What system is fight or flight?
Sympathetic
What system is rest and digest
parasympathetic
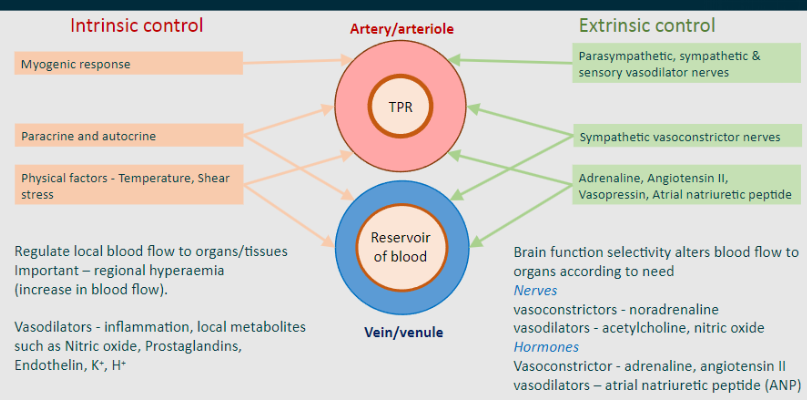
What is the point of the intrinsic control of blood?
Regulate local blood flow to organs/tissues
What is the point of the extrinsic control of blood?
Brain function selectivity alters blood flow to organs according to need
What are some vasodilators relating to intrinsic control? (includes inflammation and local metabolites such as…) (5)
-Nitric oxide
-Prostaglandins
-Endothelin
-K+
-H+
What are some vasoconstrictors and vasodilators relating to nerves of the extrinsic control mechanisms? (3)
Vasoconstrictors - noradrenaline
Vasodilators - acetylcholine, nitric oxide
What are some vasoconstrictors and vasodilators relating to hormones of the extrinsic control mechanisms? (3)
Vasoconstrictor - adrenaline, angiotensin II
Vasodilators – atrial natriuretic peptide (ANP)
What nerves and neurotransmitters control the artery/arteriole during extrinsic control? (TPR)
-Parasympathetic, sympathetic and sensory vasodilator nerves
-Sympathetic vasoconstrictor nerves
-Adrenaline, Angiotensin II, Vasopressin, Atrial natriuretic peptide
What nerves and neurotransmitters control the Vein/venule during extrinsic control? (Reservoir of Blood)
-Sympathetic vasoconstrictor nerves
-Adrenaline, Angiotensin II, Vasopressin, Atrial natriuretic peptide
What Mechanisms and factors control the artery/arteriole during Intrinsic control? (TPR) (3)
-Myogenic response
-Paracrine and autocrine mechanisms
-Physical factors = Temperature, Shear stress
What nerves control the Vein/venule during Intrinsic control? (Reservoir of Blood)
-Paracrine and autocrine mechanisms
-Physical factors - Temperature, Shear stress
Picture demonstrating an overview of vascular control:
What is the most widespread and important extrinsic control system?
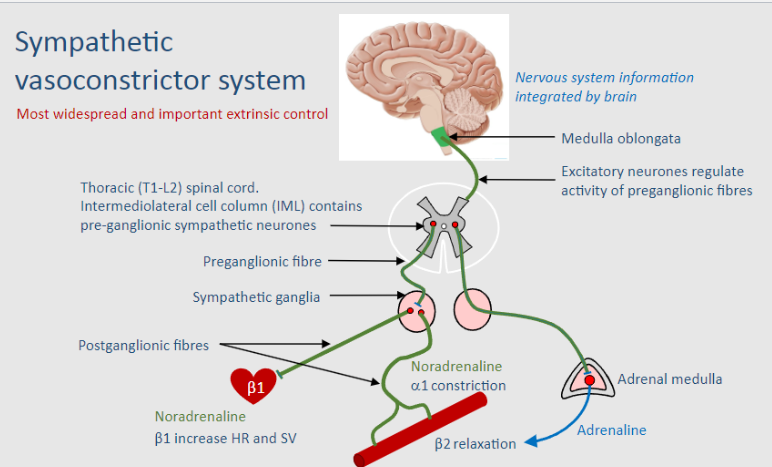
Sympathetic vasoconstrictor system
State how neurotransmitters (NA) act at the Sympathetic vasoconstrictor nerves: (6 steps)
1. An action potential moves down the axon and arrive at a varicosity
2. Depolarisation at the varicosity activating voltage gated Ca2+ channels
3. Ingress of calcium causes release of neurotransmitters - mainly noradrenaline
4. NA diffuses to the vascular smooth muscle cells where it binds mainly α1 – contraction; some α2 – contraction and β2 – relaxation. Modulation of responses in both constriction and dilatation
5. The noradrenaline is then taken up again and recycled or broken down
6. Adrenaline from the adrenals and released into the circulation can also act at α1 or β2 receptors
Release of NA at the varicosity can be modulated by what? And where does it act on? What is increased?
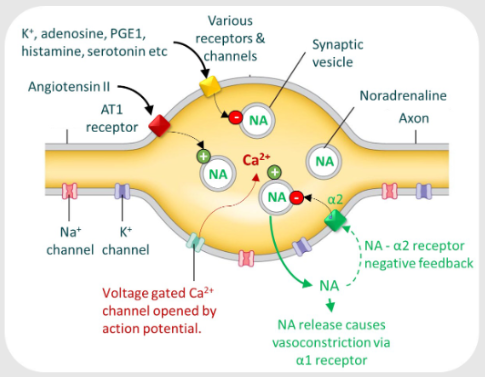
-Angiotensin II
-On the AT1 receptor
-Increases NA release
Metabolites prevent what to maintain blood flow?
Vasoconstriction
What are some examples of metabolites? (4)
-K+
-Adenosine
-Histamine
-Serotonin
How can NA negatively feedback on itself?
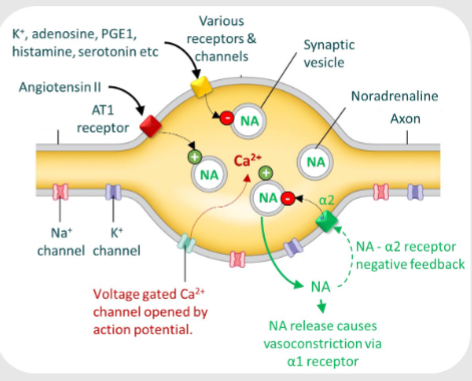
Via a2 receptors to limit its own release
What 2 main things are controlled by the brainstem? Whats the purpose?
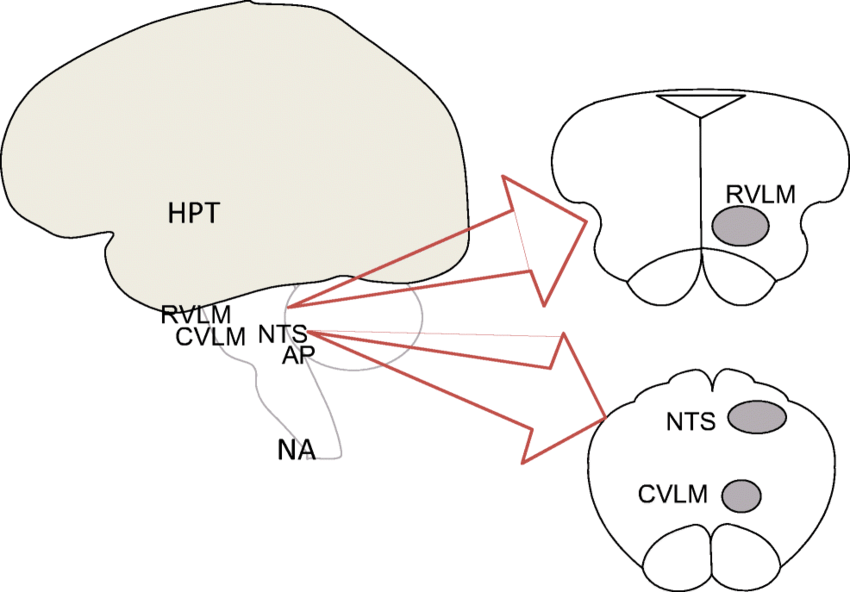
-Rostral ventrolateral medulla (RVLM) – this is controlled by other areas such as:
-Caudal ventrolateral medulla (CVLM) hypothalamus -Provides central control of blood flow & blood pressure
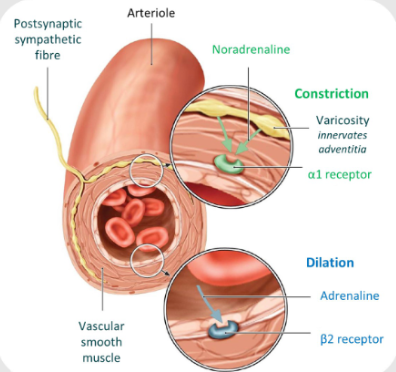
How are arterioles and veins innerverted?
-NA activates a1-adrenoceptors on vascular smooth muscle cells, causing vasoconstriction
-Sympathetic nerve activity is tonic (1 action potential per second), Tonic sympathetic activity sets vascular tone
-Decrease in sympathetic activity producing vasodilatation is an important principle in pharmacological treatment of cardiovascular disease, e.g. Hypertension
What does tonic mean?
1 action potential occurs per second
What are the main roles of the Distinct sympathetic pathway innervation of different tissues? (1)
-Switching on vasoconstriction in some vessels and off in other vessels (producing vasodilation)
e.g. During exercise increased sympathetic nerve stimulation to GI (less blood flow), reduces sympathetic nerve stimulation to skin (more blood flow, to assist heat loss)
What are the main roles of the control of resistance arterioles? (1)
-Produces vascular tone, allows vasodilatation/vasoconstriction controlling TPR
-Maintains arterial blood pressure and blood flow to brain myocardium & kidney etc
What are the main roles of Pre-capillary/arteriole vasoconstriction? (1)
-Leads to downstream capillary pressure drop, so increased absorption of interstitial fluid into blood plasma to maintain blood volume (important in hypovolaemia).
What are the main roles of the Control of venous blood volume?
Venoconstriction results in reduced venous compliance, promoting more efficient venous return and enhancing preload. This increased preload, as per Starling's law, leads to increased stroke volume and subsequently elevates cardiac output
When does vasodilation usually occur? (sympathetic)
Occurs when vascular tone produced by sympathetic vasoconstrictor nerves are inhibited
Picture elaborating vasodilator nerves: (sympathetic)
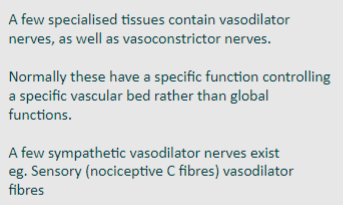
Specific vasodilator nerves are mainly......
Parasympathetic
Picture elaborating on vasodilator nerves: (Parasympathetic)
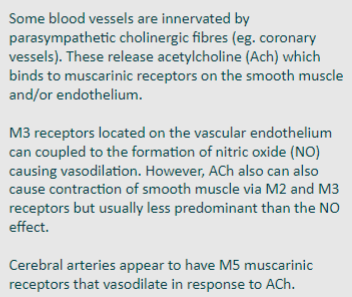
What are 3 good examples of Parasympathetic vasodilators? (organs and components of the body, NOT neurotransmitters)
-Salivary glands
-Pancreas and intestinal mucosa
-Male genitalia (erectile tissue)
How do the salivary glands vasodilate? (1)
Release acetylcholine (Ach) vasoactive intestinal peptide (VIP)
How do the pancreas and intestinal mucosa vasodilate? (2)
-Release VIP; Both these tissues need high blood flow to maintain fluid secretion
-Ach/VIP act on endothelium to cause release of nitric oxide (NO) - vasodilatation

How do the male genitalia vasodilate? (1) How does Viagra enhance this effect? (1)
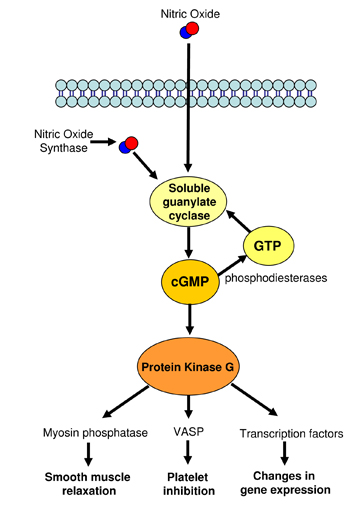
-Release of NO by parasympathetic nerves causes production of cGMP which leads to vasodilatation
-Sildenafil (Viagra) enhances this effect of NO by inhibiting the breakdown of cGMP by phosophodiesterase-5
What is a good example of sympathetic vasodilators?
Skin (sudomotor fibres)
How does the skin (sudomotor fibres) vasodilate? (4)
-Release Ach, VIP (Vasoactive Intestinal Peptide) causing vasodilation via NO associated with sweating
-Increased blood flow cause more sweat and also allows heat loss via skin
-Sympathetic activity vasoconstriction would only reduce blood flow, limit sweat production and limit cooling
-Emotional centres in the brain have some control over these fibres, head, face, upper chest, involved in blushing
Stimulation of sensory axon reflex (C-fibres) by trauma, infection etc will release what?
Substance P or calcitonin gene-related peptide (CGRP)
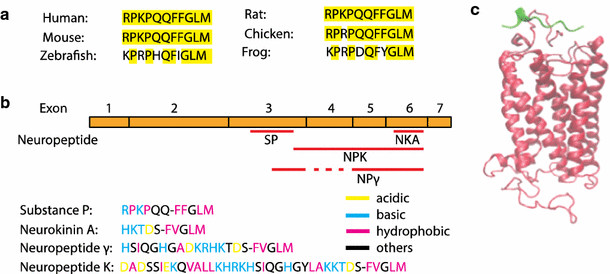
What does Substance P or calcitonin gene-related peptide (CGRP) do? (act on) (2)
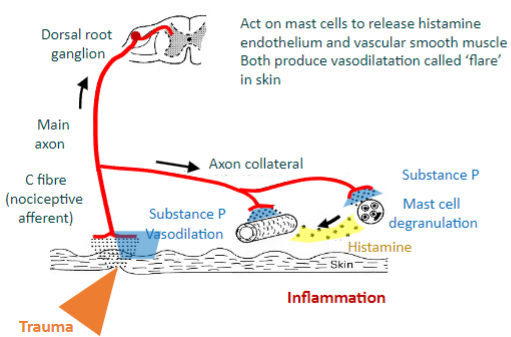
-Act on mast cells to release histamine (which acts on the endothelium and vascular smooth muscle)
-Both produce vasodilatation called ‘flare’ in skin
Inflammation is part of the Lewis triple response, What are the parts of the Lewis triple response? (elaborate slightly on each)
1. Redness, caused by capillary vasodilation
2. Flare, a redness in the surrounding area due to arteriolar dilation mediated by axon reflex
3. Wheal, exudation of extracellular fluid from capillaries and venules
Why is the lewis triple response important?
Increases delivery of immune cells & antibodies to site of damage to deal with invading pathogens
Name 3 hormones that cause vasoconstriction:
-Adrenaline
-Angiotensin II (Ang II)
-Vasopressin (Anti-Diuretic Hormone, ADH)
Name 1 hormone that causes vasodilation:
-Atrial natriuretic peptide (ANP)
Where is adrenaline released from? (1) Via the action of what? (4)
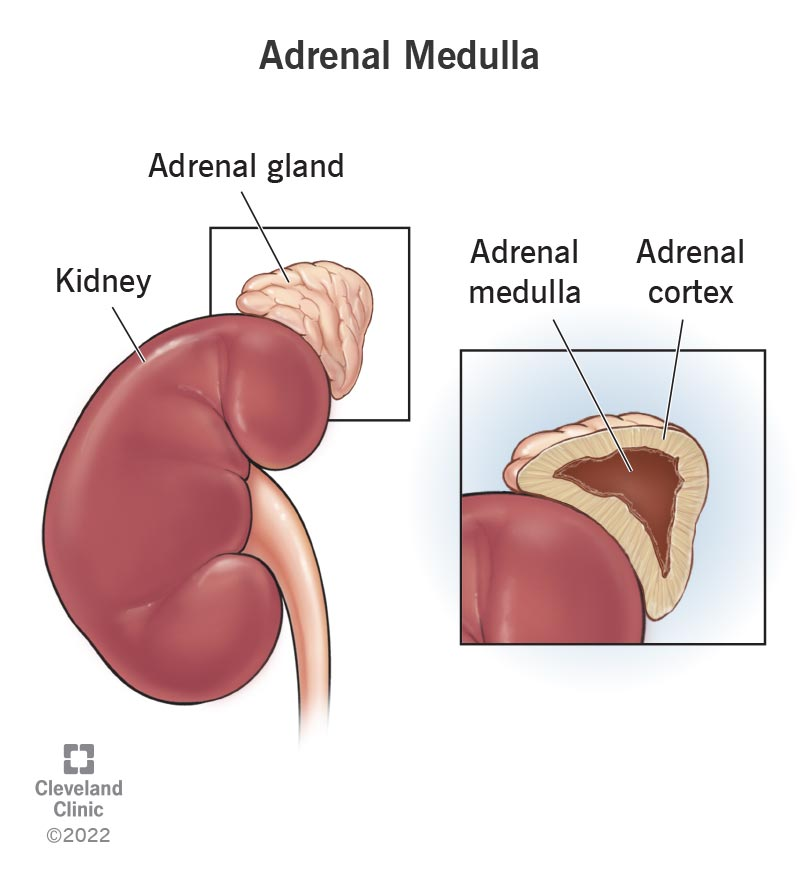
-Released from adrenal medulla
-via action of acetylcholine on nicotinic receptors during: Exercise and Flight-or-Fight responses
-Fear response (increase sympathetic drive), Hypotension (baroreceptor reflex), Hypoglycaemia
What are the Main roles of adrenaline? (metabolic and CVS effects)
-Glucose mobilisation (skeletal muscle glycogenolysis, fat lipolysis, β3)
-Stimulation of heart rate & contractility during normal exercise (β1)
-Vasodilatation of coronary and skeletal muscle arteries (β2)
STATEMENT:
Skeletal muscle and coronary arteries have less b2 than a1 adrenoceptors
Is this true?
No
Skeletal muscle and coronary arteries have more b2 than a1 adrenoceptors
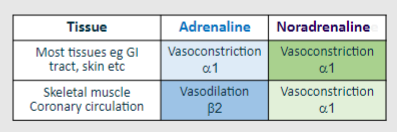
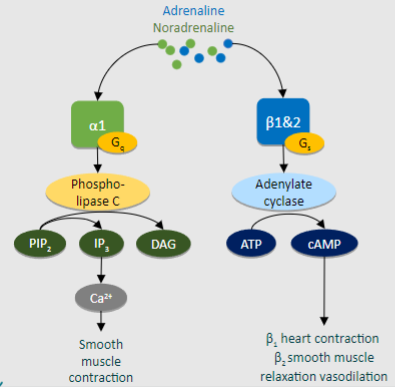
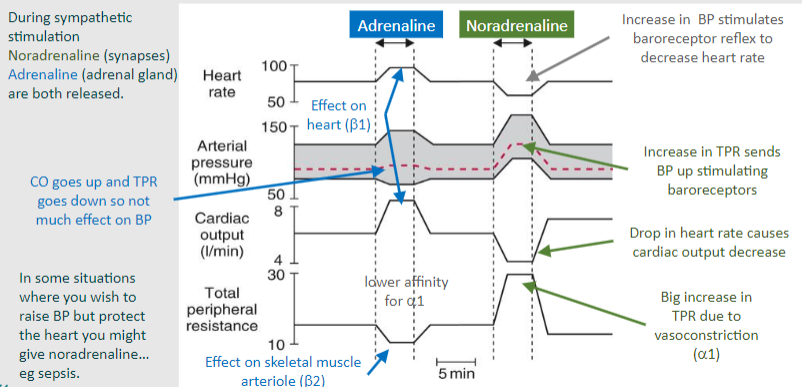
Adrenaline has a higher affinity for what type receptor over another receptor, what are these receptors?
Where does adrenaline usually act and to do what?
-Higher affinity for b over a
-mainly acts at b2 to dilate vessels
Noradrenaline has a higher affinity for what type receptor over another receptor, what are these receptors?
Where does noradrenaline usually act and to do what?
-Higher affinity for a over b
-Mainly acts at a1 receptors to constrict vessels
Picture summarising Adrenaline vs Noradrenaline impacts on tissues
What does the b1 receptor generally do relating to the heart?
Heart increases rate and force of contraction
What does the a2 receptor generally do relating to adenylate cyclase?
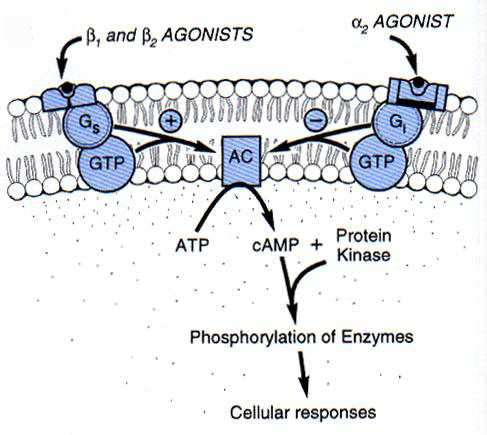
Inhibits adenylate cyclase, leading to ATP unable to be converted to cAMP, leads to reduced Ca2+ and inhibits release of noradrenaline from varicosity
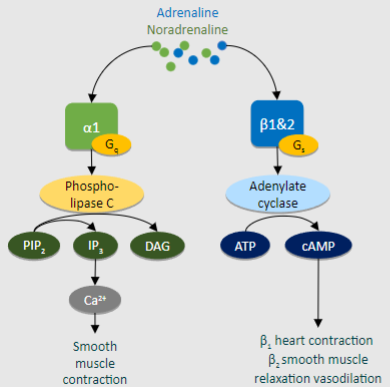
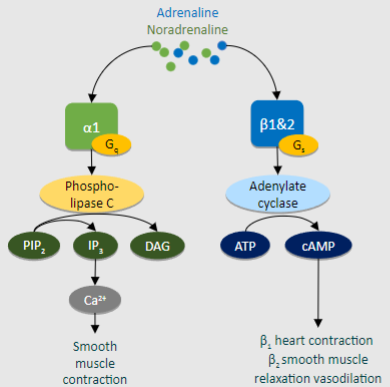
Outline the action of Noradrenaline at the a1 adrenoceptor:
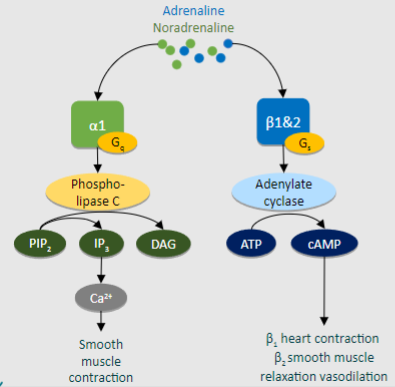
Binding: Noradrenaline binds to α1 adrenoceptors.
Activation: α1 adrenoceptor activation causes conformational changes.
G-protein Coupling: Activated receptor interacts with Gq/11 protein.
Phospholipase C Activation: Stimulates phospholipase C (PLC) enzyme.
Intracellular Signaling: PLC hydrolyzes PIP2 into IP3 and DAG.
IP3-Mediated Calcium Release: IP3 triggers calcium release from ER stores.
Calcium Signaling: Increased calcium activates downstream effectors.
Smooth Muscle Contraction: Resultant signaling leads to smooth muscle contraction, particularly in blood vessels, causing vasoconstriction.
Outline the action of Adrenaline at the b1 adrenoceptor:
Binding: Adrenaline binds to β1 adrenoceptors.
Activation: β1 adrenoceptor activation causes conformational changes.
G-protein Coupling: Activated receptor interacts with Gs protein.
cAMP Production: Gs protein stimulates adenylyl cyclase.
Intracellular Signaling: Adenylyl cyclase produces cAMP, activating PKA.
Cardiac Effects: Increased contractility, heart rate, and conduction velocity.
Vascular Effects: Some vasodilation in select vascular beds.
Picture demonstrating the effect of iv adrenaline versus iv noradrenaline on circulation
Picture outlining the cycle of the renin-angiotensin-aldosterone system (RAAS)
State the process of the release of Vasopressin (antidiuretic hormone - ADH) (3)
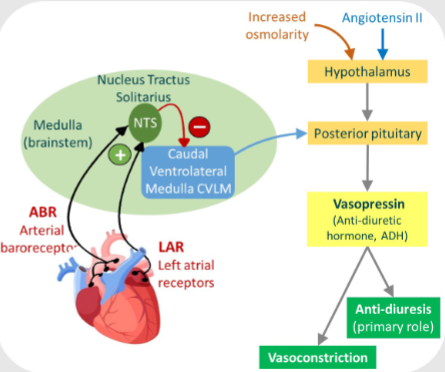
-Stretch receptors in the left atrium send continuous signals via afferent fibres to the NTS.
-The NTS sends out inhibitory nerves to the CVLM
-CVLM signals stimulate the pituitary gland to release vasopressin so stretching of the heart inhibits this
How does dehydration or haemorrhage impact the NTS?
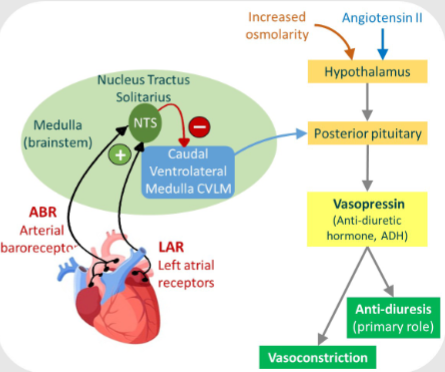
NTS inhibition is switched off and CVLM stimulates vasopressin
How is the response of the hypothalamus stimulated by? (in this context)
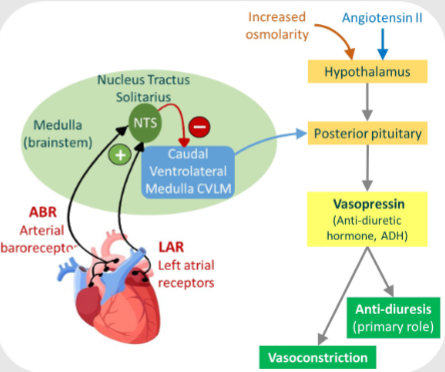
Increase in osmolarity, i.e. dehydration or low blood volume
Where is vasopressin synthesised and released?
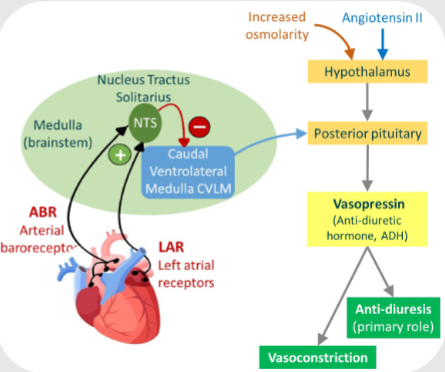
Synthesised in hypothalamus and released from vesicles in posterior of pituitary gland
What does vasopressin actually do? (1 long answer)
-Causes insertion of water aquaporin channels into the apical membrane of renal collecting tubules and collecting duct epithelial cells, allowing water to move out of the nephron and back into the bloodstream
What else does vasopressin do? (2)
-Reabsorption of fluid by kidney-Vasoconstriction, both maintain blood pressure
What does ANP stand for?
Atrial natriuretic peptide
What releases ANP? How is it secreted?
-By specialised atrial myocytes
-Secreted by increased filling pressures which stimulate stretch receptors
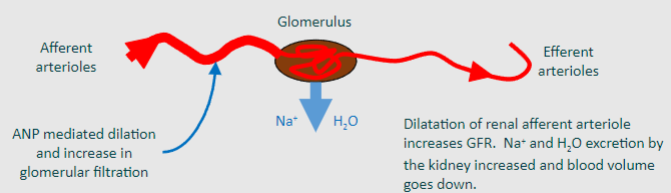
Where does ANP act and what does it do?
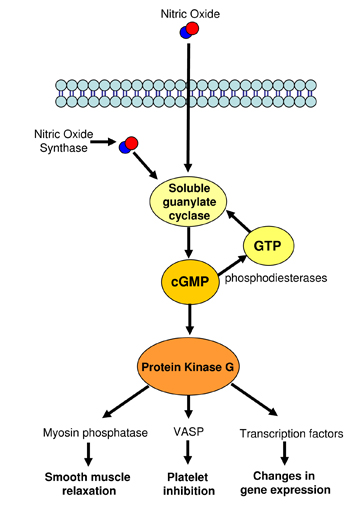
Act at ANP receptors on vascular smooth muscle cells increasing cGMP pathway (like nitric oxide)
ANP action allows for systemic vasodilation, therefore it opposes the action of what?
Opposes action of noradrenaline, RAAS, ADH.
Picture demonstrating the action of ANP:
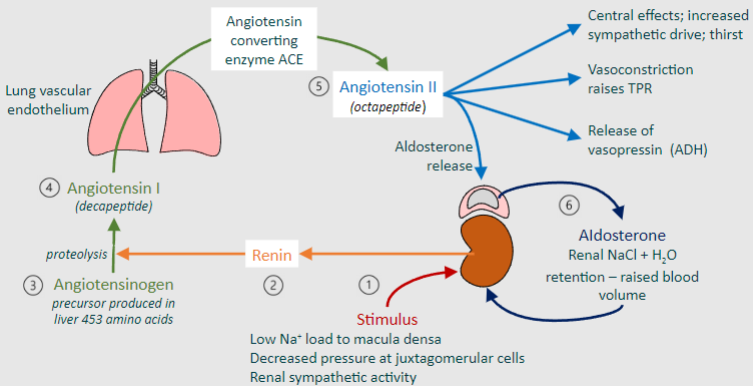
The Renin-Angiotensin-Aldosterone System (RAAS) is a vital physiological pathway involved in regulating blood pressure and fluid balance. State the first 3 steps of the cycle:
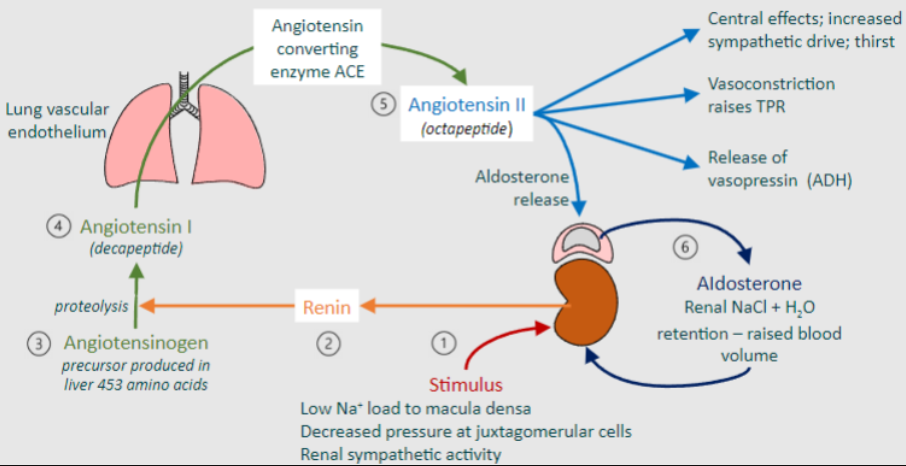
Stimulus: Various stimuli can trigger the activation of the RAAS, including low sodium (Nat) load to the macula densa, decreased pressure at juxtaglomerular cells, or increased renal sympathetic activity.
Renin Release: In response to the stimulus, renin is released from the juxtaglomerular cells in the kidneys. Renin acts on angiotensinogen, a precursor produced in the liver, to initiate proteolysis, converting angiotensinogen into angiotensin I, a decapeptide.
Angiotensin Converting Enzyme (ACE): Angiotensin I travels through the bloodstream to the lungs, where it encounters angiotensin converting enzyme (ACE). ACE catalyzes the conversion of angiotensin I into angiotensin II, an octapeptide.
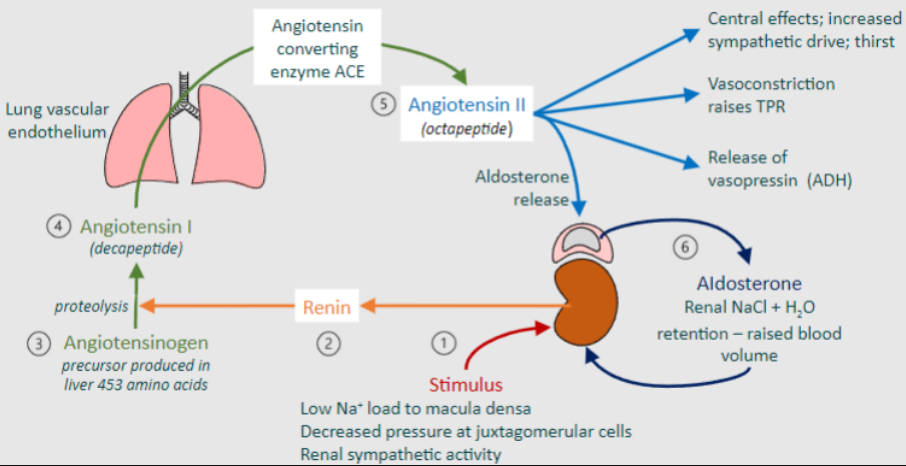
The Renin-Angiotensin-Aldosterone System (RAAS) is a vital physiological pathway involved in regulating blood pressure and fluid balance. State the last 3 steps of the cycle:
Angiotensin II: Angiotensin II is a potent vasoconstrictor that acts on blood vessels throughout the body, leading to vasoconstriction and raising total peripheral resistance (TPR). It also stimulates the release of vasopressin (antidiuretic hormone, ADH) from the posterior pituitary gland.
Central Effects: Angiotensin II has central effects, including increasing sympathetic drive and thirst sensation, which further contribute to blood pressure regulation.
Aldosterone Release: Angiotensin II also stimulates the release of aldosterone from the adrenal cortex. Aldosterone acts on the kidneys to increase the reabsorption of sodium chloride (NaCl) and water, leading to renal NaCl + H2O retention and raising blood volume.