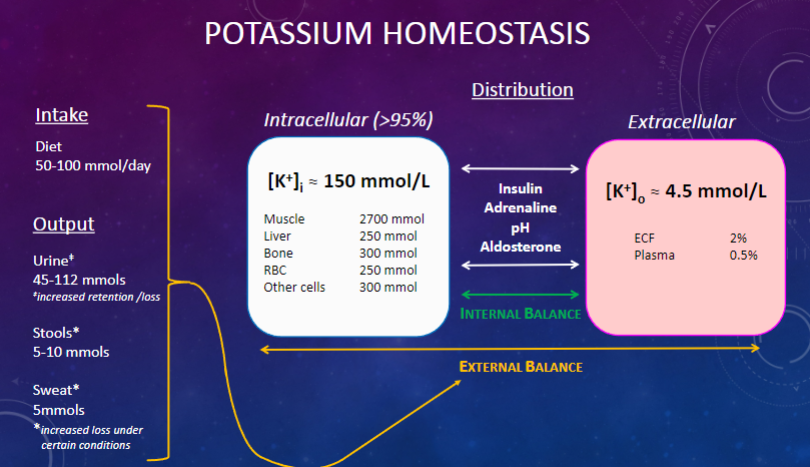
Picture demonstrating potassium homeostasis:
What is the focus of acute potassium regulation? (1)
✿ Distribution of potassium (K+) between intra- and extra-cellular fluid compartments.
How is acute potassium regulation described in terms of internal balance? (1)
Acute regulation largely involves maintaining internal K+ balance.
What is the primary mechanism of chronic potassium regulation? (1)
✿ Chronic regulation is primarily achieved by the kidney adjusting K+ excretion and reabsorption.
How is chronic potassium regulation described in terms of external balance? (1)
✿ Chronic regulation mainly involves the "output part" of external K+ balance.
What are the functions of potassium in the body? (3)
✿ Determines intracellular fluid osmolality, affecting cell volume.
✿ Determines resting membrane potential (RMP), crucial for the normal functioning of excitable cells such as myocytes, cardiomyocytes, and neurons.
✿ Affects vascular resistance.
Where is the majority of bodily potassium (K+) located? (1)
Intracellularly, accounting for over 95% of total potassium.
What percentage of bodily potassium (K+) is found in the extracellular fluid (ECF)? (1)
Only 2.5% of bodily potassium is found in the extracellular fluid (ECF).
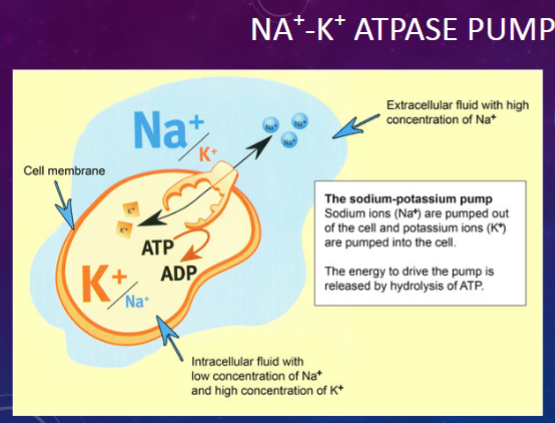
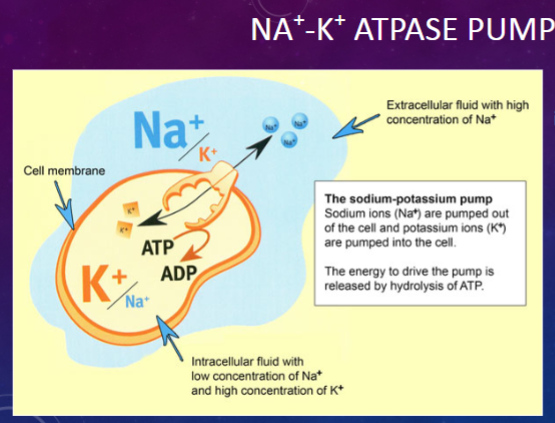
What is the role of the Na+/K+ ATPase pump? (1)
![<p>✿ The Na+/K+ ATPase pump maintains a <span class="tt-bg-yellow">high</span> intracellular concentration of <span class="tt-bg-yellow">potassium</span> ([K+]) and a <span class="tt-bg-blue">low</span> intracellular concentration of <span class="tt-bg-blue">sodium</span> ([Na+]).</p>](/flashcards/cardimage2/10be9ece/254/8254837_back.png)
✿ The Na+/K+ ATPase pump maintains a high intracellular concentration of potassium ([K+]) and a low intracellular concentration of sodium ([Na+]).
How does the extracellular fluid (ECF) pool respond to changes in body potassium (K+) distribution? (1)
✿ The ECF pool will change more dramatically with changes in body K+ distribution.
What happens to plasma [K+] after a meal, and what is its subsequent effect? (1)
✿ After a meal, there is a slight increase in plasma [K+], which is shifted into the intracellular fluid (ICF) compartment.
What are the primary factors controlling the shift of potassium (K+) between plasma and intracellular compartments? (1)
The shift is mainly subject to hormonal control, including insulin, adrenaline, aldosterone, and pH changes.
Why is it crucial for plasma [K+] to remain in the right range? (1)
✿ It is very important for plasma [K+] to remain in the right range for proper physiological function.
How is hyperkalemia clinically defined? (1)
Hyperkalemia is defined as plasma [K+] greater than 5.5mM.
How is hypokalemia clinically defined? (1)
Hypokalemia is defined as plasma [K+] less than 3.5mM.
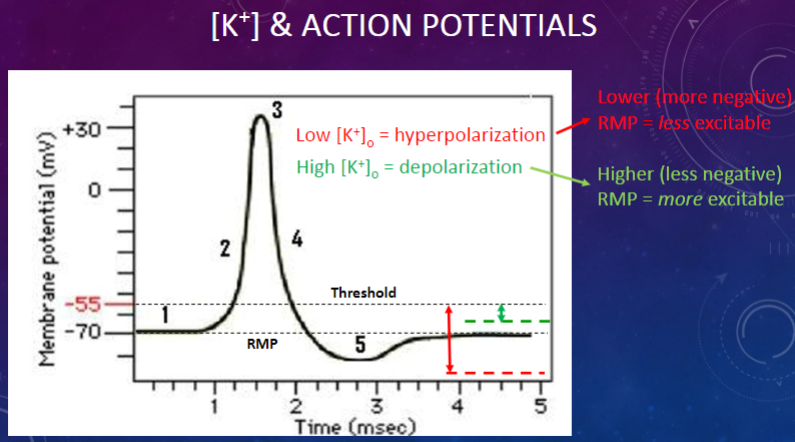
How is the resting membrane potential (RMP) formed? (1)
✿ The resting membrane potential (RMP) is formed by the creation of ionic gradients, which is a combination of chemical and electrical gradients.
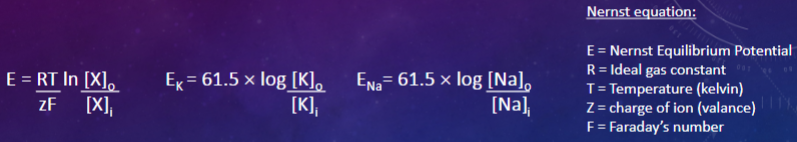
Picture demonstrating Nernst equation:
How is the normal resting membrane potential (RMP) maintained? (1)
The normal resting membrane potential (RMP) is maintained by a dynamic balance between sodium (Na+) and potassium (K+) concentrations.
What occurs when plasma [K+] is altered above or below normal levels? (1)
Alterations in plasma [K+] above or below normal levels can impact the resting membrane potential (RMP) and cellular function.
What are the normal potassium concentrations ([K]o and [K]i), and the resulting equilibrium potential (EK)? (1)
Normal: [K]o = 4.5mM and [K]i = 140mM ⇒ EK = -91.8 mV
What are the potassium concentrations ([K]o and [K]i) and the resulting equilibrium potential (EK) during hyperkalemia? (1)
Hyperkalemia: [K]o = 7mM and [K]i = 140mM ⇒ EK = -80 mV
What are the potassium concentrations ([K]o and [K]i), and the resulting equilibrium potential (EK) during hypokalemia? (1)
Hypokalemia: [K]o= 1.5mM and [K]I = 140mM ⇒ EK = -121.5 mV
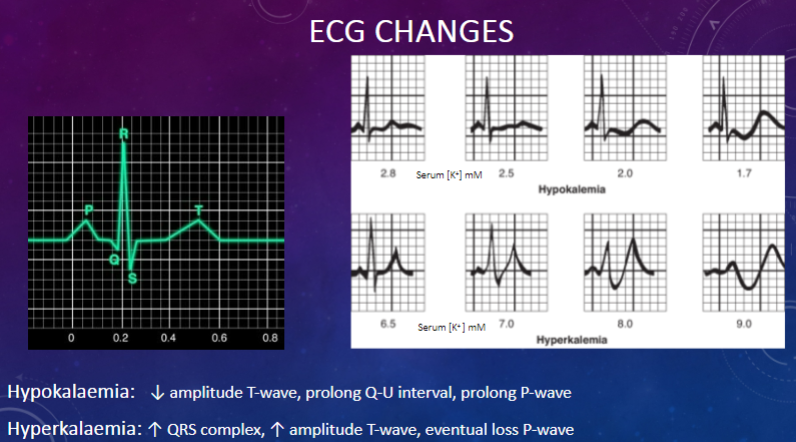
How can alterations in potassium levels affect cardiomyocyte membrane potential and ECG? (1)
Alterations in potassium levels can severely affect cardiomyocyte membrane potential, producing characteristic changes in the electrocardiogram (ECG).
Picture demonstrating ECG changes:
Picture demonstrating [K+] and Action potentials:
What are the potential causes of hypokalemia? (5)
Hypokalemia can be caused by renal or extra-renal loss of potassium (K+) or by restricted intake, such as:
✿ Long-standing use of diuretics without potassium chloride (KCl) compensation
✿ Hyperaldosteronism/Conn’s Syndrome (increased aldosterone secretion)
✿ Prolonged vomiting leading to sodium (Na+) loss and increased aldosterone secretion, resulting in potassium (K+) excretion in the kidneys
✿ Profuse diarrhea (diarrhea fluid contains 50 mM K+)
What are the consequences of hypokalemia? (1)
Hypokalemia results in a decrease in resting membrane potential and a decrease in the release of adrenaline, aldosterone, and insulin.
What are the potential causes of hyperkalemia? (4)
Hyperkalemia can be caused by various disease states and factors, including:
✿ Insufficient renal excretion
✿ Increased release from damaged body cells (e.g., during chemotherapy, long-lasting hunger, prolonged exercise, or severe burns)
✿ Long-term use of potassium-sparing diuretics
✿ Addison’s disease (adrenal insufficiency)
What are the potential consequences of severe hyperkalemia? (1)
Severe hyperkalemia, with plasma [K+] > 7mM, can be life-threatening, leading to asystolic cardiac arrest.
How is hyperkalemia managed acutely? (2)
Acute management of hyperkalemia may involve insulin/glucose infusion to drive potassium (K+) back into cells.
Insulin is particularly important, although the mechanism is unclear; it may stimulate the Na-K-ATPase. Glucose is given with insulin to facilitate its entry into cells and provide energy.
Which hormones, besides insulin, stimulate the Na+-K+ pump, leading to increased cellular K+ influx? (1)
Other hormones such as aldosterone and adrenaline stimulate the Na+-K+ pump, resulting in increased cellular K+ influx.
How is external potassium (K+) balance primarily maintained in a healthy person? (1)
External K+ balance is primarily maintained by the kidney in a healthy individual.
Is potassium (K+) excretion in the stools under regulatory control? (1)
K+ excretion in the stools is not under regulatory control, meaning that large amounts can be lost by extra-renal routes.
Why is the maintenance of normal potassium (K+) homeostasis increasingly important in the therapy of cardiovascular disease (CVD)? (1)
The maintenance of normal potassium (K+) homeostasis is becoming an increasingly important limiting factor in the therapy of cardiovascular disease (CVD).
How do drugs like β-blockers and ACE inhibitors affect serum [K+]? (1)
Drugs like β-blockers and ACE inhibitors can increase serum [K+], thereby increasing the risk of hyperkalemia.
How do loop diuretics, used to treat heart failure, affect serum [K+]? (1)
Loop diuretics, used to treat heart failure, can increase the risk of hypokalemia.
What is the evolutionary adaptation of human kidneys regarding sodium (Na+) and potassium (K+)? (1)
Human kidneys have evolved to conserve sodium (Na+) and excrete potassium (K+).
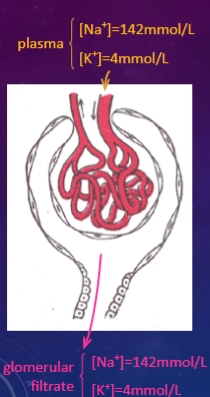
How are sodium (Na+) and potassium (K+) handled at the glomeruli? (1)
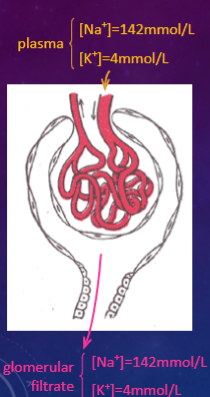
Sodium (Na+) and potassium (K+) are filtered freely at the glomeruli.
What is the relationship between plasma and glomerular filtrate (GF) concentrations of sodium (Na+) and potassium (K+)? (1)
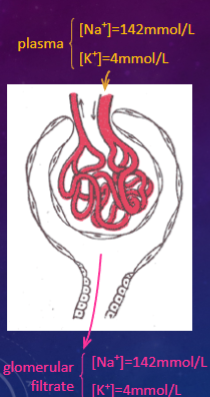
Plasma and glomerular filtrate (GF) have the same concentrations of sodium (Na+) and potassium (K+).
How much sodium (Na+) and potassium (K+) does the entire glomerular filtrate contain in a 24-hour period? (2)
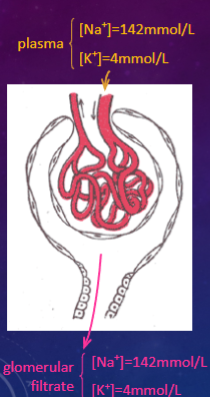
In a 24-hour period, the entire glomerular filtrate (~180 liters) contains approximately:
✿ 25 moles of sodium (Na+) (equivalent to 1.5 kg of NaCl)
✿ 0.7 moles of potassium (K+) (equivalent to 50 g of KCl)
What percentage of sodium (Na+) and potassium (K+) is reabsorbed in the proximal convoluted tubule (PCT)? (1)
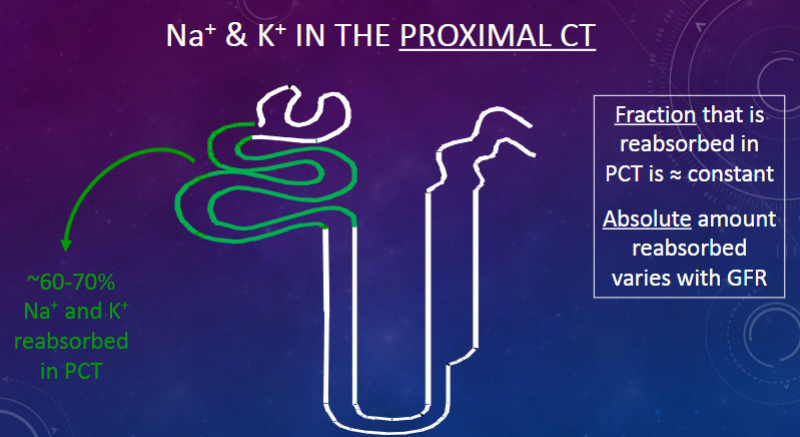
Approximately 60-70% of sodium (Na+) and potassium (K+) are reabsorbed in the proximal convoluted tubule (PCT).
How does the fraction of sodium (Na+) and potassium (K+) reabsorbed in the PCT vary? (1)
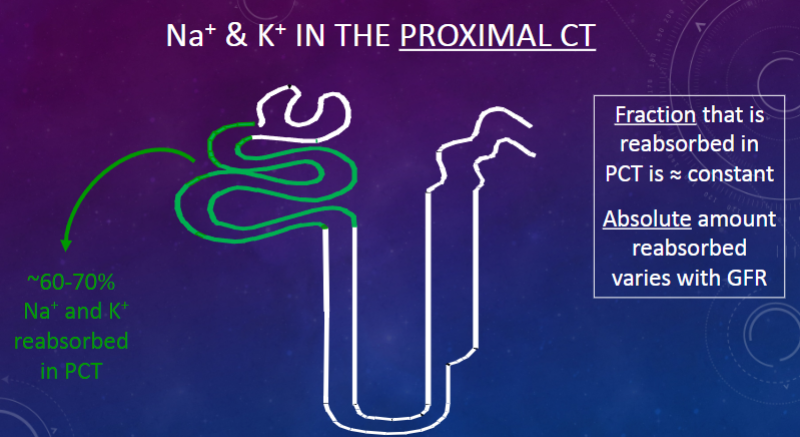
The fraction of sodium (Na+) and potassium (K+) reabsorbed in the PCT is approximately constant.
How does the absolute amount of sodium (Na+) and potassium (K+) reabsorbed in the PCT vary? (1)
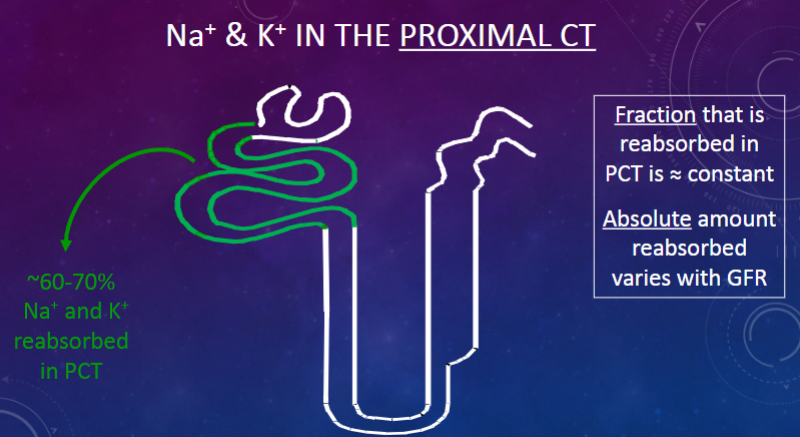
While the fraction remains constant, the absolute amount of sodium (Na+) and potassium (K+) reabsorbed in the PCT varies with glomerular filtration rate (GFR).
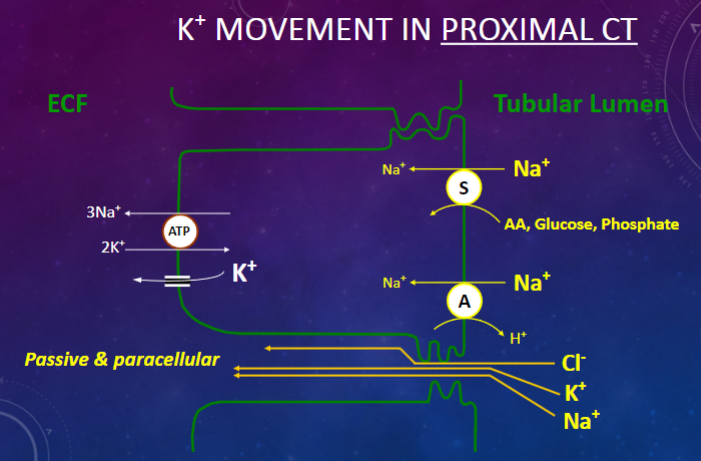
Picture demonstrating K+ Movement in the Proximal Convoluted Tubule:
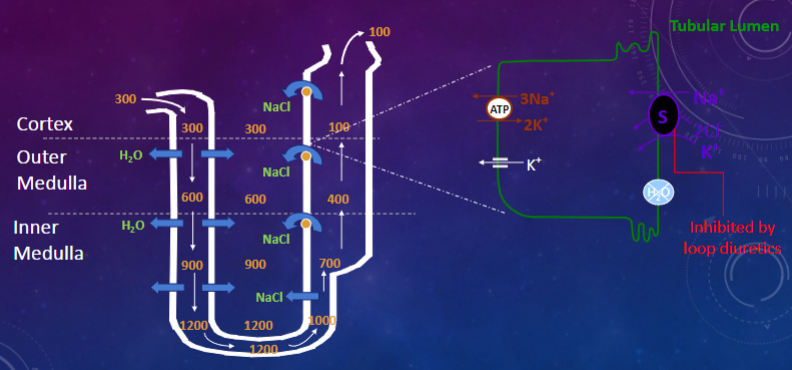
Picture demonstrating NA+/K+ Movement in the Loop of Henle:
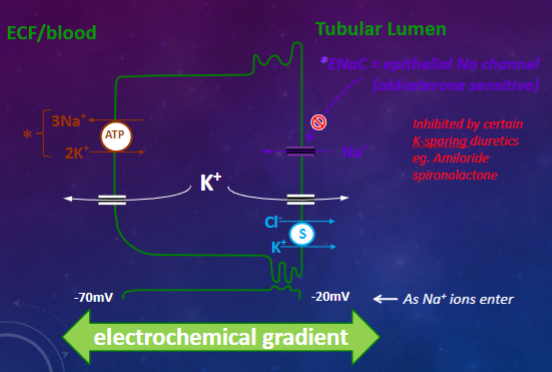
Picture demonstrating K+ Movement in the Distal Convoluted Tubule:
What percentage of filtered potassium (K+) is reabsorbed in the proximal convoluted tubule (PCT) and the loop of Henle (LoH)? (1)
Greater than 90% of filtered potassium (K+) is reabsorbed in the proximal convoluted tubule (PCT) and the loop of Henle (LoH)
How is the excretion of potassium (K+) into urine controlled in the case of potassium overload? (1)
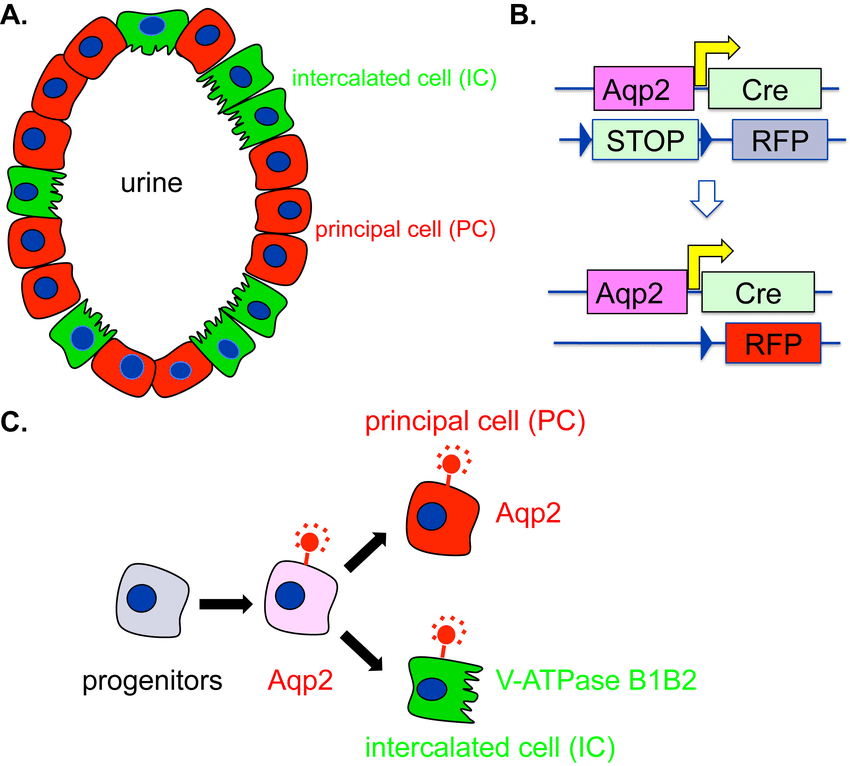
The excretion of potassium (K+) into urine during potassium overload is controlled by potassium (K+) secretion by principal cells of the late distal convoluted tubule (DCT) and the collecting duct (CD).
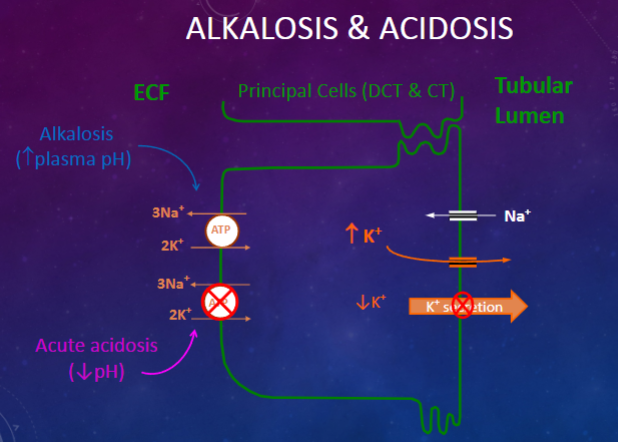
What factors determine potassium (K+) secretion in the distal convoluted tubule (DCT)? (1)
Potassium (K+) secretion in the DCT is determined by factors such as increased K+ intake and changes in blood pH. Alkalosis leads to increased excretion of K+, resulting in decreased serum [K+], while acute acidosis leads to decreased excretion of K+, resulting in increased serum [K+].
How is potassium (K+) secretion achieved in the DCT? (3)
Potassium (K+) secretion in the DCT is achieved through:
✿ Activity of the Na-K-ATPase pump
✿ Electrochemical gradient
✿ Permeability of the luminal membrane channel
How does an increase in plasma potassium (K+) concentration affect K+ secretion? (3)
![<p><u>An increase in plasma potassium (K+) concentration increases K+ secretion in three ways:</u></p><p>✿ <span class="tt-bg-yellow">Slows exit from the basolateral membrane,</span> leading to an increase in intracellular potassium concentration ([K+]i) and creating a cell-lumen concentration gradient.</p><p>✿ Increases the activity of the Na+/K+ ATPase, resulting in an increase in intracellular potassium concentration ([K+]i).</p><p>✿ <span class="tt-bg-green">Stimulates aldosterone secretion.</span></p>](/flashcards/cardimage2/3b44a48a/254/8254948_back.png)
An increase in plasma potassium (K+) concentration increases K+ secretion in three ways:
✿ Slows exit from the basolateral membrane, leading to an increase in intracellular potassium concentration ([K+]i) and creating a cell-lumen concentration gradient.
✿ Increases the activity of the Na+/K+ ATPase, resulting in an increase in intracellular potassium concentration ([K+]i).
✿ Stimulates aldosterone secretion.
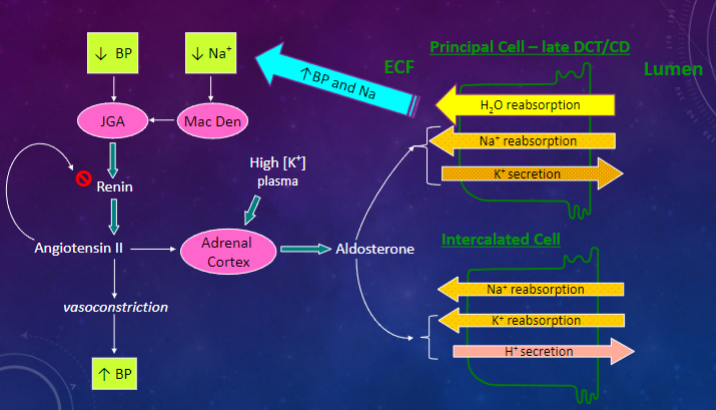
What is the major regulator of potassium balance in the body? (1)
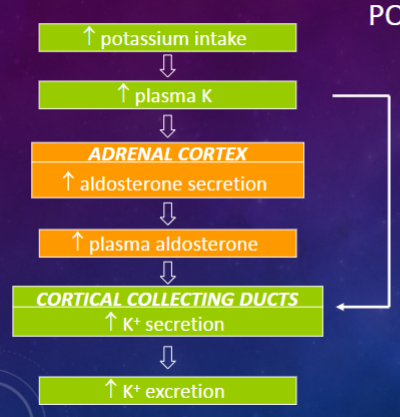
Aldosterone is the major regulator of potassium balance in the body.
How does aldosterone act to regulate potassium balance? (4)
![<p><u>Aldosterone acts to:</u></p><p>✿ <span class="tt-bg-green">Increase the activity of the Na+/K+ pump</span>, resulting in increased potassium (K+) influx and intracellular potassium concentration ([K+]i), establishing a cell-lumen concentration gradient.</p><p>✿<span class="tt-bg-green"> Increase the number of </span>epithelial sodium channels <span class="tt-bg-green">(ENaC)</span>, leading to increased sodium (Na+) reabsorption, reduced cell negativity, increased lumen negativity, and establishment of a voltage gradient.</p><p>✿ Redistribute ENaC from intracellular localization to the membrane.</p><p>✿Increase the permeability of the luminal membrane to potassium (K).</p>](/flashcards/cardimage2/48e368f0/254/8254956_back.png)
Aldosterone acts to:
✿ Increase the activity of the Na+/K+ pump, resulting in increased potassium (K+) influx and intracellular potassium concentration ([K+]i), establishing a cell-lumen concentration gradient.
✿ Increase the number of epithelial sodium channels (ENaC), leading to increased sodium (Na+) reabsorption, reduced cell negativity, increased lumen negativity, and establishment of a voltage gradient.
✿ Redistribute ENaC from intracellular localization to the membrane.
✿Increase the permeability of the luminal membrane to potassium (K).
Picture demonstrating Alkalosis and Acidosis:
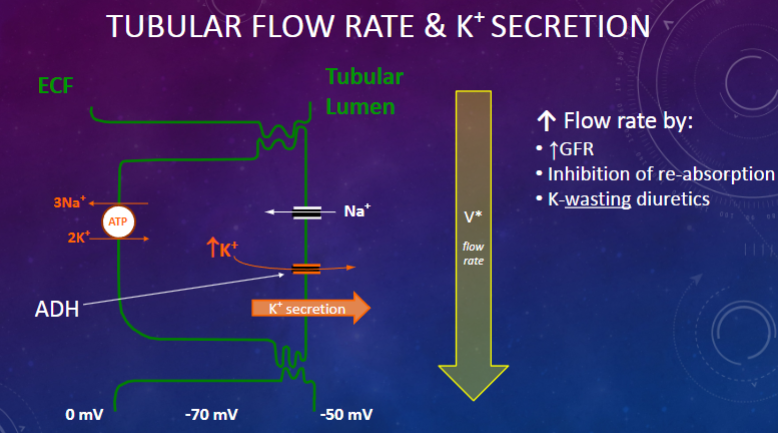
Picture demonstrating Tubular flow rate and K+ Secretion:
Picture demonstrating the reabsorption of K+ in severe Hypokalemia:
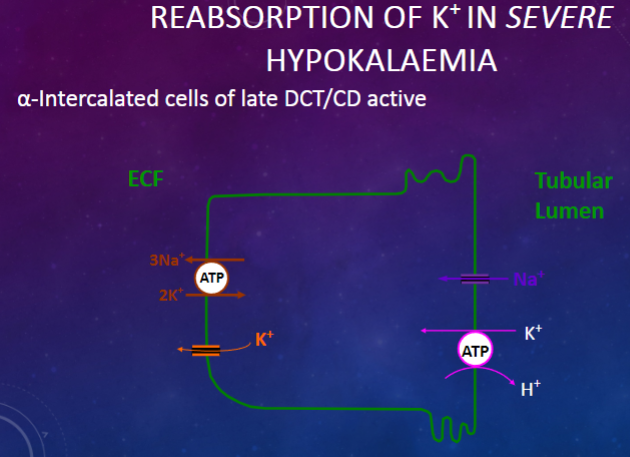
What cells are active in the reabsorption of potassium (K+) during severe hypokalemia? (1)
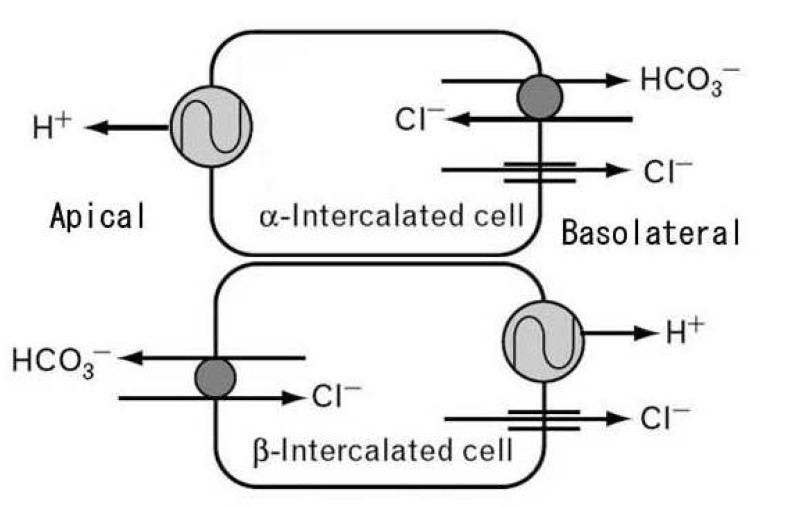
α-Intercalated cells of the late distal convoluted tubule (DCT) and collecting duct (CD) are active in the reabsorption of potassium (K+) during severe hypokalemia.
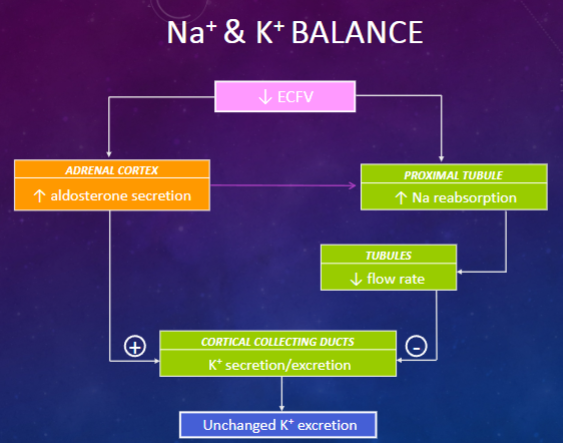
What potential problem arises from the dependence of potassium secretion on sodium and flow rate? (1)
Coupling potassium (K+) excretion to distal flow rate could jeopardize potassium balance.
Picture demonstrating Na+ and K+ Balance
Picture demonstrating the roles of the Renin-Angiotensin-Aldosterone system:
What hormones are produced by the adrenal cortex? (3)
The adrenal cortex produces:
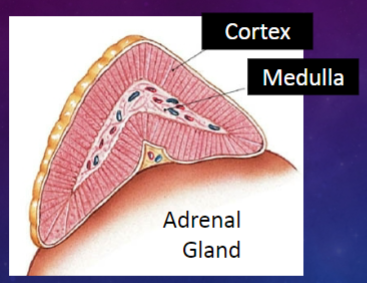
Glucocorticoid hormones (e.g., cortisol)
Sex hormones (androgens and estrogens)
Mineralocorticoid hormones (e.g., aldosterone)
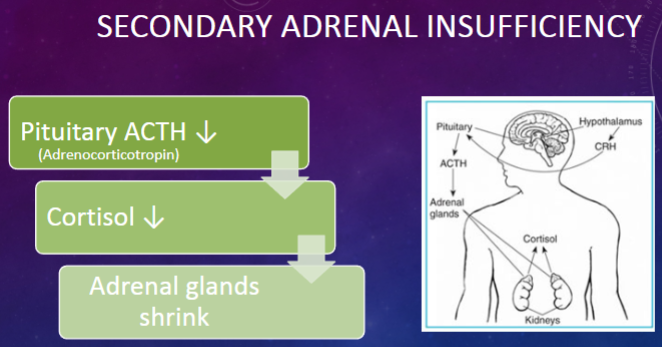
What is Addison's disease? (1)
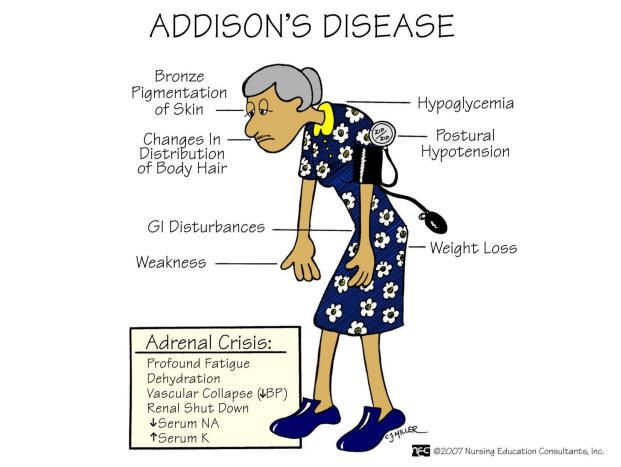
Addison's disease is a condition characterized by primary adrenal insufficiency, which is rare compared to secondary adrenal insufficiency. It involves damage to the adrenal cortex, resulting in significantly decreased hormone production and numerous symptoms.
How does Addison's disease affect aldosterone levels and electrolyte balance? (1)
Addison's disease results in a deficiency of aldosterone, leading to the body secreting large amounts of sodium (Na+), low serum sodium levels, retention of potassium (K+), and hyperkalemia.
What is the usual treatment for Addison's disease? (1)
The usual treatment for Addison's disease involves corticosteroid (steroid) replacement therapy for life.
Picture demonstrating Secondary Adrenal Insufficiency:
What is Conn's Syndrome, also known as primary aldosteronism? (1)
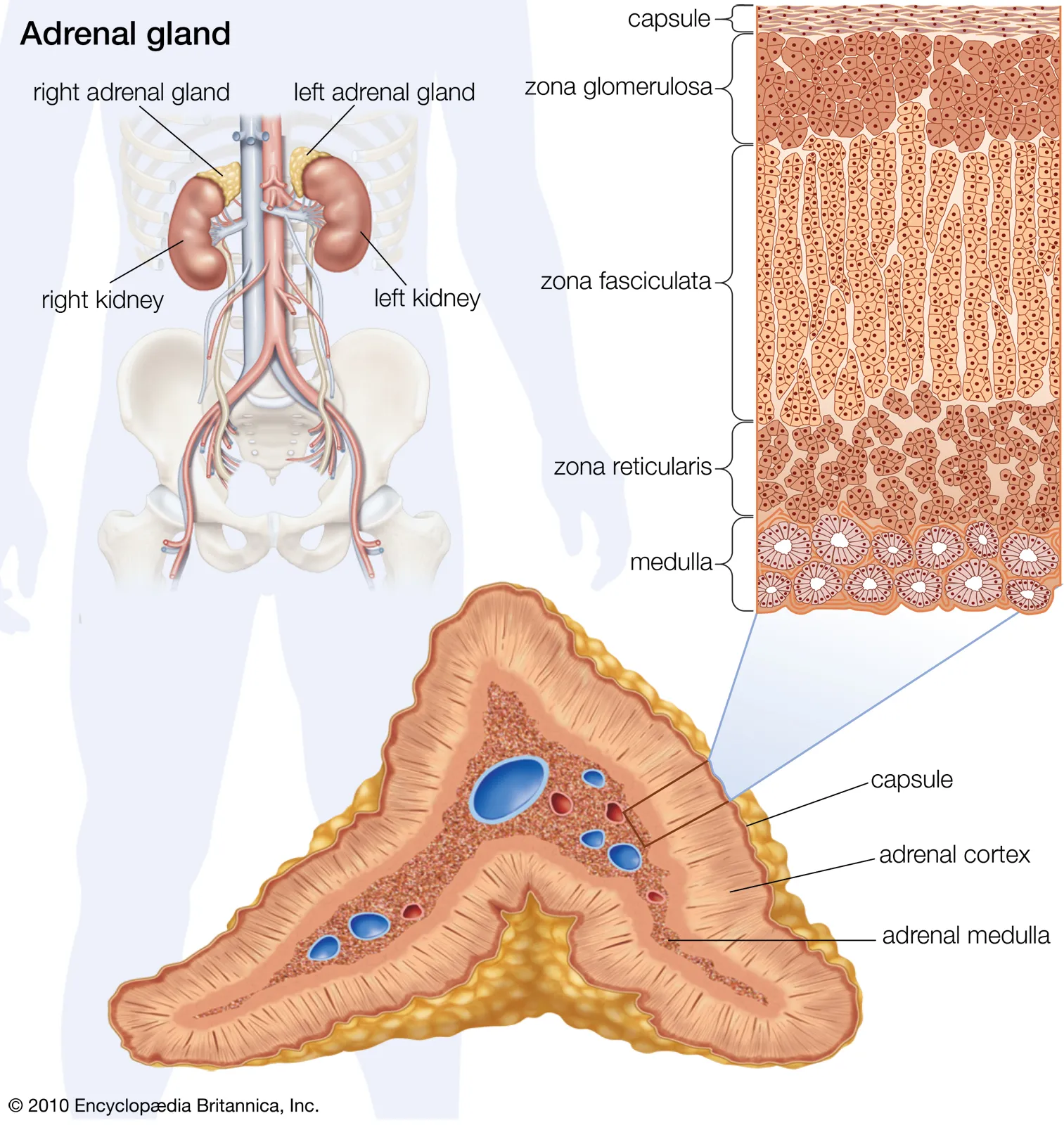
✿ Conn's Syndrome, also known as primary aldosteronism, is characterized by excess release of aldosterone due to an aldosterone-producing adenoma of the adrenal gland zona glomerulosa.
✿ These adenomas are typically less than 3cm in size, unilateral, and renin-unresponsive.
What causes hyperaldosteronism in chronic diseases? (1)
Hyperaldosteronism, characterized by excess release of aldosterone, can result from a variety of chronic diseases. Most commonly (50-60% of cases), it is due to Conn's syndrome, while the remaining 40-50% are due to bilateral adrenal hyperplasia.
How does aldosterone release occur in Conn's Syndrome? (1)
In Conn's Syndrome, aldosterone is released in the absence of stimulation by angiotensin II.
What are the effects of increased plasma aldosterone in Conn's Syndrome? (1)
In Conn's Syndrome, there is a significant increase in plasma aldosterone levels, leading to stimulation of sodium (Na+) reabsorption and potassium (K+) excretion by the kidneys. This results in the development of hypertension, increased fluid volume, and electrolyte imbalances such as hypokalemia, hypernatremia, and alkalosis.
How does Conn's Syndrome contribute to hypertension? (1)
Conn's Syndrome leads to hypertension due to increased blood pressure (bp) and sodium delivery to the macula densa, resulting in decreased release of renin. This creates a renin-independent cause of hypertension, making it very difficult to control.
What are the treatment options for Conn's Syndrome? (1)
Treatment options for Conn's Syndrome include surgical removal of the tumor-containing adrenal gland and controlling hypertension and hypokalemia with potassium-sparing agents such as spironolactone.