Infective endocarditis comes in two forms. What are they and briefly describe them.
Subacute: the defective heart valves are invaded by organisms such Streptococcus viridans.
Acute: normal heart valves are attacked by organisms such as Staph. A.
What is the general pathophysiology of infective endocarditis?
The infective organisms invade the heart valves causing inflammation and the formation of vegetations on the cusps. In the acute stage, vegetations may interfere with the opening and closing of the cusps. Eventually, pieces with break away causing septic emboli that cause infarction. This causes additional destruction and scarring of the valve.
Name some factors that predispose someone to infection to infective endocarditis.
- abnormal valves in heart
- bacteremia
- reduced immunity
Name the signs and symptoms of acute and subacute infective endocarditis.
Acute:
- chills
- spiking fever
- sudden onset
Subacute:
- anorexia
- splenomegaly
- CHF
- increasing fatigue
- insidious onset
What is pericarditis?
Inflammation of the pericardium (usually secondary to another condition) and is classified by its cause and the type of exudate. Effusion may develop when a large volume of fluid accumulated in the pericardial sac; fluid may be serous or fibrinous and purulent.
What is chronic pericarditis and its effects on the body?
Chronic inflammation of the pericardium which results in the formation of adhesions between the pericardial membranes. This limits the movement of the heart during diastole and systole --> reduced CO. Because of the reduced CO and systemic venous congestion it causes fatigue, weakness, and abdominal discomfort.
What is primary hypertension and what are its initial signs?
Idiopathic HTN; the areas most affected are the kidneys, heart, brain and retina. The initial signs are typically vague and nonspecific: fatigue, malaise, sometimes morning occipital headache.
How can you treat primary/essential HTN?
- lifestyle changes
- reduction of Na
- weight loss
- reduction of stress
- diuretics (high bp)
What is secondary HTN?
HTN secondary to another condition. Ex. HTN resulting from renal (nephrosclerosis) or endocrine (hyperaldosteronism) disease. To reduce bp, the underlying problem needs to be addressed.
What is malignant/resistant HTN?
Hypertensive emergency with extremely high bp. Results in organ damage.
What is peripheral vascular disease (PVD)?
Abnormality of the peripheral arteries and veins, this causes a build of atheromas.
What is an aortic aneurysm?
When a bulge is formed somewhere in the aorta.
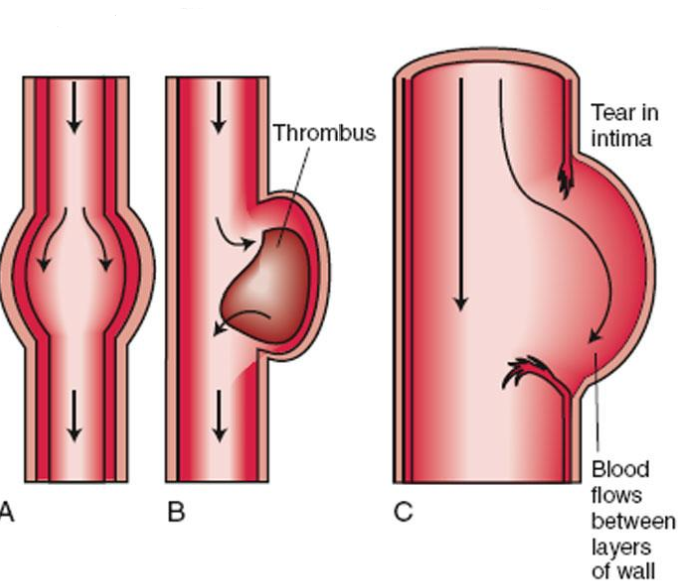
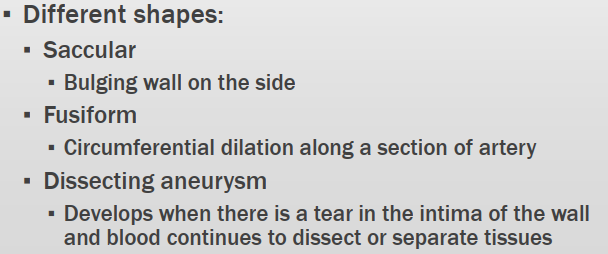
Name the different forms of aortic aneurysm.
What may be some causes of an aortic aneurysm?
- atherosclerosis
- trauma
- infections
- congenital defects
What are varicose veins?
Irregular, bulging veins that most commonly affect the superficial or deep veins (legs, esophagus, and rectum). The bulging is due to weakening of the valves which leads to excessive hydrostatic pressure (push). This causes the walls to dilate and stretch and the backflow of blood.
What is thrombophlebitis and phlebothrobosis?
Thrombophlebitis: the formation of a clot in an inflamed vein.
Phlebothrombosis: formation of a clot without prior inflammation (forms independently) and the clot is attached loosely.
Name some factors for thrombus development.
- stasis of blood or sluggish blood flow
- endothelial injury
- ^blood coagulability (more clotting)
What is hypovolemic and cardiogenic shock?
Hypovolemic: due to a loss of blood or plasma (excess loss of fluids) and was caused by either: hemorrhage, burns, dehydration, peritonitis, pancreatitis.
Cardiogenic: the inability of the heart to maintain adequate CO to circulation. Can be due to: MI of left ventricle, cardiac arryhthmia, embolus.
What are the three factors that determine blood pressure?
- blood volume
- heart contractions
- peripheral resistance
What is vasogenic, anaphylactic and septic shock?
Vasogenic: sudden vasodilation of the vessels due to loss of sympathetic and vasomotor tone.
Anaphylactic: systemic vasodilation and increased permeability owing to severe allergic reaction.
Septic: vasodilation from severe infection.
Name some compensations mechanisms when blood pressure drops.
- renin secreted to activate angiotensin which constricts the vessels to increase blood volume.
- ^ADH to promote reabsorption of water to increase blood volume.
- secretion of glucocorticoids which stabilize the vascular system.
- SNS increase heart rate which forces contractions creating systemic vasoconstriction.
What are some complications of shock?
- acute renal failure
- ARDS
- hepatic failure
- hemorrhagic ulcers
- infection/septicemia
- depression of cardiac function
Why is essential hypertension so dangerous?
Answer
Differentiate angina and MI with regard to its cause and the characteristics of pain associated with it.
Angina is primarily caused from a lack of O2 to the heart muscle, this lack of O2 can be due to many reasons (atheroma, vasospasm, anemia, etc.). The pain is felt substernal to the chest. An MI is caused from a blockage of a coronary artery (most likely from an atheroma), this leads to cell death and an infarction of the heart wall. The pain can be felt distant from the actual source and substernally.
What are the three ways an infarction can occur?
- thrombus from atheroma can obstruct an artery
- vasospasm due to a partial occlusion from an atheroma
- due to an embolus from a thrombus