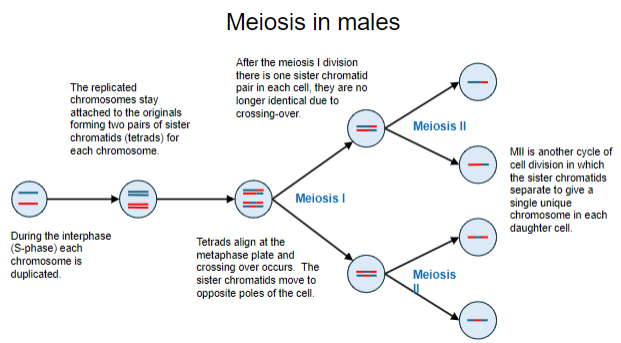
A tetrad consists of two pairs of sister chromatids attached together.
It allows for alignment and crossing over at the metaphase plate.
What key event occurs when tetrads align at the metaphase plate in meiosis I? (1)
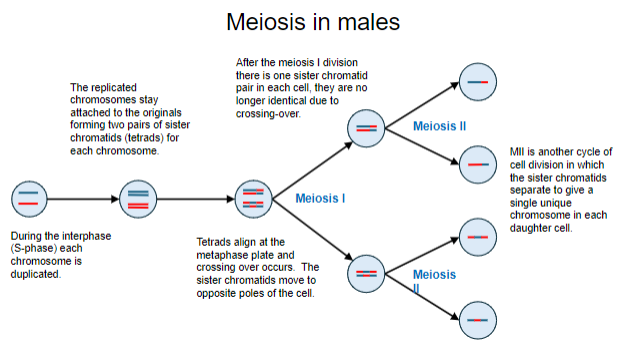
Crossing over occurs, allowing genetic material to be exchanged between chromatids.
What is the result of meiosis I in terms of chromosome arrangement in each cell? (2)
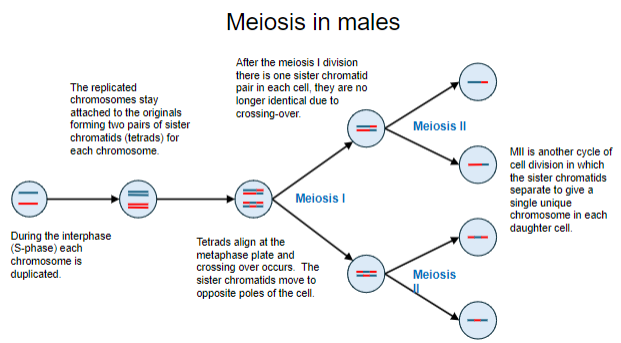
Each cell contains one pair of sister chromatids.
These chromatids are no longer identical due to crossing-over.
What is the role of germ cells in spermatogenesis? (2)
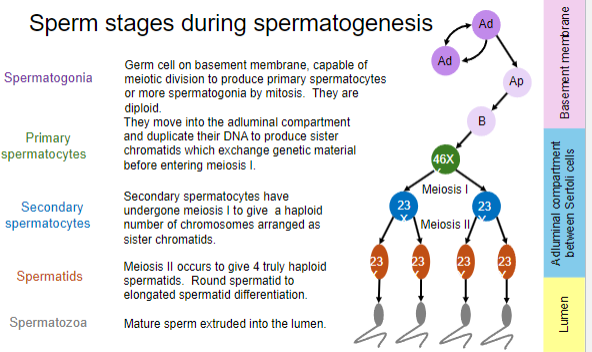
Germ cells on the basement membrane are diploid and capable of meiotic division.
They produce primary spermatocytes or more spermatogonia by mitosis
What happens when primary spermatocytes enter the adluminal compartment? (2)
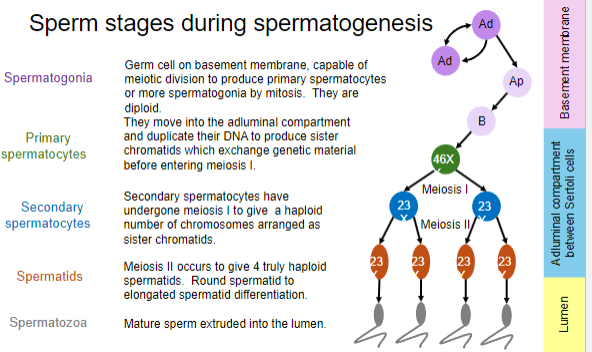
"Primary spermatocytes begin Meiosis I, where homologous chromosomes pair up and exchange genetic material via crossing over.
They progress through prophase I in the adluminal compartment, actively undergoing recombination and preparing for the reductional division (which will occur in the subsequent stages of Meiosis I).
What defines secondary spermatocytes in spermatogenesis? (1)
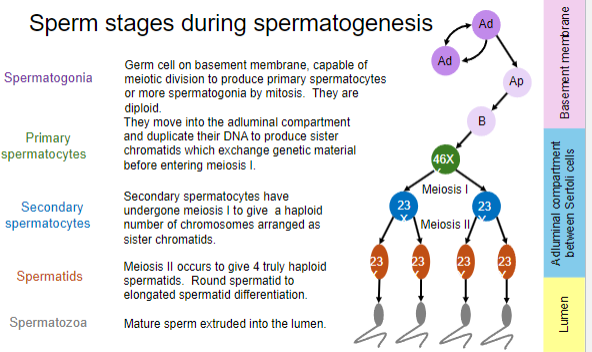
Secondary spermatocytes have completed meiosis I and contain a haploid number of chromosomes arranged as sister chromatids.
What occurs during meiosis II in spermatogenesis? (2)
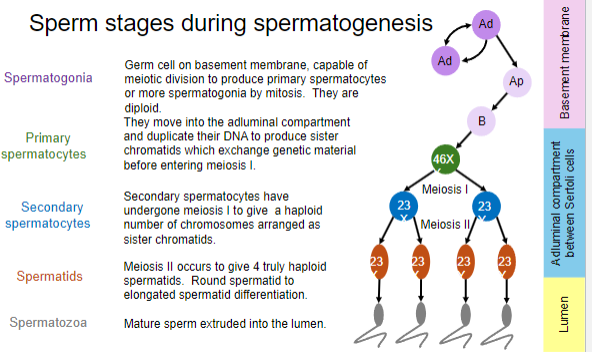
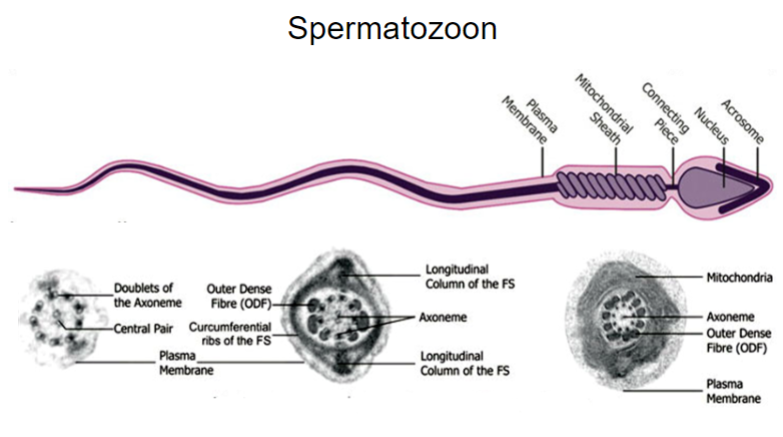
Meiosis II produces four truly haploid spermatids.
Spermatids then undergo differentiation from a round to an elongated shape.
How do mature sperm reach the lumen? (1)
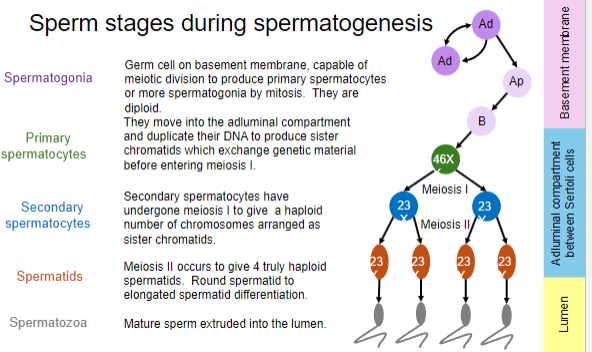
Mature sperm, or spermatozoa, are extruded into the lumen.
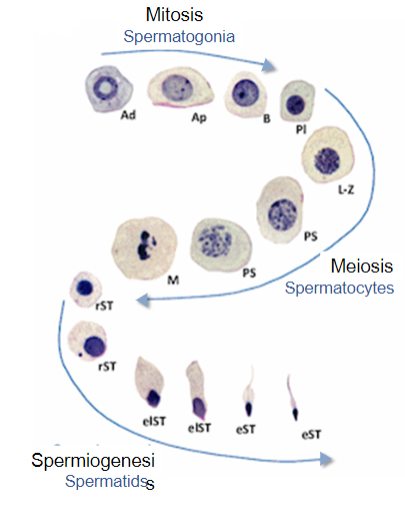
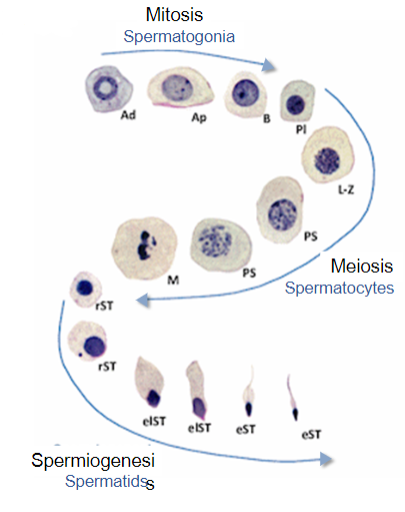
List the main stages of sperm development in order. (5)
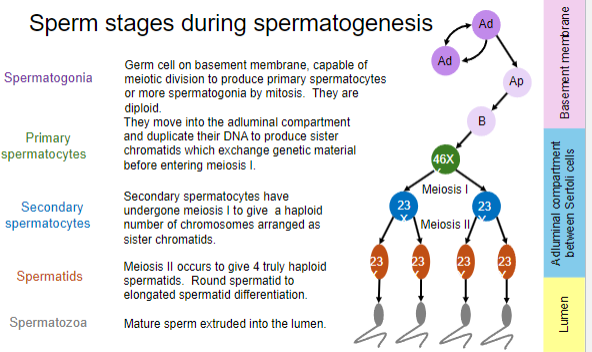
Spermatogonia
Primary spermatocytes
Secondary spermatocytes
Spermatids
Spermatozoa
How often does a new cycle of spermatogenesis begin, and how long does the full process take? (2)
A new cycle begins every 16 days.
The full process of spermatogenesis takes approximately 74 days.
What is unique about cell division from spermatogonium to spermatid? (2)
Each division is incomplete; cells remain connected by cytoplasmic bridges.
This forms a syncytium, allowing cells to develop synchronously.
What is the role of syncytia in spermatogenesis? (1)
Syncytia at various developmental stages within seminiferous tubules ensure a continuous supply of developing sperm.
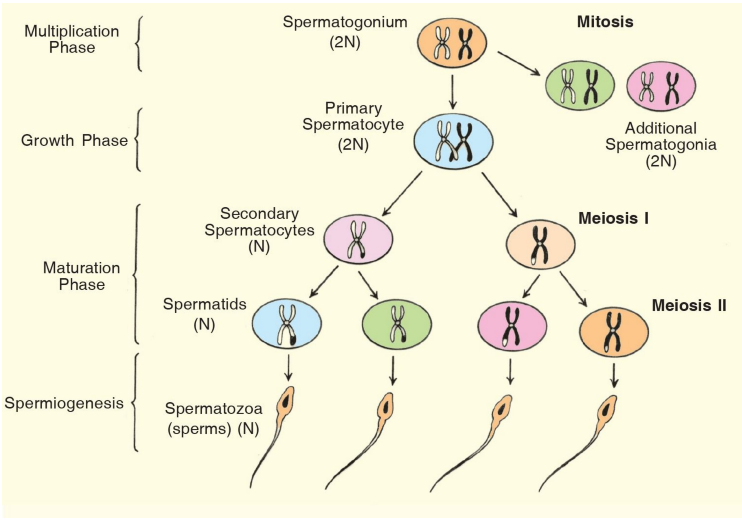
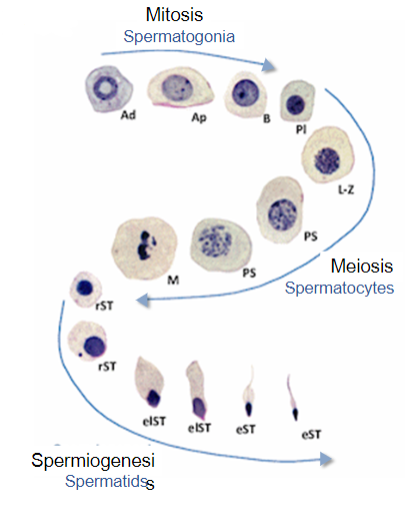
What are the three main stages of spermatogenesis? (3)
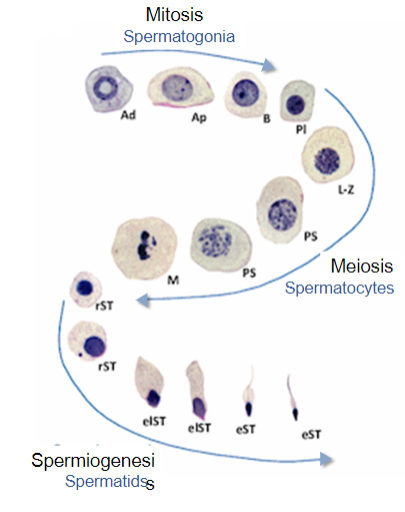
Mitosis: Proliferation of spermatogonia.
Meiosis: Development of spermatocytes.
Spermiogenesis: Elongation, cytoplasm loss, and reorganization of cellular contents.
What occurs during spermiogenesis? (3)
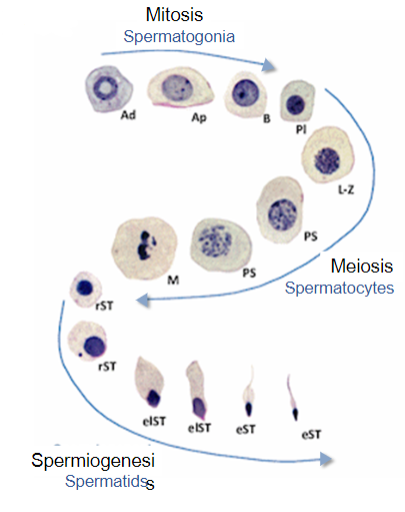
Elongation of spermatids.
Loss of excess cytoplasm.
Movement and reorganization of cellular contents.
What is the ploidy and developmental timing of oogonia? (2)
Oogonia are diploid cells.
All oogonia are established during fetal development.
What happens to oogonia before birth? (2)
Oogonia begin meiosis to develop into primary oocytes before birth.
Once initiated, they do not continue to produce more oogonia.
What is the availability of oogonia? (1)
Oogonia provide a limited supply of cells.
What is the ploidy and developmental timing of spermatogonia? (2)
Spermatogonia are also diploid cells.
They are produced during fetal development but only begin meiosis to form spermatocytes after puberty.
How do spermatogonia proliferate? (2)
Spermatogonia can undergo mitosis to produce more spermatogonia.
This allows for a lifetime supply of sperm-producing cells.
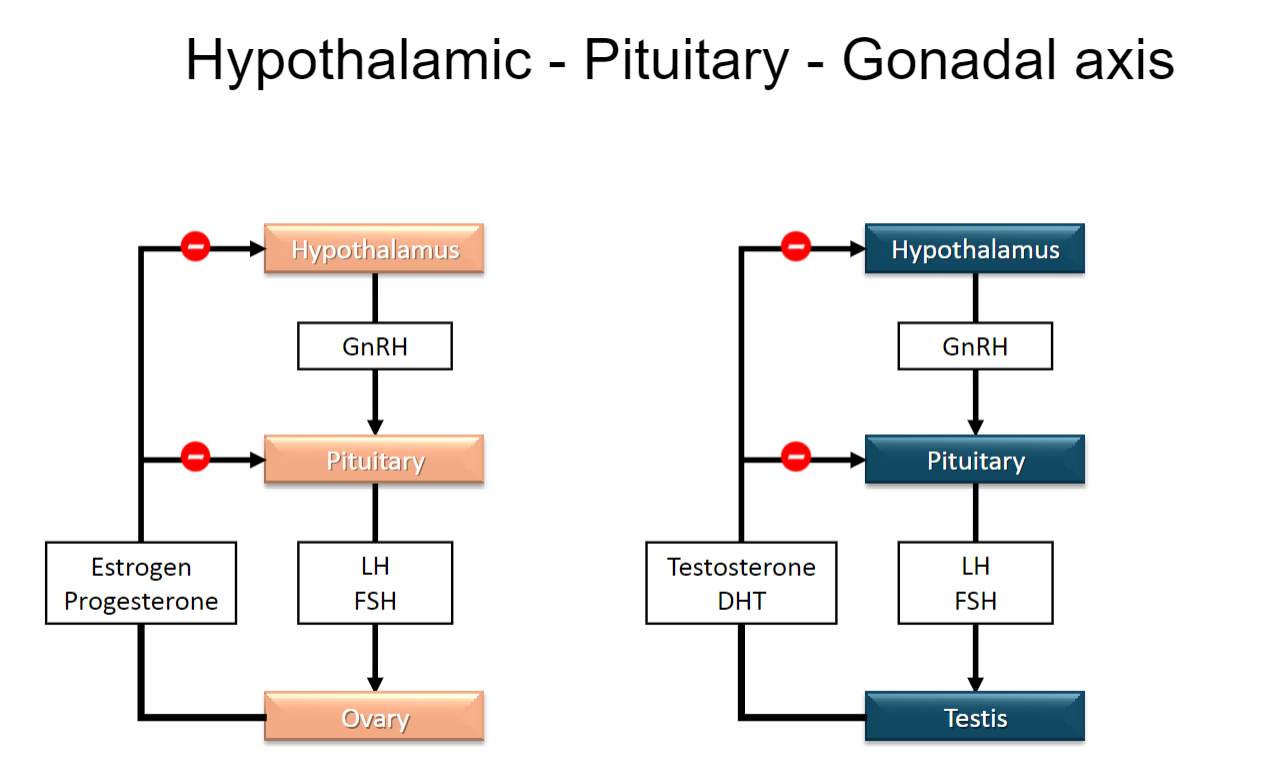
Picture demonstrating the Hypothalamic - Pituitary - Gonadal axes:
What is the primary function of Leydig cells in the testes? (2)
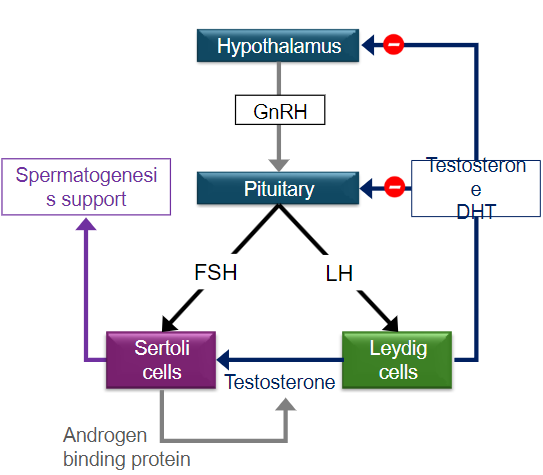
Leydig cells contain LH receptors.
They primarily convert cholesterol into androgens, which are crucial for male reproductive function.
How do androgens affect Sertoli cells? (2)
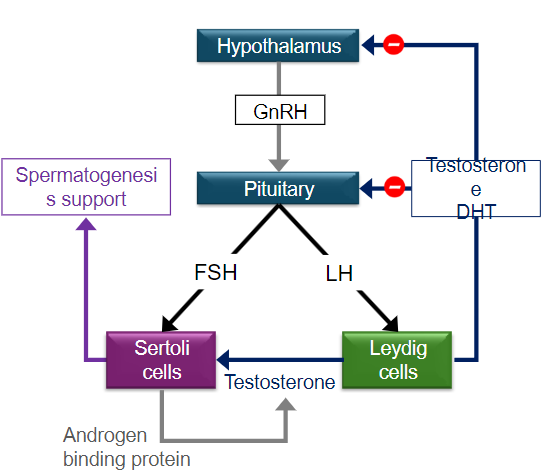
Androgens stimulate Sertoli cell function.
This stimulation initiates and maintains sperm production within the seminiferous tubules.
What role do Sertoli cells play in spermatogenesis? (2)
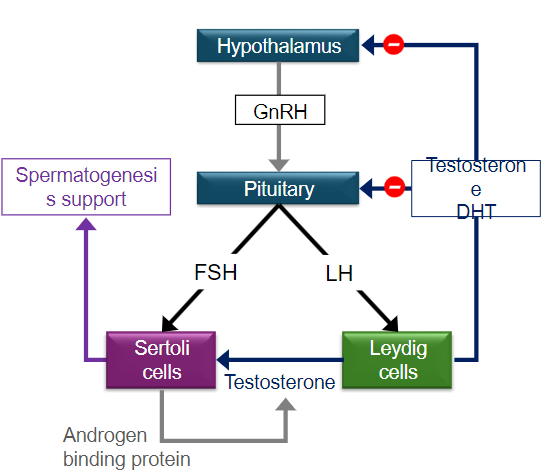
Sertoli cells contain FSH receptors that are essential for establishing a healthy Sertoli cell population.
They support the development and maturation of sperm cells throughout spermatogenesis.
What is the function of Androgen Binding Protein (ABP)? (2)
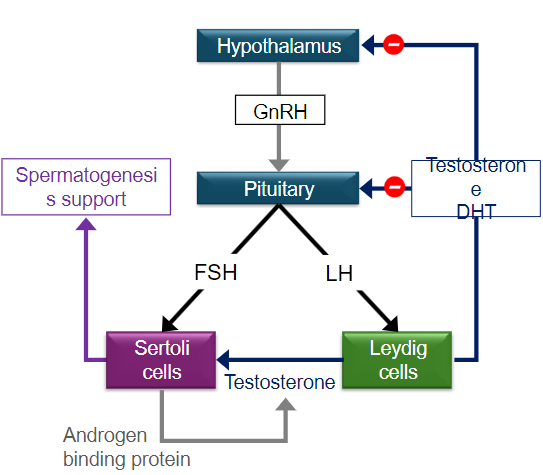
ABP binds to testosterone and dihydrotestosterone (DHT), keeping them concentrated in the seminiferous tubules, and not diffusing into the bloodstream
This high concentration of androgens is essential for spermatogenesis (sperm production).
How do intra-testicular testosterone levels compare to plasma levels? (1)
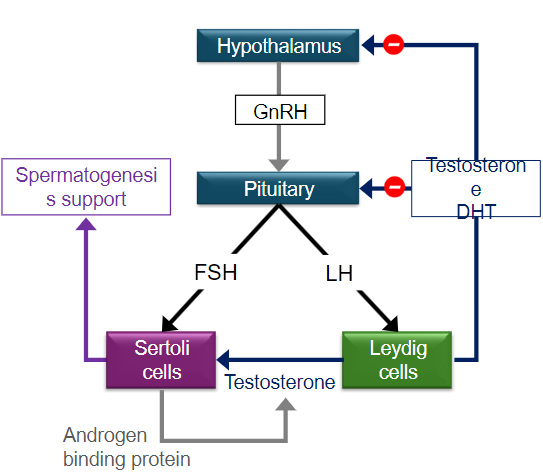
Intra-testicular testosterone levels are 100 times higher than those found in plasma, which is vital for effective spermatogenesis.
What is the relationship between ABP and sex hormone binding globulin (SHBG)? (2)
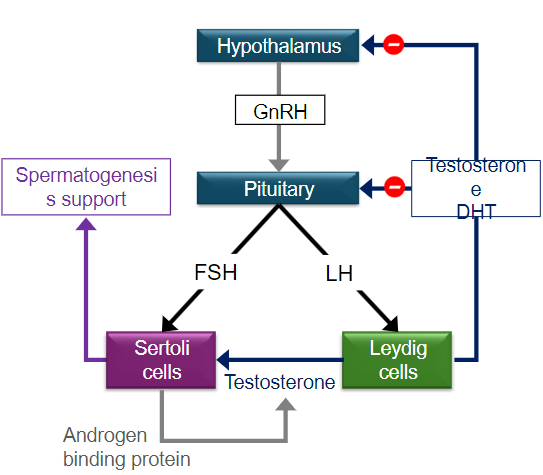
Same Protein, Different Roles: ABP (Androgen-Binding Protein) and SHBG (Sex Hormone-Binding Globulin) are the same protein but are called different names depending on where they are found and what they do.
ABP is made in the testes and helps concentrate testosterone for sperm production.
SHBG is made in the liver and carries sex hormones like testosterone and estrogen in the bloodstream to other parts of the body.
Role in Hormone Transport: Both ABP and SHBG bind to androgens (like testosterone) and help control how much is available to target tissues.

How do anabolic steroids affect the hormonal feedback loop in males? (3)

Anabolic steroids reduce the secretion of FSH and LH from the pituitary gland.
This decrease in gonadotropins leads to testicular atrophy, as the testes are not stimulated adequately.
The overall balance of the hypothalamic-pituitary-gonadal (HPG) axis is disrupted, reducing levels of testosterone and dihydrotestosterone (DHT) produced by the testes.
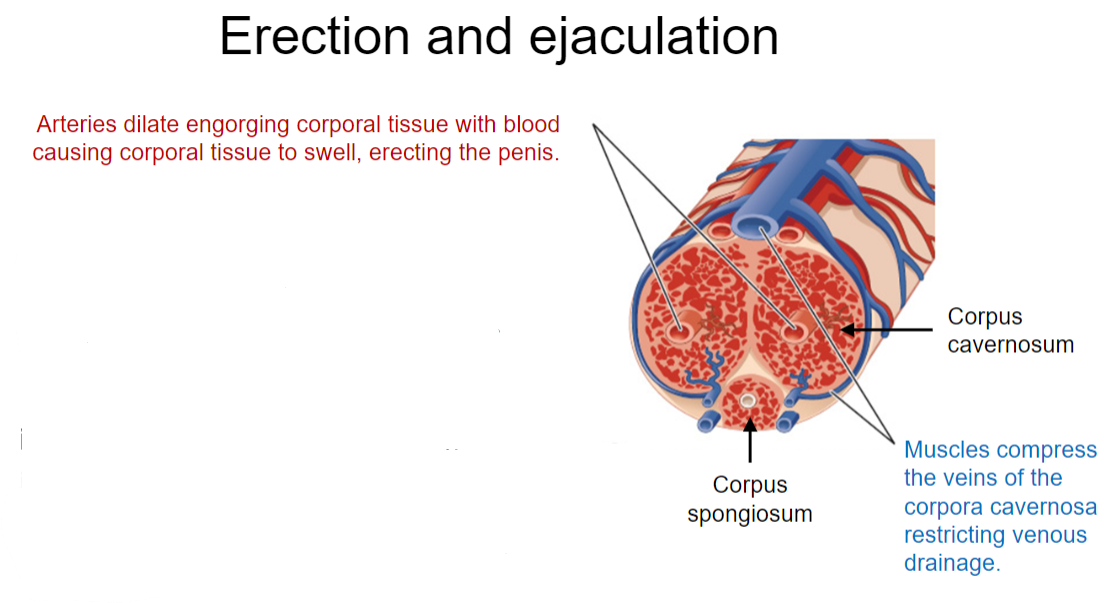
What are the physiological processes involved in erection? (3)
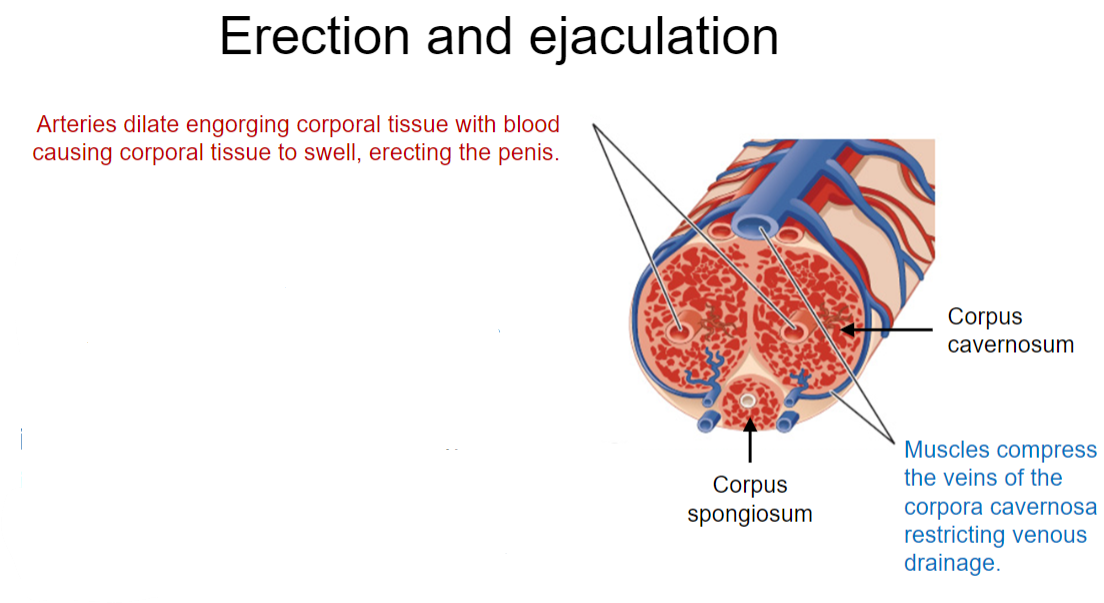
Arterial Dilation: The arteries dilate, leading to increased blood flow and engorgement of the corporal tissue.
Parasympathetic Activation: The erection is primarily mediated by the parasympathetic nervous system, resulting in vasodilation of the corpus cavernosum and compression of veins to reduce venous drainage.
Tissue Swelling: The engorged corporal tissue causes the penis to swell and become erect.
How is ejaculation achieved in males? (3)
Sympathetic Activation: Ejaculation is coordinated by the sympathetic nervous system, leading to smooth muscle contractions.
Emission: Sperm is moved from the epididymis into the vas deferens and through the penile urethra.
Expulsion: The process concludes with the expulsion of glandular secretions and the evacuation of the urethra, completing ejaculation.
What is the mechanism of arterial blood flow during erection? (4)
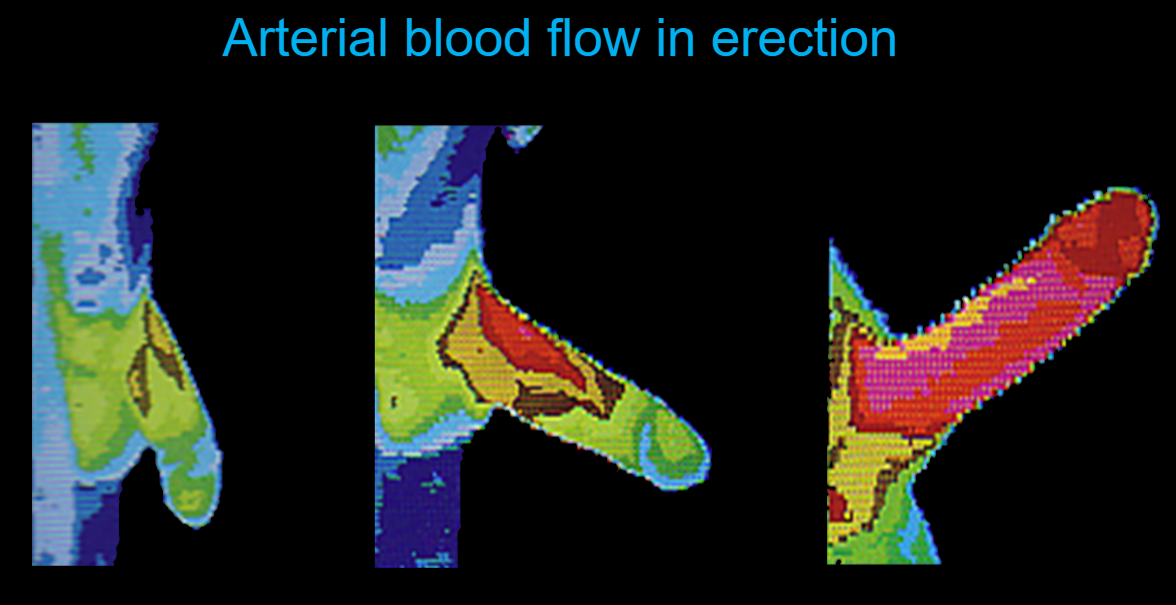
Neurotransmitter Release: Acetylcholine, derived from the parasympathetic nervous system, binds to muscarinic receptors on the endothelium of blood vessels.
Nitric Oxide Production: This binding stimulates the release of nitric oxide (NO).
Smooth Muscle Relaxation: Nitric oxide diffuses into the arterial smooth muscle, leading to relaxation and vasodilation.
Increased Blood Flow: The enhanced blood flow into the penis compresses the veins, causing partial constriction of venous return, which maintains the erection.
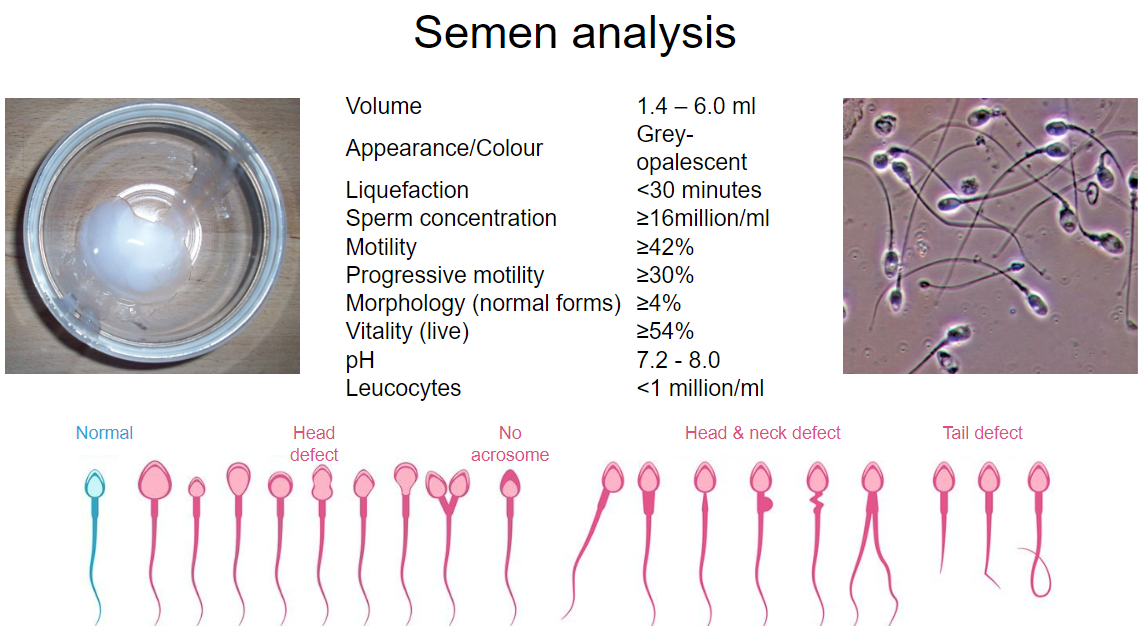
What are the characteristics of normal ejaculate? (5)
Volume: Normal ejaculate volume ranges from 1.5ml to 6ml, equivalent to about one-third to just over a teaspoon.
Sperm Density: The initial portion of the ejaculate contains the highest concentration of sperm.
Sperm Count: An average ejaculate contains 120 million or more sperm, but only around 120,000 sperm reach the egg.
Seminal Fluid Composition: Seminal fluid is primarily made up of secretions from the seminal vesicles and prostate, combined with epididymal fluid.
Functionality: The combined secretions provide the necessary environment for sperm mobility and survival.
What is the role of the Bulbo-Urethral Gland in seminal fluid production? (4)
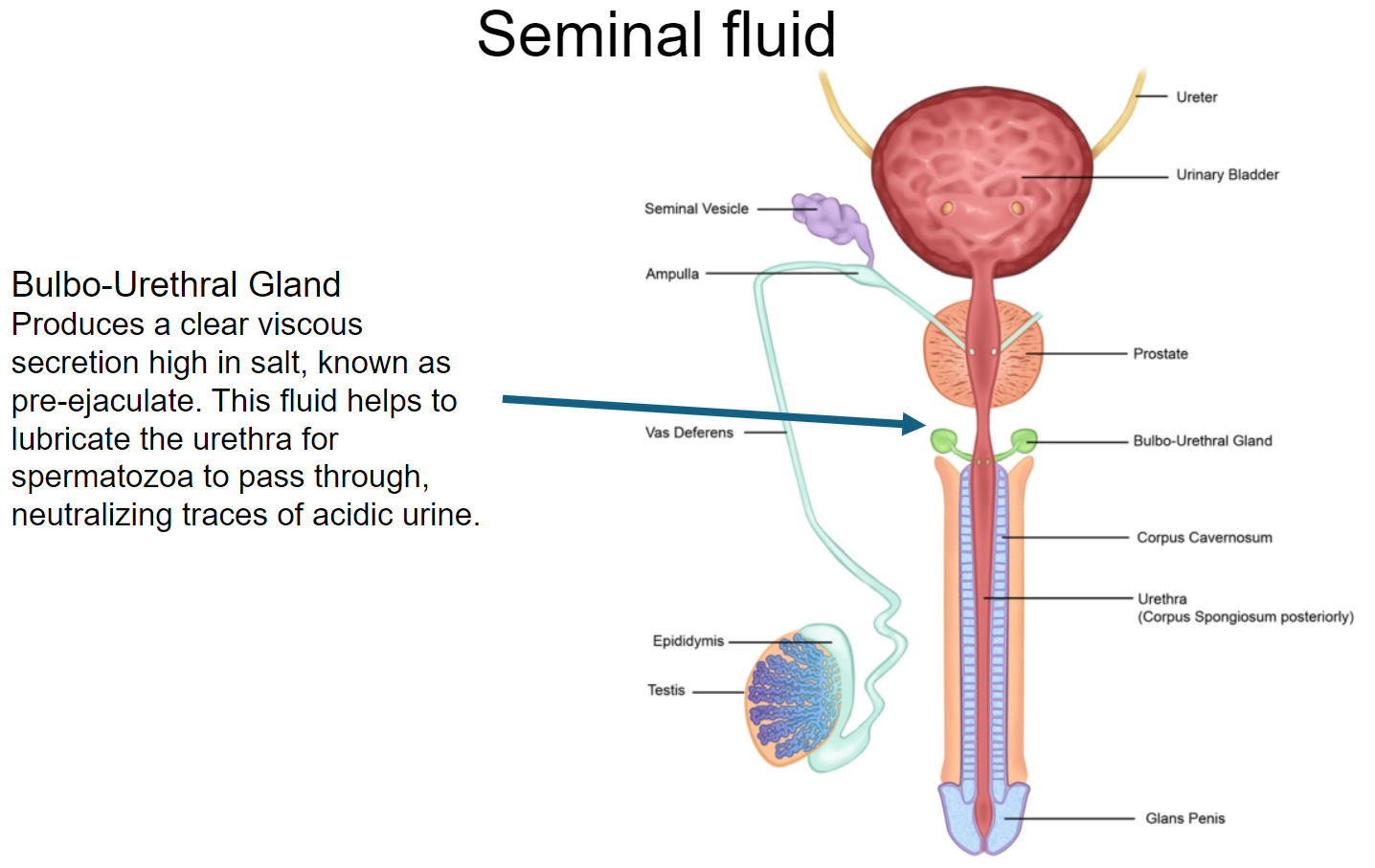
Secretion Type: Produces a clear, viscous secretion high in salt, known as pre-ejaculate.
Lubrication: The secretion helps lubricate the urethra, facilitating the passage of spermatozoa.
pH Neutralization: It plays a crucial role in neutralizing traces of acidic urine in the urethra.
Functionality: This fluid prepares the urethra for the passage of sperm during ejaculation.
What are the functions of the Seminal Vesicles in seminal fluid production? (5)
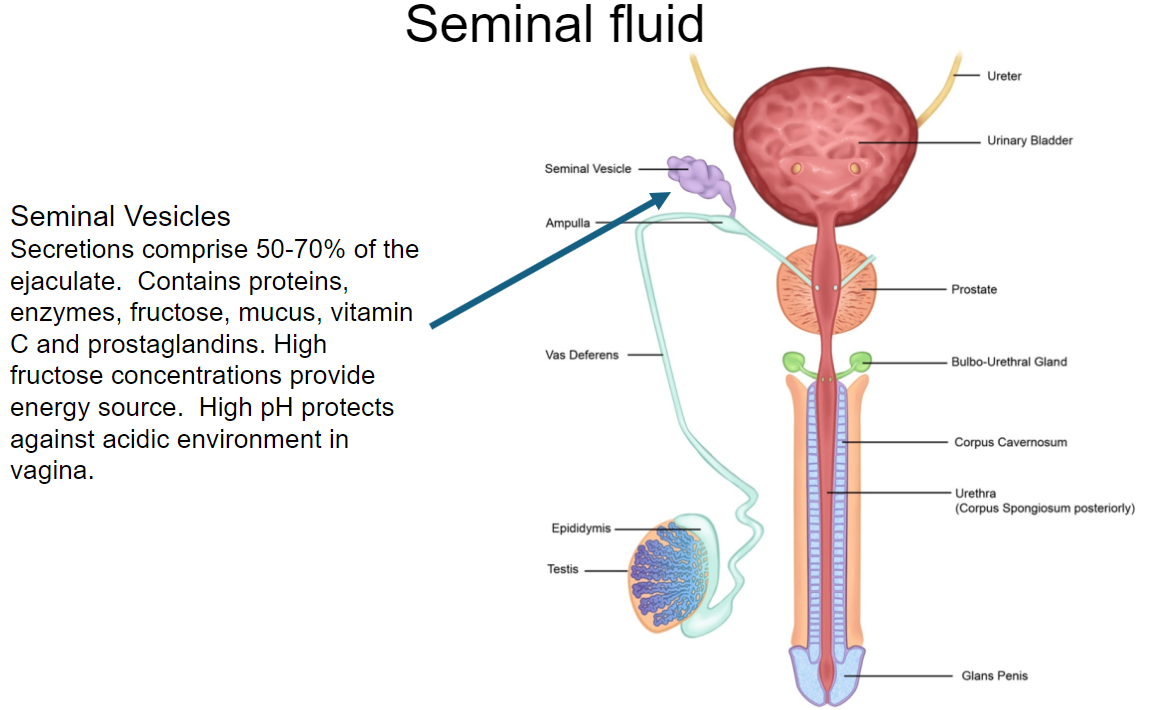
Contribution to Ejaculate: Secretions from the seminal vesicles comprise 50-70% of the ejaculate.
Nutritional Components: Contains proteins, enzymes, fructose, mucus, vitamin C, and prostaglandins.
Energy Source: High fructose concentrations provide a crucial energy source for sperm.
pH Regulation: The secretion has a high pH, which helps to protect sperm against the acidic environment of the vagina.
Function of Prostaglandins: Prostaglandins are involved in sperm motility and may facilitate smooth muscle contractions in the female reproductive tract.
What is the role of the prostate in seminal fluid production? (5)
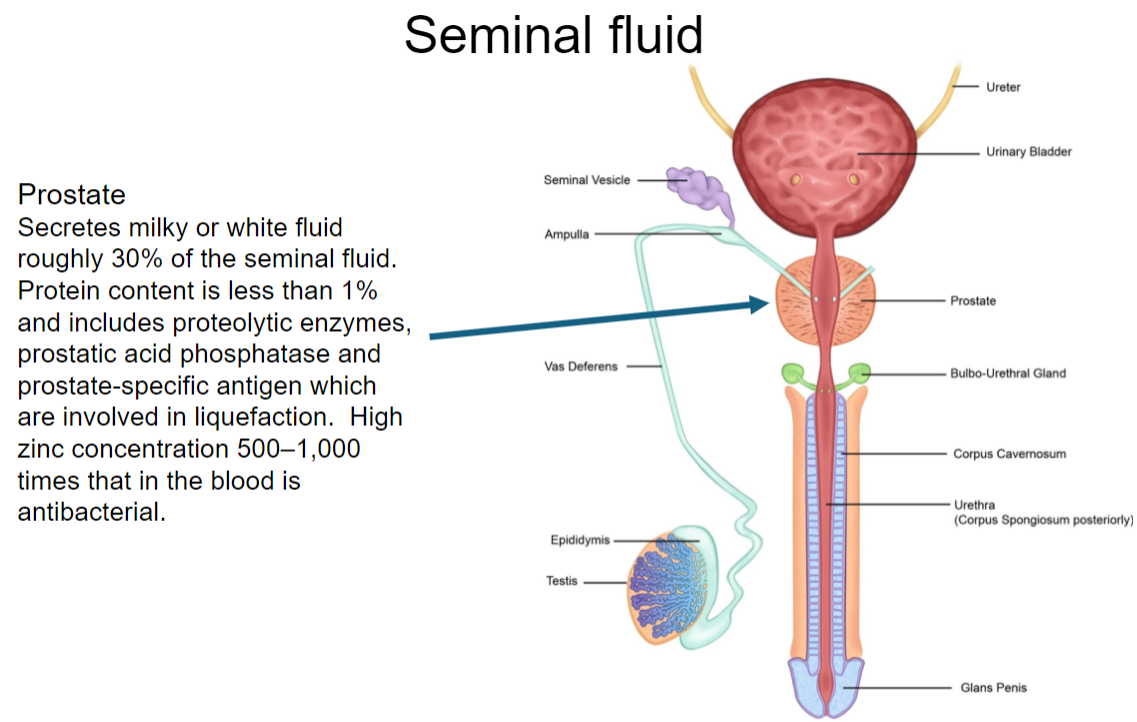
Volume Contribution: The prostate secretes a milky or white fluid that accounts for roughly 30% of seminal fluid.
Protein Content: The protein content in prostatic fluid is less than 1%.
Key Enzymes: Contains proteolytic enzymes, prostatic acid phosphatase, and prostate-specific antigen (PSA), which are important for liquefaction of semen.
Zinc Concentration: Prostatic fluid has a high zinc concentration (500–1,000 times that in blood), which provides antibacterial properties.
Overall Function: These components help to ensure sperm viability and promote successful fertilization.
Picture demonstrating Semen Analysis:
Picture Demonstrating Spermatozoon:
What structural features of the testis are specialized for the production of sperm? (5)
Seminiferous Tubules: Composed of 90% seminiferous tubules, where spermatogenesis occurs.
Temperature Regulation: Located in the scrotum, providing an optimal temperature (1.5-2.5°C below body temperature) for sperm production.
Vascularization: The testes are well-vascularized, ensuring a good blood supply for nutrient delivery and waste removal.
Leydig Cells: Interstitial cells that produce androgens, essential for regulating spermatogenesis.
Sertoli Cells: Provide structural support and nutrients to developing sperm and create the blood-testis barrier to protect germ cells.
What roles do Leydig and Sertoli cells play in supporting spermatogenesis? (4)
Leydig Cells:
Produce testosterone and other androgens, stimulating spermatogenesis.
Provide hormonal regulation necessary for the maturation of sperm cells.
Sertoli Cells:
Nourish developing sperm through secretion of various growth factors and nutrients.
Create a blood-testis barrier via tight junctions, maintaining a specialized environment for spermatogenesis.
Regulate the passage of hormones and other substances critical for sperm development.
Phagocytose residual cytoplasm during spermatogenesis.
What role does mitosis play in the maintenance of the spermatogonia pool? (3)
Production of New Spermatogonia: Mitosis allows spermatogonia to divide and produce new spermatogonia, maintaining the pool of precursor cells.
Sustaining Sperm Production: Continuous mitotic division ensures a steady supply of cells that can enter spermatogenesis.
Adaptation to Needs: Mitotic activity can adjust according to the body's demand for sperm, helping to ensure reproductive capacity.
How does meiosis I differ from meiosis II in the context of spermatogenesis? (4)
Meiosis I:
Reduction Division: Reduces the diploid number of chromosomes (2n) to haploid (n) by separating homologous chromosomes.
Tetrad Formation: Homologous chromosomes pair up and can undergo crossing over, increasing genetic diversity.
Resulting Cells: Produces two secondary spermatocytes, each containing sister chromatids.
Meiosis II:
Equational Division: Similar to mitosis, separating sister chromatids into individual chromosomes.
No DNA Replication: Occurs without an intervening round of DNA replication.
Resulting Cells: Produces a total of four haploid spermatids from the two secondary spermatocytes.
What process leads to nitric oxide (NO) contributing to erection? (3)
Neurotransmitter Release: During sexual arousal, the parasympathetic nervous system releases acetylcholine and other neurotransmitters.
Nitric Oxide Synthesis: Acetylcholine stimulates the endothelium of blood vessels in the penis to release nitric oxide.
Vasodilation: NO diffuses into the smooth muscle of the arteries, causing relaxation and vasodilation, increasing blood flow into the penis, leading to erection.
What role do the accessory glands (seminal vesicles & prostate) play in the composition of semen? (5)
Seminal Vesicles:
Produce 50-70% of semen volume.
Secrete fructose (energy source for sperm), mucus, proteins, and prostaglandins.
Prostaglandins help with sperm motility and transport within the female reproductive tract.
Prostate Gland:
Contributes approximately 30% of seminal fluid.
Secretes a milky fluid containing proteolytic enzymes that aid in semen liquefaction.
Contains high zinc levels, providing antibacterial properties and protecting sperm.
What parameters are assessed in a routine semen analysis, and what can they tell us about male fertility? (5)
Semen Volume: Normal range is 1.5ml - 6ml; low volume may indicate issues with the accessory glands.
Sperm Concentration: Number of sperm per milliliter; low concentration can suggest fertility problems.
Sperm Motility: Percentage of sperm that are moving; reduced motility can hinder the ability to reach and fertilize an egg.
Sperm Morphology: Percentage of sperm with a normal shape; abnormal morphology may affect fertility potential.
pH Level: Normal semen pH is slightly alkaline; abnormal pH can indicate infections or other issues affecting fertility.
A Glossary:
Spermatogonia – primary male germ cells
Spermatocytes – male germ cells undergoing meiosis
Spermatids – immature haploid spermatozoa
Mitosis – Cell division giving rise to diploid daughter cells
Meiosis – Cell division giving rise to haploid daughter cells
Seminiferous tubules – testicular structures that are the site of spermatogenesis
Spermiogenesis – final phase of sperm maturation
Adluminal compartment – space between tight junctions of sertoli cells where sperm develop
Epididymis – duct behind the testis, along which sperm passes to the vas deferens.
Vas deferens – duct which conveys sperm from the testicle to the urethra