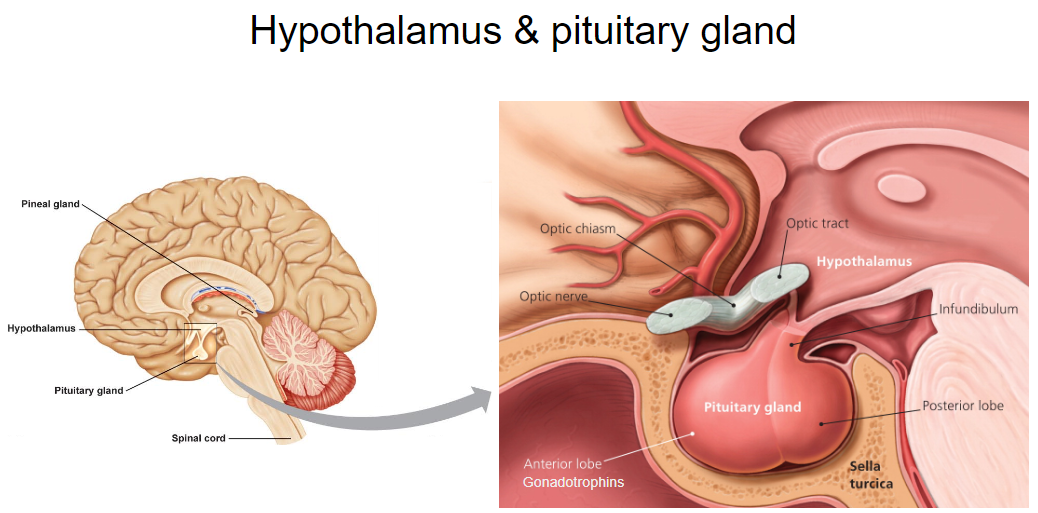
Picture demonstrating the Hypothalamus and the Pituitary gland
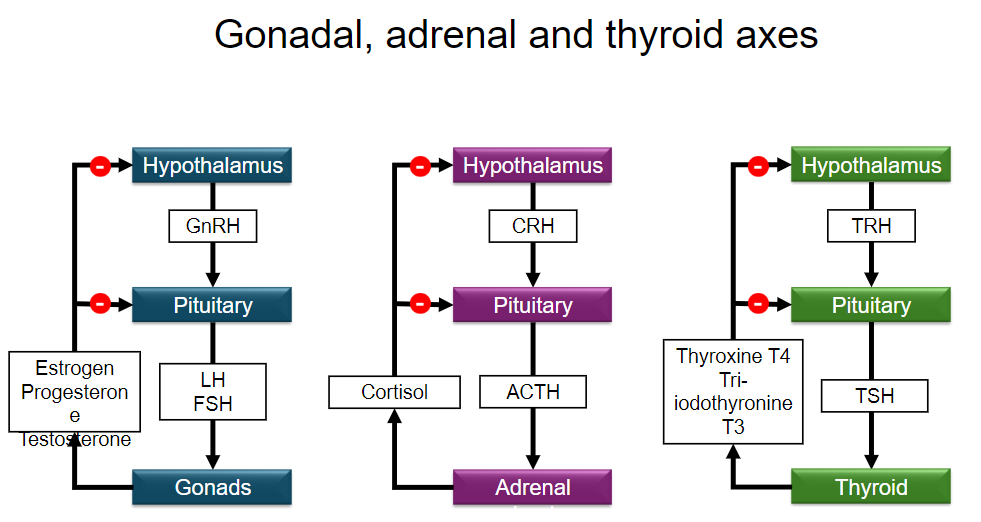
What are the three main hormone types involved in the Hypothalamic-Pituitary-Gonadal Axis? (3)
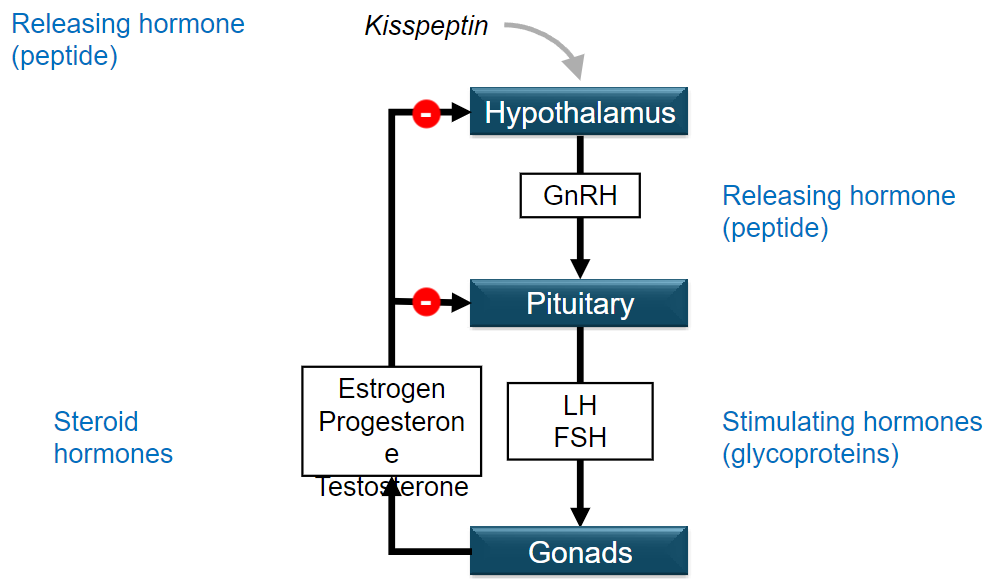
•Releasing hormones (peptides)
•Stimulating hormones (glycoproteins)
•Steroid hormones
What role does Kisspeptin play in the Hypothalamic-Pituitary-Gonadal Axis? (1)
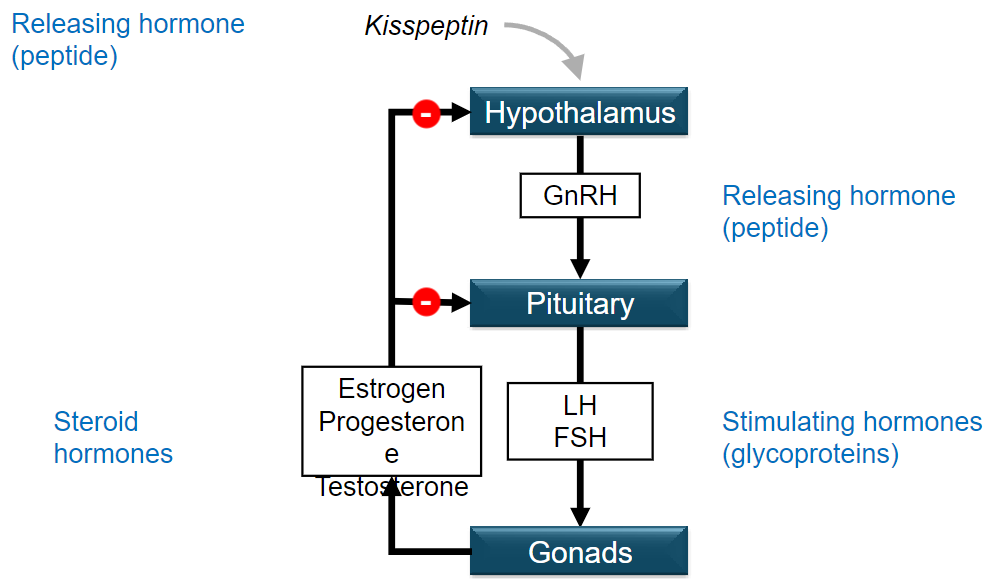
•Stimulates the release of GnRH (Gonadotropin-Releasing Hormone) from the hypothalamus.
Where is GnRH released from, and what does it stimulate? (2)
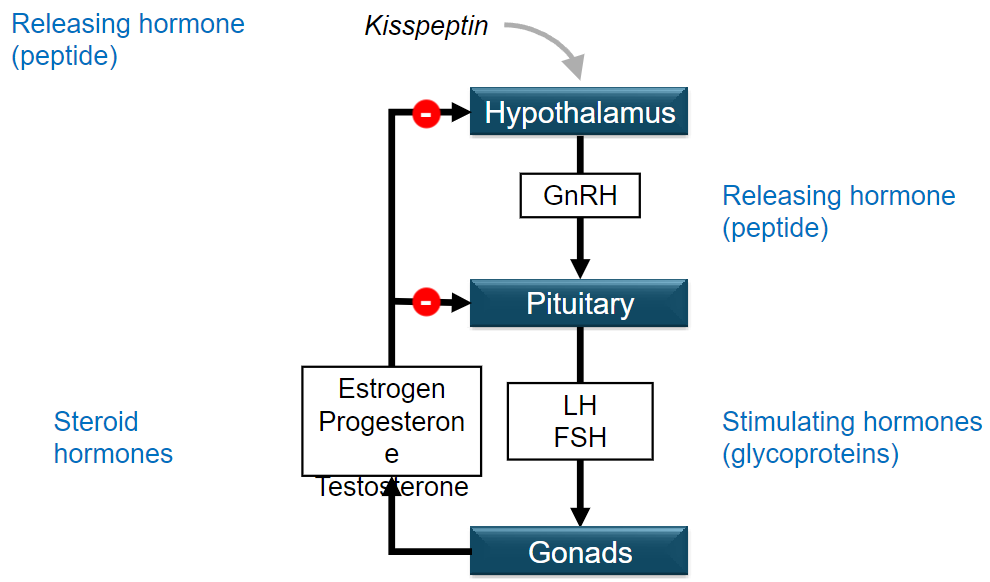
•Released from the hypothalamus.
•Stimulates the pituitary gland to secrete LH and FSH.
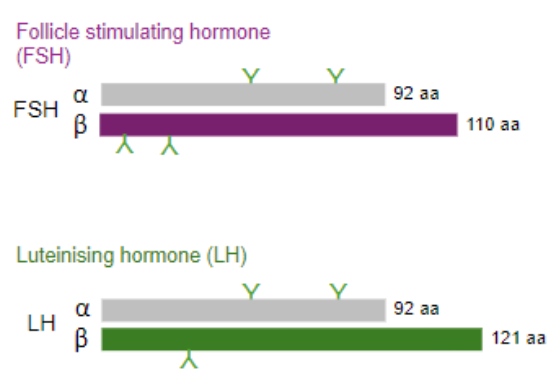
What are the two main hormones secreted by the pituitary gland in this axis, and what type are they? (3)
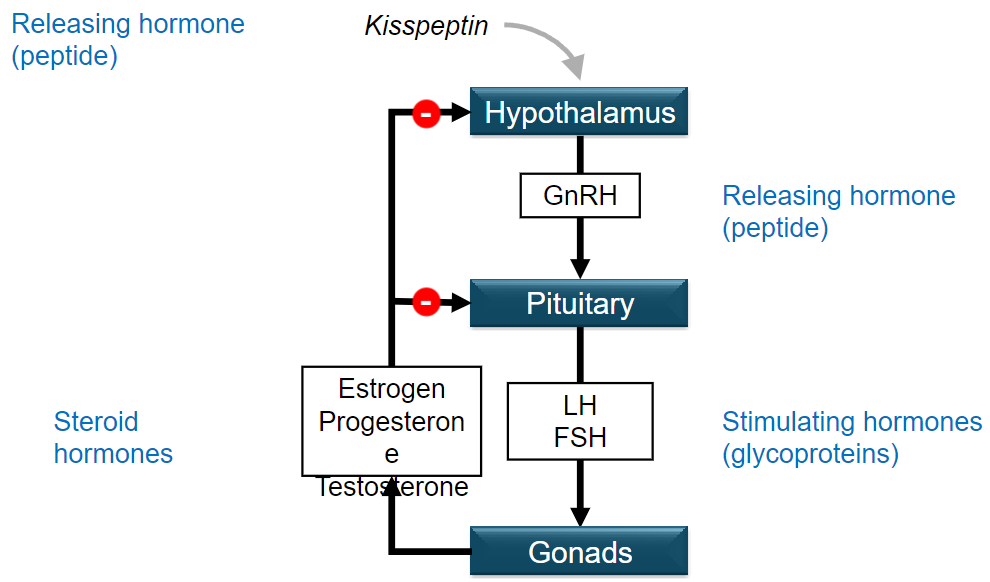
•LH (Luteinizing Hormone)
•FSH (Follicle-Stimulating Hormone)
Both are glycoproteins (stimulating hormones).
Which hormones are produced by the gonads in the Hypothalamic-Pituitary-Gonadal Axis? (3)
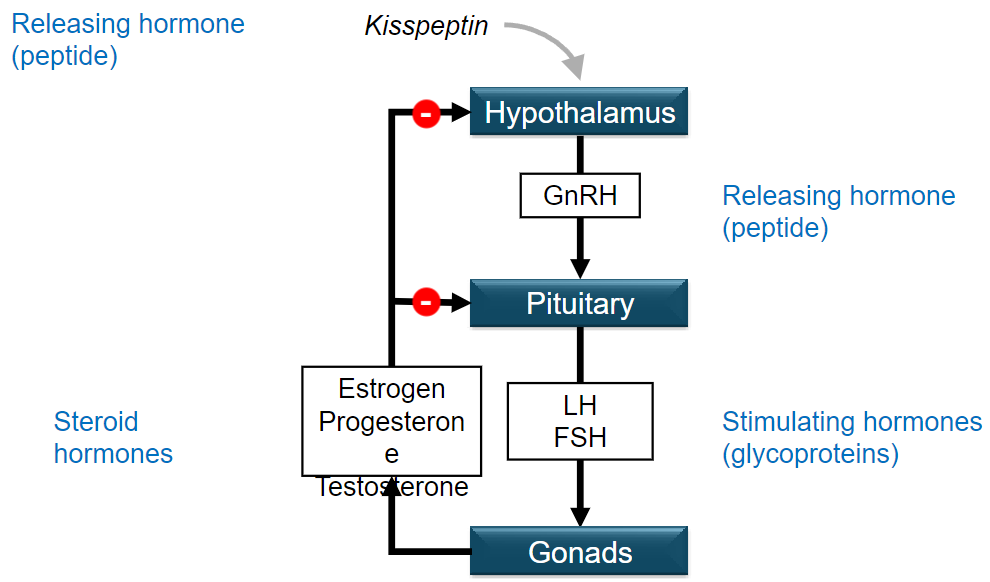
•Estrogen
•Progesterone
•Testosterone
Where was the gene for Kisspeptin first isolated, and when? (2)
•Isolated from a cancer cell around 1996.
•Found in a lab in Hershey, Pennsylvania, home to Hershey's Kisses chocolate factory.
When was Kisspeptin found to play a role in hypogonadotropic hypogonadism? (1)
Around 2003.
What role does Kisspeptin play in the hypothalamic-pituitary axis? (2)
•Involved in regulating the hypothalamic-pituitary axis.
•Plays a role in sexual maturation.
Where are kisspeptin neurons expressed in the hypothalamus? (2)

•Arcuate nucleus (ARC).
•Anteroventral periventricular nucleus (AVPV).
What is the role of kisspeptin neurons in relation to GnRH neurons? (2)
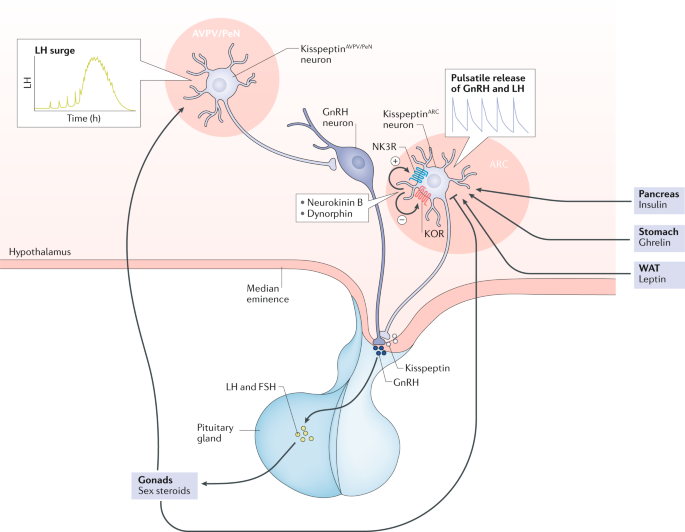
•Kisspeptin neurons project to GnRH neurons.
•They stimulate synthesis and release of GnRH.
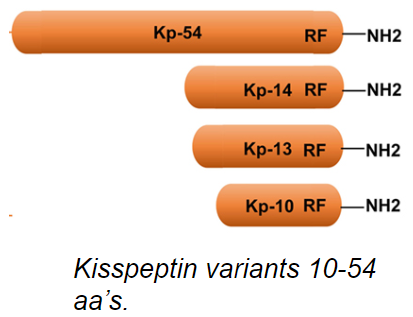
What are the lengths of kisspeptin variants in amino acids (aa)? (1)
Kisspeptin variants are 10-54 amino acids long.
What is the kisspeptin receptor, and where is it expressed? (2)
•GPR54/KISS1R (2 names for the same receptor), a G-protein coupled receptor.
•Expressed on GnRH neurons in the hypothalamus.
What role does the Kisspeptin/KISS1R system play in puberty? (2)
•Involved in triggering the onset of puberty.
•Inactivating mutations can lead to failure to undergo puberty.
What effect can activating mutations of KISS1R have? (1)
Can lead to precocious (early) puberty.
Picture demonstrating the kisspeptin variants 10-54 aa's:
Picture demonstrating the Hypothalamus & pituitary secretion of gonadotrophins
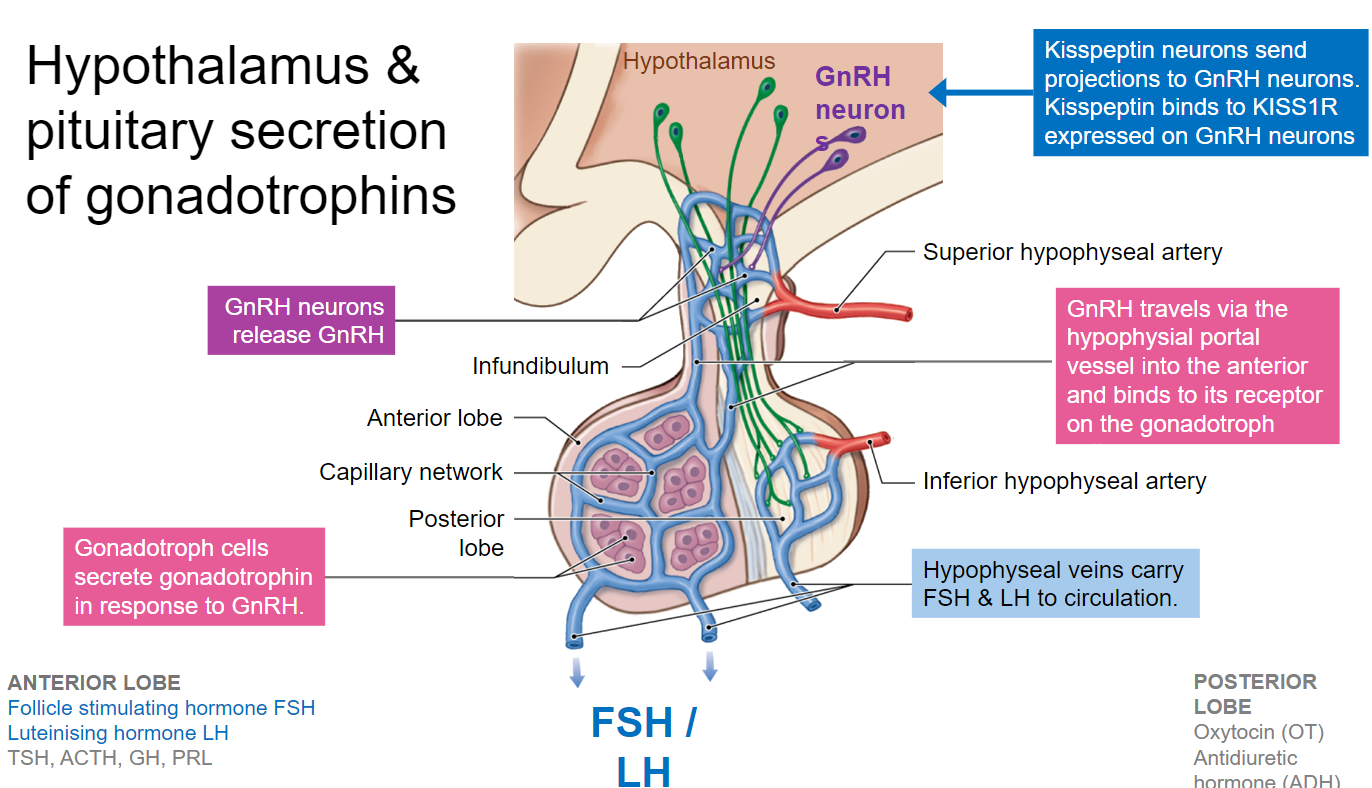
What is Gonadotrophin Releasing Hormone (GnRH), and where is it released from? (3)
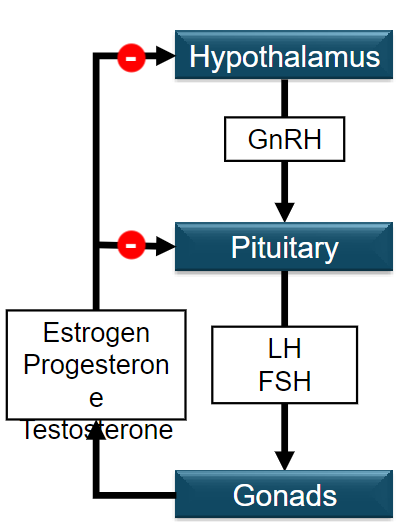
•A 10 amino acid long peptide.
•Released in pulses from the hypothalamus.
•Travels to the pituitary.
What are the gonadotrophin hormones released by the pituitary? (2)
•Follicle Stimulating Hormone (FSH).
•Luteinising Hormone (LH).
These are glycoprotein hormones known collectively as gonadotrophins.
What are the primary sex steroids produced by the gonads in males and females? (2)
•Males: Main sex steroid is testosterone.
•Females: Main sex steroids are estrogen and progesterone.
All three steroids are produced in both sexes.
Why is pulsatile secretion of GnRH important, and what happens if it is continuous? (3)
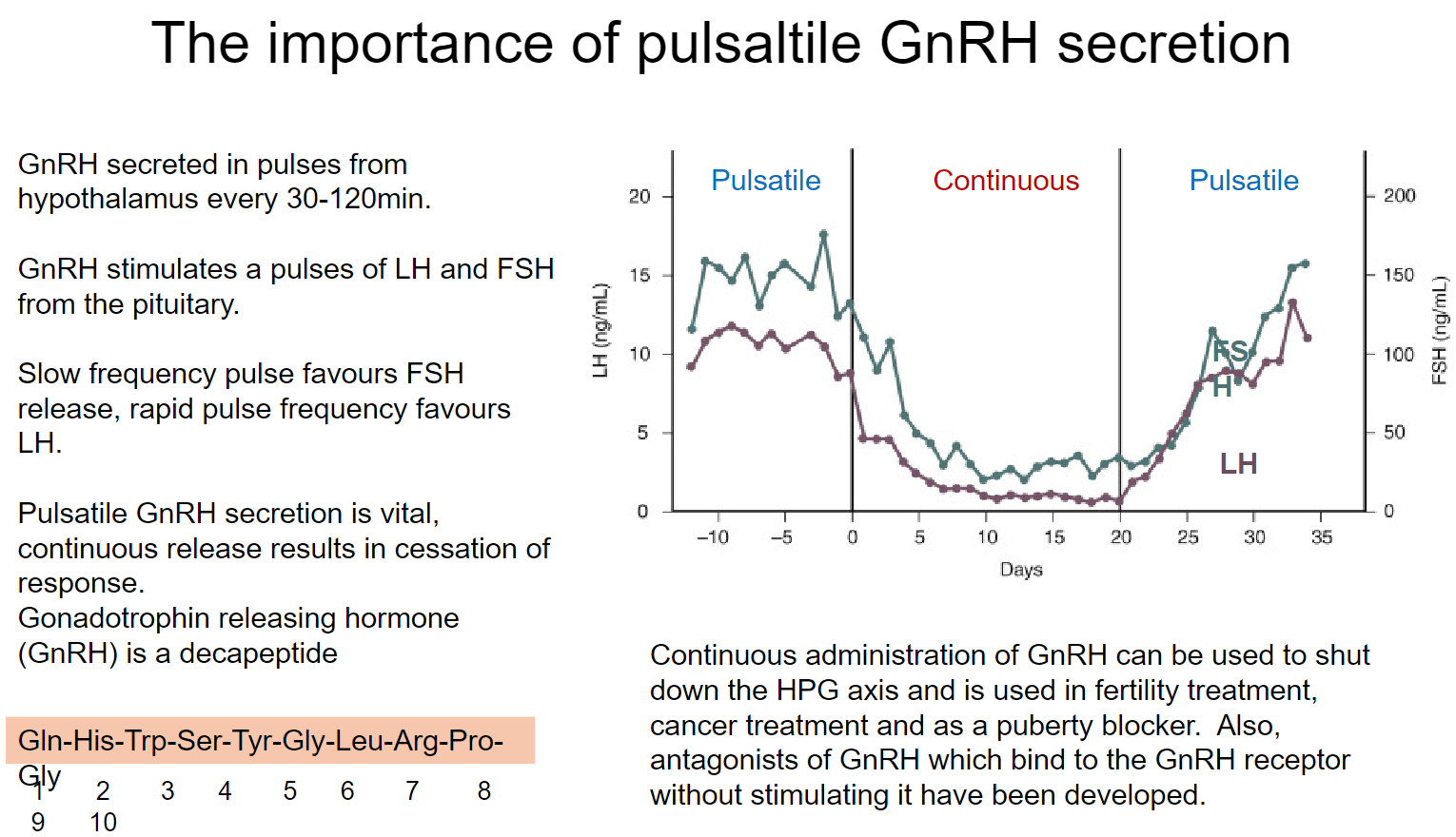
•GnRH secreted in pulses every 30-120 minutes from the hypothalamus.
•Stimulates pulses of LH and FSH from the pituitary.
•Continuous GnRH release leads to cessation of response, shutting down the HPG axis.
How does pulse frequency of GnRH affect hormone release? (2)
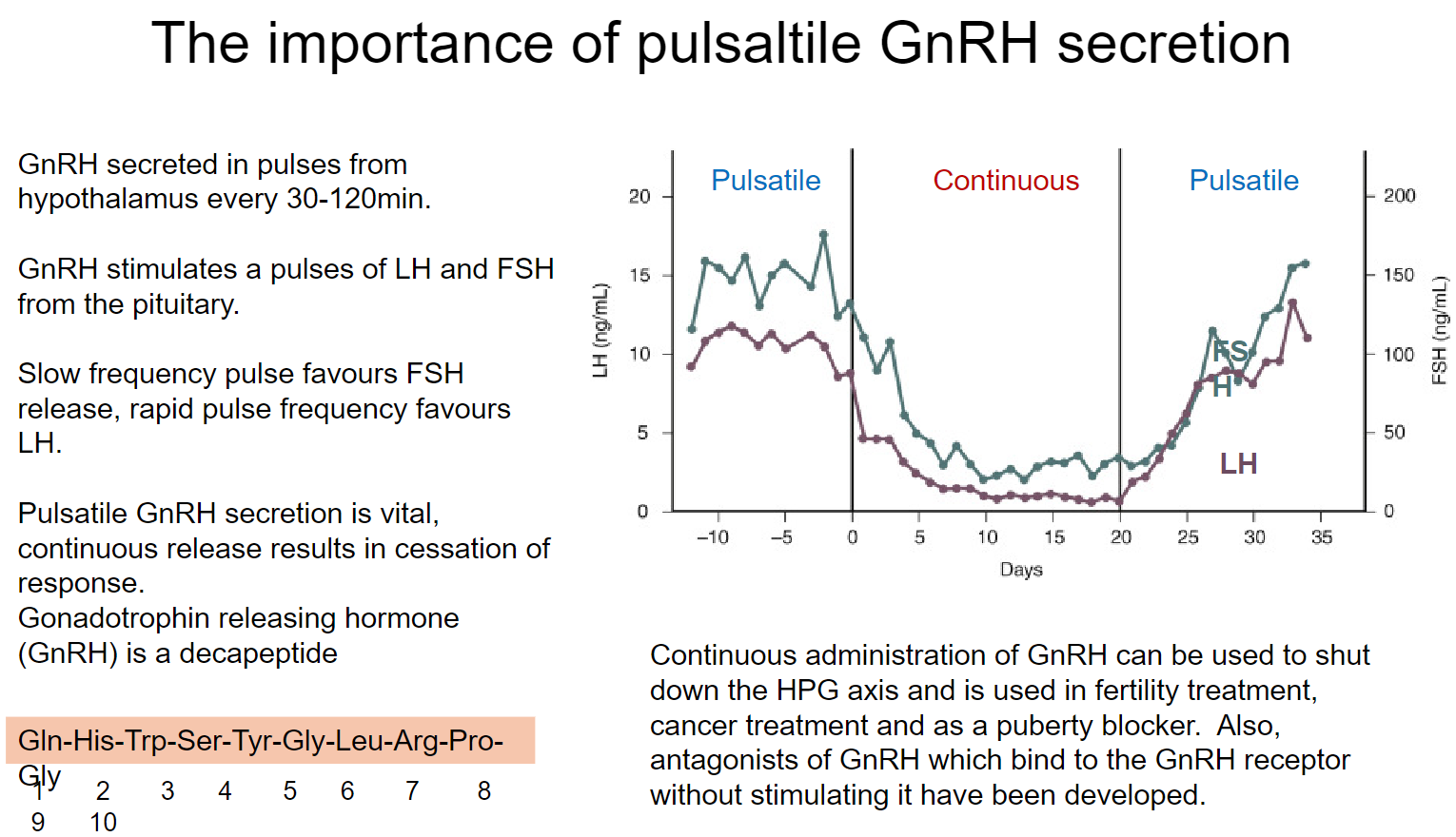
•Slow frequency pulse favours FSH release.
•Rapid pulse frequency favours LH release.
What are some clinical uses of continuous GnRH administration or GnRH antagonists/analogues? (3)
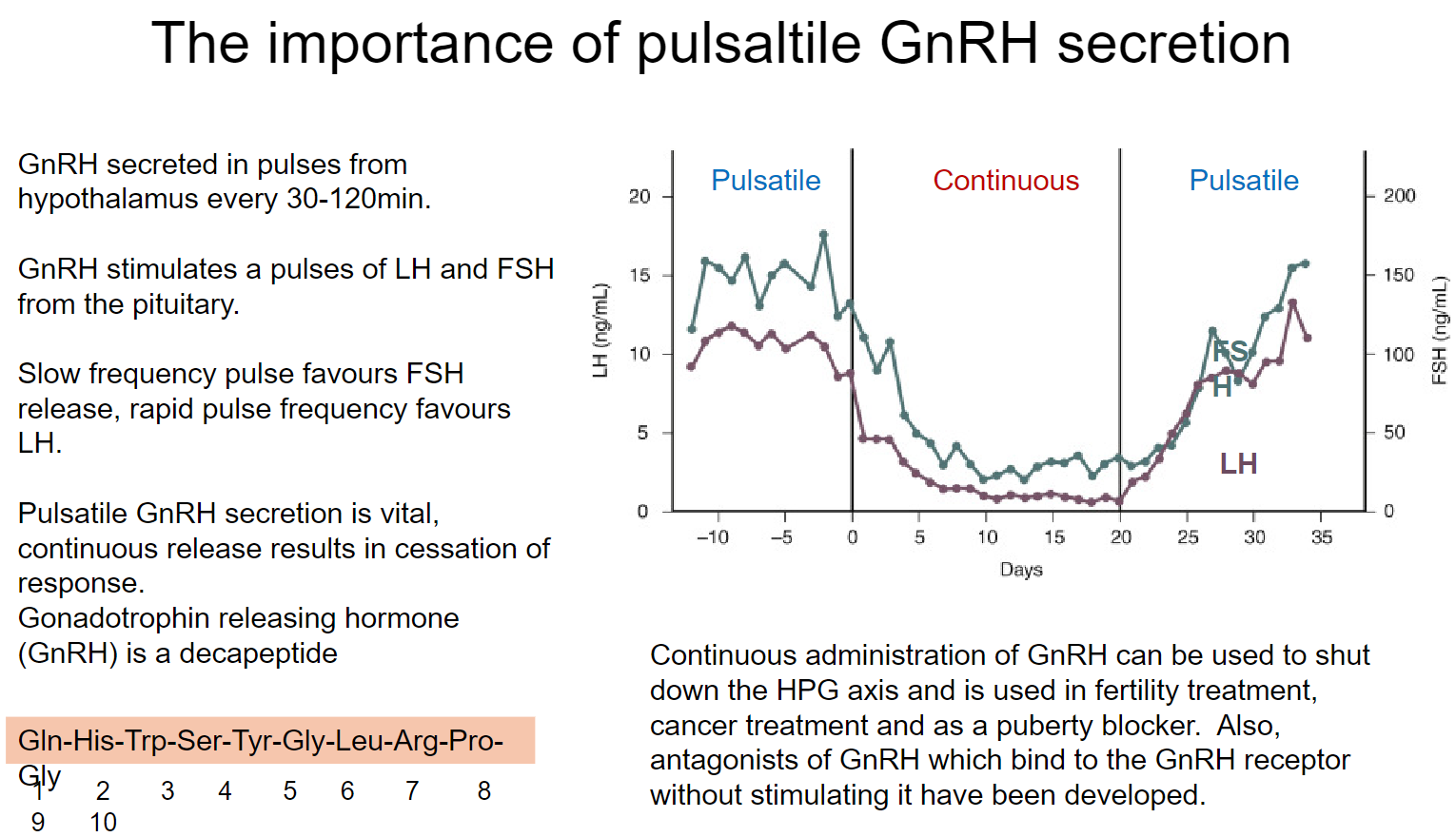
•Used to shut down the HPG axis.
•Applied in fertility and cancer treatments.
•Also used as a puberty blocker.
What is the role of GnRH, and where is it released from? (2)
•Gonadotrophin Releasing Hormone (GnRH) is a 10-amino-acid-long peptide.
•Released in pulses from the hypothalamus and travels to the pituitary.
What are the gonadotrophin hormones released by the pituitary? (2)
•Follicle Stimulating Hormone (FSH).
•Luteinising Hormone (LH).
What are gonadotrophins, and what is their classification? (2)
•FSH and LH are glycoprotein hormones.
•Known collectively as gonadotrophins.
What are the main sex steroids, and which gonads produce them? (3)
•In males, the main sex steroid is Testosterone.
•Estrogen and Progesterone are the primary sex steroids in females.
•All three steroids are produced in both sexes.
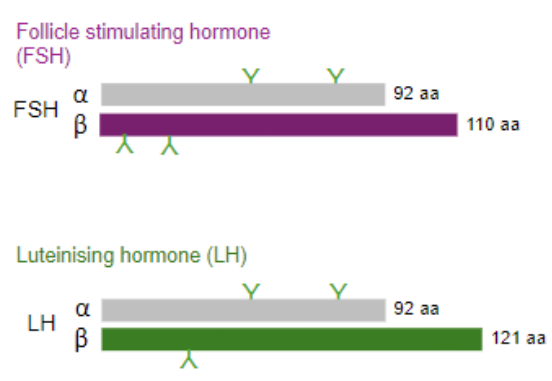
What are gonadotrophin hormones made up of? (2)
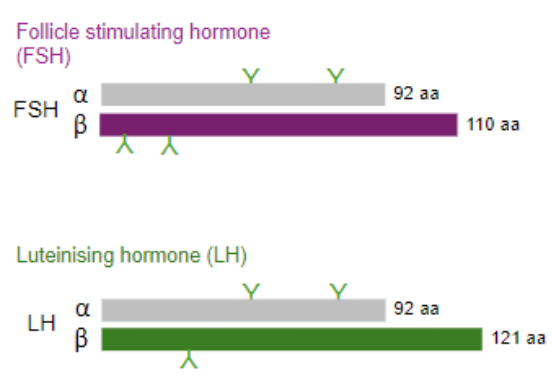
•Heterodimeric peptides.
•Common alpha-subunit and a hormone-specific beta-subunit.
What causes the pulsatile secretion of gonadotrophins, and is it necessary for their biological activity? (2)
Cause: Pulsatile secretion is driven by the pulsatile release of GnRH from the hypothalamus.
Importance: Pulsatile secretion is essential for maintaining normal LH and FSH levels and their biological activity. Continuous GnRH secretion leads to desensitization of GnRH receptors, decreasing FSH and LH secretion.
What are the main pharmacological uses of gonadotrophins? (3)
•To stimulate the gonads.
•Primarily used in cases of infertility or subfertility.
•Commonly used for ovulation induction or in IVF cycles.
What is the role of the hypothalamus in the release of sex steroids? (2
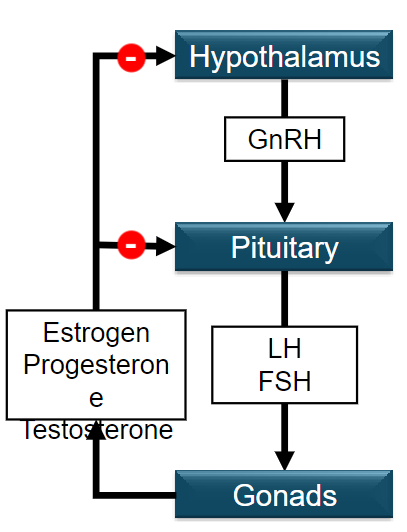
•Hypothalamus releases Gonadotrophin Releasing Hormone (GnRH).
•GnRH is a 10-amino-acid-long peptide, released in pulses to travel to the pituitary.
What hormones are released from the pituitary in response to GnRH? (2)
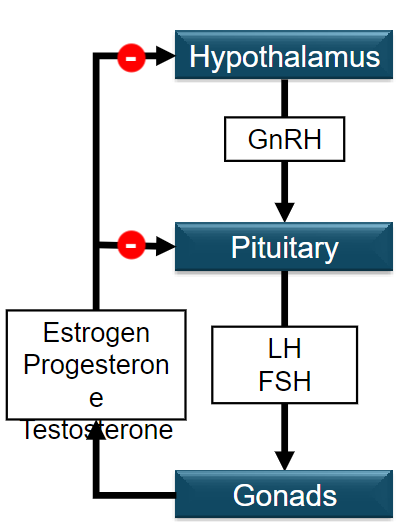
•Follicle Stimulating Hormone (FSH).
•Luteinising Hormone (LH), both collectively known as gonadotrophins.
What are the main sex steroids produced by the gonads in each sex? (3)
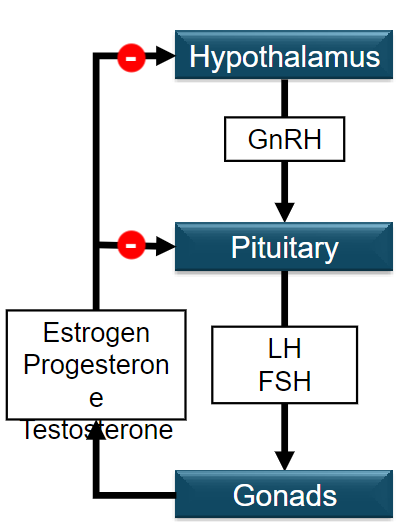
•In males, the main sex steroid is Testosterone.
•In females, the main sex steroids are Estrogen and Progesterone.
•All three steroids are produced in both sexes to some degree.
Picture demonstrating the Gonadal, adrenal and thyroid axes Hypothalamus:
What is puberty, and what are its key features? (3)
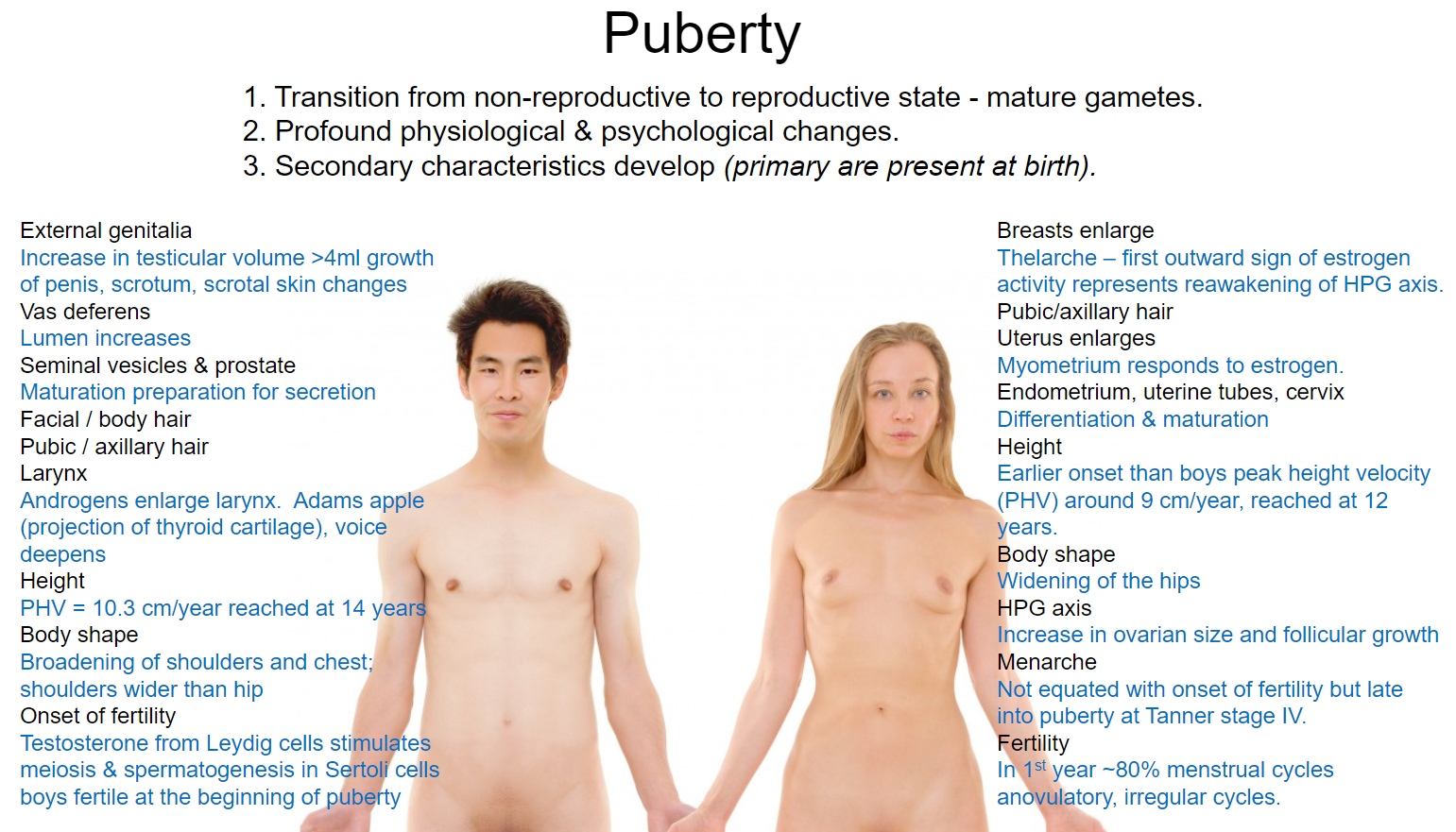
•Transition from non-reproductive to reproductive state, leading to mature gametes.
•Involves profound physiological and psychological changes.
•Development of secondary sexual characteristics (primary characteristics are present at birth).
List the secondary characteristics that develop during puberty in females. (6)
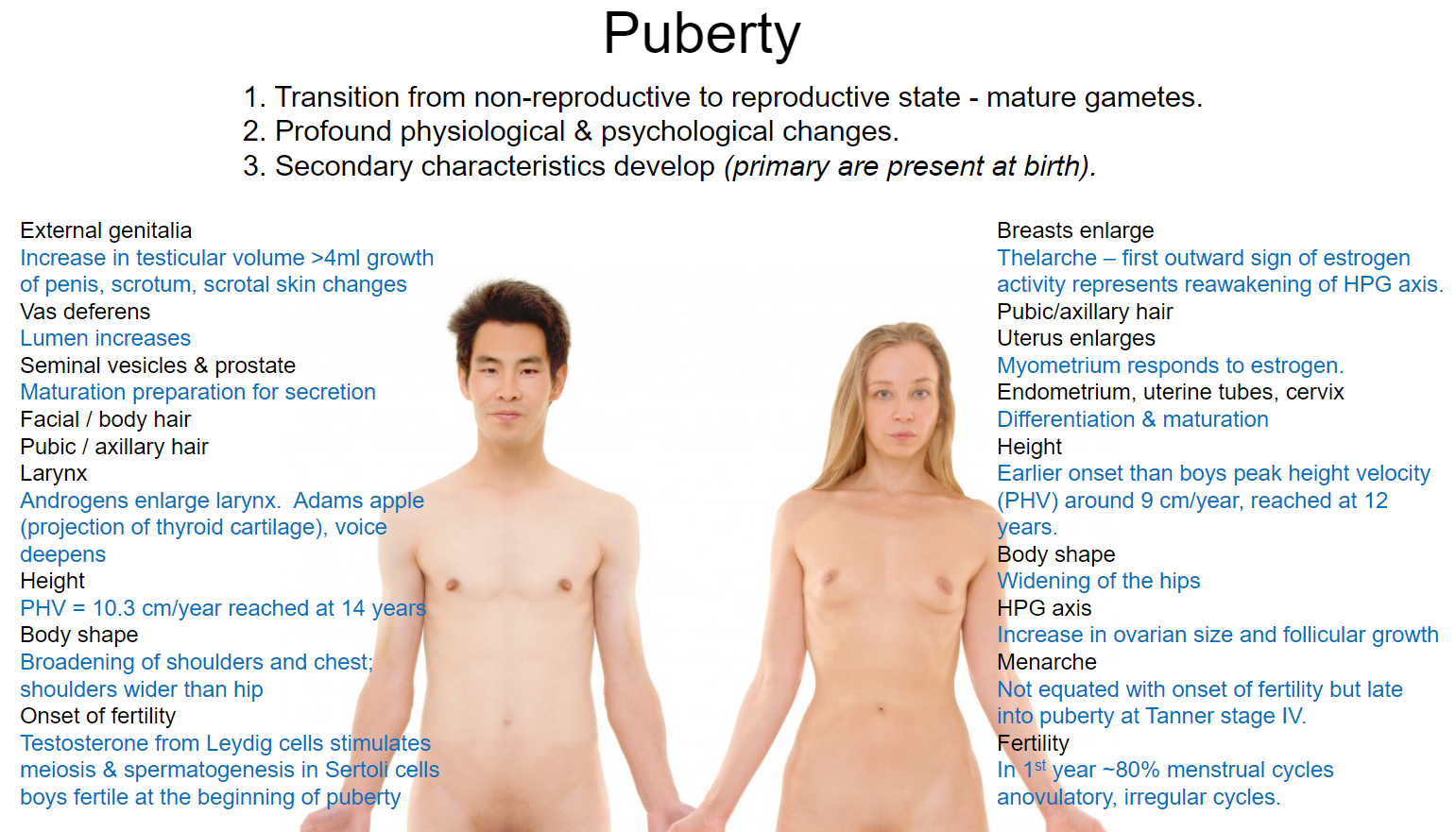
•Breast enlargement: Thelarche is the first outward sign, indicating estrogen activity and reawakening of the HPG axis.
•Pubic/axillary hair growth.
•Uterine enlargement: Myometrium responds to estrogen; endometrium, uterine tubes, and cervix undergo differentiation and maturation.
•Height increase: Earlier onset than boys, with peak height velocity (PHV) around 9 cm/year, reached at age 12.
•Body shape changes: Hips widen.
•Menarche: Occurs in late puberty, typically at Tanner stage IV; initial cycles are often anovulatory.
What are the secondary characteristics that develop during puberty in males? (7)
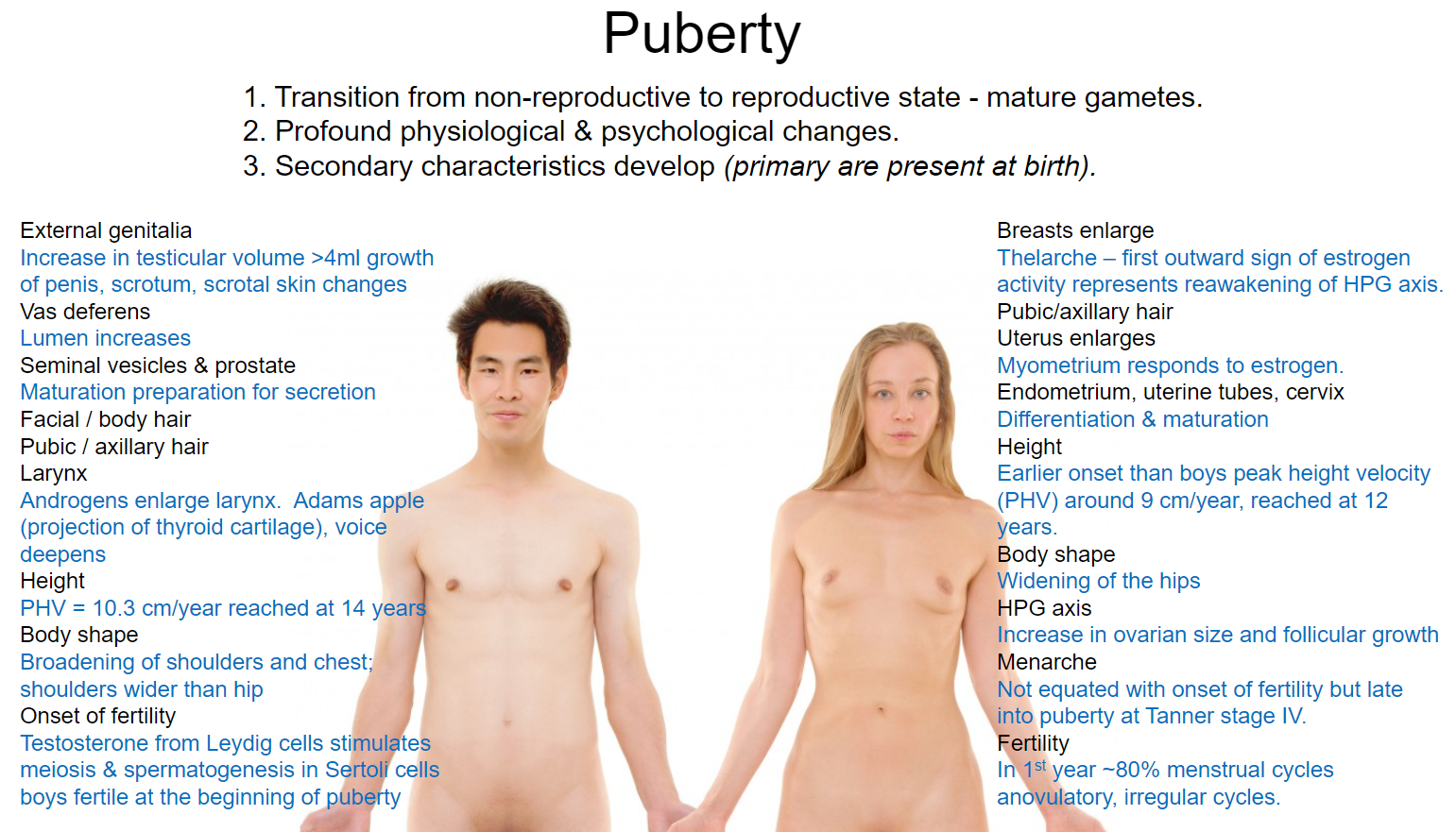
•Increase in testicular volume (>4 ml) and growth of the penis and scrotum; scrotal skin changes.
•Pubic/axillary hair growth and onset of facial/body hair.
•Voice deepening: Androgens enlarge the larynx (Adams apple forms).
•Height increase: PHV of about 10.3 cm/year, reached at age 14.
•Body shape changes: Broadening of shoulders and chest, with shoulders becoming wider than hips.
•Onset of fertility: Testosterone stimulates meiosis and spermatogenesis in Sertoli cells.
•Maturation of the vas deferens, seminal vesicles, and prostate, preparing for secretion.
What are the two endocrine events of puberty? (2)
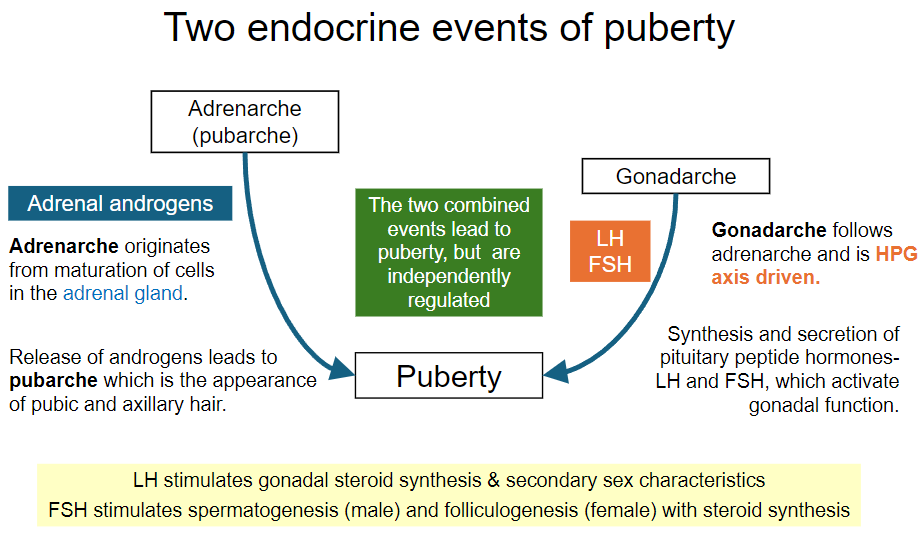
Adrenarche:
•Originates from the maturation of cells in the adrenal gland.
Involves the release of androgens, leading to the appearance of pubic and axillary hair (pubarche).
Gonadarche:
•Follows adrenarche and is driven by the hypothalamic-pituitary-gonadal (HPG) axis.
Involves the synthesis and secretion of pituitary peptide hormones (LH and FSH), which activate gonadal function.
How do adrenarche and gonadarche interact during puberty? (2)
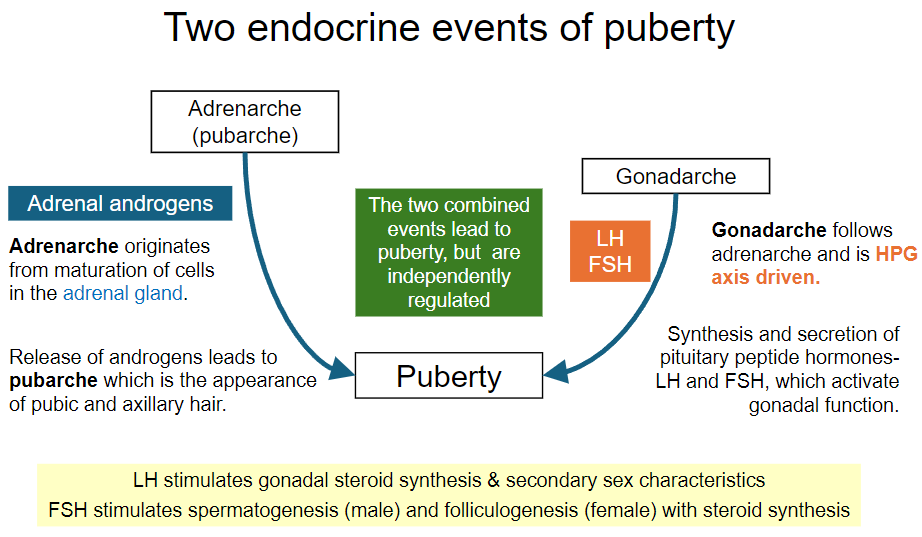
•The two events lead to puberty but are independently regulated.
•Their combined effects contribute to the physiological changes associated with sexual maturation.
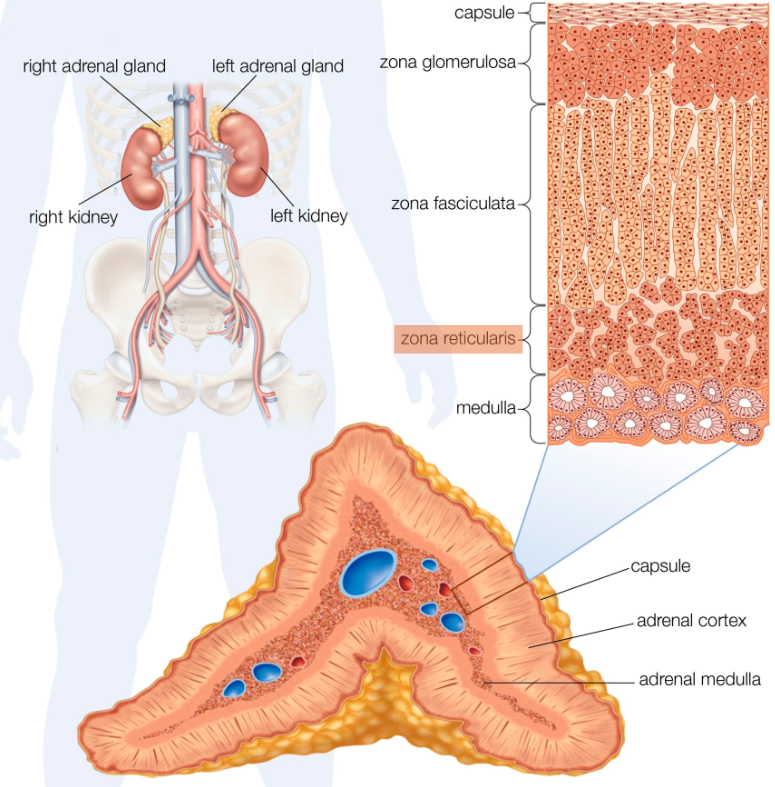
What is adrenarche? (1)
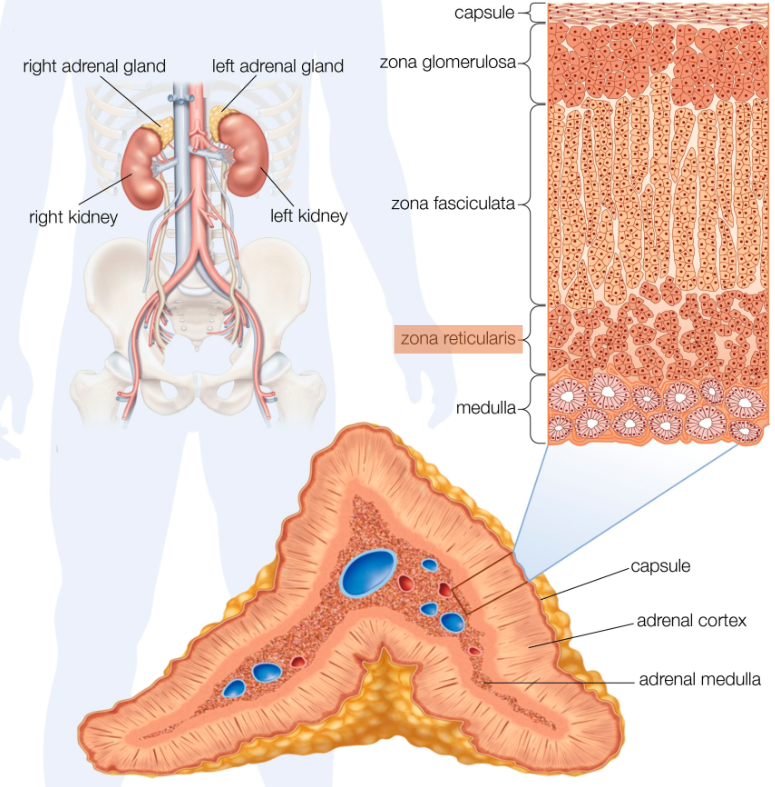
Definition: A marked change in adrenal secretion resulting from the remodeling of the adrenal glands from childhood.
What changes occur in the adrenal glands during adrenarche? (3)
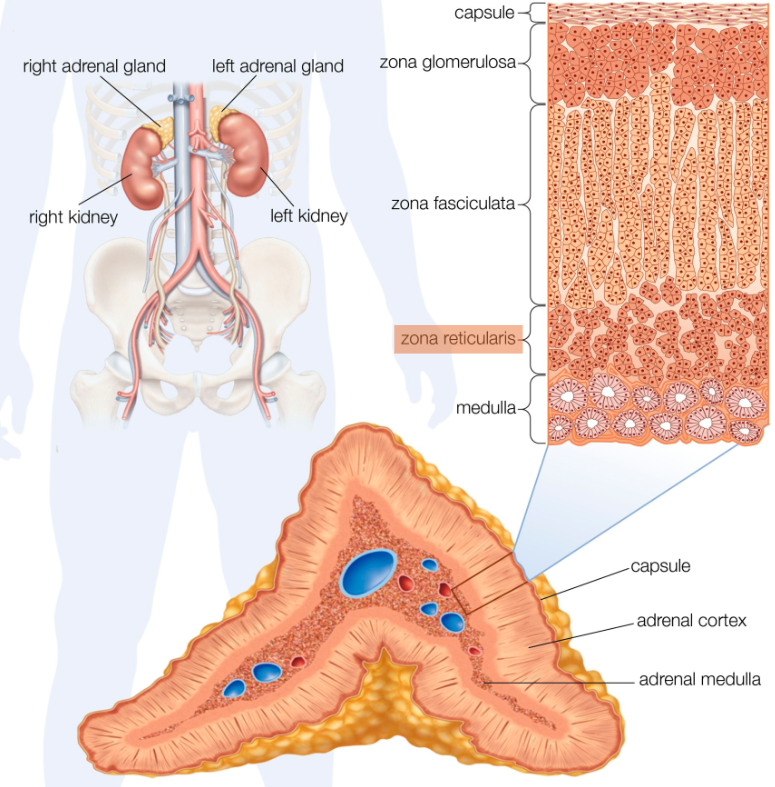
Development of the zona reticularis:
•This zone becomes apparent during adrenarche, transitioning from its undeveloped state in neonates.
Secretion of hormones:
•Increased production of Dehydroepiandrosterone (DHEA) and Dehydroepiandrosterone sulfate (DHEAS).
Timing of hormone secretion:
•Levels of DHEA and DHEAS begin to increase around age 10, peak in the mid-20s, and decline throughout life.
What are the possible causes of adrenarche? (3)
Unknown molecular trigger:
•The precise trigger for adrenarche remains unclear.
Potential hormonal influences:
•Leptin or insulin may be related to body mass and play a role in initiating adrenarche.
Normal remodelling:
•This process may be a part of the natural remodelling of the adrenal glands during growth and development.
What happens to DHEAS during adrenarche? (3)
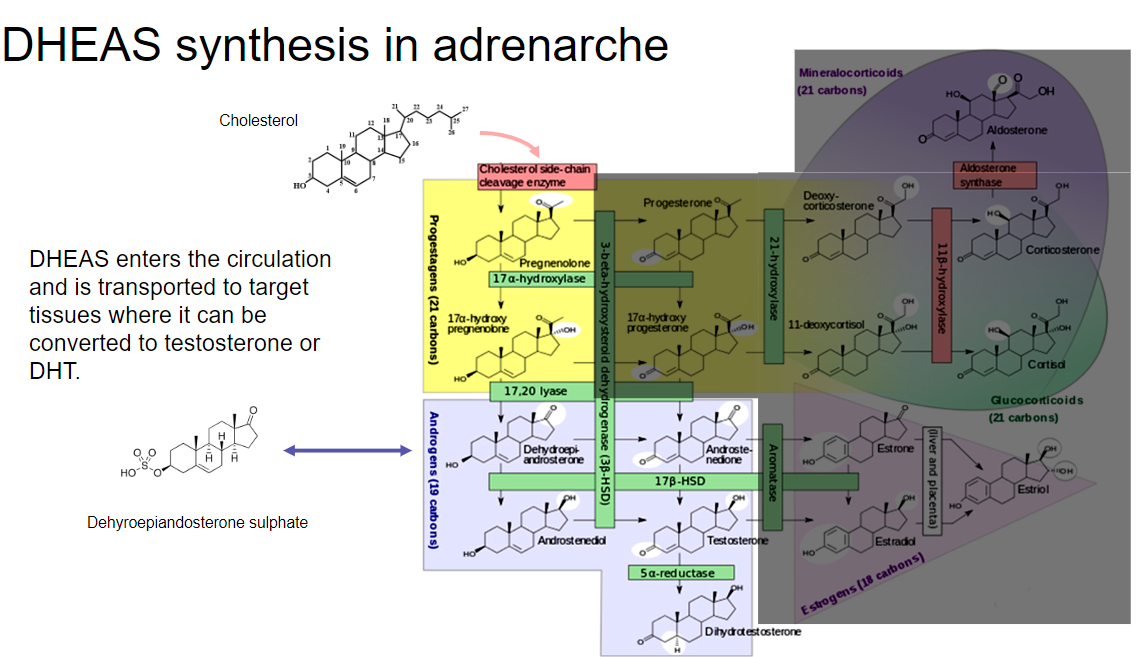
Synthesis and release:
•DHEAS is synthesized in the adrenal glands and enters the circulation.
Transport to target tissues:
•Once in the bloodstream, DHEAS is transported to various target tissues throughout the body.
Conversion to active hormones:
•In target tissues, DHEAS can be converted to testosterone or dihydrotestosterone (DHT), which are key hormones involved in the development of secondary sexual characteristics.
What is pubarche and its significance? (3)
Definition:
•Pubarche refers to the appearance of pubic and axillary hair due to the secretion of adrenal androgens during adrenarche.
Associated conditions:
•It is often associated with acne due to increased sebum production, which can lead to infections and abnormal keratinization of the skin.
Precocious pubarche:
•Pubarche is considered precocious if it occurs before 8 years in girls or 9 years in boys, potentially indicating hormonal imbalances or other underlying conditions.
What are pilosebaceous units (PSUs) and their role in androgen action? (4)
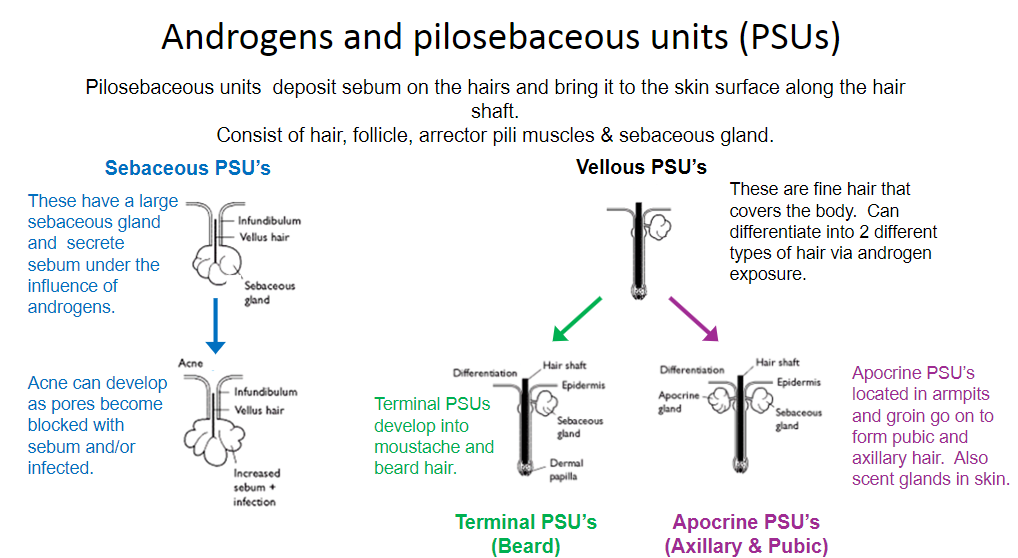
Definition:
•Pilosebaceous units consist of hair, hair follicle, arrector pili muscles, and sebaceous glands. They deposit sebum on hairs, bringing it to the skin surface along the hair shaft.
Vellous PSUs:
•These units contain fine vellous hair that covers the body and can differentiate into two types of hair through exposure to androgens.
Sebaceous PSUs:
•Larger sebaceous glands in these units secrete sebum under the influence of androgens, contributing to skin lubrication.
Acne development:
•Acne can occur when pores become blocked with excess sebum and/or infected, leading to increased sebum production and potential infections in the skin.
What is gonadarche and its significance in puberty? (4)
Definition:
•Gonadarche is the stage in puberty where the hypothalamic-pituitary-gonadal (HPG) axis is reactivated, leading to the maturation of gonads and production of viable gametes.
Activation timeline:
•The HPG axis is first activated at the 16th gestational week, with pulsatile GnRH secretion occurring in the fetus until 1-2 years postnatally.
Pulsatile GnRH secretion:
•After the postnatal period of 10 years or more, GnRH neurons are initially 'restrained' but gradually reactivate at gonadarche, resulting in an increase in pulsatile GnRH release.
Role of Kisspeptin:
•Increased Kisspeptin levels promote the secretion of GnRH, leading to the production of gonadotrophins and stimulating gonadal steroidogenesis, ultimately enabling the formation of viable gametes.
What is Gonadotropin-Releasing Hormone (GnRH) and its role in puberty? (3)
Pulsatile Release:
As puberty progresses, there is an increase in the consistency of pulsatile GnRH release, crucial for stimulating the gonadotropic hormones.
Adult Pulse Frequency:
In adults, the pulse frequency of GnRH occurs throughout the day, influencing the secretion of luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
Measurement Challenges:
GnRH is difficult to measure directly; therefore, LH levels are often used as a surrogate marker to assess GnRH activity and its effects on the reproductive axis.
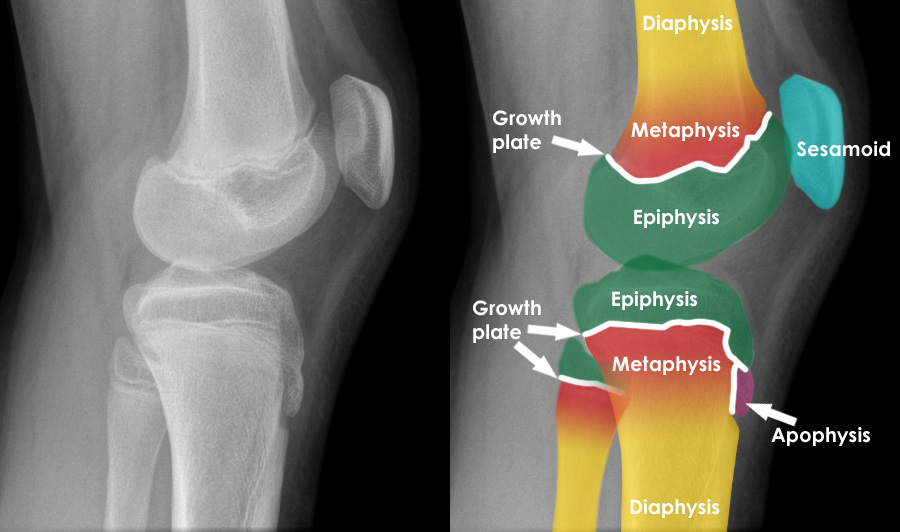
What is epiphyseal fusion and its significance in growth? (3)
Definition:
•Epiphyses are the rounded ends of bones that initially form separately from the main shaft of long bones and gradually fuse with it as a person ages.
Growth Promotion:
•Initially, low estrogen levels during the reawakening of the HPG axis promote linear bone growth, contributing to a rapid growth spurt.
End of Growth:
As estrogen levels increase, they lead to epiphyseal fusion, signaling the cessation of linear growth and finalizing bone length.
What is the growth spurt and its regulating factors? (3)
Definition:
•A growth spurt is a period of rapid physical growth characterized by significant increases in height and weight during puberty.
Regulating Factors:
•The growth spurt involves a complex interaction between growth hormone and estrogen in both boys and girls.
Timing and Effects:
•The growth spurt occurs approximately 2 years earlier in girls than in boys.
Biphasic Effect of Estrogen:
•Low Estrogen Levels: Promote linear growth and bone elongation, contributing to the initial rapid growth spurt.
•High Estrogen Levels: Lead to epiphyseal fusion (at the ends of bones), causing growth to stop.
What stimulates the onset of puberty? (4)
Maturational Event in the CNS:
•The onset of puberty is primarily a maturational event within the central nervous system (CNS), though the exact details of this process are not fully understood.
Genetic Factors:
•There is an inherent genetic component involved, marked by the maturation of 1,000 to 3,000 GRH-synthesizing neurons.
Environmental and Nutritional Influences:
•Improved nutrition over the last century has led to earlier onset of puberty.
•Conditions like anorexia nervosa or malnutrition can delay puberty.
•There is a theory that 17-18% body fat is required to initiate puberty, and 22% body fat is needed to maintain the menstrual cycle, possibly linked to leptin levels.
Kisspeptin:
•The newest theory suggests that mutations in Kisspeptin can either activate or inactivate the initiation of puberty.
What is consonance in the context of puberty? (2)
Definition:
•Consonance refers to a smooth, ordered progression of changes that occur during puberty.
Order of Changes:
•Regardless of how long each pubertal transition takes for an individual, the order in which the changes happen remains consistent across individuals.
What are the psychological changes that occur during puberty? (3)
Increasing Need for Independence:
•Adolescents often seek greater autonomy and decision-making power, distancing themselves from parental control.
Increasing Sexual Awareness/Interest:
•There is a heightened awareness and interest in sexual feelings, relationships, and identity.
Development of Sexual Personality:
•Adolescents begin to form their sexual identity, explore sexual orientation, and establish preferences in relationships.
What is central precocious puberty and its characteristics? (6)
Definition:
•Gonadotrophin-dependent precocious puberty is characterized by early activation of the hypothalamic-pituitary-gonadal (HPG) axis, leading to early onset of secondary sexual characteristics.
Causes:
•Excess GnRH Secretion: Can be idiopathic or secondary to other factors.
•Excess Gonadotrophin Secretion: Often due to a pituitary tumour.
Clinical Features:
•Accelerated linear growth for age.
•Advanced bone age.
•Increased levels of FSH, LH, estradiol, and testosterone.
What are the treatment options for central precocious puberty? (3)
Individualized Assessment:
•Treatment is tailored based on age, psychological benefits, and the wishes and expectations of the patient and caregivers.
GnRH Analogues:
•These can be used to suppress puberty until the child reaches 11-12 years of age if deemed appropriate.
Other Interventions:
•Possible options include surgery, radiotherapy, or chemotherapy depending on the underlying cause.
What is peripheral (pseudo) precocious puberty and its characteristics? (3)
Definition:
•Occurs due to early activation of sex steroid production without the involvement of the HPG axis, leading to loss of the typical progression of pubertal changes.
Causes:
•Testotoxicosis: An activating mutation of the LH receptor causes early androgen production by Leydig or theca cells, without an increase in FSH, thus no spermatogenesis.
•Sex Steroid-Secreting Tumor or Exogenous Steroids: These result in the development of secondary sexual characteristics.
•McCune-Albright Syndrome: Characterized by constitutive activation of adenylyl cyclase, leading to hyperactivity of signaling pathways associated with gonadotrophin hormones.
•Congenital Adrenal Hyperplasia: Causes increased androgen production by the adrenal glands.
What are the implications of peripheral precocious puberty? (3)
Growth Effects:
•Accelerated linear growth due to excess sex steroids can lead to an earlier growth spurt but may result in reduced adult height due to premature epiphyseal fusion.
Sexual Development:
•Early development of secondary sexual characteristics can lead to psychological stress or confusion for the child.
Management:
•Treatment focuses on addressing the underlying cause, which may involve surgical intervention, hormone therapy, or other targeted therapies based on the specific aetiology.
What is pubertal delay (1)
Definition:
•Pubertal delay is defined as the absence of secondary sexual maturation by 14 years in boys or 13 years in girls, or the absence of menarche by 18 years.
Causes of Pubertal Delay (3)
Causes:
Constitutional Delay:
•Accounts for approximately 90% of all cases.
•More common in boys (10x more often).
•Often hereditary with multiple genetic factors.
•May be secondary to chronic illnesses, such as diabetes or cystic fibrosis.
Hypogonadotrophic Hypogonadism:
•Characterized by low LH and FSH levels.
•Conditions include Kallmann's syndrome (impairment of GnRH neurone migration), hypopituitarism, and the effects of high doses or long-term use of opioids or glucocorticoids.
Hypergonadotrophic Hypogonadism:
•High LH and FSH levels due to low sex steroid levels causing low negative feedback.
•Congenital causes include Klinefelter's syndrome (XXY) and Turner’s syndrome (XO), along with viral infections such as mumps.
What are the management strategies for pubertal delay? (3)
Assessment:
•Comprehensive evaluation to determine the underlying cause, including hormonal assays and genetic testing if necessary.
Treatment Options:
•Hormonal therapy may be considered to induce puberty if hypogonadism is confirmed, using testosterone in boys or estrogen/progesterone in girls.
•For constitutional delay, reassurance and monitoring may be sufficient, as most individuals eventually progress to puberty without intervention.
Follow-Up:
•Regular follow-up to monitor growth, development, and psychological health, as well as adjusting treatment plans as needed.