What is the myometrium and what is its function? (2)
The myometrium is the smooth muscle layer(s) of the uterus.
It plays a crucial role in uterine contractions during labor and menstruation.
What are gap junctions and what do they do? (2)
Gap junctions are connections between cells that allow the transfer of electrical signals.
They enable coordinated contractions in the uterus.
What are voltage-gated calcium channels (VGCC), and why are they important in uterine function? (3)
VGCC are channels that open in response to changes in membrane potential, allowing calcium ions to enter cells.
Calcium influx through VGCC is essential for uterine muscle contraction.
This process is involved in labor and menstrual cycles.
What is ergometrine and how does it affect the uterus? (2)

Ergometrine is a potent uterine contractor found in ergot.
It induces strong uterine contractions and is used to control postpartum hemorrhage.
What is a functional syncytium, and how is it relevant to uterine function? (2)
A functional syncytium is a mass of cells that function as one.
In the uterus, the myometrium forms a functional syncytium to allow coordinated contractions during labor.
What are the main components of the smooth muscle in the myometrium? (3)
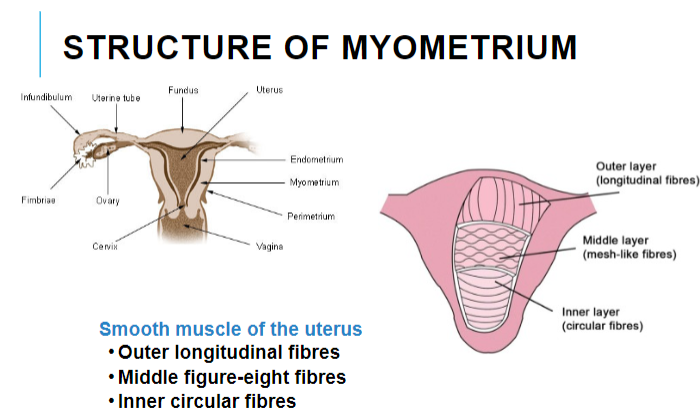
The myometrium consists of three main muscle fiber orientations:
Outer longitudinal fibers
Middle figure-eight fibers
Inner circular fibers
What is the function of the outer longitudinal fibers in the myometrium? (2)
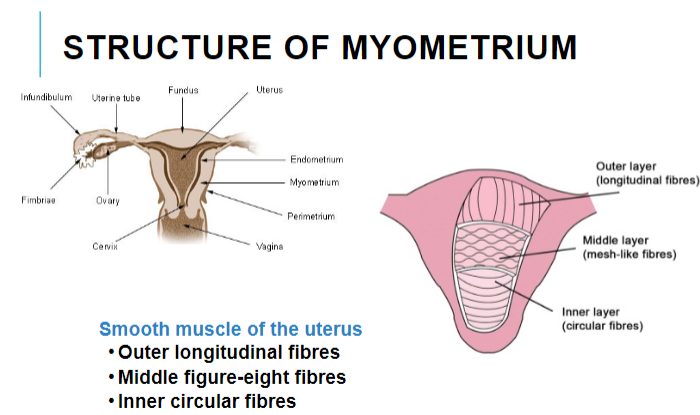
The outer longitudinal fibers help with the overall shortening of the uterus during contractions.
They assist in facilitating the expulsion of the fetus during labor.
What is the role of the middle figure-eight fibers in the myometrium? (2)
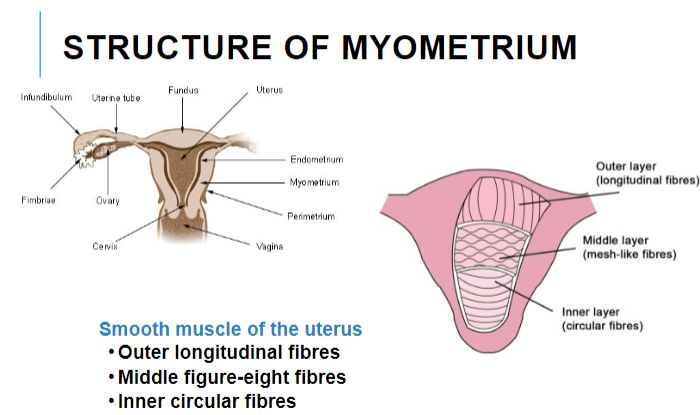
The middle figure-eight fibers help coordinate the contractions of the uterus by forming a lattice-like structure.
They play a role in both the squeezing and relaxing of the uterus during contractions.
What is the purpose of the inner circular fibers in the myometrium? (2)
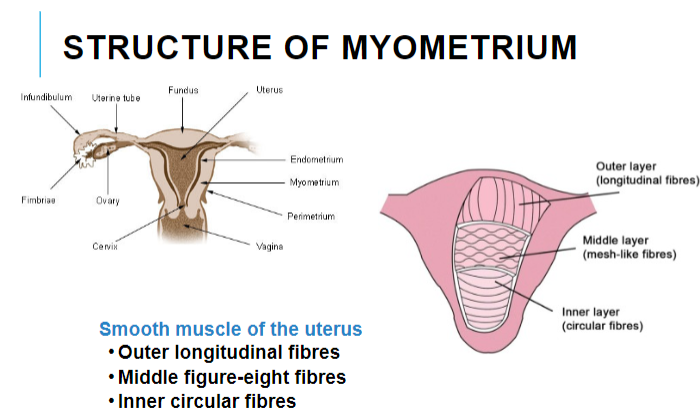
The inner circular fibers help regulate the tightness of the uterus during contractions.
They also assist in controlling the passage of the fetus through the birth canal during labor.
What are the key features of rhythmic contractions in the myometrium? (4)
The myometrium has spontaneously active rhythmic contractions.
These contractions vary during the menstrual cycle and pregnancy.
The force of contractions is directed towards the cervix.
Contractions are an intrinsic property of the muscle itself.
Does the myometrium require external input for contractions? (2)
The myometrium can generate contractions without neuronal or hormonal input (it is myogenic).
However, it is highly sensitive to external factors, such as sex hormones, which can influence contraction patterns.
How do the contractions of the myometrium change during the menstrual cycle and pregnancy? (2)
The strength and frequency of myometrial contractions vary throughout the menstrual cycle and pregnancy.
Hormonal changes, such as those driven by estrogen and progesterone, influence these variations.
What initiates contraction in the myometrium? (2)
Spontaneous depolarization of 'pacemaker' cells in the myometrium.
These pacemaker cells generate action potentials that trigger contractions.
How is electrical communication spread within the myometrium? (2)
Electrical signals are spread between cells through gap junctions.
These gap junctions allow the depolarization signal to propagate throughout the muscle tissue.
What is the role of the myometrium's syncytium? (1)
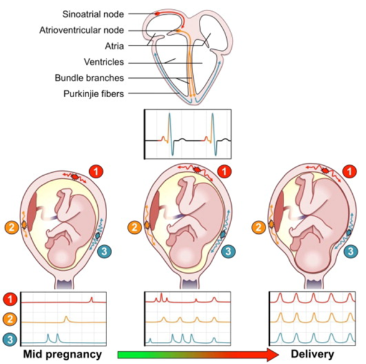
The myometrium functions as a syncytium, meaning that the cells work together as a coordinated unit due to electrical communication through gap junctions.
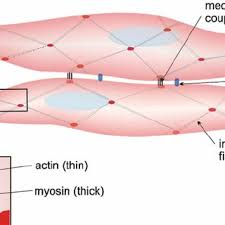
What is excitation-contraction coupling in the myometrium? (2)

Electrical activity in pacemaker cells triggers mechanical activity in smooth muscle cells (SMCs).
This process is mediated by the conduction of electrical signals via the syncytium.
How is the membrane potential of pacemaker cells related to smooth muscle contraction? (1)
The membrane potential of pacemaker cells generates electrical signals that lead to mechanical contractions in smooth muscle.
How do slow waves of pacemaker activity affect smooth muscle contractions? (2)
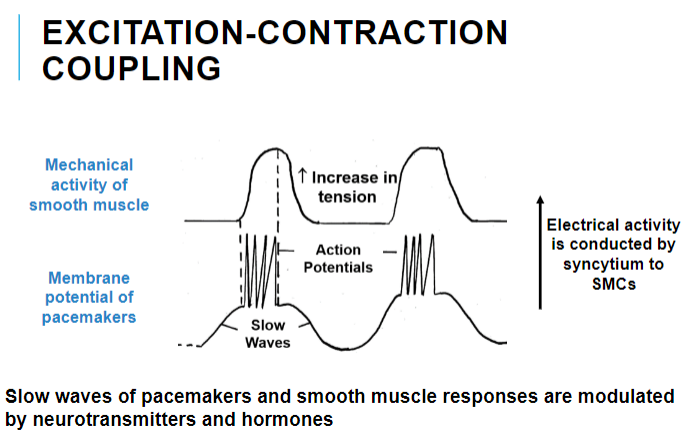
Slow waves in pacemaker cells influence the smooth muscle's responses.
These responses are modulated by neurotransmitters and hormones, affecting the overall contraction pattern.
How does an increase in intracellular calcium ([Ca²⁺]i) affect smooth muscle contraction? (1)
![<p>An increase in [Ca²⁺]i leads to smooth muscle contraction.</p>](/flashcards/cardimage2/1c68286c/782/8782027_back.png)
An increase in [Ca²⁺]i leads to smooth muscle contraction.
What is the relationship between incremental increases in [Ca²⁺]i and force of contraction? (1)
Incremental increases in [Ca²⁺]i lead to proportional increases in the force of contraction.
How do hormones and neurotransmitters modulate smooth muscle contraction in the uterus? (1)
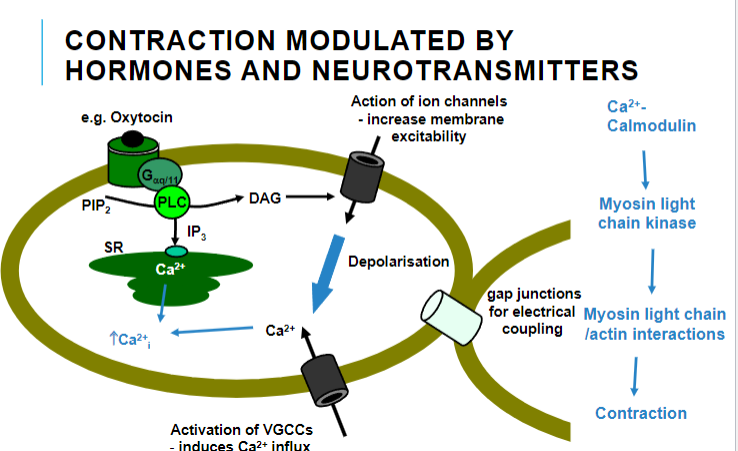
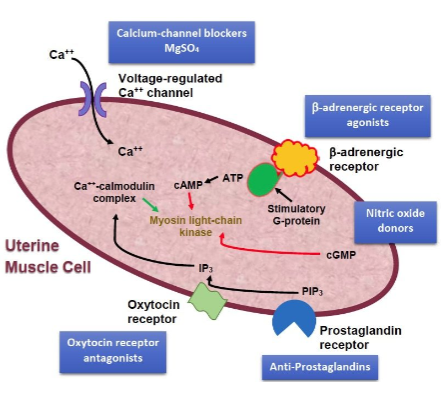
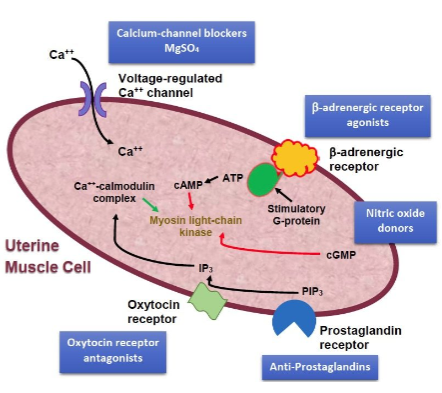
Hormones and neurotransmitters modulate contraction by affecting ion channels, increasing membrane excitability, and activating voltage-gated calcium channels (VGCCs), leading to calcium influx.
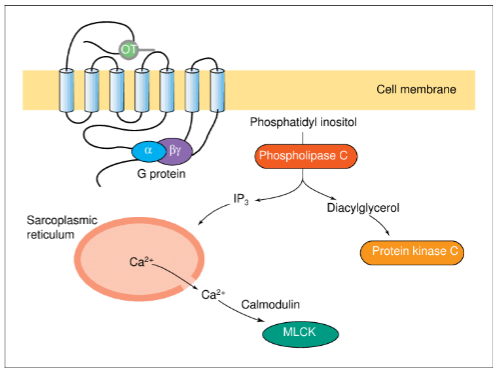
What is the role of calcium-calmodulin in smooth muscle contraction? (1)
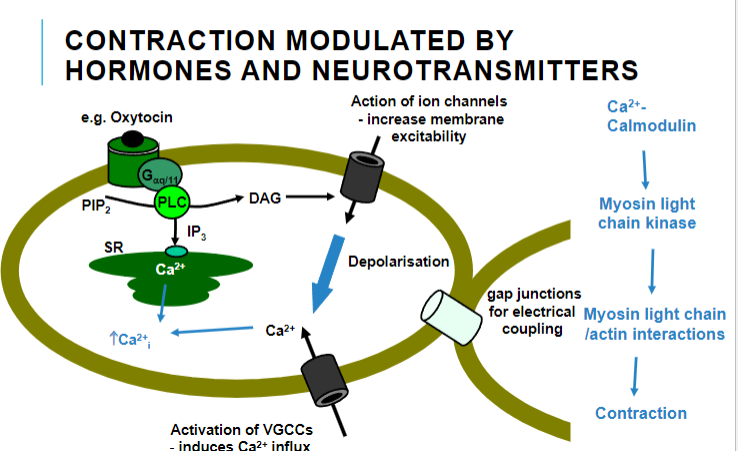
Calcium-calmodulin activates myosin light chain kinase (MLCK), which is involved in smooth muscle contraction.
How does phosphatidylinositol (PIP2) contribute to smooth muscle contraction? (1)
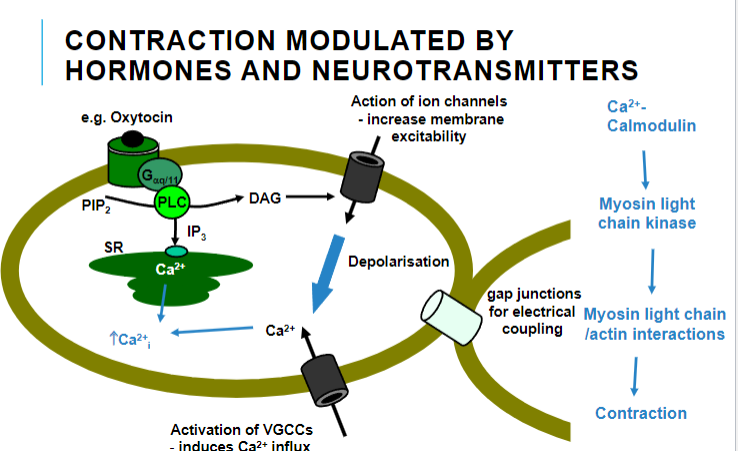
PIP2 activates phospholipase C (PLC), which leads to the production of inositol trisphosphate (IP3) and diacylglycerol (DAG), both of which play roles in the calcium signaling cascade that triggers contraction.
What is the function of gap junctions in smooth muscle contraction? (1)
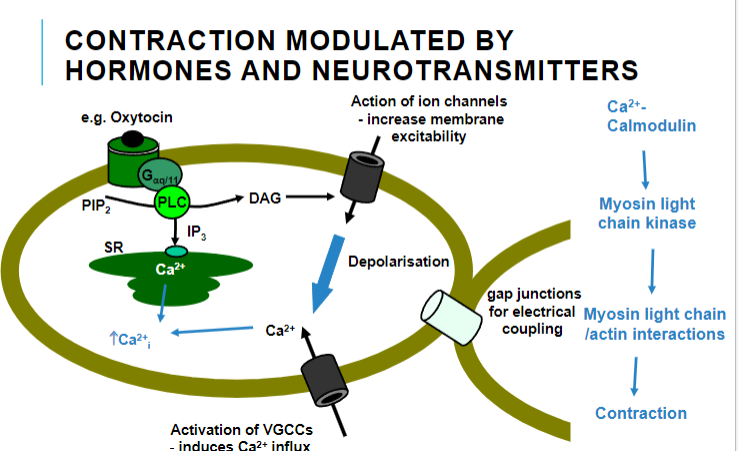
Gap junctions allow for electrical coupling between smooth muscle cells, facilitating coordinated contraction.
How does depolarization affect contraction in smooth muscle? (1)
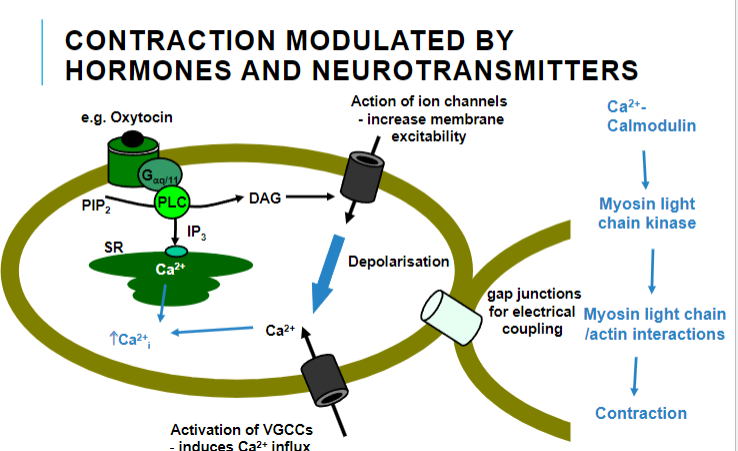
Depolarization activates voltage-gated calcium channels (VGCCs), leading to calcium influx, which triggers smooth muscle contraction.
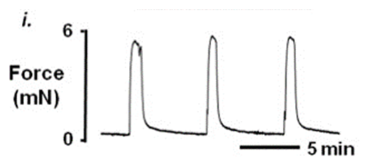
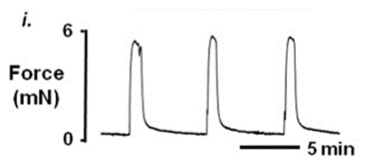
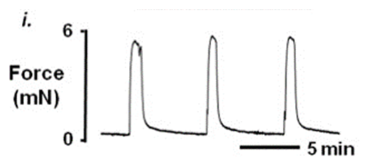
How is uterine contraction measured using isometric tension recording? (1)
Isometric tension recording measures the tension generated by the uterine muscle while keeping the diameter of the muscle ring constant.
What is the purpose of large organ baths in uterine contraction experiments? (1)
Large organ baths, such as those used in Y1 practicals for aortic ring experiments, are used to investigate the functional properties of smooth muscle segments, including uterine smooth muscle.
What types of smooth muscle are commonly studied using these techniques? (1)
Techniques like isometric tension recording are widely used to study the functional properties of uterine, vascular, airway, and bladder smooth muscle segments.
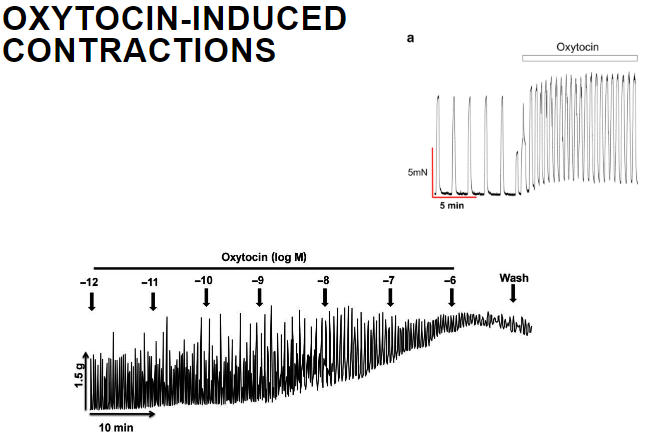
What is the role of oxytocin in uterine contractions? (1)
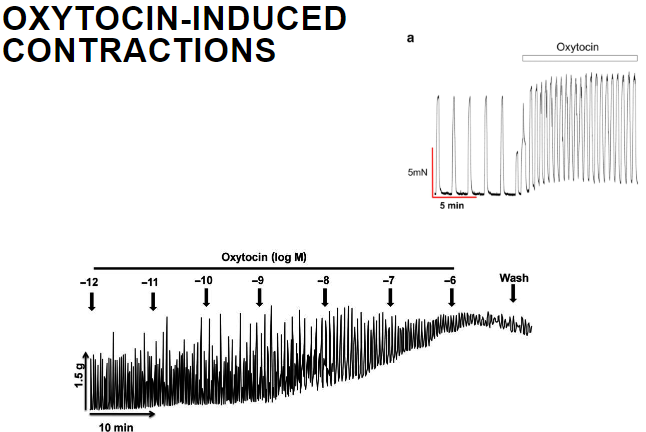
Oxytocin induces strong uterine contractions by increasing intracellular calcium levels and activating myosin light chain kinase, which promotes contraction.
How does oxytocin affect the uterine smooth muscle? (1)
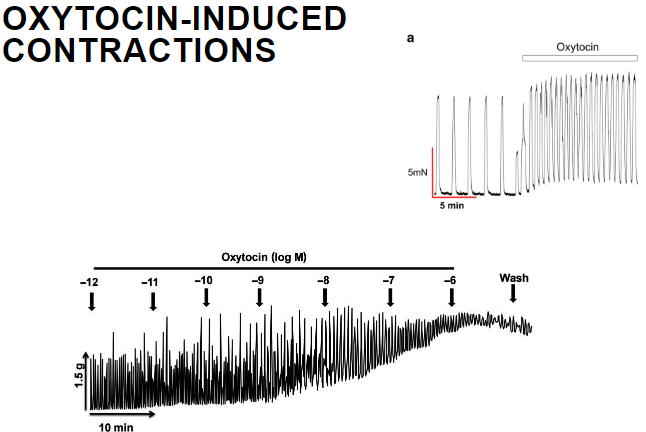
Oxytocin binds to its receptors on uterine smooth muscle, which activates phospholipase C (PLC), leading to increased production of inositol trisphosphate (IP3) and diacylglycerol (DAG), which in turn increases calcium ion concentration and induces contraction.
What intracellular processes are involved in oxytocin-induced uterine contraction? (2)
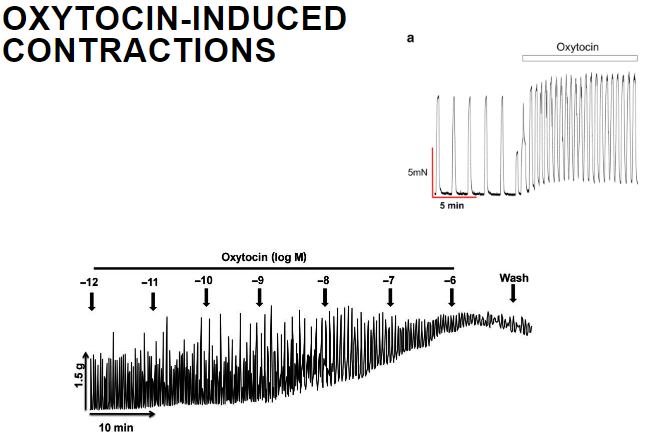
Oxytocin activates PLC, leading to the production of IP3 and DAG. IP3 triggers the release of calcium from the sarcoplasmic reticulum (SR), and DAG enhances the action of calcium. Calcium then activates myosin light chain kinase, resulting in contraction.
What is the effect of increased calcium on uterine smooth muscle? (1)
Increased calcium levels activate myosin light chain kinase, which phosphorylates the myosin light chain, leading to smooth muscle contraction.
What is the effect of a Ca²⁺ channel blocker on uterine contractions? (1)
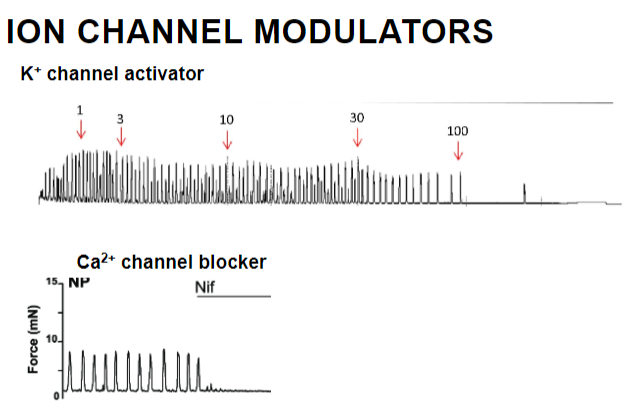
A Ca²⁺ channel blocker reduces intracellular calcium levels, inhibiting the contraction of uterine smooth muscle by preventing calcium influx.
How does a K⁺ channel activator affect uterine smooth muscle? (1)
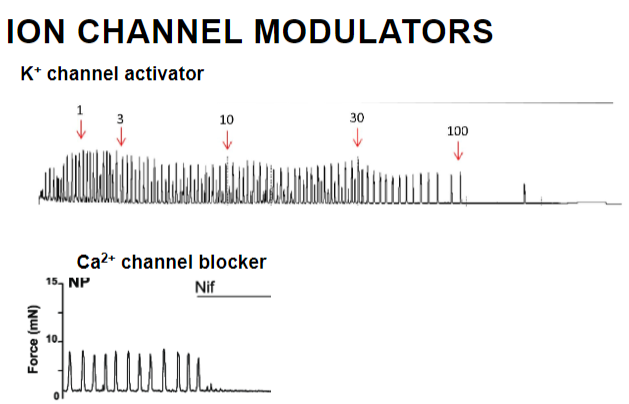
A K⁺ channel activator increases potassium efflux, leading to hyperpolarization of the uterine smooth muscle membrane, making it less excitable and reducing contraction.
What are the key characteristics of the uterus's contractile properties? (5)
The uterus has strong contractile properties due to its smooth muscle content in the myometrium.
It is spontaneously contractile, meaning it can initiate contractions without external stimuli.
Pacemaker cells in the uterus initiate depolarization.
This depolarization spreads from cell to cell, facilitating coordinated contraction.
Depolarization results in calcium entry, which triggers contraction.
Contractile activity can be modulated by hormones and neurotransmitters.
How do neurotransmitters regulate uterine contractions? (4)
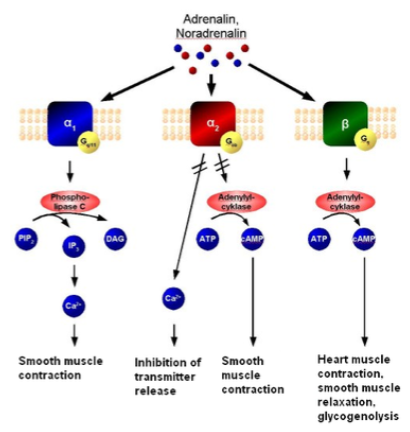
The uterus is regulated by sympathetic (not parasympathetic) innervation.
α-adrenoceptor agonists cause contraction of the uterine muscle.
β2-adrenoceptor agonists cause relaxation of the uterine muscle.
The uterus expresses α- and β- adrenoceptors, which mediate these effects.
How do sex hormones regulate uterine contractions? (4)
Progesterone inhibits uterine contractions.
Oestrogen increases uterine contractions.
In the non-pregnant uterus, there are weak contractions early in the menstrual cycle and strong contractions during menstruation (when progesterone levels are low).
Both hormones act at nuclear and membrane receptors to modulate uterine contractility.
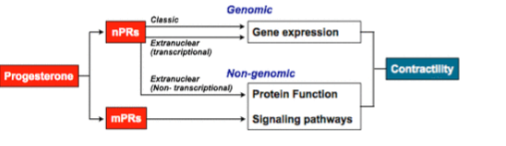
Picture demonstrating the genomic and non-genomic effects on contractility:
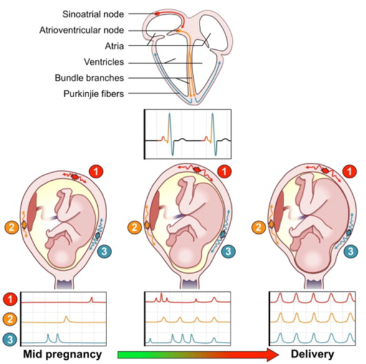
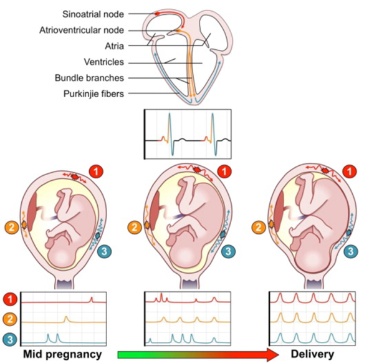
How do sex hormones regulate uterine contractions in pregnancy? (5)
Early pregnancy: Weak and uncoordinated contractions due to high progesterone.
From 7 months to term, oestrogen levels increase, while progesterone remains constant.
The oestrogen/progesterone ratio increases in the last trimester.
This ratio culminates in strong, coordinated contractions for delivery.
The hormonal changes contribute to the preparation of the uterus for labor.
How does oxytocin regulate uterine contractions during pregnancy? (5)
Oxytocin is a non-peptide hormone synthesized in the hypothalamus and released from the posterior pituitary gland.
It is released in response to suckling and cervical dilation.
Oestrogen, released in the later stages of pregnancy, causes:
Increased oxytocin release.
Increased expression of oxytocin receptors in the uterus.
Oxytocin also increases prostaglandin synthesis, which enhances uterine contraction.
How do prostaglandins regulate uterine contractions and what is their role in menstrual and post-partum conditions? (5)
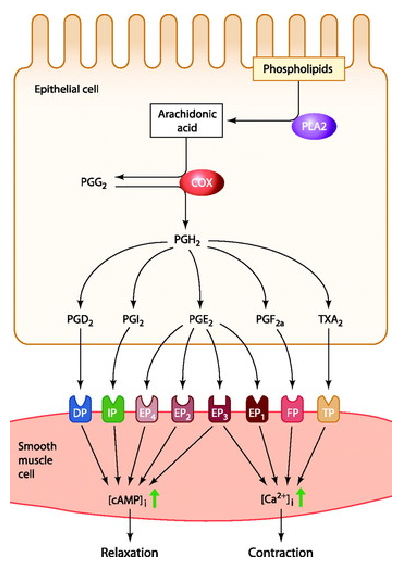
Prostaglandins (PGE and PGF) induce myometrial contraction.
They play a role in dysmenorrhoea (severe menstrual pain), menorrhagia (severe menstrual blood loss), and pain after parturition.
NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) are effective in reducing contraction and pain by inhibiting prostaglandin production.
Oxytocin stimulates the release of prostaglandins, further promoting uterine contraction.

Summarize the regulation of myometrial contractility by hormones and prostaglandins. (5)
Myometrial contractility is sensitive to sex hormones, oxytocin, and prostaglandins.
Progesterone and oestrogen have opposite effects on contractility, influencing the menstrual cycle and pregnancy.
Oxytocin and prostaglandins increase contractility.
Oestrogen can stimulate oxytocin release, and oxytocin stimulates prostaglandin synthesis.
These hormones act in concert to facilitate delivery.
List and describe the contractile agents affecting the uterus. (3)

Ergots: A potent uterine contractor found in ergot, which stimulates smooth muscle contraction.
Oxytocin: A hormone that promotes uterine contractions, especially during labor, by binding to oxytocin receptors.
Prostaglandins: Lipid compounds that induce uterine contractions (e.g., PGE and PGF), playing a role in menstruation, labor, and dysmenorrhea.

Describe ergot and its role in uterine contraction. (3)

Ergot: A fungus that grows on certain cereals (e.g., rye) and grasses, containing ergometrine.
Action: Induces powerful and prolonged uterine contractions.
Mechanism: Likely stimulates α-adrenoceptors and 5-HT receptors.
Uses: Primarily used for post-partum bleeding, but not for inducing labor.
Describe the use of oxytocin in uterine contraction. (3)
Induction and augmentation of labor: Oxytocin is used to initiate or strengthen contractions during labor.
Dose-dependent effects: It increases contractions, but excessive amounts can cause sustained contraction, leading to fetal distress.
Other uses: Used to treat postpartum hemorrhage and in the management of miscarriage.
Describe the use of prostaglandins in uterine contraction. (3)
Induction of labor: Prostaglandins are used to induce labor.
Induction of abortion: Misoprostol and gemeprost are examples of prostaglandins used to induce abortion.
Postpartum bleeding: Prostaglandins also help manage postpartum bleeding.
What are myometrial relaxants used for in premature labor? (3)
Delay delivery: Myometrial relaxants are used to delay delivery by 48 hours.
Transfer to specialist unit: This delay allows the mother to be transferred to a specialized unit.
Antenatal corticosteroids: The delay enables the administration of antenatal corticosteroids, which help fetal lung maturation and increase survival chances.
How is progesterone used in preterm labor or miscarriage prevention? (2)
Preterm labor: Progesterone can be used to prevent premature labor.
Miscarriage prevention: It is also used to reduce the risk of miscarriage in some cases.
What are the types of myometrial relaxants used in premature labor and their mechanisms of action? (4)
Ca2+ channel antagonists: e.g. nifedipine, which works by inhibiting calcium influx, reducing muscle contraction.
Oxytocin receptor antagonists: e.g. Retosiban, which blocks oxytocin receptors, preventing uterine contractions.
β2-adrenoceptor stimulants: e.g. terbutaline sulfate, which stimulates β2 receptors to relax the uterus.
Direct action on the myometrium: All of these agents reduce the strength of uterine contractions by acting directly on the myometrium.
Are myometrial relaxants recommended for uncomplicated preterm labor? (1)
Not recommended: Myometrial relaxants are no longer recommended for uncomplicated preterm labor.
What are the pharmacological agents used for induction of labor at term? (2)
Oxytocin
Prostaglandins
What pharmacological agent is used for termination in early term and why is oxytocin not used? (2)
Prostaglandins are used for termination in early term.
Oxytocin is not used because there are no oxytocin receptors present in early term.
What agents are used to manage post-partum bleeding? (3)
Prostaglandins
Oxytocin
Ergots
What pharmacological agents are used to prevent premature birth? (4)
Ca2+ channel blockers
Oxytocin inhibitors
β2 agonists