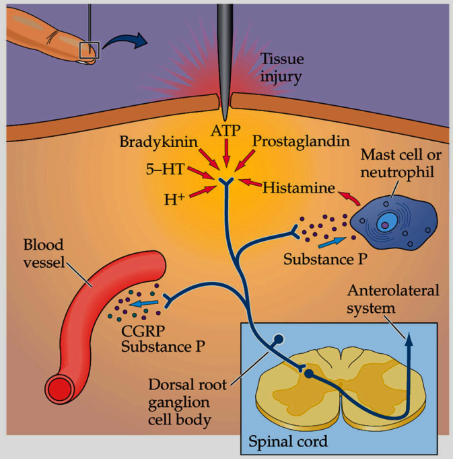
What are the two major central pathways of the somatosensory system? (2)

Dorsal column-medial lemniscal system (DCML).
Spinothalamic tract (STT) (anterolateral system).
What do the ascending pathways mediate regarding sensory aspects of pain? (3)

Sensory aspects of pain for the body and face.
2nd order neurons decussate and project to the ventral-posterior nuclear complex of the thalamus.
VPL: mediates pain for the body.
VPM: mediates pain for the face.THIS IS THE STT PATHWAY
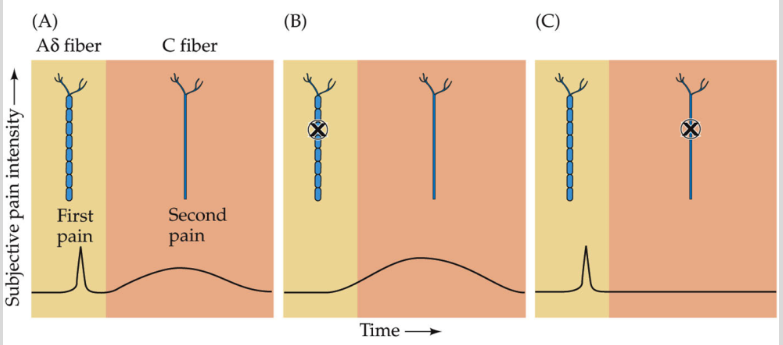
How do the DCML and STT pathways differ in crossing the midline? (1)
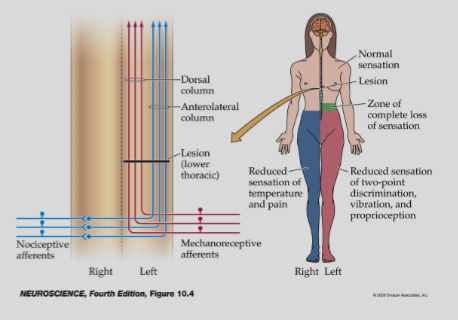
DCML and STT cross the midline at different sites, affecting the loss of sensory modalities.
What are the differences in sensory loss between the DCML and STT pathways? (2)
Temperature and pain are mediated by the STT.
Fine tactile discrimination is mediated by the DCML.
What is pain? (1)
Pain is a complex experience involving both sensory-discriminative and affective-motivational components.
What are the components of the dual-aspect model of pain? (2)
Sensory-discriminative:
Determines the location, intensity, duration, and quality of pain.
Affective-motivational:
Relates to the unpleasantness (painfulness of pain).
Influences arousal, mood (affect), and behaviour.
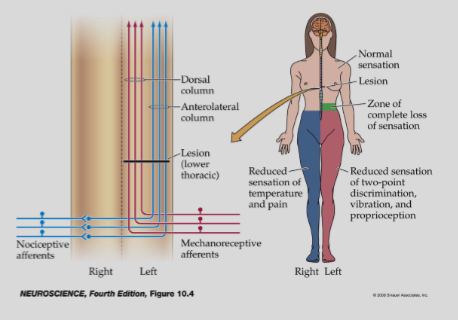
Picture demonstrating Nociceptors are neurons specializedfor detection of painful stimuli:
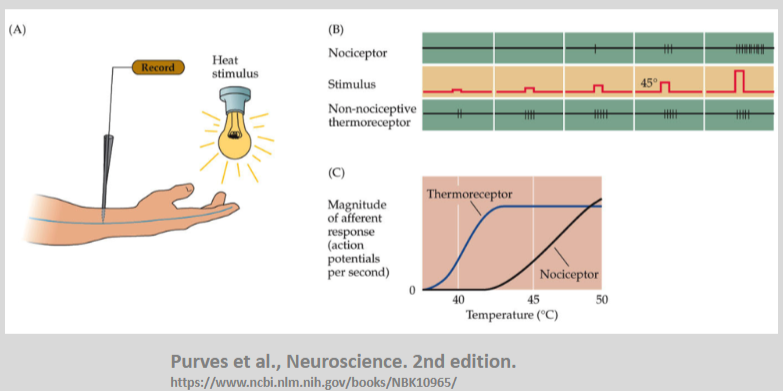
A-delta and C-fibres contribute different aspects of pain sensation:
What is the TRPV1 receptor, and what does it do? (2)
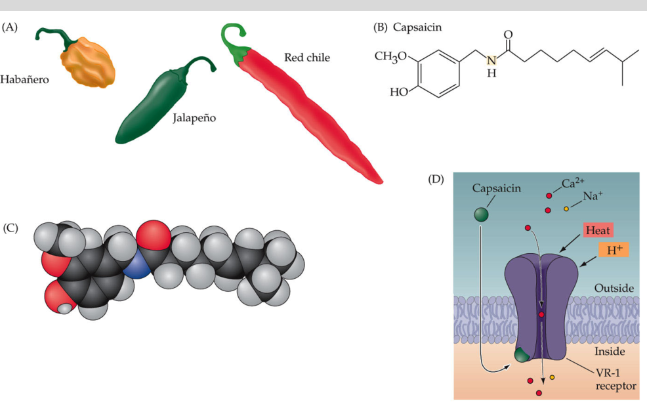
The TRPV1 receptor is involved in the transduction of noxious heat.
It was originally called the vanilloid receptor.
Where is the TRPV1 receptor found? (2)
It is present in A-δ fibres and C-fibres.
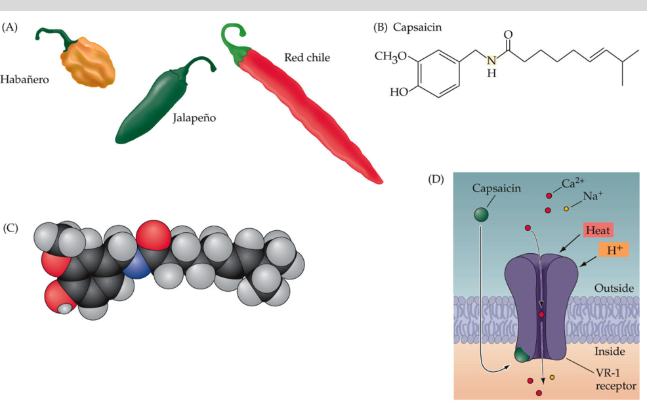
What maintains nociceptor activity after an injury? (2)

An ‘inflammatory soup’ of cytokines, prostaglandins, and small signaling molecules.
This maintains the depolarization and sensitivity of C-fibre terminals after the original stimulus.
What are the effects of maintaining nociceptor activity after an injury? (2)
Hyperalgesia: Increased sensitivity to painful stimuli.
Allodynia: Pain caused by stimuli that are not normally painful.
What are the characteristics of dorsal horn interneurons in the anterolateral system (STT)? (5)
Located in superficial and deep layers of the dorsal horn.
Receive synaptic input from C-fibres and A-δ fibres.
Axons cross and ascend in the anterolateral white matter.
Some interneurons are multi-modal, receiving both nociceptive and non-nociceptive inputs.
Some interneurons receive convergent input from visceral afferents.
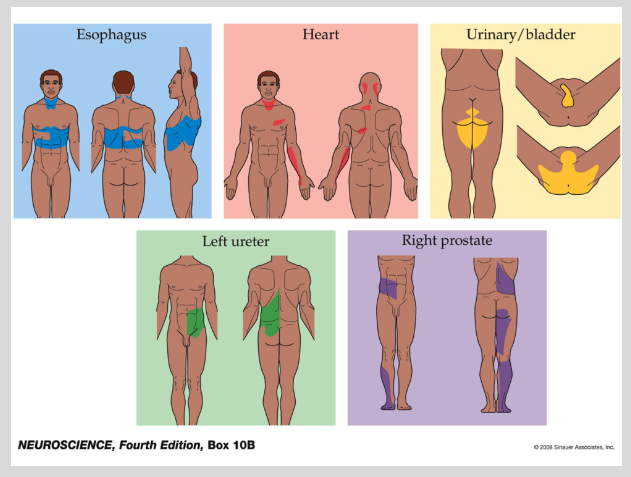
Picture demonstrating Referred pain:
What are the characteristics of cortical representation of pain? (4)
STT projects to S1 via VP nuclei of thalamus (like DCML system).
STT and DCML axons do not converge on the same thalamic neurons – pathways are parallel.
S1 is necessary for the localization of pain but stimulation of S1 gives rise to referred tactile sensations, not pain.
Additional areas are involved in pain sensations.
What are the two systems in central pain processing? (4)
Lateral system
VP nuclei of thalamus, in parallel with the DCML system.
Includes primary and secondary somatosensory cortex (SI and SII).
Medial system
Midline nuclei of thalamus (intralaminar).
Includes anterior cingulate cortex and insular cortex.
What are the characteristics of the lateral and medial pain systems? (4)
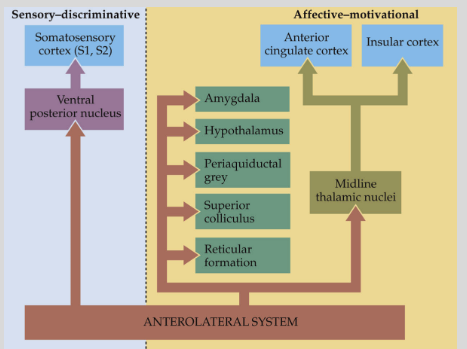
Mnemonic: "Lateral Loves Specifics, Medial Moves Emotions"
Lateral = Loves Specifics:
Sensory-discriminative (location, intensity, duration).
Projects via specific somatosensory thalamic nuclei (e.g., ventral posterior nuclei).
Medial = Moves Emotions:
Affective-motivational (emotions, unpleasantness of pain).
Projects to different cortical areas via non-specific midline thalamic nuclei (e.g., intralaminar nuclei).
What is descending modulation of pain and how does it involve endogenous opioids? (4)
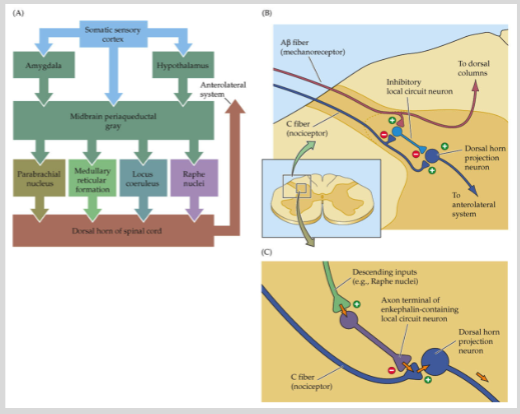
Descending modulation of pain is when the brain reduces pain through inhibitory pathways.
Opium’s analgesic properties have been known for centuries.
In the 1970s-80s, endogenous opioids like enkephalins and endorphins were discovered.
These opioids bind to opioid receptors to reduce pain perception.
What is the difference between acute and chronic pain? (7)
Acute pain:
Nociceptive response to tissue damage.
Mechanisms are fairly well understood.
Resolves as healing occurs.
Treatment is relatively successful.
Chronic pain:
Persists beyond tissue damage or may be caused by CNS damage.
Mechanisms are poorly understood.
Treatment is often ineffective.
What are the treatments for acute and chronic pain? (3)
Acute pain:
NSAIDs and opiate drugs are commonly used to manage pain as a neurophysiological response to tissue damage.
Chronic pain:
Antidepressants (e.g., amitriptyline, duloxetine) used at lower dosages and without clinical depression diagnosis.
Experimental treatments include neurosurgery and deep brain stimulation, though these are rare and anecdotal.
What is chronic pain, and how is it defined? (4)
Chronic pain lasts for more than 3 months.
It has a high prevalence and may be caused by nerve damage (neuropathic pain) or in the absence of nerve damage (e.g., stroke).
It can result from neuroplasticity, leading to sensitization in the dorsal horn interneurons or higher up in the pain pathway.
Chronic pain may involve cortical reorganization.
How does Loeser (2022) distinguish between chronic and acute pain? (2)
Nociceptor-driven pain: Associated with acute pain, driven by direct tissue damage.
Centrally maintained pain: A characteristic of chronic pain, where pain is maintained by changes in central nervous system pathways.
What are examples of pain dissociated from tissue damage? (2)
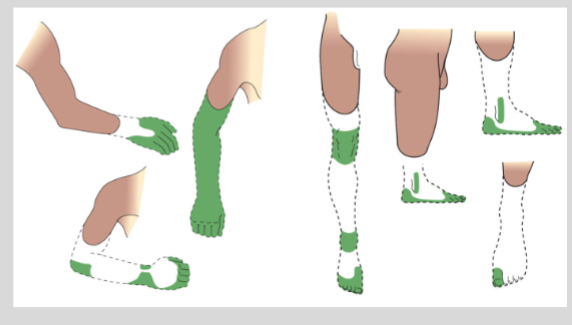
Phantom limb pain: Pain experienced in a limb that has been amputated, despite no actual tissue damage.
Central pain: Pain resulting from damage to the central nervous system (CNS), even without peripheral tissue damage.
What are the differences between the lateral and medial pain systems? (4)
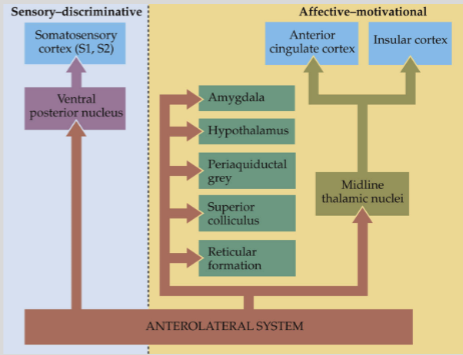
Lateral pain system:
Involved in the sensory-discriminative aspect of pain.
Projects through specific somatosensory thalamic nuclei to the sensory cortex.
Medial pain system:
Involved in the affective-motivational aspect of pain.
Projects to different cortical areas via non-specific midline thalamic nuclei.
What does the dissociation of the lateral and medial pain systems refer to? (2)
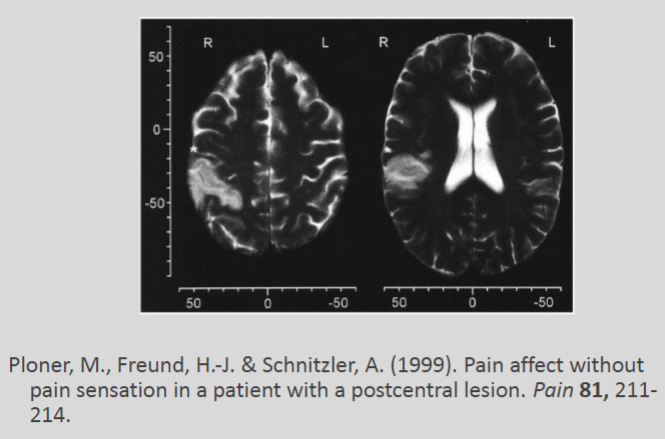
The lateral pain system is responsible for the sensory-discriminative aspect, allowing the brain to recognize the location, intensity, and type of pain.
The medial pain system is responsible for the affective-motivational aspect, influencing the emotional response and motivation related to pain.
What is anterior cingulotomy and how is it used in the treatment of intractable pain? (3)
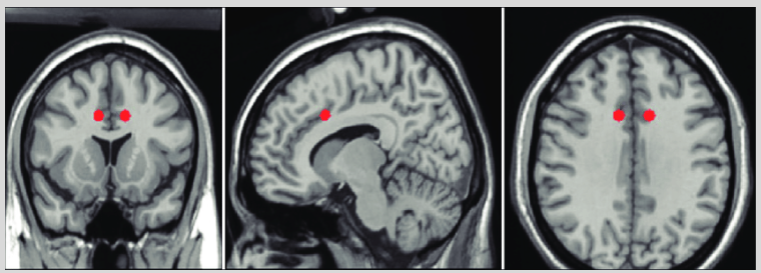
Anterior cingulotomy involves creating a targeted lesion to disconnect the anterior cingulate cortex on both sides of the brain.
This procedure has been used for decades as a last resort treatment for patients with intractable pain.
It is typically considered when other treatments fail to manage severe, chronic pain.