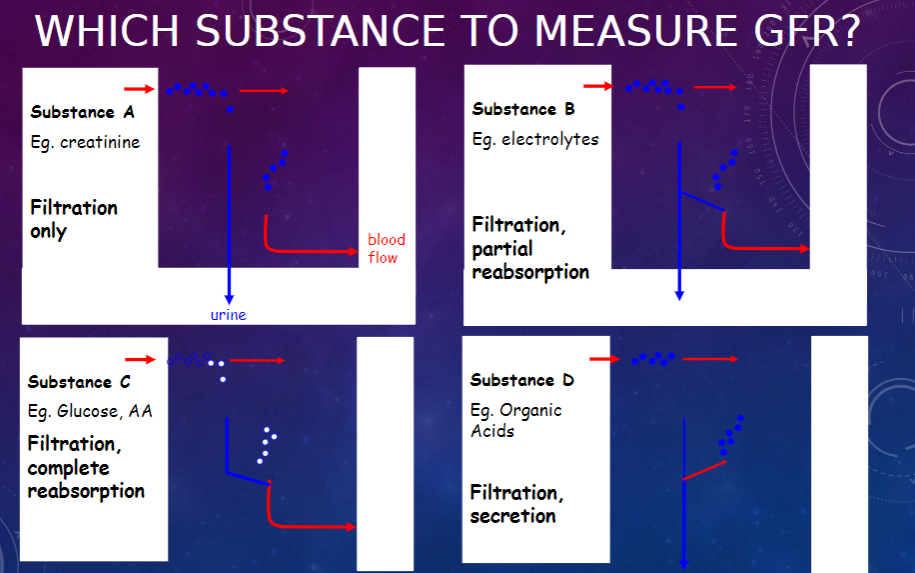
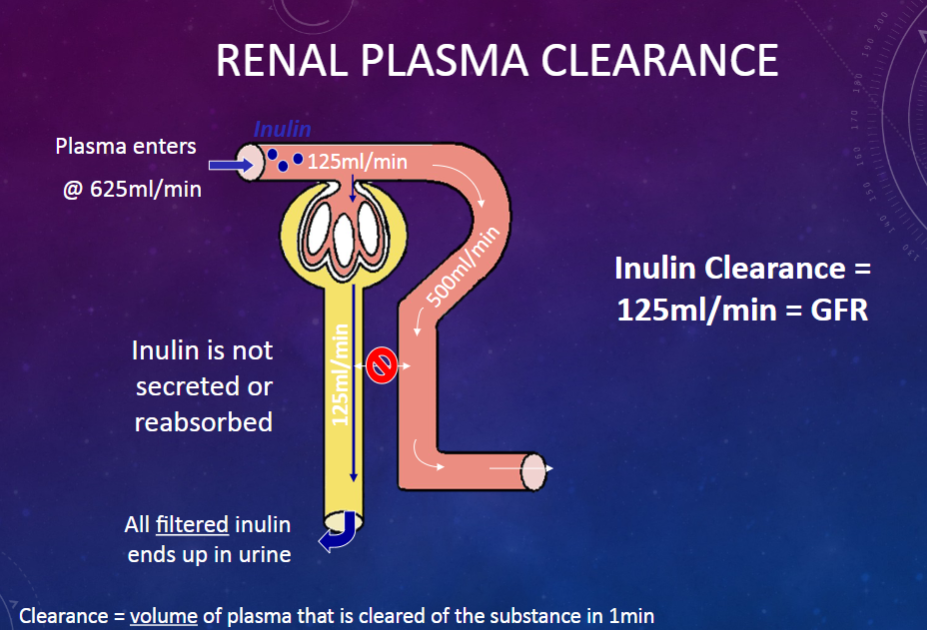
Picture demonstrating WHICH SUBSTANCE is used TO MEASURE GFR:
What is the Inulin Method used for in renal studies? (4)
𖹭 Inulin (not insulin)
𖹭 An inert polysaccharide, MW ~5,000
𖹭 Filters freely through the glomerular membrane
𖹭 Not absorbed, secreted, or metabolized
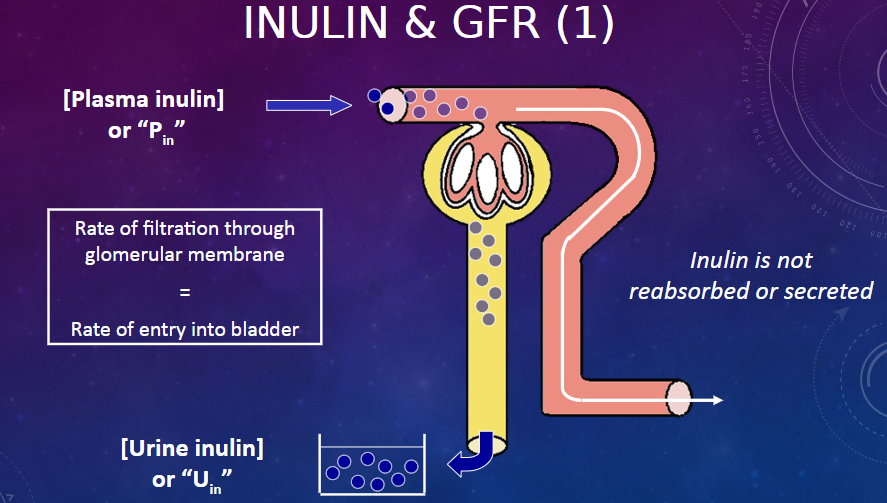
PictureS demonstrating inulin and GFR
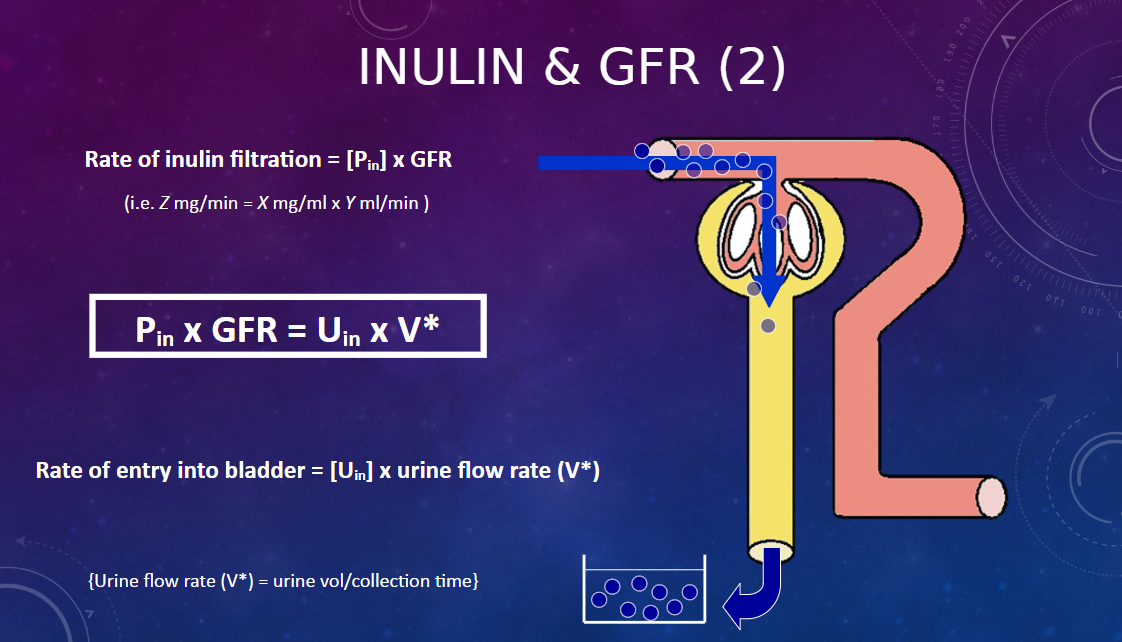
How is the rate of inulin filtration related to the rate of entry into the bladder? (5)
𖹭 Inulin is not reabsorbed or secreted
𖹭 Rate of filtration through the glomerular membrane = Rate of entry into bladder
𖹭 Rate of inulin filtration = [Plasma inulin] x GFR
𖹭 Rate of entry into bladder = [Urine inulin] x urine flow rate (V*)
𖹭 Urine flow rate (V*) = urine volume / collection time
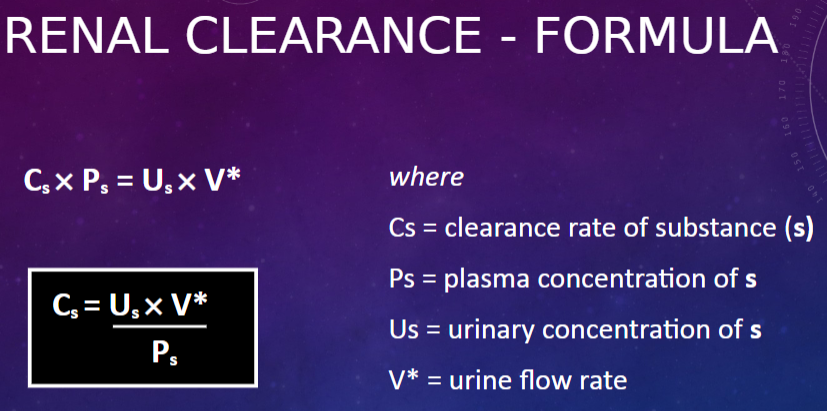
How is the calculation for inulin filtration rate represented? (1)
𖹭 Z mg/min = X mg/ml x Y ml/min
What is the formula for calculating Glomerular Filtration Rate (GFR) using inulin? (4)
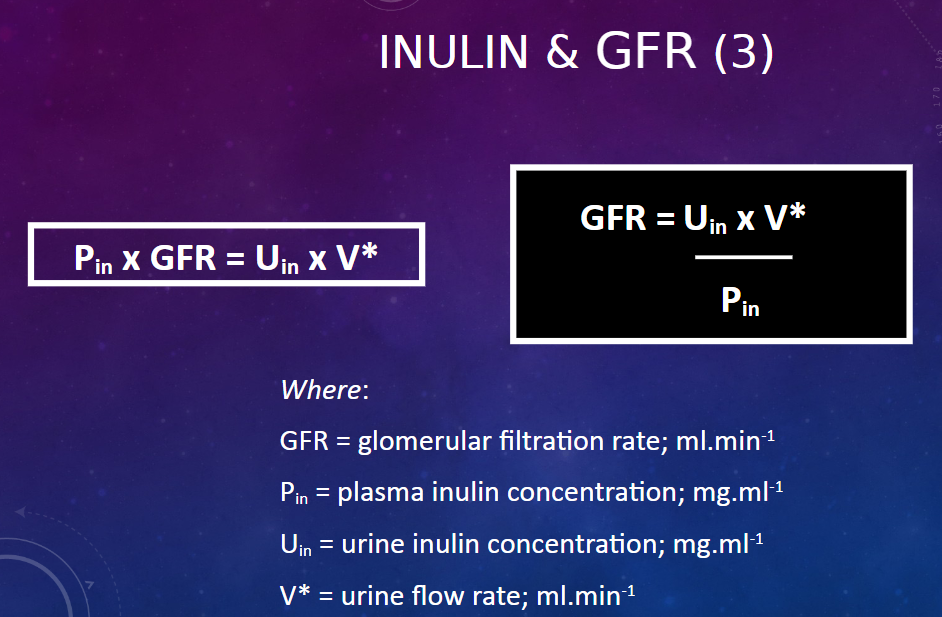
𖹭 GFR = Uin x V* / Pin 𖹭 Where:
GFR = glomerular filtration rate; ml.min^-1
Pin = plasma inulin concentration; mg.ml^-1
Uin = urine inulin concentration; mg.ml^-1
V* = urine flow rate; ml.min^-1 𖹭 Pin x GFR = Uin x V*
What is the definition of renal clearance of a substance?
𖹭 Renal clearance of a substance is the volume of plasma that is completely cleared (excreted into urine) of the substance by the kidney per unit of time, expressed in ml/min.
Picture demonstrating renal plasma clearance:
Picture demonstrating renal clearance formula:
What are the drawbacks of the inulin method in measuring Glomerular Filtration Rate (GFR)?
𖹭 Prolonged infusion
𖹭 Repeated plasma samples
𖹭 Difficult routine clinical use
What substance is used as an alternative for clinical GFR measurement due to the drawbacks of the inulin method?
𖹭 Creatinine
What are the advantages of using creatinine for measuring Glomerular Filtration Rate (GFR)?
𖹭 An intrinsic inert substance
𖹭 Released at a steady level in plasma from skeletal muscle
𖹭 No infusion needed
𖹭 Freely filtered
𖹭 Not reabsorbed in the tubule
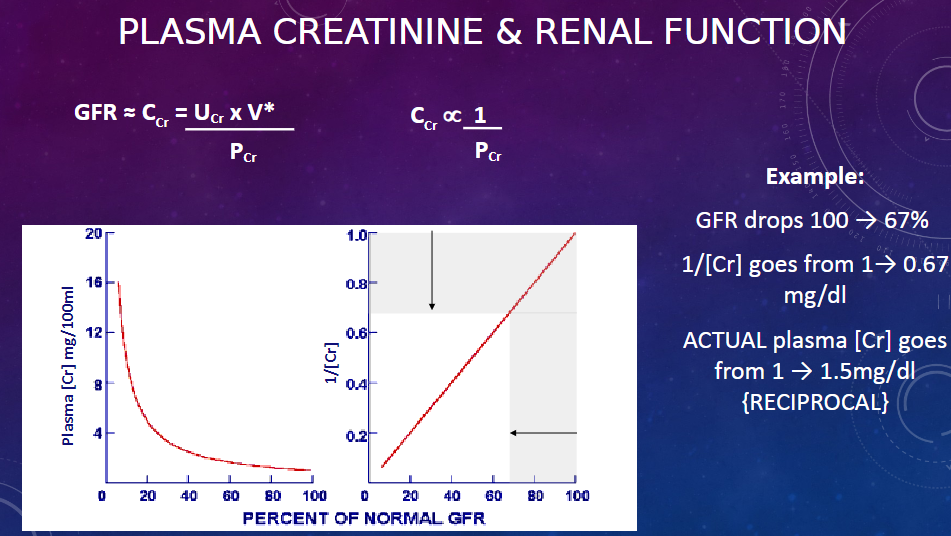
What are the disadvantages associated with measuring GFR using creatinine?
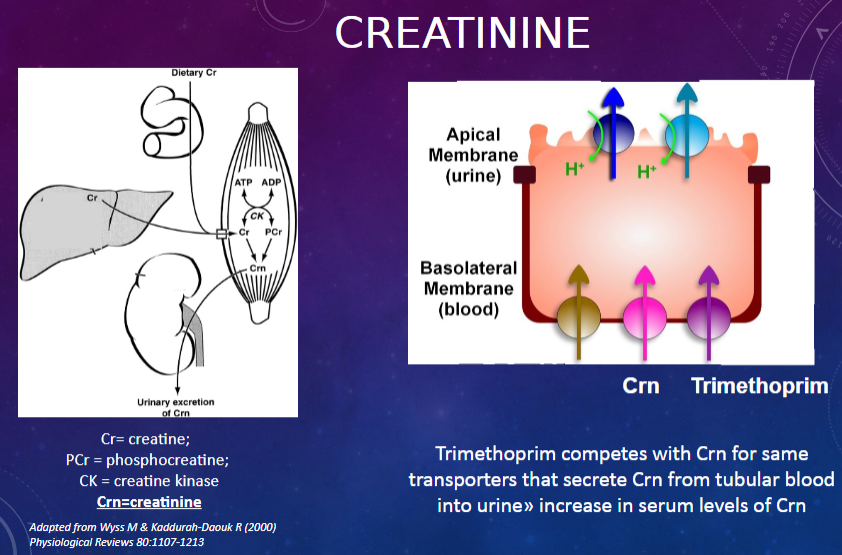
𖹭 Some secreted into the tubule
𖹭 GFR < Ccr = Ucr× V* (~150 ml/min) Pcr (rather than 125 ml/min)
What does "Cr" stand for in the context of creatinine measurement?
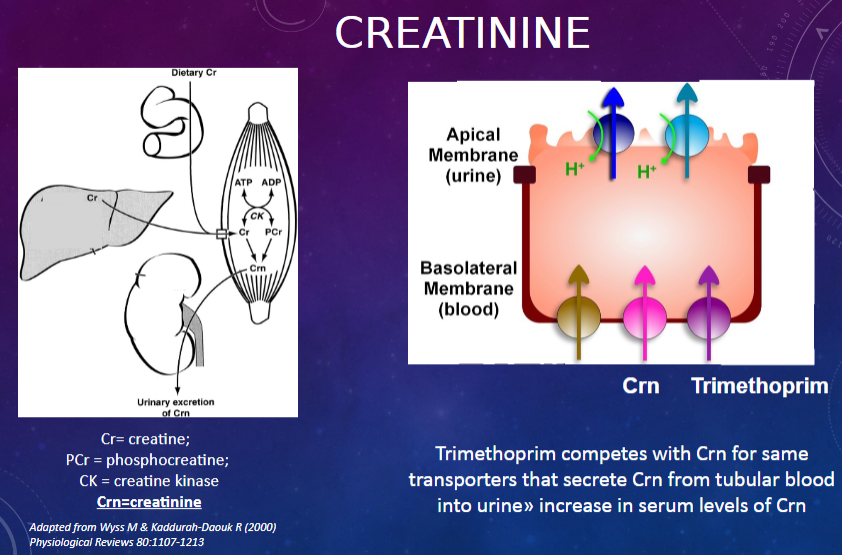
𖹭 Cr = creatine; PCr = phosphocreatine; CK = creatine kinase
What is the abbreviation used for creatinine in the context of this discussion?
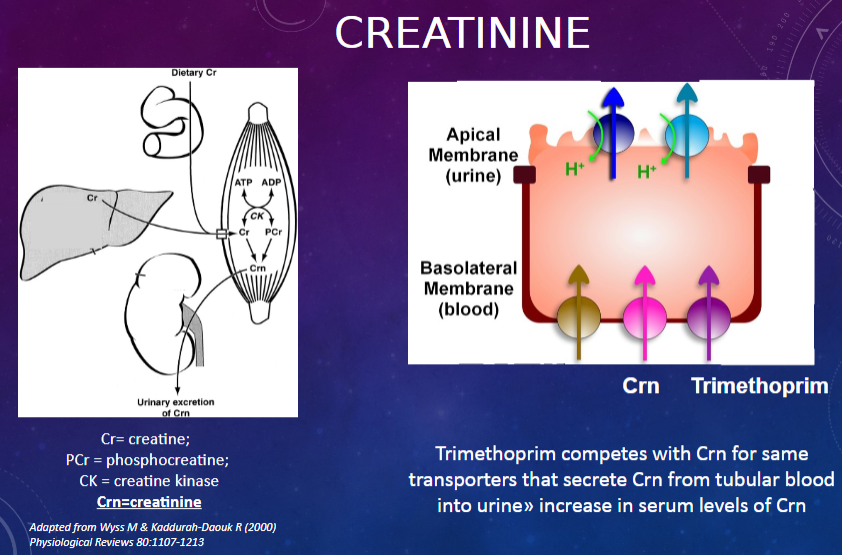
𖹭 Crn = creatinine
How does trimethoprim affect serum levels of creatinine?
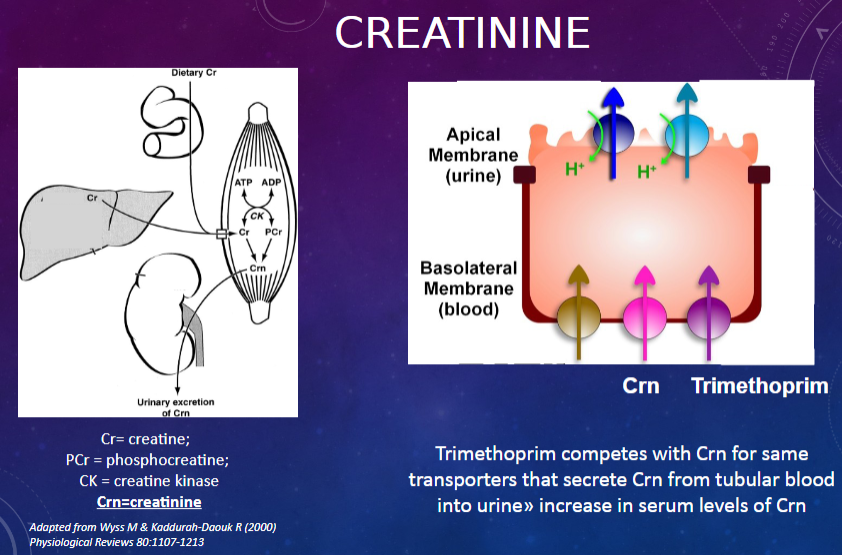
𖹭 Trimethoprim competes with Crn for the same transporters that secrete Crn from tubular blood into urine, resulting in an increase in serum levels of Crn.
Picture demonstrating plasma creatine and normal function:
Picture demonstrating the DECLINE IN GFR WITH AGE:
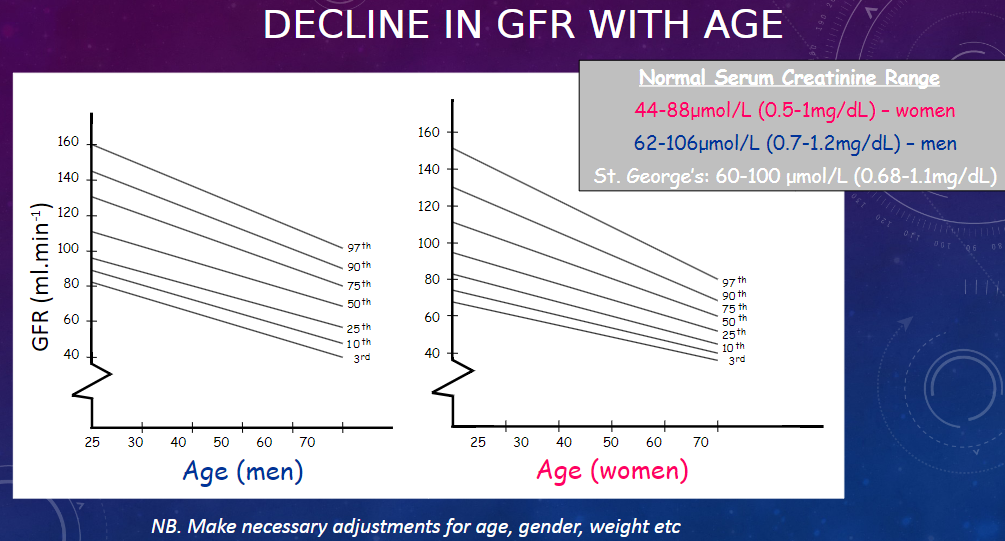
What are the creatinine levels indicating normal kidney function for the little girl and the body-builder?
𖹭 The little girl has normal kidney function and a creatinine level less than 60 μmol/L.
𖹭 The body-builder has normal kidney function and a creatinine level of 120 μmol/L.
How would a creatinine level of 120 μmol/L be interpreted differently for the little girl and the body-builder?
𖹭 For the girl, a creatinine level of 120 μmol/L would indicate very poor kidney function.
What does eGFR stand for in the context of kidney function?
𖹭 eGFR stands for estimated Glomerular Filtration Rate.
How is eGFR calculated?
𖹭 eGFR is calculated using an equation that incorporates blood tests, age, sex, and other relevant information to estimate Glomerular Filtration Rate.
What is the current equation used for estimating eGFR in adults?
𖹭 The current equation used is CKD-EPI Adults (Chronic Kidney Disease Epidemiology Collaboration).
How does eGFR compare to direct measurement methods like 24-hour urine collection?
𖹭 While eGFR isn't as accurate as direct measurement methods such as 24-hour urine collection, it is much simpler as it requires just one blood test.
What advantage does eGFR offer in detecting kidney disease?
𖹭 eGFR can spot kidney disease earlier than would be possible using just creatinine measurements.
What is the formula used in the CKD-EPI equation for estimating Glomerular Filtration Rate (GFR)?
𖹭 GFR = 141 × min (Scr/κ, 1)^α × max (Scr/κ, 1)^-1.209 × 0.993^Age × 1.018 [if female] × 1.159 [if black]
What do the variables represent in the CKD-EPI equation?
𖹭 Scr = serum creatinine in mg/dL or μmol/L
𖹭 κ = 0.7 for females and 0.9 for males
𖹭 α = -0.329 for females and -0.411 for males
What adjustments are made in the CKD-EPI equation for individuals over 75 years of age?
𖹭 The CKD-EPI equation is less biased at GFR ≥60ml/min/1.73m^2 and performs better in people >75 years than previous equations. However, in the UK, this adjustment is no longer made.
What recommendation does the National Kidney Disease Education Program (USA) make regarding reporting GFR values?
𖹭 The National Kidney Disease Education Program (USA) recommends reporting GFR values ≥60ml/min/1.73m^2 as such and not an exact number, with reference to CKD stages.
What are the stages of Chronic Kidney Disease (CKD) based on?
𖹭 The stages of CKD are mainly based on measured or estimated Glomerular Filtration Rate (GFR).
How many stages are there in CKD, and what is the kidney function status in Stages 1 and 2?
𖹭 There are five stages of CKD. Kidney function is normal in Stage 1, and minimally reduced in Stage 2.
What are the characteristics of Stage 1 Chronic Kidney Disease (CKD)?
𖹭 GFR: 90+
𖹭 Description: Normal kidney function but urine findings or structural abnormalities or genetic trait point to kidney disease
𖹭 Treatment stage: Observation, control of blood pressure.
What are the characteristics of Stage 2 Chronic Kidney Disease (CKD)?
𖹭 GFR: 60-89
𖹭 Description: Mildly reduced kidney function, and other findings (as for stage 1) point to kidney disease
𖹭 Treatment stage: Observation, control of blood pressure and risk factors.
What are the characteristics of Stage 3 Chronic Kidney Disease (CKD)?
𖹭 GFR: 45-59
𖹭 Description: Moderately reduced kidney function
𖹭 Treatment stage: Observation, control of blood pressure and risk factors.
What are the characteristics of Stage 3 Chronic Kidney Disease (CKD)?
𖹭 GFR: 30-44
𖹭 Description: Moderately reduced kidney function
𖹭 Treatment stage: Observation, control of blood pressure and risk factors.
What are the characteristics of Stage 4 Chronic Kidney Disease (CKD)?
𖹭 GFR: 15-29
𖹭 Description: Severely reduced kidney function
𖹭 Treatment stage: Planning for end stage renal failure.
What are the characteristics of Stage 5 Chronic Kidney Disease (CKD)?
𖹭 GFR: <15 or on dialysis
𖹭 Description: Very severe, or end stage kidney failure (sometimes called established renal failure)
𖹭 Treatment stage: Treatment choices.
What are the limitations of estimated Glomerular Filtration Rate (eGFR)?
𖹭 It is only an estimate, and a significant error is possible.
𖹭 eGFR is most likely to be inaccurate in people at extremes of body type, for example, malnourished individuals, amputees, etc.
𖹭 It is not valid in pregnant women or children, and its accuracy decreases in patients older than 70 years.
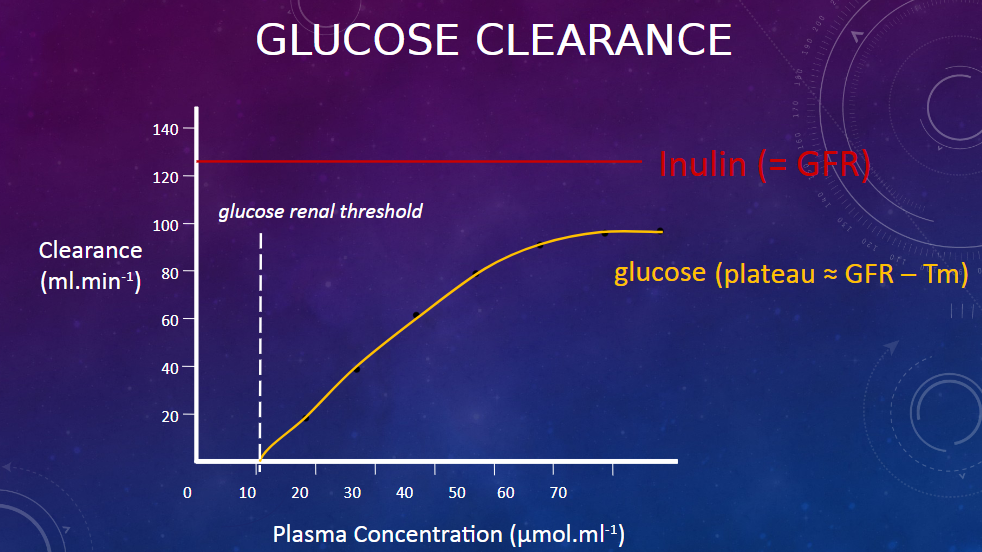
What are the characteristics of substances with clearance equal to inulin (= GFR)?
𖹭 Approximately 125ml/min in adult males and 10% less in females
𖹭 Examples include antibiotics (streptomycin/gentamicin)
What distinguishes substances with clearance less than inulin (< GFR)?
𖹭 Either not filtered freely
𖹭 Or reabsorbed from the tubule
What defines substances with clearance greater than inulin (> GFR)?
𖹭 Secreted into the tubule
What characterizes substances with clearance less than Glomerular Filtration Rate (GFR)?
𖹭 Not freely filtered
𖹭 For example, Albumin clearance = 0ml/min
𖹭 Similarly for drugs bound to albumin, such as digoxin, warfarin
What happens to substances that are re-absorbed in relation to their clearance?
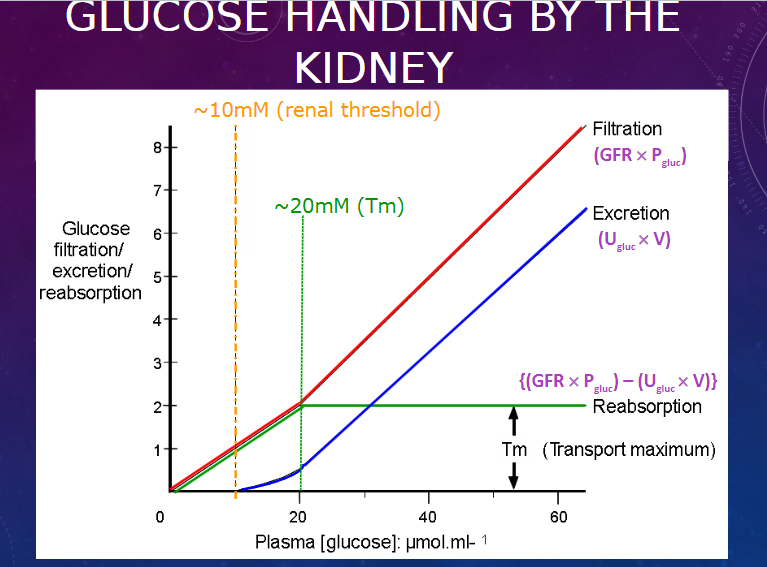
𖹭 They filter freely but are usually absent from urine, indicating complete reabsorption.
𖹭 For instance, Glucose clearance = 0ml/min
Picture demonstrating glucose handling by the kidney:
Picture demonstrating GLUCOSE CLEARANCE:
What substances are actively reabsorbed, and what are their characteristics?
𖹭 All amino acids:
Clearance = 0ml/min unless excess filtered
Occurs in pathological conditions (e.g., myeloma)
Associated with the production of Bence-Jones protein in plasma
𖹭 Ca2+, Na+, PO42-, Mg2+
𖹭 Water-soluble vitamins
What substances are passively reabsorbed?
𖹭 Cl–, urea, some drugs
What factors influence the display transport maximums of substances?
𖹭 They are dependent on electrochemical gradients.
What characterizes substances with clearance greater than Glomerular Filtration Rate (GFR)?
𖹭 They are substances that are actively secreted.
𖹭 They filter freely but are actively secreted against the electrochemical gradient.
Examples include:
Endogenous substances such as weak organic acids & bases, adrenaline, dopamine, steroids.
Exogenous substances such as penicillin, probenecid, para-aminohippuric acid (PAH).
What is Renal Plasma Flow (RPF), and how is it defined?
𖹭 RPF is the rate at which plasma flows through the kidney.
How does estimating Renal Plasma Flow (RPF) help in determining Renal Blood Flow (RBF)?
𖹭 Estimating the RPF through the kidneys allows us to estimate the rate of total blood flow (RBF) through the kidneys.
What are the components of blood, and how do they contribute to the estimation of Renal Blood Flow (RBF)?
𖹭 Blood consists of about 55% plasma and about 45% cellular components, mostly red blood cells (RBCs).
What is para-aminohippuric acid (PAH), and what are its characteristics?
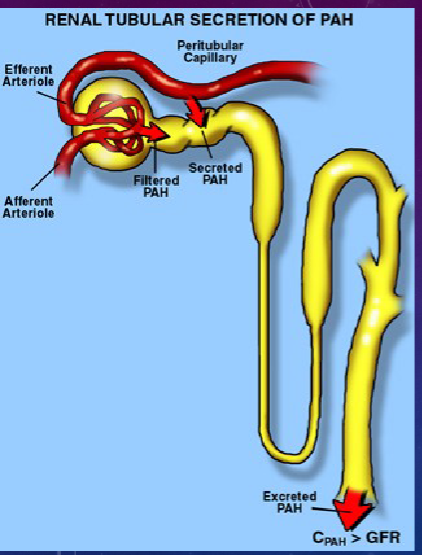
𖹭 PAH is a weak acidic metabolite of glycine, originally found in horse’s urine.
𖹭 It is filtered freely and enters the glomerular filtrate, but a large amount remains in the plasma.
𖹭 The majority of PAH is secreted back into the proximal convoluted tubule, leading to its excretion in urine.
𖹭 PAH is suitable as a marker to measure renal plasma flow.
How does the secretion of para-aminohippuric acid (PAH) occur in the kidney?
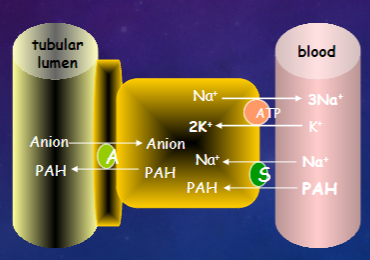
𖹭 Active transport occurs in the basolateral membrane.
𖹭 Passive transport occurs across the luminal membrane into the tubule.
How does the concentration of para-aminohippuric acid (PAH) in plasma relate to its clearance through the kidney?
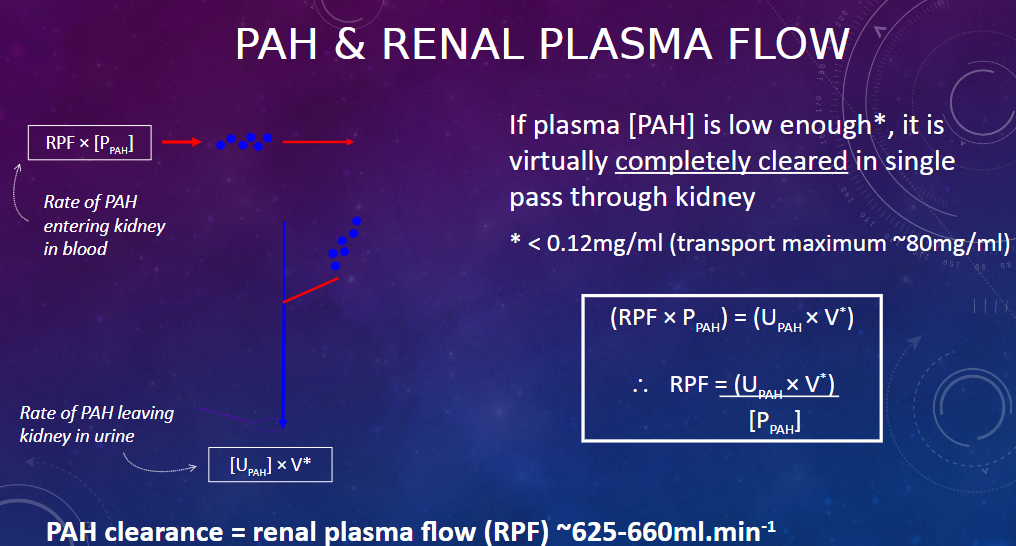
𖹭 If the plasma concentration of PAH is low enough, it is virtually completely cleared in a single pass through the kidney
What is the threshold concentration for PAH in plasma, below which it is almost completely cleared in a single pass through the kidney?
![<p>𖹭 Plasma [PAH] < 0.12mg/ml (transport maximum ~80mg/ml)</p>](/flashcards/cardimage2/85558a4f/354/8354536_back.png)
𖹭 Plasma [PAH] < 0.12mg/ml (transport maximum ~80mg/ml)
How can the filtration fraction be calculated using Glomerular Filtration Rate (GFR) and Renal Plasma Flow (RPF)?
𖹭 The filtration fraction is the fraction of plasma that is filtered through the glomeruli.
𖹭 GFR is determined from Inulin clearance.
𖹭 RPF is determined from para-aminohippuric acid (PAH) clearance.
𖹭 Given:
RPF = 660
GFR = 125
𖹭 Filtration Fraction = (GFR / RPF) x 100 = (125 / 660) x 100 ≈ 19%
A summary:
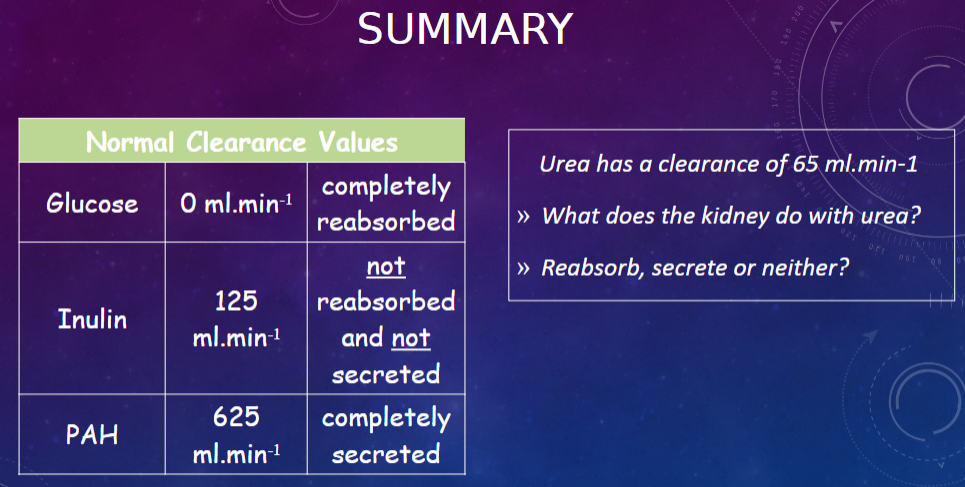
Urea Clearance:
Urea has a clearance of 65 ml/min.
The kidney neither completely reabsorbs nor secretes urea.
Normal Clearance Values:
Glucose: 0 ml/min, completely reabsorbed.
Inulin: 125 ml/min, not reabsorbed and not secreted.
PAH: 625 ml/min, completely secreted.