What is the anatomy of the esophagus? (4)
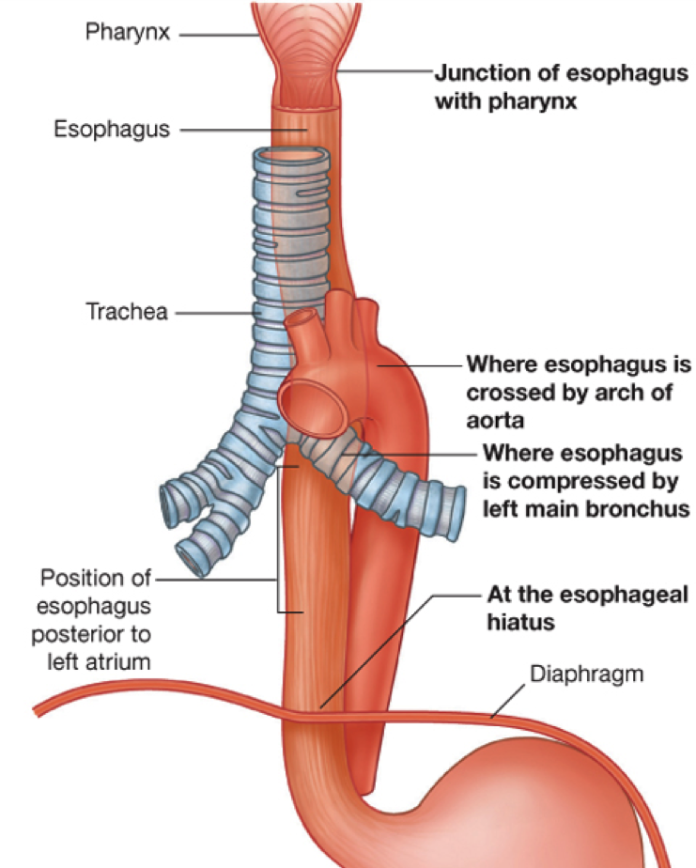
𖹭 The esophagus is a fibromuscular tube approximately 25 cm in length
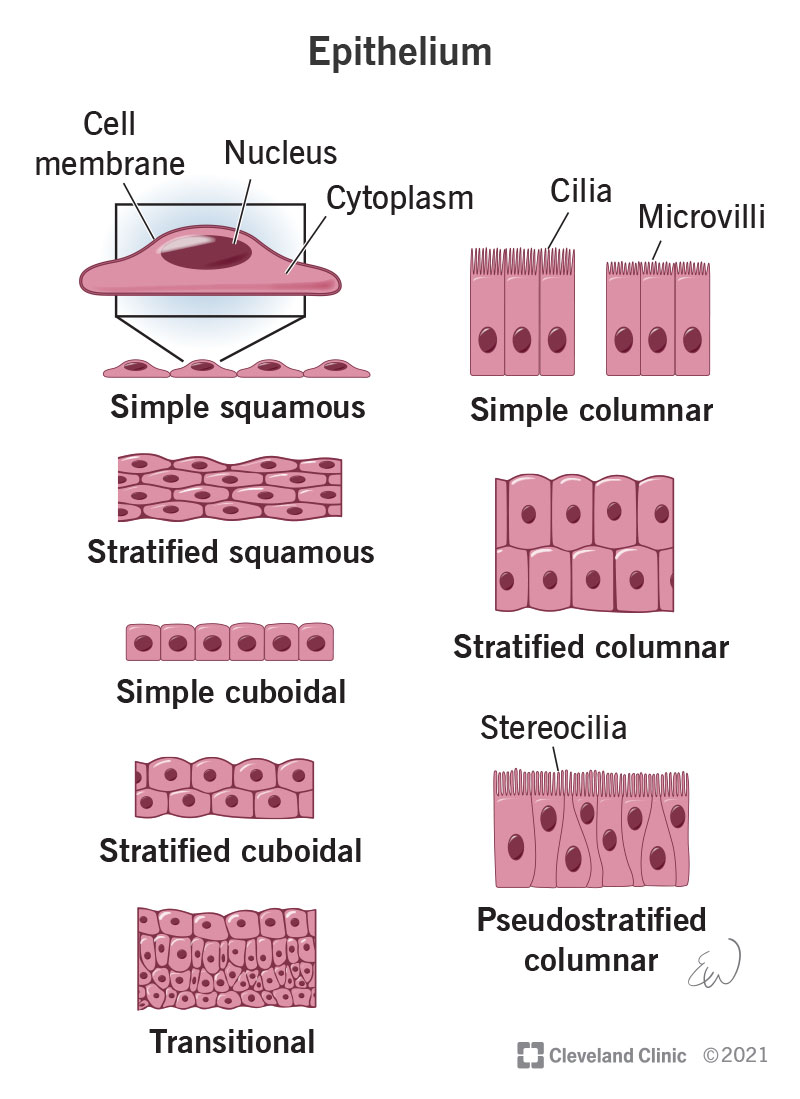
𖹭 It is lined with stratified squamous epithelium
𖹭 The oesophagus lies posterior to the trachea
𖹭 It begins at the end of the laryngopharynx and joins the stomach a few centimetres from the diaphragm, specifically at the cardiac orifice of the stomach
What is the primary function of the esophagus? (2)
𖹭 The esophagus functions to transport food to the stomach, often referred to as the "eating gullet"
𖹭 Additionally, it secretes mucus to aid in the lubrication of food passage
What promotes the transport of ingested food into the stomach? (2)
𖹭 The transport of ingested food into the stomach is promoted by a highly coordinated muscular process involving the contraction and relaxation of the esophagus
𖹭 Relaxation of the upper oesophageal sphincter (UOS) and lower oesophageal sphincter (LOS) also facilitates the passage of food through the esophagus
What is a sphincter, and how many sphincters does the esophagus have? (2)
𖹭 A sphincter is a ring-like muscle that can constrict to close off a passage or opening in the body
𖹭 The oesophagus has two sphincters
Describe the upper oesophageal sphincter (UOS) in terms of its muscle structure and function (2)
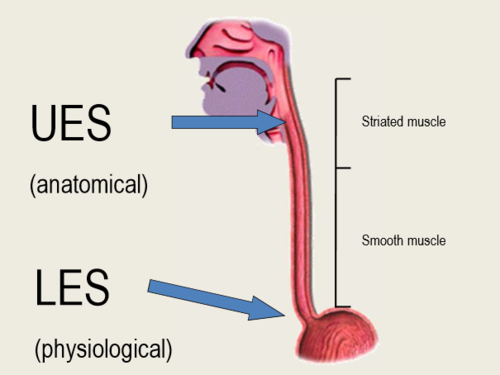
𖹭 The upper oesophageal sphincter (UOS) is composed of striated muscle and is a muscle-cartilaginous structure
𖹭 Its primary function is to constrict to prevent air from entering the esophagus
What are the characteristics of the lower oesophageal sphincter (LOS)? (3)
𖹭 The lower oesophageal sphincter (LOS) is composed of smooth muscle and acts as a flap valve
𖹭 It forms an area of high pressure zone
𖹭 The LOS has both intrinsic and extrinsic components
What components make up the intrinsic and extrinsic parts of the lower oesophageal sphincter (LOS)? (2)
𖹭 Intrinsic components of the LOS include oesophageal muscles, which are under neurohormonal influence
𖹭 Extrinsic components of the LOS include the diaphragm muscle, which acts as an adjunctive (means added to something else) external sphincter
How do the intrinsic and extrinsic sphincters of the esophagus work together? (2)
𖹭 The intrinsic and extrinsic sphincters work in concert to push food into the stomach
𖹭 Malfunction of these components can lead to gastro-oesophageal reflux disease (GORD)
Describe the distribution of skeletal and smooth muscles along the length of the esophagus
𖹭 Skeletal muscles surround the esophagus below the pharynx (the upper third), while smooth muscles surround the lower two-thirds of the esophagus
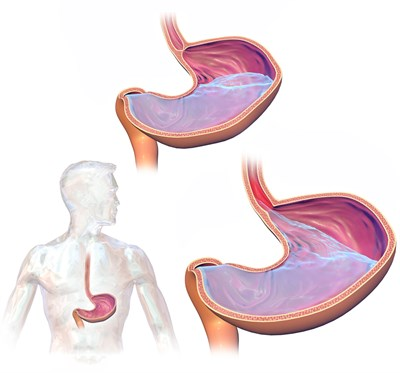
What are the intrinsic components of the lower oesophageal sphincter (LOS)? (4)
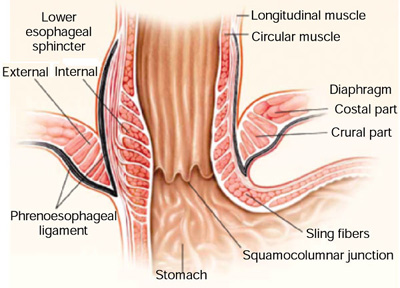
𖹭 Thick circular smooth muscle layers and longitudinal muscles
𖹭 Clasp-like semicircular smooth muscle fibres on the right side, which exhibit myogenic activity with some resting tone initiated by cells within and are less responsive to acetylcholine (ACh)
𖹭 Sling-like oblique gastric (angle of His) muscle fibres on the left side, which work in concert with the clasp-like semicircular smooth muscle fibres to help prevent regurgitation
𖹭 They are responsive to cholinergic innervation
What is the significance of the angle of His in the lower oesophageal sphincter? (2)
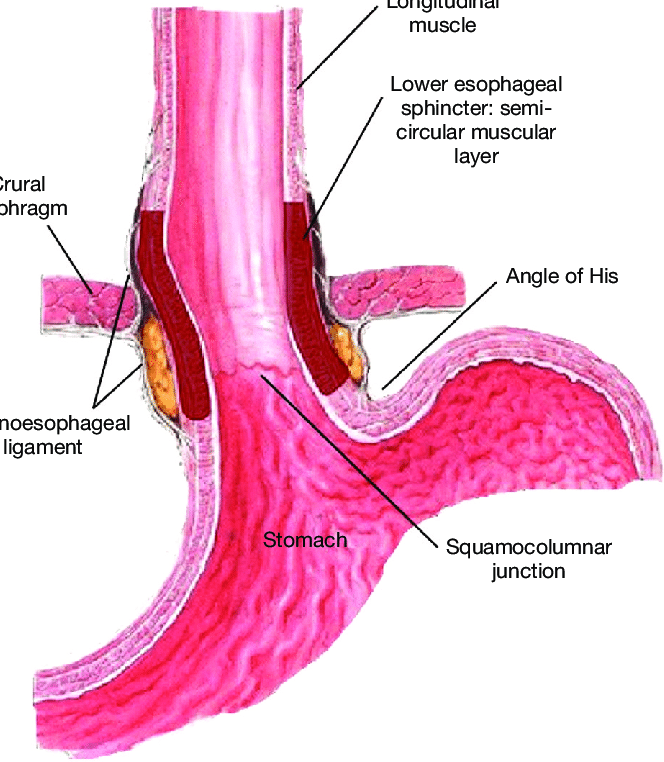
𖹭 The angle of His, characterized by sling-like oblique gastric muscle fibres, helps prevent regurgitation by working in concert with the clasp-like semicircular smooth muscle fibres
𖹭 In infants, the angle of His is poorly developed, resulting in a vertical junction with the stomach, which is why reflux is common in infants
What are the extrinsic components of the lower oesophageal sphincter (LOS)? (3)
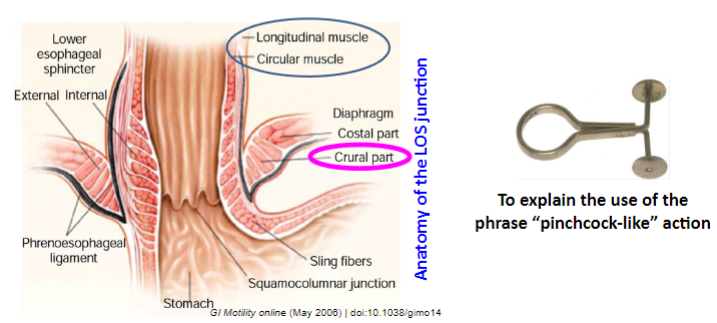
𖹭 The extrinsic components of the LOS include:
𖹭 The crural diaphragm, which encircles the LOS and forms a channel through which the esophagus enters the abdomen
𖹭 Fibres of the crural portion of the diaphragm possess a "pinchcock-like" action, acting as an extrinsic sphincter or diaphragmatic sphincter, exhibiting myogenic tone
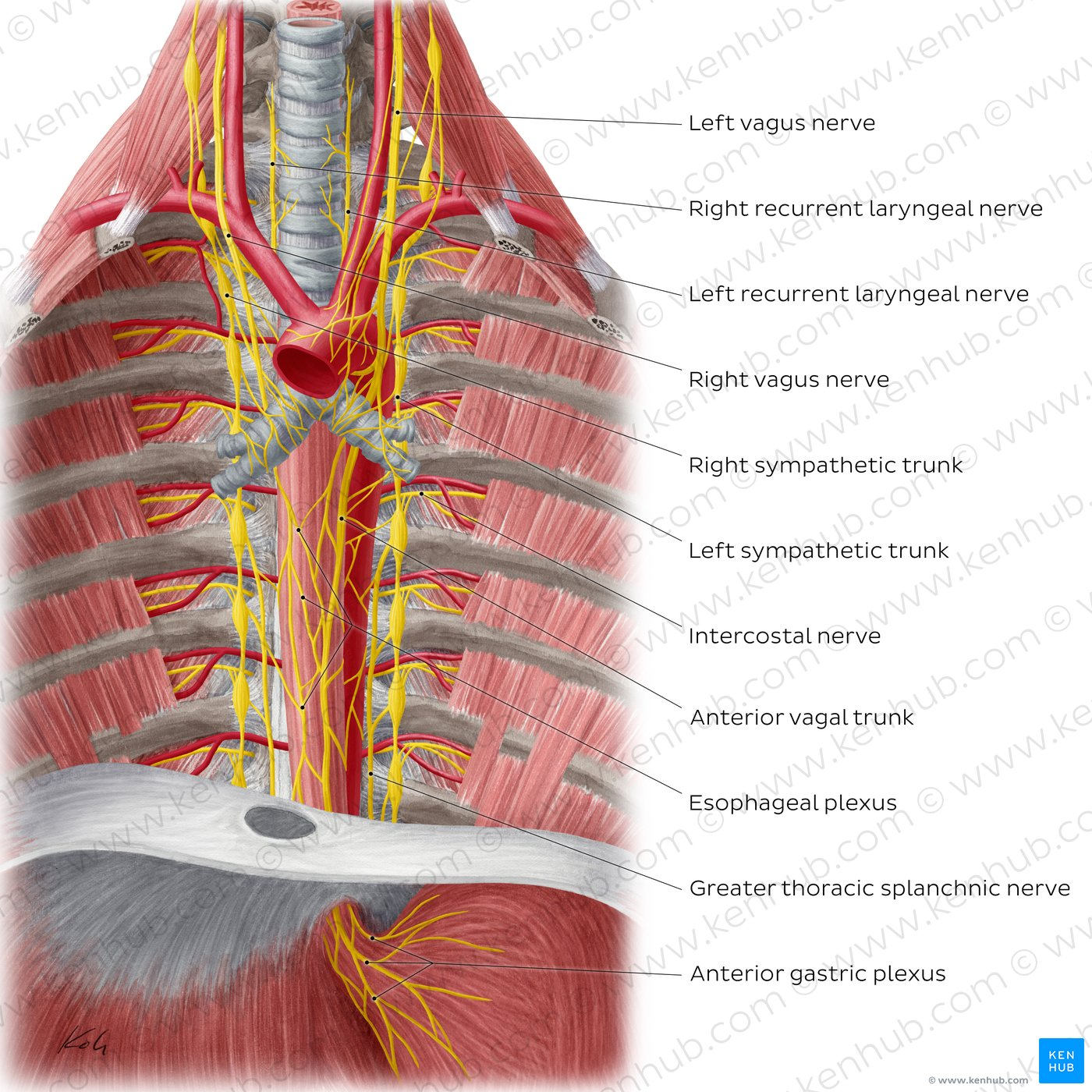
How is the upper part of the esophagus innervated, considering its striated muscle composition? (2)
𖹭 The upper part of the esophagus, which consists of striated muscle, is supplied by somatic motor neurons of the vagus nerve without interruption
𖹭 Innervation includes: the vagus nerve and splanchnic nerves originating from the thoracic sympathetic trunks
What innervates the lower part of the esophagus, primarily composed of smooth muscles? (2)
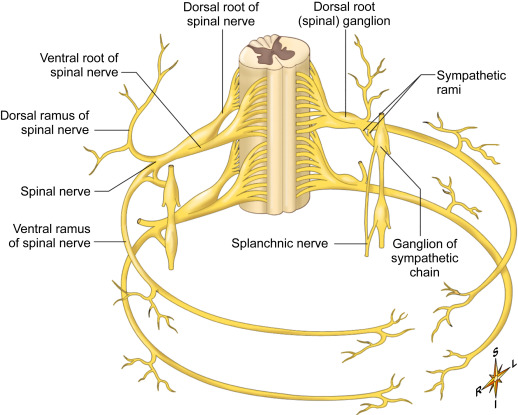
𖹭 The lower part of the esophagus, composed of smooth muscles, is innervated by visceral motor neurons of the vagus nerve with interruptions
𖹭 Interruptions occur via synapse with postganglionic neurons, with cell bodies located in the esophagus and splanchnic plexus
Picture demonstrating Oesophageal motor innervation:
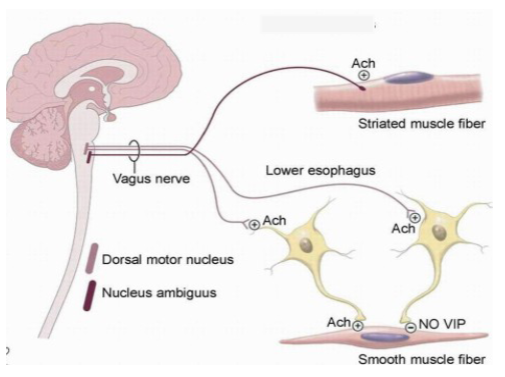
What is the involvement of cholinergic and non-cholinergic, NANC (Noradrenergic, noncholinergic) innervation in controlling the tone of the lower oesophageal sphincter? (4)
𖹭 Cholinergic innervation, mediated by acetylcholine (ACh), contracts the intrinsic sphincters of the lower esophagus
𖹭 Non-cholinergic, non-adrenergic, or NANC innervation also plays a role
𖹭 These neurotransmitters include substance P (SP), which contracts the intrinsic sphincters, while gastrin has a similar effect
𖹭 On the other hand, nitric oxide (NO) and vasoactive intestinal peptide (VIP) act to relax the intrinsic sphincters
How is the neural control of the oesophageal sphincters facilitated?
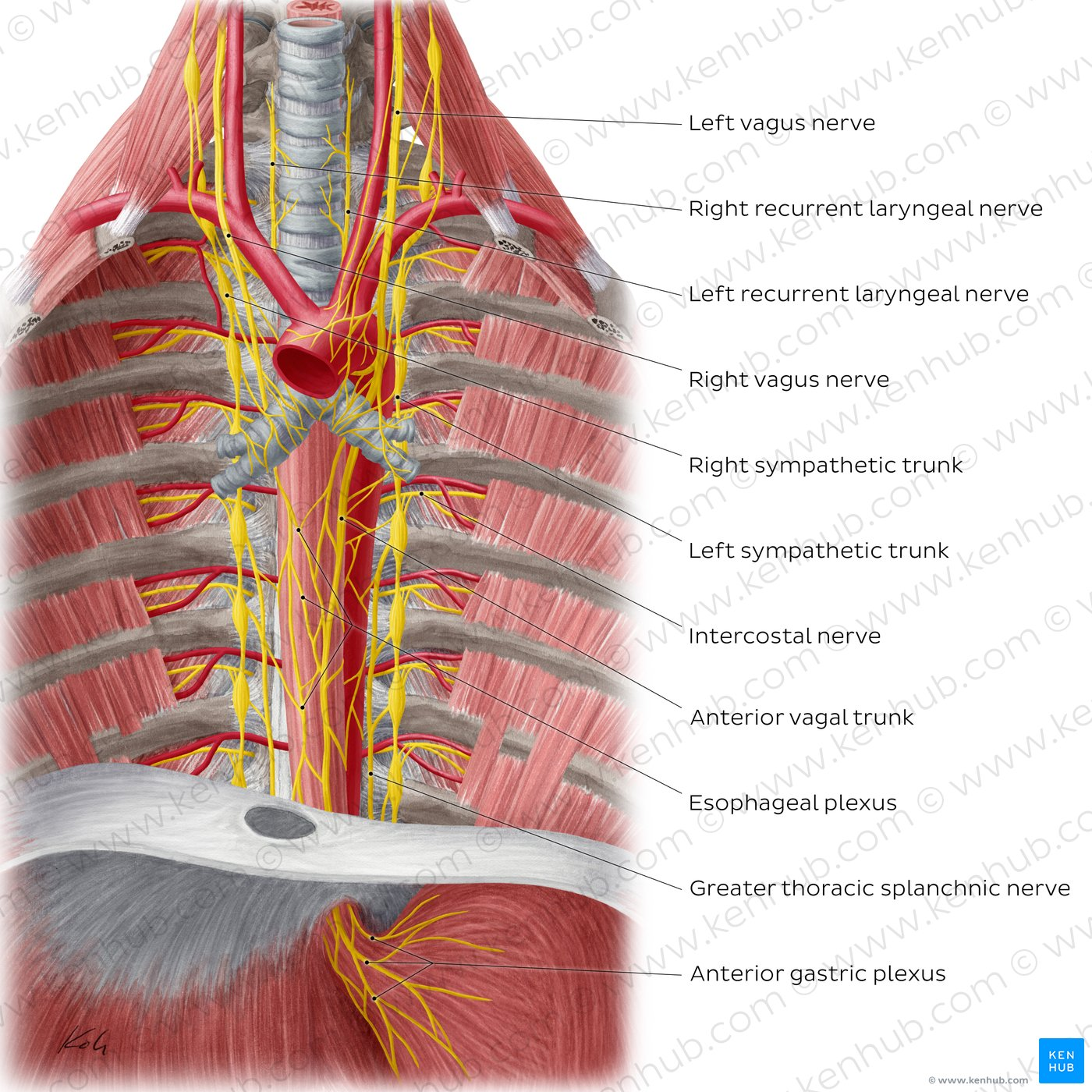
𖹭 The oesophagus is encircled by nerves of the oesophageal plexus
𖹭 Acetylcholine and substance P contract the intrinsic sphincters, while gastrin also contributes to this effect
𖹭 Conversely, nitric oxide and vasoactive intestinal peptide relax the intrinsic sphincters
Picture demonstrating the innervation of the oesophagus
What are the functions of the esophagus? (7)
𖹭 Swallowing, also known as deglutition
𖹭 Conveying food and fluids from the pharynx to the stomach
𖹭 The presence of food in the mouth triggers the swallowing reflex
𖹭 Afferent impulses in the glossopharyngeal-vagal reflex are involved
𖹭 Integration of impulses occurs in the nucleus of tractus solitarius (NTS), nucleus ambiguus (NA), and dorsal vagal nucleus
𖹭 Efferent impulses/motor pathways pass to the pharyngeal musculature, tongue, esophagus, and lower oesophageal sphincter (LOS)
𖹭 Swallowing is characterized by coordinated opening and closing of the upper oesophageal sphincter (UOS) and lower oesophageal sphincter (LOS)
How is swallowing initiated? (3)
𖹭 Voluntary action: The initiation of swallowing involves a voluntary action where material is collected on the tongue and pushed backward into the pharynx
𖹭 This action is facilitated by skeletal muscles and the mucus membrane
𖹭 Involuntary contractions: Waves of involuntary contractions push the material from the pharynx into the esophagus
Describe the movement of food from the mouth to the stomach
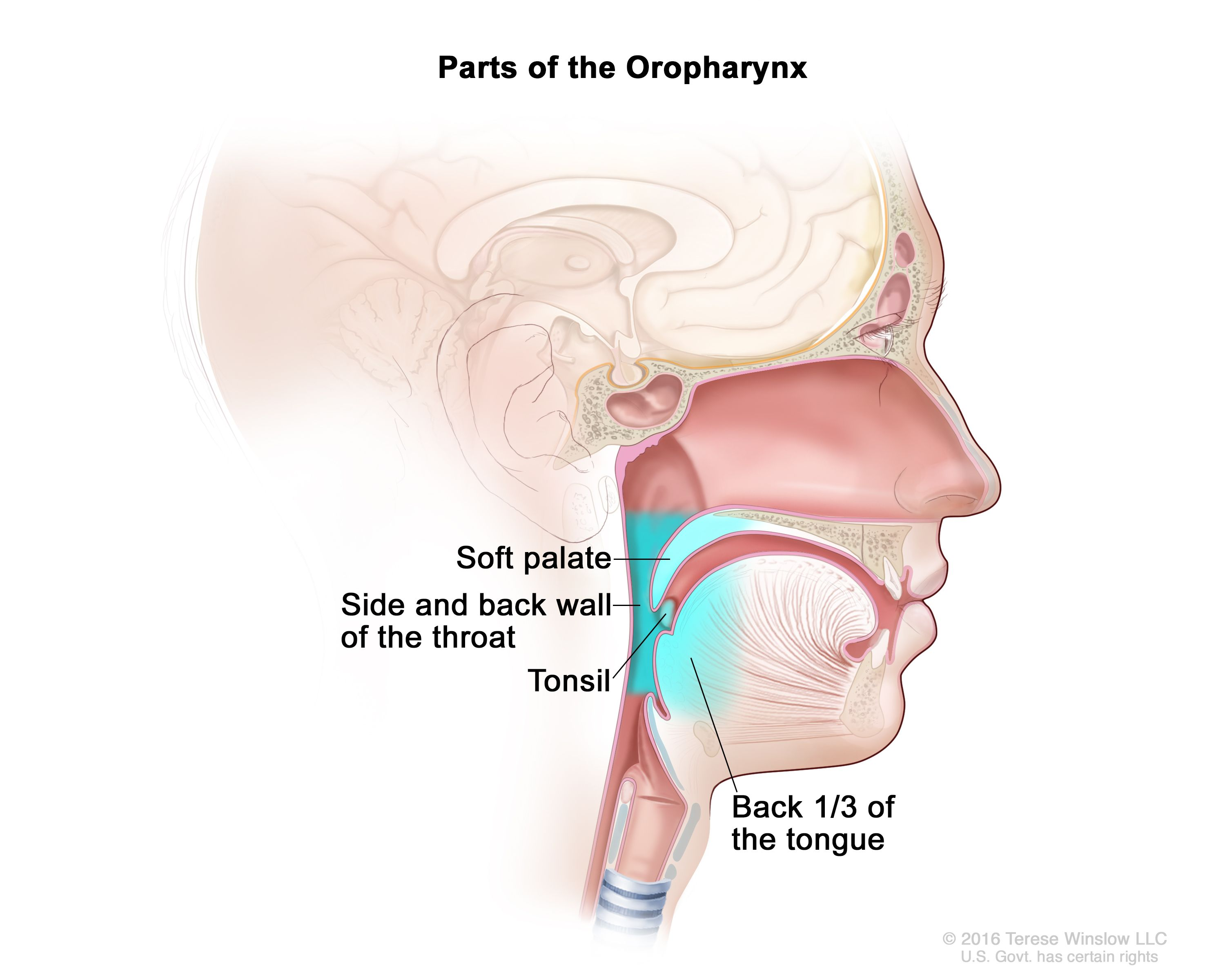
𖹭 Food moves from the mouth to the oropharynx, then to the laryngopharynx, and finally into the oesophagus and stomach
What reflex responses occur during swallowing?
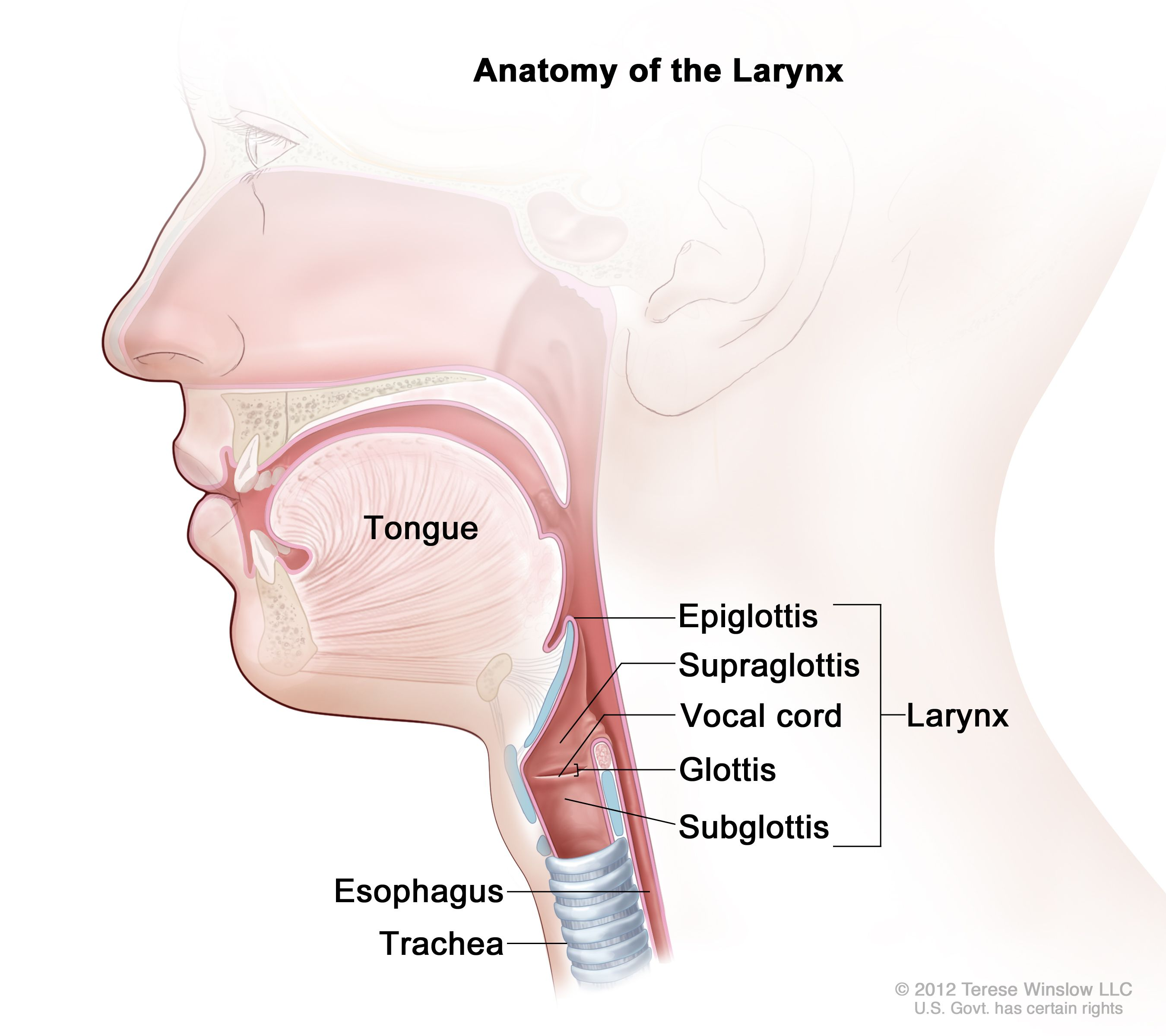
𖹭 During swallowing, reflex responses include inhibition of respiration (breathing), where the nasopharynx is closed off, and closure of the glottis by the epiglottis to prevent food from entering the trachea
What facilitates the movement of food towards the stomach?
𖹭 A ring of peristaltic waves, moving at a rate of approximately 4 cm per second, develops behind the food mass, pushing it towards the stomach
What happens after the initial peristaltic wave?
𖹭 Following the initial peristaltic wave, a second wave of peristalsis moves any remaining food remnants along the esophagus
Picture demonstrating how swallowing is initiated:
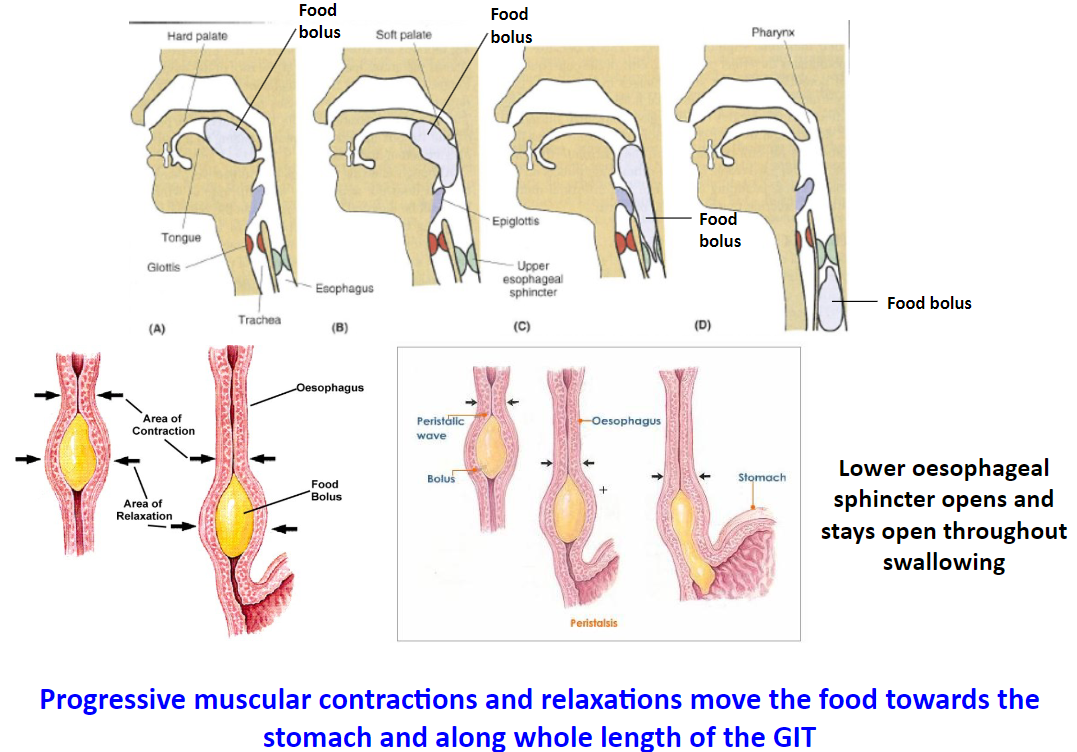
What is secondary peristalsis? (2)
𖹭 Secondary peristalsis occurs when the upper esophageal sphincter (UOS) relaxes, allowing food to pass into the esophagus. After the food passes, the UOS closes, the glottis opens, and breathing resumes. Similarly, the lower esophageal sphincter (LOS) closes after the food mass has passed
𖹭 Large food material often doesn't reach the stomach after the first peristaltic wave. Distension of the esophageal lumen by food remnants stimulates receptors, leading to repeated waves of peristalsis (secondary peristalsis). This ensures that ingested food reaches the stomach
What mechanisms prevent the reflux of gastric contents?
𖹭 The lower oesophageal sphincter (LOS) closes after the food mass has passed
𖹭 The "pinchcock" effect of the diaphragmatic sphincter on the lower esophagus, which involves side-to-side compression between the "two pillars" of the crus
𖹭 The plug-like action of mucosal folds in the cardia, which occludes the lumen of the gastro-oesophageal junction
𖹭 Additionally, factors such as abdominal pressure acting on the intra-abdominal parts of the esophagus and the valve-like effect of the oblique entry of the esophagus into the stomach contribute to preventing reflux
What are the roles of the sphincter muscles of the upper and lower oesophageal sphincters? (2)
𖹭 The sphincter muscles of the upper and lower oesophageal sphincters are strong circular muscles that act as valves.
𖹭 They promote and control the movement of the food mass towards the anus, preventing reflux by forming an opening when relaxed and closing completely when contracted
What are the types of esophageal disorders? (5)
𖹭 Oropharyngeal dysphagia/aphagia: Difficulty swallowing due to UOS malfunction or coordination issues between UOS opening and pharyngeal movement
𖹭 Oesophageal spasm: Abnormal contractions hindering food passage
𖹭 Diffuse oesophageal spasm: Causes angina-like chest pain originating from the esophagus
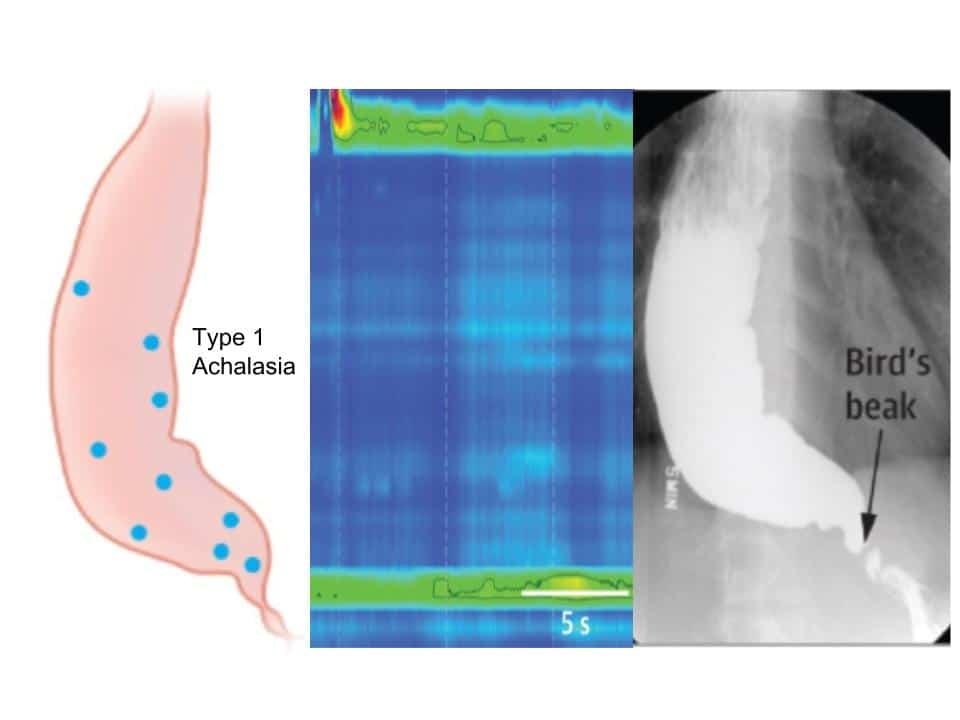
𖹭 Achalasia: Impaired oesophageal motility affecting UOS, LOS, and oesophageal body
𖹭 Regurgitation: Stomach acid reflux into the esophagus, often due to a weak LOS (Gastro-oesophageal reflux disease or GORD)
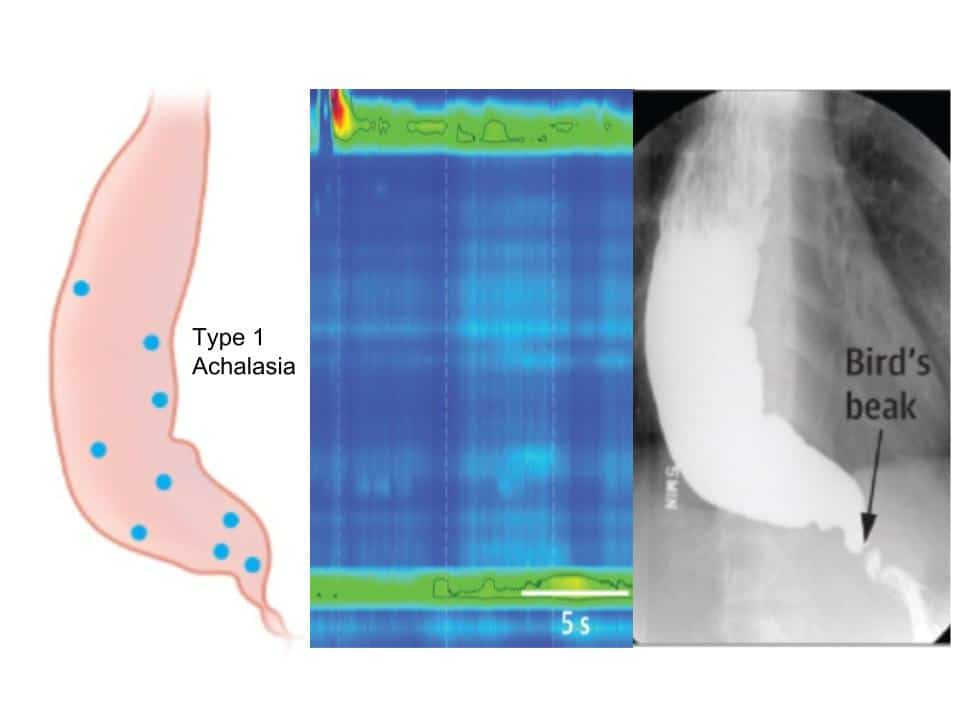
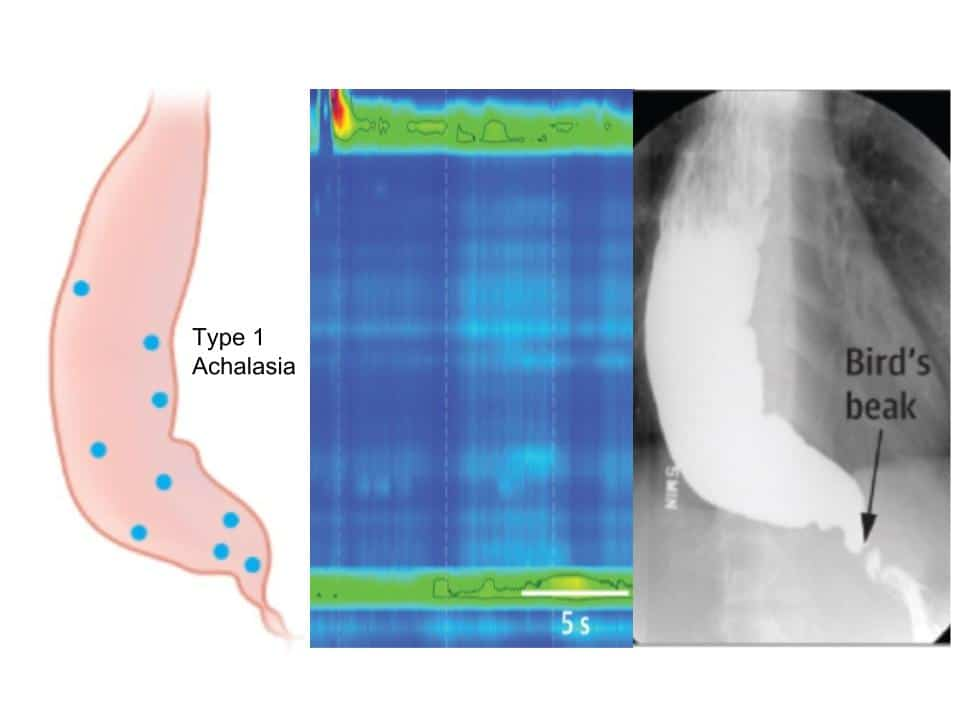
What is the pathophysiology of achalasia? (5)
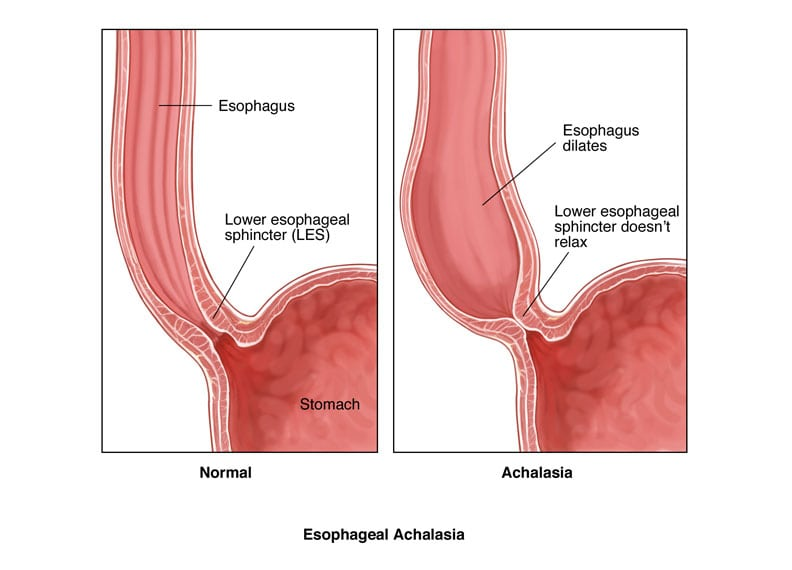
𖹭 Achalasia occurs at a rate of 1 per 100,000 individuals and can present at any age
Findings may include:
𖹭 Impaired relaxation of the lower esophageal sphincter (LOS), often accompanied by spasms
𖹭 Impaired peristalsis, resulting in sphincter spasms
𖹭 Food and liquids fail to reach the stomach due to delayed opening of the LOS
𖹭 This leads to dilation of the esophageal body with distal narrowing, giving rise to a "bird’s beak appearance" of the barium-filled esophagus on esophagram
𖹭 Patients may experience sporadic dysphagia (difficulty swallowing) over a long period and regurgitation of food
What are the causes of achalasia? (4)
𖹭 Disorders of motility or peristalsis of the esophagus, involving impaired motor function of the upper oesophageal sphincter (UOS), oesophageal body, and lower oesophageal sphincter (LOS)
𖹭 Damage to the innervation of the esophagus
𖹭 Degenerative lesions affecting the vagus nerve and loss of myenteric plexus ganglionic cells in the esophagus
𖹭 The exact initiating factor is unknown, but it is believed to be autoimmune or triggered by infection
What are the symptoms of achalasia? (6)
𖹭 Dysphagia: Difficulty or pain during swallowing
𖹭 Vomiting/regurgitation: Backflow of food or liquid from the stomach
𖹭 Heartburn: Retrosternal burning sensation attributed to oesophageal dysmotility, possibly due to:
𖹭 Retention of ingested (acidic) food
𖹭 Generation of lactic acid from the decomposition of retained food
𖹭 Retention of small quantities of gastric acid refluxed into the esophagus due to poor emptying and incomplete relaxation of the lower oesophageal sphincter (LOS)
What is the purpose of oesophageal manometry? (3)
Oesophageal manometry is performed too:
𖹭 Determine the cause of non-cardiac chest pain
𖹭 Evaluate the cause of gastro-oesophageal reflux (regurgitation) of stomach acid and other contents into the esophagus (GORD)
𖹭 Assess the cause of difficulty swallowing food, including the proper function of the upper oesophageal sphincter (UOS) and lower oesophageal sphincter (LOS)
What does oesophageal manometry assess? (3)
Oesophageal manometry evaluates:
𖹭 The strength and coordination of muscle contractions in the esophagus
𖹭 The relaxation function of the lower oesophageal sphincter (LOS)
𖹭 Overall, it assesses whether the esophagus is contracting and relaxing properly
How are the results of oesophageal manometry interpreted? (3)

The interpretation of results includes:
𖹭 A normal pressure of the lower oesophageal sphincter (LOS) is <26 mm Hg
𖹭 100 mm Hg is considered indicative of achalasia, while >200 mm Hg suggests nutcracker achalasia
𖹭 Low LOS pressure may suggest GORD, but it's essential to note that GORD can occur even with normal LOS pressure
What are normal results of oesophageal manometry? (3)
Normal results of oesophageal manometry include:
𖹭 Normal lower oesophageal sphincter (LOS) pressure and muscle contractions during swallowing
𖹭 Muscle contractions follow a normal pattern down the esophagus
𖹭 Normal pressure of the LOS is about 15 mmHg, but it relaxes to less than 10 mmHg to allow food passage into the stomach. 𖹭 However, if the LOS pressure remains less than 10 mmHg without food passage, gastro-oesophageal reflux disease (GORD) may be suspected
What are abnormal results of oesophageal manometry? (3)
Abnormal results of oesophageal manometry are characterized by:
𖹭 Muscle spasms in the oesophageal body
𖹭 Weak contractions along the length of the esophagus
𖹭 In achalasia, the lower oesophageal sphincter (LOS) pressure is high, and the LOS fails to relax after swallowing, indicating a lack of coordinated relaxation in response to swallowing
What is reflux like in normal individuals? (3)
𖹭 Brief and relatively infrequent
𖹭 Occurs after meals due to transient spontaneous lower oesophageal sphincter (LOS) relaxation (TSR)
𖹭 Typically stimulates salivation, which serves as a natural antacid by diluting and neutralizing refluxed gastric acid
How does saliva contribute to managing reflux?
Saliva, stimulated by reflux, acts as an effective natural antacid by:
𖹭 Diluting and neutralizing refluxed gastric acid
What factors can lead to gastro-oesophageal reflux disease (GORD) in individuals with normal reflux patterns? (2)
𖹭 A low rate of salivation.
𖹭 Inability to swallow one's own saliva, leading to prolonged contact of refluxed material with the esophagus.
What is gastro-oesophageal reflux disease (GORD)? (2)
𖹭 GORD refers to the retrograde movement of gastric contents into the esophagus, primarily due to prolonged relaxation of the lower oesophageal sphincter (LOS)
𖹭 It is characterized by more frequent and troublesome reflux episodes compared to normal reflux patterns
What are the consequences of GORD? (3)
𖹭 Oesophageal irritation and damage
𖹭 Chronic oesophagitis, which can be erosive or non-erosive, with a prevalence of approximately 30%
𖹭 Angina-like chest pains, especially after meals
What are the symptoms of gastro-oesophageal reflux disease (GORD)? (6)
𖹭 Heartburn: Retrosternal pain resembling angina
𖹭 Coughing due to reflux irritating the larynx
𖹭 Poor sleep quality, often waking up at night
𖹭 Belching
𖹭 Regurgitation
𖹭 Dysphagia (difficulty swallowing)
What are the causes of reflux in individuals with gastro-oesophageal reflux disease (GORD)? (3)
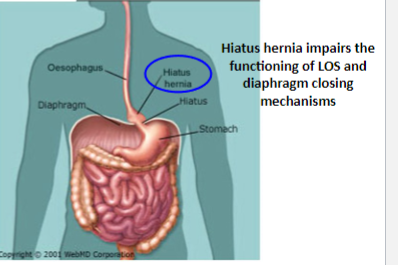
𖹭 Transient spontaneous lower oesophageal sphincter (LOS) relaxation (TSR)
𖹭 Weak resting pressure of the LOS, insufficient to resist the pressure within the stomach
𖹭 Sudden and sustained relaxation of the LOS that is not induced by swallowing
What is transient spontaneous LOS relaxation (TSR)?
𖹭 The sudden and often sustained relaxation of the lower oesophageal sphincter (LOS) that occurs spontaneously, without being triggered by swallowing
𖹭 It contributes to the retrograde movement of gastric contents into the esophagus, particularly in individuals with gastro-oesophageal reflux disease (GORD)
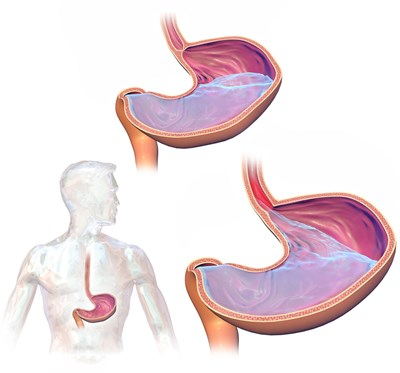
How does malfunction of the extrinsic and intrinsic components of the lower oesophageal sphincter (LOS) contribute to GORD? (2)
𖹭 Allowing for increased susceptibility to transient spontaneous LOS relaxation (TSR)
𖹭 Resulting in a weakened LOS that cannot effectively resist the pressure within the stomach, facilitating reflux
What factors contribute to the severity of gastro-oesophageal reflux disease (GORD)? (8)
𖹭 Weak or uncoordinated oesophageal contractions, leading to poor oesophageal peristalsis and reduced clearance of gastric acid
𖹭 Prolonged duration of contact between refluxed digestive contents and the oesophagus
𖹭 Impaired gastric emptying, which can independently cause severe GORD
𖹭 Increased gastric acid secretion, combined with the presence of bile in gastric contents, leading to severe oesophageal damage
𖹭 Reduced functional lower oesophageal sphincter (LOS) tone or absence of resting LOS tone, particularly when lying flat or during pregnancy
𖹭 Certain dietary factors, such as consuming heavy meals or lying down (supine) after eating
𖹭 Use of certain medications
𖹭 Conditions such as pregnancy/obesity
How does weak or uncoordinated oesophageal contractions contribute to GORD severity?
𖹭 Weak or uncoordinated oesophageal contractions lead to poor oesophageal peristalsis, resulting in reduced clearance of gastric acid and prolonged contact between refluxed contents and the oesophagus, exacerbating GORD severity
What role does impaired gastric emptying play in GORD severity?
𖹭 Impaired gastric emptying can independently cause severe GORD by prolonging the duration of contact between gastric contents and the oesophagus, leading to increased severity of reflux symptoms
How is suspected heartburn or gastro-oesophageal reflux disease (GORD) investigated? (4)
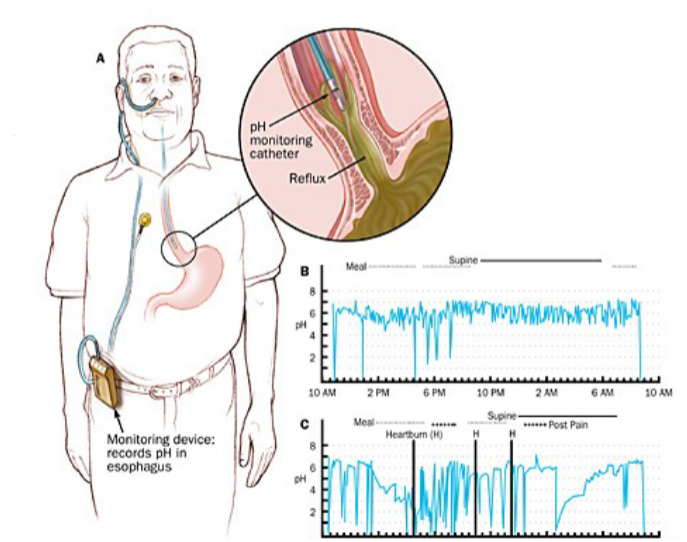
Suspected heartburn or GORD can be investigated through:
𖹭 Low-dose proton pump inhibitor (PPI) challenge
𖹭 Upper gastrointestinal (GI) endoscopy
𖹭 Manometry
𖹭 24-hour ambulatory pH monitoring
What does continuous pH monitoring reveal in the investigation of GORD? (2)
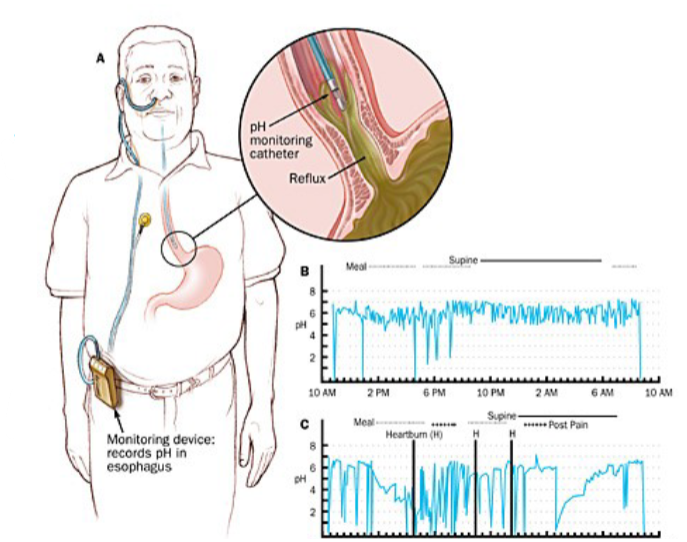
𖹭 Continuous pH monitoring provides insights such as:
𖹭 Most normal individuals (non-refluxers) experience daily reflux episodes
𖹭 GORD is characterized by reflux episodes exceeding those experienced by non-refluxers
How does pregnancy contribute to gastro-oesophageal reflux disease (GORD)? (3)
𖹭 During the last trimester of pregnancy:
𖹭 Increased abdominal pressure forces gastric contents into the oesophagus
𖹭 The growing fetus exerts pressure on abdominal contents, pushing the terminal segments of the oesophagus into the thoracic cavity
𖹭 Heartburn typically subsides in the final months of pregnancy as the uterus descends into the pelvis
What are the management and drug treatment options for gastro-oesophageal reflux disease (GORD)? (6)
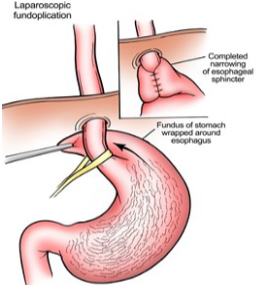
𖹭 Lifestyle changes such as raising the head of the bed at night, weight loss, and modifying food intake
𖹭 Decreasing intake of foods and drinks that exacerbate symptoms
𖹭 Anti-reflux surgery, particularly fundoplication, which involves wrapping the fundus around the lower oesophageal sphincter (LOS)
𖹭 Antacids
𖹭 H2 receptor antagonists and proton pump inhibitors
𖹭 Metoclopramide or domperidone, which may enhance peristalsis and aid in gastric acid clearance
What lifestyle changes can alleviate the symptoms of GORD? (5)
𖹭 Avoiding large meals
𖹭 Weight loss for those who are overweight
𖹭 Avoiding foods that increase gastric acidity or slow gastric emptying, such as fatty foods
𖹭 Avoiding lying down after meals and elevating the head of the bed
𖹭 Avoiding certain medications and smoking
How do antacids function in the treatment of gastro-oesophageal reflux disease (GORD)? (2)
Antacids work by:
𖹭 Neutralizing gastric acid, thereby increasing the pH of the gastric lumen
𖹭 Inhibiting peptic activity and reducing acid secretion
What are the potential side effects of antacids, and how can they be mitigated? (3)
Potential side effects include:
𖹭 Magnesium salts may cause diarrhoea
𖹭 Aluminium salts may cause constipation
𖹭 To mitigate these effects, a combination of both magnesium and aluminium salts is often used to ensure proper bowel function
How are alginates used in conjunction with antacids for the treatment of oesophageal reflux? (2)
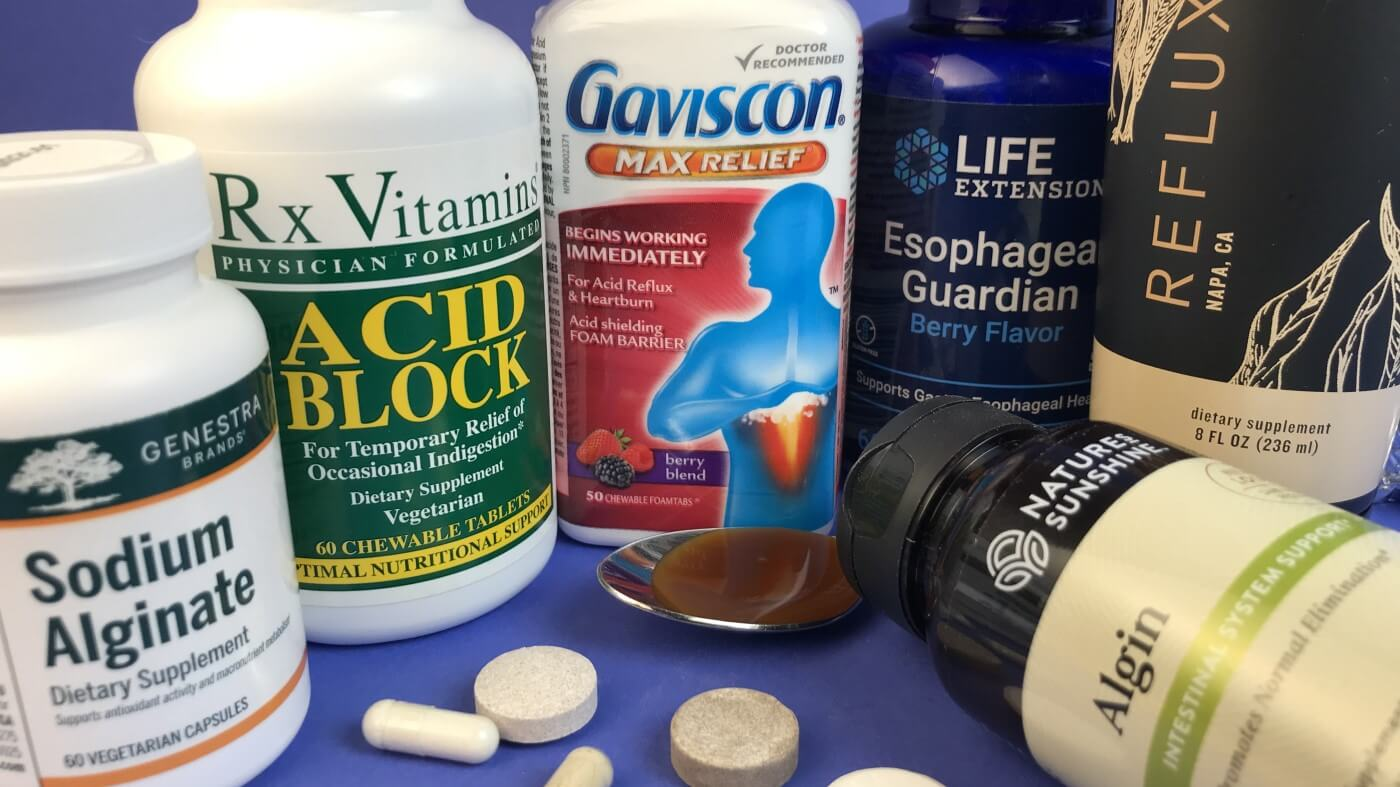
𖹭 Alginates, such as Gaviscon, are combined with antacids to address oesophageal reflux
𖹭 Alginic acid, when combined with saliva, forms a raft that floats on the contents of the gastric lumen, protecting the oesophageal mucosa from reflux
Besides reducing acid secretion and aiding ulcer healing, what is another essential aspect for preventing ulcer recurrence?

𖹭 Removal of H. pylori infection is essential to prevent ulcer recurrence, even with the use of acid-reducing agents
What are the complications of gastro-oesophageal reflux disease (GORD)? (4)
𖹭 Desquamation of oesophageal cells due to acid reflux, resulting in injury to the squamous mucosa
𖹭 Increased cell loss leading to basal cell hyperplasia
𖹭 Excessive desquamation may lead to ulceration, which can haemorrhage, perforate, or heal by fibrosis with strictures
𖹭 Long-term complications may include Barrett's oesophagus and oesophageal cancer
What are the potential long-term effects of gastro-oesophageal reflux disease (GORD)? (4)
𖹭 Oesophagitis and oesophageal strictures
𖹭 Squamous cell carcinoma
𖹭 Barrett's syndrome, which may predispose someone to oesophageal adenocarcinoma
𖹭 Oesophageal ulcers
When should manometry be ordered for patients experiencing symptoms? (2)
𖹭 Heartburn or nausea after eating (indicative of GORD)
𖹭 Problems swallowing, including the feeling that food is stuck behind the breastbone (suggestive of achalasia)
How is achalasia diagnosed? (5)
Diagnosis of achalasia involves:
Examination and patient history evaluation to identify swallowing disorders.
Considering patient-reported symptoms to guide further diagnostic tests.
Note: Some swallowing abnormalities may be common in the elderly.
Diagnostic tests include:
Barium radiography (barium swallow): Identifies dilatation of the oesophagus with a characteristic beak deformity at the lower end.
Oesophageal manometry: Typically reveals absent peristalsis.
Achalasia is characterized by distal narrowing (bird's beak appearance) of the barium-filled oesophagus on oesophagram
Oesophageal manometry: why do it? (3)
𖹭 To determine the cause of non-cardiac chest pain
𖹭 To evaluate the cause of reflux (regurgitation) of stomach acid and other contents back up into the oesophagus (GORD?)
𖹭 To determine the cause of difficulty of swallowing food (does UOS/LOS contract and relax properly?)
What does oesophageal manometry evaluate? (3)
𖹭 Strength and coordination of muscle contractions in the oesophagus
𖹭 Relaxation function of LOS
𖹭 Overall, test evaluates if the oesophagus is contracting and relaxing properly
Interpretation of oesophageal manometry results: LOS pressure (4)
𖹭 Pressure of LOS <26 mm Hg is normal
𖹭 Pressure of LOS >100 mm Hg is considered achalasia
𖹭 Pressure of LOS >200 mm Hg is nutcracker achalasia
𖹭 Low LOS pressure suggests GORD, but GORD can occur in individuals with normal LOS pressure
Normal results of oesophageal manometry (3)
𖹭 Normal LOS pressure and normal muscle contractions upon swallowing
𖹭 The muscle contractions follow a normal pattern down the oesophagus
𖹭 Normal pressure of the LOS is about 15 mmHg, but:
When the LOS relaxes to let food pass into the stomach, the pressure is less than 10 mmHg
In the absence of food passing through, LOS pressure less than 10 mmHg may suggest GORD
Abnormal results of oesophageal manometry (3)
𖹭 Presence of muscle spasms in the oesophageal body
𖹭 Presence of weak contractions along the length of the oesophagus
𖹭 Achalasia is characterised by high LOS pressure and the LOS failing to relax after swallowing
Lack of coordinated LOS relaxation in response to swallowing
What is Gastro-oesophageal reflux disease (GORD)? (5)
𖹭 GORD is the retrograde movement of gastric content into the oesophagus due to prolonged relaxation of the LOS
𖹭 GORD occurs when reflux is more frequent and troublesome
𖹭 GORD causes oesophageal irritation and oesophageal damage
𖹭 Chronic oesophagitis (erosive or non-erosive) has a 30% prevalence
𖹭 GORD causes a burning sensation in the chest (angina-like pains), often after meals
Symptoms of GORD (5)
𖹭 Heartburn – retrosternal pain (angina-like pains)
𖹭 Coughs (reflux irritates the larynx); poor sleep due to waking up at night
𖹭 Belching
𖹭 Regurgitation
𖹭 Dysphagia
Causes of reflux in those with GORD (3)
𖹭 Transient spontaneous LOS relaxation (tsr)
𖹭 Resting LOS pressure is too weak to resist the pressure within the stomach
𖹭 Sudden (& sustained) relaxation of the LOS that is not induced by swallowing
Recap: Malfunction of extrinsic and intrinsic components of LOS → GORD (1)
𖹭 Malfunction of extrinsic and intrinsic components of LOS leads to GORD
Factors that contribute to the severity of GORD (8)
𖹭 Weak or uncoordinated oesophageal contractions/poor oesophageal motor activity, leading to poor oesophageal peristalsis and decreased clearance of gastric acid
Prolonged duration of contact of refluxed digestive contents with oesophagus
𖹭 Length of time the oesophagus is exposed to gastric acid
Impaired gastric emptying alone can cause severe GORD
𖹭 Increased gastric acid secretion coupled with the presence of bile in gastric contents, leading to severe oesophageal damage
𖹭 Amount of pressure placed on the anti-reflux barrier and less functional LOS or resting LOS tone is low or absent
LOS tone fails to increase when lying flat or during pregnancy
𖹭 Certain foods and lying down (supine) after eating a heavy meal
𖹭 Certain drugs
𖹭 Pregnancy
𖹭 Obesity
Investigating GORD (4)
𖹭 Low dose proton pump inhibitor (PPI) challenge
𖹭 Upper GI endoscopy
𖹭 Manometry
𖹭 24-hour ambulatory pH monitoring
Findings from continuous pH monitoring (2)
𖹭 24-hour pH monitoring shows that most normal individuals (non-refluxers) reflux on a daily basis
𖹭 GORD implies not just the presence of reflux, but reflux in excess of that experienced by non-refluxers
Pregnancy and GORD (3)
𖹭 Last trimester of pregnancy is associated with increased abdominal pressure, which forces gastric contents into the oesophagus
𖹭 The foetus increases pressure on abdominal contents, pushing terminal segments of the oesophagus into the thoracic cavity
𖹭 Heartburn subsides in the last months of pregnancy as the uterus descends into the pelvis
Management and drug treatment of GORD (8)
𖹭 Life-style changes: raise the head of the bed at night, weight loss, modify food intake
𖹭 Decrease intake of foods and drinks that cause symptoms
𖹭 Anti-reflux surgery (fundoplication – wrap fundus around LOS)
Caution: Fundoplication can cause dysphagia as it reduces the distensibility of LOS
𖹭 Antacids
𖹭 H2 receptor antagonists
𖹭 Proton pump inhibitors
𖹭 Metoclopramide – may enhance peristalsis and help with gastric acid clearance
𖹭 Domperidone – may enhance peristalsis and help with gastric acid clearance
List of lifestyle changes that help alleviate the symptoms of GORD (7)
𖹭 Some people need to avoid large meals
𖹭 Lose weight (if overweight)
𖹭 Avoid foods that increase gastric acidity
𖹭 Avoid foods that slow gastric emptying (decrease fat intake)
𖹭 Avoid lying down after meals - elevate the head of the bed
𖹭 Avoid some drugs and smoking
𖹭 Implement lifestyle changes based on knowledge of what aggravates symptoms
Use of antacids in the treatment of GORD (7)

𖹭 Antacids neutralize gastric acid and increase pH of gastric lumen
𖹭 Antacids inhibit peptic activity and stop acid secretion
𖹭 Magnesium salts may cause diarrhoea
𖹭 Aluminium salts may cause constipation
𖹭 Use a mixture of both to ensure bowel function
𖹭 Combine alginates (e.g. Gaviscon) with antacids for oesophageal reflux
𖹭 Alginic acid + saliva form a raft which floats on the content of gastric lumen and protects the oesophageal mucosa from reflux
Complications of GORD (5)
𖹭 Acid reflux causes desquamation of oesophageal cells (injury of squamous mucosa)
𖹭 Increased cell loss leads to basal cell hyperplasia
𖹭 Excessive desquamation can result in ulceration
𖹭 Ulcers may hemorrhage, perforate, or heal by fibrosis with strictures
𖹭 Complications may lead to Barrett’s oesophagus and oesophageal cancer
Potential long-term effects of GORD (4)
𖹭 Oesophagitis, oesophageal strictures
𖹭 Squamous cell carcinoma
𖹭 Barrett's syndrome, which may predispose someone to oesophageal adenocarcinoma
𖹭 Oesophageal ulcer
When should manometry be ordered for patients experiencing symptoms? (2)
𖹭 Heartburn or nausea after eating (GORD)
𖹭 Problems swallowing, including the feeling that food is stuck behind the breastbone (achalasia)