What is an atheroma?
♡ Degeneration of the walls of the arteries caused by accumulated fatty deposits and scar tissue, leading to restriction of the circulation and a risk of thrombosis
What is an infarction?
♡ Obstruction of the blood supply to an organ or region of tissue, typically by a thrombus or embolus, causing local death of the tissue
How are infarctions formed (in context of lipoproteins)?
♡ Lipoproteins transfer fats around the body, so they are available to be taken up by the cells via receptor mediated endocytosis
♡ The lipids carried by LDLs include cholesterol, phospholipids, and triglycerides
Atherosclerosis and inflammation is complex, what is this inflammation process mediated by?
♡ Mediated by low density lipoprotein (LDL), angiotensin II and various inflammatory substances
Where are some common sites (larger arteries) where Atherosclerosis and inflammation occurs (4)
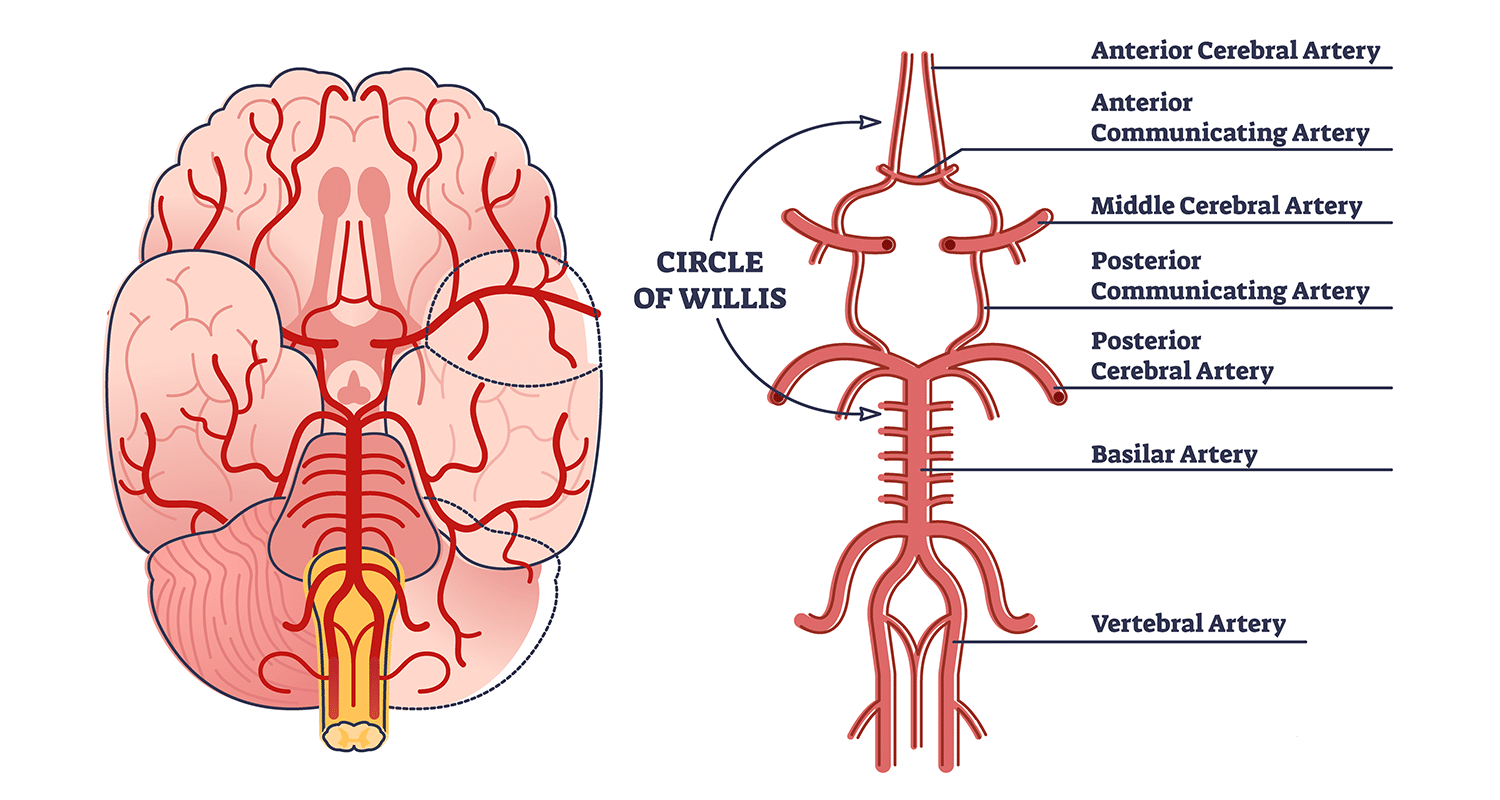
♡ Carotid arteries
♡ Circle of Willis
♡ Coronary arteries
♡ Iliac arteries
♡ Aorta
State how inflammation is initiated (4 steps)

Activation of Endothelial Cells:
Inflammatory triggers activate arterial endothelial cells.
Oxidized LDL particles, stimulated by necrotic cell debris and free radicals, contribute to this activation.
Expression of Inflammatory Signals:
Activated endothelial cells express cytokines and adhesion molecules in response to LDL and inflammation.
Monocyte Adhesion and Migration:
Circulating monocytes bind to the activated endothelium.
These monocytes express adhesion molecules and migrate into the intimal layer.
Differentiation and Mediator Release:
Monocytes differentiate into macrophages within the tissue.
Macrophages release inflammatory mediators, leading to an immune response in the affected area.
State how plaque is formed (3 steps)
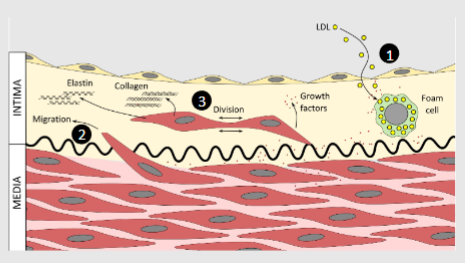
1)
-Macrophages begin to accumulate LDL from the circulation and become foam cells
2)
-Activated foam cells release other growth factors which cause smooth muscle cells to leave the medial layer and cross the internal elastic lamina entering the intima
3)
-The activated smooth muscle cells also release growth factors and may also begin synthesising collagen and elastin in the intima layer
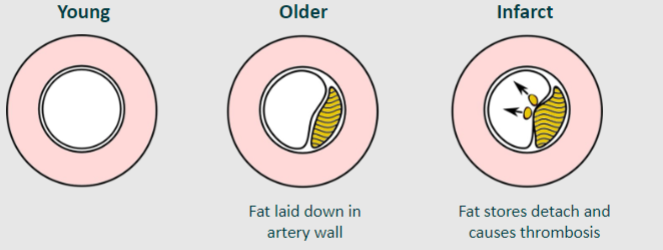
State how the plaque matures (3 steps)
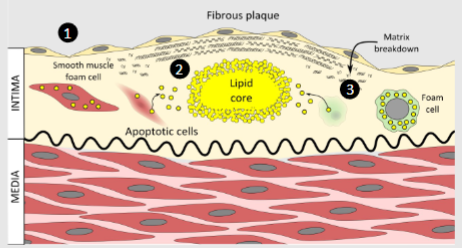
1)
-Smooth muscle cells accumulate LDL becoming a second type of foam cell, but they continue to make extracellular matrix of elastin and collagen which forms a fibrous plaque
2)
-Cells underneath this plaque become oxygen starved they begin to undergo apoptosis and release their fat which forms a globule of fat that is now accumulating in the intima, known as the lipid core
3)
-The dying cells release matrix metalloproteases and other enzymes which can break down the fibrous matrix towards the edge of the plaque leaving a large lipid core covered by a thinner fibrous plaque.
Later in life calcium deposits may form around the......
How can this be visible?
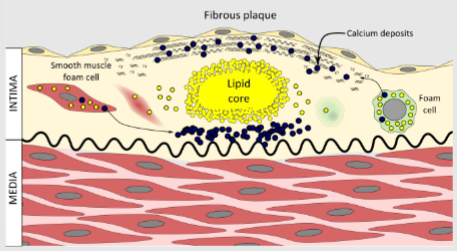
Atheroma
-These are visible on a CT scan
What is the role of calcium deposits?
♡ The role of calcium deposits remains uncertain, there have been arguments that calcification may actually stabilise the plaque
Is calcium a good or bad thing?
♡ Calcium may be a bad thing, but paradoxically a lot of calcium deposits rather than a few could be a slight advantage.
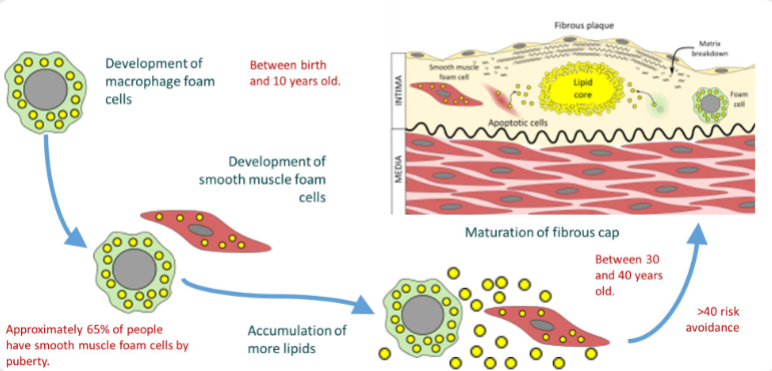
Picture demonstrating how atheroma begins when we are young
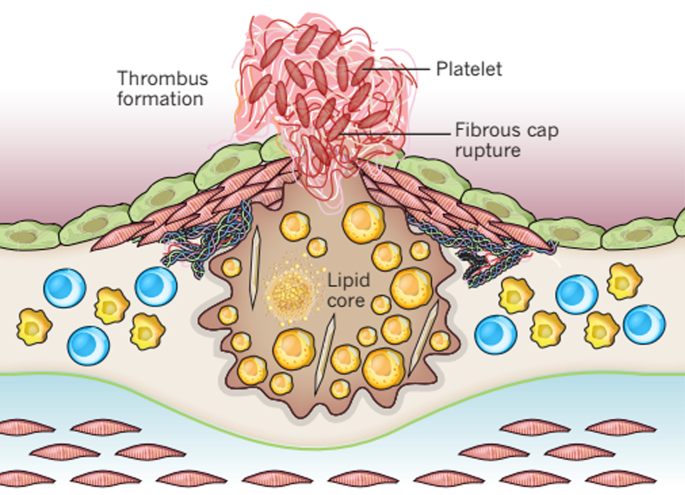
How can a plaque rupture occur?
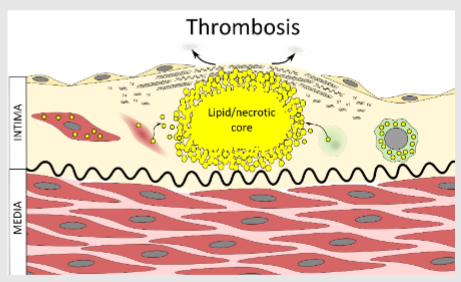
♡ If the central core becomes too large, plaque rupture can occur and the sub-endothelium is exposed. The endothelium is normally an anticoagulant surface
Why is collagen useful in this context?
♡ Collagen forms a very good bases for clotting along with other proteins and factors in the intima
♡ This gives us a procoagulant surface in an artery
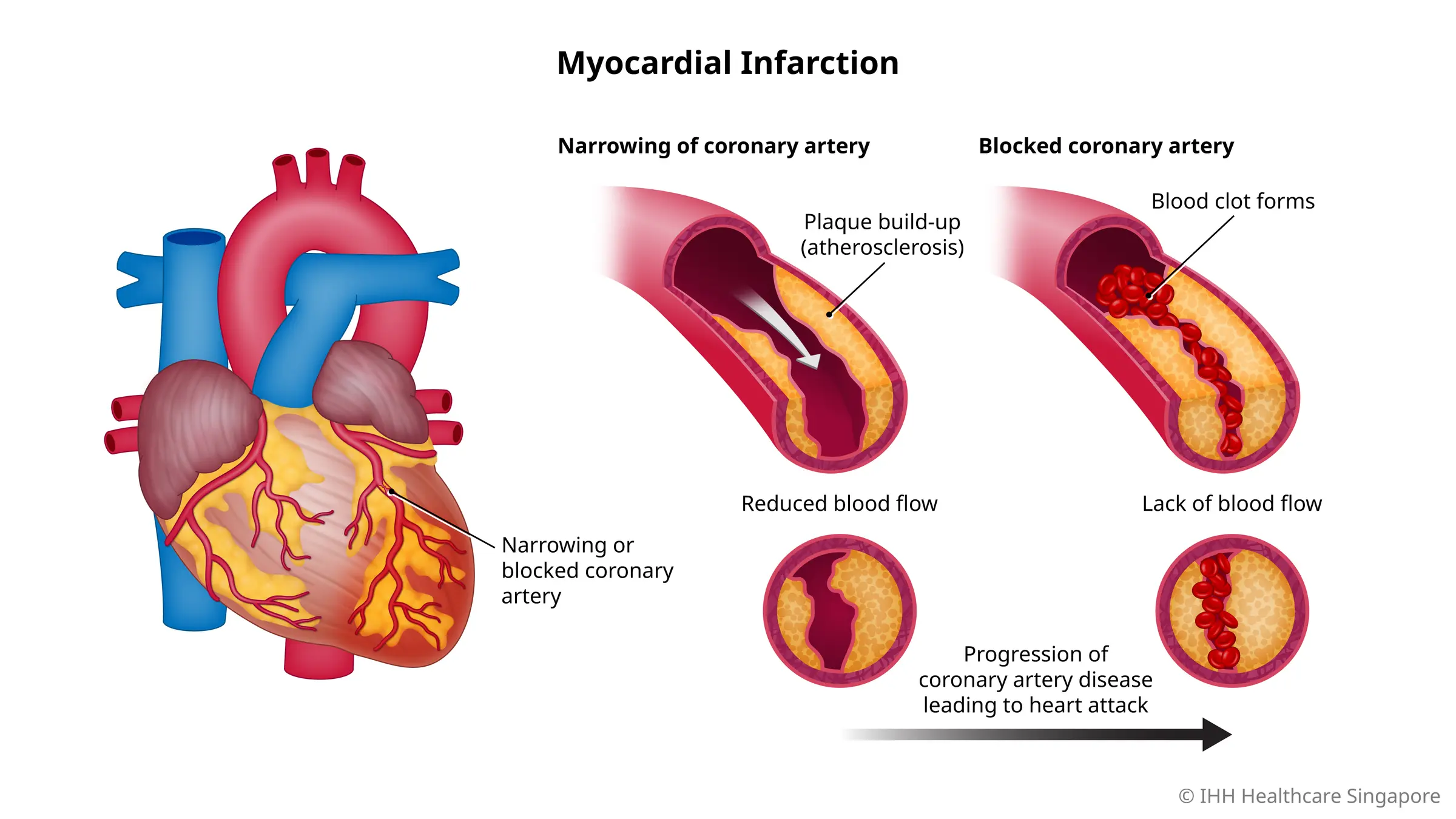
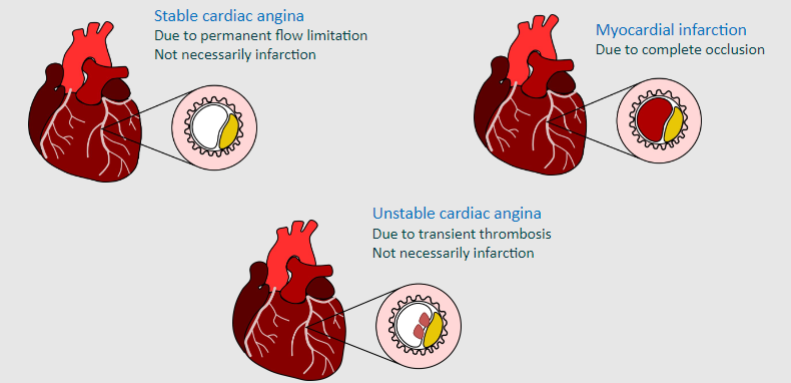
What is occlusive thrombosis?
e.g. Myocardial infarction
-Commonly known as a heart attack, occurs when blood flow decreases or stops to a part of the heart, causing damage to the heart muscle
What is thromboembolism?
e.g. Ischaemic stroke
-In this case obstruction due to an embolus from elsewhere in the body (usually carotid artery) blocking blood supply to part of the brain
-Other types of ischaemic strokes occur
What does 'Aneurysm due to wall thickness' actually mean?
e.g. Aortic aneurysm
-Cause weakness in the wall of the aorta and increase the risk of aortic rupture
-When rupture occurs, massive internal bleeding results and, unless treated immediately, shock and death can occur
State some information about Arterial occlusion?
♡ Particularly cardiac and carotid arteries. Anything downstream from arterial occlusion becomes starved of oxygen
♡ The reduced blood flow can lead to symptoms such as angina on exercise
♡ A thrombus becoming detached can block the cardiac arteries (MI)or cerebral arteries (stroke) and cause death or serious damage very quickly.
State some information about Venous occlusion?
♡ We tend to think of it as happening in the legs, but here an occlusion doesn’t cut off the oxygen supply
♡ It will cause pain and swelling, as hydraulic pressure causes oedema
♡ However, a thrombus may detach and return to the right side of the heart and could enter the pulmonary circulation causing a pulmonary embolism
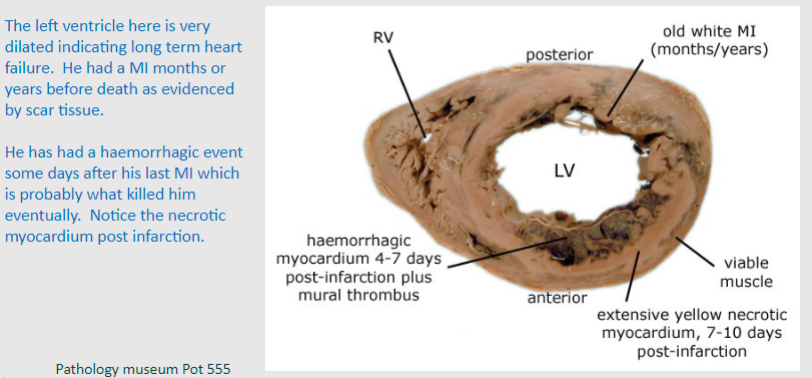
Example of a left ventricle that has experienced Myocardial infraction
What is stable cardiac angina, unstable cardiac angina and myocardial infarction due to?
What are some complications of myocardial infarction?
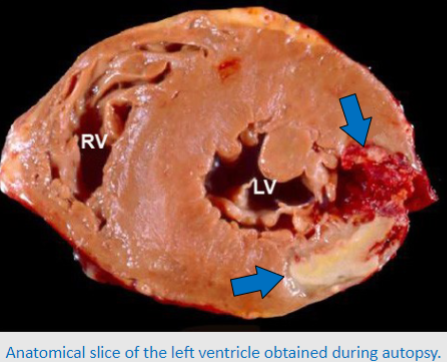
♡ Acute cardiac failure
♡ Conduction problems – arrhythmia
♡ Papillary damage – valve dysfunction
♡ Mural thrombosis - stroke
♡ Wall rupture
♡ Chronic heart failure – myocardial scarring
State some information about Strokes due to thromboembolism (Ischaemic)
♡ Thrombus at carotid plaque rupture travels into smaller cerebral vessels
♡ 85% from carotid atheroma rupture, 15% from stasis in left atrium due to arrhythmia
State some information about Non-thromboembolic stroke (Haemorrhagic)
♡ Due to hypoperfusion, loss of blood pressure (e.g. heartfailure, haemorrhage, shock), or aneurysm rupture andbleeding in the brain