When does GI tract development occur in embryonic age?
GI tract development occurs during the 3rd to 12th weeks of embryonic age (5 to 14 weeks LMP).
What are the main stages in the development of the GI tract?
The main stages include primary germ layer formation, gut tube formation, and regionalized changes caused by rotation, swelling, and elongation.
How are organs and glands produced during GI tract development?
Organs and glands are produced by budding from the gut tube.
What controls some key events in GI tract development?
Molecular control regulates some key events in GI tract development.
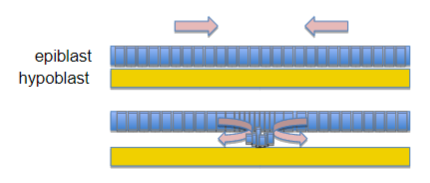
Picture demonstrating a picture of blastocyst formation:
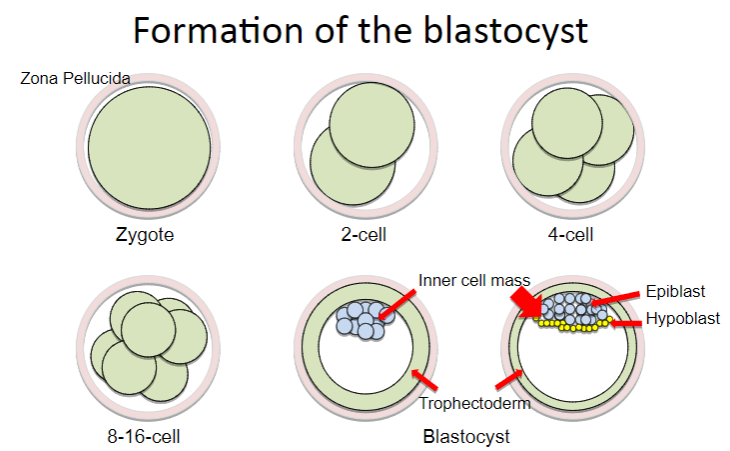
When are the primary germ layers formed?
The primary germ layers are formed during the process of gastrulation.
What happens at the beginning of the third week of embryonic development?
At the beginning of the third week, the embryo has implanted into the uterine wall.
What is the structure of the embryo at the beginning of the third week?
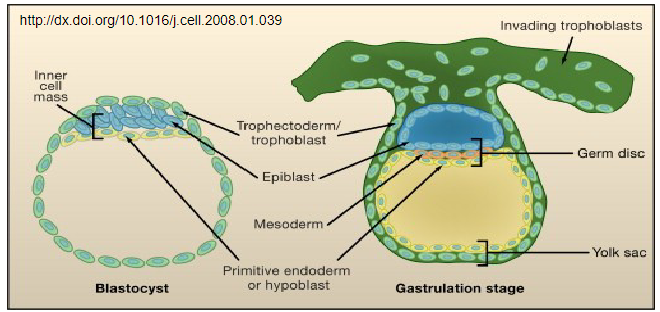
The embryo is a flat disc comprised of two cell layers.
What are the two cell layers of the early embryo?
The two cell layers are the epiblast and the hypoblast.
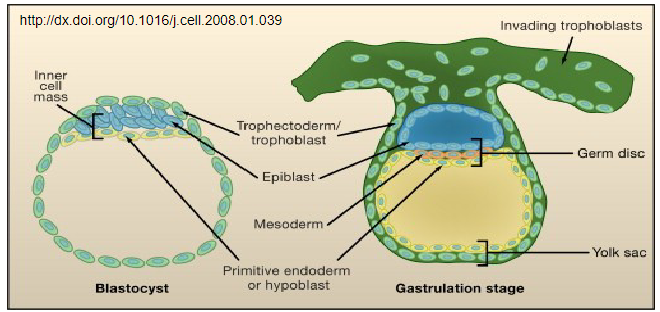
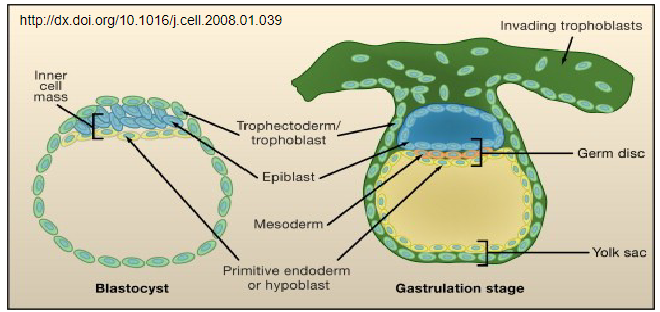
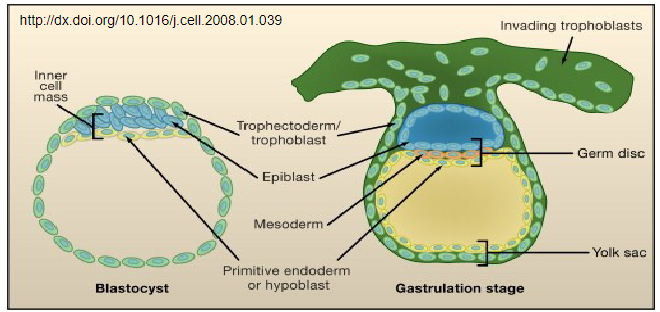
Picture demonstrating the formation of the primitive streak
Where does the primitive streak form during gastrulation?
The primitive streak forms at the caudal end of the embryonic disc.
What processes do the cells undergo during gastrulation?
During gastrulation, cells involute, ingress, migrate, and differentiate.
What does gastrulation generate?
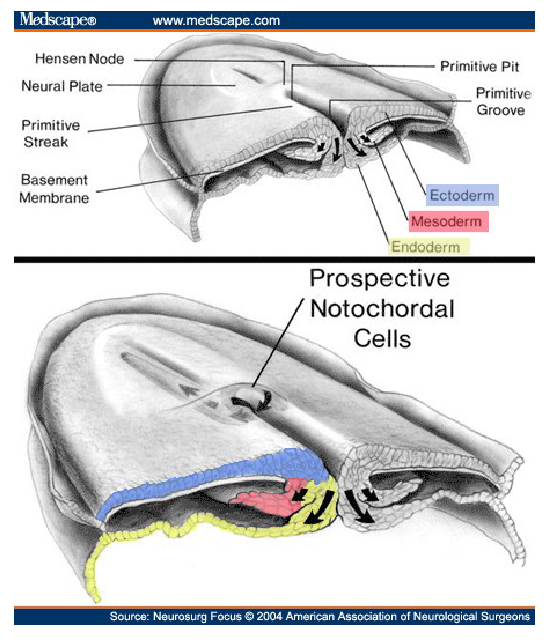
The three primary germ layers
What do the cells of the primitive streak give rise to?
The cells of the primitive streak give rise to the mesoderm and endoderm (definitive endoderm).
What does the mesoderm develop into?
The mesoderm develops into surrounding muscle, connective tissue, and mesenteries.
What does the endoderm (definitive endoderm) develop into?
The endoderm develops into the epithelium of the gut tube.
What does the epiblast give rise to?
The epiblast gives rise to the ectoderm.
What does the ectoderm develop into?
The ectoderm develops into the innervation of the gut.
What does the hypoblast (primitive endoderm) primarily give rise to?
The hypoblast primarily gives rise to extra-embryonic tissue.
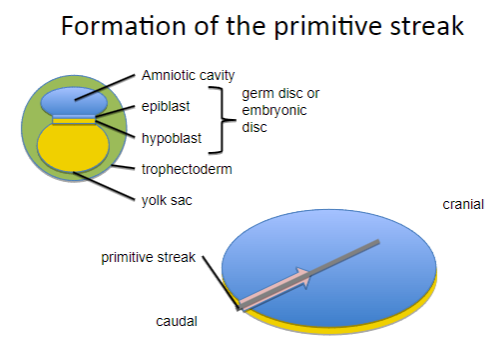
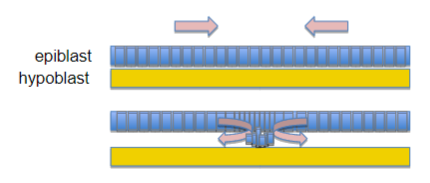
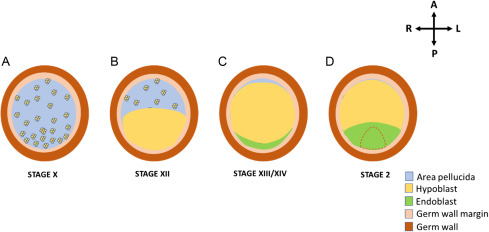
How is the gut tube formed?
The gut tube is formed by folding sheets of cells in two directions.
In which directions do the cells fold to form the gut tube?
The cells fold towards the midline along the cranial-caudal axis and towards the yolk sac at the cranial and caudal ends.
Picture demonstrating gut folding (transverse view):
Picture demonstrating gut folding (sagittal view):
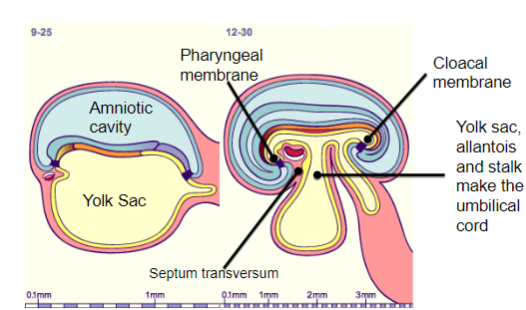
What is the initial structure of the embryo in relation to the yolk sac?
The embryo is initially a solid flat disc attached to the hemispherical yolk sac (and similarly to the amnion).
How is the gut tube formed from the yolk sac?
Part of the yolk sac cavity is enclosed within the embryo by pinching off the yolk sac to form a yolk stalk and balloon-like yolk sac.
How do the cranial and caudal intestinal portals contribute to the formation of the gut tube?
The cranial and caudal intestinal portals extend the tube towards the mouth and anus, delimited by the prochordal and cloacal plates.
What are the primary components of the gut tube?
The primary gut tube is made up of a sheet of endoderm (which makes the epithelia) and surrounding mesoderm (which makes muscle and connective tissue, including mesentery).
What are the regions of the primary gut tube?
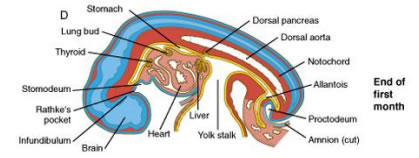
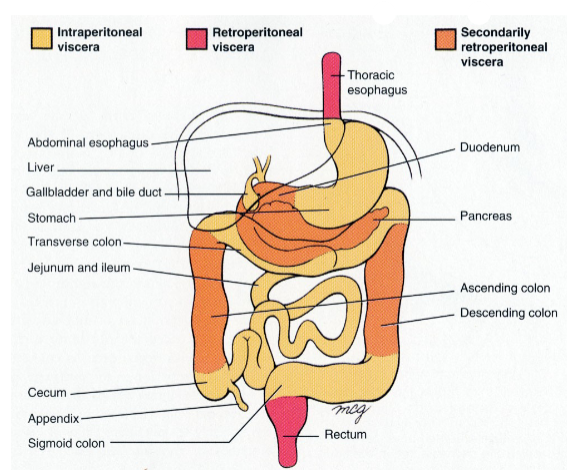
The primary gut tube is divided into the foregut, midgut, and hindgut.
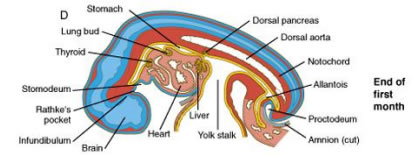
What structures are derived from the foregut?
The foregut gives rise to the pharynx, esophagus, stomach, cranial half of the duodenum, and the Ampulla of Vater (where the common bile duct and pancreatic duct join).
What structures are derived from the midgut?
The midgut gives rise to the caudal duodenum, jejunum, ileum, cecum, appendix, ascending colon, and proximal 2/3 of the transverse colon.
What structures are derived from the hindgut?
The hindgut gives rise to the distal 1/3 of the transverse colon, descending colon, and rectum.
What is the role of Homeotic (Hox) genes in embryonic development?
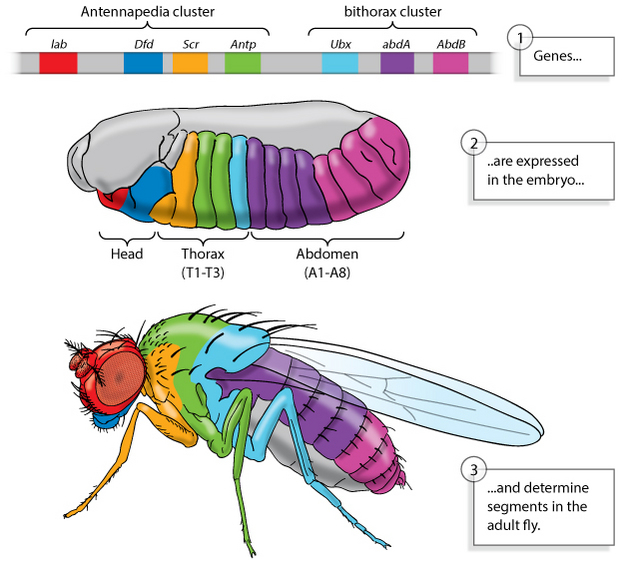
Homeotic (Hox) genes determine the position along the cranial-caudal axis.

What is an example of a mutation in Hox genes in Drosophila?
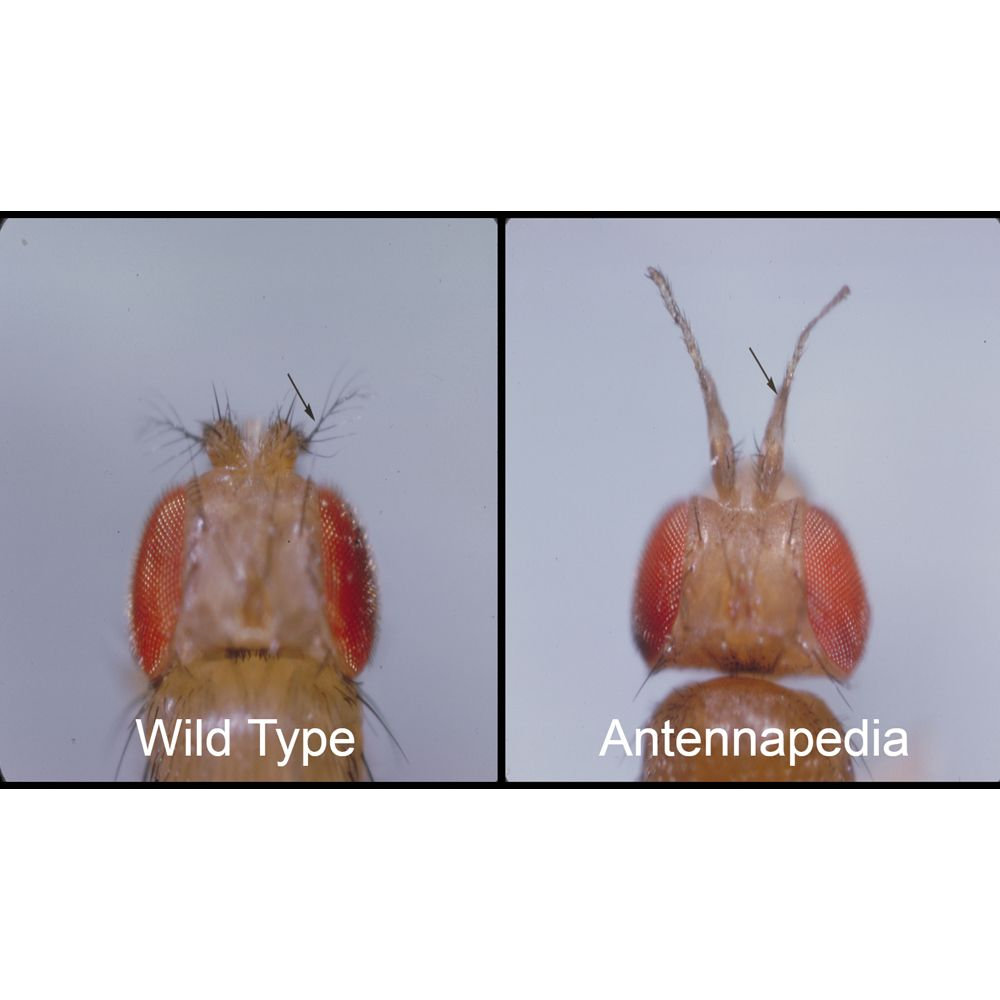
In Drosophila, Antennapedia mutants have legs instead of antennae.
How do Hox gene expression boundaries affect GI tract development?
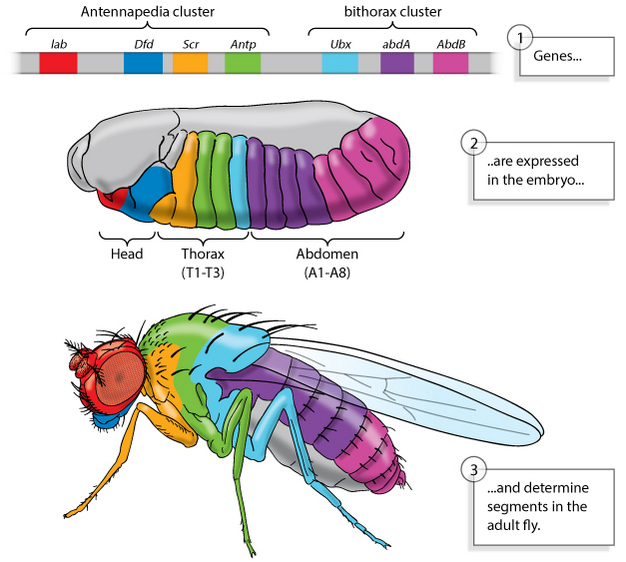
Boundaries of Hox gene expression along the cranial-caudal axis specify the position of GI tract structures.
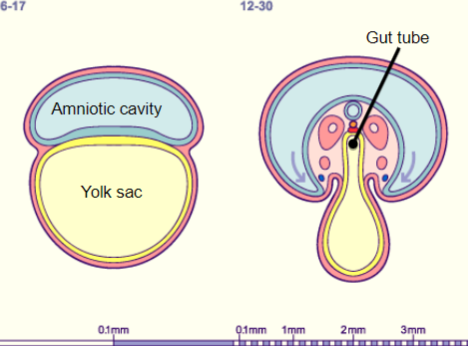
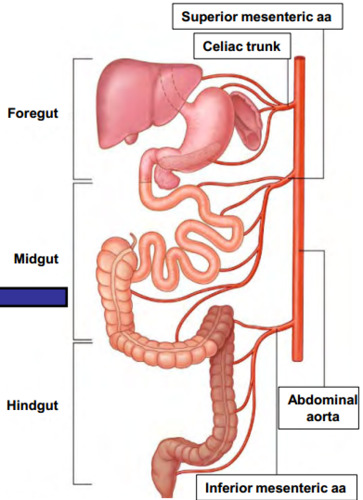
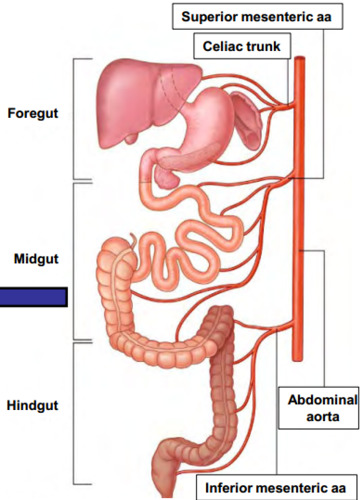
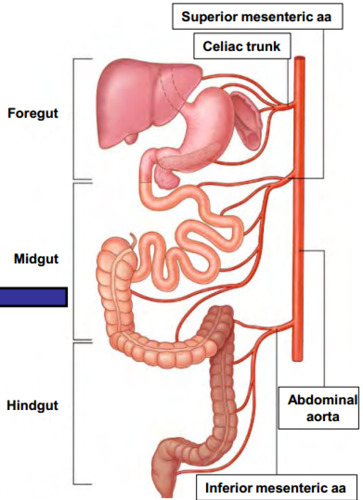
Picture demonstrating arterial supply defining regions of the gut:
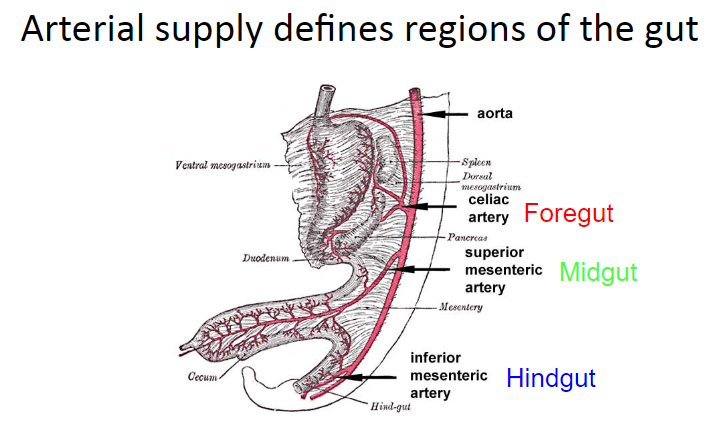
How is the gut initially surrounded by blood vessels?
The gut is surrounded by a plexus of blood vessels, joining vitelline vessels to the aorta.
How are the arteries that supply the GI tract formed?
The plexus of blood vessels resolves to form the arteries that supply the GI tract from the aorta.
Which artery supplies the foregut?
The celiac artery supplies the foregut.
Which artery supplies the midgut?
The superior mesenteric artery supplies the midgut.
Which artery supplies the hindgut?
The inferior mesenteric artery supplies the hindgut.
Where do sympathetic ganglia develop in relation to the aorta?
Sympathetic ganglia develop next to the major branches of the aorta.
What do post-ganglionic sympathetic axons innervate?
Post-ganglionic sympathetic axons innervate the same tissues that the arteries supply with blood.
Which ganglion is associated with the foregut?
The celiac ganglion is associated with the foregut.
Which ganglion is associated with the midgut?
The superior mesenteric ganglion is associated with the midgut.
Which ganglion is associated with the hindgut?
The inferior mesenteric ganglion is associated with the hindgut.
How does the regionalized development of the gut tube occur?
Regionalized development of the gut tube occurs simultaneously.
What kind of process is gut development?
Gut development is a dynamic and three-dimensional process.
What drives the development of the gut?
Gut development is driven by growth, expansion, and rotation.
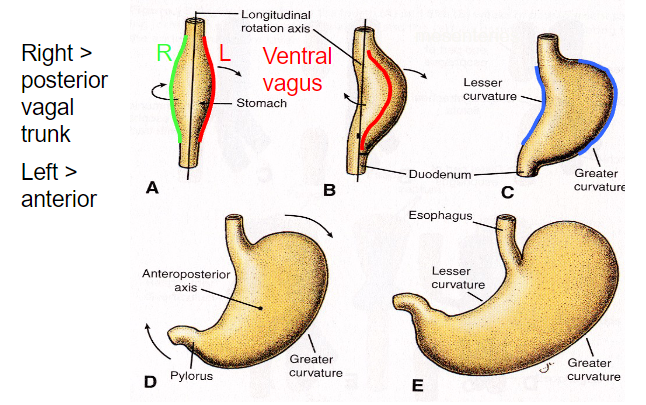
Picture demonstrating Stomach expansion & rotation:
What causes gastric outlet obstruction in pyloric stenosis?
Pyloric stenosis is caused by smooth muscle hypertrophy.
What is the incidence of pyloric stenosis?
The incidence of pyloric stenosis is 3 in 1000.
What symptom is commonly associated with pyloric stenosis?
Projectile vomiting shortly after feeding is a common symptom of pyloric stenosis.
What characteristic changes are observed in the pyloric channel in pyloric stenosis?
Pyloric channel elongation, often described as a “railroad track” appearance, is observed.
What are the measurement criteria for diagnosing pyloric stenosis?
The pyloric channel length is greater than 16mm, the wall thickness is greater than 4mm, and the diameter is greater than 14mm.
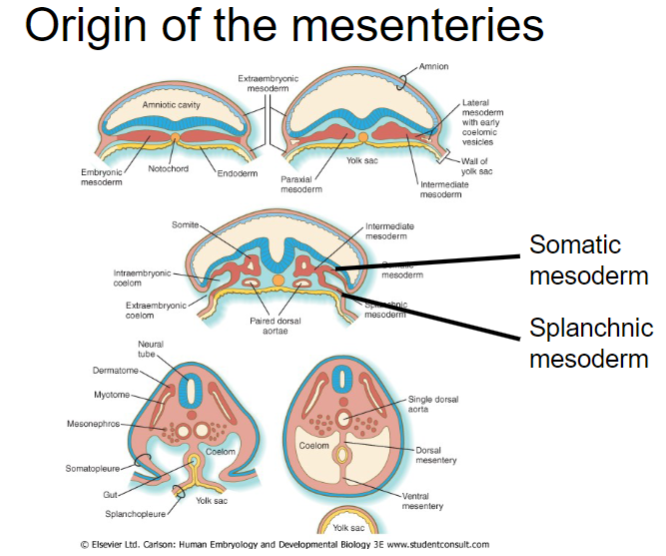
Picture demonstrating the origin of the mesenteries:
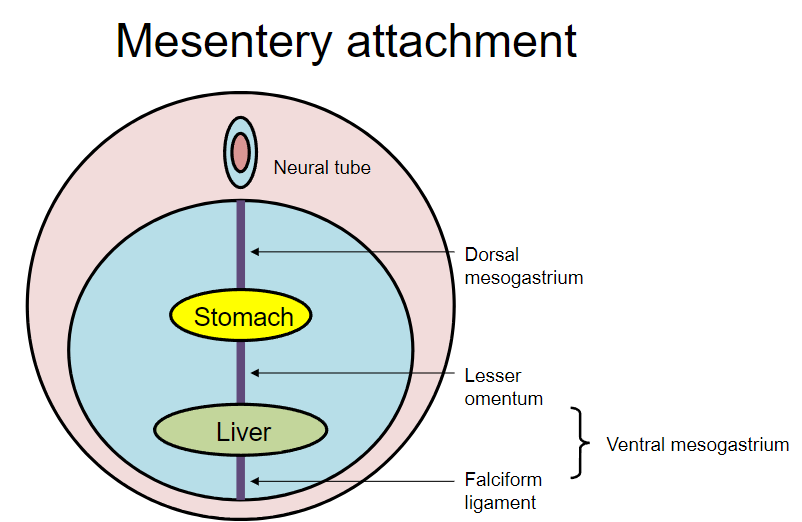
Picture demonstrating Mesentery attachment:
What happens to the dorsal mesogastrium during stomach rotation?
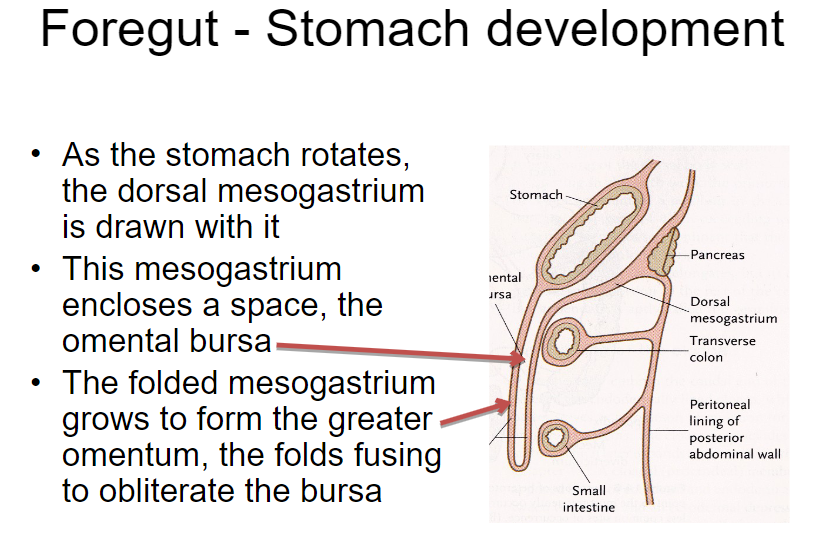
As the stomach rotates, the dorsal mesogastrium is drawn with it.
What is enclosed by the dorsal mesogastrium during stomach rotation?
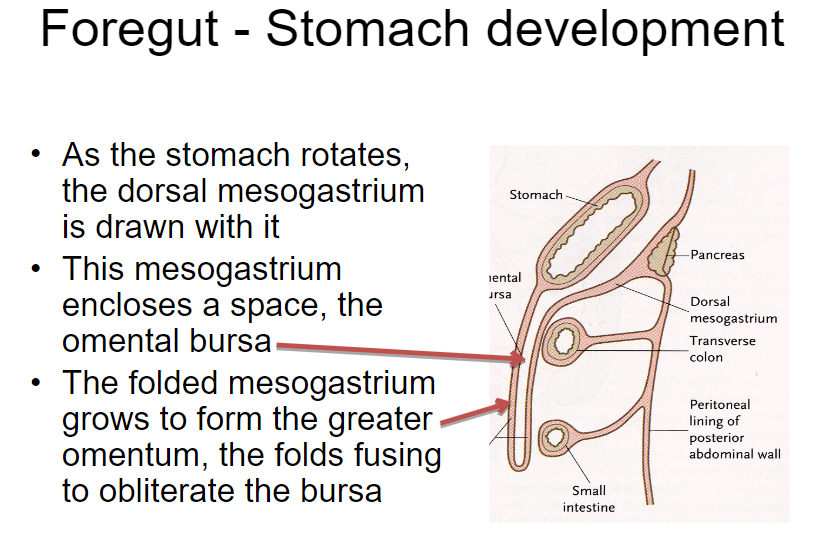
The dorsal mesogastrium encloses a space called the omental bursa.
What structure is formed from the folded mesogastrium during stomach development?
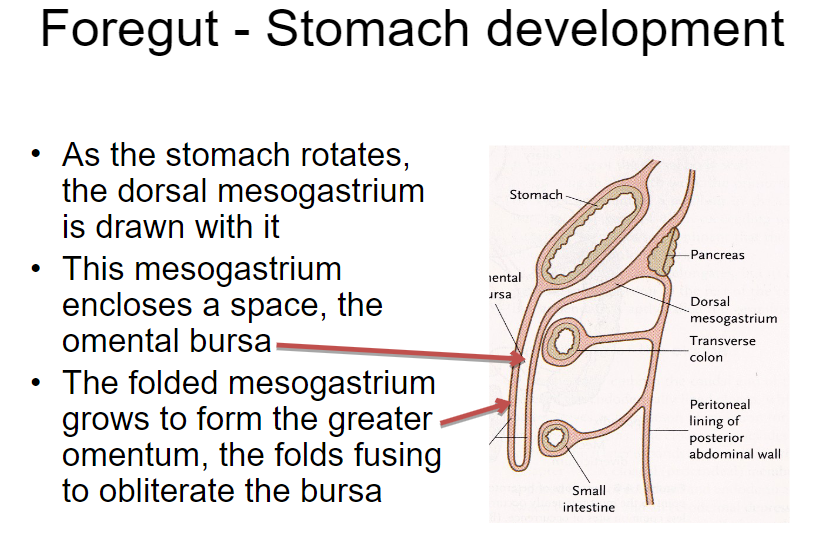
The folded mesogastrium grows to form the greater omentum.
What happens to the omental bursa during stomach development?
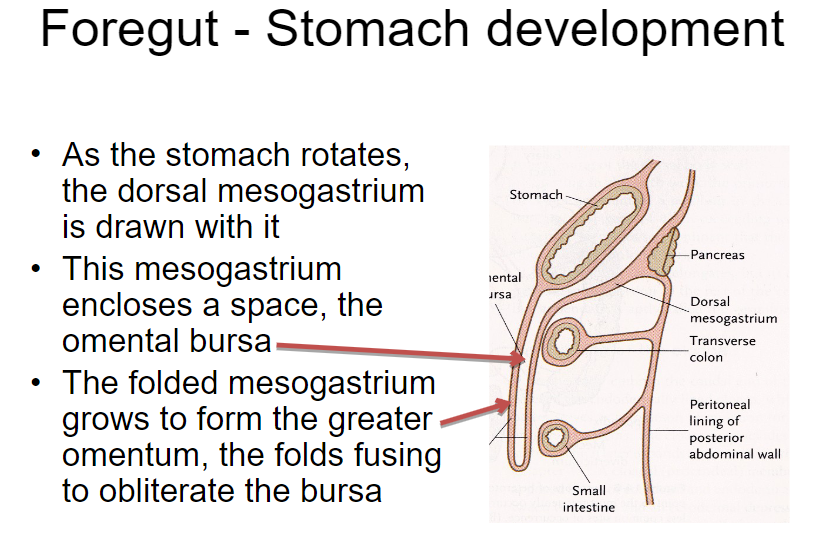
The folds of the greater omentum fuse to obliterate the omental bursa.
Picture demonstrating the Fusion of the mesenteries with the posterior abdominal wall fixes the mature gut in place:
What is the inducing signal for liver development?
The inducing signal for liver development is from the heart to the ventral gut endoderm.
Where does the hepatic diverticulum grow into during liver development?
The hepatic diverticulum grows into the mesenchyme of the septum transversum.
What structures proliferate within the hepatic diverticulum during liver development?
Cords of hepatic endoderm, bile drainage ducts, and blood vessels proliferate, arranged as sinusoids.
How does the liver expand during development?
The liver exceeds the size of the septum transversum and expands into the ventral mesentery.
What structures arise from the remaining ventral mesentery during liver development?
The remaining ventral mesentery gives rise to the falciform ligament between the liver and the body wall, and the lesser omentum between the liver and the stomach.
How many pancreatic buds are formed during pancreas development?
Two pancreatic buds are formed.
Where does the dorsal pancreatic bud arise from?
The dorsal pancreatic bud arises from the duodenal endoderm and is induced by the notochord.
Where does the ventral pancreatic bud arise from?
The ventral pancreatic bud arises from the hepatic diverticulum and is induced by hepatic mesoderm.
What happens as the duodenum rotates during pancreas development?
As the duodenum rotates, the ventral and dorsal pancreatic buds meet and fuse.
What complication can occur if the ventral pancreatic bud is bifid?
If the ventral pancreatic bud is bifid (bi-lobed) and one part rotates around the duodenum, it can lead to the formation of an annular pancreas, which can obstruct the duodenum.
How does an annular pancreas develop?
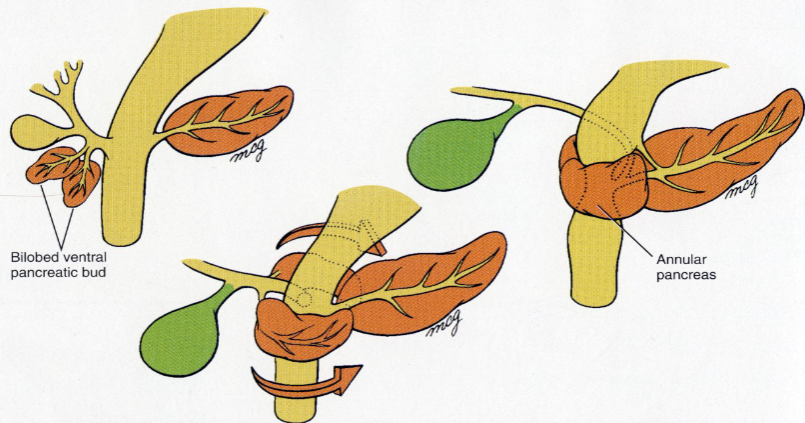
An annular pancreas develops from bi-lobed ventral buds that migrate in opposite directions around the duodenum.
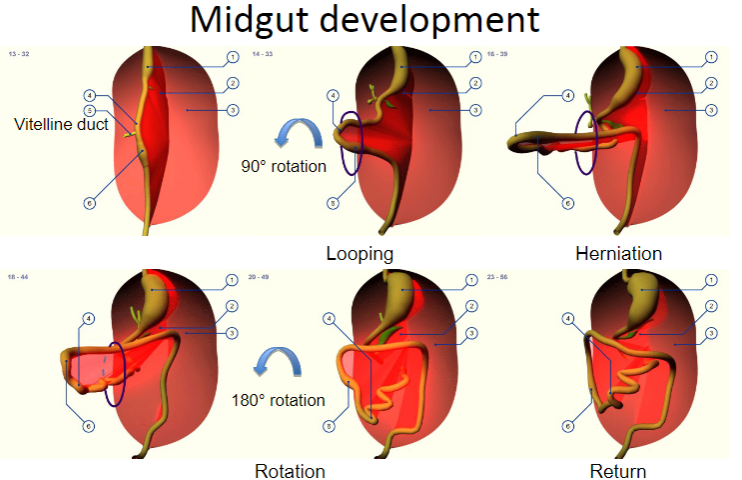
How are the intestines attached throughout their length during midgut development?
The intestines are attached throughout their length by the dorsal mesentery, but not the ventral mesentery.
What leads to the stereotypical folding of the gut during midgut development?
The mesentery and gut grow at different rates, leading to the stereotypical folding of the gut.
What artery supplies the midgut?
The ventral branch of the aorta, known as the superior mesenteric artery (SMA), supplies the midgut.
What happens to the intestines with a rapid increase in length during midgut development?
With a very rapid increase in length, the intestines rotate around the superior mesenteric artery (SMA).
What occurs at around 6 or 7 weeks of development regarding the intestines?
At around 6 or 7 weeks, the abdomen is too small to accommodate the rapidly growing intestines, so they herniate into the umbilical stalk.
When do the intestines return to the abdominal cavity after herniating into the umbilical stalk?
By 10 weeks, the abdomen is bigger, and the intestines return to the abdominal cavity.
Picture demonstrating mid gut development:
What is the most common intestinal abnormality related to midgut development?
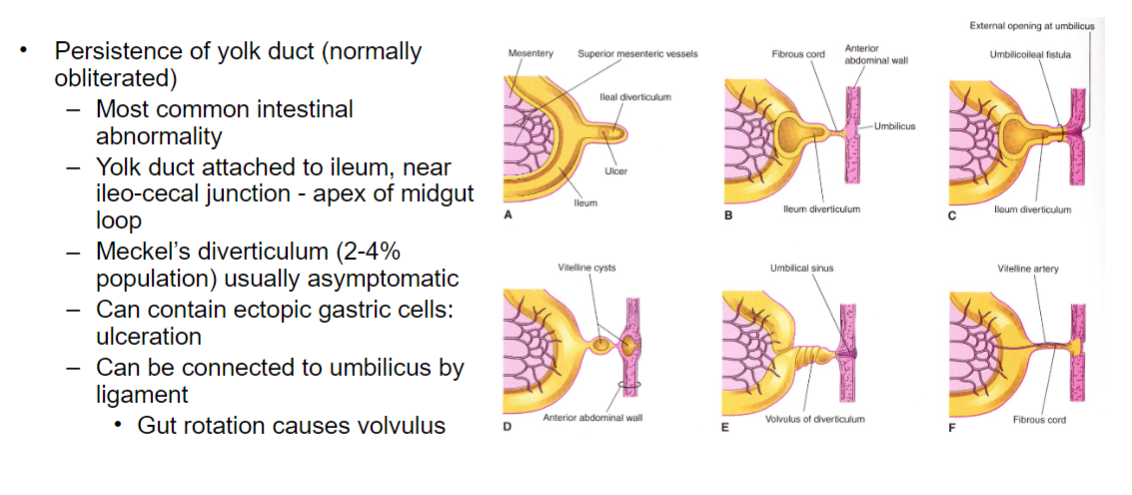
The most common intestinal abnormality related to midgut development is the persistence of the yolk duct.
Where is the yolk duct typically attached in cases of its persistence?
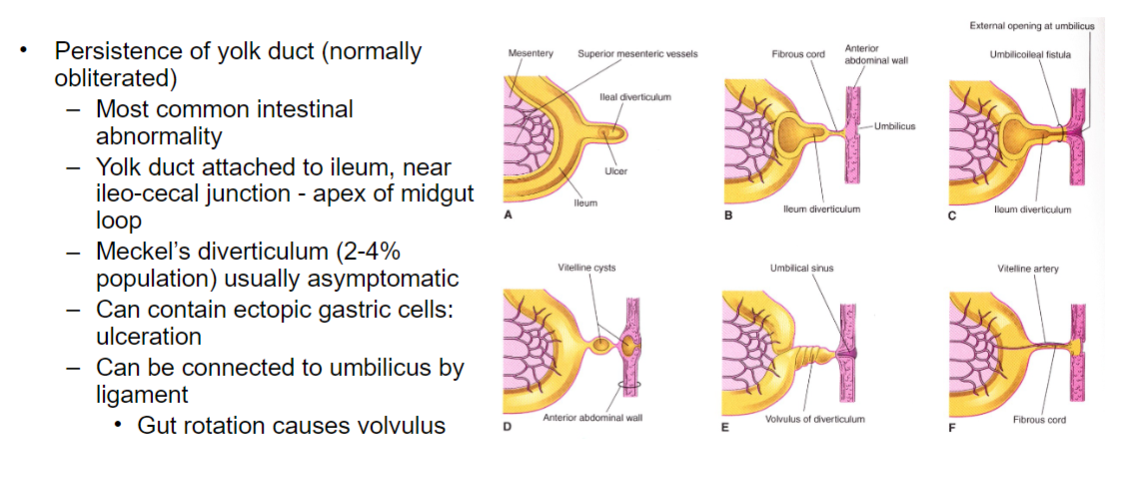
The yolk duct is typically attached to the ileum, near the ileocecal junction, which is the apex of the midgut loop.
What structure can result from the persistence of the yolk duct, and what is its prevalence in the population?
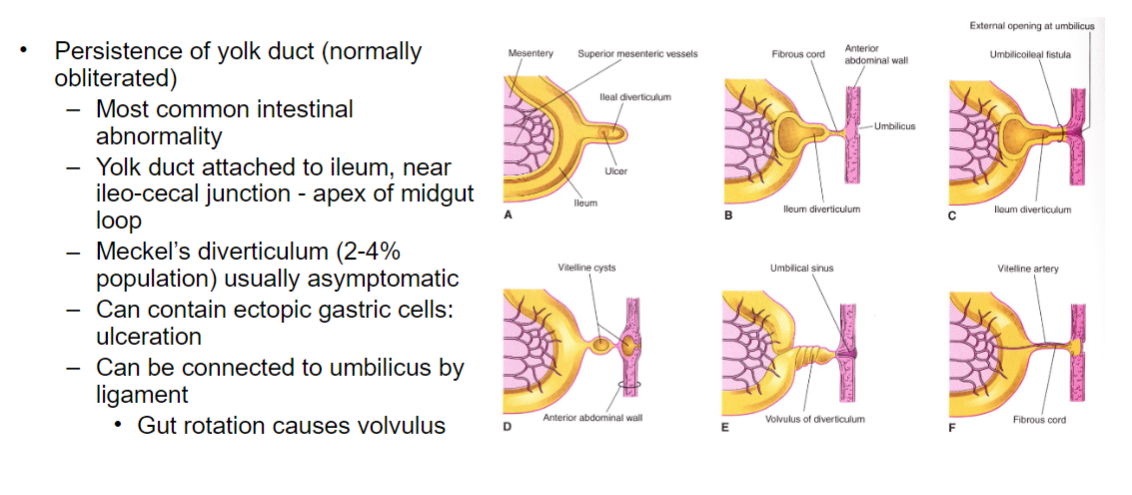
Meckel's diverticulum (2-4% of the population) usually results from the persistence of the yolk duct and is typically asymptomatic.
What complications can arise from Meckel's diverticulum?
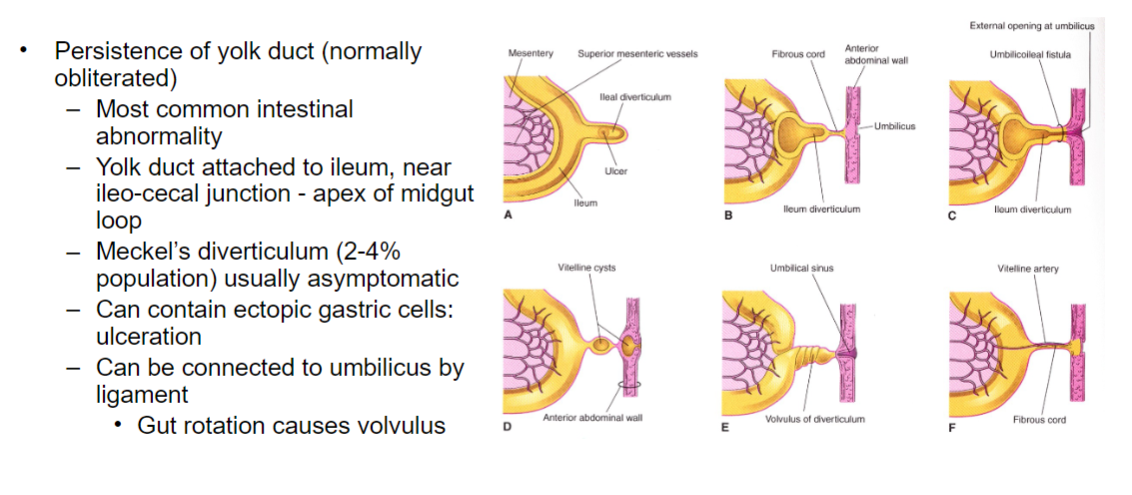
Meckel's diverticulum can contain ectopic gastric cells, leading to ulceration. Additionally, it can be connected to the umbilicus by a ligament.
What complication can arise from gut rotation during midgut development?
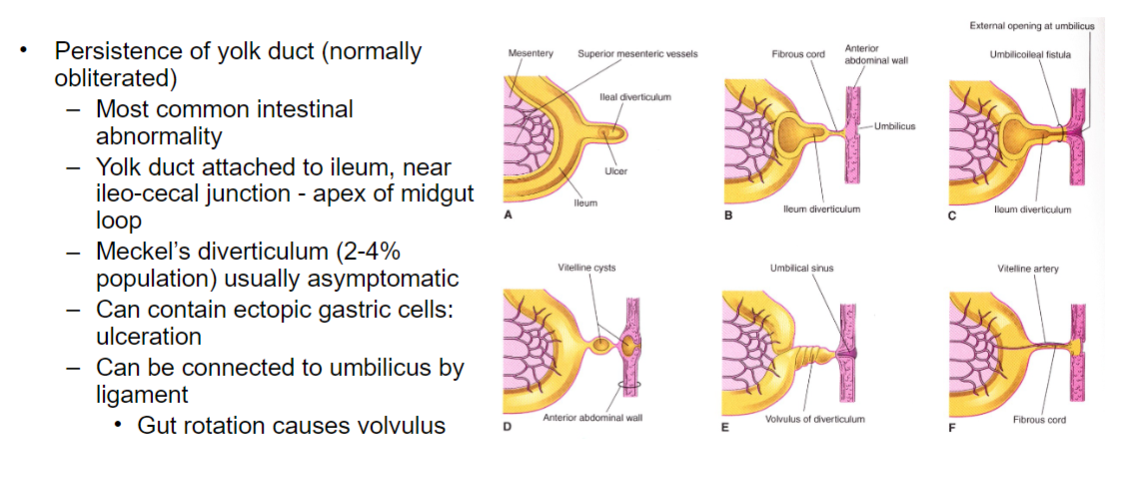
Gut rotation can cause volvulus, which is a twisting of the intestine that can lead to obstruction and ischemia.
What occurs in an umbilical hernia?
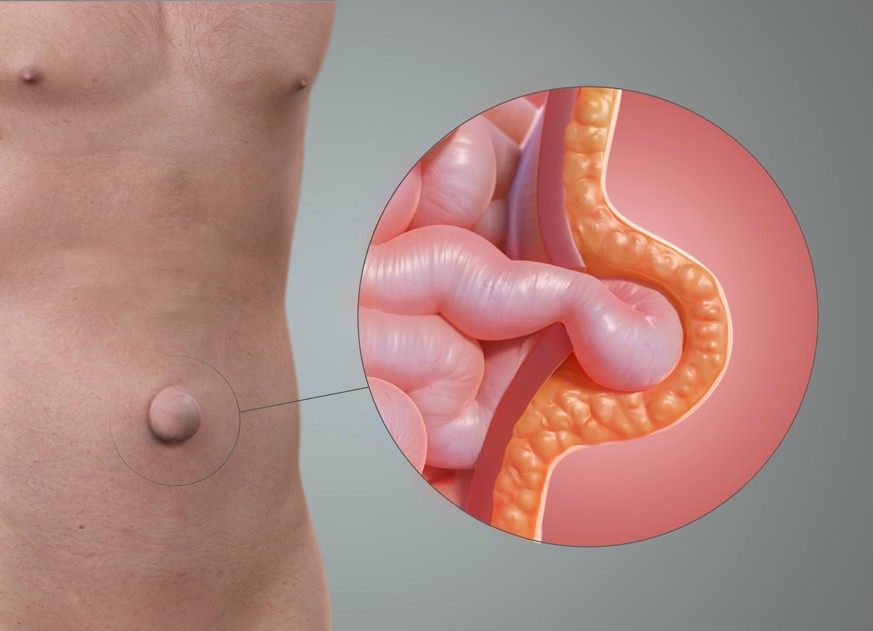
In an umbilical hernia, the intestines return normally to the abdominal cavity, but the rectus abdominis muscle fails to fuse around the umbilicus, leading to protrusion of the gut covered in skin.
What is omphalocele?
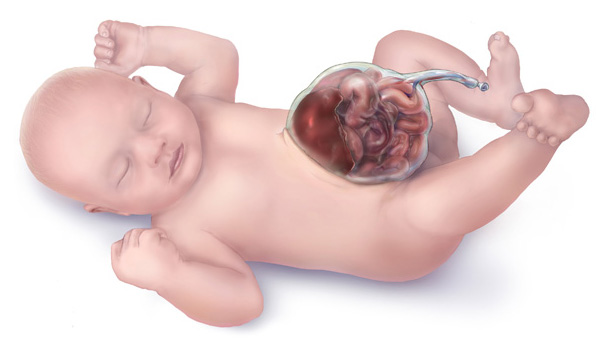
Omphalocele is a condition characterized by the failure of intestinal loops to return into the abdomen, resulting in a hernia covered in amnion.
What factors are associated with omphalocele?
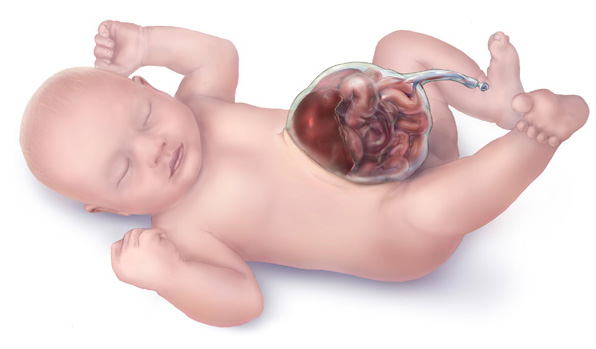
Omphalocele is associated with maternal obesity, alcohol/tobacco use, and SSRI (selective serotonin reuptake inhibitor) use during pregnancy.
What is gastroschisis?

Gastroschisis is a condition characterized by the failure of the ventral body wall to fuse, resulting in exposed intestines without covering.
What is the incidence of gastroschisis?

The incidence of gastroschisis is increasing and is estimated to be 1 in 3000 births.
What factors are associated with gastroschisis?

Gastroschisis is markedly associated with young maternal age, low maternal BMI, and recreational drugs, especially cocaine, during pregnancy.
What is Hirschsprung's disease?
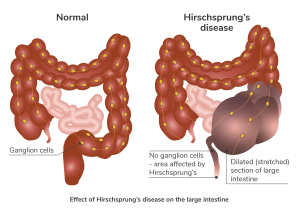
Hirschsprung's disease is a condition characterized by aganglionic megacolon, primarily affecting the hindgut.
What is the primary pathology seen in Hirschsprung's disease?
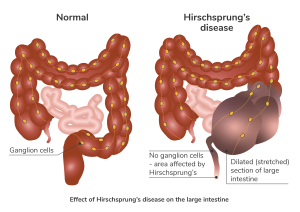
In Hirschsprung's disease, there is a lack of enteric ganglia in the affected segment of the colon, leading to abnormal peristalsis and tone.
What are the clinical manifestations of Hirschsprung's disease?
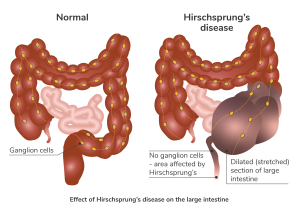
The dilatation of sections of the colon with lack of tone and peristalsis leads to profound constipation.
What causes Hirschsprung's disease?
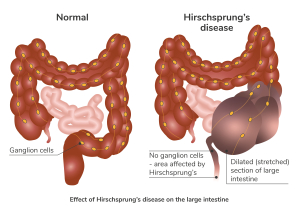
Hirschsprung's disease is caused by a lack of neural crest cells, which are responsible for the formation of enteric ganglia in the colon.
How does the absence of enteric ganglia affect intestinal contraction?
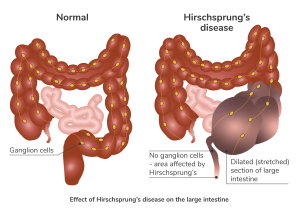
In Hirschsprung's disease, the absence of enteric ganglia leads to tonic contraction of the affected segment of the colon because normal inhibitory innervation is absent.
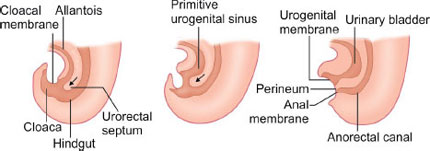
What are neural crest cells?
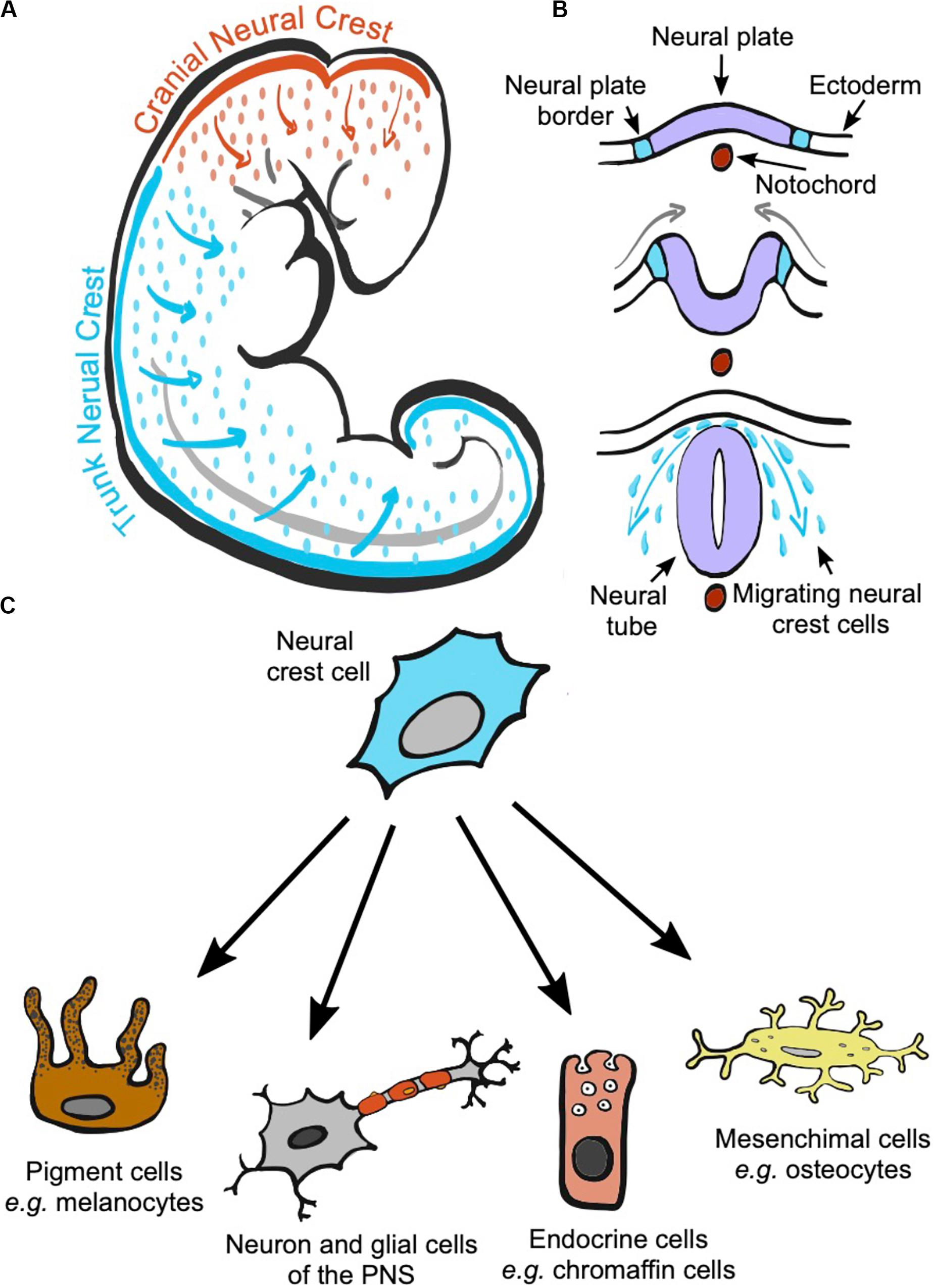
Neural crest cells are a population of cells that originate from the dorsal region of the neural tube during embryonic development.
What is the role of neural crest cells?
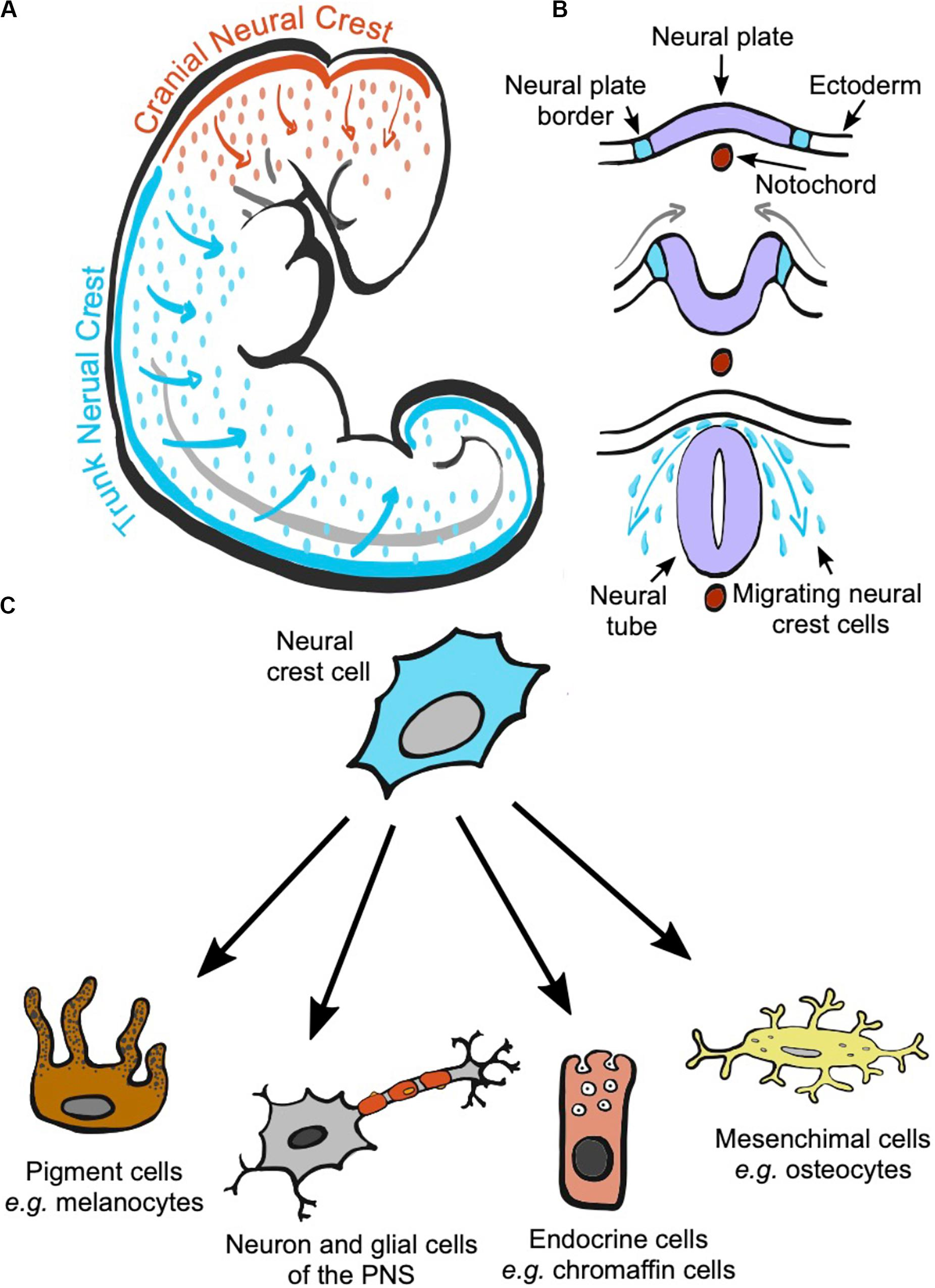
Neural crest cells contribute to a wide variety of tissues in the embryo, including the formation of various structures in the head and neck, peripheral nervous system, and certain endocrine cells.
What specific role do neural crest cells play in gut development?
Neural crest cells contribute to the parasympathetic innervation of the gut, playing a crucial role in regulating gastrointestinal function.
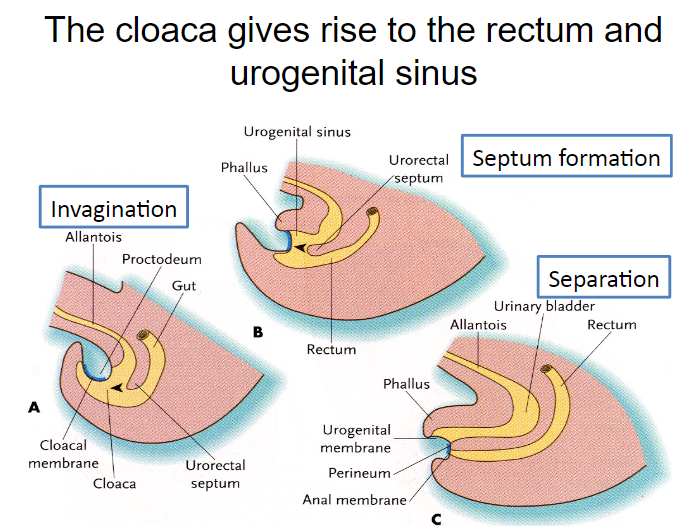
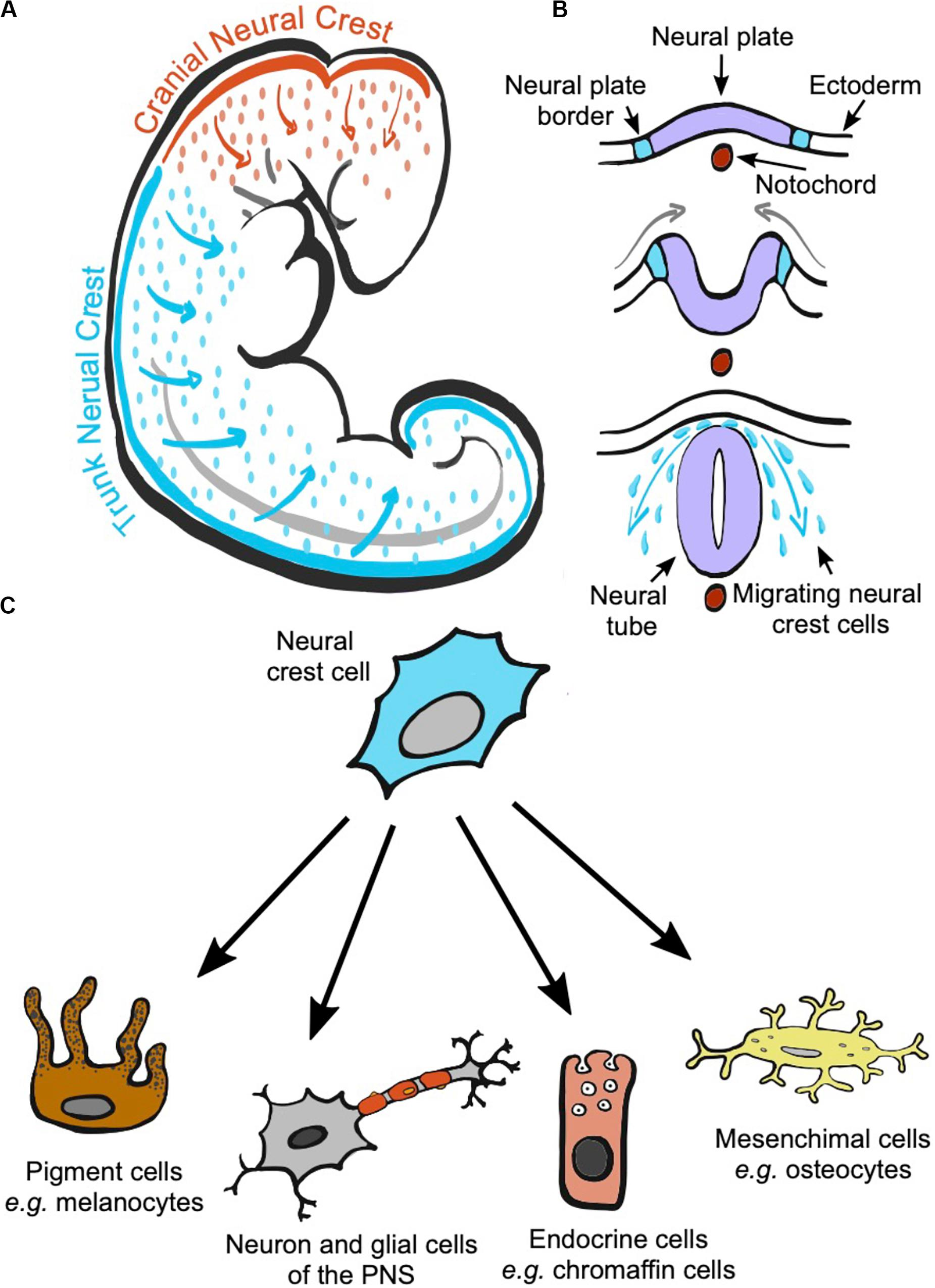
What is the cloaca?
The cloaca is the transient common end of the digestive and urogenital systems, including the base of the allantois, which forms the urogenital sinus.
What covers the cloaca externally?
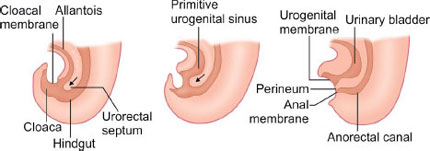
The cloaca is covered externally by the cloacal (proctodeal) membrane, which overlies the ectoderm depression known as the proctodeum.
What structure divides the cloaca during development?
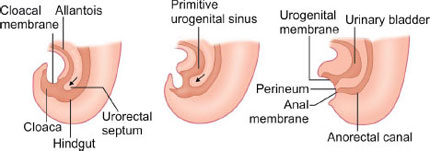
The cloaca is split by the urorectal septum, which gives rise to the urogenital membrane and the anal membrane.
When does the anal membrane perforate during development?
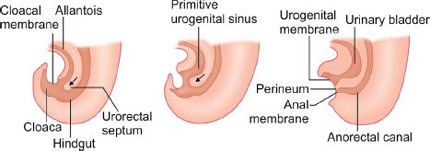
The anal membrane perforates around 7-8 weeks of development.
What are the possible causes of imperforate anus?
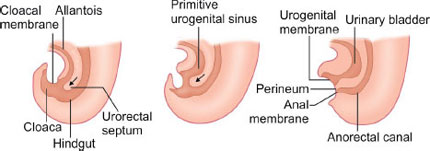
Imperforate anus can result from the persistence of the anal membrane or atresia of the anal canal, rectum, or both.
Picture demonstrating The cloaca giving rise to the rectum andurogenital sinus: