State Darcy's law:
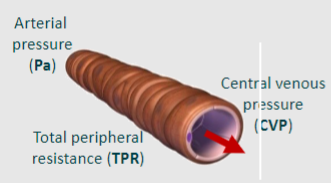
Flow = Pa-CVP/TPR
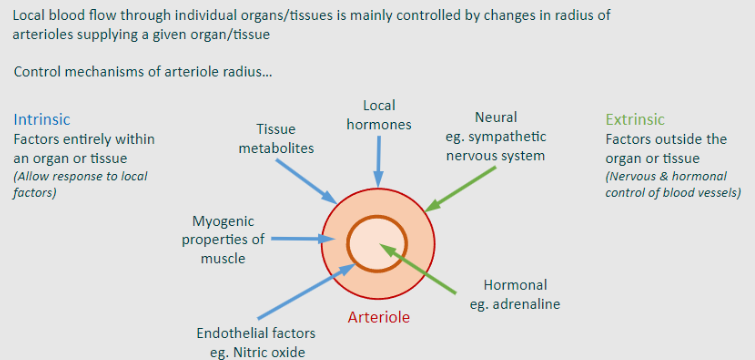
What controls TPR?
-Darcy’s and Poiseulle’s laws
-Myogenic response (reflexive contraction)
-Blood viscosity
Conductance (G) is the reciprocal of TPR. Can you write a formula that includes TPR and G?
G = 1/TPR
State a formula for flow that includes G?
Flow = Pa - CVP x G
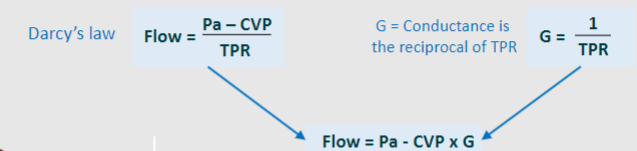
TPR controls blood flow and blood pressure. How?
Increase in resistance means need to increase pressure to keep same flow
How does resistance (TPR) affect the behaviour of arteries. Arterioles and the capillaries
-Decrease in TPR. Decreased blood pressure upstream, but greater capillary flow
-Increase in TPR. Increased blood pressure upstream, but less capillary flow
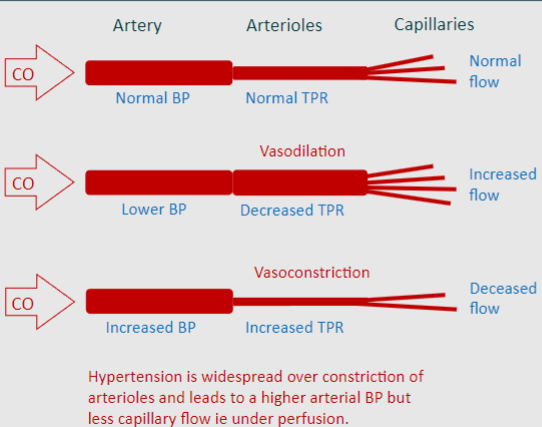
During exercise the superior mesenteric constricts, this leads to decreased flow to....?
The intestines
During exercise the Common iliac dilates, this leads to increased flow to....?
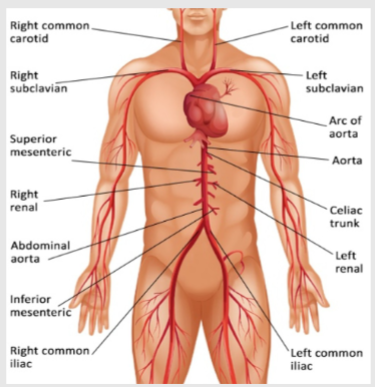
The legs
During sedentary activity the superior mesenteric dilates, this leads to increased flow to....?
The intestines
During sedentary activity Common iliac constricts, this leads to decreased flow to....?
The legs
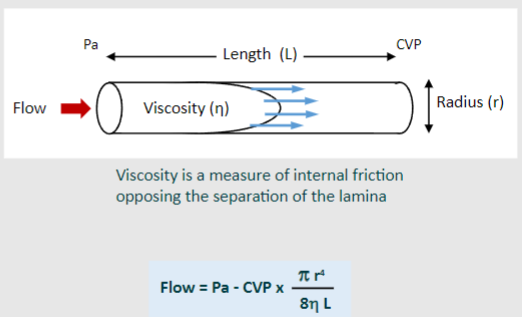
What is the equation for flow that includes viscosity?
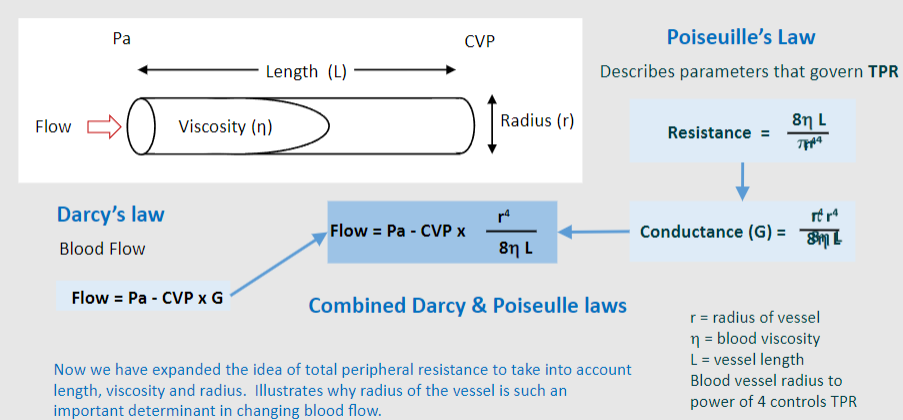
Flow = Pa -CVP x (r^4/8n L)
Picture demonstrating the r4 effect:
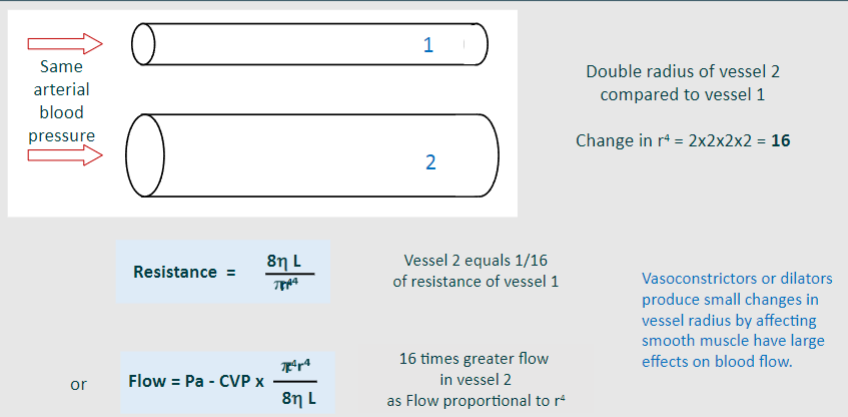
What does each term mean in this equation, Flow = Pa -CVP x (r^4/8n L)? (picture)
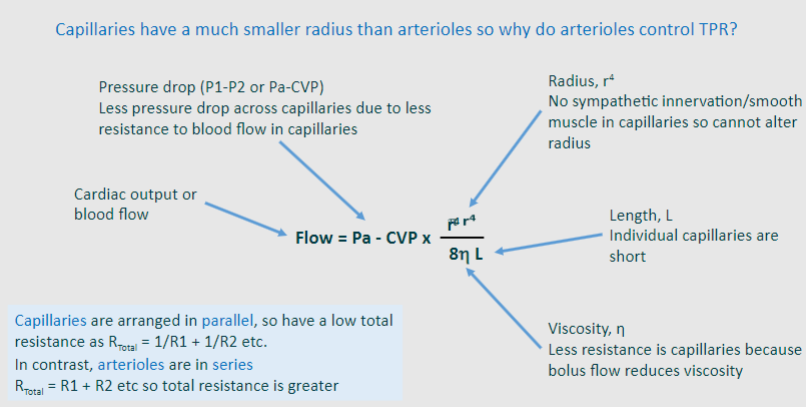
What vessel has the largest pressure drop? What is this pressure drop?
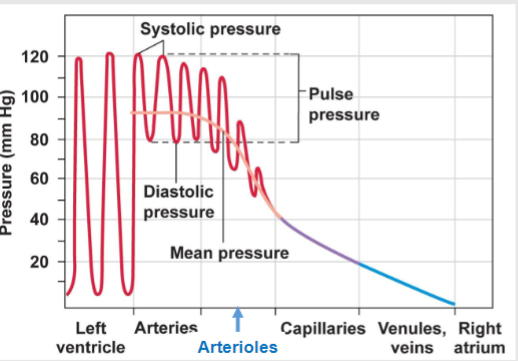
-Arterioles
-Pressure drop of 40-50 mmHg amongst vessels
Picture demonstrating the control of local blood flow (TPR) of the arteriole
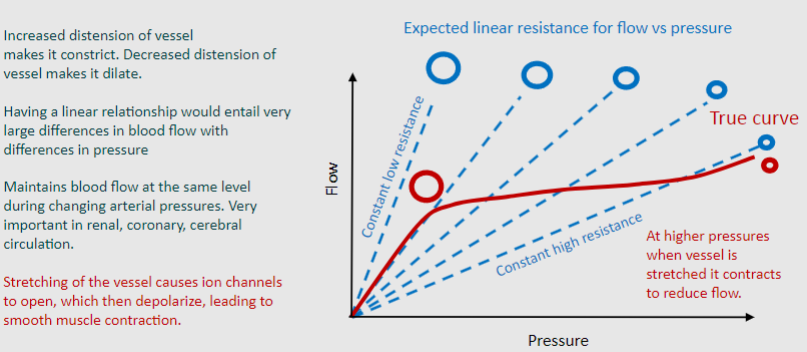
What does distension refer to?
Refers to the expansion or dilation of the vessel walls in response to increased pressure or volume of blood flowing through them
Increased distension does what to a blood vessel?
Makes it dilate
Decreased distension does what to a blood vessel?
Makes it constrict
Picture demonstrating the importance of Bayliss myogenic response (regulate their own diameter and thus blood flow in response to changes in blood pressure)
What does blood flow depend on? One starts with V..... (2)
-Viscosity of blood Vessel diameter
-Haematocrit
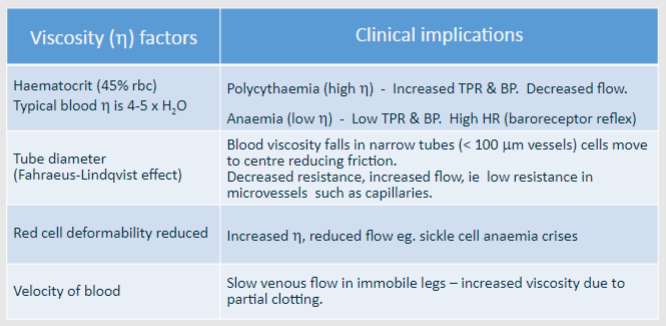
Picture showing viscosity (n) factors and mirroring clinical implications:
State some characteristics of the veins: (3)
-Thin walled, collapsible, voluminous vessels
-Contain 2/3rd of blood volume
-Contractile, so contain smooth muscle, innervated by sympathetic nerves but thinner than arterial muscle & more compliant (so form blood reservoir)
State, some information about the Volume of blood in veins & contractility
Contraction of vessels – Expels blood into central veins– Increases venous return/CVP/end-diastolic volume– Increases stroke volume (Starling’s law)
State some typical venous pressures:
Limb vein, heart level 5-10 mmHg
Central venous pressure (entering heart) 0-7 mmHg
Foot vein, standing 90 mmHg
At low pressures, what happens to the veins?

They collapse
At high pressures, what happens to the veins?

They distend
Where is venous pressure the highest?
The feet
Stimulation of sympathetic nerves causes vasoconstriction, which shifts blood centrally. What happens after this?
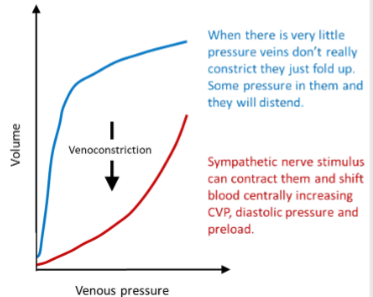
-Increases venous return, CVP & end-diastolic pressure
-Increased CVP increases preload and so increases
stroke volume (Starling's law)
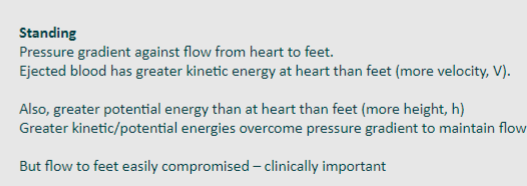
What Law explains arterial blood flow?
Bernoulli's Law
What is the Bernuolli's theory?
Mechanical energy of flow is determined by pressure, kinetic, potential energies (ρ = fluid mass)
What is the formula for energy that involves kinetics?
Energy = Pressure (P) + kinetic (ρV^2/2) + potential (ρgh)
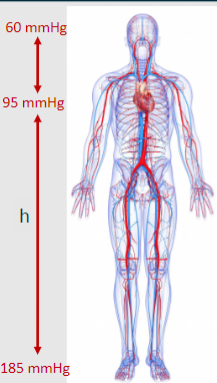
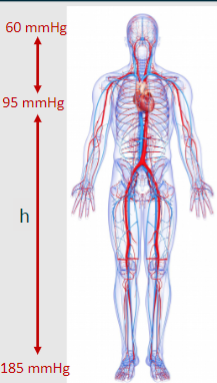
Some information of the importance of standing pressure:
What is the pressure at the feet, heart and head? (mmHg)
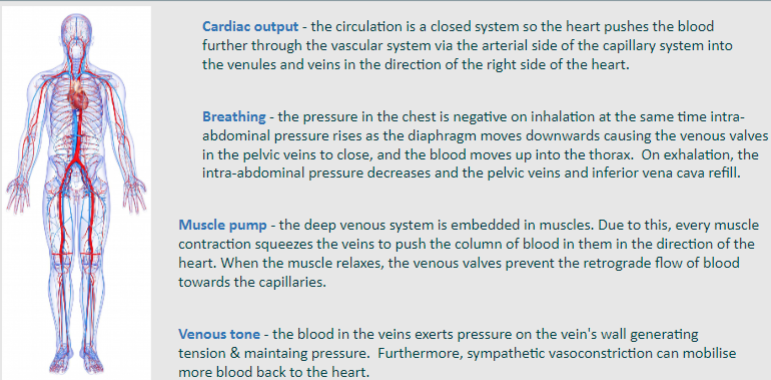
Picture demonstrating info about venous return in the parts; Cardiac output, breathing, muscle pump and venous tone.
What are 3 drugs that relate to vasodilation/vasoconstriction?
-Nitrates
-ARBs (Angiotensin receptor blockers)
-ACE inhibitors (Angiotensin Converting Enzyme Inhibitors)
What do nitrates do?
Causes vasodilation (lowers blood pressure)
What do ARB's do?
Prevent vasoconstriction by blocking the action of angiotensin II at its receptor
What do ACE inhibitors do?
Prevents vasoconstriction caused by ACE (Angiotensin Converting Enzyme)