What is folliculogenesis? (4)
Folliculogenesis is the process of follicle maturation in the ovary.
It involves several stages: Primordial → Primary → Secondary → Mature (Graafian) follicles.
During growth, the oocyte (egg) matures while surrounded by follicular cells.
Follicles secrete estrogen as they grow, which is essential for the reproductive cycle.
What are primordial germ cells (PGCs)? (3)
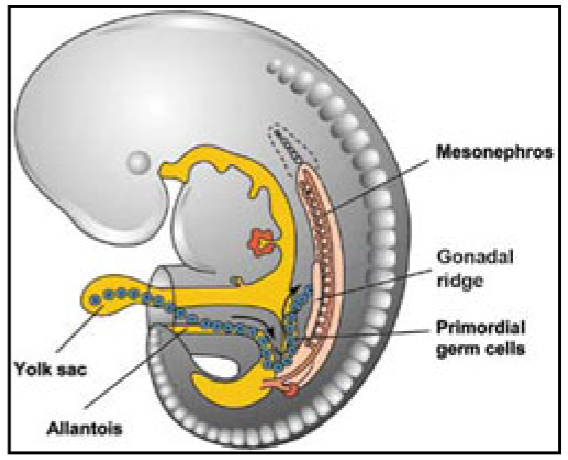
PGCs are the cells that will eventually become eggs (oocytes) in females or sperm in males.
They are first identifiable in the yolk sac of the developing embryo at around 3 weeks after conception.
These cells undergo multiple rounds of mitosis to increase their number.
Where do PGCs migrate after formation? (3)
After their formation in the yolk sac, PGCs migrate to the genital ridge, which will eventually form the gonads.
The genital ridge is located near the developing kidneys.
This migration is essential for the further differentiation of PGCs into mature gametes.
What is the genital ridge, and how does it contribute to gamete formation? (3)
The genital ridge is a precursor structure that forms the gonads (ovaries in females, testes in males).
It begins as an undifferentiated structure in the embryo.
As PGCs arrive, the genital ridge differentiates into either ovaries or testes depending on the genetic sex of the embryo.
How do PGCs become differentiated into male or female gametes? (4)
PGCs migrate to the genital ridge and are exposed to different developmental signals based on genetic sex.
In males, under the influence of SRY gene (Sex-determining Region Y), the genital ridge differentiates into testes.
In females, in the absence of the SRY gene, the genital ridge becomes ovaries.
Males produce sperm in the testes, and females produce oocytes (eggs) in the ovaries.
What must be achieved for reproduction to occur? (7)
Differentiation into male or female: This determines the gametes (sperm or eggs).
Sexual maturation: Puberty triggers the ability to produce viable gametes.
Production, storage, and release of gametes: The body must create, store, and release enough eggs or sperm for fertilization.
Correct chromosome number in gametes: Eggs and sperm must contain half the genetic material (haploid) to form a complete embryo when combined.
Gametes must meet: Sperm must reach the egg for fertilization.
Creation of a new embryo: The combination of genes from both parents results in a unique embryo.
Nurturing of the embryo: The embryo must be supported until it can develop into an independent organism.
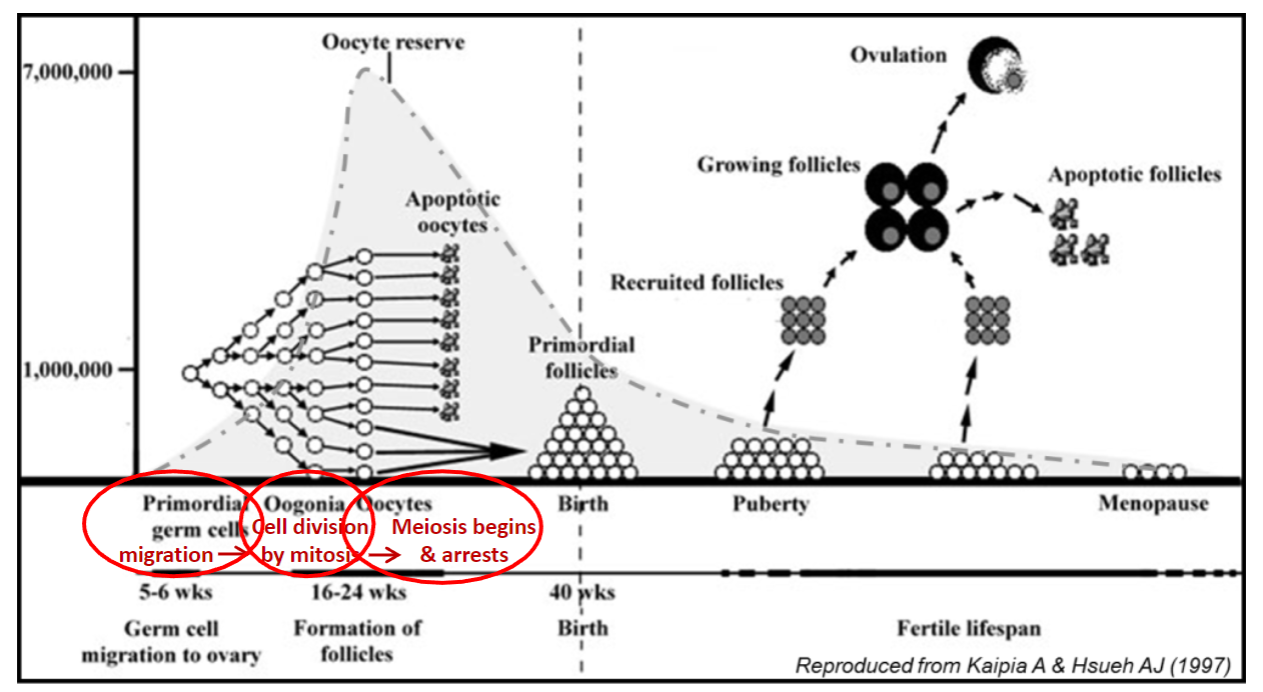
What happens to PGCs when they enter the ovary? (2)
PGCs (primordial germ cells) that enter the ovary differentiate into oogonia.
Oogonia are the precursors to eggs and are diploid cells that multiply by mitosis.
What are oogonia, and how do they develop? (3)
Oogonia are the egg precursors formed in the ovary.
These cells are diploid and undergo multiple mitotic divisions to increase their number.
Once mitosis stops, oogonia enter meiosis and become primary oocytes.
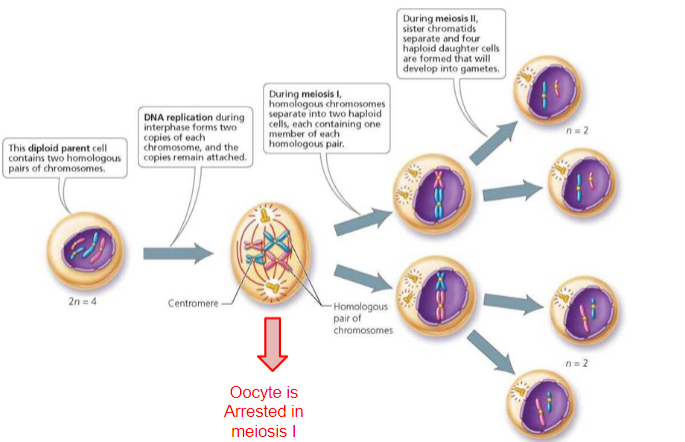
What happens when oogonia enter meiosis? (3)
Once oogonia enter the first stage of meiosis, they are referred to as primary oocytes.
Primary oocytes are arrested in prophase I of meiosis and remain in this stage until ovulation or death.
No further mitotic divisions occur after they enter meiosis.
What is the significance of the mitotic divisions of oogonia? (2)
The mitotic divisions of oogonia are crucial because all the eggs a woman will ever have are produced at this stage.
These divisions increase the number of oogonia before they enter meiosis and become primary oocytes.
How long do primary oocytes remain arrested in meiosis? (2)
Primary oocytes remain arrested in prophase I of meiosis, sometimes for many years (up to 52 years).
They remain in this arrested state until they are either ovulated or undergo degeneration.
Where are primary oocytes located in the ovary? (2)
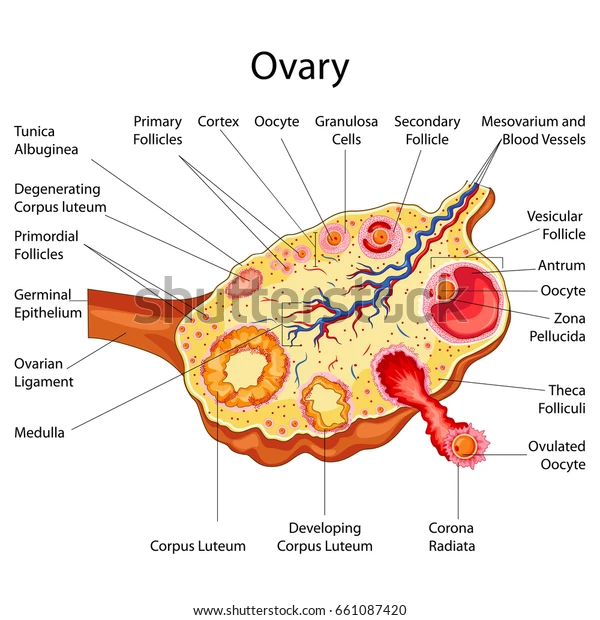
Primary oocytes are located in the outer layer of the ovary, known as the cortex.
This outer region contains the ovarian follicles, each of which houses a primary oocyte.
Why is the primary oocyte considered important? (2)
The primary oocyte is arguably the most important cell in the body, as it is the precursor to all mature eggs (ova) a female will ever have.
It remains in the first meiotic phase for many years, making it vulnerable.
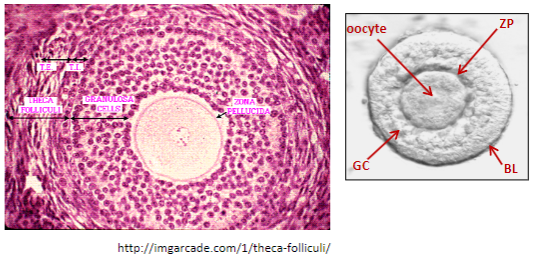
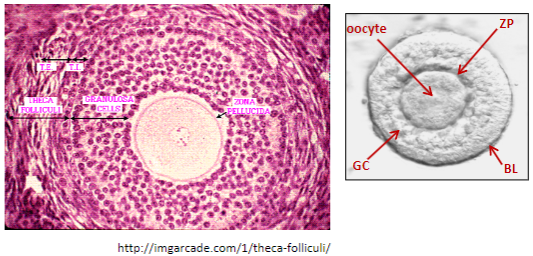
How does the primary oocyte get protection during its arrested phase? (3)
Each primary oocyte becomes surrounded by protective layers and supporting cells.
These cells help protect the oocyte as it remains arrested in meiosis for years.
In the fetal ovary, granulosa cells (GC) differentiate around the oocyte to provide this support.
What happens to the surrounding cells in the fetal ovary? (2)
In the fetal ovary, the granulosa cells (GC) condense around the primary oocyte.
These granulosa cells then differentiate into specialized cells that surround and protect the oocyte.
What is the basal lamina (BL), and what is its role? (2)
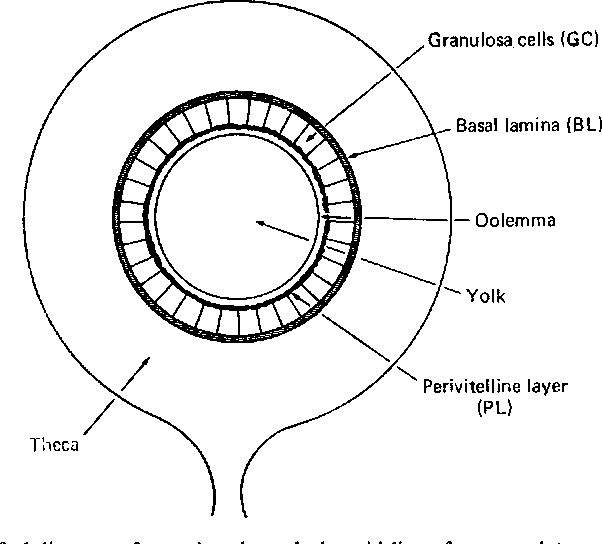
The granulosa cells secrete an acellular layer called the basal lamina (BL).
The basal lamina provides additional structure and protection to the oocyte.
What is a primordial follicle? (2)
The structure formed by the primary oocyte surrounded by granulosa cells and the basal lamina is called a primordial follicle.
This is the earliest stage of follicle development in the ovary.
When do chromosomes replicate during the cell cycle? (1)
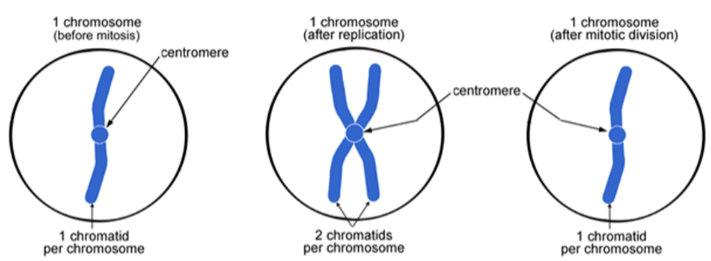
Chromosomes replicate during the S-phase of the cell cycle.
How are chromatids formed after chromosome replication? (2)
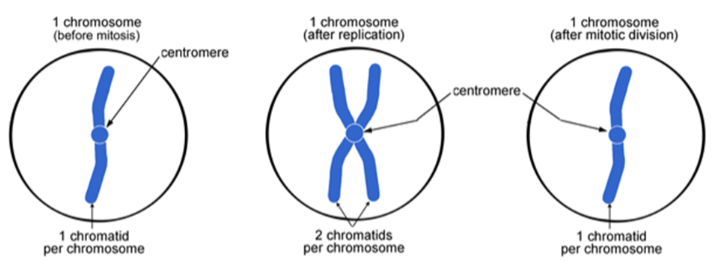
After chromosome replication, the two copies remain attached at the centromere.
Each copy is called a chromatid, and the two copies are identical to each other, known as sister chromatids.
What are sister chromatids? (1)
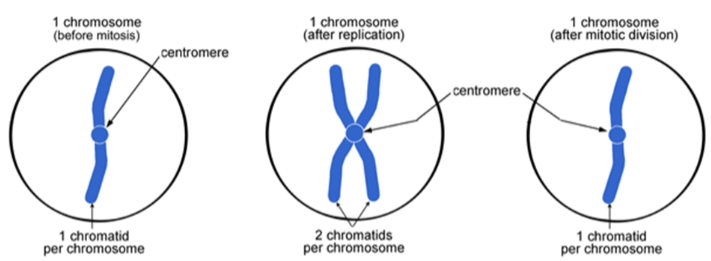
Sister chromatids are the two identical copies of a chromosome, formed after replication.
What is the relationship between the original chromosome and the chromatids? (1)
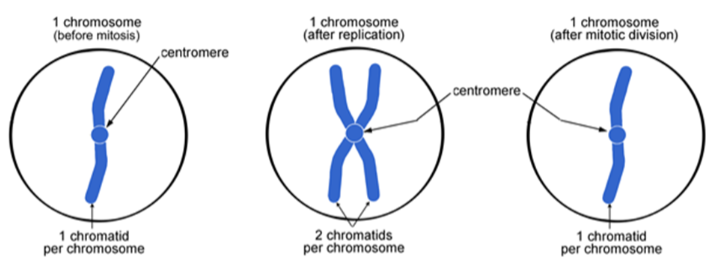
The chromatids are an exact copy of the original chromosomes.
What are the 4 stages of Mitosis? (4)
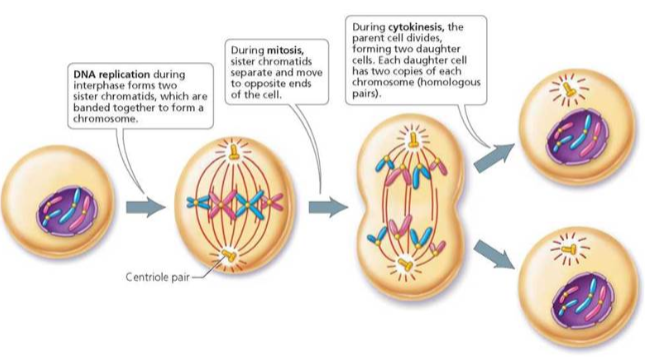
Prophase
Metaphase
Anaphase
Telophase
Picture demonstrating an overview of meiosis:
What is the significance of unequal division of cytoplasm during cytokinesis in folliculogenesis and oogenesis? (1)
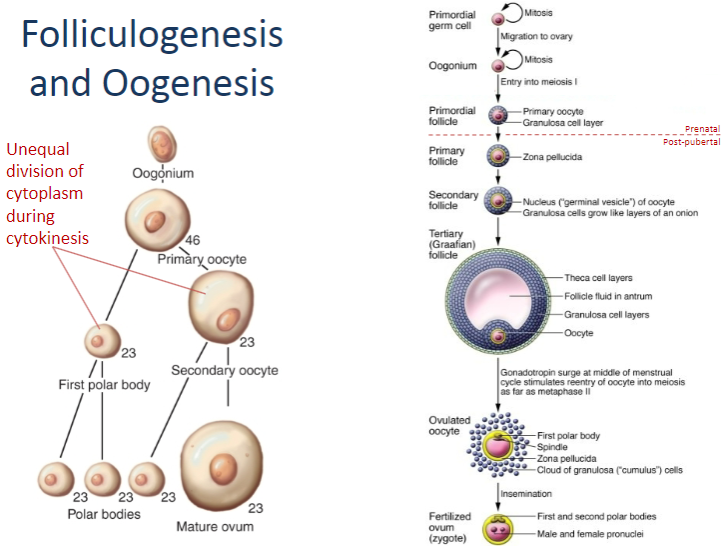
The unequal division of cytoplasm during cytokinesis leads to the formation of a larger oocyte and smaller polar bodies. This ensures that the oocyte has enough resources (like nutrients) to support the developing embryo if fertilization occurs.
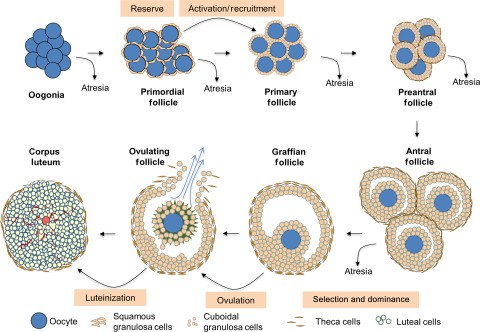
What is folliculogenesis? (1)
The growth and development of follicles from their earliest "resting" stages in the fetus to ovulation.
What happens to the majority of follicles in the ovary after puberty? (1)
Most follicles in the ovary are not growing. After puberty, a cohort of follicles initiates growth each day.
What occurs as the follicles start to grow? (2)
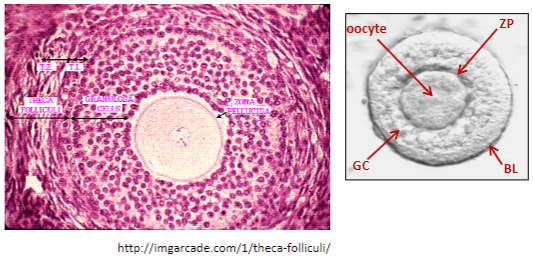
Granulosa cells (GC) multiply.
The oocyte secretes another protective acellular layer called the zona pellucida (ZP).
What is the second layer of cells that forms around the basal lamina (BL) during folliculogenesis? (1)
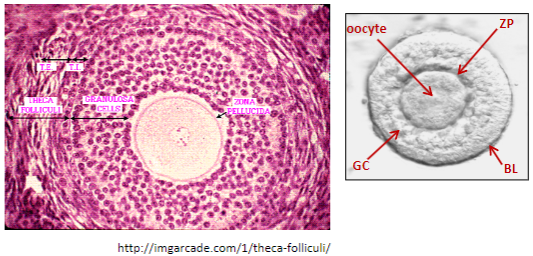
The theca, which becomes vascularized.
What factors control the initiation of follicle growth? (2)
The factors controlling initiation of growth and early stages are largely unknown.
Granulosa cells multiply and the oocyte enlarges, though it remains in meiotic arrest.
How does FSH influence folliculogenesis? (2)
FSH (follicle-stimulating hormone) drives most of folliculogenesis.
Early growth of the follicle is independent of FSH and is driven by local factors.
What happens in FSH-deficient patients or those with FSH receptor mutations? (1)
Follicles still initiate early growth but do not fully mature and eventually die.
What happens when FSH is suppressed, such as on the COCP? (2)
Follicles will still undergo early growth despite suppressed FSH.
However, the follicles will eventually die.
Picture demonstrating Follicle classification:
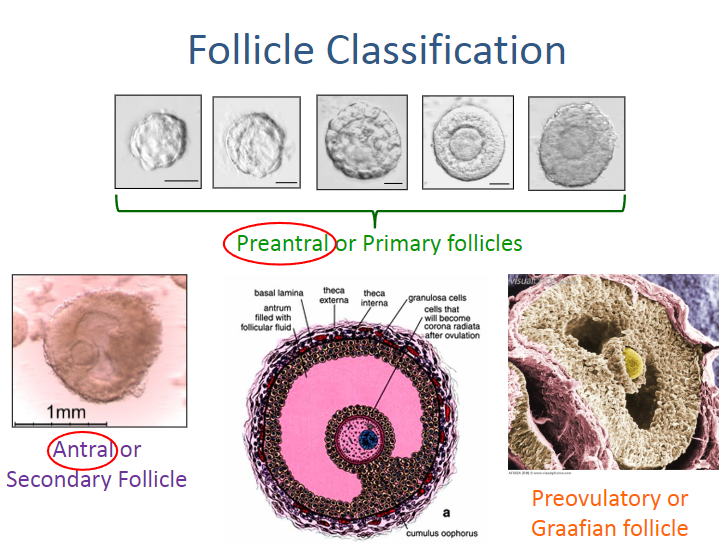
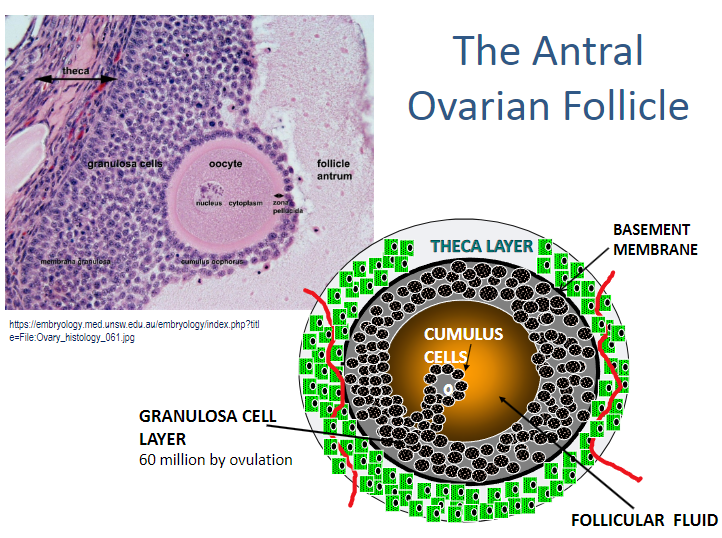
What characterizes an antral follicle? (2)
An antral follicle is characterized by the presence of a cavity or “antrum.”
The antrum is filled with fluid, known as follicular fluid.
What is follicular fluid composed of? (2)
Follicular fluid is formed as an exudate of plasma.
It contains secretory products from the oocyte and granulosa cells (GC).
What happens as the volume of follicular fluid and the antrum expand? (1)
As the volume of follicular fluid and the antrum expand, the oocyte is displaced to one side of the follicle.
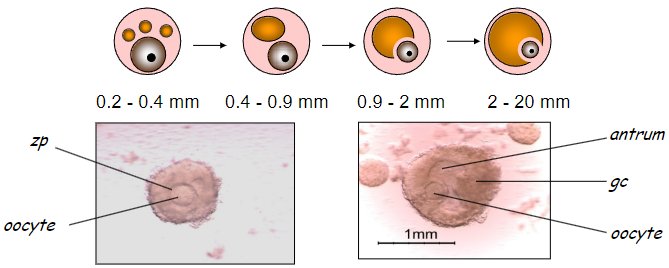
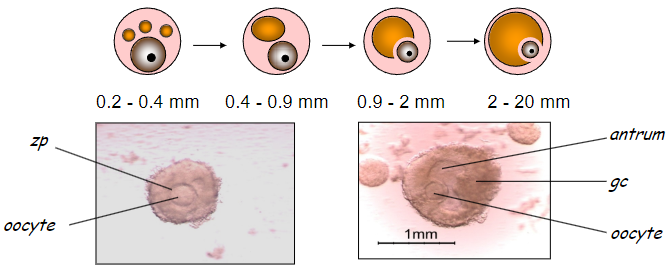
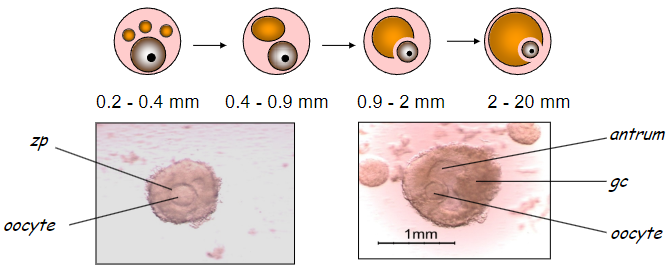
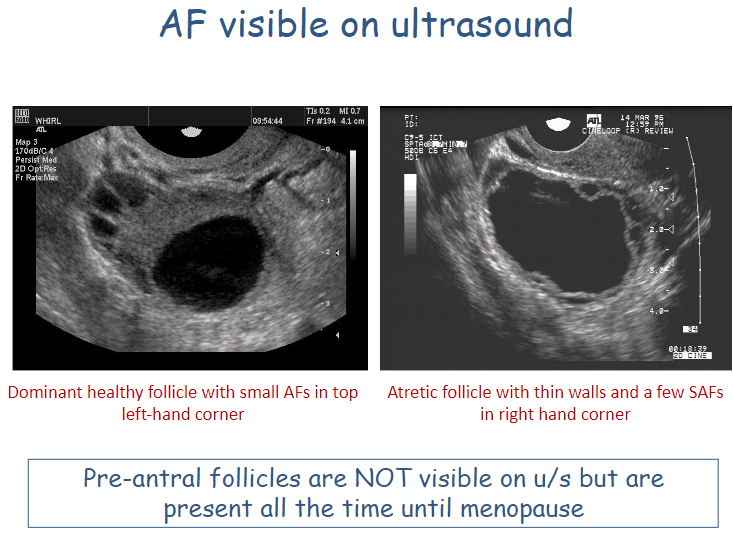
Picture demonstrating AFs Visible on ultrasound:
What is follicle initiation in folliculogenesis? (2)
A group of early primordial follicles leave the resting pool.
These follicles begin to grow continuously.
What is the role of FSH in folliculogenesis? (2)
At a certain point, follicles need FSH to continue growing.
FSH drives the growth of follicles after they reach a certain size.
What is follicle recruitment in folliculogenesis? (2)
A cohort of early antral follicles grows to the right stage and size.
This corresponds to the start of the intercycle rise in FSH.
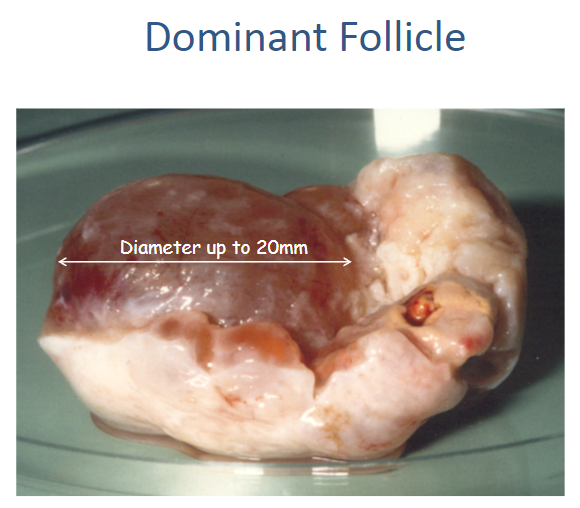
What happens during dominant follicle selection? (2)
From the recruited antral follicles, only one will be selected for ovulation.
This selection occurs because the human pelvis is designed to carry a single fetus.
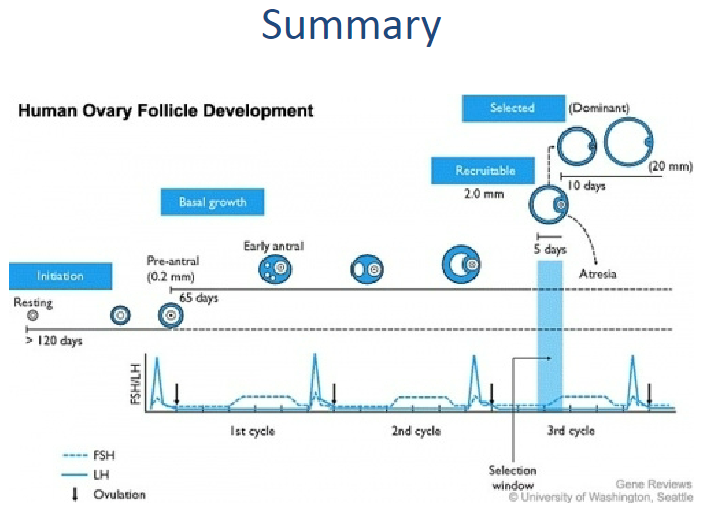
What are the stages of folliculogenesis? (4)
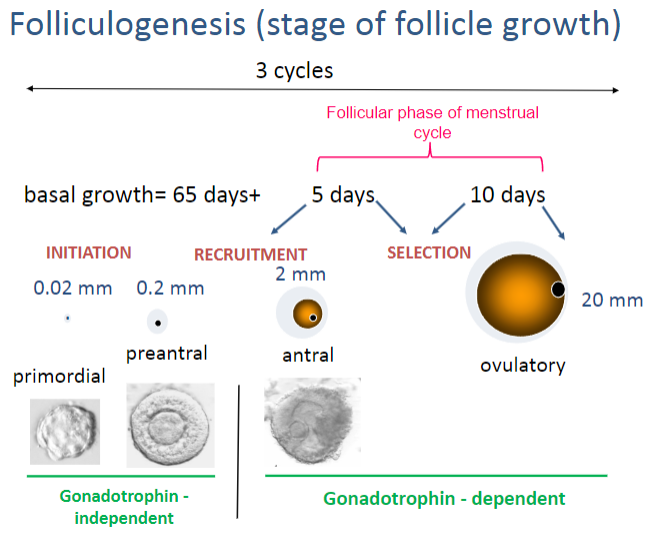
Initiation
Recruitment
SelectionDominance
What is the basal growth duration of a follicle during initiation? (1)
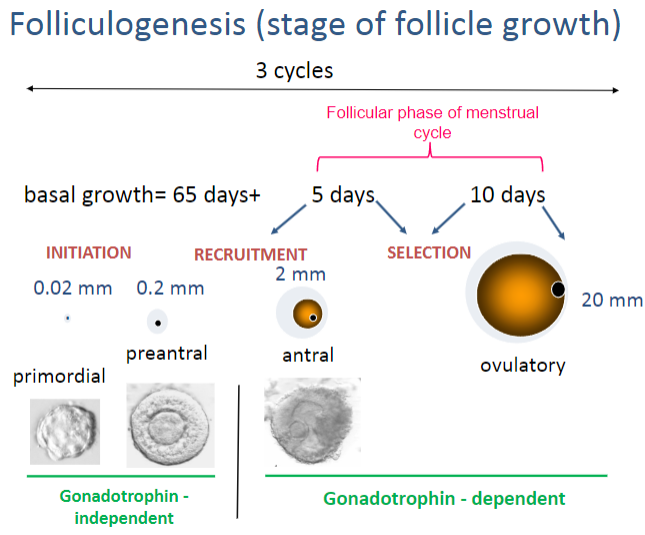
Basal growth lasts for 65 days or more.
How many cycles does it take for the follicle to reach the antral stage? (1)
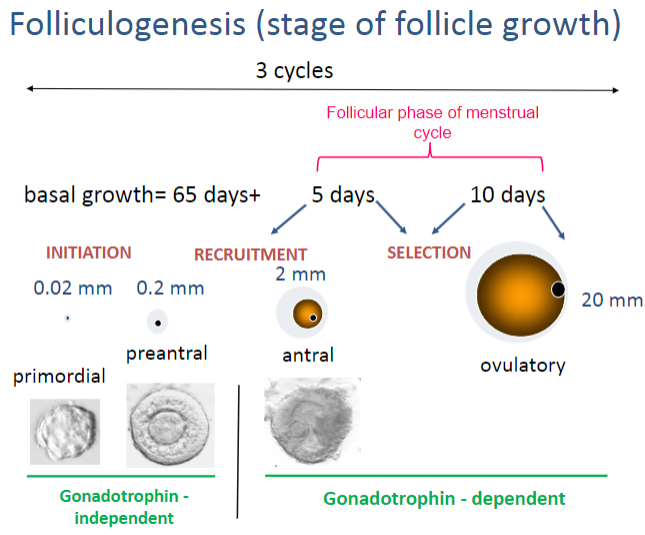
It takes 3 cycles (menstrual) for the follicle to reach the antral stage.
What is the size of a follicle at the antral stage? (1)
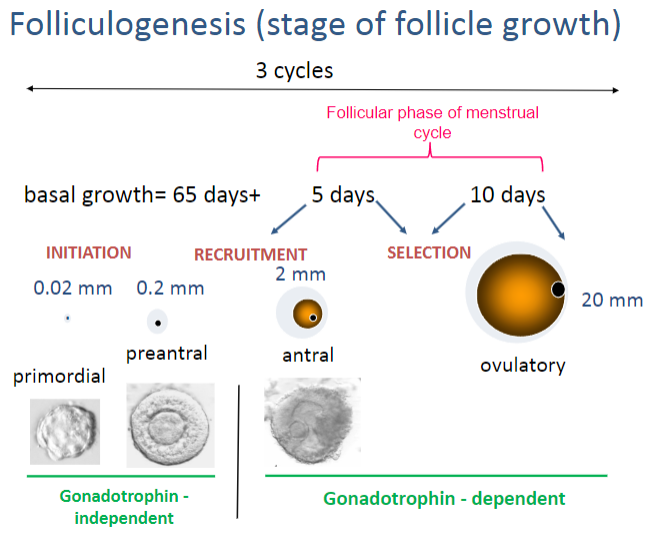
The antral follicle measures 2 mm in diameter.
What is the size of a follicle at the ovulatory stage? (1)
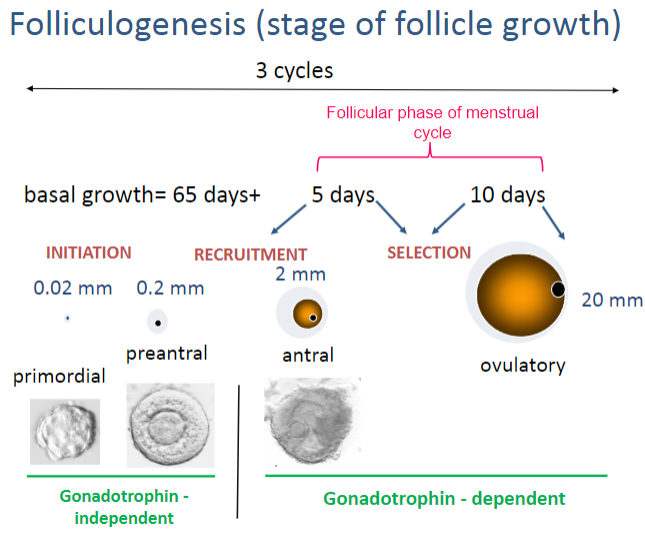
The follicle reaches 20 mm in diameter during ovulation.
How long does it take for follicular selection to occur? (1)
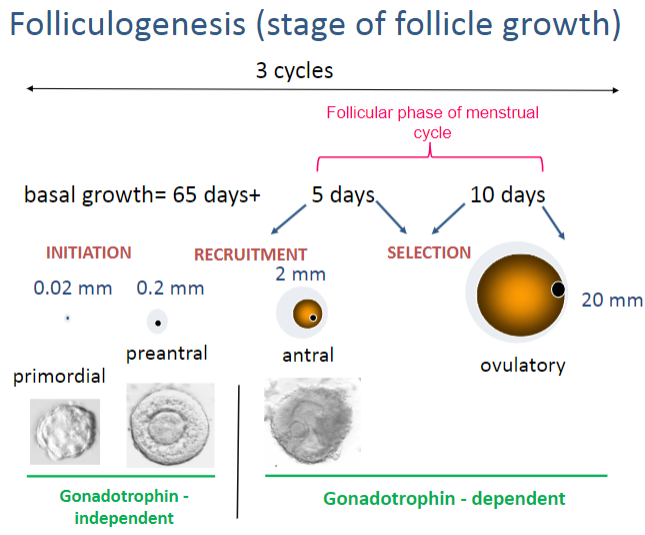
Follicular selection takes around 5 days to 10 days.
What is the role of gonadotrophins in folliculogenesis? (2)
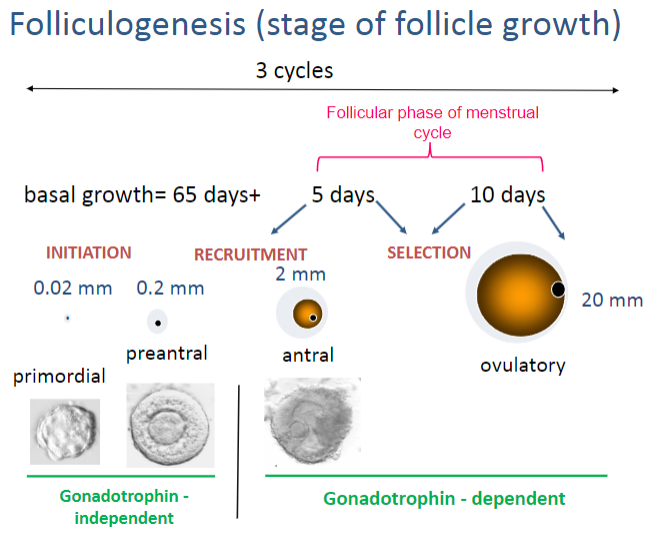
In initiation, growth is gonadotrophin-independent.
In recruitment and beyond, growth becomes gonadotrophin-dependent.
During which phase of the menstrual cycle does folliculogenesis occur? (1)
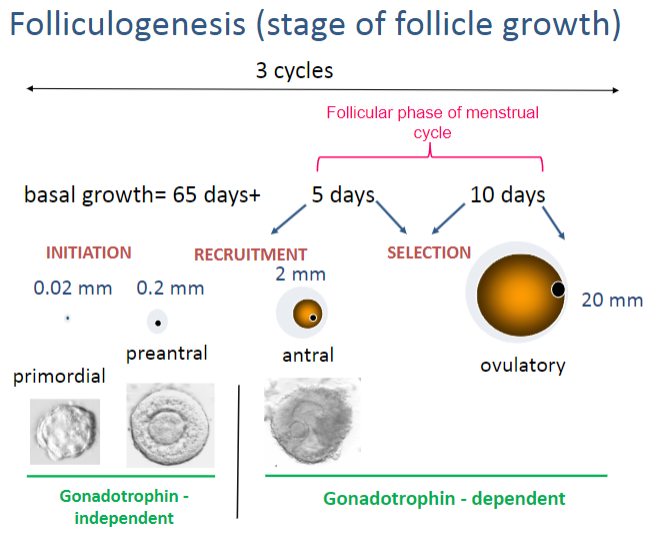
Folliculogenesis occurs during the follicular phase of the menstrual cycle. (day 1 menses/start of cycle towards ovulation, so 14 days)
Picture demonstrating the antral ovarian follicle:
Picture demonstrating a real life dominant follicle:
What is the importance of the vasculature to the follicle? (1)
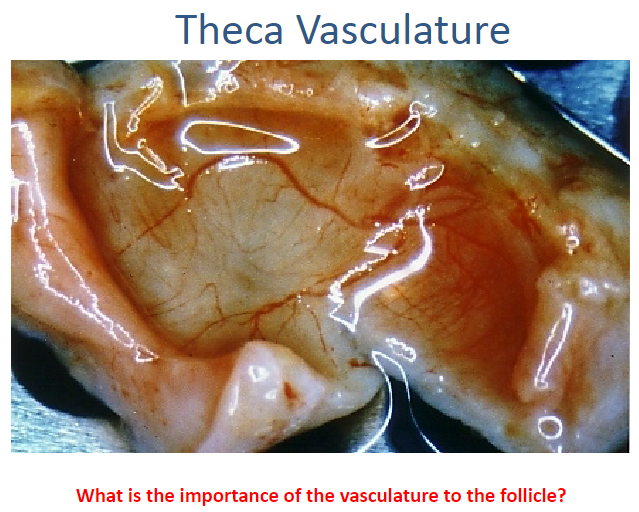
The vasculature supplies oxygen and nutrients to the follicle, which is essential for its growth and development, particularly in the theca layer, which is highly vascularized.
How does the ovarian follicle produce steroids? (2)
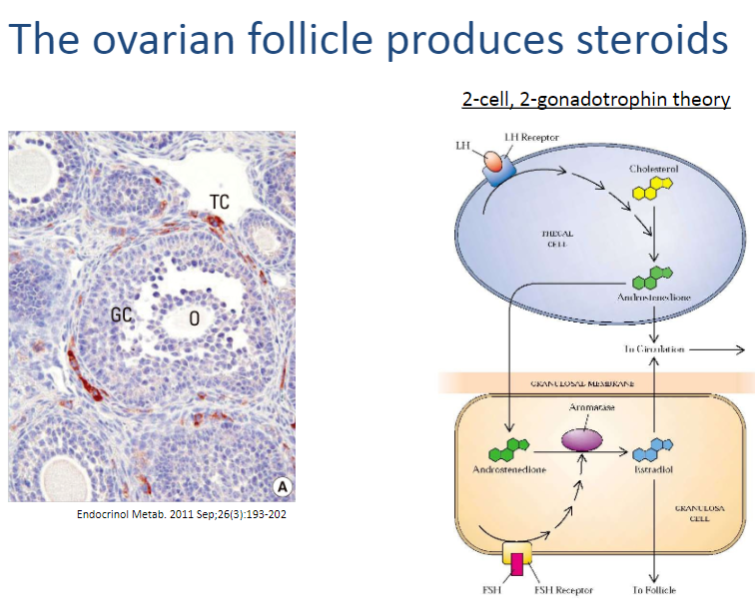
The ovarian follicle produces steroids through the theca cells and granulosa cells, working together in a two-step process:
Theca cells convert cholesterol into androstenedione, a precursor steroid.
Granulosa cells convert androstenedione into estrogen (estradiol), with the help of the enzyme aromatase.
What are the roles of LHR (Luteinizing Hormone Receptor) and FSHR (Follicle Stimulating Hormone Receptor) in folliculogenesis? (5)
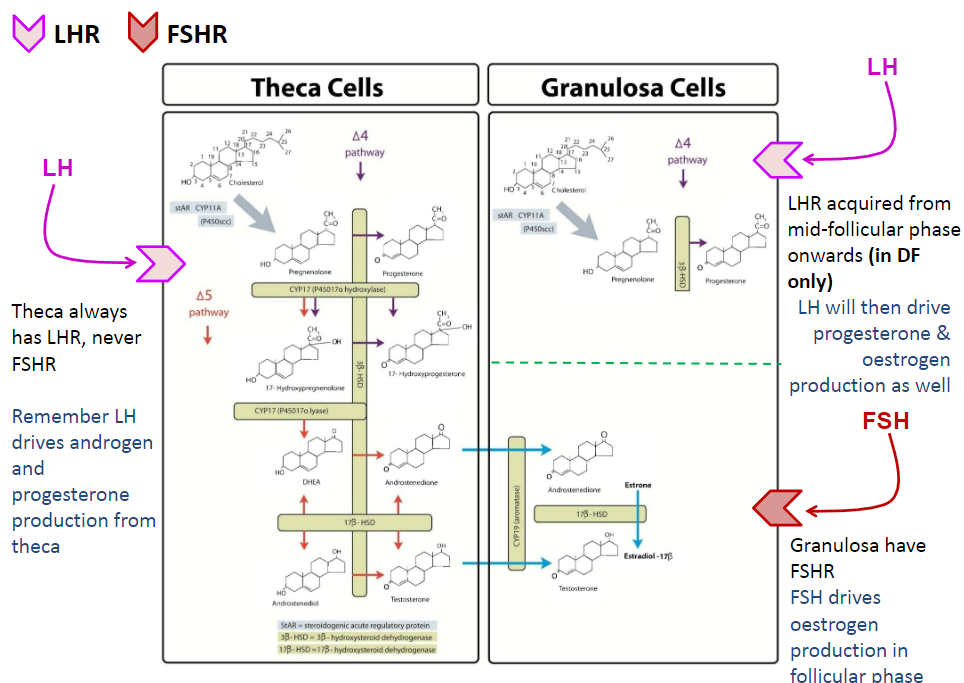
Theca cells always have LHR (Luteinizing Hormone Receptor), but never FSHR (Follicle Stimulating Hormone Receptor).
LH stimulates the theca cells to produce androgens and progesterone.
Granulosa cells have FSHR, which allows them to respond to FSH.
FSH stimulates granulosa cells to produce estrogen during the follicular phase.
LHR is acquired by granulosa cells from the mid-follicular phase onwards, but only in the dominant follicle (DF), enabling LH to also drive progesterone and estrogen production in the later stages.
What is the control mechanism of folliculogenesis involving the hypothalamus, anterior pituitary, and ovary? (5)
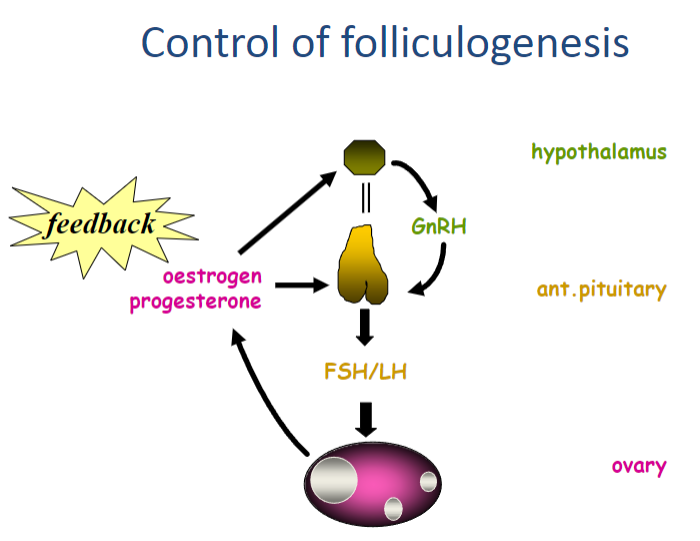
Hypothalamus secretes GnRH (Gonadotropin-Releasing Hormone).
GnRH stimulates the anterior pituitary to release FSH (Follicle-Stimulating Hormone) and LH (Luteinizing Hormone).
FSH and LH act on the ovary, promoting follicle growth and hormone production.
Estrogen and progesterone are produced by the ovaries, especially as the follicle develops.
The production of estrogen and progesterone provides feedback to regulate the secretion of GnRH, FSH, and LH to maintain balance in folliculogenesis.
What happens to the many follicles during folliculogenesis? (4)
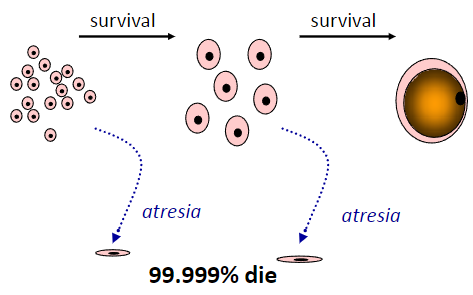
Thousands of primordial follicles are present at birth.
Most follicles die through a process called atresia (shrink and reabsorbed by the ovary).
A few follicles progress into the menstrual cycle.
Only about 400-500 follicles will ultimately ovulate throughout a woman's reproductive lifespan.
What is the summary of follicle formation and growth? (6)
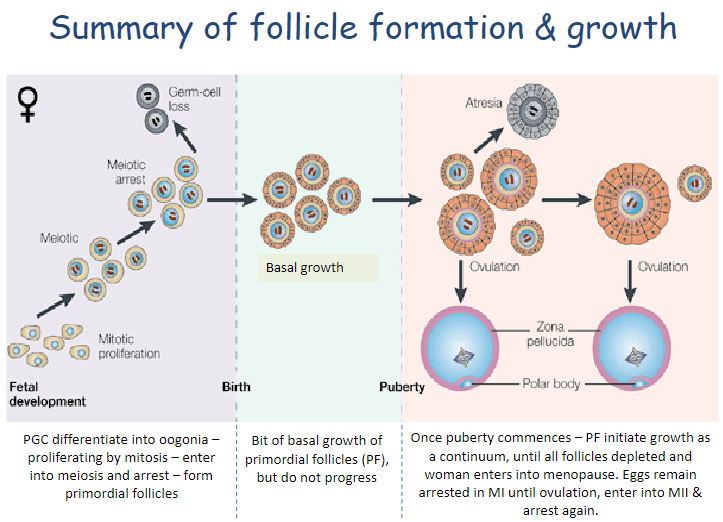
PGCs (Primordial Germ Cells) differentiate into oogonia through mitosis.
Oogonia enter meiosis and become arrested, forming primordial follicles (PF).
There is a bit of basal growth in PF, but they do not progress further.
At puberty, PF initiate growth in a continuous process.
Follicles are depleted over time, leading to menopause.
Eggs remain arrested in meiosis I (MI) until ovulation, then enter meiosis II (MII) and arrest again.
Picture demonstrating a summary of the lecture:
What are Primordial Germ Cells (PGCs)? (1)
Precursor stem cells that will become either egg or sperm.
What are oogonia? (2)
Precursors to eggs.
They are diploid and multiply by mitosis.
What are primary oocytes? (2)
Eggs that have entered meiosis.
Arrested at meiosis I.
What are secondary oocytes? (2)
Eggs that have completed meiosis I.
Entered into meiosis II and arrested again.
What is oogenesis? (1)
The process of egg development covering stages from an immature oogonium to a mature, ovulated egg ready for fertilization.
What is a follicle? (1)
An oocyte-containing structure with several cell types (e.g., granulosa and theca cells).
What is an antrum? (1)
A fluid-filled space in a follicle.
What is a preantral follicle? (2)
A follicle without an antrum.
Consists of various stages depending on the number of granulosa cell layers.
What is an antral follicle (AF)? (1)
A follicle with an antrum filled with follicular fluid.
What is folliculogenesis? (2)
The process of follicle development.
Covers stages of growth from a resting primordial follicle to antral follicles and the selection of the dominant follicle destined for ovulation.
What are sex steroids? (3)
A group of molecules derived from the common precursor cholesterol.
Includes 4 main families: progestogens, androgens, oestrogens, and corticosteroids.
Only the first three (progestogens, androgens, oestrogens) are defined as sex steroids.