What hormones are released by the hypothalamus and what are their functions? (5)
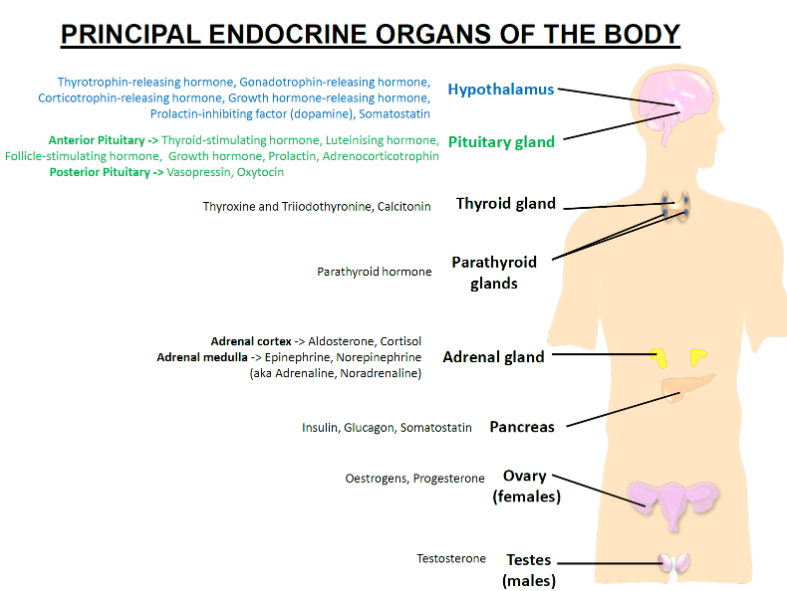
Thyrotrophin-releasing hormone (TRH): Stimulates the release of thyroid-stimulating hormone (TSH) from the anterior pituitary.
Gonadotrophin-releasing hormone (GnRH): Stimulates the release of luteinising hormone (LH) and follicle-stimulating hormone (FSH) from the anterior pituitary.
Corticotrophin-releasing hormone (CRH): Stimulates the release of adrenocorticotrophic hormone (ACTH) from the anterior pituitary.
Growth hormone-releasing hormone (GHRH): Stimulates the release of growth hormone (GH) from the anterior pituitary.
Prolactin-inhibiting factor (Dopamine): Inhibits prolactin secretion from the anterior pituitary.
What hormones are released by the anterior pituitary and what are their functions? (6)
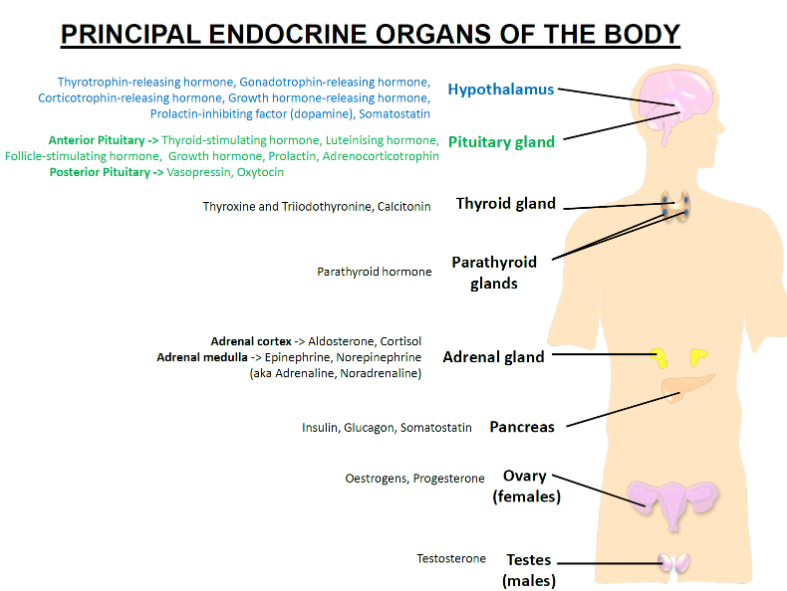
Thyroid-stimulating hormone (TSH): Stimulates the thyroid gland to release thyroid hormones (T3 and T4).
Luteinising hormone (LH): Stimulates ovulation in females and testosterone production in males.
Follicle-stimulating hormone (FSH): Stimulates the growth of ovarian follicles in females and sperm production in males.
Growth hormone (GH): Stimulates growth and cell reproduction.
Prolactin (PRL): Stimulates milk production in females.
Adrenocorticotrophin (ACTH): Stimulates the adrenal cortex to release cortisol.
What hormones are released by the posterior pituitary and what are their functions? (2)
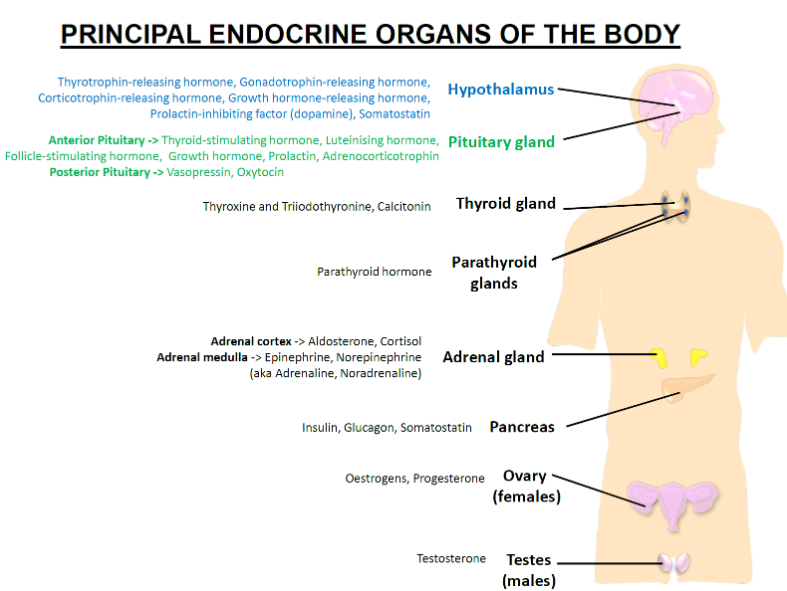
Vasopressin (ADH): Regulates water balance in the body by promoting water reabsorption in the kidneys.
Oxytocin: Stimulates uterine contractions during childbirth and milk ejection during breastfeeding.
What hormones are released by the thyroid gland and what are their functions? (3)
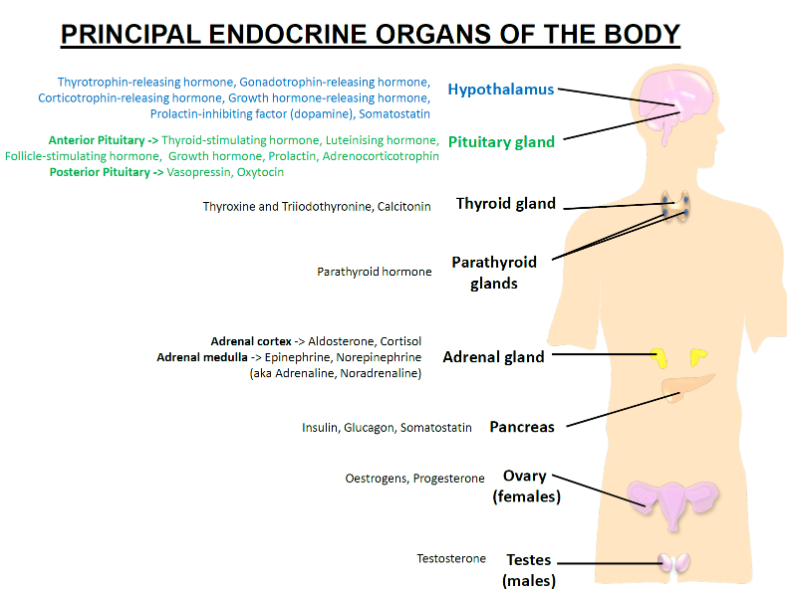
Thyroxine (T4): Regulates metabolism and growth.
Triiodothyronine (T3): More potent than T4, also regulates metabolism and growth.
Calcitonin: Lowers blood calcium levels by inhibiting osteoclast activity.
What hormones are released by the parathyroid glands and what is their function? (1)
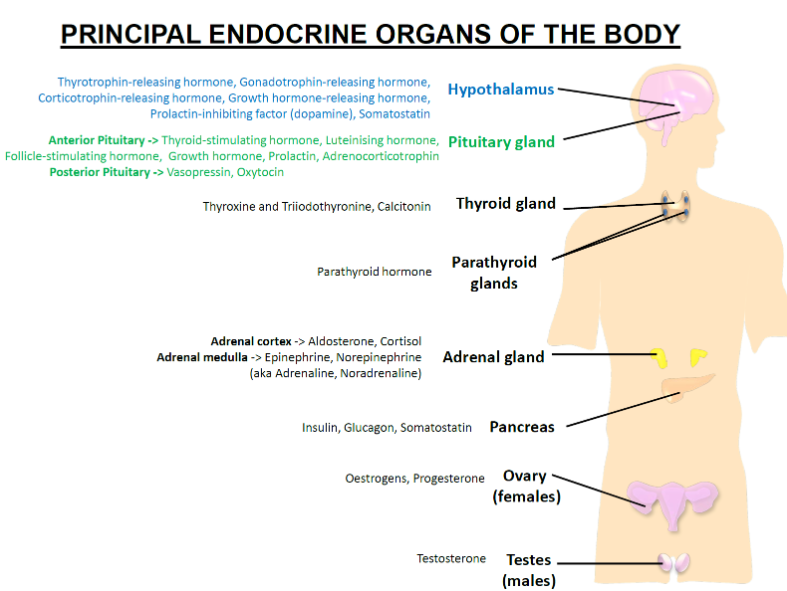
Parathyroid hormone (PTH): Increases blood calcium levels by promoting osteoclast activity and calcium reabsorption in the kidneys.
What hormones are released by the adrenal cortex and what are their functions? (2)
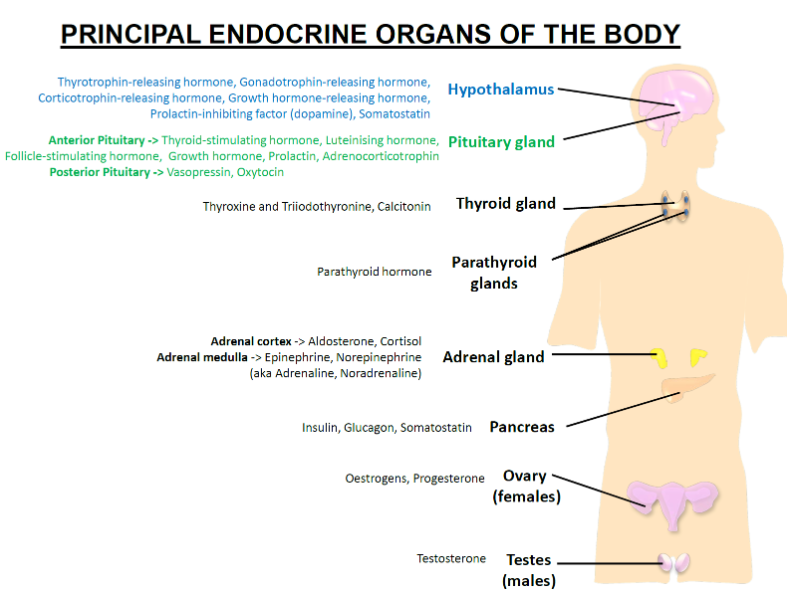
Aldosterone: Regulates sodium and potassium balance by increasing sodium reabsorption in the kidneys.
Cortisol: Regulates metabolism and the body's stress response.
What hormones are released by the adrenal medulla and what are their functions? (2)
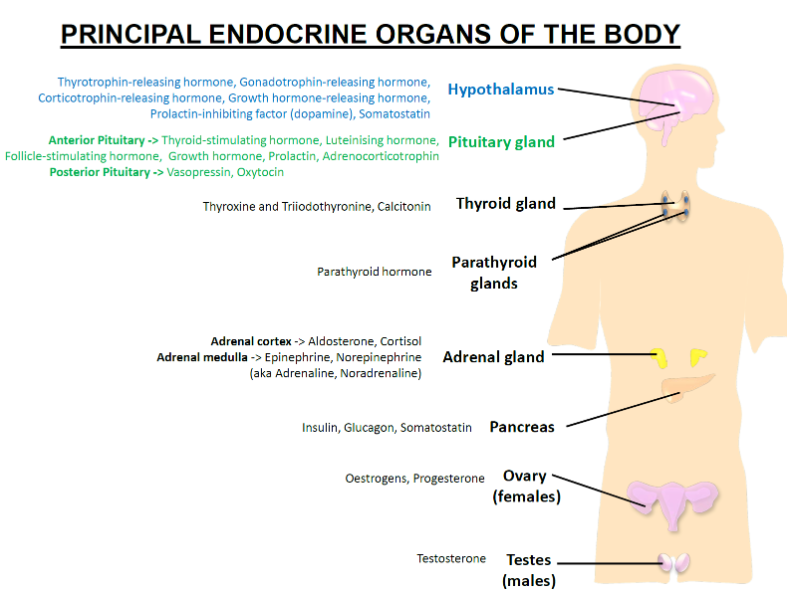
Epinephrine (Adrenaline): Increases heart rate, blood flow to muscles, and blood glucose levels during the fight or flight response.
Norepinephrine (Noradrenaline): Increases heart rate and blood pressure, and prepares the body for stress.
What hormones are released by the pancreas and what are their functions? (3)
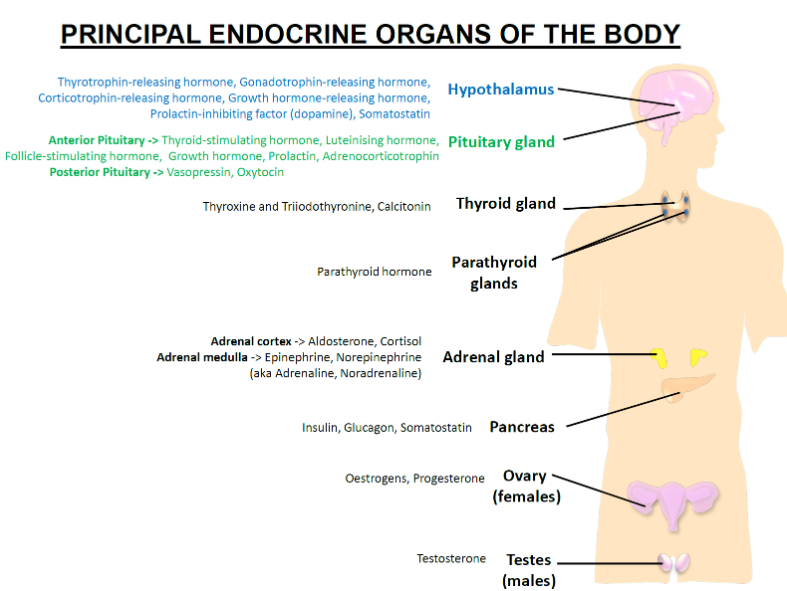
Insulin: Lowers blood glucose levels by promoting glucose uptake into cells.
Glucagon: Raises blood glucose levels by stimulating the liver to release glucose.
Somatostatin: Inhibits the release of both insulin and glucagon.
What hormones are released by the ovaries and what are their functions? (2)
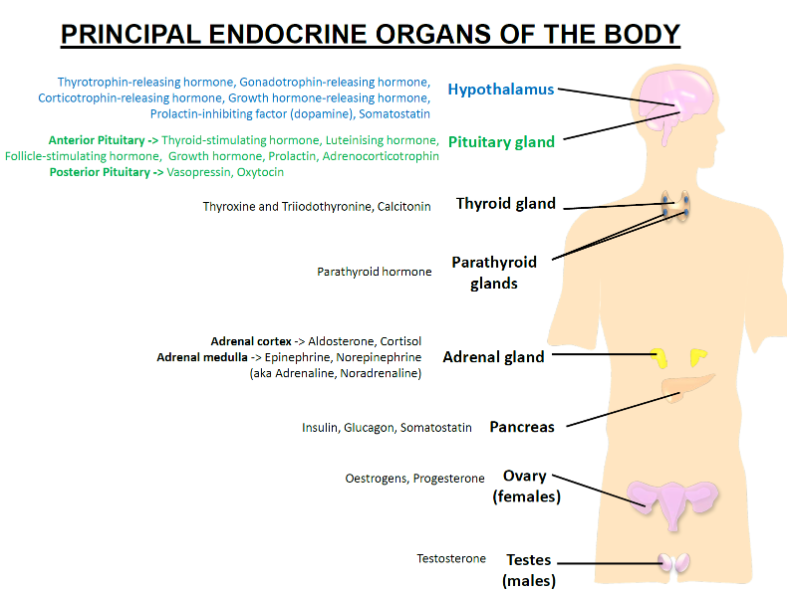
Oestrogens: Regulate the menstrual cycle, promote secondary sexual characteristics, and support pregnancy.
Progesterone: Prepares the uterus for pregnancy and maintains pregnancy.
What hormone is released by the testes and what is its function? (1)
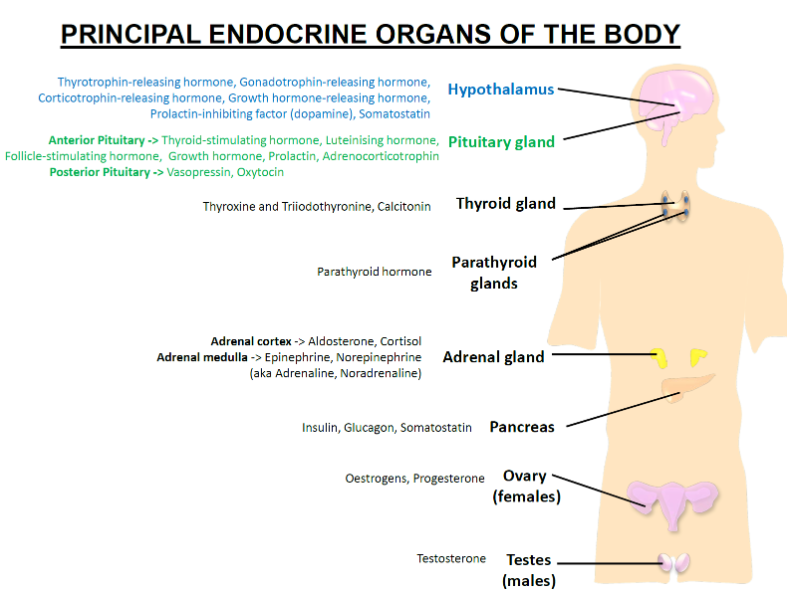
Testosterone: Promotes sperm production, the development of male secondary sexual characteristics, and the maintenance of male reproductive health.
What is point-to-point communication? (1)
Fast, restricted
What are the neurons of the secretory hypothalamus? (1)
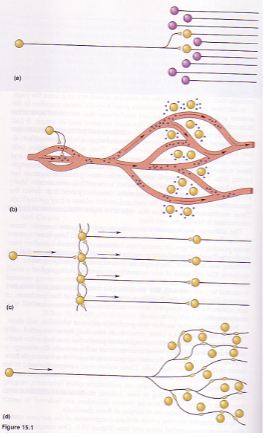
Slow but widespread
What is the function of networks of interconnected neurons? (1)
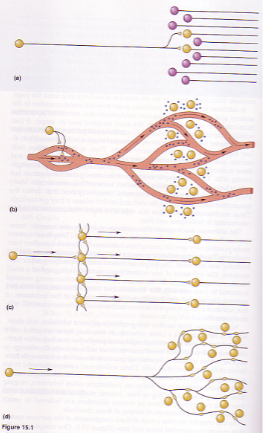
Fast, widespread influence
What is the autonomic nervous system's communication style? (1)

Fast, widespread influence
What are diffuse modulatory systems? (1)
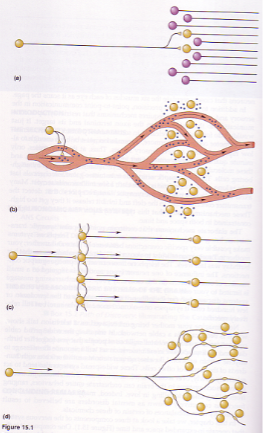
Slower, widespread influence
What are the characteristics of the nervous system's control? (4)
Signalling along nerve fibres
Transmission of electrical impulses
Fast communication
Effects are generally short-acting
What are the characteristics of the endocrine system's control? (4)
Mediators travel within blood vessels
Utilizes chemical mediators (hormones)
Slow communication
Effects can be long-lasting
What are neurohormones and how are they produced? (2)
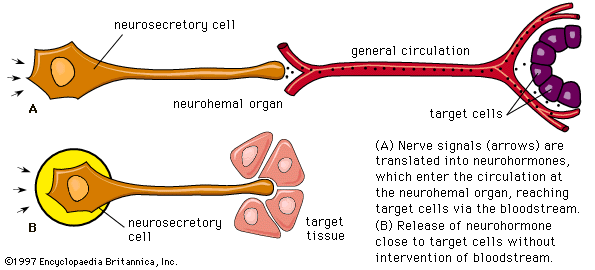
Produced by specialized nerve cells called neurosecretory cells
Released into the blood and can act on distant cells
How do neurohormones function? (2)
Can act as neurotransmitters
Can act as autocrine (self) or paracrine (local) messengers
What are protein & peptide hormones and their characteristics? (4)
Vary considerably in size
Can be synthesized as a large precursor and processed before secretion (e.g., GH, somatostatin, insulin)
Can be post-translationally modified (e.g., glycosylation)
Can have multiple subunits synthesized independently and assembled (e.g., FSH, LH, TSH)
What are amino acid derivative hormones and their characteristics? (3)
Mostly derived from tyrosine
Act as neurotransmitters and hormones
Examples include Epinephrine, Norepinephrine, and Dopamine
What are steroid hormones and their characteristics? (3)
Derived from cholesterol
Include hormones such as Cortisol, Aldosterone, Testosterone, Progesterone, and Oestradiol
Classified as lipids
What is the role of neuropeptides in the Hypothalamo-pituitary axis (HPA)? (1)
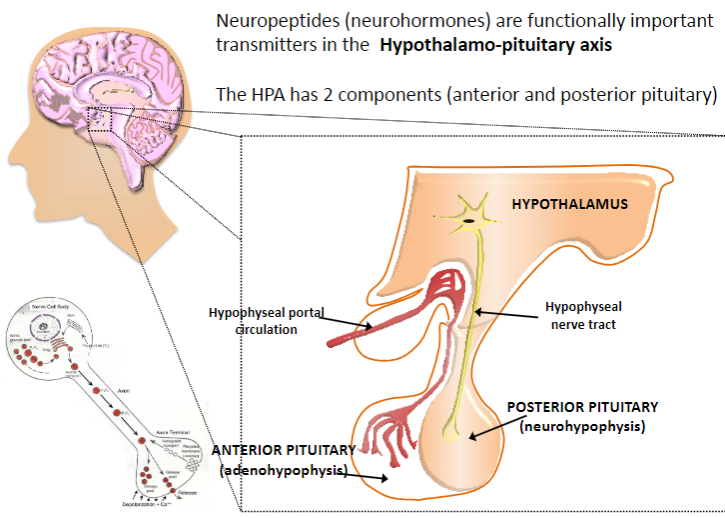
Neuropeptides (neurohormones) are functionally important transmitters in the Hypothalamo-pituitary axis
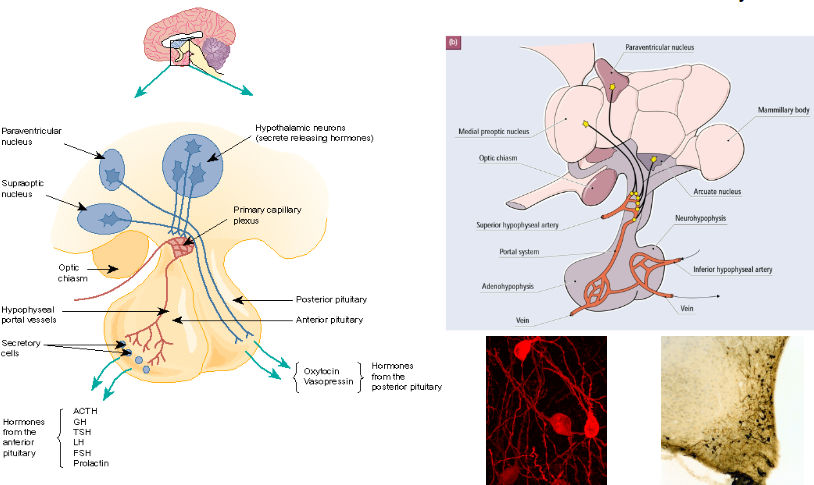
What are the two components of the Hypothalamo-pituitary axis (HPA)? (2)
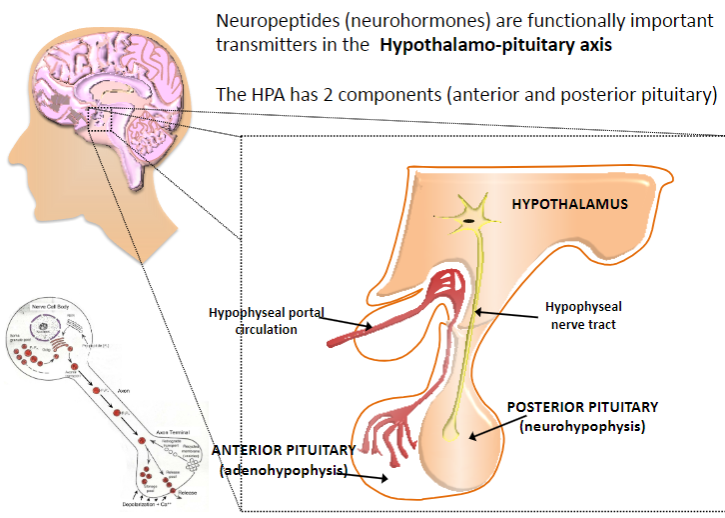
Anterior pituitary
Posterior pituitary
What is the dual role of some peptides in the body? (2)
Some peptides act both as hormones and neurotransmitters
In some cases, their endocrine and neural functions are linked, while in others, they are not
Where are the neuroendocrine secretory cells located in the hypothalamus? (2)
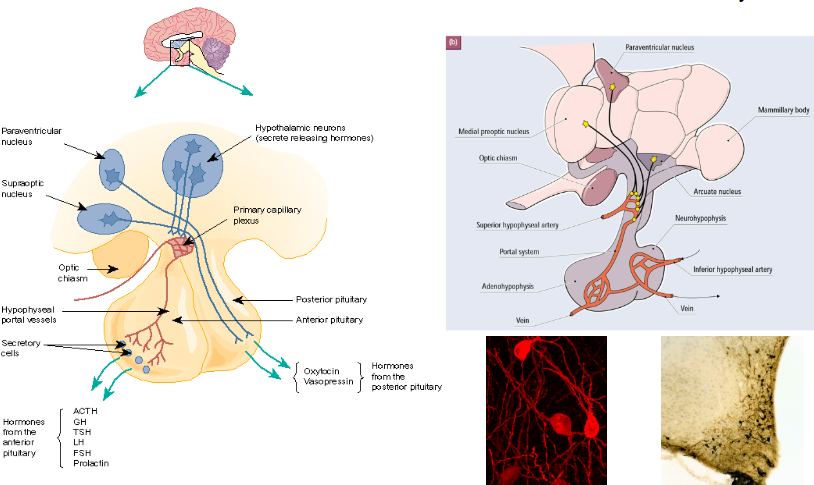
Scattered throughout the hypothalamus
Key nuclei include the medial pre-optic, arcuate, and paraventricular nuclei
What is the function of Corticotrophin Releasing Hormone (CRH)? (2)
CRH is a 41 amino acid peptide
It controls the release of adrenocorticotrophin (ACTH)
What is the function of Thyrotrophin Releasing Hormone (TRH)? (2)
TRH is a 3 amino acid peptide
It controls the release of thyroid stimulating hormone (TSH) and prolactin (PRL)
What is the function of Gonadotrophin Releasing Hormone (GnRH)? (2)
GnRH is a 10 amino acid peptide
It controls the release of luteinising hormone (LH) and follicle-stimulating hormone (FSH)
What is the function of Growth Hormone Releasing Hormone (GHRH)? (2)
GHRH is a 44 amino acid peptide
It controls the release of growth hormone (GH)
What is the function of Growth Hormone Release Inhibiting Hormone (Somatostatin)? (7)
Somatostatin is a 14 amino acid peptide
It inhibits the release of growth hormone (GH), gastrin, vasoactive intestinal polypeptide (VIP), glucagon, insulin, thyroid stimulating hormone (TSH), and prolactin (PRL)
What is the function of Dopamine in relation to prolactin release? (2)
Dopamine is a monoamine
It inhibits the release of prolactin (PRL)
What do Gonadotroph cells secrete and in response to what? (2)
Gonadotroph cells secrete luteinising hormone (LH) and follicle-stimulating hormone (FSH)
They respond to Gonadotrophin Releasing Hormone (GnRH)
What do Somatotroph cells secrete and in response to what? (2)
Somatotroph cells secrete growth hormone (GH)
They respond to Growth Hormone Releasing Hormone (GHRH)
What do Corticotroph cells secrete and in response to what? (2)
Corticotroph cells secrete adrenocorticotrophin (ACTH)
They respond to Corticotrophin Releasing Hormone (CRH)
What do Thyrotroph cells secrete and in response to what? (2)
Thyrotroph cells secrete thyroid stimulating hormone (TSH)
They respond to Thyrotrophin Releasing Hormone (TRH)
What do Lactotroph cells secrete and in response to what? (3)
Lactotroph cells secrete prolactin (PRL)
They respond to Thyrotrophin Releasing Hormone (TRH), somatostatin, and dopamine
What is Adrenocorticotrophic hormone (ACTH) and what is its role? (3)

ACTH is a 39 amino acid peptide with a molecular weight of 4.5 kDa
It is derived from a large precursor glycoprotein called pro-opiomelanocortin (POMC)
ACTH stimulates the production of glucocorticoids and sex hormones from the zona fasciculata of the adrenal cortex
What is the process by which ACTH is released into circulation? (3)
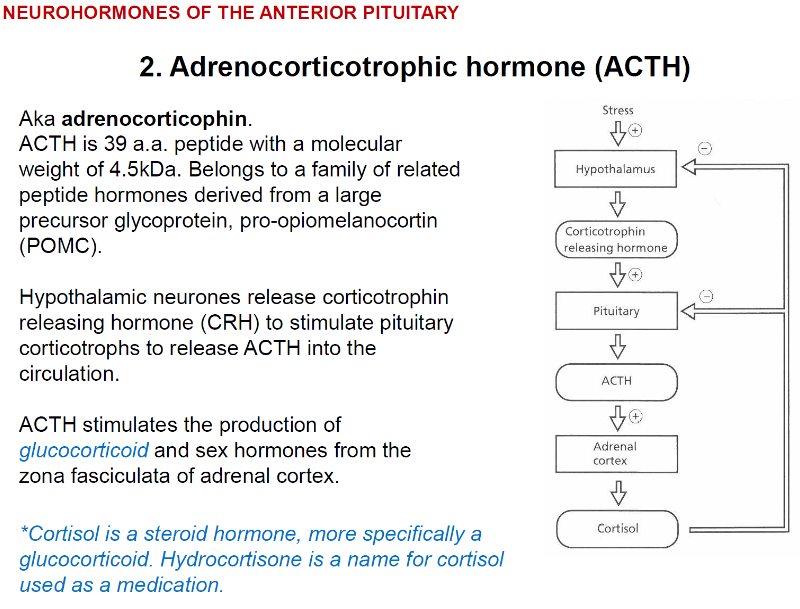
Hypothalamic neurons release corticotrophin releasing hormone (CRH)
CRH stimulates pituitary corticotrophs
Pituitary corticotrophs release ACTH into the circulation
What is cortisol and how is it related to ACTH? (2)
Cortisol is a steroid hormone and a type of glucocorticoid
ACTH stimulates the adrenal cortex to produce cortisol, which is also known as hydrocortisone when used as a medication
What is the pattern of glucocorticoid secretion throughout the day? (2)
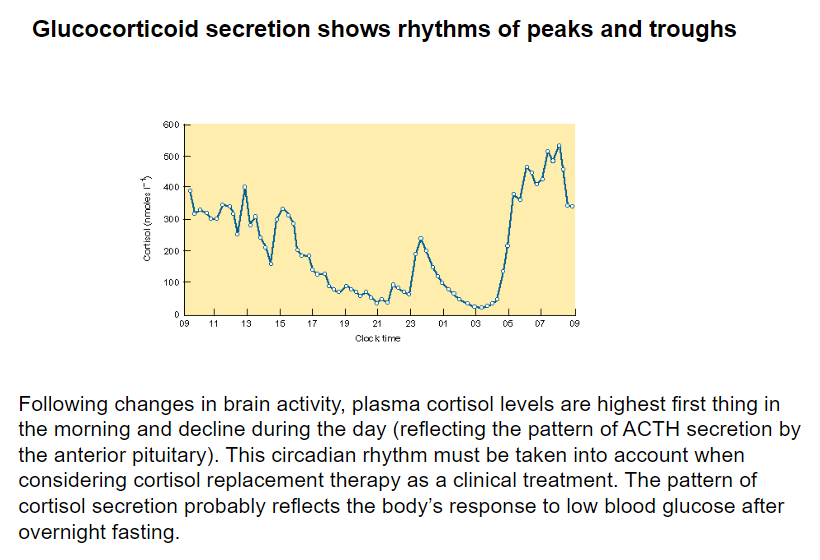
Glucocorticoid secretion follows a circadian rhythm, with peaks in the morning and troughs throughout the day
Plasma cortisol levels are highest first thing in the morning and decline during the day, reflecting the pattern of ACTH secretion by the anterior pituitary
Why is it important to consider the circadian rhythm of cortisol when planning cortisol replacement therapy? (2)
The circadian rhythm of cortisol affects the timing and effectiveness of replacement therapy
Cortisol replacement therapy must take into account the body's natural rhythm of cortisol secretion, which peaks in the morning after overnight fasting
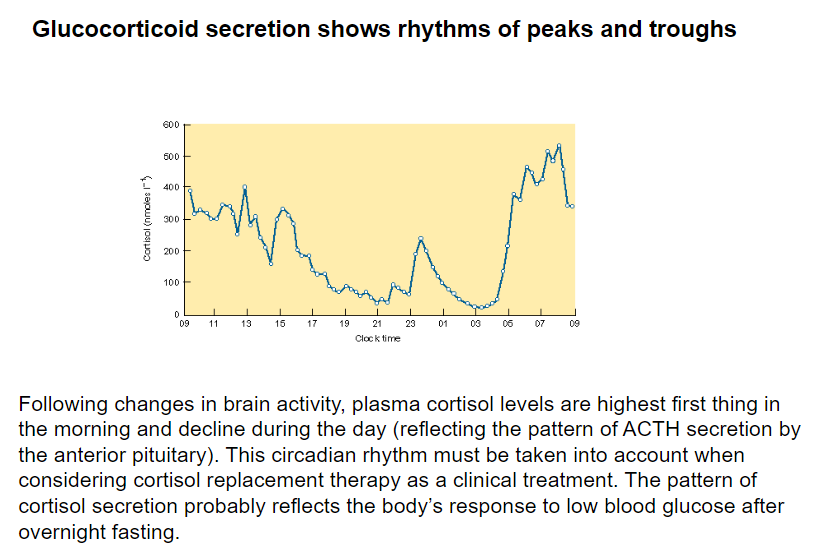
What is the role of Thyrotrophic Releasing Hormone (TRH) in the regulation of thyroid secretion? (2)
TRH is released by the hypothalamus and stimulates the anterior pituitary to release thyroid-stimulating hormone (TSH)
TSH acts on the thyroid to increase the secretion of T4/T3 hormones
How is T4 converted to its more potent form, T3? (2)

T4 is converted to T3 by a deiodinase enzyme (DI) found in target tissues
The pituitary also expresses deiodinase to convert T4 to T3, which facilitates negative feedback regulation
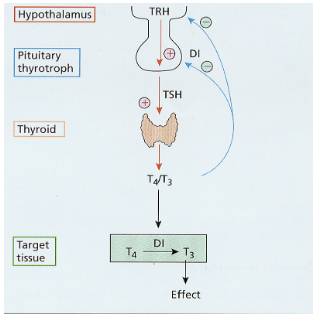
What are the hypothalamic neurohormones that regulate the posterior pituitary? (2)
Vasopressin
Oxytocin
Where are Vasopressin and Oxytocin synthesized? (1)
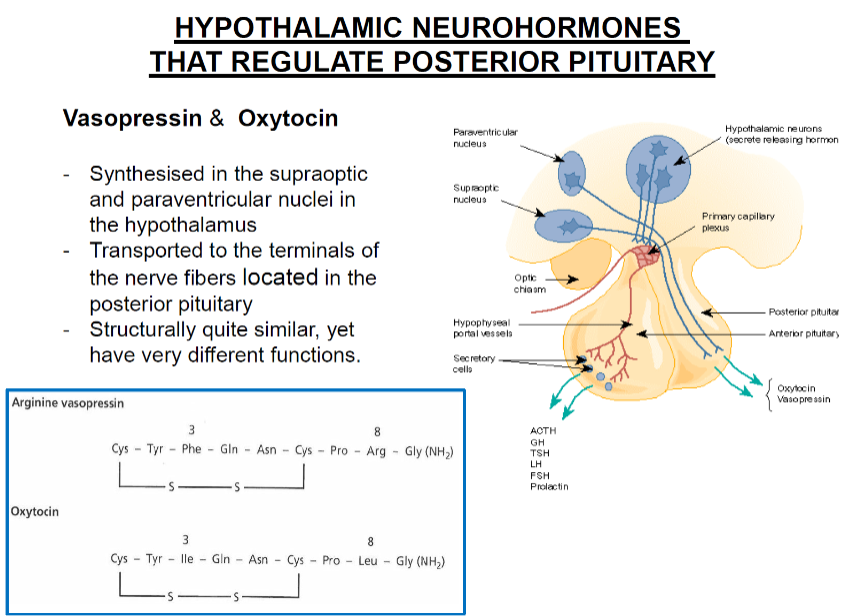
Both are synthesized in the supraoptic and paraventricular nuclei of the hypothalamus
How are Vasopressin and Oxytocin transported to the posterior pituitary? (1)

They are transported to the terminals of the nerve fibers located in the posterior pituitary
How are Vasopressin and Oxytocin structurally similar and different in function? (2)
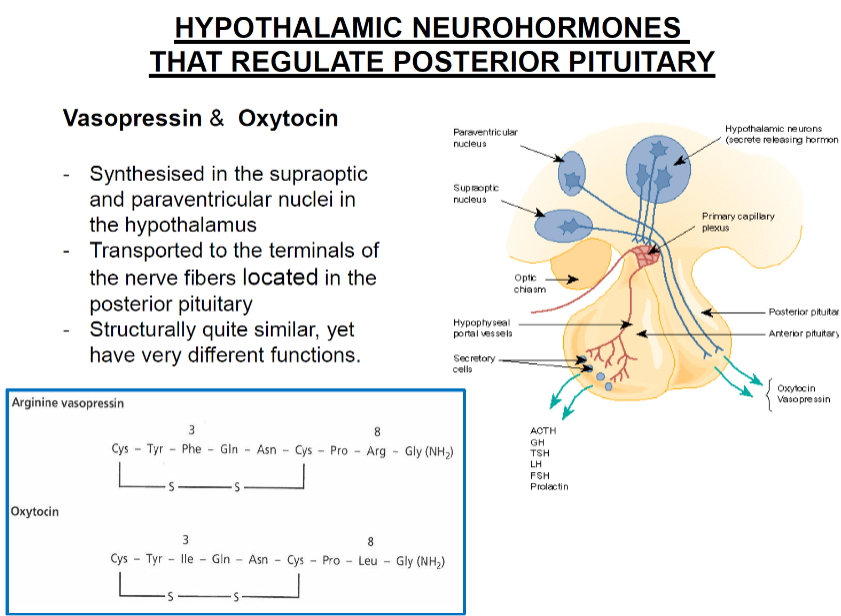
They are structurally quite similar
They have very different functions
What is Vasopressin also known as, and how is its release stimulated? (2)
Also known as Anti-diuretic hormone (ADH)
Release is stimulated by changes in the activity of the osmoreceptor complex in the hypothalamus
What are the functions of Vasopressin? (2)
Controls plasma osmolality by regulating water excretion and drinking behavior
Stimulates vascular smooth muscle contraction in the distal tubules of the kidney to reduce water loss and raise blood pressure
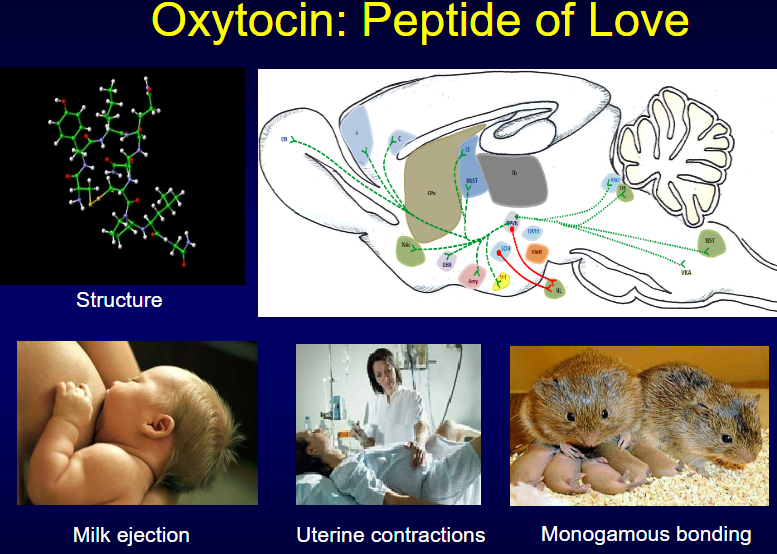
What is Oxytocin involved in, and when is it elevated? (2)
Normally undetectable but elevated during parturition, lactation, and mating
Released in response to peripheral stimuli such as cervical stretch receptors and suckling at the breast
What are the functions of Oxytocin? (3)
Regulates smooth muscle contraction (e.g., uterus during labor, myoepithelial cells lining the mammary duct)
Contributes to contraction of the reproductive tract during sperm ejaculation
May also be involved in responses to stroking, caressing, and grooming
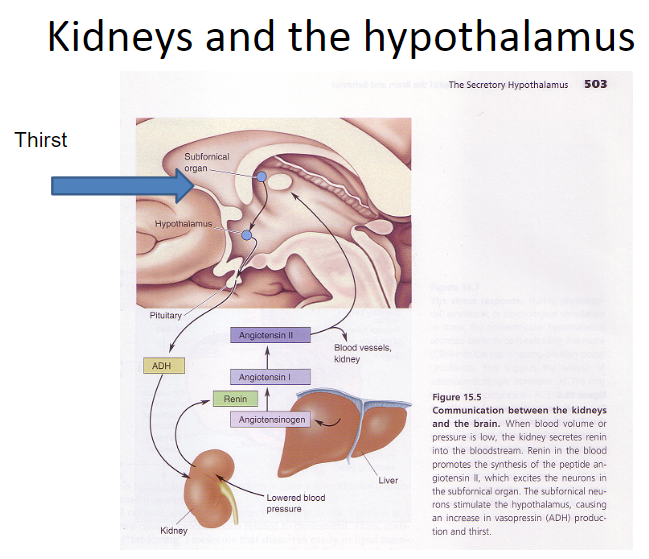
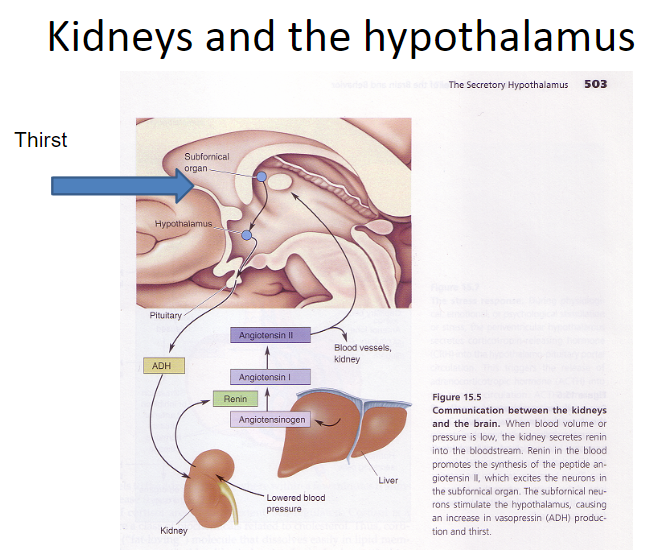
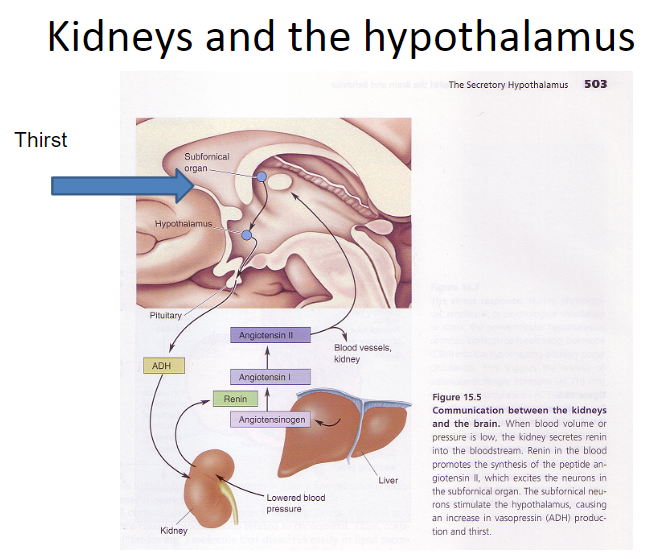
How do kidneys and the hypothalamus interact? (5)
Kidneys secrete renin
Renin converts Angiotensinogen to Angiotensin I
Angiotensin I is converted to Angiotensin II
Angiotensin II is detected by the subfornical organ
Subfornical organ projects to vasopressin cells and neurons in the lateral hypothalamus, affecting kidney function
Picture demonstrating the history of oxytocin:
Picture demonstrating the peptide of love.... Oxytocin:
What are the Hormonal Feedback Mechanism during Labour (5)
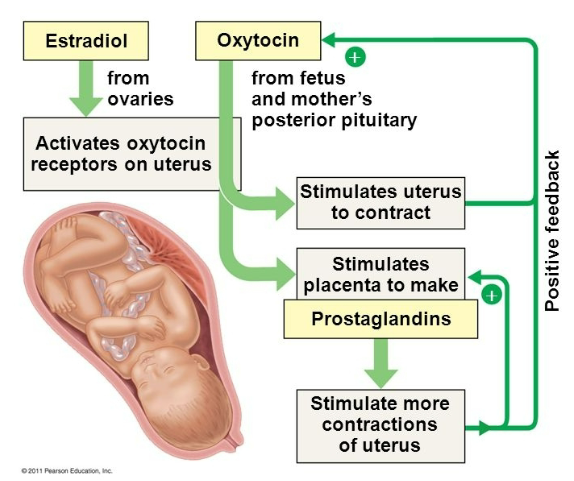
Estradiol (from ovaries) activates oxytocin receptors on the uterus
Oxytocin (from fetus and mother's posterior pituitary) stimulates the uterus to contract
Oxytocin also stimulates the placenta to produce prostaglandins
Positive feedback occurs, stimulating more contractions in the uterus
This cycle continues to amplify until labour is completed
What are the CNS Effects of Oxytocin (7)
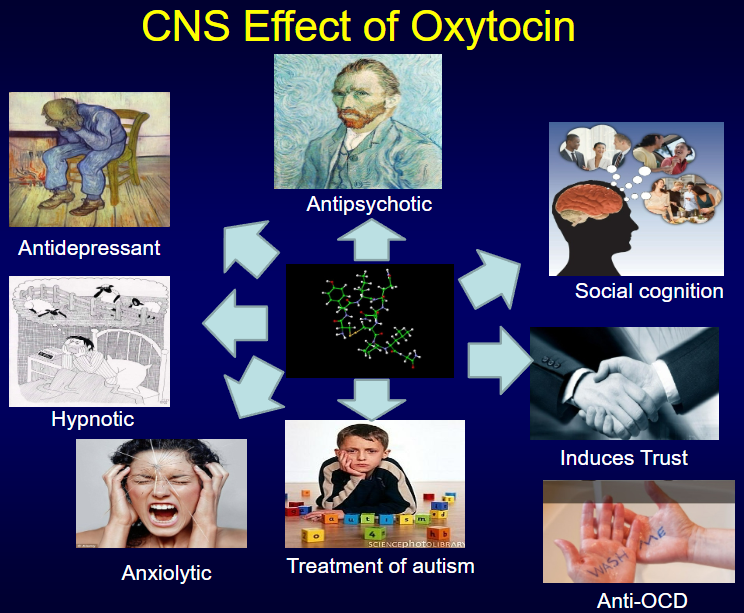
Antipsychotic
Antidepressant
Social cognition enhancement
Hypnotic
Induces trust
Anxiolytic
Treatment for autism and anti-OCD
What is the mechanism of action of peptide and protein hormones at the cellular level? (3)
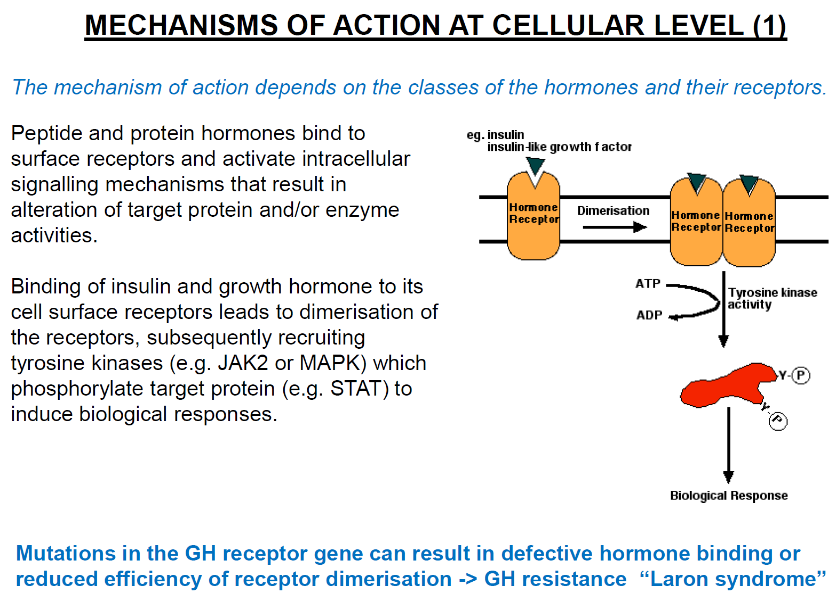
Peptide and protein hormones bind to surface receptors on the target cell.
This activates intracellular signalling mechanisms that lead to changes in target protein and/or enzyme activities.
These actions result in the alteration of cellular functions.
How do insulin and growth hormone activate intracellular signalling mechanisms? (3)
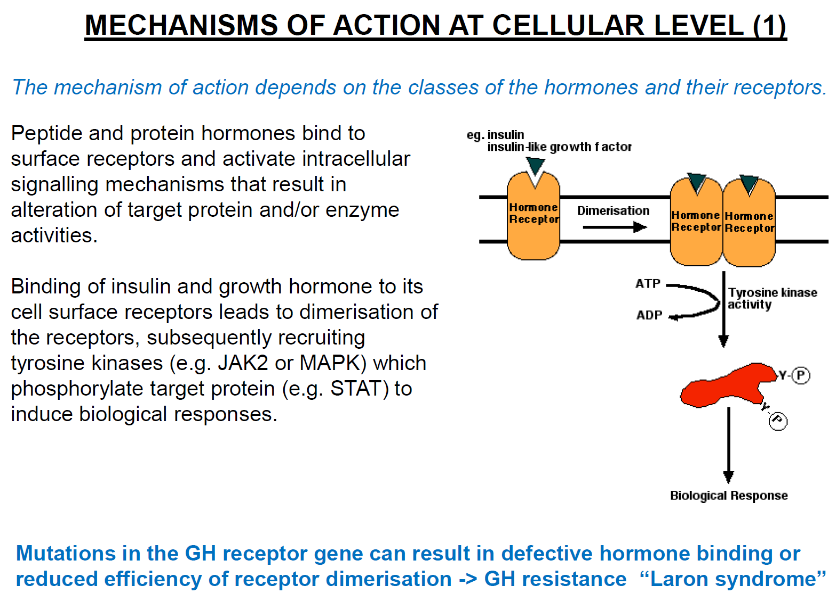
Insulin and growth hormone bind to cell surface receptors, causing receptor dimerization.
This dimerization recruits tyrosine kinases (e.g., JAK2 or MAPK).
The kinases phosphorylate target proteins (e.g., STAT), triggering biological responses.
How do mutations in the growth hormone receptor affect its function? (2)
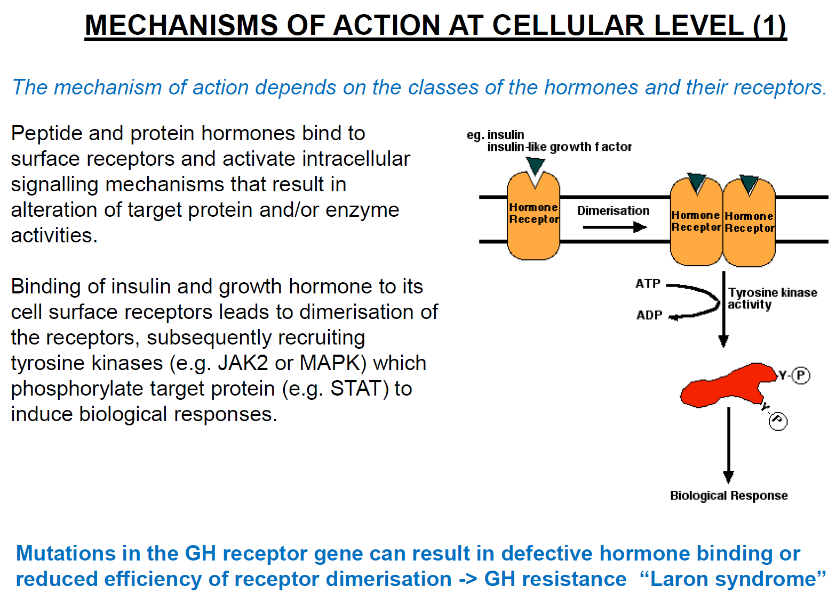
Mutations in the GH receptor gene can cause defective hormone binding or reduced receptor dimerization.
This results in GH resistance, such as in Laron syndrome.
What is the G-protein/adenylate cyclase pathway and how does it work? (3)
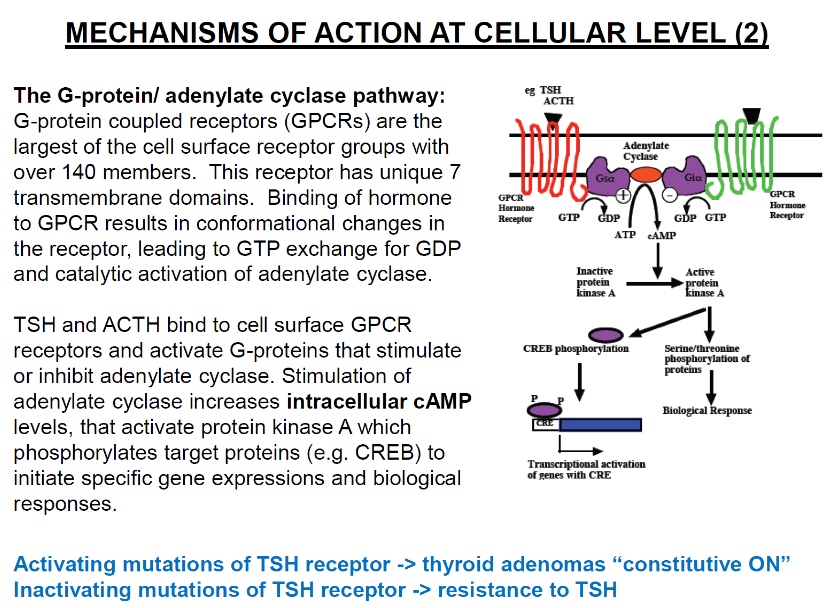
G-protein coupled receptors (GPCRs): Largest group of cell surface receptors with over 140 members; characterized by 7 transmembrane domains.
Hormone binding: Binding of hormone to GPCR causes conformational changes, leading to GTP exchange for GDP and activation of adenylate cyclase.
Activation of adenylate cyclase: Increases intracellular cAMP levels, activating protein kinase A (PKA), which phosphorylates target proteins (e.g., CREB).
What are the effects of mutations in the TSH receptor in the G-protein/adenylate cyclase pathway? (2)
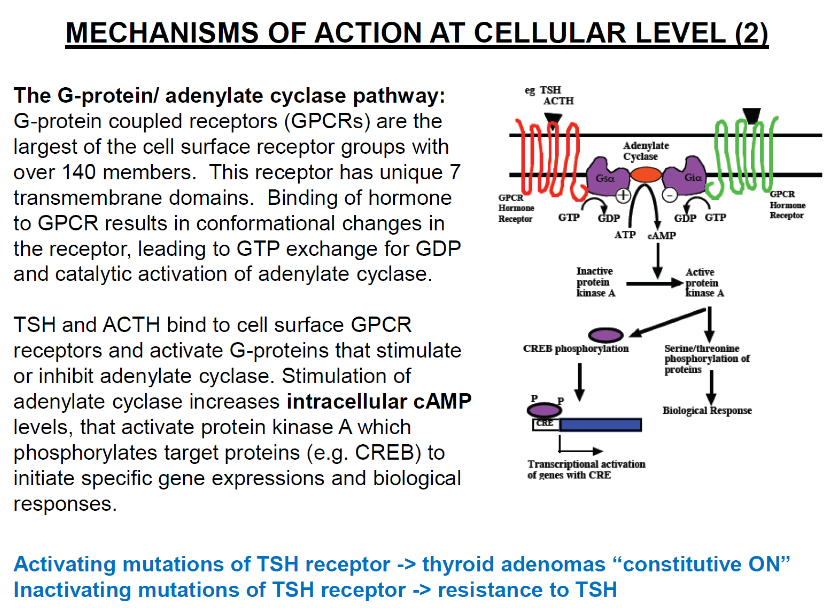
Activating mutations of TSH receptor: Can cause thyroid adenomas (constitutive ON).
Inactivating mutations of TSH receptor: Lead to resistance to TSH.
How does the DAG/IP3 pathway work and what are its effects? (4)
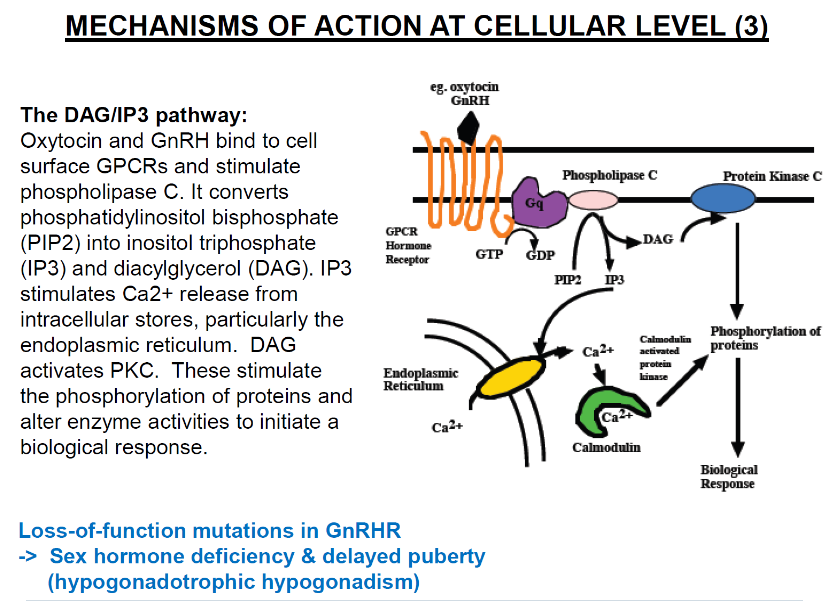
Hormone binding: Oxytocin and GnRH bind to cell surface GPCRs.
Activation of phospholipase C: Stimulates conversion of phosphatidylinositol bisphosphate (PIP2) into inositol triphosphate (IP3) and diacylglycerol (DAG).
IP3 effects: Stimulates Ca2+ release from intracellular stores (particularly the endoplasmic reticulum).
DAG effects: Activates protein kinase C (PKC), which leads to phosphorylation of proteins and altered enzyme activities to initiate a biological response.
What are the effects of loss-of-function mutations in the GnRH receptor? (1)
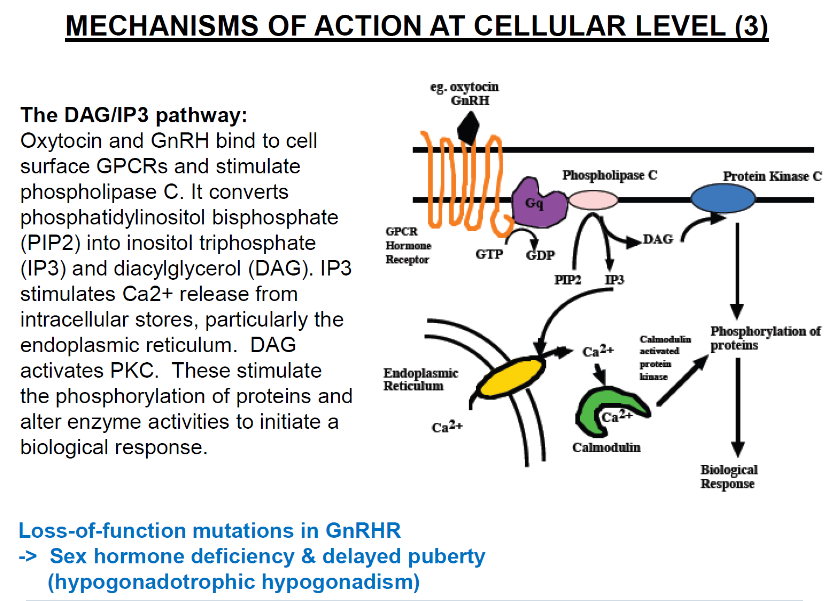
Loss-of-function mutations in GnRHR: Lead to sex hormone deficiency and delayed puberty (hypogonadotropic hypogonadism).
How do steroid and thyroid hormones act at the cellular level through cytoplasmic/nuclear receptors? (3)
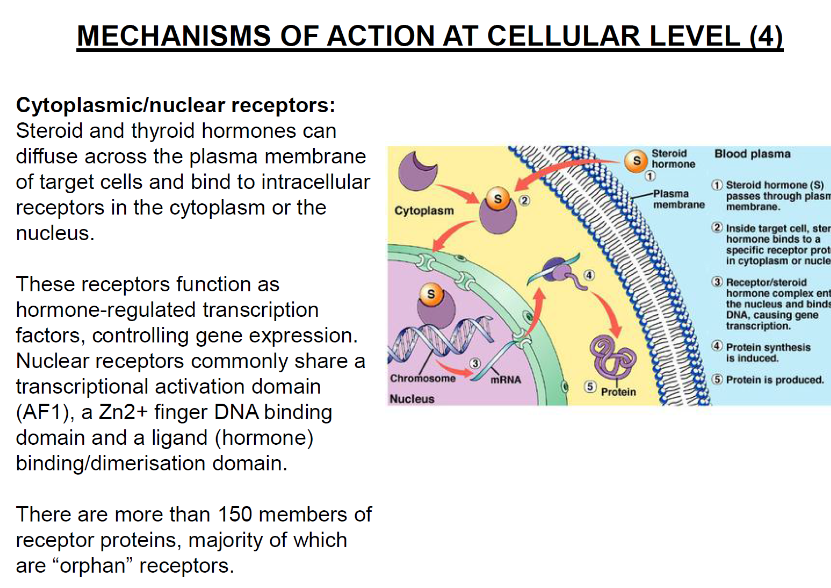
Hormone diffusion: Steroid and thyroid hormones diffuse across the plasma membrane of target cells.
Receptor binding: The hormones bind to intracellular receptors in the cytoplasm or nucleus.
Transcriptional function: These receptors act as hormone-regulated transcription factors, controlling gene expression.
What are the key features of nuclear receptors? (3)
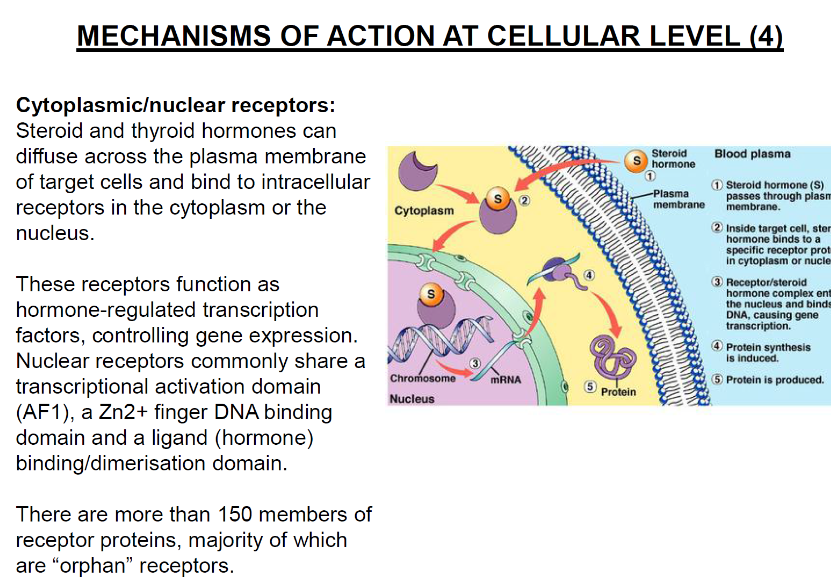
Transcriptional activation domain (AF1): A domain involved in transcription activation.
Zn2+ finger DNA binding domain: A structural feature for binding to DNA.
Ligand binding/dimerisation domain: A domain for binding to the hormone (ligand) and dimerising with other receptors.
What are the effects of too much growth hormone (GH)? (2)
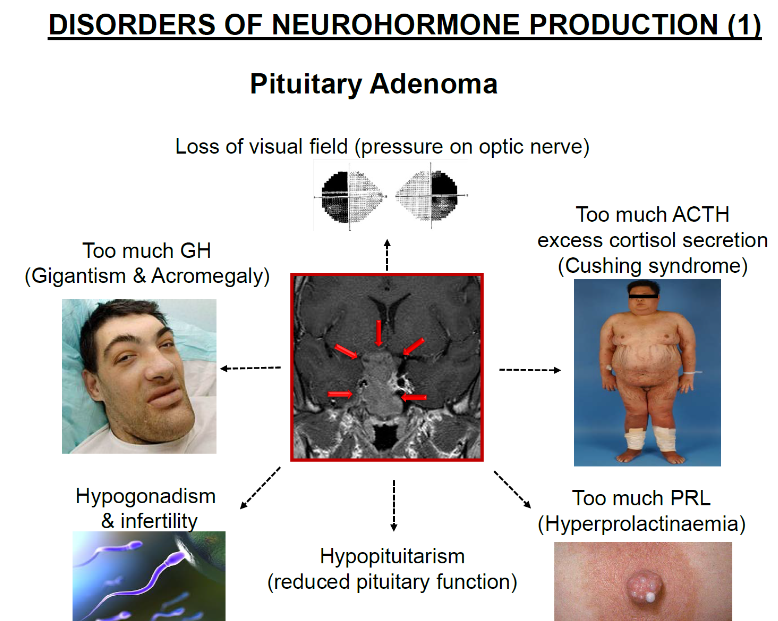
Gigantism: Excess GH in children leads to abnormal growth, particularly in height.
Acromegaly: Excess GH in adults leads to thickening of bones and tissues, especially in the hands, feet, and face.
What are the effects of a pituitary adenoma? (2)
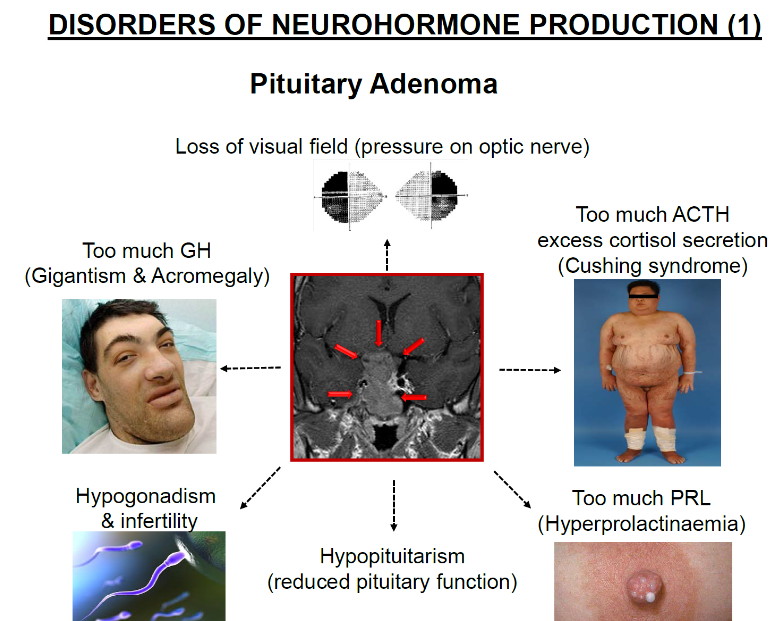
Loss of visual field: Pressure from the adenoma on the optic nerve can cause loss of vision.
Hormone imbalances: Pituitary adenomas can cause excessive secretion of hormones such as ACTH, GH, or PRL.
What are the effects of too much ACTH? (1)
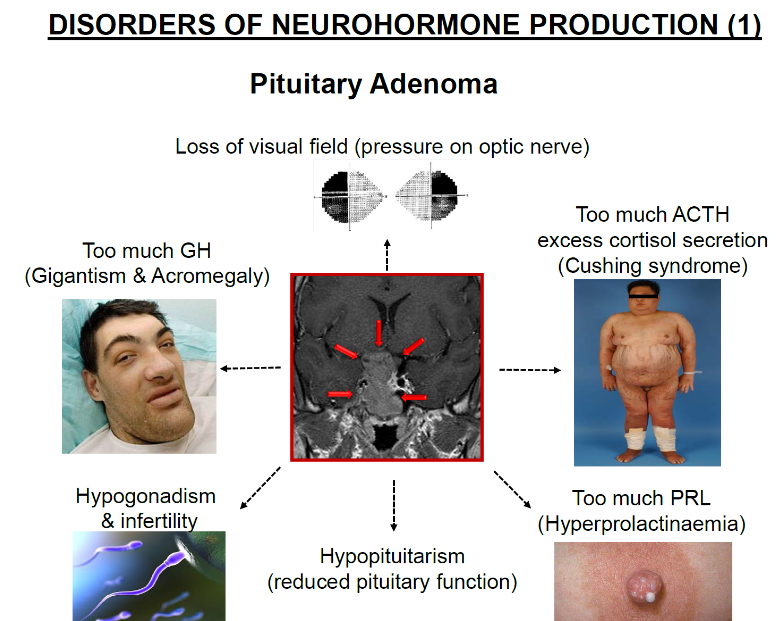
Cushing syndrome: Excess ACTH leads to increased cortisol secretion, causing symptoms such as weight gain, high blood pressure, and a round face.
What are the effects of too much prolactin (PRL)? (1)
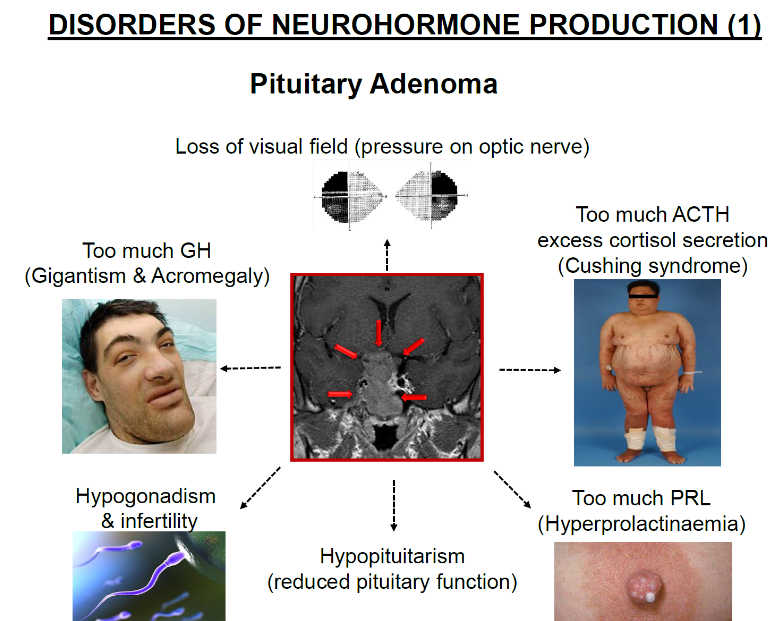
Hyperprolactinaemia: Excess PRL can cause symptoms such as infertility and irregular menstrual cycles in women and erectile dysfunction in men.
What is hypopituitarism? (1)
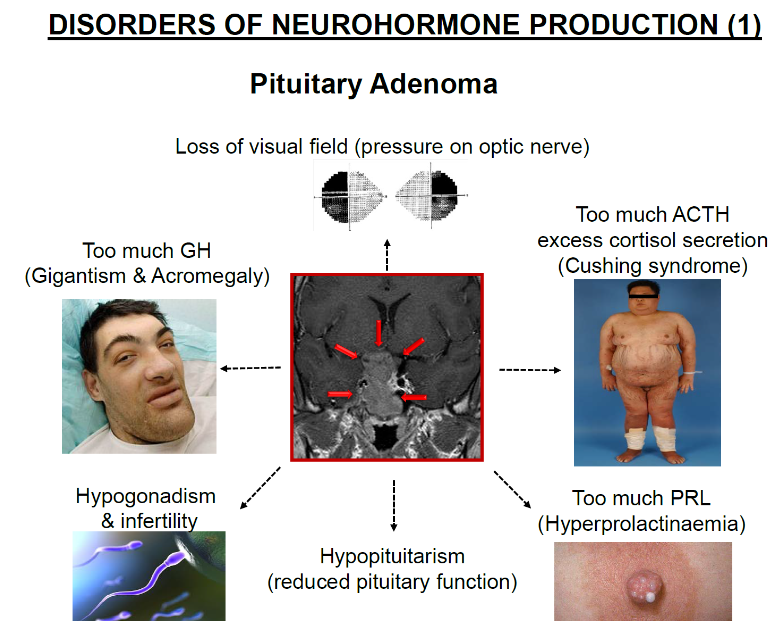
Reduced pituitary function: This condition involves a decrease in the production or secretion of one or more pituitary hormones, affecting various bodily functions.
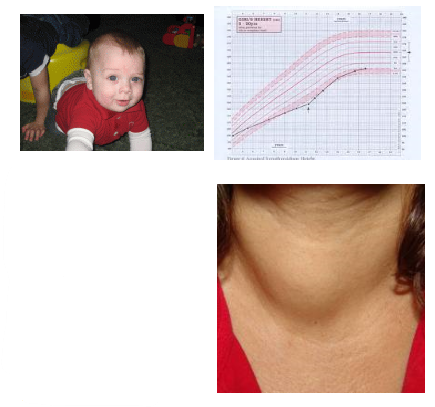
What is hypothyroidism and what are its effects? (4)
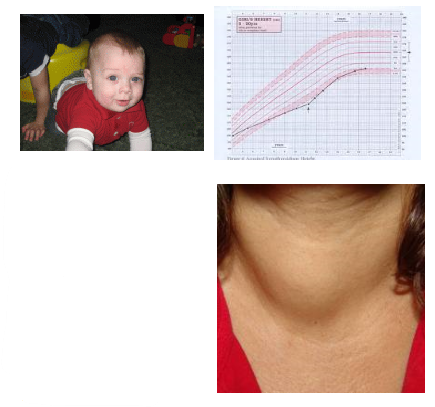
Hypothyroidism: A condition where there is too little thyroid hormone in the body.
Effects: Can lead to mental retardation, slow growth, cold hands and feet, lack of energy, and other symptoms.
Causes: The most common cause is Hashimoto's disease, an autoimmune disorder where the immune system attacks the thyroid.
Risk Factors: More common in women, those with a family history of thyroid disease, or following radioactive iodine treatment, thyroid surgery, or pituitary dysfunction.
What are the potential effects of hypothyroidism in older individuals? (4)
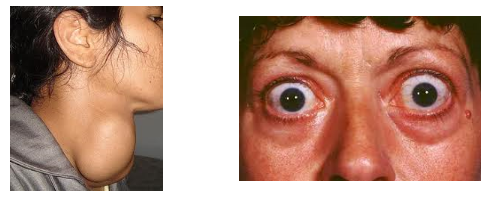
Goitre: Swelling of the thyroid gland.
Heart failure: Due to the effects on heart function.
Depression: Commonly seen in older individuals with hypothyroidism.
Slowed mental functioning: Can lead to cognitive decline.
What are the risks of untreated hypothyroidism in infants and children? (2)
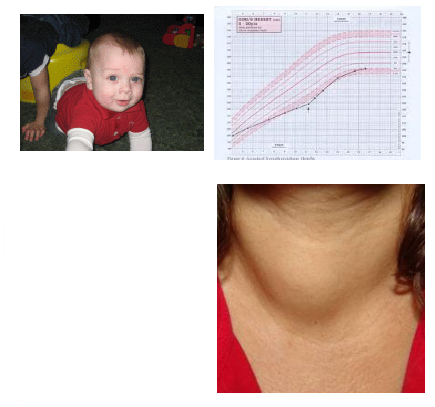
Mental retardation and slow growth: If untreated, hypothyroidism can cause developmental delays.
Stillbirth or premature birth: Babies may be born with lower IQ and developmental issues later in life.
What is the brain mechanism behind hypothyroidism? (1)
Unclear: The exact brain mechanisms underlying the changes in function due to hypothyroidism are not well understood.
What is hyperthyroidism and what is its cause? (3)
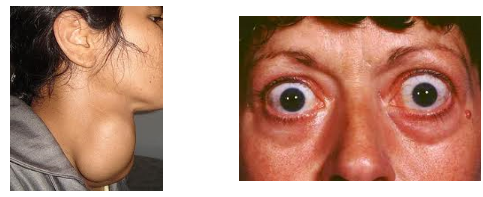
Hyperthyroidism: A condition where the thyroid gland produces too much thyroid hormone.
Cause: The most common cause is Graves' disease, an autoimmune disorder where antibodies attack the thyroid gland and mimic TSH, causing excessive thyroid hormone production.
Risk Factors: More common in women, especially between ages 20-50, and those with a family history of thyroid disease.
What are the signs and symptoms of hyperthyroidism? (7)
Goitre: Enlarged thyroid gland.
Difficulty breathing: Due to the enlarged thyroid.
Anxiety and irritability: Emotional symptoms.
Difficulty sleeping: Related to the overstimulation of the body.
Fatigue: Despite the hyperactive thyroid.
Rapid or irregular heartbeat: Increased heart rate due to excess thyroid hormones.
Trembling fingers, excess perspiration, heat sensitivity, weight loss: Despite normal food intake.
What are the complications associated with hyperthyroidism? (4)
Heart failure: Due to excessive strain on the heart.
Osteoporosis: Weakening of bones due to hormone imbalance.
Pregnancy complications: Increased risk of miscarriage, premature birth, and low birth weight in babies.
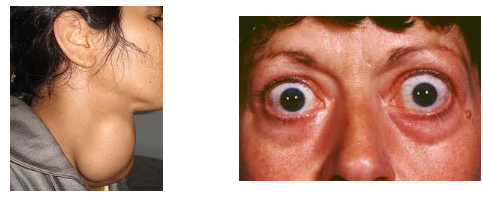
Graves' ophthalmopathy: Rare condition causing bulging eyes if untreated.
What is adrenal insufficiency (Addison’s disease) and what causes it? (2)

Adrenal insufficiency (Addison’s disease): A condition where the adrenal glands do not secrete enough steroids.
Cause: The most common cause of primary adrenal insufficiency is an autoimmune disorder.
What are the symptoms of adrenal insufficiency (Addison’s disease)? (8)

Fatigue and muscle weakness: Common due to lack of cortisol.
Decreased appetite and weight loss: Resulting from hormonal imbalance.
Nausea, vomiting, and diarrhea: Gastrointestinal symptoms.
Muscle and joint pain: Affects mobility.
Low blood pressure and dizziness: Due to insufficient cortisol.
Low blood glucose: As cortisol is involved in glucose regulation.
Sweating and darkened skin: Particularly on the face, neck, and back of the hands.
Irregular menstruation: Hormonal disruptions in women.
What is Cushing's syndrome and what causes it? (3)

Cushing's syndrome: A condition caused by excess cortisol secretion.
Exogenous Cushing's syndrome: Caused by taking cortisol-like medications (e.g., prednisone) for treating inflammatory disorders, asthma, rheumatoid arthritis, or after organ transplants.
Endogenous Cushing's syndrome (Cushing's disease): Occurs when a pituitary tumor produces too much ACTH, leading to excess cortisol production.
What are the signs and symptoms of Cushing's syndrome? (7)

Weight gain and rounded face: Often seen in the upper back and face.
Excess fat on the upper back and above the clavicles: Characteristic fat deposits.
Diabetes and hypertension: Resulting from high cortisol levels.
Osteoporosis: Bone weakness due to cortisol excess.
Muscle loss and weakness: As a result of protein breakdown.
Thin, fragile skin: Bruising easily and purple-red stretch marks.
Facial hair in women and irregular menstruation: Hormonal disruptions in females.
What is homeostasis and which part of the body regulates it? (2)
Homeostasis: The maintenance of the body's internal environment within a narrow physiological range.
Regulation: The hypothalamus is the prime regulator of homeostasis.
What are neurohormones and give two examples? (2)
Neurohormones: Hormones produced by nerve cells and secreted directly into the blood circulation.
Examples: Vasopressin and noradrenaline.
What are hypophysiotropic hormones and where are they produced? (3)
Hypophysiotropic hormones: Hormones produced by endocrine cells in the hypothalamus.
Production location: These hormones are released at a capillary bed called the median eminence.
Transport: They are conveyed directly to the adenohypophysis (anterior pituitary) via the hypophyseal portal vessels.
What is the hypothalamic-pituitary portal circulation and its function? (3)
Hypothalamic-pituitary portal circulation: A system of blood vessels in the microcirculation at the base of the brain, connecting the hypothalamus with the anterior pituitary.
Main function: To quickly transport and exchange hormones between the hypothalamus (specifically the arcuate nucleus) and the anterior pituitary gland.
What is Addison’s disease and what are its symptoms? (5)
Addison’s disease: A disorder that occurs when the body produces insufficient amounts of hormones from the adrenal glands.
Symptoms: Progressive anaemia, low blood pressure, great weakness, and bronze discoloration of the skin.
Hormones affected: Insufficient cortisol and aldosterone levels.
What is Cushing’s syndrome and what are its common features? (4)
Cushing’s syndrome: A metabolic disorder caused by overproduction of corticosteroid hormones by the adrenal cortex.
Common features: Obesity, high blood pressure, and other metabolic complications.