Morale
absolute universal principles which:
•The society accepts
• Govern the behavior of oil citizens at all times
• Not relative o any context or era
• Religion is a m4jor source of morals
Ethics
Moral principles governing the behavior of a principle group in relation
to i†s distinctive role in society (medical ethics)
Core ethical principles in heal the cure: 4 major ethical principles:
1-non maleficence(not harm . avoid physical or psychic harm due †o:
• negligence (careless omission of what should be done).
•Lock of medical experience (due to sufficient knowledge or skills).
2 beneficence (to do good}. to be of benefit to patient & prevent harm:
• individual patient (treatment 6 promotion of health)
• society (preventing disease. researches6 vaccines)
Core ethical principles in heal the cure: 4 major ethical principles:(2,0)
3-justice( to be fair) Fairness in he distribution of medical services
• Fair criteria: criteria must be determined for allocating limited resources
(resource allocation) e.g. urgency of †he condition, first comes first served.
4- Respect for autonomy (free decision). Patient must indicate his approval &
willingness to accept proposed treatments. It is the basis of informed consent):
Choice should be:
• intentional free of undue or controlling outside influence
• mode with rational understanding
• patient is not highly confused or impaired cognition
professional ethical principles ( Medical professionalism )
They are basic, universal & shared by professional ethical codes around the world. They are concerned with 2 main broad issues :
• Duties & responsibilities of physician towards his patients, colleagues & society.
• moral activates ( moral traits ) that should characterize the behavior of physician
Responsibilities o f Therapists towards patients:
-1 Primacy of patient's interest &welfare: Serve the interest of the patient, not his own interest
2- Respect of the patient's autonomy: honest with patients &empower them ot make informed decision about treatment
-3 Respect patient's rights as wel as his dignity & privacy
4-Treat the patient, as a person with benefits, Values, goals &concerns, not a disease i.e. provide medical care with a caring, compassionate &human manner.
5- Commitment to absolute confidentiality: about his patient, even after his death. It is broken only by conditions dictated by law (patient endangers others)
6- Social justice &equality: Fair distribution of health care resources &treated equally without discrimination whether based on race, gender, socioeconomic status, ethnicity, religion,
7- Provide care for patients who are unable t o p a y & facilitate access of health care for undeserved areas
Professional Competence
Competence: "possession of required skil, knowledge, qualification or capacity"
1- Commitment to professional competence: Life-long learning of knowledge &skills → provision of quality care. Profession must ensure that continuous medical education &training programs are available for physicians to accomplish this goal.
-2 Recognize the limits of his professional competence (refer the patient if beyond capacity)
3- Exercise great caution i n using new diagnostic or treatment method. Be sure that they have been evaluated &certified according to approved ethical & scientific research criteria.
Boundary issues of Medical Profession
-1 Maintain honesty, integrity &self-discipline interactions with patients, families&colleagues (reliability, availability &timeliness of task completion).
2- keep appropriate professorial relationship . Physicians should never exploit patients for personal purposes (financial gain, emotional or sexual ...).
-3 Maintain a dignified professional image in manner, dress, speech &relationships consistent with medical profession's accepted standards in the community.
Do Not seek private gain from for-profit industries (pharmaceutical/medical
equipment/insurance companies). I† should be disclosed to the public.
Responsibilities towards society and humanity
1- Have an obligation of preserving human life
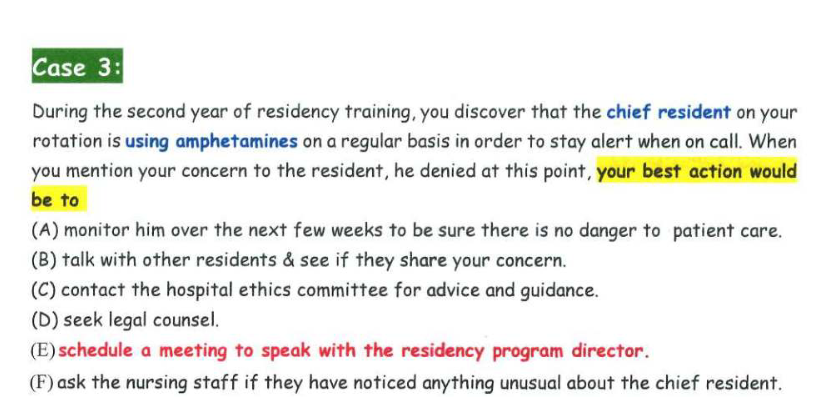
2- Recognize & deal with unethical behavior of colleagues & health care team.
3- Certify only that which he has verified
4- Provide health care based on wise & appropriate allocations of limited medical resources (avoid prescribing unnecessary medication, investigation, procedure)
5- Obligation of public reporting of significant, medical hazards (epidemic infection)
6- Obligation to the health of society. Participate in all efforts to provide, improve & maintain health care quality for society as a whole.
Responsibilities towards society and humanity(Malpractice)
Harm to a patient as a result of action or inaction of a physician.
Elements are (4D):
• Dereliction or negligence (deviation from standard care)
• Duty: established physician-patient relation-ship that causes:
• Damage, injury
• Directly to the patient (by negligence, not another factor)
Responsibilities towards society and humanity(Relation-ship with patient)
• Inappropriate relation is prohibited with current or previous patient
• Avoid treating family members, close friends (feelings may interfere)
• Avoid accepting valuable gifts
• Impairment in physician functioning:
a. Drug or alcohol abuse
b. Physical (handicapping) or mental illness
c. Old age with functional or sensory impairment
framework for ethical reasoning and decisions making
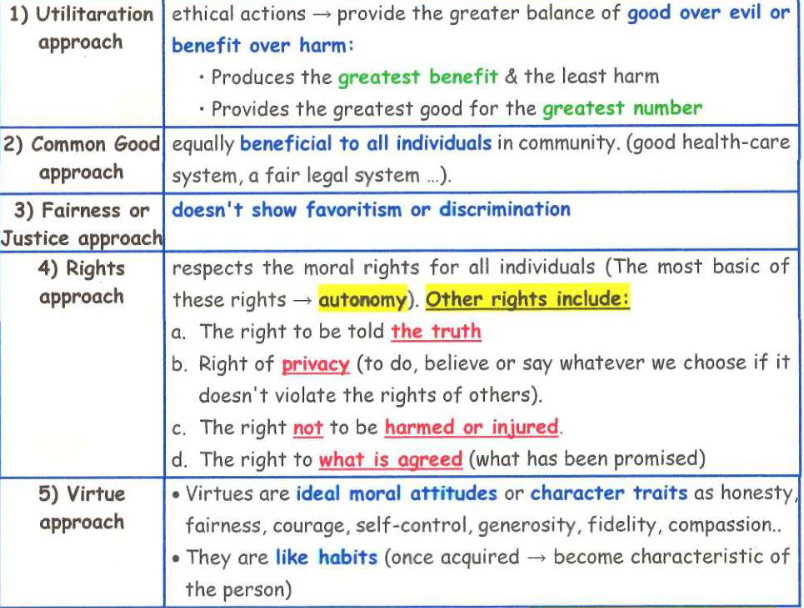
In order to evaluate whether an action is ethical or not we should ask ourselves 5 questions:
1- What benefits&what harms will this action produce?
An ethical action produces the greatest benefit and the least harm.
2- What far does it advance the common good?
An ethical action advances common good over individual interests.
3- Does this action treat everyone the same?
An ethical action, treats everyone equally (no discrimination or favoritism).
4- Does this action violate any o f the moral rights of affected parties? An ethical action should respect the moral rights of all individuals.
5- Is this action consistent with moral virtues?
An ethical action should not contradict or violate moral virtues.
Ethical dilemmas in medicine(Conflict between 2 or more guiding ethical principles)
1 - Conflict between 2 or more guiding ethical principles:
a- In patient with acutely infected appendix may create a conflict between:
• Obligation to provide greatest "benefit" to the patient (immediate surgery).
• Obligation to respect patient's "autonomy" (free decision) not to operate as he is concerned about the risk of anesthesia, operation or blood transfusion
The Physician has to balance the demands of these principles & decide which course of action carries the greatest benefit & least harm.
Ethical dilemmas in medicine(Conflict between 2 or more guiding ethical principles)(2.0)
b- Patient refused blood transfusion in a life-threatening situation → conflict between:
• Obligation to "benefit" the patient'
• Obligation to respect his "autonomy"
c- Terminal illness patients refusing life sustaining procedures (respirator or dialysis) → conflict between:
• Obligation to "preserving life"
• Obligation to respect patient's "autonomy"
Euthanasia: is concerned with whether or not to help the death of patients suffering from terminal illness out of mercy. It is either directly killing the patient, or physician-assisted suicide. Either act is a criminal act.
Ethical dilemmas in medicine(Legal standards of death:)
Irreversible cessation of all brain & brain-stem functions while heart is still beating. Absence of:
Response to external events or painful stimuli
• Spontaneous respiration
• Cephalic reflexes (light & corneal & pharyngeal)
• Cerebral blood flow › 30min
• Electrical potential of cerebral origin over 2mV from symmetrically placed electrodes more than 10cm apart
If the patient is dead according to these legal standards the physician is authorized to remove the life supports.
Ethical dilemmas in medicine(Legal standards of death:)(2.0)
d- Dangerous Patients to others or society (serious contagious disease) conflict between:
• Obligation to respect "confidentiality"
• Obligation to report the condition "avoid harm to others"
2- Conflict between guiding ethical principles & other interests
a. Conflict between:
• our goal of advancing communication efficiency, computerizing patient's records & exchange of medical information by tele-medicine (internet consultation between physicians) & cyber-medicine (internet dealing with patient)
• Obligation to ethical confidentiality & patient's privacy & autonomy).
b. Conflicts related to: abortion, new reproductive technologies, maternal-fetal conflicts of rights, organ transplantation, genetic testing & genetic modification....
Conflict between guiding ethical principal & other interests
a. Conflict between:
• our goal of advancing communication efficiency, computerizing patient's records & exchange of medical information by tele-medicine (internet consultation between physicians) &cyber-medicine (internet dealing with patient)
• Obligation to ethical confidential&patient privacy& autonomy).
b. Conflicts related to: abortion, new reproductive technologies, maternal-fetal
conflicts of rights, organ transplantation, genetic testing &genetic modification..
Special Ethical Issues(Informed consent)
It is the cornerstone of the autonomy principle.
Process by which a fully informed patient can participate in choices about his health care for any medical or surgical procedure and before entering a patient in a research study. 3 essential elements for valid informed consent:
I-The patient should be fully informed about:
1. His diagnosis
2. The nature of the treatment
3. The alternatives of the intervention
4. The risk & benefits of each alternative
5. The prognosis of proposed intervention
6. The information should be easily understood by the patient.
Special Ethical Issues(Informed consent)(2.0)
II-The patient should be competed to make a decision: ability to make decision should not be impaired by illness (mental illness or chronic brain impairment).
Legal competency: adult › 18 years is competent - he must understand the risks,benefits & outcome of decisions.
III- The patient's decision should by voluntary: (should not be under pressure)
The patient can withdraw the consent at any time before the procedure.
Medical interventions requiring informed consent:
Special Ethical Issues(Informed consent)(Medical interventions requiring informed consent)
1) Health care institutions should have policies about medical interventions requiring a signed informed consent: surgery, anesthesia, other invasive procedure.
2) For a wide range of other decisions:
• Written consent is not required or needed.
• A verbal approval with the patient is considered sufficient.
Special Ethical Issue(Exceptions to the requirement of informed consent:)
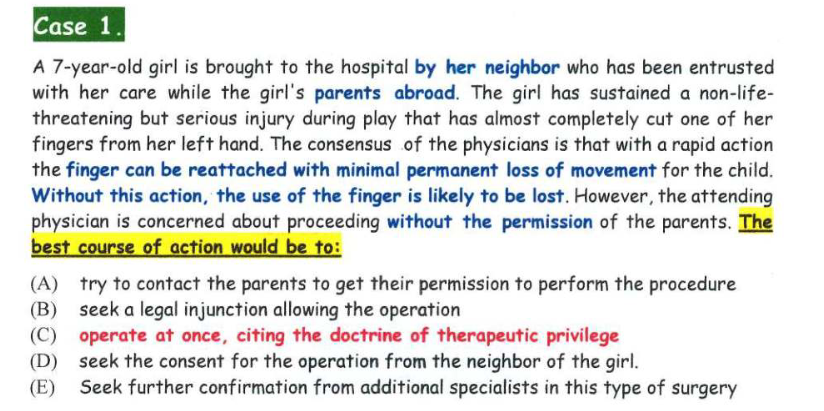
1 -Emergency situations when the patient:
• Is unable to give consent (e.g. unconscious)
• Is suffering from an acute life-threatening crisis
• Is required immediate intervention.
2- Incompetent to make decisions (should be obtained from a substitute decision maker) as when the patient:
a- Is a child
b- His cognitive capacities are impaired.
3- Cases in which fully informing the patient would seriously worsen his condition. Others stressed that competent patients have the right to refuse to consent even if their health will suffer or even death will result.
Special Ethical Issue(Confidentiality)
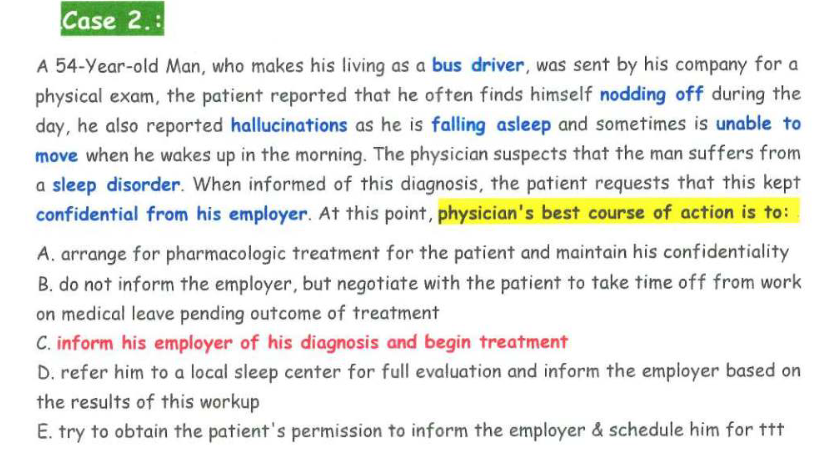
Definition: keeping secret and not disclosing any information about the patient.
This commitment extends after the patient dies
Aim: respects the patient's privacy, autonomy, benefit the patient & prevents possible harms that may result from disclosure of information about his health or personal life.
Breaking confidentiality:
1) Serious harm to others
- Possible murder
- Serious contagious disease
- Patient lacking fitness for some jobs (pilots & bus driver)
2) Possible commitment of suicide
3) Abuse to victims unable to protect themselves (kids)
Physician should be certain, then notify law enforcement officials or social service agency & warn the intended victim or inform his family & provide proper management to patient
Research Ethics
The World Medical Association (Declaration of Helsinki) →ethical principles of
medical research →strict ethical rules ®ulations for conducting research on human subjects.
Special Ethical Issue(Violating ethical principles of medicine)
Common examples of violations:
1) Boundary violation: crossing the boundaries in doctor- patient relationship.
Improper emotional or sexual relation or personal financial gain
2) Mistreatment or patient incompetence: Negligence/lack of sufficient knowledge or skills
3) violation of confidentiality: Patient information's are disclosed to others
without consent
4) violation of the rules of ethical conduct with other members of the profession
6) Illegal activities: illegal abortion or illegal business or financial transactions
Special Ethical Issue(Medical Behavior)
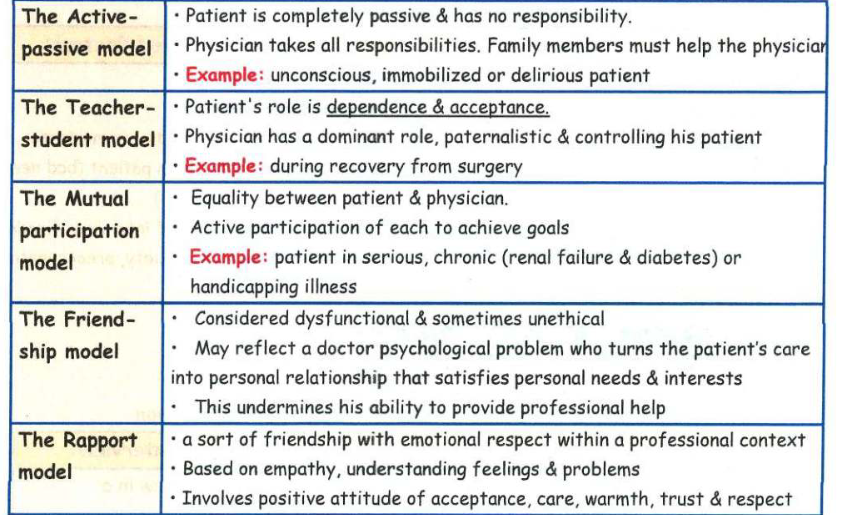
Models of the doctor-patient / relationship Models are often operating unconsciously. Doctor must learn how & when to shift models
Special Ethical Issue(Doctor-patient communication)
A successful doctor can establish a good rapport & communicate efficiently to:
• Reach an accurate diagnosis
Enhance patient cooperation and compliance to treatment plan
Special Ethical Issue(Medical Interview)
(most powerful instrument = corner-stone of problem-
solving). Principles to measure competence in medical education:
1. Patients care
2. Interpersonal and communication skills
3. Medical knowledge
4. Learning and improvement based on practice
5. Professionalism: high standard well-trained
6. Evidence-based medical practice: integrating clinical expertise with best available external clinical evidence from systematic research
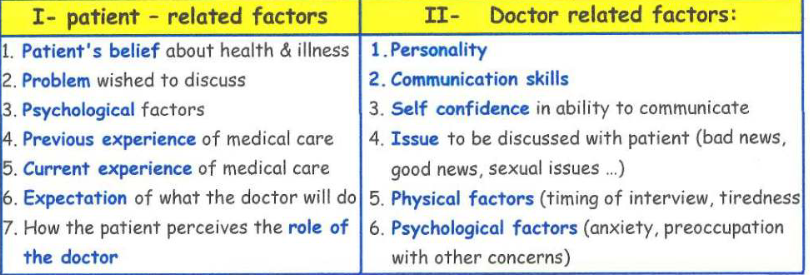
Factors influencing medical interview:
People cope with illness differently (deny, anxiety, depression...). Most express anxiety and apprehension while consulting a doctor
Special Ethical Issue(Steps of Proper Medical Interview)
Before & Beginning of interview: Preparation, establishing relation, identify the reason of consultation
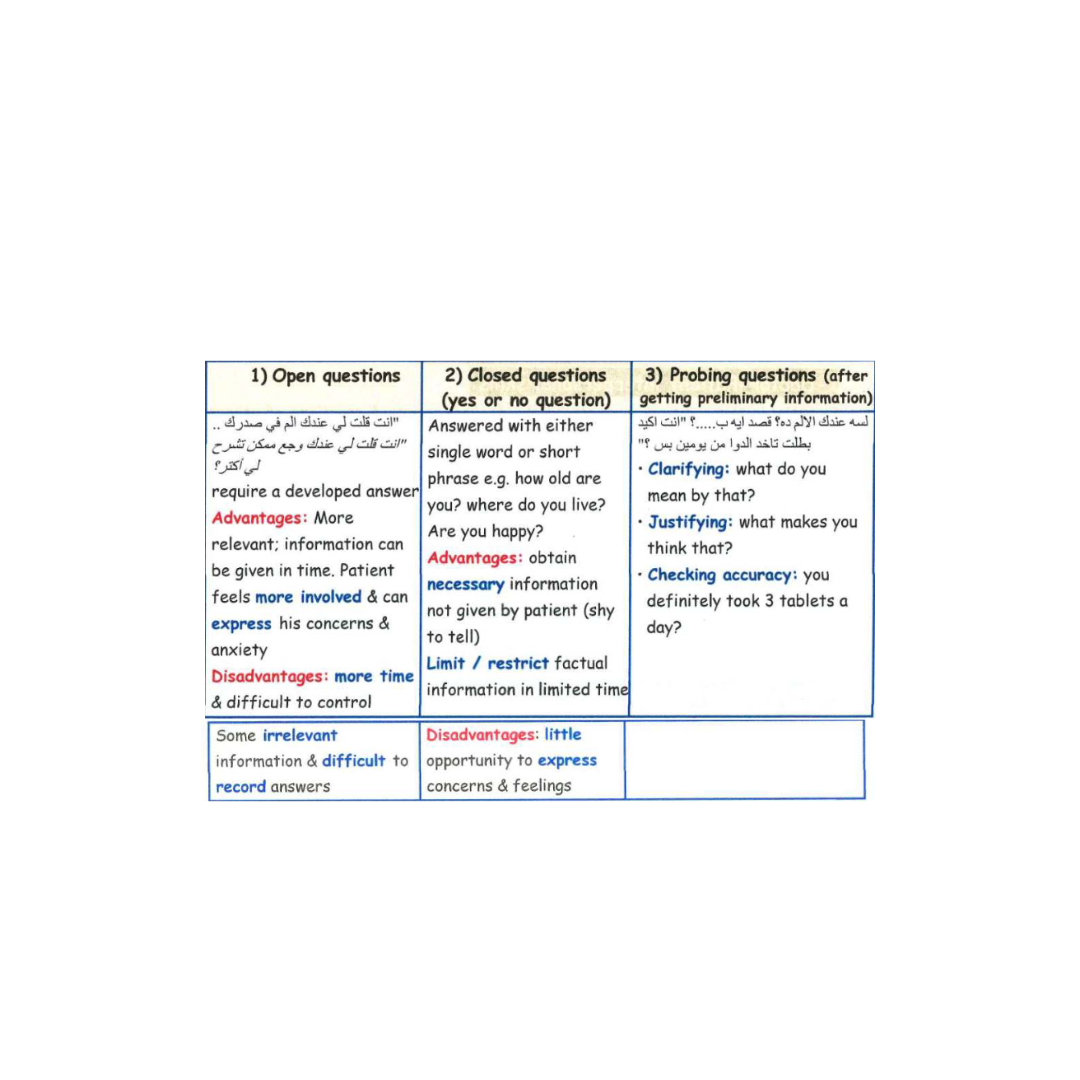
4) Avoided questions:
• Avoid complex questions (to be understood)
• Avoid several questions in one (confusing) [did you have pain in your chest? Was your cough related to this pain? Did it affect your routine physical activities?
• Avoid leading questions (imposes your opinion & mislead diagnosis): can be used to;
• Open / stimulate conversation (encourage rapport)
• Influence patient to agree with interviewee
• Influence the respondent
closing (ending) the interview:
• understanding properly his medical condition
• instructions & prescriptions should be written clearly & accurate recall
• whole treatment plan should be clearly understood for a shared decision making
• future planning & date for next meeting should be decide
Communication skills(Doctor-Patient interpersonal skills)
Empathy is the ability to understand the feelings, needs & reactions of others (patients). It depends on doctor's personality but can be learnt:
1. Good eye contact
2. Appropriate posture & tone of voice
3. Attentive listening
4. Picking up & responding to verbal & non-verbal cues from patient
5. Indicate that you understand him
6. Showing respect & concern,
7. Showing support & warms,
8. Developing a collaborative & cooperative relation
Communication skills(Information-gathering skills)
1. Listening to patient: concentrate on what he says, try to understand his feeling
a. Verbal: active listening by asking questions; don't interrupt him: silences are allowed to give time to patient to reflect on what has been said & to the doctor to observe the patient & plan for the next stage
b. Non-verbal: appropriate posture → lean forward, nod your head, eye contact
2. Facilitation: help the patient to talk through
b. Non-verbal: appropriate posture: lean forward, nod your head, eye contact
3.clarification of vague information
4. Reflection: mirroring back what they have just said help them to proceed their story
5. Helping the patient to be relevant: interrupt at a certain point & try to redirect
6. Signposting: indicate to the patient what you want to discuss next"
( signposts on a road direct us to our destination)
Communication skills(Information giving skills)
1. Clear and simple information (no technical terms)
2. Categorizing information
3. Using repetition & summarizing.
4. Using specific advice and concrete examples.
5. Using explanatory tools e.g. diagrams & written information.
6. Checking patient's understanding
Failure to give information is the most common of dissatisfaction
Giving information has major effect on:
1. Decrease anxiety and stress before investigations & surgery
2. Decrease time spent in hospital; decrease the dose of pain-relieving drugs
3. Satisfaction with care
4. Increase the compliance with treatment
Communication skills(Information giving skills)(2.0)
How to improve your way of giving information?
1. Begin the interview by summary of patient's problem
2. Describe & clarify given information:
a. Results of physical examination
b. Results of tests
c. Diagnosis or provisional diagnosis
d. Cause of problem
e. Necessary further investigations
f. Treatment planned
g. Prognosis
h. Advice about life stile
Communication skills(Information giving skills)(3.0)
3. Describe & explain each part of information with appropriate language:
a. Give the most important first
b. Short words; short sentences
c. Avoid medical jargon
d. Be specific; vague information → increases anxiety
4. If relevant, use drawing to supplement the information
5. Outline the plan of the rest of the interview: discuss diagnosis; treatment;
future investigation -» improve patient's recall
6. Assess the patient's understanding of the condition
7. Most Important first; particularly when giving advice
8. Explore his view & encourage him to ask questions
9. Negotiate management with him; help him to decide which treatment
10. Check the patient's understanding
Communication skills(skills for motivating patient adherence to treatment plans.)
a. Treatment that suits the patient circumstances.
b. A clear rationale for the required behavior change.
c. Example of role models e.g. films showing similar procedures.
d. Motivational feedback i.e.
• +ve reinforcement e. g. praise for committed behavior.
• -ve reinforcement e.g. criticism for uncommitted behavi
Communication skills(Communication skills for special situations e.g.)
a. Special groups of disorders (disabled, mentally retarded, chronic, terminal illness, chronic pain & addictive patients).
b. Special personality problems (non-cooperative, hostile, over dependent)
c. Special clinical situations (giving bad news, dealing with sensitive (sexual) issues, preparing for life threatening diagnostic or treatment procedures)
Communication problems: Poor communication is related to
1- Lack of information:
Many health professionals give only good news (no news is not good news for most patients). This may lead to:
• Uncertainty → Anxiety & depression of patients
• Affect the patient sense of participation, response & cooperation in ttt plan Communication gap: Information is not understood or wrongly understood.
Causes: a. Doctor may use a jargon (technical term)
b. Patient may use some terms not familiar to some doctors
c. Patient may pretend that he understands (not to look stupid/ignorant)
3- Poor recall (remembering) of information given to patient. Categorizing, summarizing & emphasizing important information → - this problem
Communication problems: Poor communication is related to(2.0)
4- Lower empathy: Doctor inability to understand patient feelings, & needs
Empathy facilitates treatment process.
5- Low compliance: Patient doesn't follow physician instructions (medications, appointments, life style) due to poor communication.
Factors associated with low compliance: (eliminated by efficient communication)
a. Perception of the physician as rejecting & unfriendly.
b. Failure of the physician to explain the diagnosis & causes of symptoms.
c. Increased complexity of treatment & instructions.
d. Verbal rather than written instructions.
Coping with physical illness
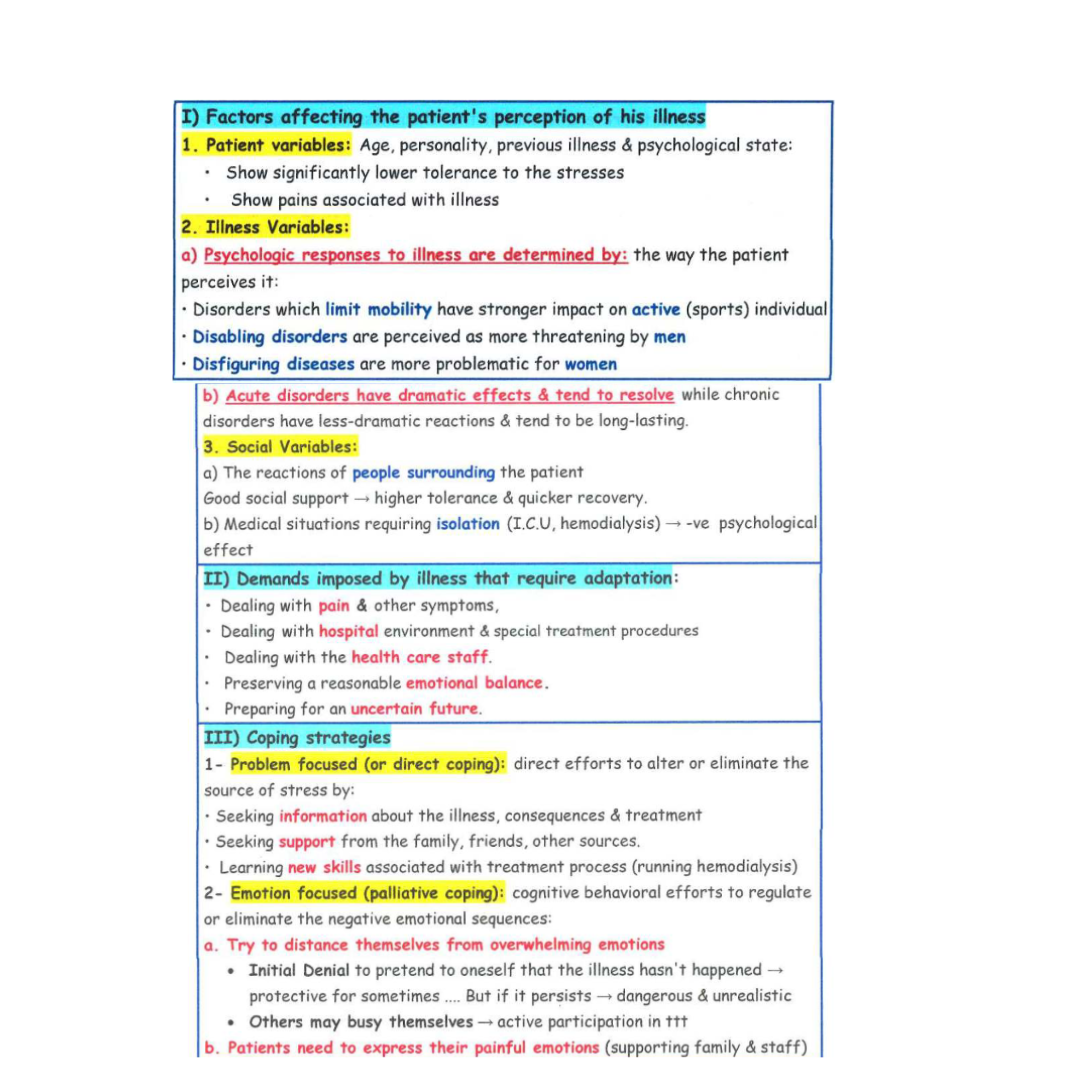
Factors that determinants ability of patients to cape with stressful events
Coping with physical illness (2.0)
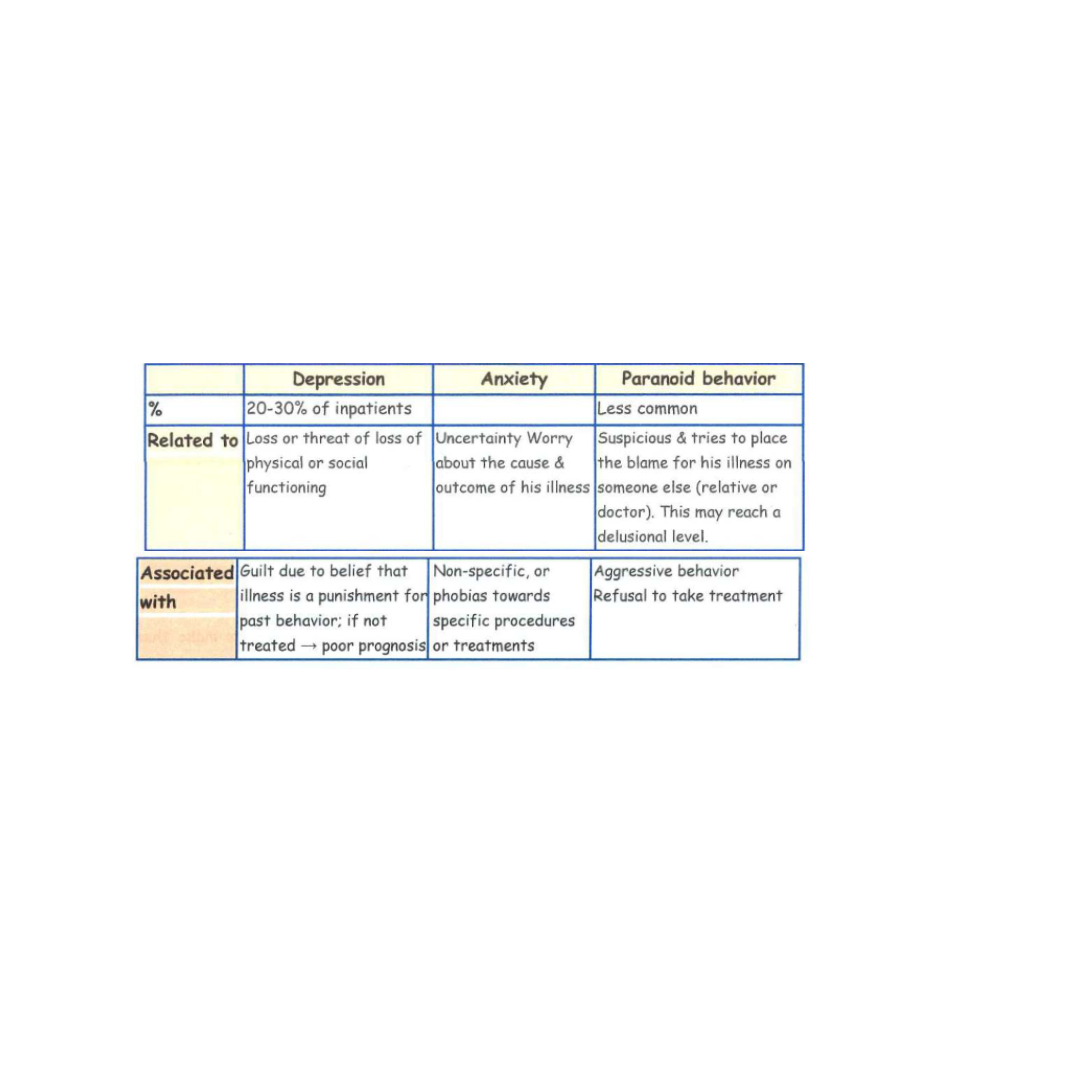
Adverse emotional reactions: Emotions related †o stress of illness take the form of one or a mixture of the following
Coping with terminal illness(Communication with a terminal patient)
There is no simple answer to whether patients should be told or not that they have terminal illness.
• Many patients want to know the truth & cope better with open honest communication. However, open communication with close relatives is better for patient and his family.
• Some patients may not respond well to direct & open communication.
• Finally, the real question shouldn't be shall I tell? But rather how do I tell?
Coping with terminal illness(Psychological responses of dying patients)
It shows wide variations, depends on: personality, situation, expectation & preparation. Coping in dying patient passes through variable & overlapped stages:
* Denial (it cannot be true, there must be a mistake)
* Anger (why me)
* Bargaining (please keep me alive until my daughter marriage)
* Depression (there is no use, it is the end)
* Acceptance (this is my destiny, I had my share in life)
Delivering bad news
Bad news is a relative concept & has a wide range of variability; it should depend on the patient's interpretation of information & reaction to it; examples;
• death of a patient / serious of illness / progressive disease / handicap
• no available bed / misplaced medical notes / cancelled operation
Delivering bad news(What is difficult about breaking bad news?)
• Bad news: loss of well-being, youth, hope, health & relationships → transition mark in life new family roles: perhaps a partner becomes a carer or a widow.
• Patients may fear disfigurement, pain, loneliness & financial ill- being.
• Fear of extreme reactions: → violence, distress & suicidal thoughts.
• Doctors had experience of personal loss → difficult to break bad news & to give support. They feel responsible for inflicting emotional pain on their patients
• Fear of 'doing it wrong' & that their own emotional reactions make them unprofessional / giving incorrect information / being blamed / experiencing
personal failure
• Junior doctor has difficulty to deal openly with patient (has no authority → creates a dilemma).
Some consultants said → patients should not be told they are dying. Agreement on how to deliver bad news should be done with respect to the professional perspective.
Delivering bad news(To whom should bad news be given?)
• Ethical guidelines: tell important information to the patient. No excuses like
"to protect the patient" or "it would hurt the patient to know"
• No simple answer to this question because it depends on many variables.
• Many patients want to know the truth about their condition → better coping.
• Open communication with close relatives → better coping for patient & family.
• Some patients may not respond well to direct & open communication (Individual
& cultural differences)
• Discuss these specific situations with a colleague or multidisciplinary team
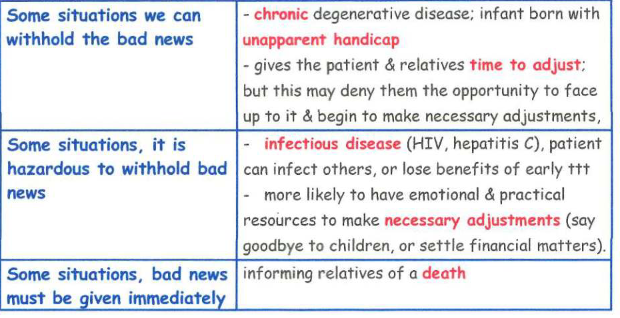
• Withhold bad news: if a patient is psychotic, poor judgment & not understanding
- Confers with the parent or guardian before breaking bad news to a child.
Delivering bad news(When should bed news be given?)(
Should you give hope and reassurance along with bad-news?
• Reassure patients that their fears for the future are probably worse than the reality. Conveying hope → emotional first aid if patients appear isolated & in extreme distress
• Sometimes reassurance is inappropriate → hide fear → come back later on
Psychological aspects of hospitalization
Hospitalization is a major stressful event that affects patients both socially and psychologically.
1 - Changes in social environment:
Patient routine life & daily habits are disrupted; Patient loses much of his privacy.
2- Psychological reactions: stressful psychological changes include:
a. Invasion of privacy
b. Loss of independence & individualism.
c. Reduced opportunities for social contact.
3- Manifestations of distress include:
a. Fear & irritability
b. Unhappiness & loss of interest in the outside world.
c. +*+ need for social reassurance from relatives & professional personnel.
4- Most of distress is related to patient illness, fear & anxiety related to uncertainty, ignorance & expectations about:
a. Nature of illness & its prognosis.
b. Medical procedures (investigations, surgery, stressful therapy)