What are the contents of gastric juice in the fasting state? (6)
And what is the pH of gastric juice in the fasting state?
♪ Cations: Na⁺, K⁺, Mg²⁺, H⁺
♪ Anions: Cl⁻, HPO₄²⁻, SO₄²⁻
♪ Pepsinogen
♪ Lipase
♪ Mucus
♪ Intrinsic factor
The pH of gastric juice in the fasting state is approximately 1-3.0
How much gastric juice does the stomach add to intestinal contents per day?
Gastric juice adds approximately 2.5 liters per day to intestinal contents
Why is gastric juice essential for digestion and absorption?
Gastric juice is essential for digestion and absorption processes in the gastrointestinal system
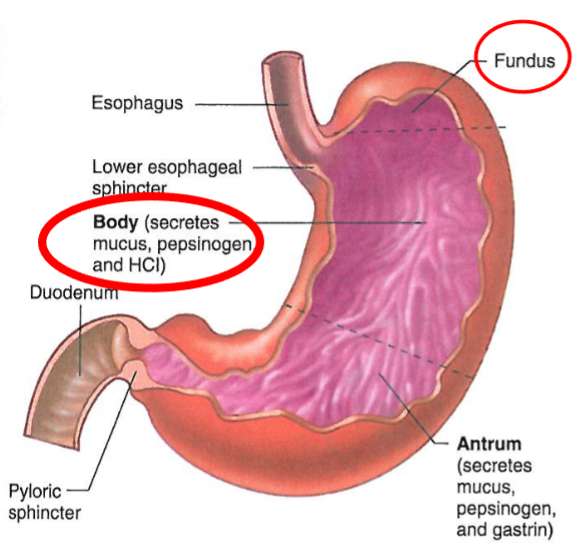
What are the main components secreted by the stomach? (3)
The stomach secretes:
♪ Mucus
♪ Hydrochloric acid (HCl)
♪ Pepsinogen
What is the function of the thick-walled lower portion of the stomach (antrum)?
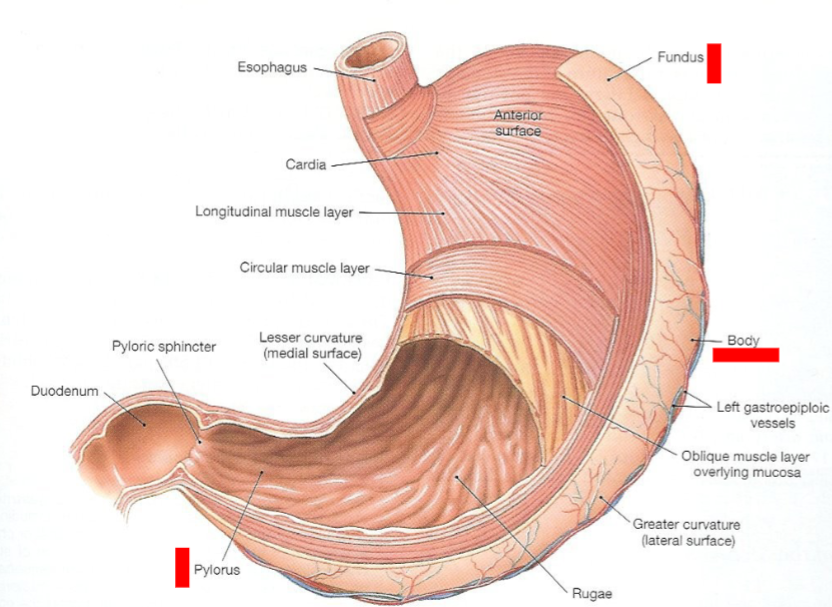
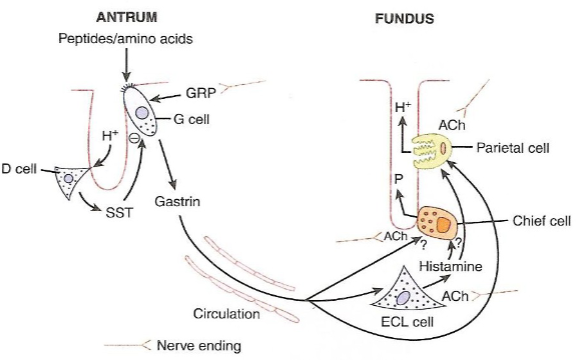
The thick-walled lower portion of the stomach secretes increased gastrin, which mediates acid secretion (HCl secretion)
What are the main cells involved in the secretion of gastric juice? (4)
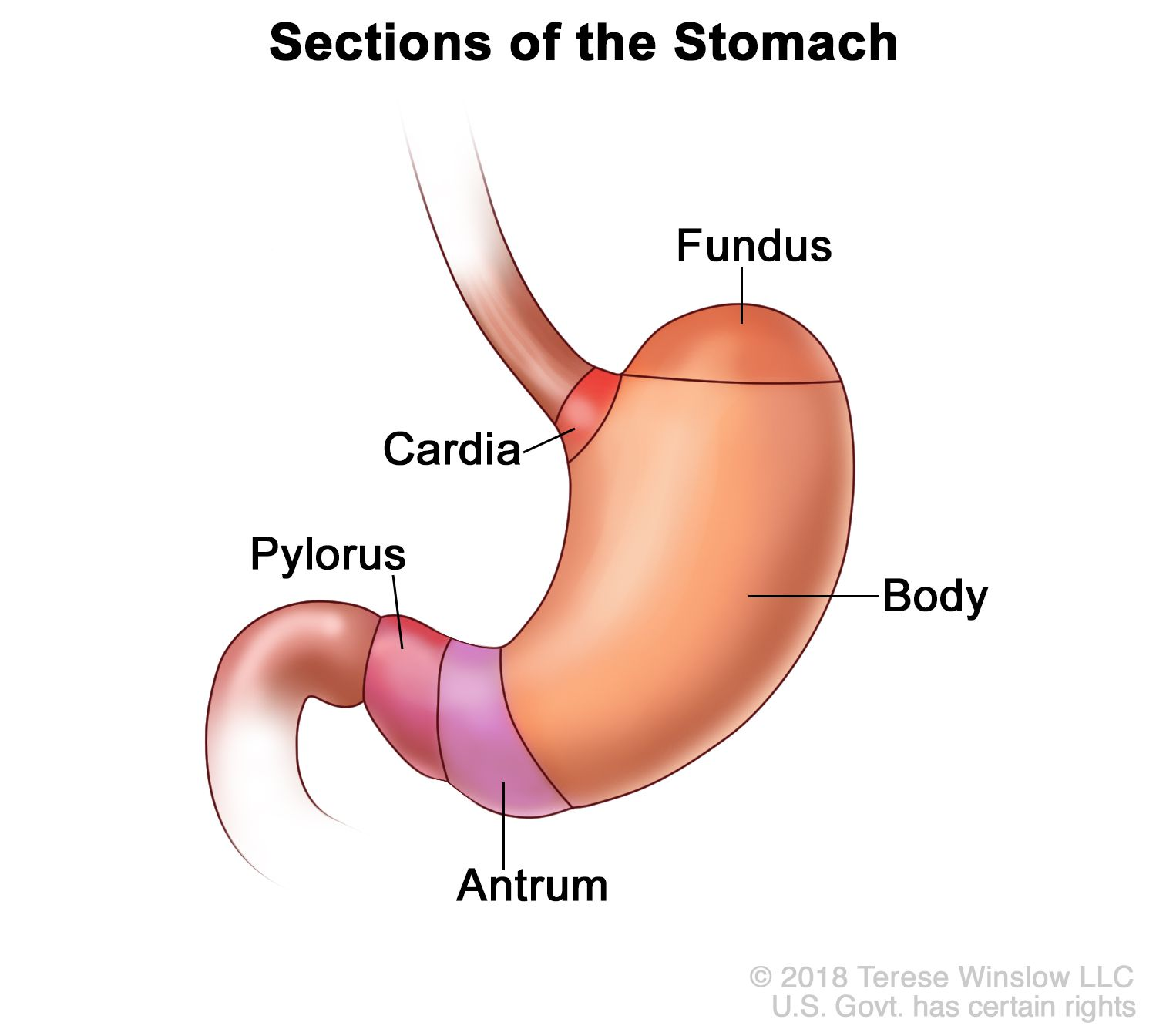
♪ Parietal cells in the stomach's tubular glands secrete HCl and intrinsic factor
♪ Enterochromaffin-like cells (ECL) produce paracrine agents such as histamine and serotonin
♪ Fundus secretes pepsinogen
♪ Pylorus secretes mucus and gastrin
How is gastric acid (HCl) produced in the stomach lumen?
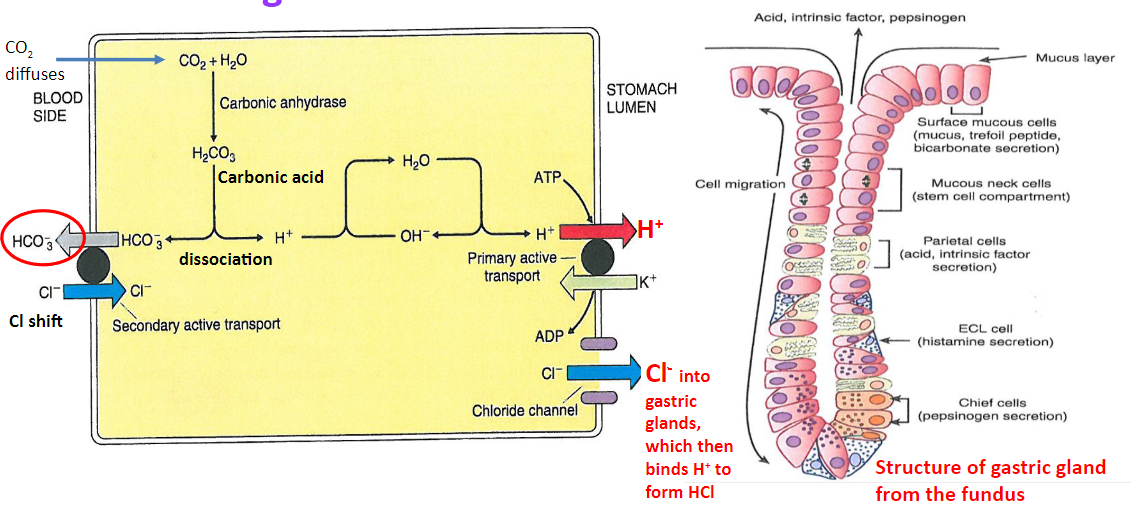
♪ HCO3- is exchanged for Cl- in the blood, leading to a decrease in the acidity of venous blood from the stomach
♪ Excess Cl- diffuses into the stomach through chloride channels, while H+ is pumped out into the stomach lumen by K+/H+-ATPase pumps
♪ The net effect is the secretion of HCl into the stomach lumen, contributing to the stomach's acidic environment
What are the components of gastric secretions? Elaborate on each:
♪ Resting juice: similar to plasma, secreted by non-parietal cells with high HCO3- content (~pH 7.4)
♪ Mucus: alkaline, thick, and sticky; forms a protective gel on the epithelial surface, containing high levels of HCO3- to neutralize acid
♪ Rennin (chymosin): curdles milk into casein clot; production replaced by pepsinogen
♪ Lipase: converts triglycerides into fatty acids and glycerol.
♪ Intrinsic factor: facilitates vitamin B12 absorption, preventing pernicious anaemia
♪ Gastric acid (HCl): kills bacteria, denatures food, activates pepsinogen to pepsin, promotes gastric lipase action, and stimulates pancreatic HCO3- secretion
What are the three phases involved in the secretion of gastric juice, particularly HCl secretion? (3)
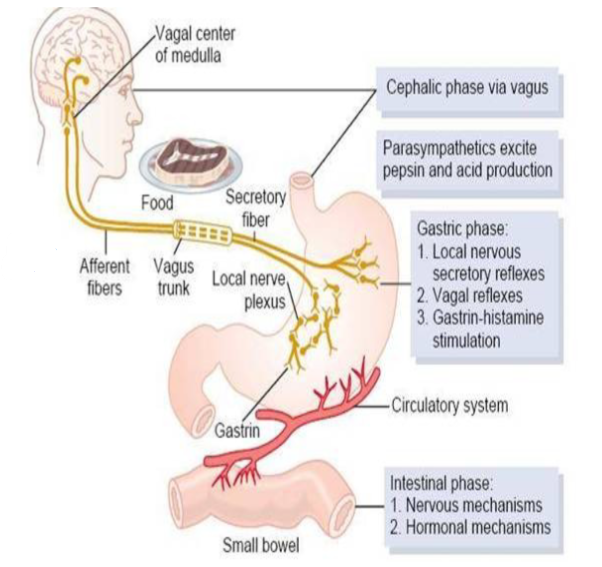
♪ Cephalic phase
♪ Gastric phase
♪ Intestinal phase
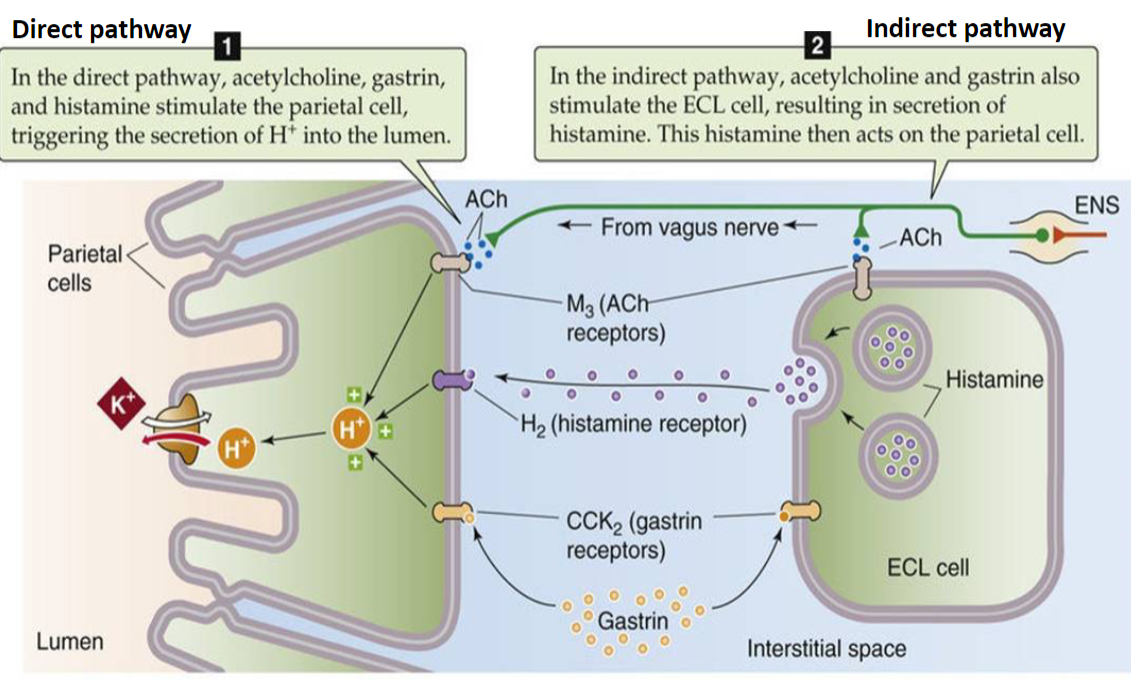
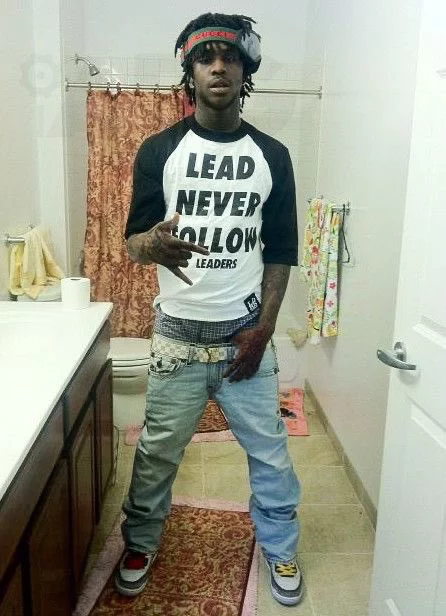
Each gastric secretion phase involves regulation by neuronal pathways and duodenal hormones, leading to increased acid secretion. This regulation can occur via what pathways? Elaborate on each: (2)
♪ Direct pathway: acting on parietal cells to increase acid secretion
♪ Indirect pathway: influencing the secretion of gastrin and histamine, which in turn increase acid secretion

How is gastric acid secretion regulated during the cephalic phase? (3)
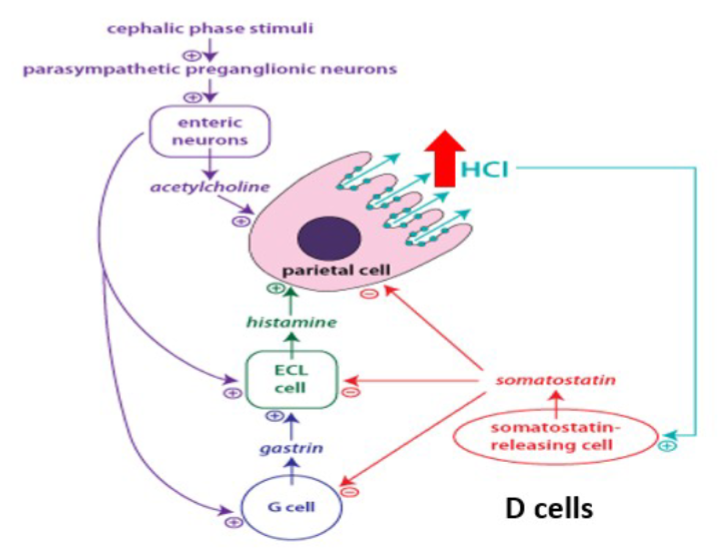
♪ACh (acetylcholine) stimulates histamine release from ECL (enterochromaffin-like) cells
♪ACh acts directly on parietal cells, leading to HCl secretion
♪Gastrin stimulates histamine release from ECL cells and acts directly on parietal cells to induce HCl secretion
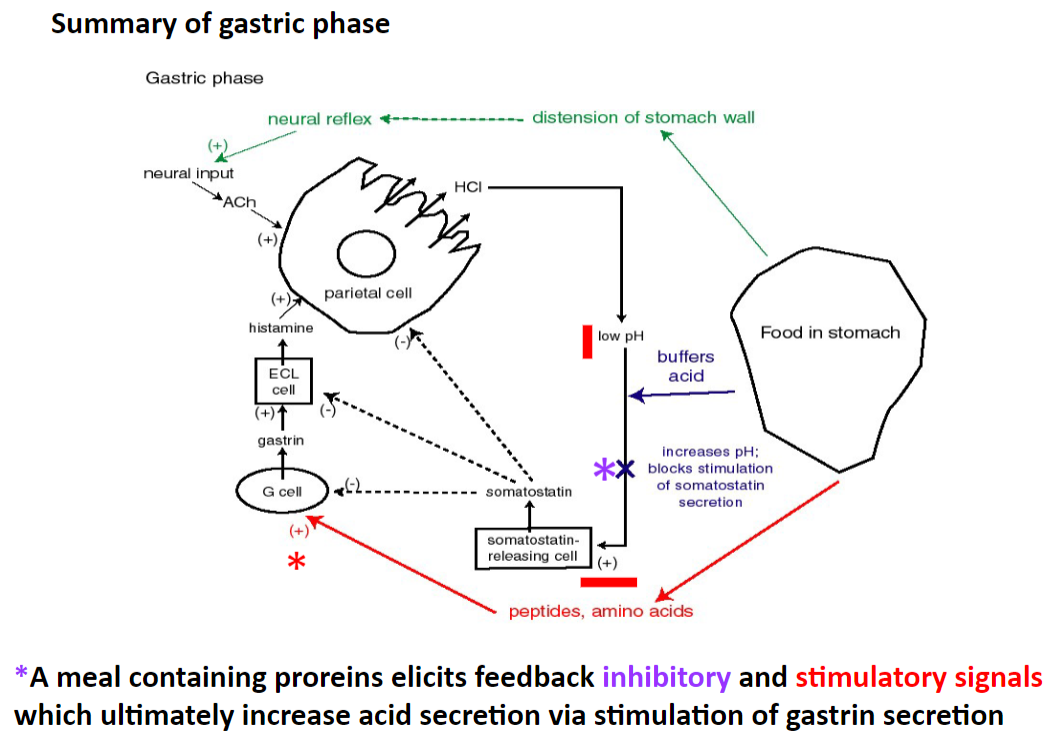
How is gastric acid secretion regulated during the gastric phase? (3)
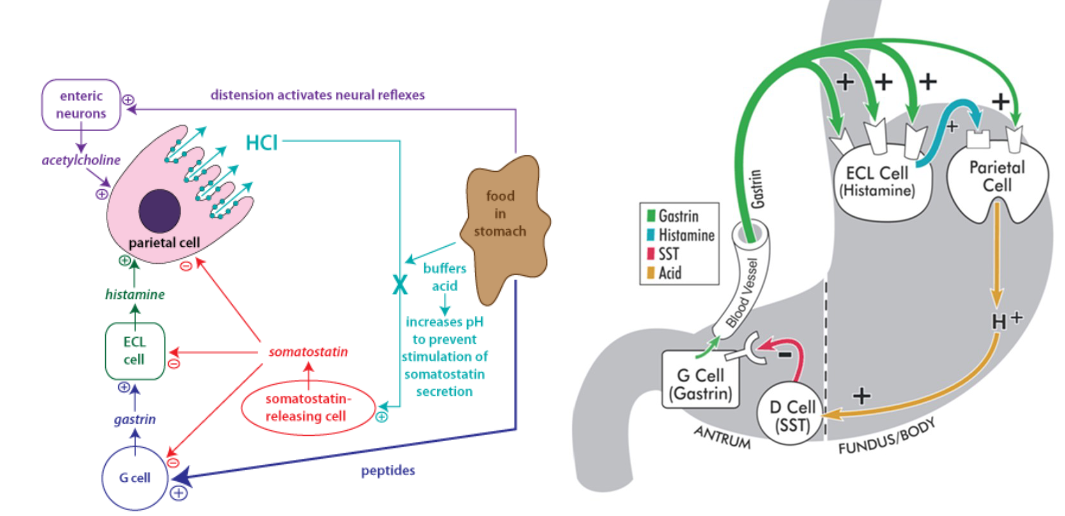
♪Gastric phase is triggered by distension of the stomach and increased peptide concentration, leading to increased acidity
♪Acid secretion decreases as the acidity of the lumen increases due to negative feedback mechanisms
♪Somatostatin inhibits gastrin-secreting cells (G cells), thereby reducing acid secretion
What effect does the protein content of a meal have on gastric acid secretion during the gastric phase? (3)
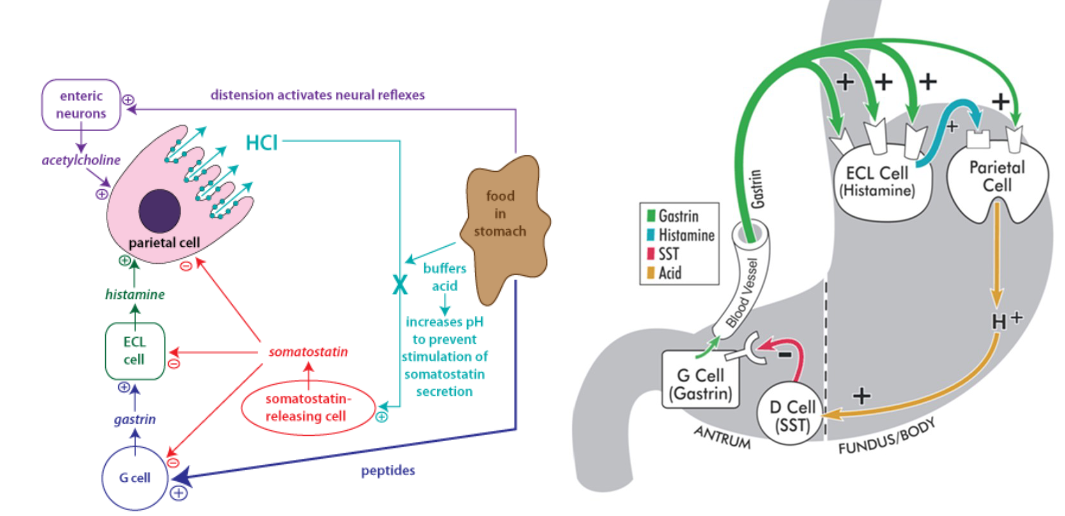
♪Proteins in the meal act as buffers in the gastric lumen, decreasing luminal acidity.
♪This reduction in luminal acidity leads to an increase in HCl secretion.
♪Mechanism: H+ ions bind to proteins, reducing the concentration of free H+ ions and acting as a buffer. This removes the inhibitory effect of HCl on gastrin secretion, leading to increased gastrin-mediated acid secretion
A picture demonstrating gastric acid secretion :Regulation
How does the intestinal phase regulate gastric acid secretion? (4)

♪The intestinal phase balances stomach secretions with the digestive and absorptive capacities of the small intestine
♪High acidity in the duodenum reflexively inhibits gastric acid secretion
♪Factors such as duodenal distension, hypertonic solutions, amino acids, fatty acids, and monosaccharides also inhibit acid secretion
♪Inhibition of acid secretion in the small intestine depends on the composition and volume of chyme, as well as duodenal distension
How is acid secretion inhibited during the intestinal phase? (2)
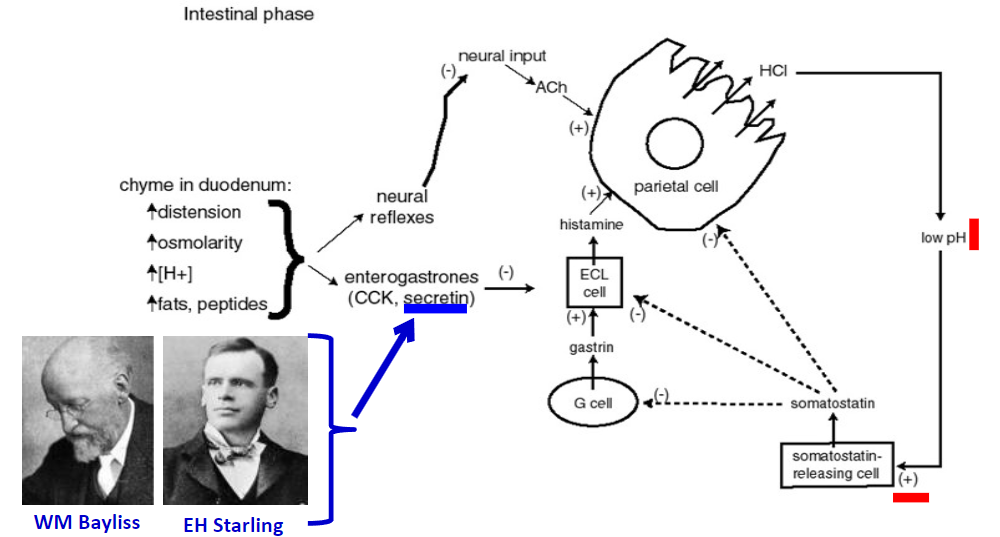
♪Short and long neuronal reflexes and hormones, such as enterogastrones (e.g., secretin, CCK), inhibit acid secretion by the parietal cells or gastrin secretion by the G cells
♪Somatostatin, produced in various locations including the stomach, intestine, delta cells of the pancreas, hypothalamus, brainstem, and hippocampus, also inhibits gastrin secretion
Picture summary of the Direct and indirect actions of the three acid secretagogues: ACh, gastrin, and histamine
What factors promote the secretion of hydrochloric acid (HCl) in the stomach? (10)
♪Histamine
♪Acetylcholine
♪Gastrin
♪Caffeine
♪Alcohol
♪NSAIDs
♪Nicotine
♪Helicobacter pylori infection
♪Zollinger-Ellison syndrome
♪Hyperparathyroidism.
Note: Avoid certain drugs like caffeine, alcohol, NSAIDs, and nicotine if you have a peptic ulcer.
What are the functions of hydrochloric acid (HCl) in the stomach? (5)
♪Defense: Kills germs
♪Protein digestion: Activates pepsinogen to pepsin, initiating protein digestion
♪Lack of HCl leads to failure of protein digestion (achlorhydria or hypochlorhydria)
♪Stimulates the flow of bile and pancreatic juice, which are rich in bicarbonate ions
♪Promotes the action of gastric lipase
What stimulates the secretion of pepsinogen in the stomach? (3)
♪Inputs to chief cells from nerve plexus
♪Parallels exist between gastric acid secretion and pepsinogen secretion
♪Stimulators/inhibitors of acid secretion during the cephalic and intestinal phases have the same effect on pepsinogen secretion
What stimulates the secretion of pepsinogen in the stomach? (4)
![<p>♪Pepsinogen is secreted by chief cells in its inactive form</p><p>♪Its activation occurs when the acidity level ([H+]) is high in the stomach lumen, altering its shape to expose its active site</p><p>♪This activation process is autocatalytic</p><p>♪Pepsinogen is inactivated upon entry of food into the small intestine, where bicarbonate (HCO3-) and peptides neutralize the acidity</p>](/flashcards/cardimage2/778f3b36/176/8176887_back.png)
♪Pepsinogen is secreted by chief cells in its inactive form
♪Its activation occurs when the acidity level ([H+]) is high in the stomach lumen, altering its shape to expose its active site
♪This activation process is autocatalytic
♪Pepsinogen is inactivated upon entry of food into the small intestine, where bicarbonate (HCO3-) and peptides neutralize the acidity
What are the functions of pepsin? (3)
♪Pepsin initiates the digestion of proteins by breaking them down into peptides
♪However, pepsin is not the only enzyme involved in protein digestion
♪Other enzymes that can digest proteins include trypsin, chymotrypsin, and elastase, which are produced in the pancreas and activated in the small intestine
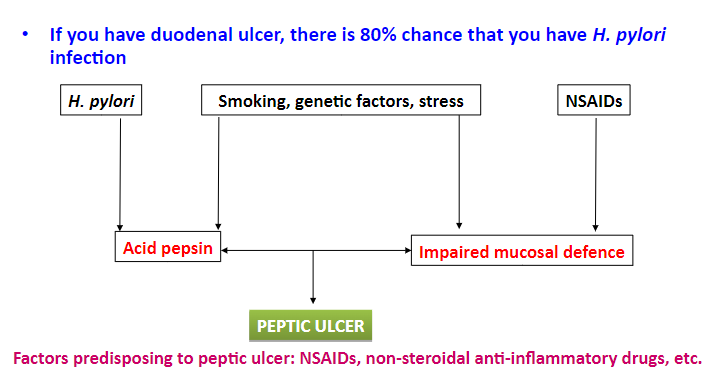
Picture demonstrating how NSAIDs (e.g. aspirin) play a role in gastric acid secretion disorders
What are the functions of HCl and pepsin? (3)
♪HCl kills aerobic microorganisms, reducing the risk of infection of the gastric mucosa
♪Pepsin initiates the digestion of proteins by breaking them down into peptides
♪Other factors that prevent infection of the gastric mucosa include mucus production, peristalsis and fluid movement, seamless epithelium with tight junctions, fast cell turnover, IgA secretion at mucosal surfaces, and the presence of Peyer's patches for protection
What protects the gastrointestinal tract (GIT) from the damaging effects of HCl? (4)
♪Factors such as mucus production, peristalsis, fluid movement, the presence of a seamless epithelium with tight junctions
♪Fast cell turnover
♪IgA secretion at mucosal surfaces
♪The presence of Peyer's patches help protect the GIT from the damaging effects of HCI
What are the protective factors that prevent autodigestion of the stomach by HCl and pepsin? (6)
The protective factors include:
♪Mucus layer protecting the gastric mucosa from low pH.
♪Secretion of alkaline mucus and bicarbonate ions.
♪Inhibition of gastrin release by somatostatin.
♪Presence of protein buffers.
♪Removal of excess H+ by epithelial cells.
♪Tight junctions preventing back diffusion of H+ ions.
How do non-steroidal anti-inflammatory drugs (NSAIDs) contribute to gastric mucosal damage? (2)
NSAIDs contribute to gastric mucosal damage by:
♪Inhibiting prostaglandin synthesis, reducing mucosal protection.
♪Increasing susceptibility to gastric erosion and ulcer formation.
How may elevated gastric acid secretion play a role in the pathogenesis of duodenal ulcers? (2)
Elevated gastric acid secretion can lead to duodenal ulcers by:
♪Damaging the duodenal mucosa.
♪Impairing the mucosal defence mechanisms.
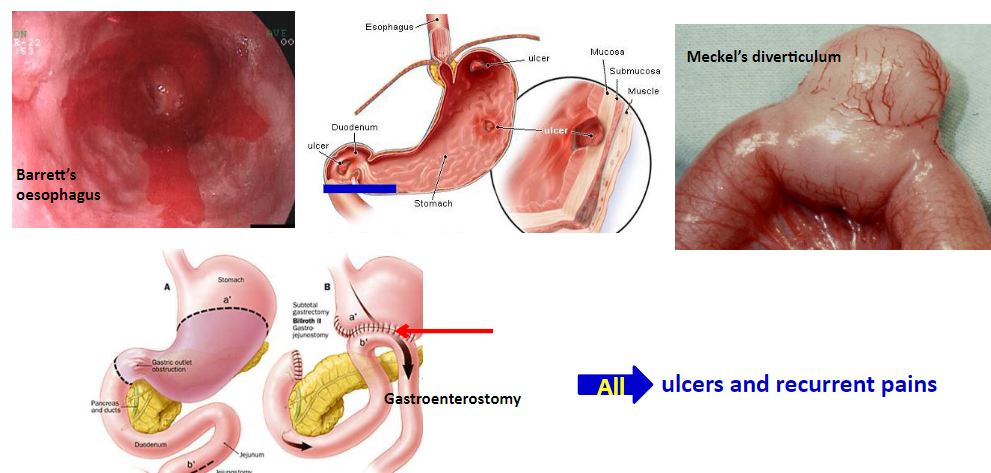
Where are peptic ulcers most commonly found in the alimentary tract? (2)
Peptic ulcers are commonly found in:
♪The stomach (gastric ulcers).
♪The duodenum (duodenal ulcers).
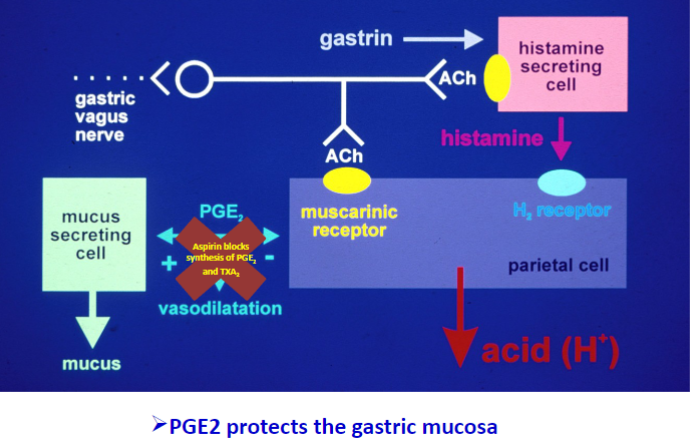
What are some factors to the formation of peptic ulcers? (2)
Factors to peptic ulcer formation include:
♪Lifestyle factors such as diet, smoking, and alcohol consumption.
♪Medical conditions like stress, chronic diseases, and genetic predisposition.
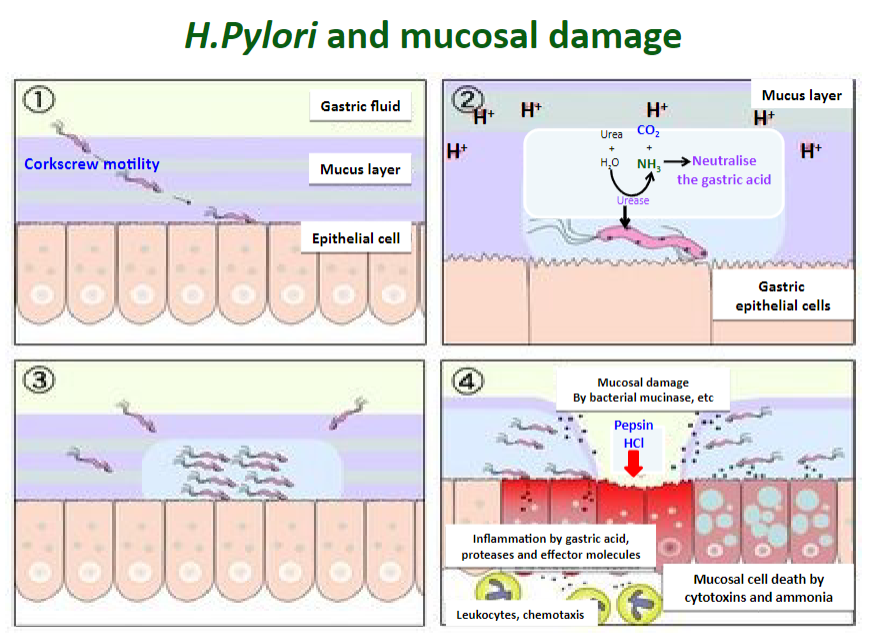
Describe the role of Helicobacter pylori in the pathogenesis of duodenal ulcers. (3)
Helicobacter pylori contributes to duodenal ulcer pathogenesis by:
♪Infecting the gastric mucosa.
♪Inducing inflammation and mucosal damage.
♪Increasing susceptibility to ulcer formation.

What are the predisposing factors to peptic ulcer formation? (3)
♪Gastric and duodenal infection with H. pylori is a major risk factor.
♪Environmental and host factors can determine the distribution and colonisation of H. pylori in the stomach.
♪If you have a duodenal ulcer, there is an 80% chance that you have H. pylori infection.
How do NSAIDs (e.g. aspirin) play a role in gastric acid secretion disorders? (5)
♪NSAIDs cause topical irritation of the gut and impair the barrier properties of the mucosa.
♪They suppress gastric prostaglandin (PG) synthesis, decrease gastric mucosal blood flow, and interfere with the repair of superficial injury.
♪NSAIDs also inhibit platelet aggregation.
♪The presence of acid in the stomach promotes NSAID-mediated gastric disorders by impairing the restitution process and inactivating fibroblast growth factor (FGF), which interferes with the haemostasis process.
What are the implications of gastric acid secretion disorders on gastrointestinal function? (5)
♪Gastric acid secretion disorders affect the gastrointestinal (GIT) function, which includes storage, secretion, digestion, absorption of nutrients, salts, water, metabolism, and elimination of (undigested) wastes.
♪Malformation of the GIT can lead to a decrease in the nutrient status of the individual.
♪Peptic ulcers affect approximately 10% of the population and can occur in various sites such as the esophagus, stomach, and duodenum.
♪Peptic ulcer formation involves the breakage of the mucosal barrier and an imbalance between protective and damaging factors of the GIT.
♪Tissues are exposed to the erosive effects of gastric acids (HCl), bile acids, and pepsin due to this imbalance, leading to ulceration.
What are the types of peptic ulcers, and what are their causes and outcomes? (3)
♪Types of peptic ulcers include those caused by hyperacidity and reflux of duodenal contents in the oesophagus, stomach, and duodenum.
♪Causes of peptic ulcers include hyperacidity, reflux of duodenal contents, presence of H. pylori (a risk factor for gastric cancer), NSAIDs, genetic factors, and male sex (there is a higher prevalence of peptic ulcers of men than women).
♪Outcome: Peptic ulcers can result in complete healing with tissue replacement and some scarring.
What are the characteristics and prevalence of chronic peptic ulcers? (4)
♪Chronic peptic ulcers are common and occur in the upper gastrointestinal tract, influenced by pepsin and HCl.
♪They are asymptomatic in over 80% of individuals, especially in people over 50 years old, with low incidence in young individuals.
♪Chronic peptic ulcers have a 90% incidence rate in developing countries.
♪Inflammation plays a key role in the disease process.
What are the characteristics and causes of acute peptic ulcers? (2)
♪Acute peptic ulcers are less frequent and typically develop from areas of corrosive gastritis in the oesophagus, stomach, or proximal duodenum, as well as severe stress or shock such as burns or trauma.
♪They result from acute hypoxia of the surface epithelium, which leads to ischaemia of the gastric mucosa.
What are the potential outcomes of acute peptic ulcers? (2)
♪Acute peptic ulcers can lead to severe bleeding.
♪They typically heal without scarring, distinguishing them from chronic peptic ulcers.
What are the virulence factors of Helicobacter pylori? (6)
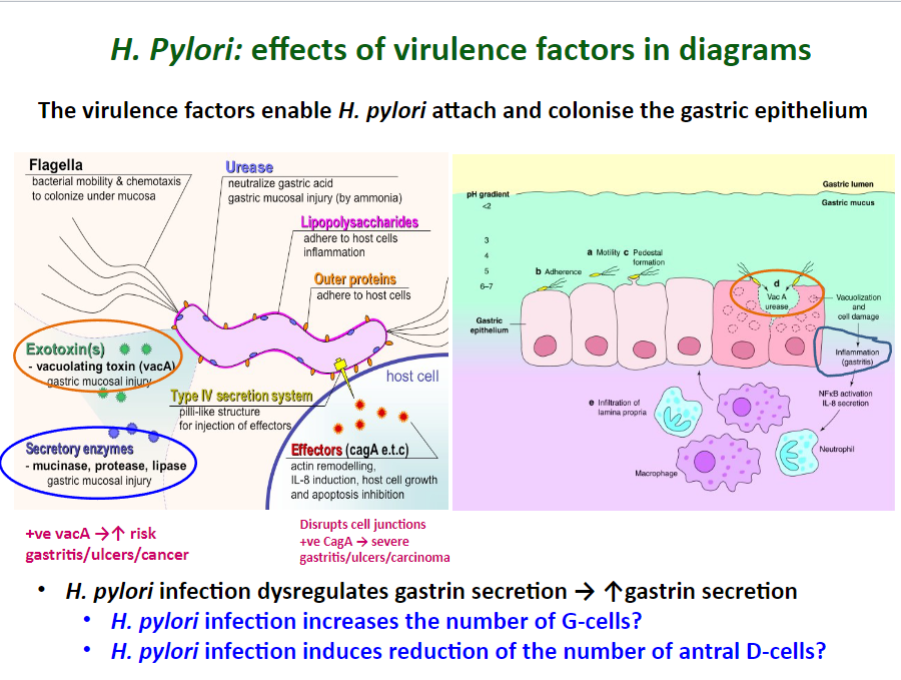
♪Motility: H. pylori possesses flagella that aid in its movement closer to the epithelium, where the pH is neutral (around 7).
♪Urease production: It produces urease, which converts urea to ammonia, buffering gastric acid and producing CO2.
♪Cytotoxin-associated antigen (CagA): CagA inserts pathogenicity islands and confers ulcer-forming potential.
♪Vacuolating toxin A (VacA): VacA alters the trafficking of intracellular proteins in gastric cells.
♪Other factors include a variety of outer membrane proteins such as adhesins (e.g., BabA), phospholipases, porins, iron transporters, and flagellum-associated proteins.
♪H. pylori is the most common cause of peptic ulcers and increases the risk of peptic ulcers by 10-20%.
Picture demonstrating H. Pylori: effects of virulence factors in diagrams:
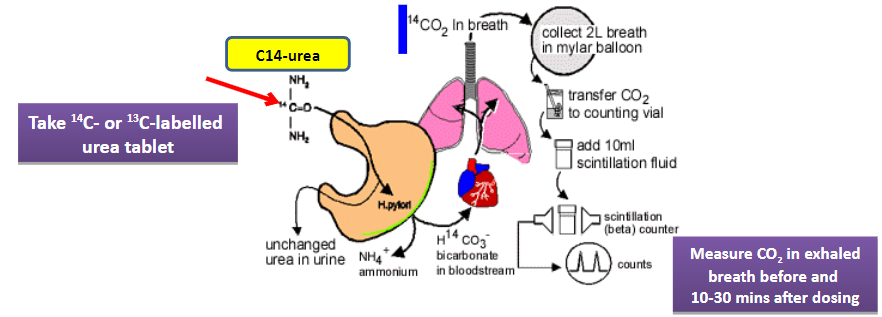
What are the diagnostic tests used for suspected peptic ulcers? (5)
♪Endoscopy (oesophagogastroduodenoscopy, EGD) allows direct visualization of the upper gastrointestinal tract.
♪Histological examination and staining of an EGD biopsy can provide detailed information about tissue abnormalities.
Tests for the presence of H. pylori include:
♪Stool antigen test
♪Evaluation of urease activity
♪Urea breath test
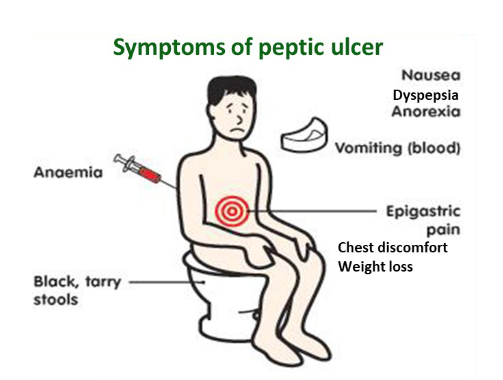
What are the complications associated with peptic ulcers? (5)
♪Haemorrhage (GI bleeding)
♪Perforation leading to peritonitis
♪Penetration, which may affect adjacent organs such as the liver and pancreas
♪Narrowing of the pyloric canal or oesophageal stricture
♪Increased likelihood of malignant transformation, especially with H. pylori infection