Vitamin D deficiency

*1880-1920, 90% of children in parts of Europe and in Boston had rickets (industrialization era)
- smoke from coal-burning fires absorbed much of UV portion of sunlight which was needed to produce vitamin D in the skin
**In 1921 it was discovered that if you exposed children to UV light, symptoms of rickets disappeared.
Thiamin deficiency
Beri beri
- 1st medical link to this dietary deficiency was made by a Japanese doctor who observed the symptoms in Japanese navy crew who ate only polished white rice but not in crew who got meat, beans and barley
- Polished rice with husk, bran and germ removed = strips nutrients
- Fatigue, together with complications affecting the cardiovascular, nervous, muscular, and GI systems
Niacin deficiency
Pellagra- three ‘D’s: dermatitis, diarrhea, dementia
- early 1900’s in the southeastern USA, cotton economy failed, and people ate corn as a staple
- niacin in corn is tightly bound and not very available for absorption
- 1907-1940 in USA (3 million cases, 100,000 deaths)
Vitamin A deficiency

- Leading cause of preventable childhood blindness and increases the risk of death from common childhood illnesses such as diarrhea
-Night blindness is one of the first signs of vitamin A deficiency
Vitamin A two compounds
- Beta-Carotene (precursor to vitamin A – plant foods)
- Retinol (pre-formed vitamin A – animal foods)
Beta-Carotene
(precursor to vitamin A – plant foods)
• Dark green vegetables
• Deep orange fruits and vegetables
• No upper tolerable limit but high intakes may turn skin yellow-orange
Retinol
(pre-formed vitamin A – animal foods)
• Animal products with fat (meat, fish, etc.)
• Vitamin A derivative (retinoids) used in some acne medications (dangerous for developing fetus
– miscarriage, severe birth defects, death). Avoid getting pregnant for 4 weeks after use
Iodine deficiency

Goiter
- Iodine is an element that is needed for production of thyroid hormone
- If deficient, leads to hypothyroidism = weight gain, inability to tolerate cold, fatigue
- Can lead to intellectual disabilities in children if mother was deficient during pregnancy
- Approximately 30% of the world’s population remains at risk for iodine deficiency
Water-Soluble Vitamins
• The B vitamins and vitamin C
• Due to water solubility, they “wash out” of the body in one to several days
– Except for B 12 as it can be stored up to one year in the liver
– This does not make them safe in high doses...
• Vitamin B 6, niacin and C can be toxic in high doses
• “Megadoses” stress the kidney
• Water soluble vitamins are easily destroyed during food storage and preparation
Minimizing Nutrient Losses:
1. Refrigerate fruits & vegetables
2. To minimize oxidation, reduce contact with air
3. Wash fruits & vegetables before cutting
4. To minimize cooking losses, steam or stir-fry vegetables. Avoid high temperature for long time.
Where is folate (natural form) and folic acid (synthetic form) found?
• Leafy green vegetables
• Legumes
• Liver
• Lentils
• Fortified grain products
*Most common food source is enriched or fortified food products.
*Synthetic folic acid more bioavailable than naturally occurring food folate.
Lack of Folate
1. DNA stability
2. Heart health
3. Fetal health
Lack of folate reduces DNA stability
- folate deficiency induces and accelerates carcinogenesis
- structure of cell’s genetic material becomes disrupted --> accumulate abnormalities --> cancer
Heart health due to lack of folate
- lack of folate causes homocysteine to accumulate in blood
- high homocysteine --> heart attacks, strokes
Fetal health and lack of folate

- Almost complete absence of spinal cord and brain deformities (neural tube defects) in babies born to mothers consuming inadequate folate.
- The two most common neural tube defects are spina bifida (treatable) and anencephaly (fatal – portion of brain and skull missing).
- Intakes should be:
400 μg all females600 μg pregnant4 mg previous neural tube defect
***WHY THEY ADDED FOLIATE IN BREAD
Vitamin C as an antioxidant
- protects tissues from oxidative stress
- oxidative stress is caused by free radicals that are produced in response to normal metabolism using oxygen; UV radiation; air pollution; tobacco smoke
- over time lead to increased risk of cancer, heart disease and arthritis
- Vitamin C along with vitamin E and other phytochemical found in fruits and vegetables neutralize free radicals
What are free radicals?
They donate electrons to unstable molecule to stabilize them, to dampen the damage of free radicals
Vitamin C as a Cofactor in collagen formation
- helps form collagen
- fibrous structural protein of connective tissues (bones, teeth, blood vessels, wounds)- assists in preventing bruising
– with vit.C deficiency tissue hemorrhage or bleeding is a major symptom
Vitamin C as a Cofactor in other reactions
- conversion of tryptophan --> serotonin (controls mood) & norepinephrine (increase heart rate)
- fatty acid transport into mitochondria for energy metabolism
- making of hormones (e.g. thyroxine)
Vitamin C in stress
- adrenal glands contain more vitamin C than any other organ
- released with stress hormones during stress reaction
- stresses: infections, burns, toxic heavy metals, chronic aspirin, barbiturates (sedatives), oral contraceptives, cigarette smoking (also B6, B12, folate)
Vitamin C role in the common cold
- 1 g/day of vitamin C led to 1 day shorter cold & reduced severity of symptoms (by 23%)
- vitamin C reduces blood histamine but at a dose of 2 g daily for 2 wks
Body's need for vitamin C
- body’s need: 10 mg prevent scurvy
- DRI: females 75 mg/d; males 90 mg/d
- excess: nausea, diarrhea, abdominal cramps, excessive gas
Vitamin D bone growth
- raises blood concentrations of Ca & phosphorus
1) increases absorption from intestine
2) increases reabsorption from kidneys
3) mobilization from bones into blood
Cancer and vitamin D
- recent research: breast, prostate, colon decreases with increased vitamin D intake
Multiple sclerosis; rheumatoid arthritis and vitamin D
- living higher than 37º latitude increases MS risk >100%
- 400 IU supplement decreases risk by 40%
Vitamin D synthesis and activation
* Production in the skin needs 10-15 min sunlight (UVB) on arms & face 2-3x per wk (dark pigment may require up to 3 hr)
What food sources contain vitamin D
• Fortified dairy foods
• Fortified margarine
• Fish oils
• Egg yolk
* fluid milk is most reliable source
Where do we see a reduced production in vitamin D?
1) 70 years and older - vitamin D production is only 30% of younger adults
2) institutionalized individuals at high risk
3) sunscreen - reduce or block vit. D synthesis, but not completely
* 15 min exposure early morning or late afternoon without sunscreen produces all that is required for a day
Phytochemicals
Biologically active compounds of plants believed to confer resistance to chronic disease
Phytochemicals in plants:
– Give pigmentation and flavor
– Promote chemical reactions/used in metabolism
– Protect them from bacteria, fungi, animals and environmental oxidants
Are phytochemicals essential?
• None of the phytochemicals are essential
• Deficiency symptoms are not observed if we do not consume them
Are phytochemicals super good for us?
• Many have protective and antioxidant properties that make them useful to our tissues
– Via antioxidant or anti-inflammatory effects
• Others are toxic to us– Too much is not better!
What do many phytochemicals protect us from?
– Cancer
– Heart disease
– High blood pressure
– Other chronic diseases
The correct balance of phytochemicals is unknown, but to get adequate levels, we need to
– Follow the advice in Canada’s Food Guide and
– Eat a variety: don’t eat the exact same foods every day
What causes free radicals
Cause:
- sun
- air pollution
- ionizing radiation
- metabolism
- smoking
How do antioxidants work?
protect cells against oxidative damage and reduce the risk of developing certain types of cancer. Phytochemicals with antioxidant activity: allyl sulfides (onions, garlic), carotenoids (carrots, tomatoes), flavonoids (berries), polyphenols (tea, grapes).
How do antioxidants affect estrogen?
• Hormonal action - Isoflavones, found in soy, imitate human estrogens and help to reduce menopausal symptoms and osteoporosis.
• Stimulation of enzymes - Indoles, which are found in cabbages & broccoli, stimulate enzymes that make estrogen less effective and could reduce the risk for breast cancer.
How do antioxidants interact with DNA?
Interference with DNA replication - Saponins found in beans interfere with the replication of cell DNA, thereby preventing the multiplication of cancer cells. Capsaicin, found in hot peppers, protects DNA from carcinogens.
What is the physical action of antioxidants?
Some phytochemicals bind physically to cell walls thereby preventing the adhesion of pathogens to human cell walls. Proanthocyanidins are responsible for the anti-adhesion properties of cranberry. Consumption of cranberries will reduce the risk of urinary tract infections and will improve dental health.
Food vs. Phytochemical Pill
1. In large doses, phytochemicals may be toxic.
2. Up to 10,000 phytochemicals identified. Cannot all be isolated and put into supplement.
3. Health benefits are associated with foods and often not supplements.
4. Many supplements are untested and some phytochemical supplements may actually harm health (e.g. beta-carotene).
- isolation may worsen rather than benefit, without other substances
Harmful plant antioxidant of potatoes:
Solanine – when potatoes are exposed to light, they turn green = natural defense against insects eating them (bitter)– diarrhea, vomiting, headache, paralysis
Harmful plant antioxidant: Aflatoxins
Aflatoxins from Aspergillus fungi growing on nuts/peanuts, dried foods, grains, and spices, which can cause liver cancer with chronic exposure. Testing done by CFIA. Discard nuts/peanuts that look moldy, discolored or shriveled.
Harmful plant antioxidant: Oxalic acid
from spinach, turnip greens, rhubarb, and other foods can bind to calcium and irritate the stomach; cause kidney stones
Harmful plant antioxidant: Phytates
found in whole grains and legumes
– bind minerals (iron and zinc); cooking, baking, sprouting, fermentation can reduce phytates
Food Biotechnology examples
A. Selective BreedingB. Genetic Engineering
Selective breeding
* selectively breeding crops & animals for centuries
* examples: wild corn = 5 kernels/stalk: super-sweet corn: leaner animals: chickens used to lay 50 eggs/year today they lay 245 eggs/year
Genetic Engineering
* modifying genetic material of living cells so they produce newsubstances or perform new functions* insert gene from one organism into another
Benefits of biotechnology
1. extend shelf life
2. efficient food processing
3. biopharming
4. improved nutrient composition
5. genetically assisted agriculture
Biotechnology and extended shelf life
* tomatoes stay firm & ripe longer
* “antisense” (mirror image) gene* binds to native gene and prevents synthesis of softening protein (in tomatoes)
* harvested at more flavorful, nutritious vine-ripe stage
Biotechnology and efficient food processing
* rennin - coagulate milk in cheese production
* traditionally from calf stomach
* today mass produced in bacteria
* save time, money & space
* in the future : lactose free milk?: decaf coffee bean?
Biotechnology and biopharming
* use animals & plants to produce drugs:
- cow produce vaccine in milk
- use bananas to make edible vaccine
- hydroponically grow tomato plants to secrete desired protein through roots into water
Biotechnology and improved nutrient composition
* soybeans: upgrade protein quality
* canola: increase monounsaturated fatty acids
* “golden rice”: genes from daffodil & bacteria to make beta-carotene
• 1.15 million child deaths are precipitated by vitamin A deficiency each year.
• One cup could supply 50% of the RDA of vitamin A for an adult
Biotechnology and genetically assisted agriculture
* 90-95% of canola crops in Canada are GM to withstand herbicides (not just for food also lip gloss, soap, others)
* farmer can spray whole field, kill weeds & not harm canola
* Canada = soy, corn, canola, sugar beets, alfalfa (imports = USA squash and 80% of Hawaiian papayas)
* hypoallergenic peanuts are being researched
What are the main issues of concern from biotechnology for human health?
• Allergenicity: In principle, the transfer of genes from commonly allergenic organisms to non-allergic organisms is discouraged in the science of GM. No allergic effects have been found relative to GM foods currently on the market.
• Gene transfer: Gene transfer from GM foods to cells of the body or to bacteria in the GI tract is of concern if the transferred genetic material adversely affects human health (e.g. antibiotic resistance genes)
• Outcrossing: The migration of genes from GM plants into conventional crops. Cases have been reported where GM crops approved for animal feed or industrial use were detected at low levels in the products intended for human consumption. Several countries have adopted strategies to reduce mixing, including a clear separation of the fields within which GM crops and conventional crops are grown.
Diet and Cancer
Both sexes: lung cancer is the #1 cancer that causes death
Men: prostate
Women: breast
******How does Cancer work?**********
Leading cause of death in Canada
1. Initiation – carcinogen permanent genetic change in a cell (carries mutation until it’s death)
2. Promotion - compounds cause the initiated cells to divide and accumulate – large number of daughter cells with the mutation
3. Progression – transformation from benign tumor to neoplasm, cells can undergo further mutations with metastatic potential
4. Metastasis - invade surrounding tissues and/or spread
Factors Affecting Cancer Development (4)
A. Genetic factors: affects riskB. Immune factors
C. Environmental factors
D. Dietary factors (initiators, promoters, antipromoters)
Cancer: immune factors
ineffective immune system may not recognize tumor as foreign
- aging decreases immune function- immunosuppressive drugs & viral infections
Cancer: environmental factors
* exposure to radiation & sun
* water & air pollution
* smoking
* lack of physical activity
Cancer: dietary factors - initiators
- carcinogens initiate cancer
- some pesticides at high doses are carcinogenic
- nitrosamines – strong carcinogens
- naturally occurring or formed during processing
* alcohol (beer & scotch)
* processed meats (ham, bacon, deli meats, hot dogs)
- in the stomach, nitrates added as preservative, can combine with amines to form nitrosamines
- linked to stomach, esophagus, liver and bladder cancer
Class One Carcinogens
• Group 1: Carcinogenic to humans
• Group 2A: Probably carcinogenic to humans
• Group 2B: Possibly carcinogenic to humans
• Group 3: Unclassifiable as to carcinogenicity in humans
• Group 4: Probably not carcinogenic to humans
Group 1 vs. group 2 carcinogens
Processed meat (Group 1) refers to meat that has been transformed through salting, curing, fermentation, smoking, or other processes
Red meat (Group 2) refers to beef, veal, pork, lamb, mutton, horse, and goat
Cancer: dietary factors - promoters
- accelerate tumor development once initiating step has occurred
- “lag time” of 10-30 years
- excess dietary fat by contributing to obesity
- omega-6 fatty acids promoters in some animals
How does fat contribute to cancer?
- fat can oxidize at high cooking temperatures (restaurant deep-frying – not so much at home)
------> may produce oxidative stress in body
- more important is time – oils become oxidized over time so buy small bottles and if it smells off – throw away
- fat stimulates bile secretion - bacteria can convert bile to cancer-causing compounds
Cancer: dietary factors - antipromoters
- high fruits & vegetables and decrease cancer risk
- fiber protective against colon cancer
- phytochemicals
- cruciferous vegetables
Recommendations for reducing cancer risk
• Choose diet rich in a variety of plant-based foods- >7 servings of whole grains, legumes, starchy vegetables; 5-10 servings of other vegetables & fruit; limit processed foods & refined sugar
• Maintain healthy weight and be active- avoid under & overweight; 1 hour of exercise daily
• Drink alcohol in moderation, if at all- for cancer prevention, it’s best not to drink alcohol
• Select foods low in fat and salt- limit fatty foods especially of animal origin; limit red meat to 3 portions per week; modest amount of vegetable oil; limit salted foods & table salt (salt-preserved foods damage stomach lining)
• Prepare and store foods safely- do not eat charred food; consume meat/fish grilled in direct flame only occasionally
And most important of all: • Do not smoke or use tobacco in any form
Do HCAs & PAHs increase cancer risk?
• Charring, burning or grilling meat, poultry and fish over high temperatures causes chemicals to form that are mutagenic (damage DNA).
– HCAs form when amino acids, sugars, creatine in muscle meats react at high temperature
– PAHs form when fat or juices from meat grilled over a heated surface or open fire drip onto the surface or fire and cause flames and smoke. Smoke contains the PAHs and thatsticks to the surface of the meat. Also formed during smoking of food.
– Well done more than rare/medium
– High temp (grilling, pan fry) or cooked longer
How to avoid HCAs and PAHs
• do not burn food when cooking by any method and remove charred portions
• marinating meats can help reduce carcinogen formation
• continuously turning meat over on a high heat source rather than leaving it without flipping often
• trim the fat (fat dripping into heat produces harmful smoke that coats the food)
• lower the temperature – “low and slow”; indirect-heat methods like stewing, steaming or poaching produce less than frying or grilling
Factors associated with site specific cancers:
1. Stomach:
2. Colorectal:
3. Liver:
4. Lung:
5. Breast
6. Prostate:
1. Stomach: salt-preserved foods; possibly grilling & BBQ-ing
2. Colorectal: saturated fat, red meat, alcohol; possibly grilling
3. Liver: alcohol; hepatitis B
4. Lung: smoking; possibly alcohol, saturated fat, cholesterol
5. Breast: obesity, early puberty, alcohol; possibly meat & fat
6. Prostate: high fat intake (especially from meat)
Single gene defects
- hundreds of diseases related to single gene defects
* PKU (phenylketonuria)
* cystic fibrosis
* sickle cell anemia
* hemochromatosis
- but most diseases are a combination of multiple genes and environment
Polygenic defects possibilities
1. Heart disease
2, Cancer
3. Hypertension
4. Obesity
Heart disease (Polygenic defects)
- high cholesterol diets --> plaque in some people- low folate & vegetable diets increase risk
Cancer (Polygenic defects)
- differs by site- endometrial [environment = 90%]- stomach [72% environment]- prostate [42% environment]
Hypertension (Polygenic defects)
- salt sensitivity = eating too much salt usually increases BP but not in everyone- salt sensitive or salt resistant
Obesity (Polygenic defects)
- Over 120 genes associated with development
Celiac disease
• An autoimmune disease that damages the small intestine• People with celiac disease have an immune reaction to a protein called gluten• Gluten is in wheat, barley, and rye• When people with celiac disease consume gluten, the immune system attacks and destroys the villi
Symptoms of celiac
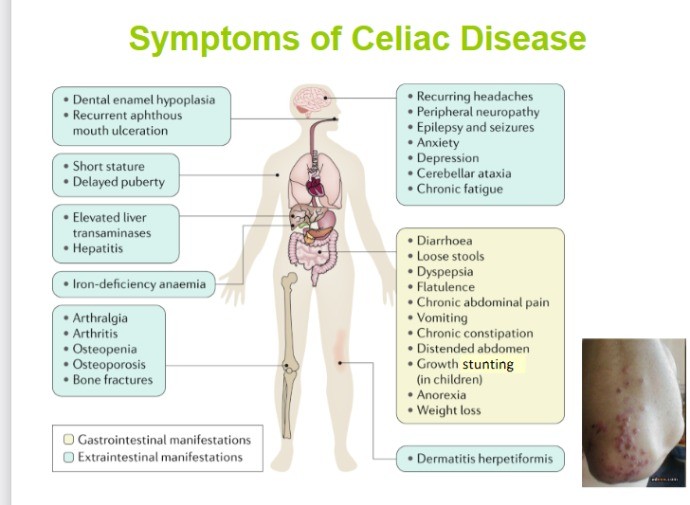
Genetic link to celiac
• Celiac disease occurs in genetically predisposed people
• HLA genes (human leukocyte antigen)
• Responsible for how the immune system distinguishes between the body’s proteins and foreign proteins
• ~99% of people with celiac disease and 60% with non- celiac gluten sensitivity have DQ2 or DQ8 risk version of HLA (but 30% of the general population have the risk version so development of the disease is dependent on the combination of risk variants)
3 types of celiac disease
Classical: signs malabsorption, including diarrhea, steatorrhea (pale, foul-smelling, fatty stools), and weight loss or growth failure in children.
Non-classical: mild gastrointestinal symptoms without clear signs of malabsorption or may have seemingly unrelated symptoms.
Silent: Patients do not complain of any symptoms, but still experience villous atrophy damage to their small intestine.
Celiac disease prevalence
• In Canada, about 1% of population is affected
– Genetic component: if a 1st degree relative has celiac disease, 1 in 10 chance family member will develop it
• Many people go undiagnosed but testing can involve:
– Blood test: tTG-IgA (tissue transglutaminase antibodies)
**must be on gluten-containing diet – how long?
– Small intestine biopsy
– Genetic screening
• Commonly misdiagnosed as:
– IBS (irritable bowel syndrome)
– Crohn’s disease
Non-Celiac Gluten Sensitivity
Develop symptoms when they consume gluten-containing foods and feel better on a gluten-free diet but do NOT have celiac disease.
- There are no biomarkers for diagnosis- Autoantibodies (TTG, EMA, DGP) are absent
- There is no villous atrophy (although newer work suggests there may be intestinal damage)
Why get an accurate diagnosis for celiac disease?
- you may pass it on
- so you know if you should avoid gluten
- uncontrolled = 2x more likely to get heart disease, 4x more likely to get colon cancer
Non-celiac gluten sensitivity triggers
Other compounds in wheat, barley and rye may trigger symptoms (e.g. proteins called amylase/trypsin inhibitors or fermentable carbohydrates).
Is eating gluten free healthy for everyone?
NO
Nutrigenomics
• The study of how genes and diet interact to increase or decrease someone’s risk for disease
• Gene × Environment interactions
• Play a role in “personalized nutrition”
What biological sample do you need for nutrigenomics?
- muscle composition
- Type 2 diabetes
- ancestry composition
- Cilantro taste aversion
What are some nutrigenomic companies?
- 23andme
- nutrigenomic (canadian)
Food selection and nutrigenomics
* food preferences largely learned
* 80 genes that help taste bitter foods
* some are highly sensitive
* vegetables taste bitter --> eat less
The future of nutrigenomics
* individualized dietary prescriptions
* complete profile with genetic risks, gut microbiota profiles, etc.
Canada’s Physical Activity Guidelines
ADULTS:
- 150 min. of moderate to vigorous physical activity per week (bouts of 10 min. or more)
- 2 sessions of strength-training per week
CHILDREN:
- 60 min. of moderate to vigorous physical activity everyday
-vigorous at least 3 days per week
-activities that strengthen muscle and bone 3 days per week
Fuel source at rest
85% from fat, 10% from CHO, 5% from protein
Fuel sources during exercise
• During Exercise:
1. Muscle glycogen
2. Blood glucose
3. Plasma fatty acids
4. Intramuscular triglycerides
Extent of contribution depends on:
1. Intensity & duration of exercise
2. Level of exercise training
3. Initial muscle glycogen stores
4. Supplementation with CHO during exercise
Energy Systems
• ATP-Phosphocreatine system
- immediate energy source
- short term, explosive power activities up to 10 sec
• Lactic acid system
- anaerobic breakdown of glucose to lactic acid (glycolysis)
- any intense effort lasting up to 2 min
• Oxygen system
- after 2 min during low to moderate intensity exercise
- glycogen provides 60-70% of fuel during first 20 min of low to moderate intensity exercise
- after 20 min fat increasingly used
Fatigue - “Hitting the Wall”
• Depletion of muscle & liver glycogen levels --> extreme fatigue
• Some carbohydrate is needed by muscles to generate energy from fat breakdown
• Water & glucose ingestion at point of fatigue may prolong exercise but severe limitations exist for high level of energy production needed for exercise
• Inability to maintain current level of activity; perception of effort greatly increased
Daily carbohydrate needs
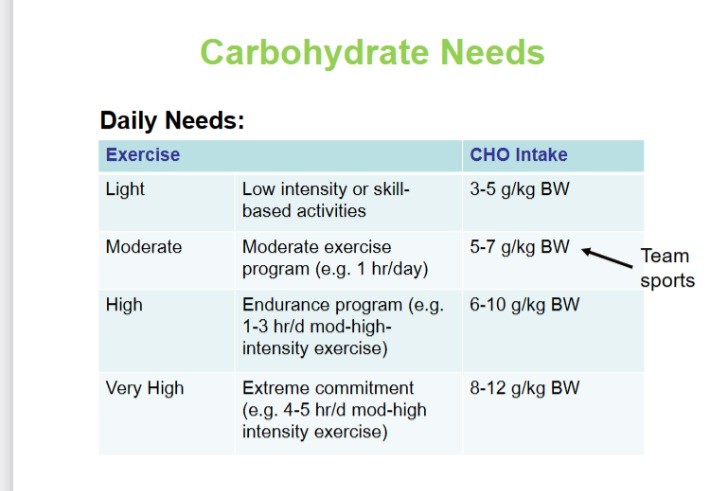
- increases with increased exercise
Light = 3-5g/kg
High = 6-10g/kg
***TEAM sports: 5-7g/kg (moderate)
Carbohydrate Pre-, During, Post- Exercise
1-4 h pre-exercise : 1-4 g/kg body weight
<1 h pre-exercise : If desired, a small amount of easily digested CHO in an amount and form the athlete prefers
During exercise : Team Sports: 30-60 g/hEndurance: depends on duration, up to 90 g/h
< 8 h to recover : 1– 1.2 g/kg/h for 4 hours
> 8 h to recover : Daily fueling plan adequate to restore muscleglycogen
Dietary Protein
Timing of protein intake– Before, During or After?
– “longitudinal training studies currently suggest that increases in strength and muscle mass are greatest with immediate post-exercise provision of protein.”
Amount of protein
– Evidence from systematic review & meta-analysis
– No further performance benefits (strength, muscle mass) when >1.62 g protein/kg/day BUT 95% CI (1.03-2.20 g pro/kg/d)
Pre-Competition Nutrition
Maximize muscle & liver glycogen - endurance
Goals of pre-comp meal:
1. Stomach should be relatively empty at start of competition.
2. Minimize gastrointestinal distress.
3. Avoid hunger, lightheadedness or fatigue.
4. Adequate fuel (carbohydrate) in blood and muscles.
5. Adequate amount of body water.
Practical considerations of pre-competition meal:
3-4 hours before competition: solid meal
– CHO rich with minimal fiber, fat, and protein which can cause GI distress during exercise
– Avoid gas formers and bulky foods like bran.
<1 hour before competition: small or liquid
– Many athletes do well with 25-30 g of CHO
– Research shows even if “rebound hypoglycemia” occurs, it does not impact performance
Ideas for Foods to Consume 1-4 Hours Before Exercise:
•Peanut butter and honey on crackers
•Fruit and yogurt smoothie
•Low-fat cottage cheese
•Yogurt + granola + fruit
•Chicken on a whole-wheat bun
Ideas for Foods to Consumer 30-60 Minutes Before Exercise:
•A piece of fruit
•Whole grain crackers
•Sports gel, sports bar
•Fruit puree pouch like applesauce
Sports Bars:
• Good source of carbohydrate, some fat & protein
• No magical qualities but are convenient
• Should be used as a substitute for a pre-competition meal not on a long-term basis to replace normal healthy eating patterns
Eating During Competition
• Generally not needed, but depends on event
• CHO --> additional energy supply
• Water --> temperature regulation
Eating during endurance sports
<30min = NOT needed
Post-comp eating
• Endurance sports need complex CHO in daily diet
• Immediately post-exercise simple sugars help restore muscle glycogen and adding some protein may enhance storage (ratio of 3:1)
• In general, balanced diet will restore nutritional status after hard physical training
• Resistance training, focus on protein
30-40 g before bed – casein or whey?
casein: slower to digest, less fast absorbed, lasts all night
Ben competed in a triathlon in August. Last year he finished in 2:19 hrs. He hoped to beat that this year. The week before the event, he had trouble getting good nutrition after his training sessions because family from out of town was visiting. On the day of the event this year, it was very hot – this killed his appetite and he didn’t consume any food during the race. He forgot one of his bottles of sports drink he normally has on his bike but still got water from the aid station during the run. Ben finished in 2:41 hrs. What happened?
- inadequate stores
- dehydration
etc.
Infant health:
- low birth weight = < 2.5 kg (5½ lbs.)
- preterm = <37 weeks of pregnancy
The lowest mortality rates occur among infants weighing ____________________
3,000 to 3,500 g (6.6 to 7.7 lb)
Critical Periods
time when cells of a tissue or organ are genetically programmed to multiply
• Critical...cannot correct for the deficiency in cells later
• Nutrients required for cell/tissue development must be available during specific time intervals, if missing developing tissue has fewer cells, forms abnormally, or functions poorly (e.g. cleft palate from too much vit. A)
Critical periods of development in babies
CNS: 2-5.25
Heart: 2.5-5.75
Dutch Hunger Winter (1944-1945)
4.5 million people affected If women were exposed to famine during pregnancy:1. lower birth weight2. offspring had an ↑ risk of diabetes and obesity as adults
**Developmental origins hypothesis
Developmental Origins Hypothesis
• Increased susceptibility to chronic disease is “programmed” by energy or nutrient imbalances during pregnancy
• Fetal tissues in critical phases make adaptations to cope with poor nutrient supply
• Adaptations produce changes in structure and function of tissues (permanent or long-lasting effect)
Weight gain typically depends on a woman’s weight entering pregnancy:
– Underweight: 28 to 40 pounds– Normal-weight: 24 to 35 pounds– Overweight: 15 to 25 pounds– Obesity: 15 to 20 pounds
• Women carrying twins typically gain 37 to 54 pounds
• Weight gained should be gradual and consistent, from a high-quality diet
Nutrition during Pregnancy
A. Calories1st trimester = +0 kcal/d2nd trimester = +340 kcal/d3rd trimester = +450 kcal/d
B. Other nutrients- choose nutrient dense foods- especially folate, iron, calcium
Folate deficiency
• Folate deficiency is associated with fetal growth failure and malformations, and neural tube defects
• Adequate folate early in pregnancy reduces neural tube defects
• 600 μg folate is needed daily before (neural tube forms before 30 days after conception) and during pregnancy
Vitamin A during pregnancy
• Too little = poor fetal growth
• Too much = fetal malformations (facial features and heart)
• Intake of 10,000-15,000 IU of retinol daily is too much
• Limit vitamin A to ~5000 IU/day and take no vitamin A-containing medications
• Beta-carotene, a precursor to vitamin A, is not harmful
Calcium during pregnancy
• Needed for mineralization of bones in fetus
• Supplied by mother’s diet and calcium in long bones of mother’s body
• Low calcium intake means greater calcium losses from maternal bones during pregnancy --- is this Ca regained after delivery?
Vitamin D during pregnancy
• Lack = compromises fetal growth and development
• Vegan women may be at greater risk because vitamin D is naturally found in animal products
• 600 IU is officially recommended for pregnancy and should not exceed 4000 IU (DRI recommendations)
Low iron neonatal and offspring risks

Alcohol and Pregnancy
• Fetal Alcohol Syndrome – permanent condition
• No amount of alcohol is absolutely safe during pregnancy
• To prevent impairments in fetal growth and development, women should not drink alcohol during pregnancy or when trying to get pregnant
Vitamins and Minerals during pregnancy
• Iron and folate are the only supplements recommended for all pregnant women
• Multivitamin-mineral pills are recommended for women who do not consume an adequate diet and for high-risk categories, such as twins, heavy cigarette smokers, and those with alcohol or drug abuse
• 83% of pregnant women take multiple vitamin and mineral supplements
Nausea/morning sickness (nutritional concern)
- get up slowly in morning
- eat dry toast or crackers
- chew gum or suck hard candies
- eat small, frequent meals
- avoid foods with offensive odors
- when nauseated do not drink citrus juice, water, milk, coffee, or tea
Constipation and hemorrhoids (nutritional concern)
- fiber, exercise & liquids
Heartburn (nutritional concern)
- relax and eat slowly
- eat small, frequent meals
- drink liquids between meals
- avoid spicy or greasy foods
- elevate head while sleeping
- wait an hour after eating before lying down
High-Risk Pregnancy Factors
1. Maternal weight before pregnancy (over or under-wt)
2. Maternal weight gain during pregnancy
3. Maternal nutrition
4. Socioeconomic status
5. Lifestyle habits (smoking, alcohol, drugs)
6. Age – geriatric pregnancy? (over 35)
7. Previous pregnancies (number, interval, outcomes, twins)
8. Maternal health (high BP, diabetes, etc.)
Exercise during pregnancy
A. Benefits- maintain fitness- prevent gestational diabetes- facilitate labor- reduce stress
B. Guidelines- “low impact” activities- avoid sports with risk of falling or being hit by other people or objects
- prevent excessive high internal temperatures & dehydration- stay out of saunas, steam rooms & hot tubs- don’t exercise lying on back after 1st trimester- don’t exercise if experience pain or discomfort
Energy needs during infancy
• Infants double birthweight by 4 months
• Infants triple birthweight by 1 year
• Length increases by 50% in first year
• After infancy growth rate declines
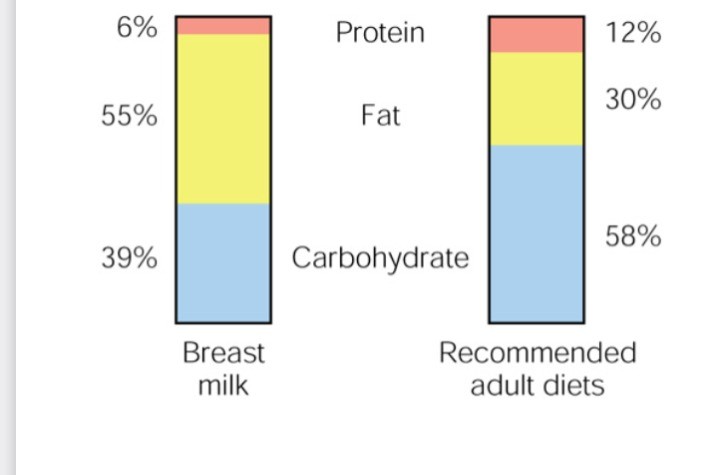
Breast milk components vs. recommended adult diet
Nutritional needs during infancy cow's milk and solid food
A. Introducing cow’s milk- 12 months- before 6 months associated with intestinalbleeding and iron deficiency
B. Introducing solid foods- typically at 6 months- iron fortified cereal first- pureed vegetables and fruits next- new recommendations don’t dictate an order- progress to family foods by 12 mths
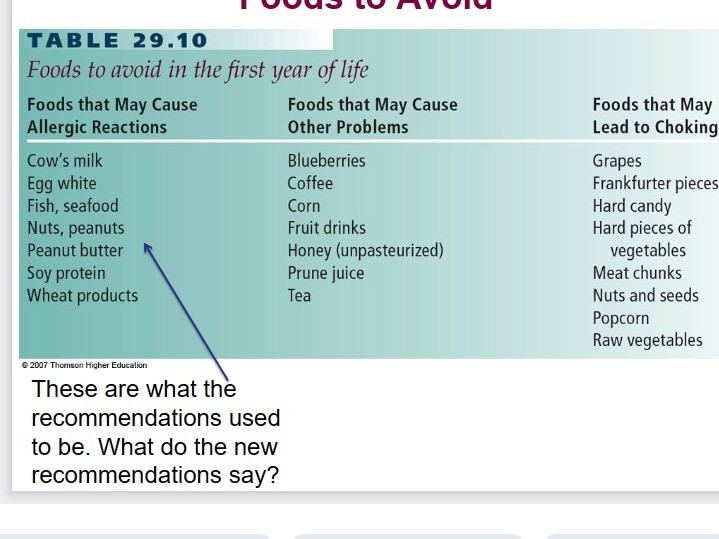
Foods to avoid
Marker of children's general nutrition and physical health:
children's general nutrition and physical health
**Poor growth often due to undernutrition or prolonged disease.
Childhood obesity associated with a higher chance of obesity, premature death and disability in adulthood.:
– Satiety responsiveness - responsiveness to internal satiety cues
– Food responsiveness - responsiveness towards external food cues, including the smell and taste of foods
Food Preferences in children
• Food preferences are not inborn – they are learned & shaped by environment
• Humans are born with caution toward new foods
• Children usually do not initially like strong-flavored vegetables, spicy foods, or mixed foods
The Struggle & Bans
• Parents have to offer new food many times – sometimes child will like it and other times the food has to be re-introduced multiple times
• Prohibiting intake of foods strengthens interest in the banned food and boosts consumption later
Healthy Eating Habits in children
• Parents decide what types of food their child should be offered, decision about how much to eat is left to child
• Born with mechanisms to regulate amount – satiation/satiety• Often children are trained to override the internal satiety cues and soon they become dampened and less likely to regulate body weight appropriately
• Don’t reward or punish children with foods– e.g. eat when you’re not hungry to reward yourself
What to do about picky eaters
• Make one family meal– Do not offer your child other options or their favorite foods if he/she refuses the family meal.
• Make sure your child comes to the table hungry
• Avoid distractions like toys and television
• Eat meals at the table as a family.– Do not offer food while your child is playing, watching television or walking around.
Fast Food? Choose Wisely
• Frequent fast food may lead to chronic diseases due to excess fat & salt, and lack of fruits, vegetables & whole grains.
• Feeding your child fast food influences lifelong foodpreferences.
• Teach moderation
Children and Milk
• Children and teens replace milk with soft drinks
• 1/2 of children have low calcium daily
• Children without milk intake have:– Low calcium intakes– Lower bone density– More fractures– Risk of osteoporosis
• Up to 2 yrs. of age, should drink whole milk (3.25% MF)
Growth spurts
1. increased hunger and food intake
2. body fat gain
3. height gain and body fat loss
WHO growth charts for Canada
• For females and males from 2 to 19 years of age to compare with norms
• Growth charts consist of graphs of:– Weight for age– Height for age
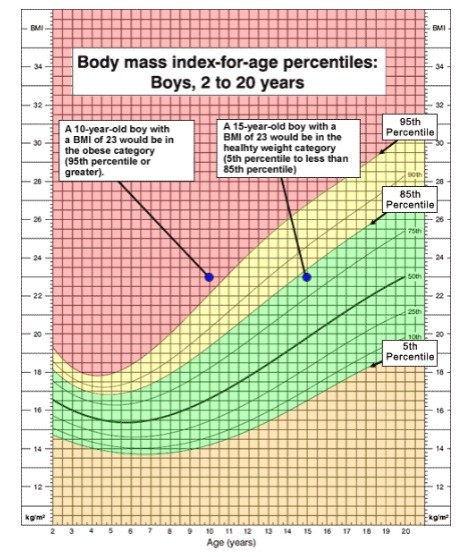
BMI Percentile
Below 5th = underweight
Above 85th = overweight
Above 95th = obesity
Adolescent growth spurt
• Occurs in girls between 11 and 15 years• Occurs in boys between 12 and 17 years
• Age of onset varies considerably
• At peak, girls gain 8 kg/yr and boys gain 9 kg/yr
• Gain 50% of adult weight, 25% of adult height, 45% of bone mass
What Determines Adult Height?
• Nutrition is the strongest non-genetic factor influencing height
• People grow taller in developed countries
• Good nutrition during pregnancy, and child diet during the growing years, exercise and freedom from illness support growth in height
Do we have more seniors or children
we have more seniors than children
Life expectancy & life span
- life expectancy (average number of years lived) is lengthened by medical science and nutrition
- life span (maximum number of years) has not increased
- human life span = 120 years
Life expectancy in Canada
A. Women- 83.9 years
B. Men- 79.5 years
Differs by province – which is the highest?
*Shortest life expectancy is in Central African Republic = 54.36 years
*Longest life expectancy is in Hong Kong = 85.29 years
II. Strategies to slow aging
- healthy habits
- calorie restriction
Healthy habits
- physiological age may not reflect chronological age - lifestyle behaviors
1. Sleep
2. Well balanced meals
3. Regular physical activity
4. No smoking
Energy restriction in animals
- increased life span
- fewer age-related diseases
- 30-50% fewer calories
- aging genes less active
- less oxidative stress
Energy restriction in humans
• Human trials are rare
• Pioneering clinical trial called Comprehensive Assessment of Long-term Effects of Reducing Intake of Energy (CALERIE).
• Young and middle-aged adults randomized into 2 groups– calorie-restricted diet for 2 years– usual diet
**Even with 2yrs of restriction, even less than what was desired, decrease in oxidative stress
Calorie Restriction Society International
- Compared with individuals consuming a typical standard Western diet, individuals in this group who have been practicing CR for a mean of 15 years have reduced body fat, markers of inflammation, and cardiovascular disease (CVD) risk.
- Is there a mimetic?
Physiological changes in aging (body comp., immune system, GI, endocrine, tooth loss, sensory losses)
1. Body composition- lose bone & muscle, increased percent fat2. Immune system- declines with age- compromised by nutritional deficiencies
3. GI tract- decreased stomach acidity- intestinal tract loses strength and elasticity - constipation
4. Endocrine- hormones increase/decrease (e.g. testosterone, estrogen)
4. Tooth loss- chewing difficult or painful- dentures
5. Sensory losses- poor eyesight- taste sensitivity declines somewhat and smell declines more- loss of vision & hearing - social isolation
Non body changes with aging
1. Psychological- depression- lose appetite and motivation to cook & eat
2. Economic- 20% of people >65 live in poverty
3. Social- malnutrition in those living alone
Energy & nutrient needs with aging
1. Water- total body water decreases with age- mild fever or hot weather dehydration
2. Energy- needs decline estimated 5% per decade
3. Protein- suggest 1 g/kg BW- important for immune system & prevent muscle wasting
4. Vitamins & minerals- vitamin B12, vitamin D, calcium, iron
Cataracts & macular degeneration in older adults
- cataracts = thickening of eye lens (makes everything look fuzzy)
- macular degeneration = deterioration of center of retina responsible for straight-ahead vision (black dot in center of vision)
- antioxidants may be protective
Arthritis
* Osteoarthritis = cushioning cartilage in joint breaks down- prebiotic fiber
* Rheumatoid arthritis = disease of immune system with painful inflammation of joints- omega-3, fish oils
Alzheimer’s
- exploring dietary inflammatory score, whole grains
Food safety concerns:
1. Food borne illnesses
2. Environmental contaminants
3. Naturally occurring toxicants
4. Pesticide residues
5. Food additives
5 signs of severe food poisoning
- vomiting so often you can't keep liquids down
- bloody diarrhea
- dehydration
- fever higher than 102 degrees
- diarrhea for more than 3 days
Causes and Consequences of food poisoning
• 250 foodborne illnesses identified
• A day or two of nausea and diarrhea to death within minutes
• Most severe in people:
– weakened immune systems
– certain chronic illnesses
– pregnant women
– young children
– older persons
• Symptoms of foodborne illness often consist of abdominal cramps, vomiting, nausea, diarrhea, fever
Food borne infections: Hepatitis A
- inflammation of the liver
- fatigue, nausea, dark urine
- primarily spread when person ingests food or water that is contaminated with the feces of an infected person
- onset: 2-7 weeks
**Raw or undercooked shellfish from contaminated waters, raw produce, contaminated drinking water (ice)
Food borne infections: Giardia (Giardia lamblia parasite)
- contaminated water
- diarrhea main symptom (sudden onset explosive or chronic)
- onset: 1-3 weeks
Food borne infections: Listeriosis (Listeria monocytogenes bacteria)
- hot dogs/deli meat, unpasteurized milk & soft cheese (feta, Brie, camembert, cream cheese, ricotta)
- mainly gut symptoms and fever but can trigger brain infection and/or sepsis
- high death rate in fetus and infants
- onset: 3-30 days or longer
**Milkshake deaths in August 2023 in Tacoma, Washington
Food borne infections: Salmonella
- raw or undercooked eggs & meat, raw dairy, F&V (sprouts and cantaloupe)
- mainly gut symptoms
- onset: 6 hours
- 6 days (last 4-7 days)
Food borne infections: E. coli (0157:H7)
- undercooked ground beef, unpasteurized milk, contaminated water, person to person
- mainly watery bloody diarrhea, cramps
- 15% children and elderly develop hemolytic uremic syndrome (can be fatal; permanent kidney damage)- onset: 1-8 days (lasts 5-10 days)
Food intoxicants: Botulism
- Clostridium botulinum grows without oxygen- botulinum toxin is responsible (one of deadliest known toxins)
- canned vegetables and meats; honey (bees pick up spores from flowers/soil); oils infused with garlic or herbs- onset: 4-36 hrs- blurred vision, difficulty speaking, paralysis, can be fatal- need antitoxin immediately
Food intoxicants: Staphylococcal toxin
- tuna, potato and macaroni salads, cream filled pastries, meats & poultry, egg products
- mainly gut symptoms, mild fever- onset: 1/2 to 8 hrs (lasts: 24-48 hrs)
Food safety in the kitchen:
1. Clean, safe kitchen- hot, soapy water
2. Avoid cross-contamination
3. Keep hot foods hot- internal cooking temperature to kill microbes differs for various meats
4. Keep cold foods cold- refrigerator = 4-6ºC- freezer = -18 to -20ºC
Mad Cow Disease
• Prion causes this deadly disease
• Small protein that transmits disease when consumed by a similar species
• Mad cow disease is transferred to humans who eat prion-infected meat
• Humans develop variant Creutzfeldt-Jakob disease from contaminated meat
– Symptoms resemble Alzheimer’s but progress much more rapidly
• Inevitably leads to death due to brain damage
• It is now illegal to feed cows any animal parts that could transmit disease (nerve, bone, intestine).
• Risk of consuming beef from cattle with mad cow disease is small but possibility exists.
Mercury Contamination
• Mercury contamination by fungicides, fossil fuel exhaust, smelting plants, pulp mills, and chemical plants
• Virtually all fish have trace amounts of mercury- shark, swordfish, bass, lake trout, walleye, chain pickerel (large game fish) have high levels
• Mercury interferes with fetal brain development, so avoid eating these fish if pregnant
• Health Canada says pregnant women should avoid shark, tile fish, swordfish, or king mackerel
• Consumption of fish by adults in general does not appear to pose a health risk
Food additives
- new additive must prove
*effective
*detectable & measurable in product
*safe (large doses to animals
)- must never have caused cancer in animal study or human experience
Intentional additives
* antimicrobial agents - salt, sugar, potassium sorbate, nitrates
* antioxidants - vitamin C, E, sulfites, BHA & BHT
* color additives - carotenoids, caramel, blue #1 & 2, yellow #5 & 6
* artificial flavors - largest group (MSG)* texture & stability - gums, pectins, etc.
* nutrient additives -
1. Thiamin, niacin, riboflavin, folate & iron in grain products
2. Iodine in salt
3. Vitamins A & D in milk
4. Vitamin C & calcium in juice
Indirect additives
microwave packaging- at high temperatures chemicals and microplastics can migrate into food
- glass or ceramic should be used- avoid disposable plastic containers
If 100 people represented the world:
• 60 Asia
• 14 Africa
• 12 Europe
• 8 Latin America and Caribbean
• 5 North America
• 1 Australia and New Zealand
• 1 person would have a college education
• 80 would live in poor housing
• 50 would be malnourished
State of Health in the World: What is monitored?
– Number of low birth weight infants
– Prevalence of child underweight
– Rates of breast feeding
– Access to safe drinking water
Health and nutrition status of developing countries monitored by:
– World Health Organization (WHO)
– United Nations International Children’s Emergency Fund (UNICEF)
– Food and Agriculture Organization (FAO)
2 types of tuna: low in mercury
Skipjack (strongest flavor, highest fat) and yellowfin (milder flavour)
- albacore: higher mercury
Why do starvation and malnutrition happen?
• Poverty
• Poor and corrupt governments
• Inequitable distribution of the food supply
• Low levels of education
• Discrimination against females
• HIV/AIDS epidemic
• Lack of economic opportunities
• Racism, ethnocentrism
• Low agricultural productivity (natural disasters; use of agricultural land for biofuel crops)
• Unsafe water
What is important
- food is for everyone