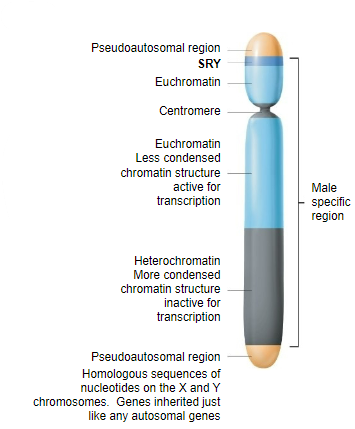
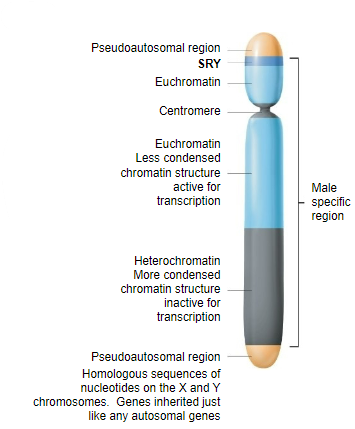
What is sexual determination? (1)
A genetically controlled process dependent on the 'switch' on the Y chromosome, leading to the chromosomal determination of male or female.
What is sexual differentiation? (1)
The process by which internal and external genitalia develop as male or female.
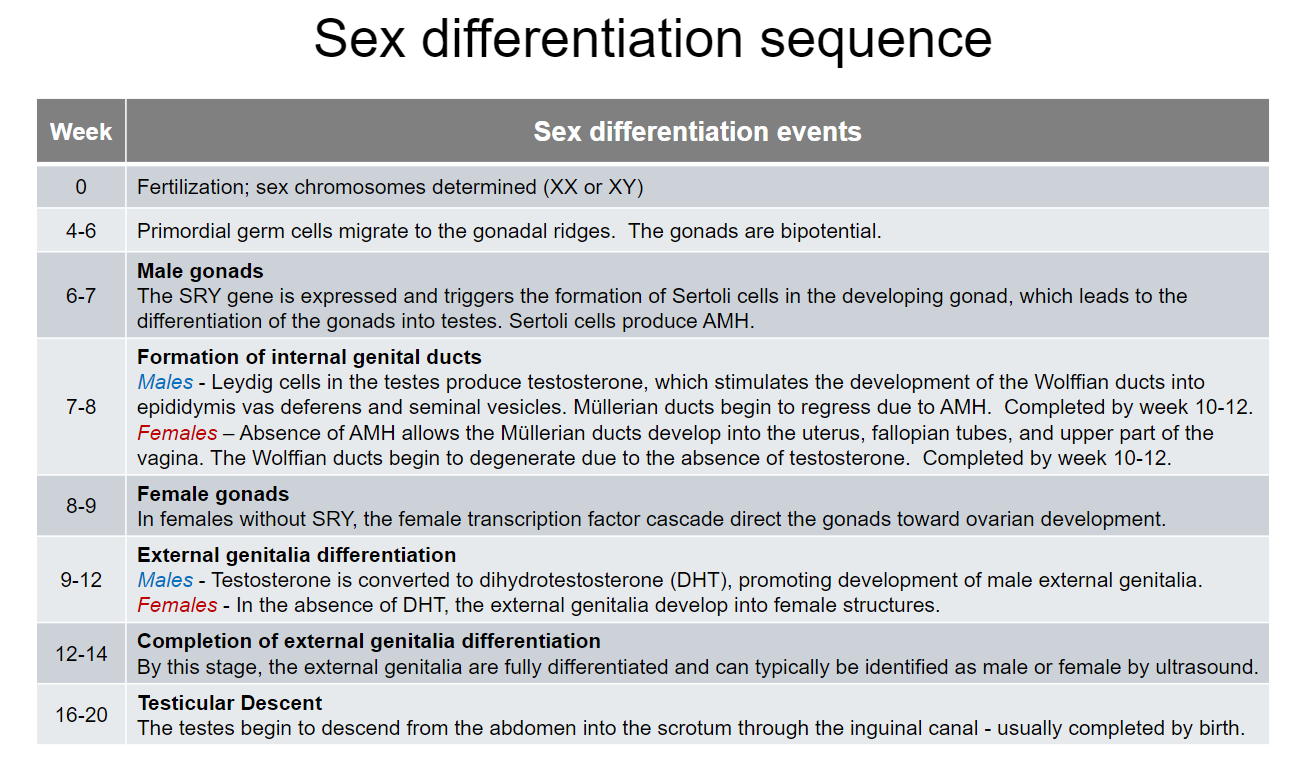
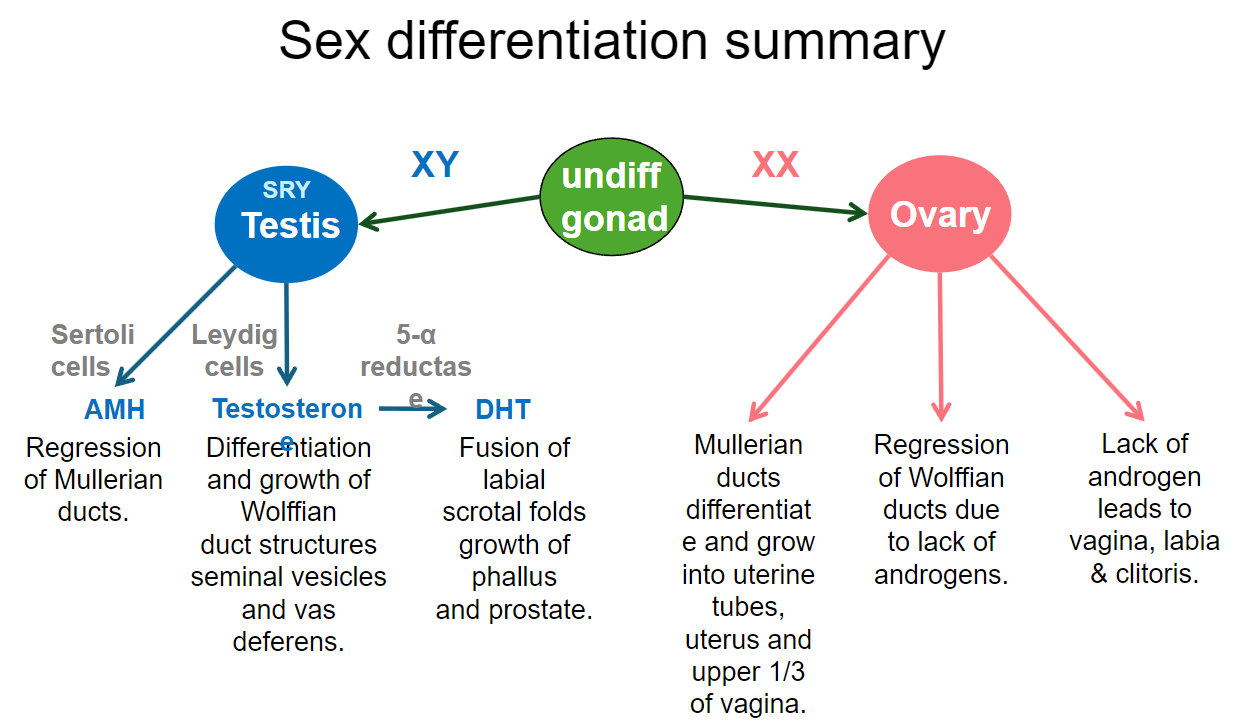
What is the overall sequence of sexual differentiation? (3)
Create gonads according to sex chromosomes.
Products of developing gonads affect differentiation of internal reproductive organs.
Differentiation of external genitalia.
What is gonadal sex? (1)
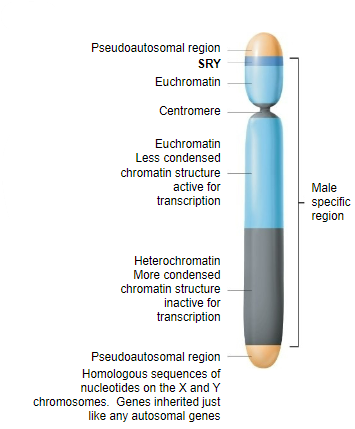
Gonadal sex is determined by the SRY gene, which creates the testis.
What is the role of the SRY gene? (2)
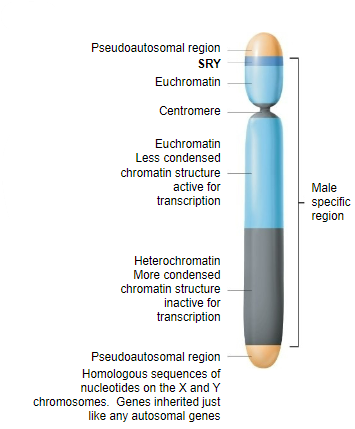
The SRY (Sex-determining Region Y) gene switches on briefly during embryo development (>week 7) to make the gonad into a testis.
In its absence, an ovary is formed.
What hormones are produced by the testis? (2)
Anti-Mullerian hormone (AMH)
Testosterone
What is the role of the products of the testis? (1)
They influence further gonadal and phenotypic sexual development.
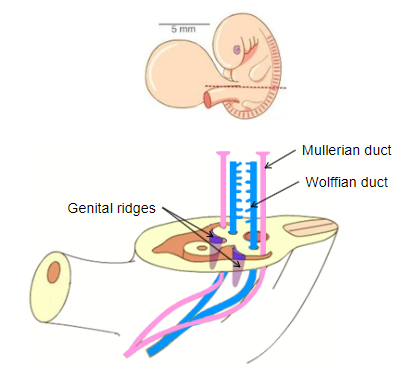
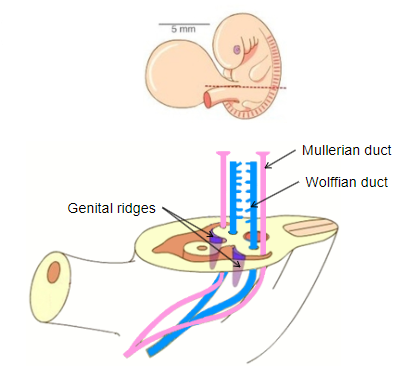
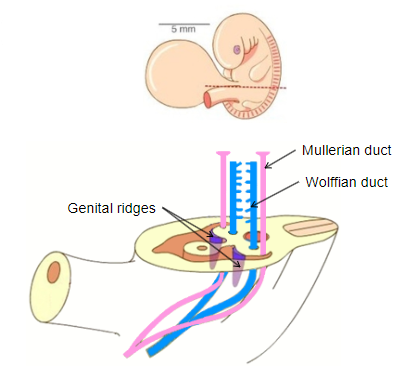
How do gonads begin developing after fertilization? (3)
As Genital ridges, which form as thickened areas of tissue near the developing kidneys in the embryo.
They are initially bipotential, meaning they have the capacity to develop into either testes or ovaries.
The presence or absence of the SRY gene on the Y chromosome determines whether they differentiate into testes (male) or ovaries (female).
What are the 3 waves of cells that invade the genital ridges? (3)
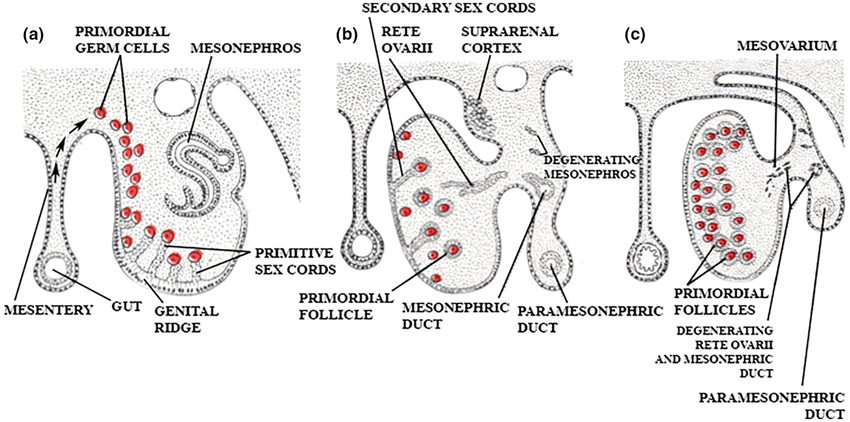
Primordial Germ Cells
Primitive Sex Cords
Mesonephric Cells (Derived from the mesonephros)
What do the invading cells in the genital ridges differentiate into? (1)
The 3 main cell types present in the ovary and the testis. (oocytes, sertoli cells and leydig cells)
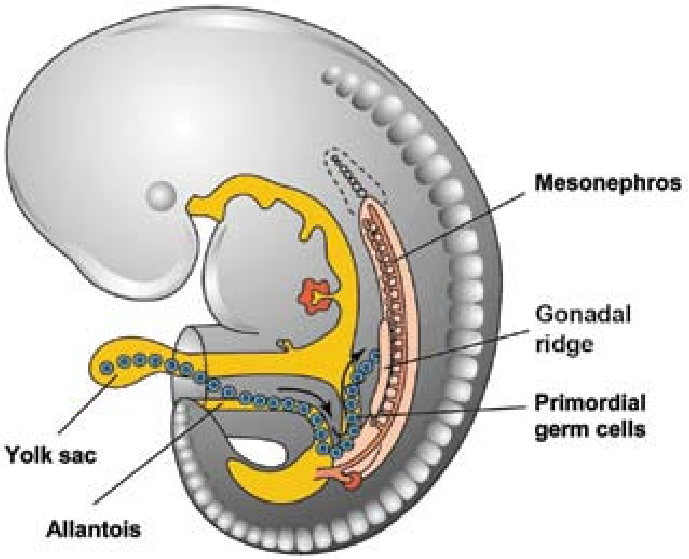
Where do primordial germ cells originate and expand? (1)
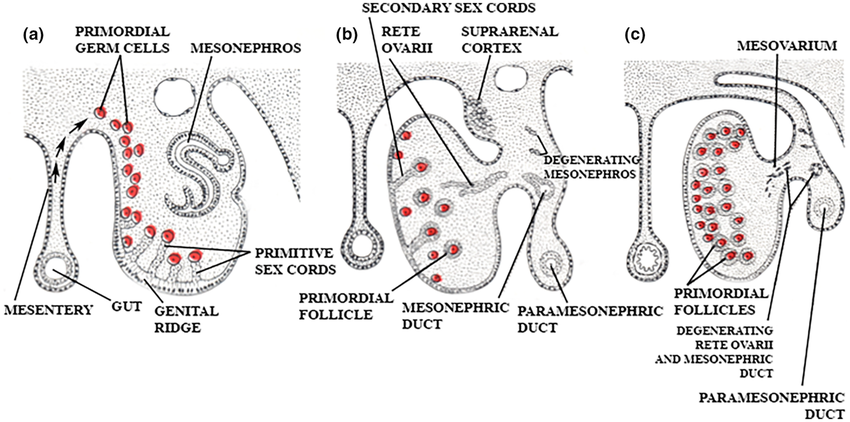
They originate in the epithelium of the yolk sac and expand by mitosis around 3 weeks of development.
Where do primordial germ cells migrate to, and by when is migration completed? (2)
They migrate to the region of the developing kidney (mesonephros) and on to the genital ridge, with migration completed by 6 weeks.
What can primordial germ cells differentiate into? (2)
They can differentiate into precursors of sperm or oocytes, depending on the type of gonad that develops.
What are primitive sex cords, and where do they originate? (1)
Primitive sex cords originate from the germinal epithelium, which is the surface layer of cells that forms the initial gonadal structures. These cells migrate inward into the genital ridge mesenchyme (the underlying mesoderm), where they form the primitive sex cords, the precursor to the gonads.
What happens to the primitive sex cords when no SRY is present? (2)
Regression of Primitive Sex Cords:
In the absence of SRY, the primitive sex cords do not develop into the seminiferous tubules of the testes. Instead, they degenerate and regress.
Formation of Ovarian Follicles:
Without SRY signaling, the gonads develop into ovaries. The regressed sex cords are replaced by cortical cords in the ovarian tissue, which will eventually differentiate into ovarian follicles, where oocytes (eggs) will develop.
What do the primitive sex cords become in females, and what is their function? (1)
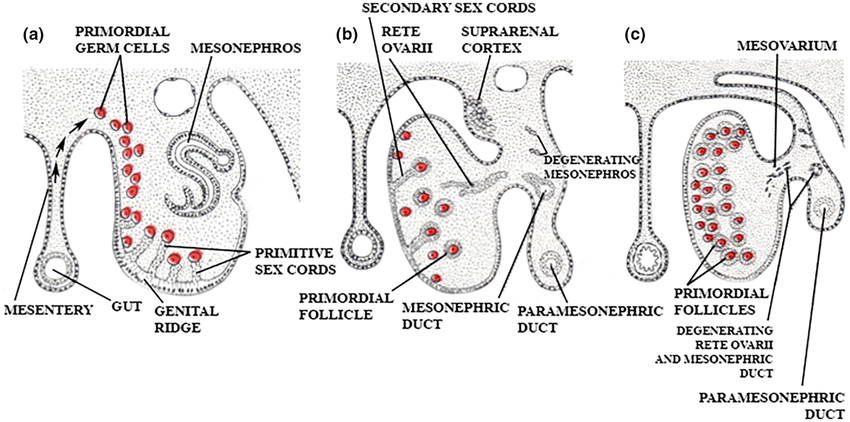
They become granulosa cells, which do not express AMH.
What happens to the primitive sex cords when SRY is expressed? (2)
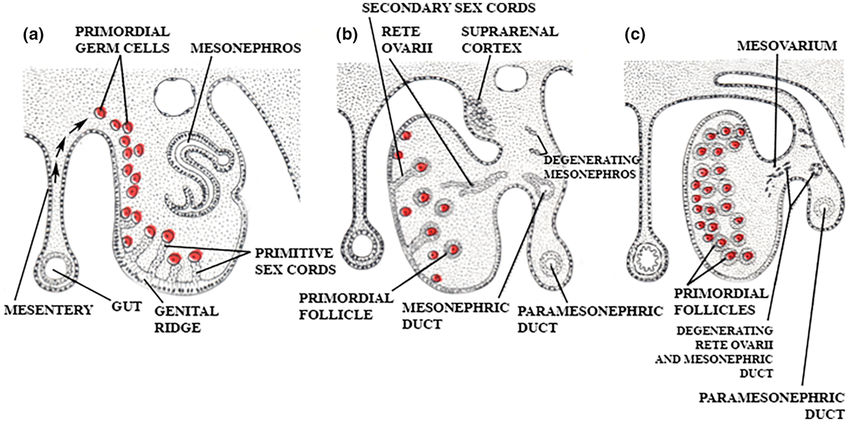
The sex cords penetrate and surround the primordial germ cells to form testis cords.
They become Sertoli cells, which express AMH.
What do the primitive sex cords become in males, and what is their function? (1)
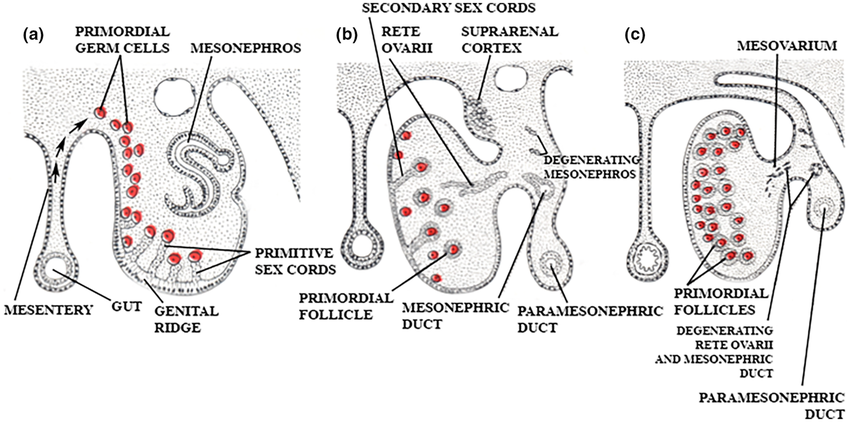
They become Sertoli cells, which express AMH (Anti-Mullerian Hormone).
Where do mesonephric cells originate? (1)
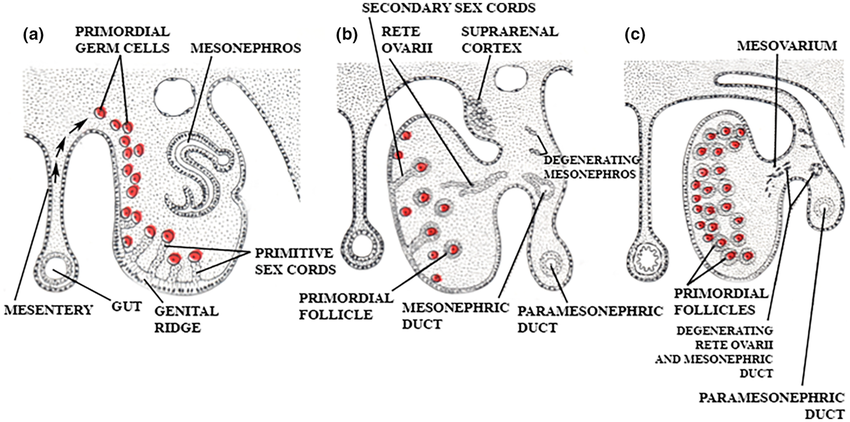
Mesonephric cells originate in the mesonephric primordium, which is located just lateral to the genital ridges.
What do mesonephric cells contribute to in gonadal development? (2)
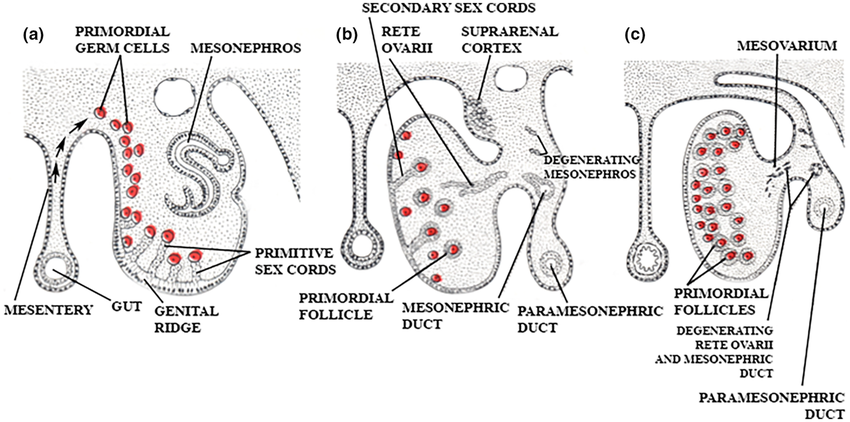
They contribute to vascular tissue and some basement membrane of the developing gonads.
What do mesonephric cells develop into in females, and what is their function? (2)
They develop into theca cells, which do not synthesize androgens until after puberty.
What do mesonephric cells develop into in males, and what influences their development? (2)
They develop into Leydig cells under the influence of Sertoli cells.
Leydig cells synthesize testosterone.
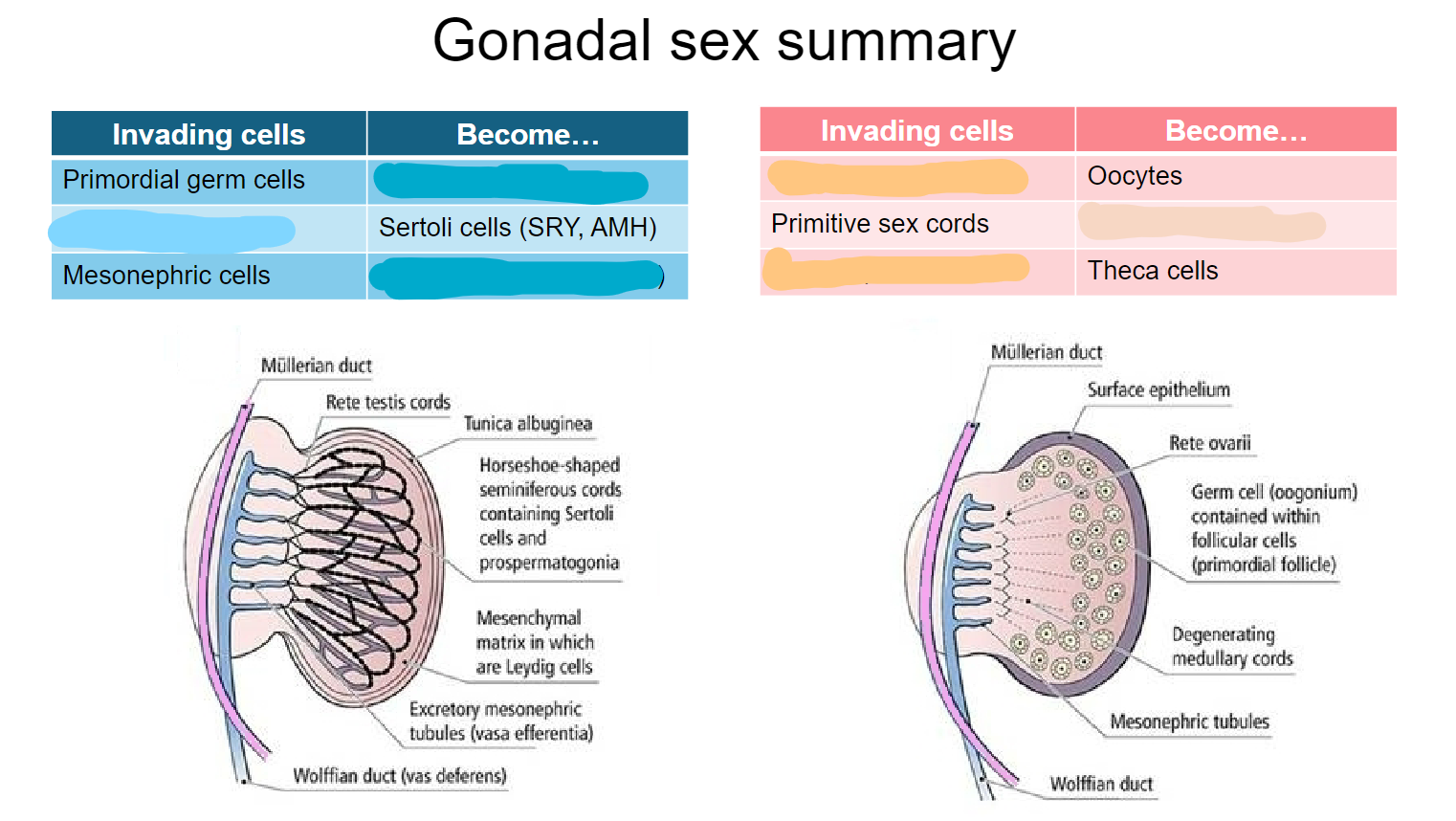
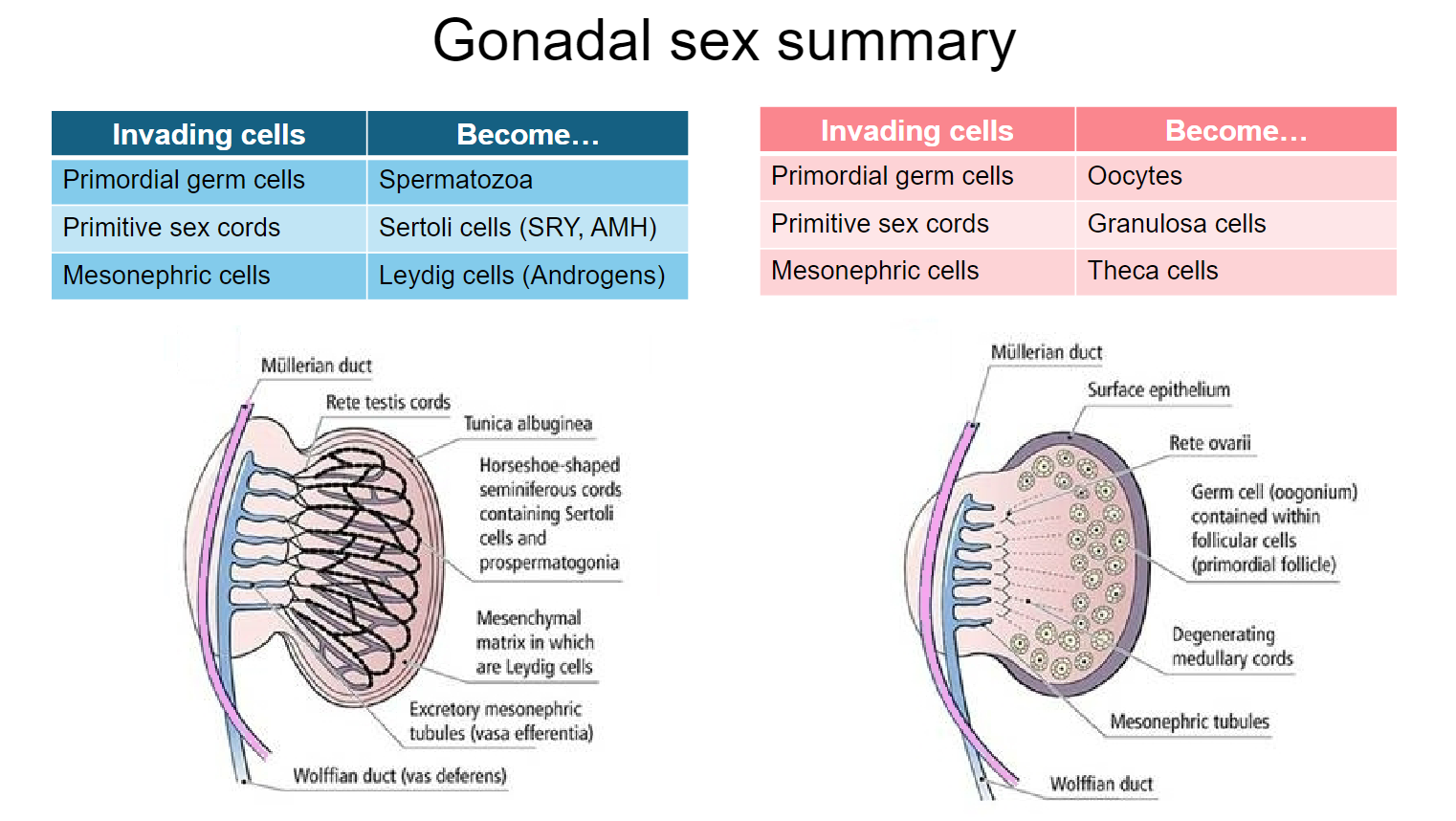
Fill out this table (6)
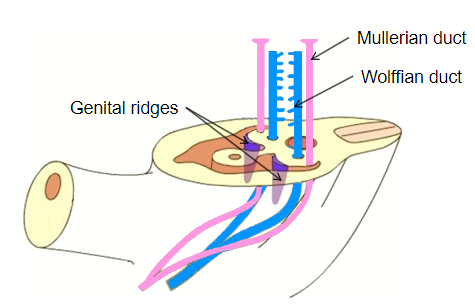
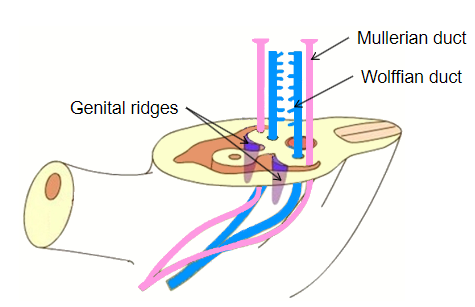
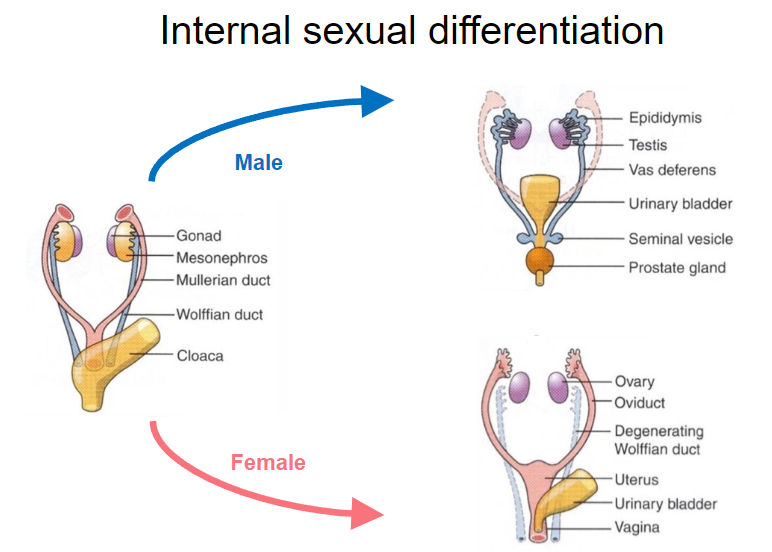
What do the Müllerian ducts develop into in females? (3)
Uterus
Uterine tubes
Upper 1/3rd of the vagina
What inhibits the development of the Müllerian ducts in males? (1)
Anti-Mullerian hormone (AMH) from Sertoli cells.
What do the Wolffian ducts develop into in males? (4)
Vas deferens
Epididymis
Seminal vesicles
Ejaculatory ducts
What stimulates the development of the Wolffian ducts in males? (1)
Testosterone from Leydig cells.
What happens to the Wolffian ducts in females without testosterone stimulation? (1)
They regress.
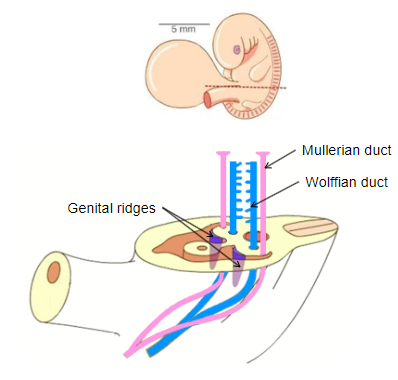
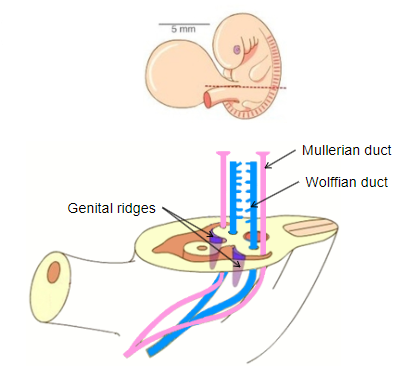
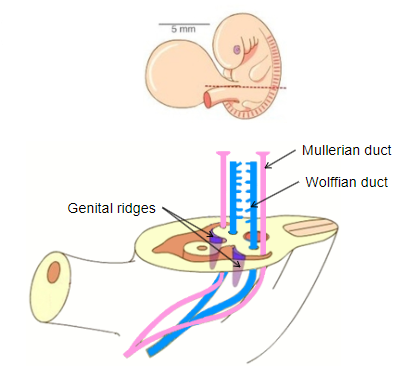
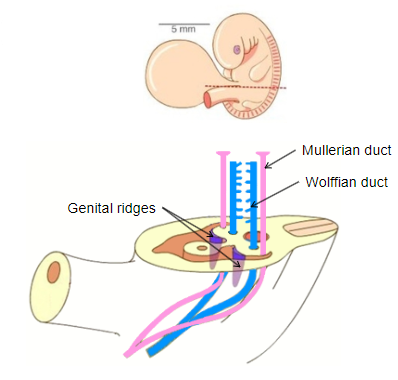
Picture demonstrating internal sexual differentiation:
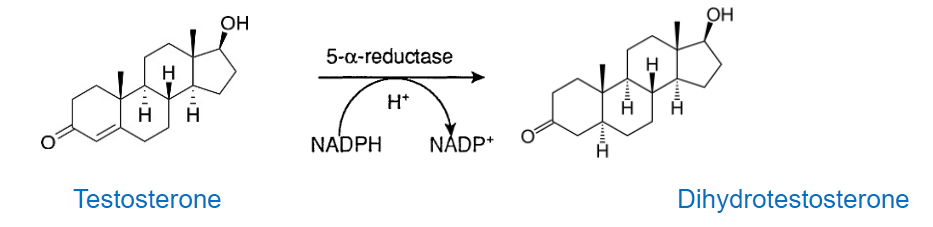
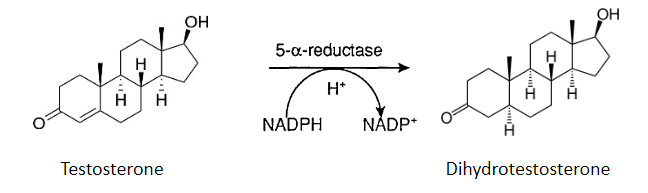
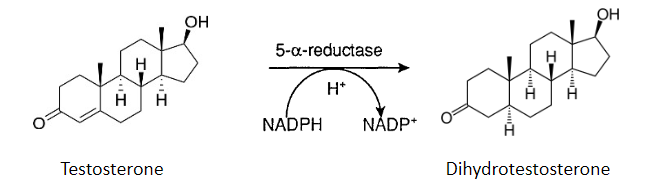
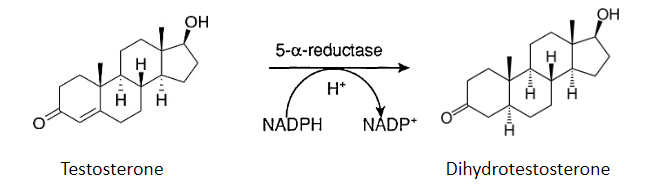
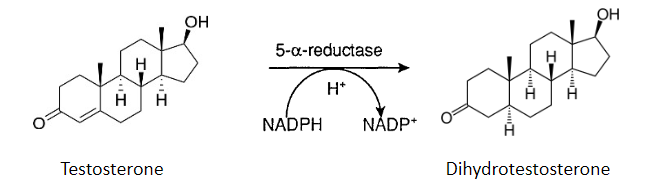
What is the role of 5-α-reductase in external differentiation? (1)
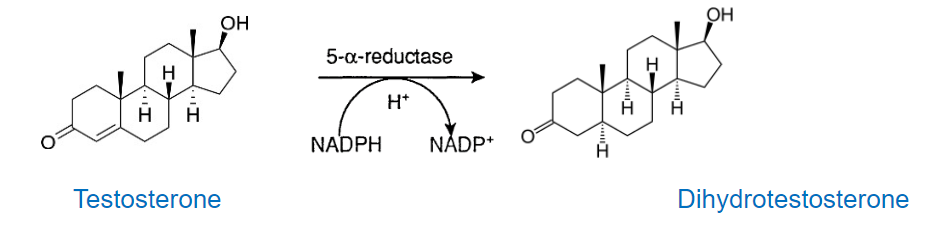
5-α-reductase converts testosterone in the genital skin to the more potent androgen, DHT (dihydrotestosterone).
How does DHT compare to testosterone? (1)
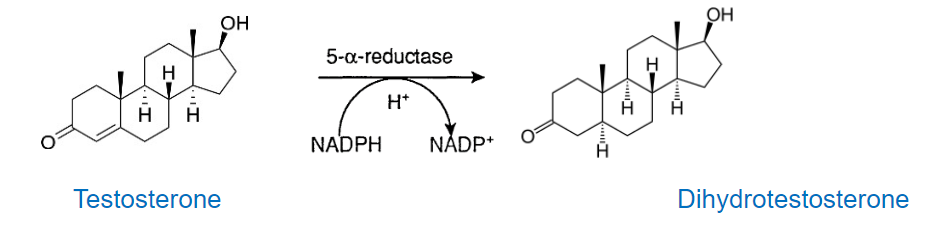
DHT binds to the testosterone receptor but is more potent than testosterone.
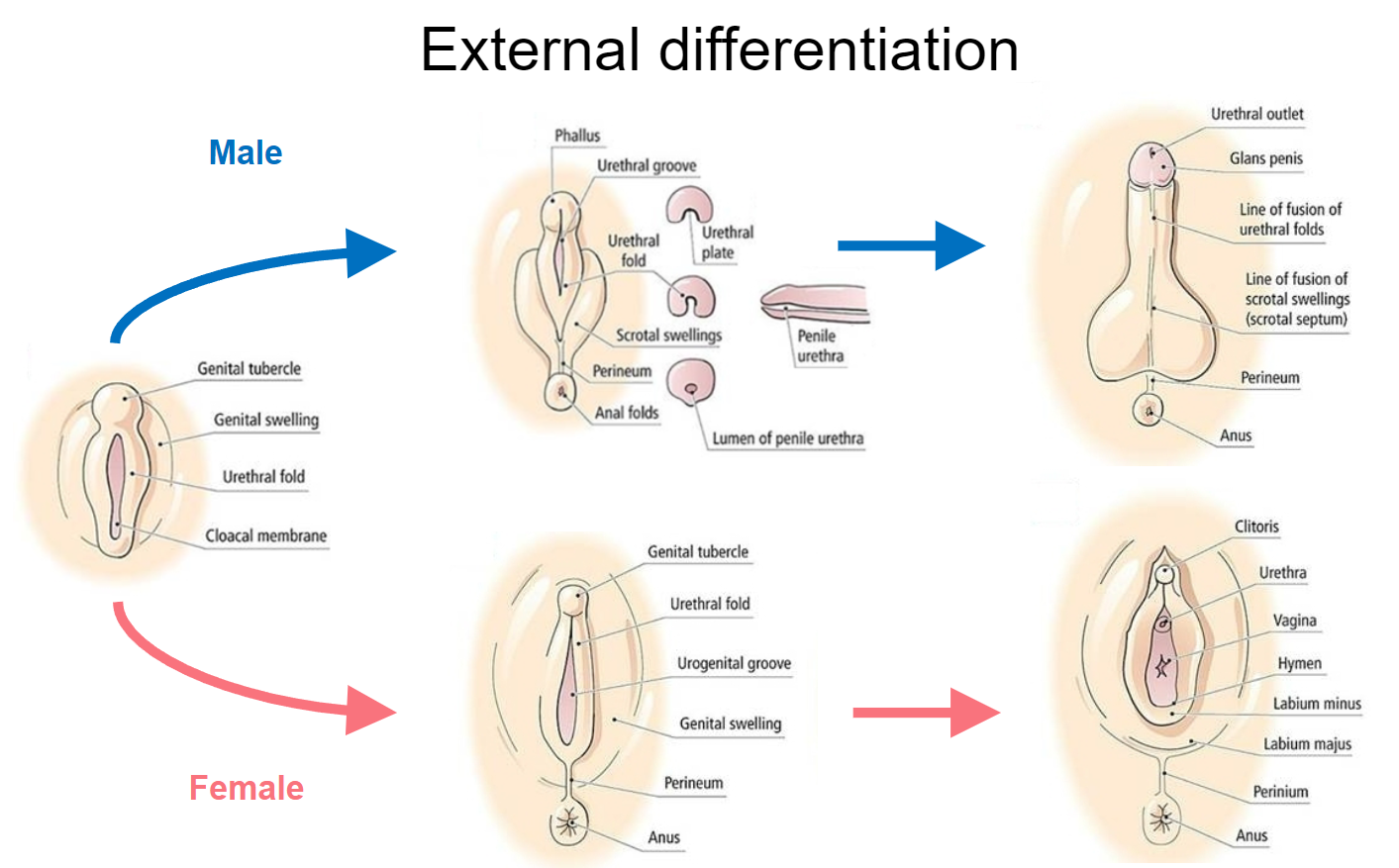
What is the role of DHT in male external genitalia differentiation? (3)
The clitoral area enlarges into the penis.
The labia fuse and become ruggated to form the scrotum.
The prostate forms.
Picture demonstrating external differentiation:
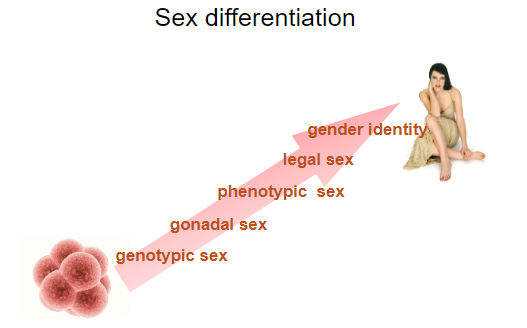
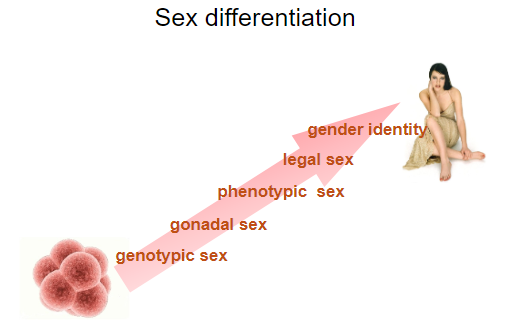
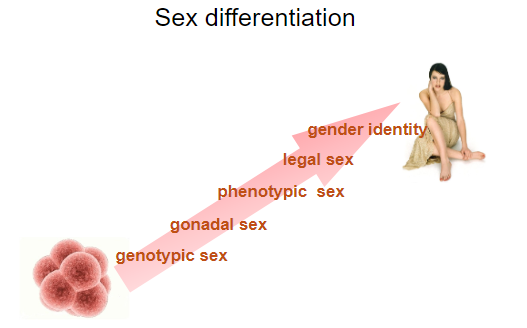
Picture demonstration the sex differentiation summary:
What is gonadal dysgenesis, and what are common causes? (2)
Gonadal dysgenesis is when sexual differentiation is incomplete.
It is usually caused by a missing SRY gene in males or a partial/complete deletion of the second X chromosome in females.
What is sex reversal? (1)
Sex reversal occurs when the phenotype does not match the genotype, such as a genotypically male individual externally appearing female.
What is intersex? (2)
Intersex individuals have some components of both reproductive tracts or have ambiguous genitalia.
The sex of the infant may be difficult to determine.
What term is preferred by patients with ambiguous genitalia? (1)
Patients prefer to be referred to as someone with a "disorder of sexual differentiation" (DSD).
What terms are now considered obsolete? (2)
Pseudohermaphrodite
Testicular feminisation
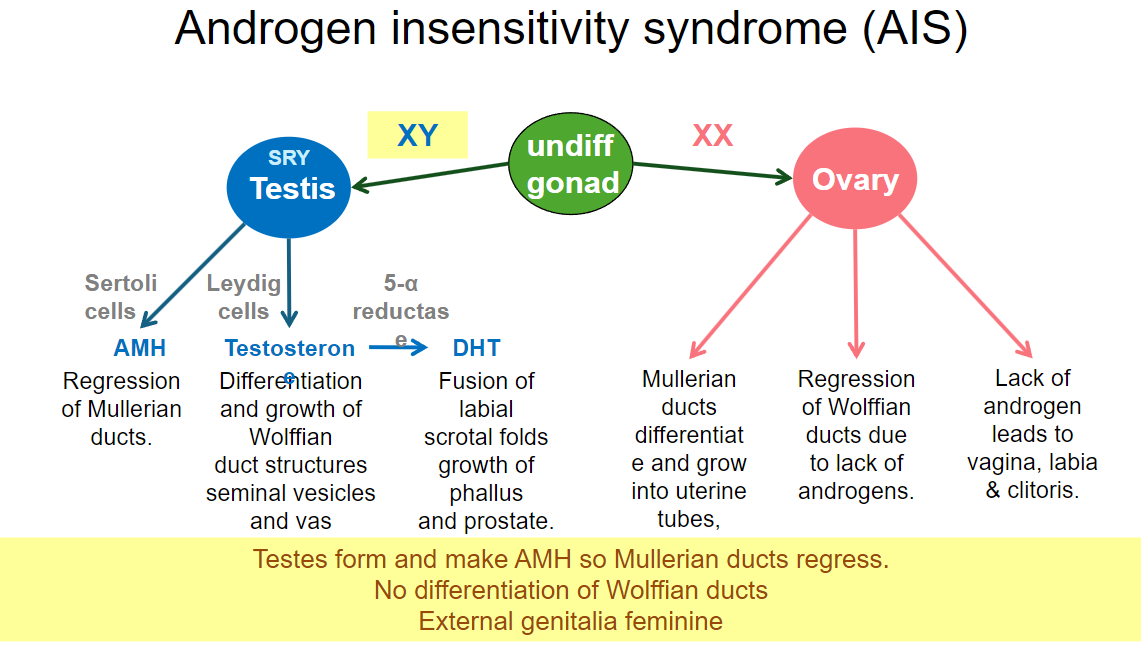
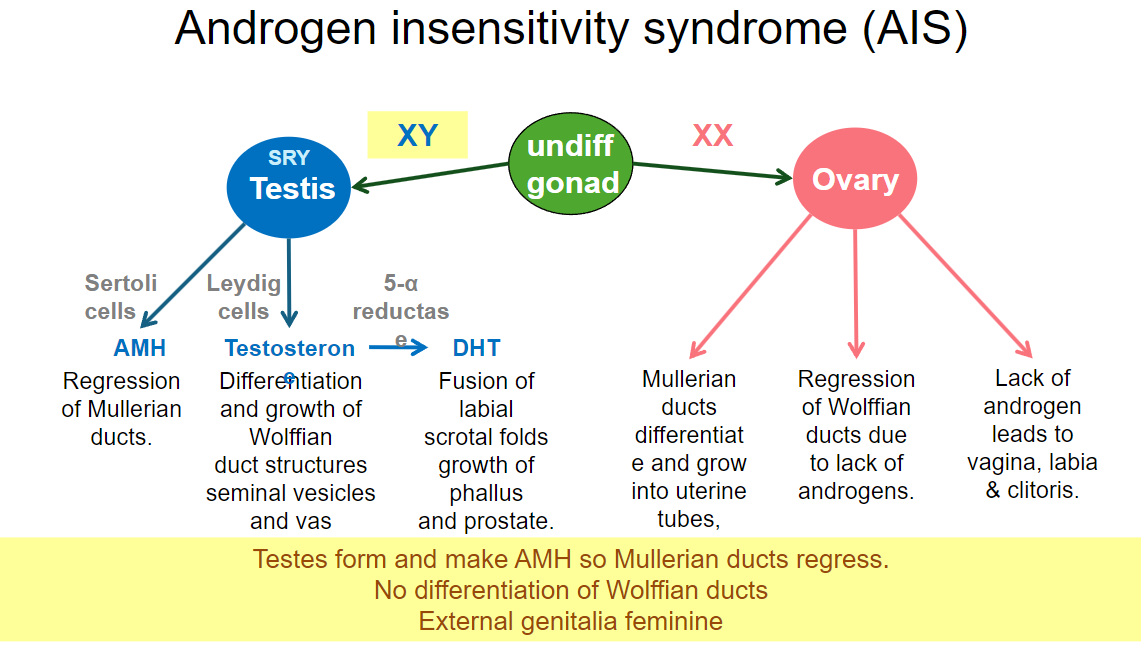
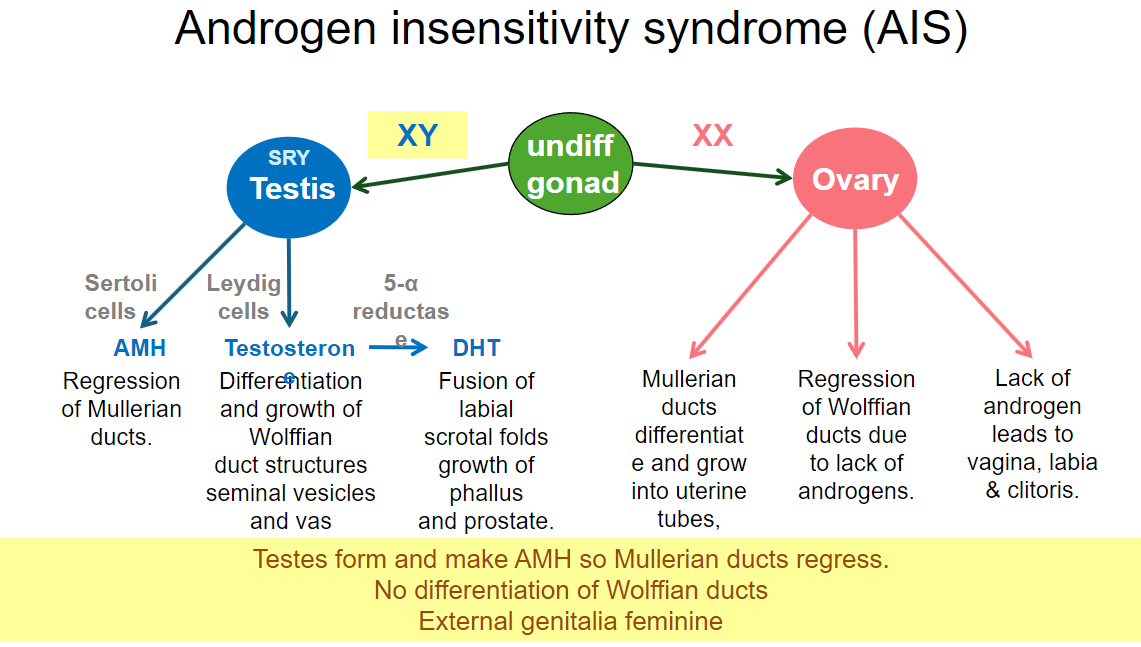
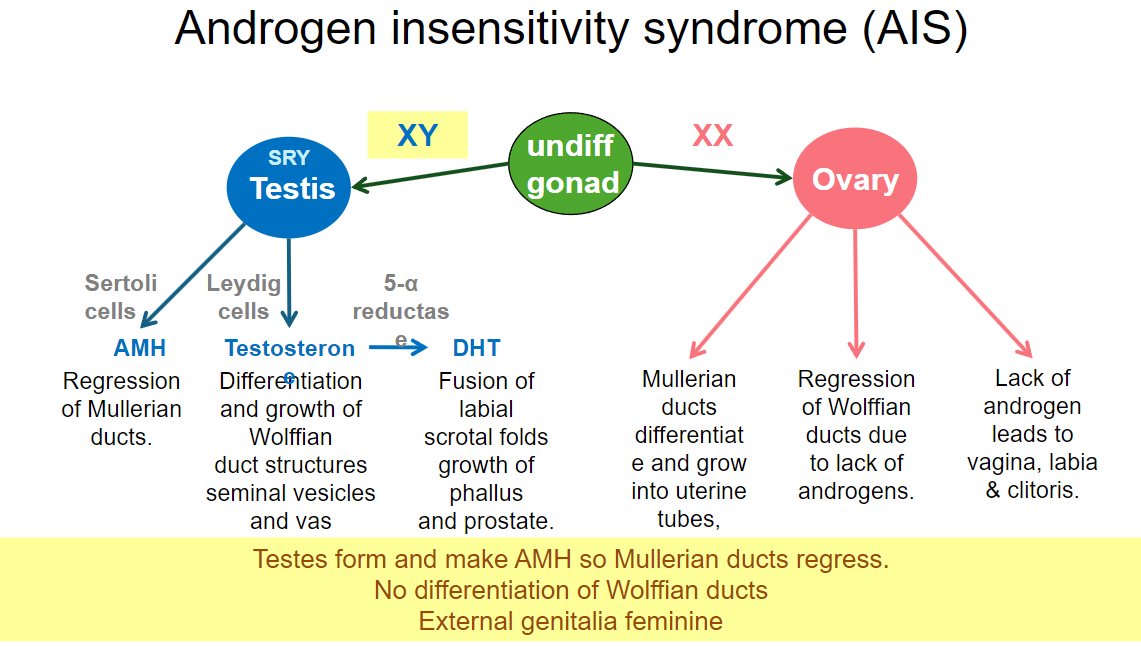
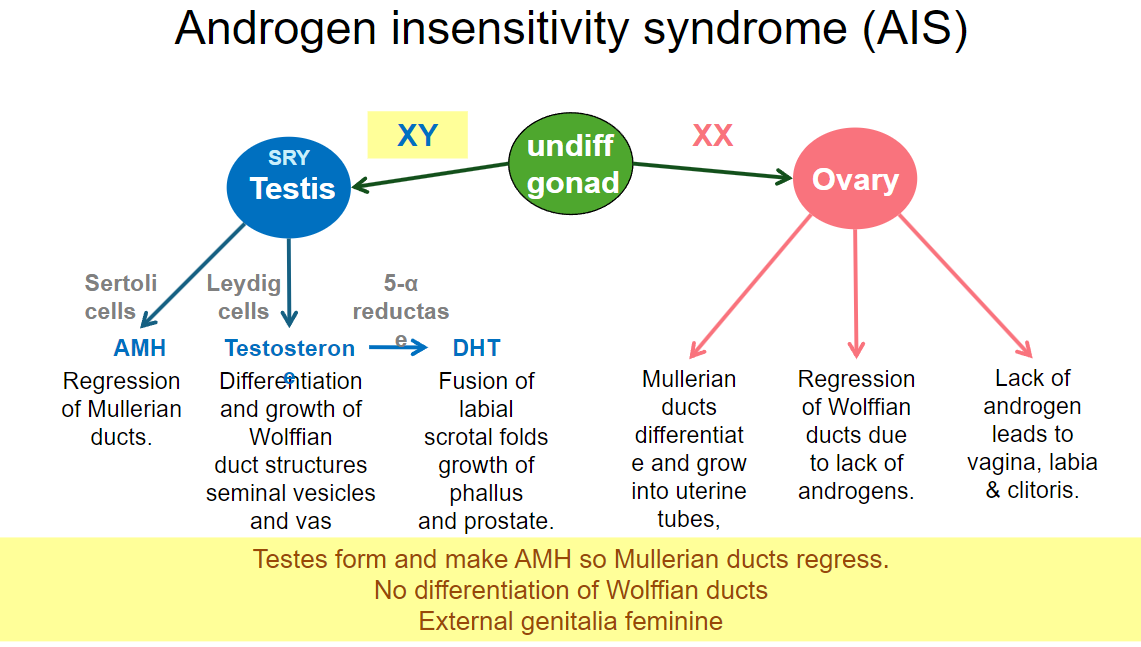
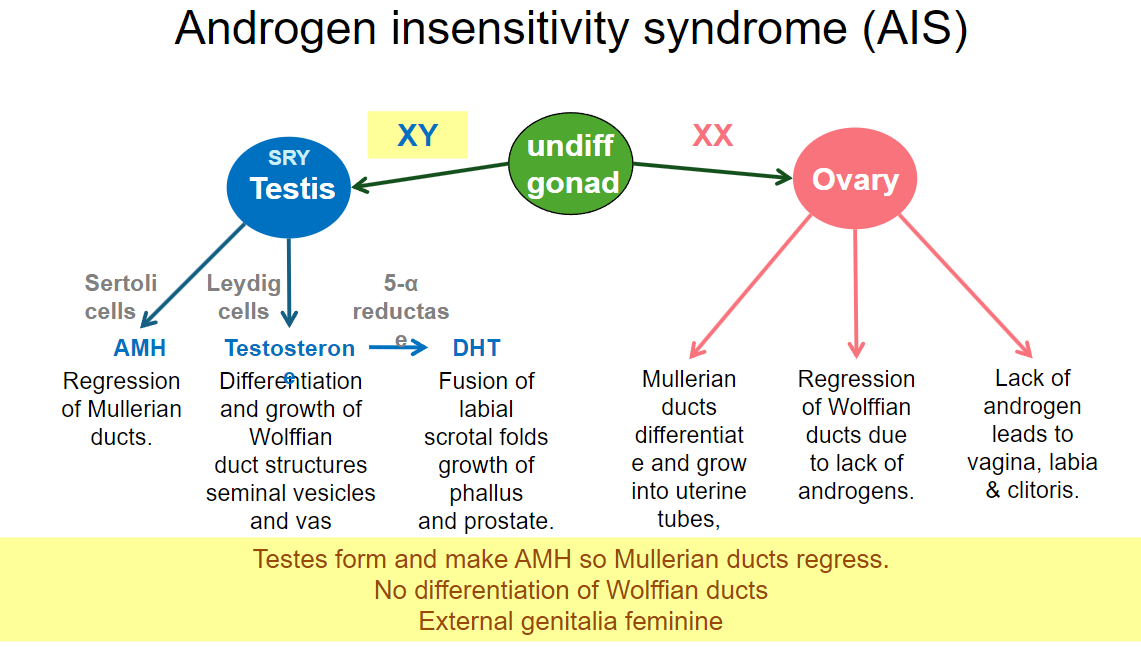
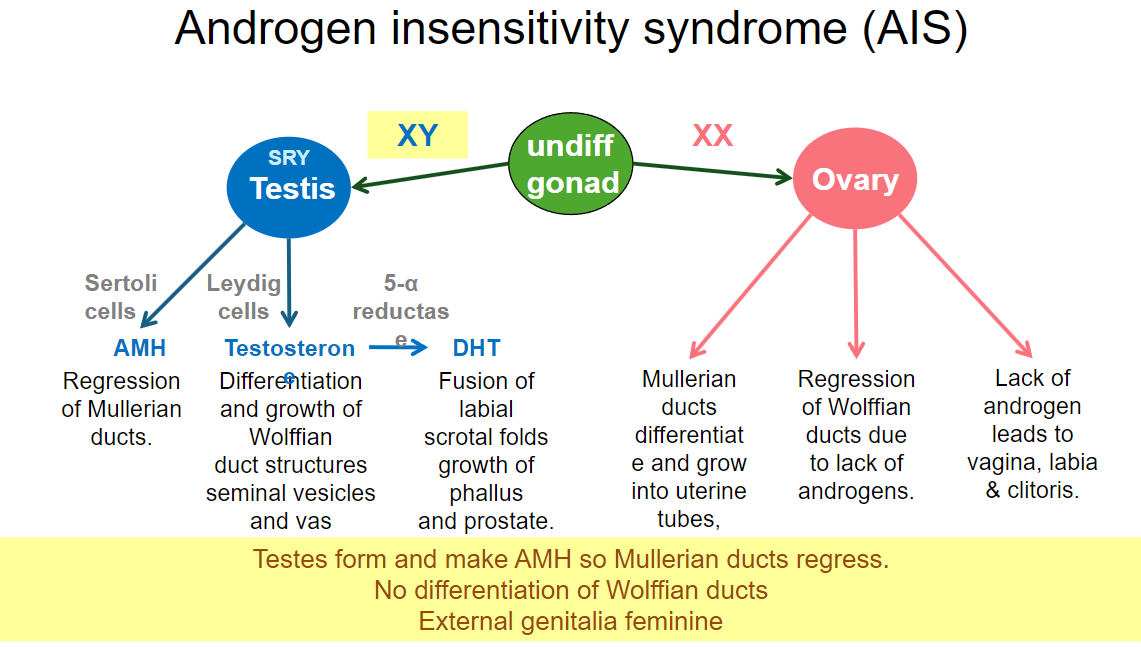
What happens to testosterone in individuals (males XY) with androgen insensitivity syndrome (AIS)? (1)
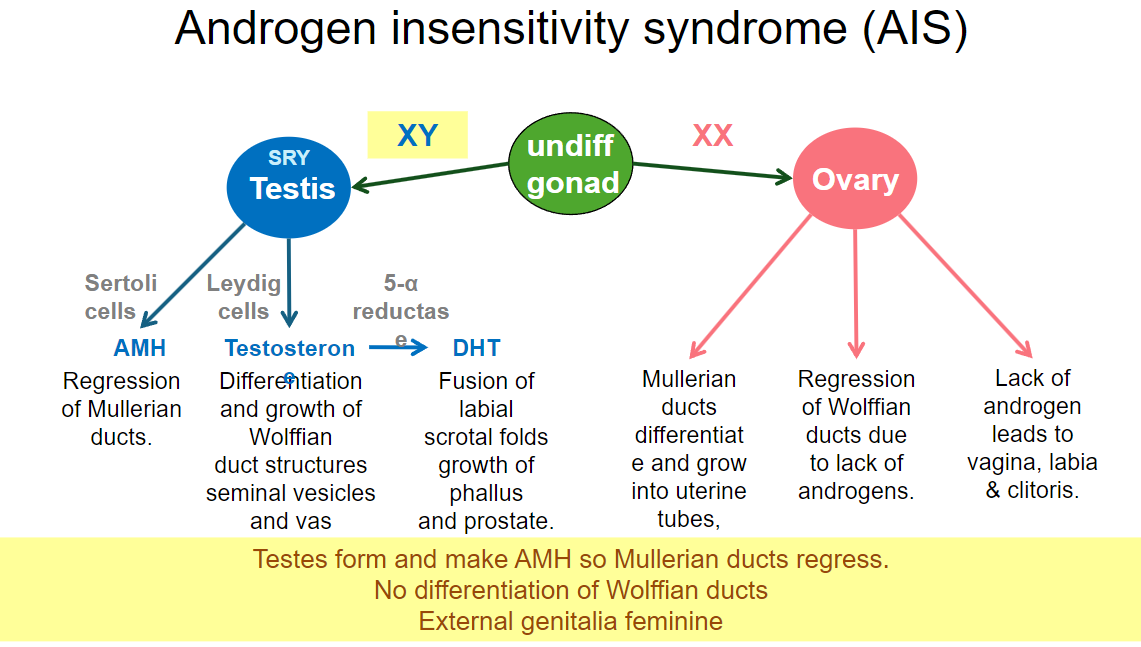
In AIS, testosterone is produced but has no effect due to the body's inability to respond to androgens.
What is the phenotype of an XY individual with AIS? (2)
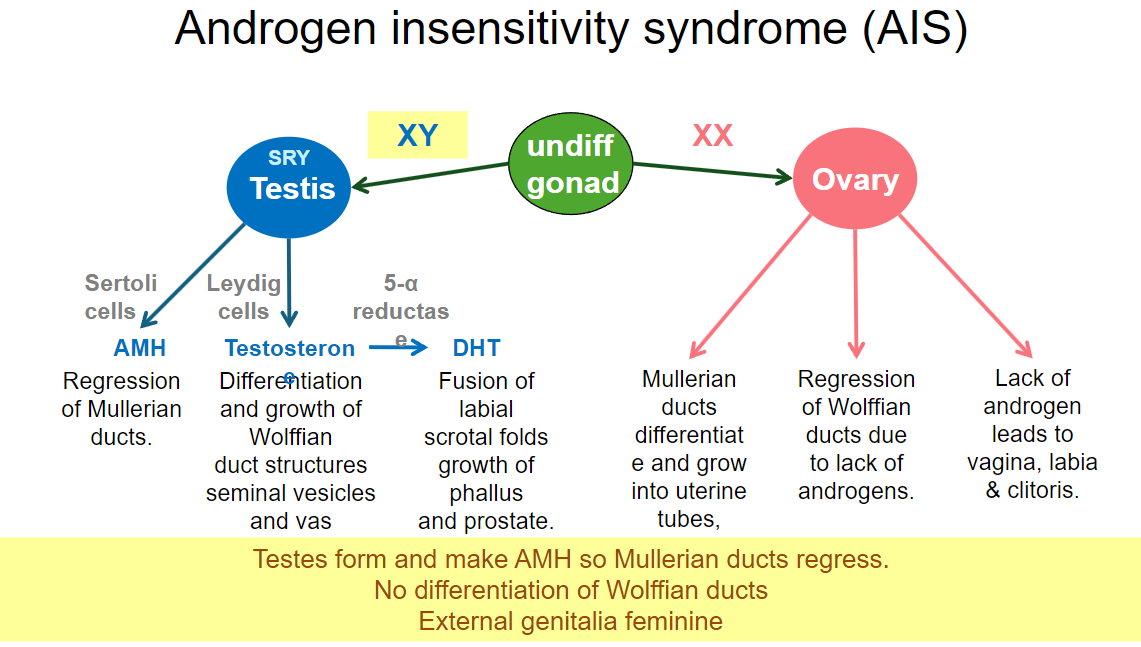
The individual develops female external genitalia.
They may have a female phenotype despite having XY chromosomes.
What happens to the internal reproductive structures in individuals with AIS? (2)
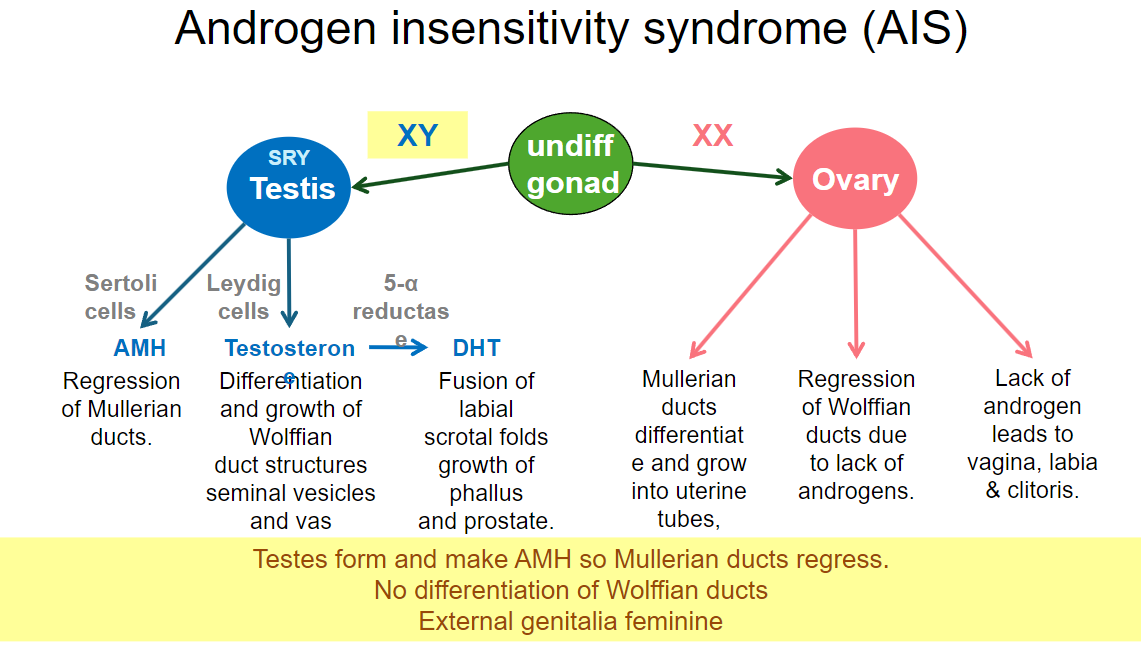
Müllerian ducts regress due to the presence of AMH from Sertoli cells, preventing the development of female reproductive organs.
Wolffian ducts do not develop properly due to lack of androgen receptor activity, preventing the formation of male internal reproductive structures.
What is the incidence of Complete Androgen Insensitivity Syndrome (CAIS)? (1)
The incidence of CAIS is approximately 1 in 20,000 births.
What are the physical characteristics of an individual with Complete AIS at birth? (2)
They appear completely female at birth.
They are assigned female gender despite having XY chromosomes.
What anatomical feature is present in individuals with Complete AIS? (1)
Individuals have undescended testes.
What is the incidence of Partial Androgen Insensitivity Syndrome (PAIS)? (1)
The incidence of PAIS is unknown, as it is likely a spectrum.
What are the varying degrees of presentation in Partial AIS? (2)
Development can range from ambiguous genitalia to a large clitoris.
There may be varying degrees of penile and scrotal development.
What was the historical approach to surgery for AIS, and what is the current perspective? (2)
Surgery was once universal for individuals with AIS.
It is now considered optional or best delayed, with decisions made based on potential, which is difficult for parents.
What are common diagnostic indicators for AIS? (3)
Primary amenorrhea (absence of menstruation).
Lack of body hair as a clue.
Ultrasound scan and karyotype reveal male levels of androgens.
How do individuals with AIS typically identify in terms of gender? (1)
They never respond to androgens, so they appear and often feel female.
What occurs in 5-α-reductase deficiency in an XY individual? (1)
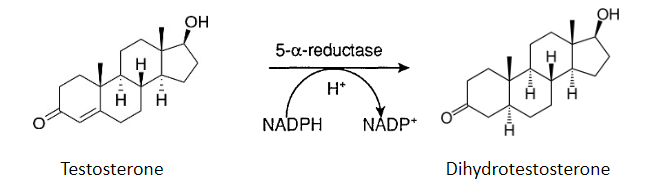
In 5-α-reductase deficiency, testosterone is produced, but dihydrotestosterone (DHT) is not synthesized.
What is the effect of lacking DHT on male external genitalia? (2)
The individual may develop ambiguous genitalia or a predominantly female phenotype at birth.
The external genitalia may remain underdeveloped, resembling female structures.
What happens to internal reproductive structures (the ducts) in individuals with 5-α-reductase deficiency? (2)
The Müllerian ducts typically regress due to the presence of anti-Müllerian hormone (AMH) from Sertoli cells.
The Wolffian ducts may partially develop under the influence of testosterone, resulting in structures like the epididymis and vas deferens.
How does 5-α-reductase deficiency affect gender identity during puberty? (1)
Many individuals may experience virilization during puberty due to increased testosterone, leading to the development of male secondary sexual characteristics.
What is the typical karyotype for individuals with 5-α-reductase deficiency? (1)
Individuals with 5-α-reductase deficiency typically have an XY karyotype.
What is the incidence of 5-α-reductase deficiency? (1)
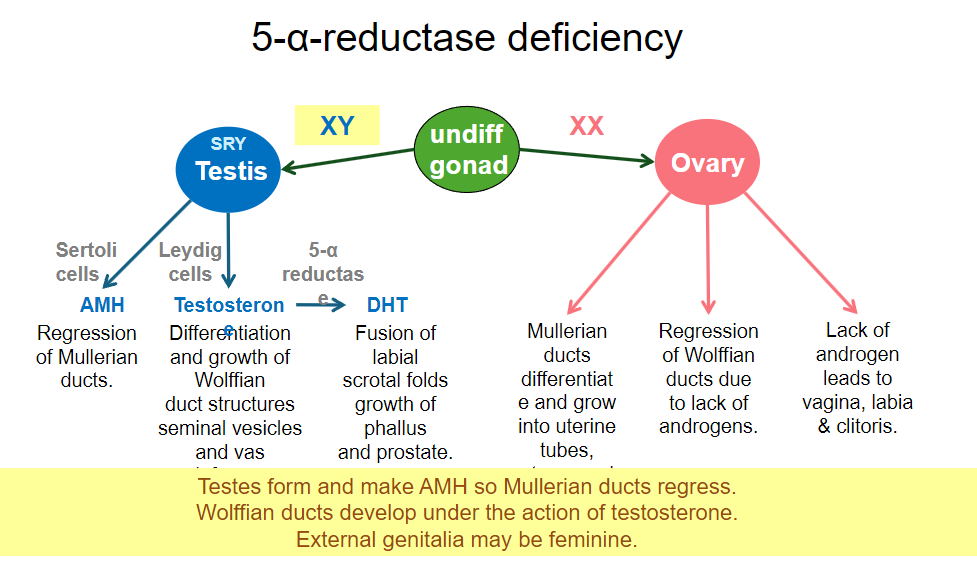
The incidence varies significantly as it is an autosomal recessive condition and can depend on inter-related marriage.
What internal structures form in individuals with 5-α-reductase deficiency? (3)
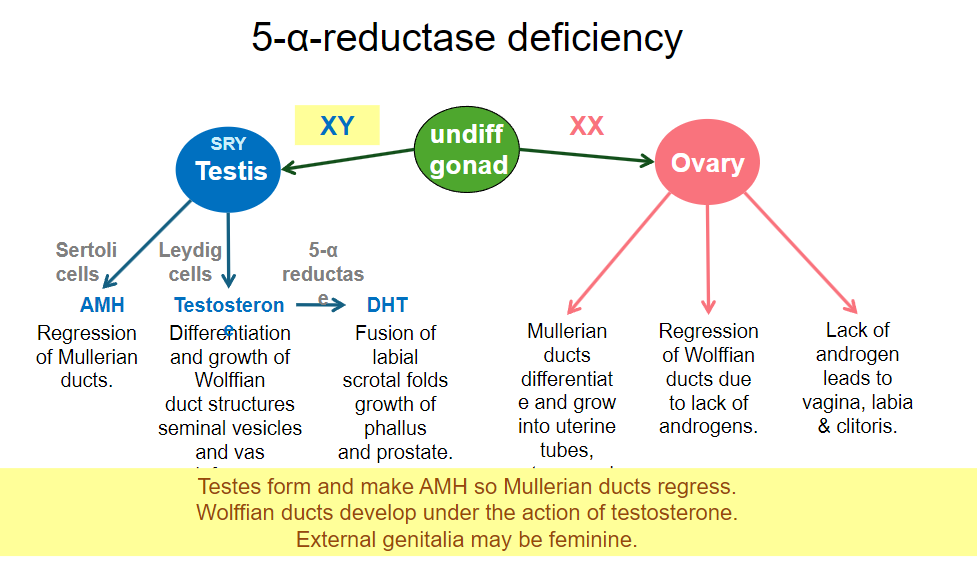
Testes develop, as the condition occurs in individuals with an XY karyotype.
Wolffian duct-derived structures (e.g., epididymis, vas deferens, and seminal vesicles) form due to the presence of testosterone.
Müllerian ducts do not develop, as AMH secreted by the testes inhibits their formation.
What is the effect of testosterone in individuals with 5-α-reductase deficiency? (1)
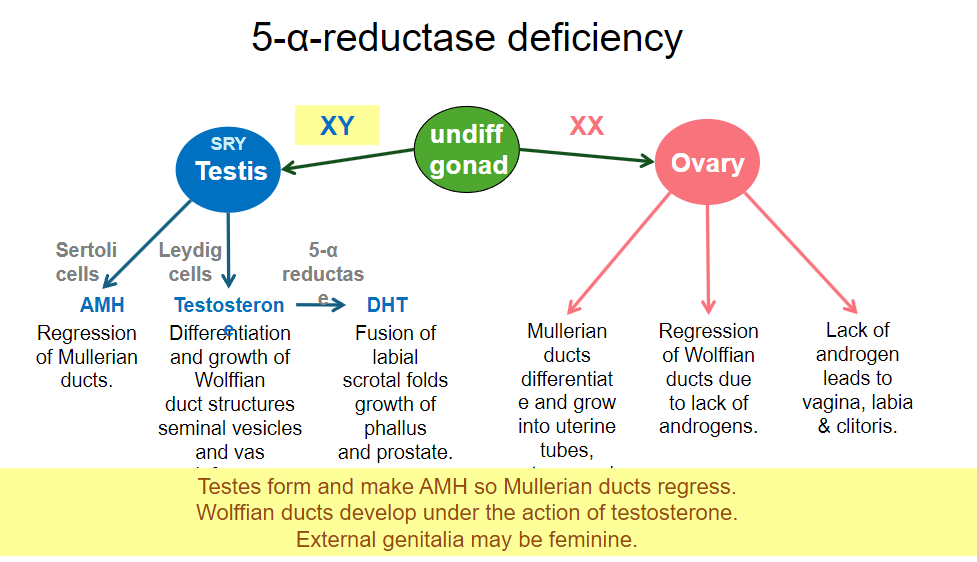
Testosterone acts to promote the formation of internal male structures.
How do external genitalia develop in individuals with 5-α-reductase deficiency? (2)
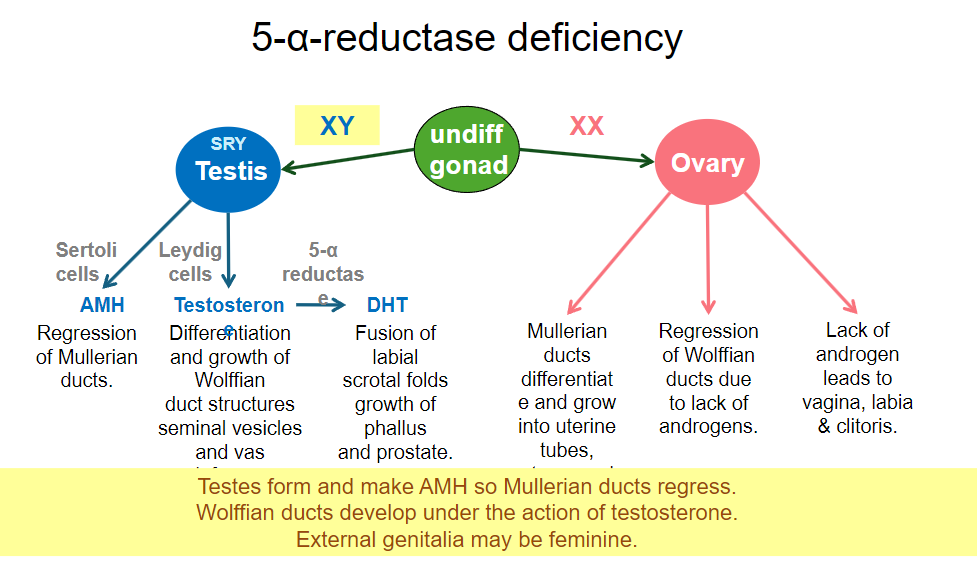
External structures do not develop normally.
Individuals may appear predominantly female or may have ambiguous genitalia.
How does the degree of enzyme block affect presentation in 5-α-reductase deficiency? (1)
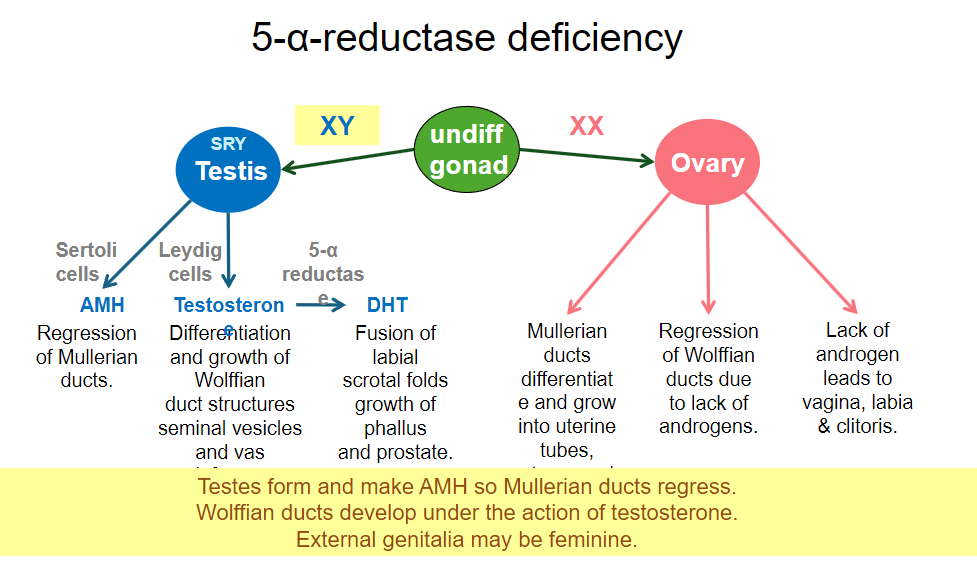
The degree of the enzyme block varies, leading to different presentations of the condition.
What should be assessed at puberty for individuals with 5-α-reductase deficiency? (1)
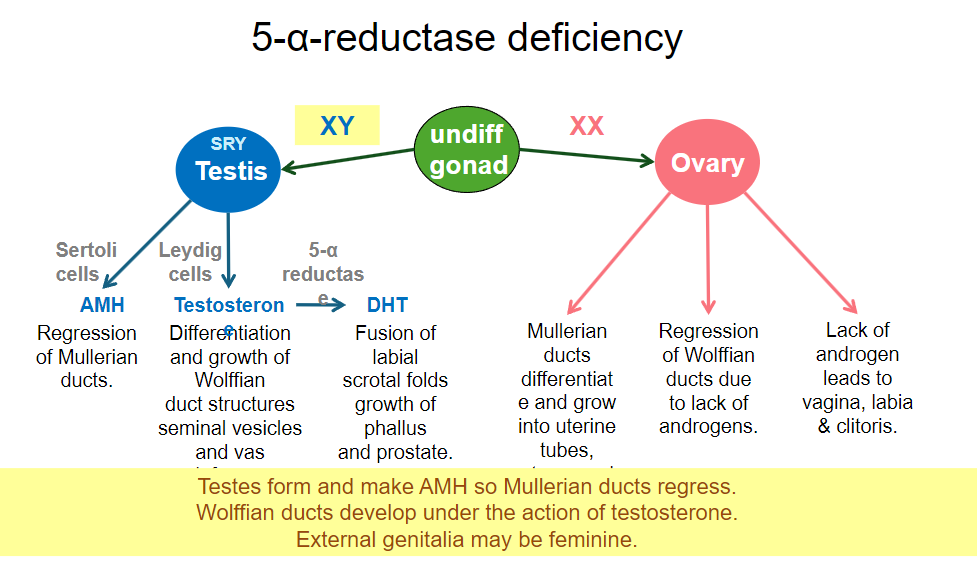
It is important to assess potential for virilization, as higher testosterone levels at puberty may induce male secondary sexual characteristics.
What is the incidence of Turner syndrome? (1)
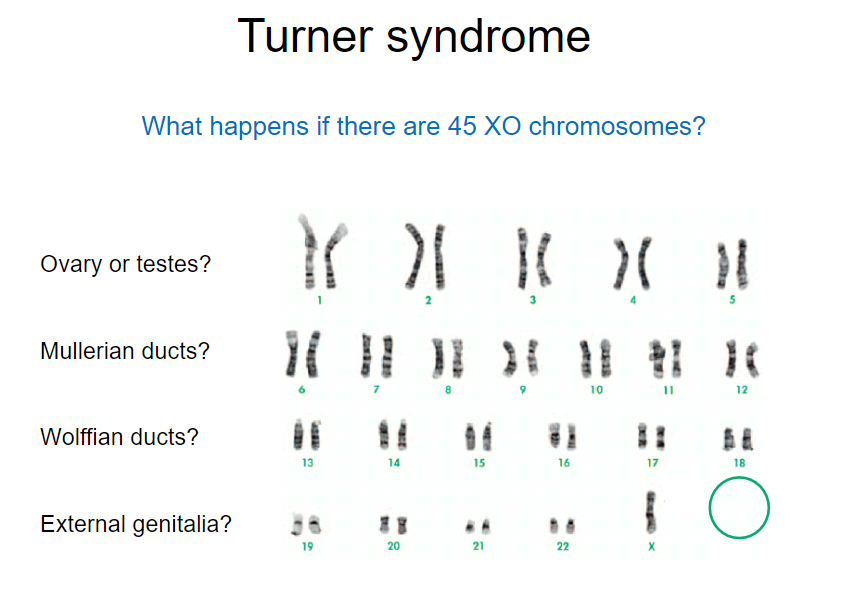
Turner syndrome occurs in approximately 1 in 3,000 live female births.
What is the chromosomal composition associated with Turner syndrome? (1)
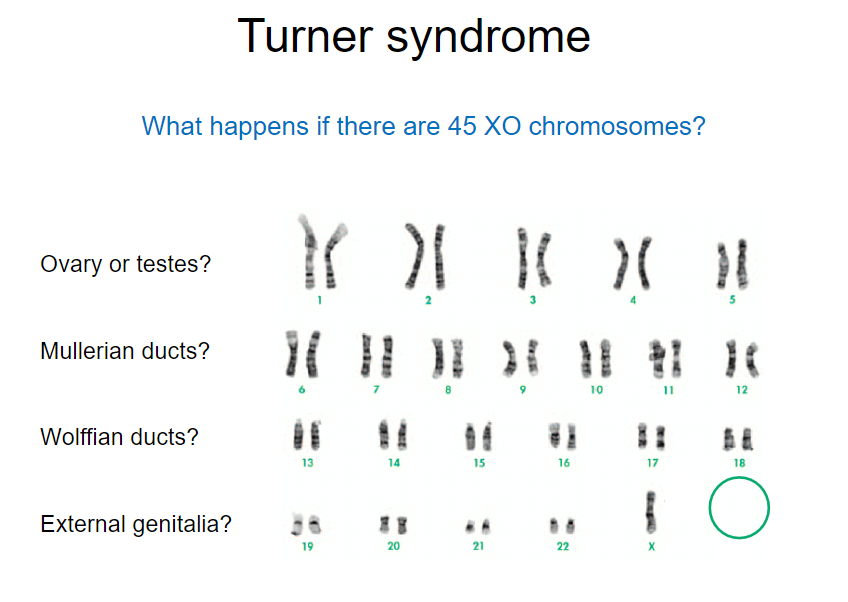
Turner syndrome is characterized by a 45, XO karyotype, indicating the absence of one X chromosome.
What is the effect of Turner syndrome on ovarian function? (1)
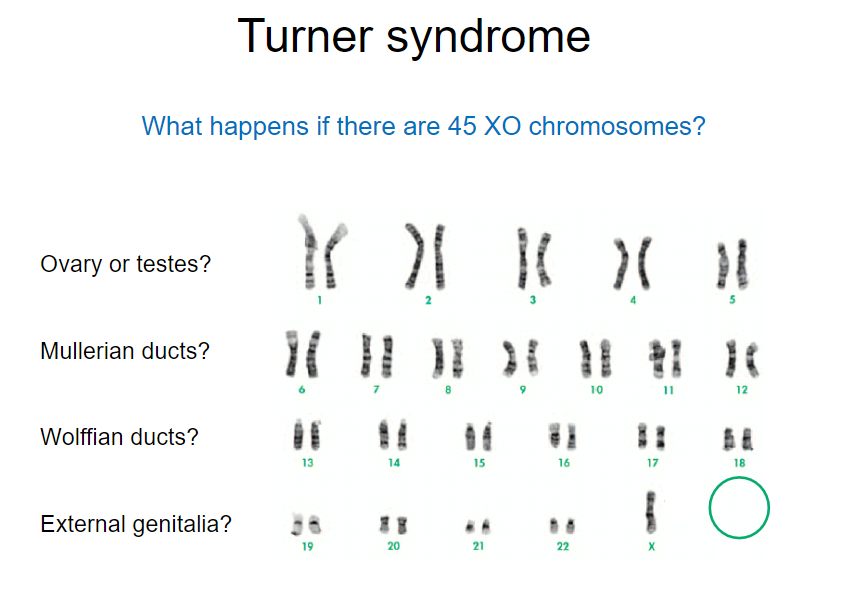
Turner syndrome results in failure of ovarian function, often leading to ‘streak’ ovaries, a form of ovarian dysgenesis.
What do ‘streak’ ovaries illustrate in Turner syndrome? (1)
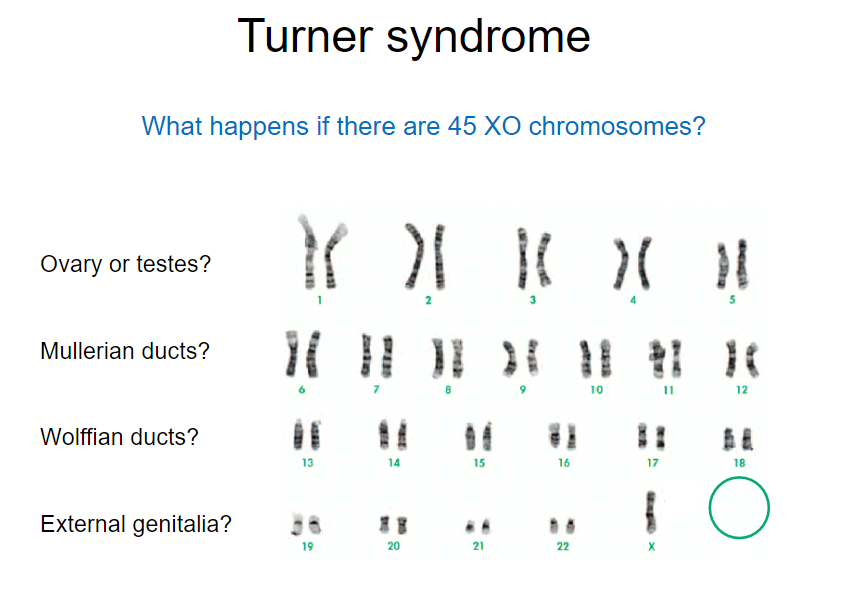
‘Streak’ ovaries illustrate the necessity of two X chromosomes for normal ovarian development.
What are the characteristics of the uterus and fallopian tubes in individuals with Turner syndrome? (2)
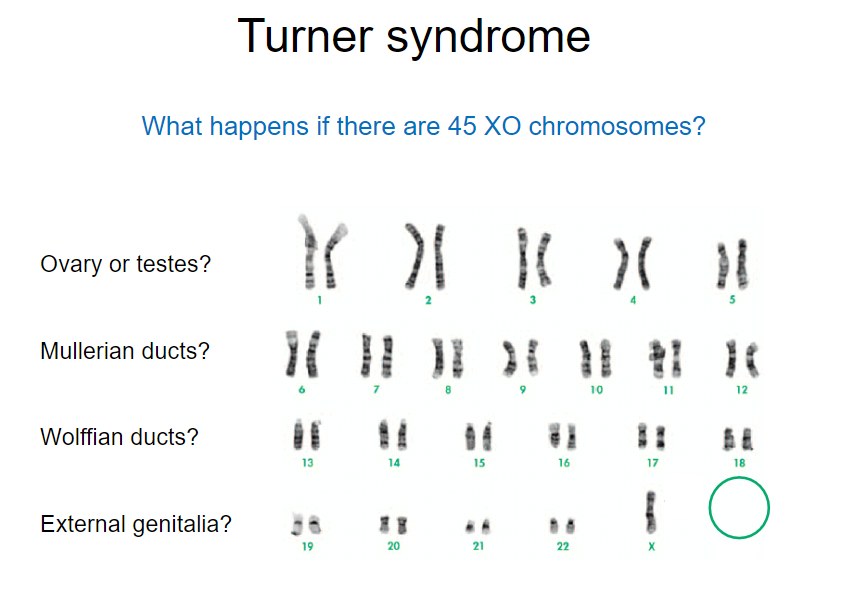
The uterus and fallopian tubes are typically present but may be smaller than normal.
Other defects in growth and development are common, and presentation can vary widely among individuals.
Can individuals with Turner syndrome be fertile? (1)
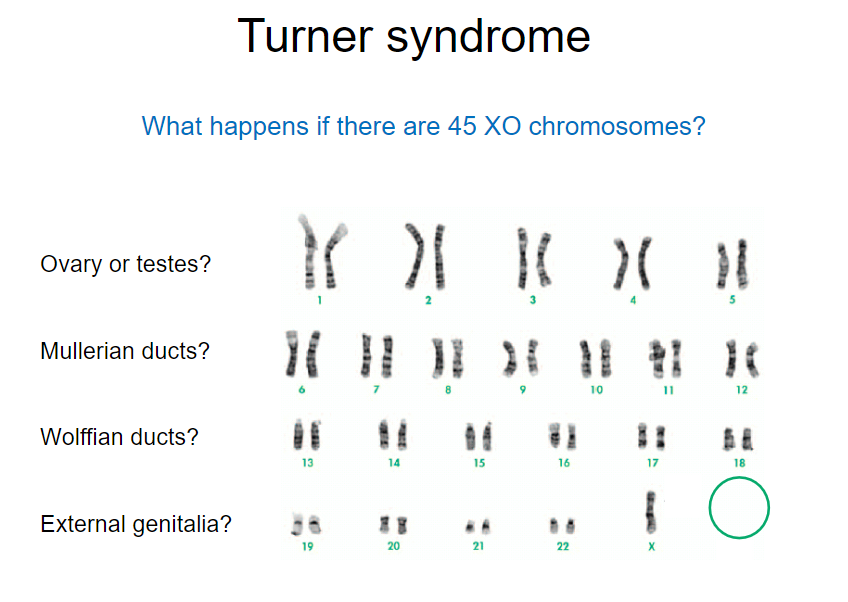
Many individuals with Turner syndrome may have mosaicism, which can lead to varying degrees of fertility.
What is the role of hormone support in individuals with Turner syndrome? (1)
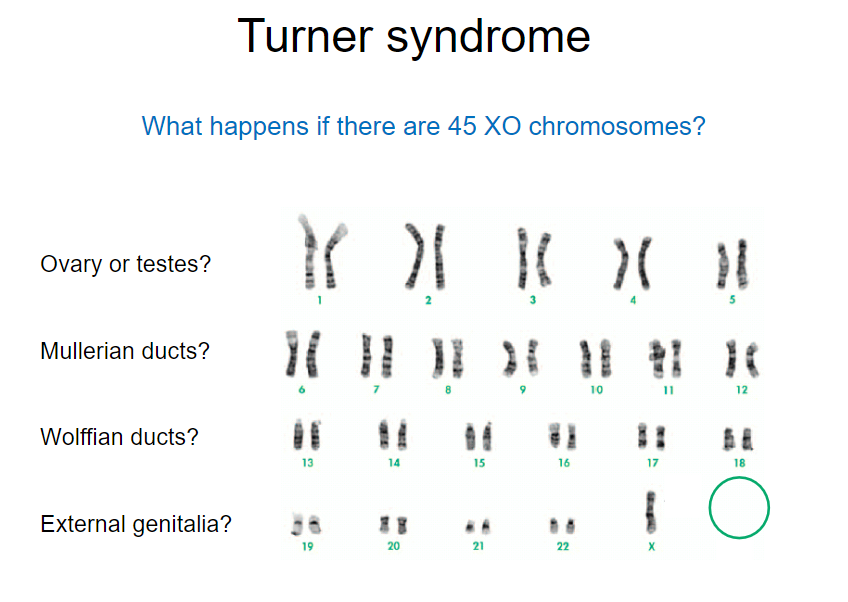
Hormone support is important for bone health and uterine development in individuals with Turner syndrome.
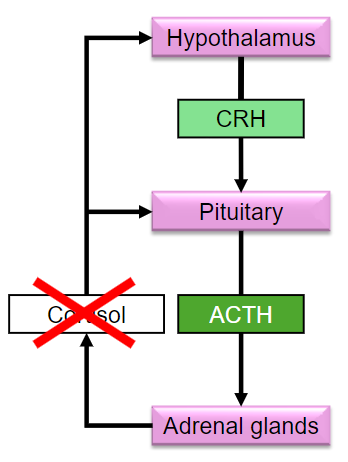
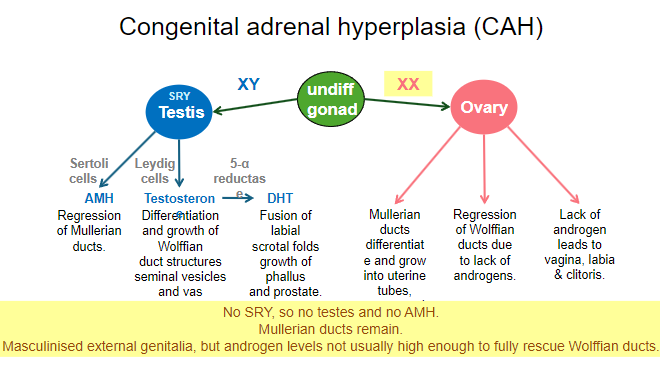
What is congenital adrenal hyperplasia (CAH)? (1)
CAH refers to a group of genetic disorders that affect the adrenal glands, leading to an overproduction of androgens.
What happens to XX females exposed to high levels of androgens in utero? (2)
They may develop male-typical external genitalia, leading to ambiguous genitalia at birth.
This exposure can also lead to various degrees of virilization, affecting physical and reproductive characteristics.
What are the implications of high androgen exposure for XX females regarding gender identity? (1)
Exposure to high levels of androgens can complicate gender identity and social development due to ambiguous genitalia.
How can congenital adrenal hyperplasia affect fertility in XX females? (2)
Fertility may be impacted due to disrupted hormone production, particularly abnormal levels of androgens, which can interfere with ovulation.
Severe cases with atypical genital development may require surgical correction, and complications can arise that further affect fertility.
What is steroidogenesis? (1)
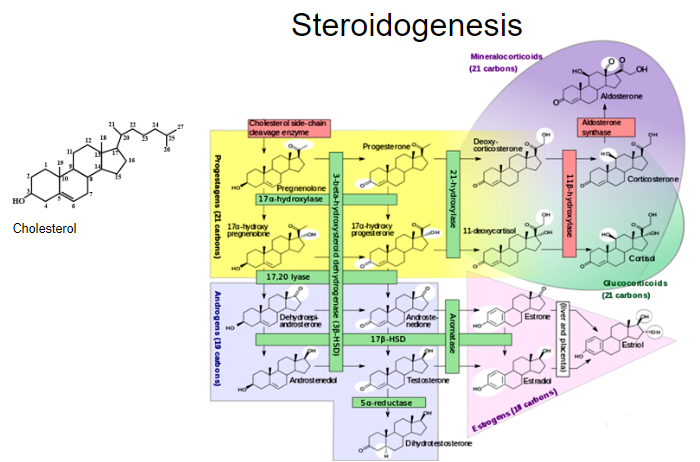
Steroidogenesis is the biological process by which steroids are generated from cholesterol and transformed into various steroid hormones.
Where does steroidogenesis occur in the adrenal glands? (1)
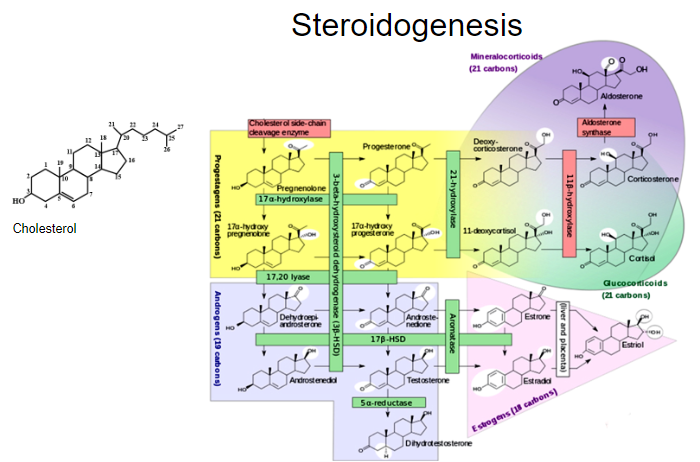
Steroidogenesis occurs in the adrenal cortex, which is the outer layer of the adrenal glands.
What is the primary precursor for steroid hormone synthesis in the adrenal cortex? (1)
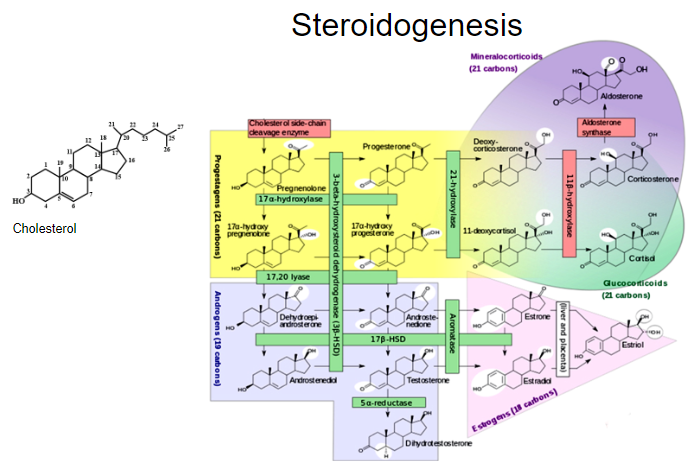
Cholesterol is the primary precursor for the synthesis of steroid hormones in the adrenal cortex.
What is the Hypothalamic-Pituitary-Adrenal (HPA) Axis? (1)
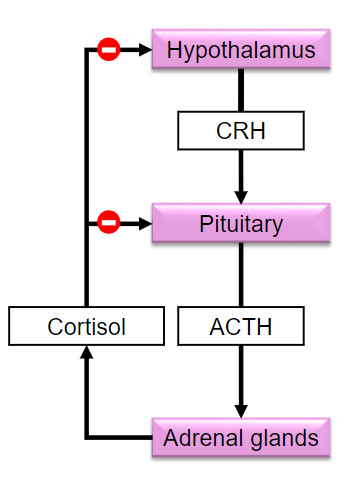
The HPA Axis is a complex set of interactions between the hypothalamus, pituitary gland, and adrenal glands that regulates stress response and various bodily functions
What hormone does the hypothalamus release to stimulate the pituitary gland in the HPA axis? IN THIS CONTEXT (1)
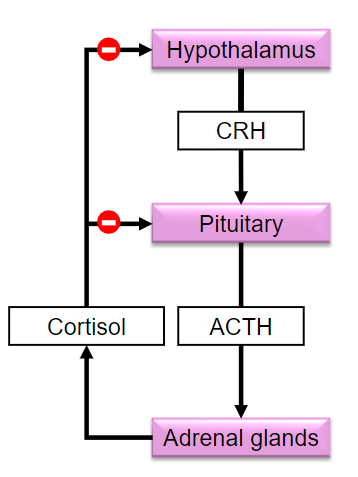
The hypothalamus releases corticotropin-releasing hormone (CRH) to stimulate the pituitary gland.
What is the role of adrenocorticotropic hormone (ACTH)? (1)
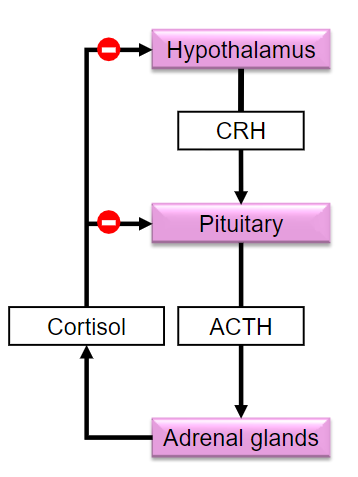
ACTH stimulates the adrenal cortex to secrete glucocorticoids, primarily cortisol.
How does CRH affect cholesterol uptake in the adrenal cortex? (1)
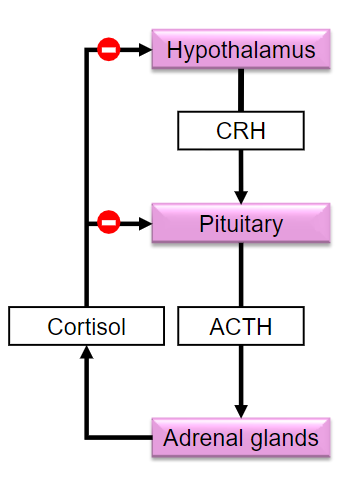
CRH stimulates the rapid uptake of cholesterol into the adrenal cortex, which is necessary for steroid hormone synthesis.
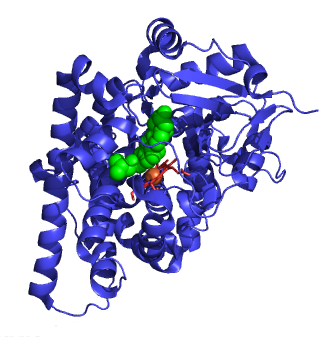
What enzyme does CRH upregulate in the adrenal cortex? (1)
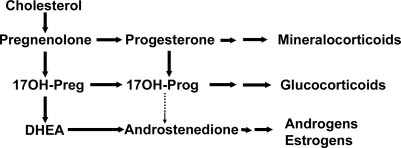
CRH upregulates the cholesterol side-chain cleavage enzyme (P450scc), which is essential for converting cholesterol into pregnenolone, the precursor for steroid hormones.
What effect does ACTH have on glucocorticoid secretion? (1)
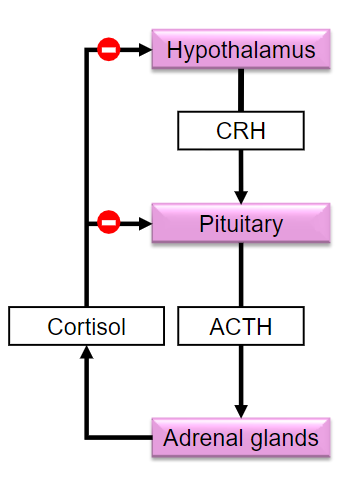
ACTH increases the secretion of glucocorticoids (e.g., cortisol) from the adrenal cortex.
What does corticotropin-releasing hormone (CRH) do? (1)
Stimulates the pituitary gland to secrete adrenocorticotropic hormone (ACTH).
What is the function of adrenocorticotropic hormone (ACTH)? (1)
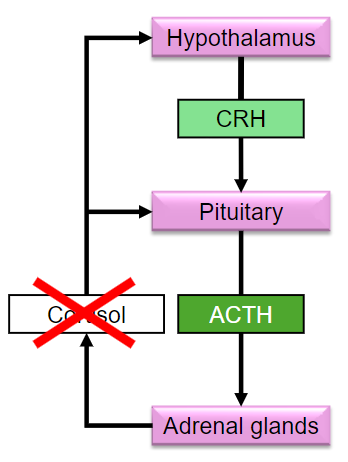
Stimulates rapid uptake of cholesterol into the adrenal cortex.
How does ACTH affect cholesterol in the adrenal cortex? (1)
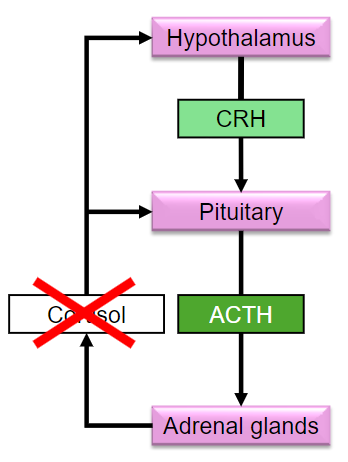
Upregulates the cholesterol side-chain cleavage enzyme (P450scc)
What is the effect of ACTH on glucocorticoid secretion? (1)
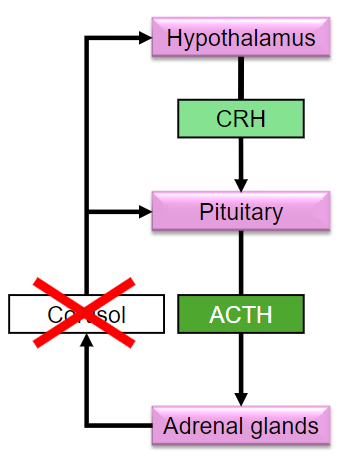
Increases glucocorticoid secretion from the adrenal cortex.
What happens if 21-hydroxylase is absent in congenital adrenal hyperplasia (CAH)? (2)
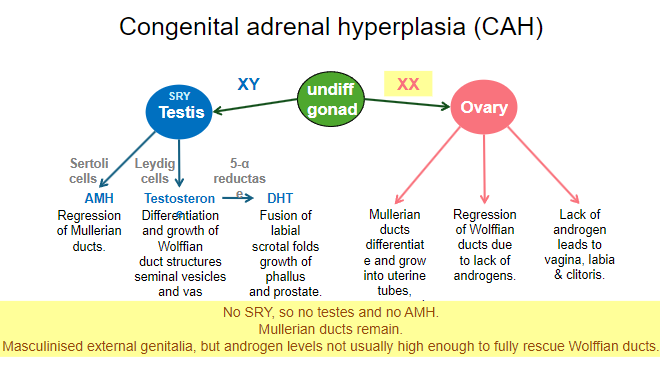
Children may be wrongly gender-assigned at birth due to atypical external genitalia.
Children may have ambiguous genitalia, particularly in XX individuals.
What is a potential lethal condition associated with CAH? (1)
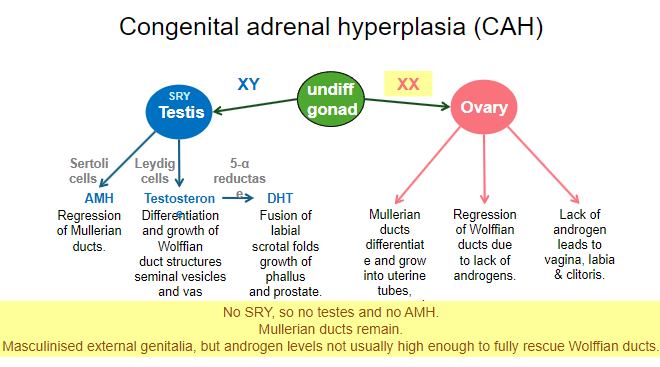
Salt-wasting due to lack of aldosterone. In CAH there is a deficiency of the enzyme 21-hydroxylase which is crucial for the synthesis of cholesterol and aldosterone.
What treatment is often required for individuals with CAH? (1)
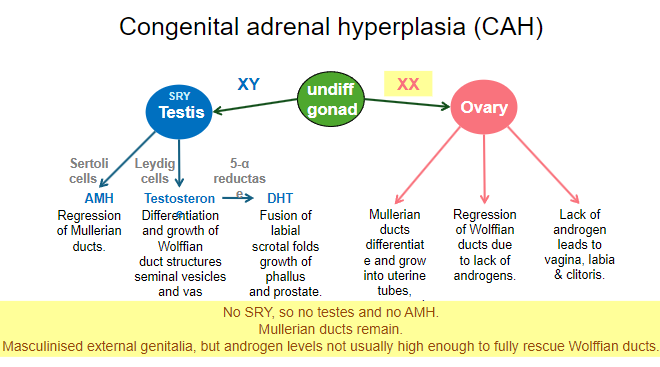
Treatment with glucocorticoids to correct feedback.
What is the incidence rate of congenital adrenal hyperplasia (CAH)? (1)
1 in 15,000 births.
What are the three components required for correct sexual differentiation? (3)
Genetic components.
Anatomical components.
Endocrine components.
Why are disorders of sexual differentiation important for scientific understanding? (1)
They allow scientists to understand the requirements for normal development.
What is the primary issue in the long-term care of individuals with abnormal sexual differentiation? (1)
Long-term functioning of the person rather than immediate 'corrective' surgery.
Picture demonstrating the sequence of sex differentiation: