What is the approximate body water composition in males and females? (2)
𖹭 Males: 60% water
𖹭 Females: 50% water
How much body water does a 70kg male and a 60kg female have? (2)
𖹭 70kg male: 42 L (0.6 x 70)
𖹭 60kg female: 30 L (0.5 x 60)
How is body water distributed between intracellular and extracellular compartments? (2)
𖹭 Two thirds of body water is intracellular (ICF)
𖹭 One third of body water is extracellular (ECF)
What are the intracellular and extracellular fluid volumes for a 70kg male? (2)
𖹭 Intracellular fluid (ICF) volume: 28 L (2/3 x 42)
𖹭 Extracellular fluid (ECF) volume: 14 L (1/3 x 42)
What are the intracellular and extracellular fluid volumes for a 60kg female? (2)
𖹭 Intracellular fluid (ICF) volume: 20 L (2/3 x 30)
𖹭 Extracellular fluid (ECF) volume: 10 L (1/3 x 30)
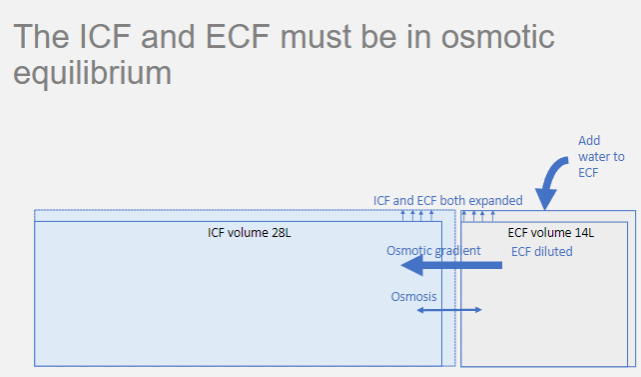
Why must the ICF and ECF be in osmotic equilibrium? (1)
𖹭 To prevent osmotic gradients that result in shifts of water between compartments
What is the permeability of the cell membrane? (2)
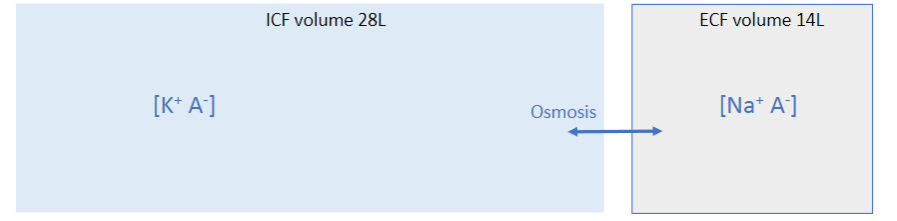
𖹭 Permeable to water (via water channels: aquaporins)
𖹭 Impermeable to most solutes
What happens when there is a change in solute concentration in either the ICF or ECF? (1)
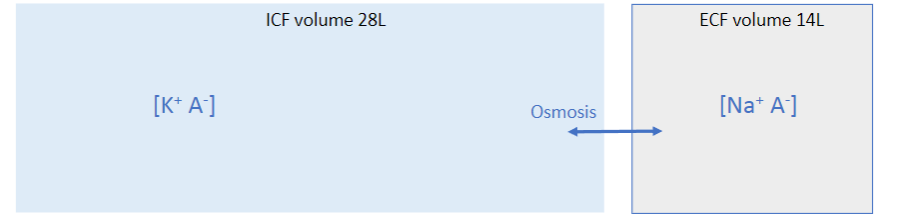
𖹭 It generates an osmotic gradient, resulting in shifts of water between compartments
Why is the osmolarity of the ECF regulated? (4)
𖹭 To avoid osmotic shifts of water between ICF and ECF volumes
𖹭 Normal range is 280-300 mOsm/L
𖹭 Large shifts must be avoided to prevent changes in cell volume
𖹭 The most serious complications are neurological
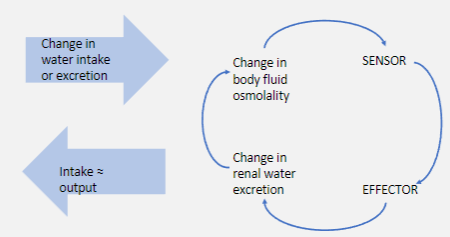
What is osmoregulation? (1)
𖹭 The physiological process that maintains constant ECF osmolarity
Why is regulation of the ECF volume important? (1)
𖹭 To ensure effective circulating volume
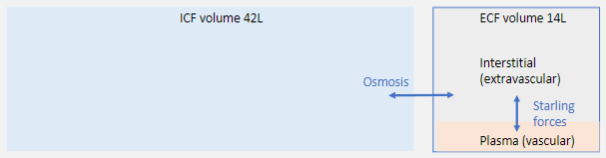
How is the ECF compartment subdivided? (2)
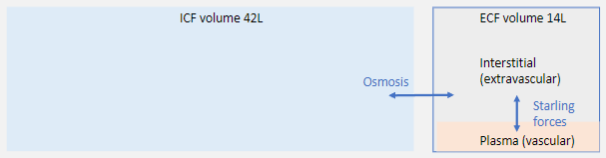
𖹭 Interstitial (or extravascular) compartment (about 75% of ECF)
𖹭 Plasma (or vascular) compartment (about 25% of ECF)
What is volume regulation? (1)
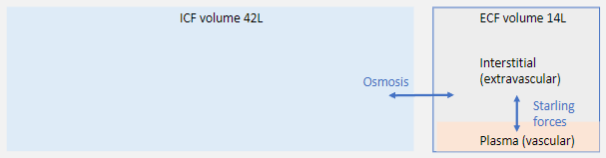
𖹭 The control of the ECF volume to ensure appropriate plasma volume (maintained by balance of Starling forces)
What is required to maintain salt and water balance? (1)
𖹭 Integration of osmoregulation and volume regulation
What is osmoregulation? (1)
𖹭 The control of salt concentration by adjusting the amount of pure water in the body
What is volume regulation? (1)
𖹭 The control of the amount of salt and water in the ECF and hence, ECF volume
Which organ is central to both osmoregulation and volume regulation? (1)
𖹭 The kidney
What is the central function of the kidney? (1)
𖹭 Homeostasis
What is the production of urine considered in relation to the kidney's central function? (1)
𖹭 A by-product of the kidney's central function of homeostasis
What are the renal functions? (7)
𖹭 Osmoregulation
𖹭 Volume regulation
𖹭 Acid-base balance
𖹭 Regulation of electrolyte balance (e.g., potassium, calcium, phosphate)
𖹭 Removal of metabolic waste products from blood
𖹭 Removal of foreign chemicals in the blood (e.g., drugs)
𖹭 Regulation of red blood cell production (erythropoietin)
What is the functional unit of the kidney? (1)
𖹭 The nephron
What does the nephron consist of? (2)
𖹭 Special blood vessels
𖹭 Elaborate tubules
How many nephrons are there per kidney? (1)
𖹭 1.25 million
What are the components of the renal tubule in the nephron? (6)
𖹭 Bowman's capsule
𖹭 Proximal tubule (proximal convoluted tubule, PCT)
𖹭 Loop of Henle
𖹭 Distal tubule (DCT)
𖹭 Collecting duct (CD)
𖹭 Collecting ducts join and ultimately drain into the ureter
What are the components of the blood vessels associated with the nephron? (5)
𖹭 Afferent arteriole
𖹭 Glomerulus
𖹭 Efferent arteriole
𖹭 Peritubular capillaries
𖹭 Vasa recta
What are the four basic processes of renal function? (4)
𖹭 Glomerular Filtration
𖹭 Tubular Reabsorption
𖹭 Tubular Secretion
𖹭 Excretion of water and solutes in the urine
What is glomerular filtration? (3)
𖹭 Glomerular filtration is driven by the balance of Starling forces across the capillary membrane.
𖹭 Small molecules pass readily, while large ones (proteins) and cells cannot pass.
𖹭 This leads to a plasma ultrafiltrate in the Bowman’s capsule, the first step in the production of urine.
What is glomerular filtration rate (GFR)? (4)
𖹭 Glomerular filtration rate is the amount of filtrate produced by the kidneys each minute.
𖹭 It averages 125 ml/min (approximately 20% of renal plasma flow).
𖹭 GFR is a very important clinical indicator, reduced in renal failure.
𖹭 Plasma creatinine can be used as an index of GFR
What is tubular reabsorption?
𖹭 Tubular reabsorption is the process by which many substances that are filtered are then reabsorbed from the tubular lumen into the peritubular capillaries.
Where does most of the reabsorption of salt and water occur?
𖹭 About 70% of filtered salt and water is reabsorbed from the proximal tubule.
How much of the filtered salt and water is reabsorbed from the loop of Henle?
𖹭 Approximately 20-25% is reabsorbed from the loop of Henle.
Where is the remaining 5-10% of filtered salt and water reabsorbed from?
𖹭 The remaining 5-10% is reabsorbed from the distal tubule and collecting duct.
What is tubular secretion?
𖹭 Tubular secretion is the process by which substances are actively transported from the peritubular capillaries into the tubular lumen.
Why is tubular secretion important?
𖹭 Tubular secretion is important for disposing of substances beyond their level in the filtrate, eliminating toxins and metabolic by-products.
What are the key roles of tubular secretion?
𖹭 Tubular secretion is important in potassium balance, as excess potassium (K+) is secreted in the distal tubule (DT) and collecting duct (CD).
𖹭 It is also crucial for acid-base balance, as H+ secretion occurs in the distal tubule (DT) and collecting duct (CD).
What happens to the tubular fluid after filtration, reabsorption, and secretion?
𖹭 The tubular fluid remaining after filtration, reabsorption, and secretion is excreted as urine.
How is the amount of solutes and water excreted in the urine calculated?
𖹭 The amount excreted equals the amount filtered minus the amount reabsorbed plus the amount secreted.
What is the significance of the equation for calculating the amount excreted in urine?
𖹭 If the amount reabsorbed and secreted are both zero for a substance, then the amount excreted equals the amount filtered. This can be used to estimate glomerular filtration rate (GFR).
How can GFR be estimated using this equation?
𖹭 For substances like creatinine, which are filtered but not reabsorbed, GFR can be estimated from their plasma concentration.
Picture demonstrating The ICF and ECF must be in osmoticequilibrium:
Picture demonstrating how the Osmoregulation depends on monitoringthe osmolality of the ECF:
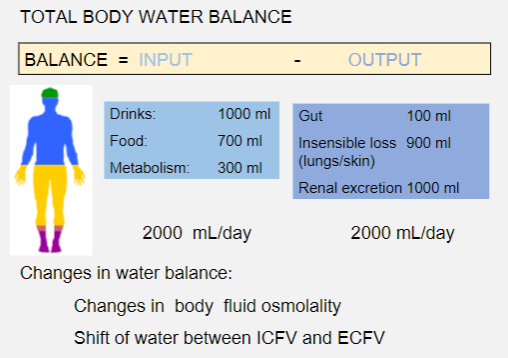
Picture demonstrating total body balance:
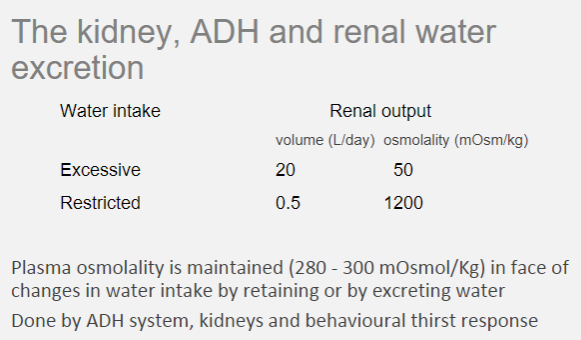
What happens in the physiological response to water restriction?
𖹭 Loss of water from the body, such as through the skin and lungs, leads to a rise in plasma osmolality.
What are the responses to increased plasma osmolality?
𖹭 The responses include increased thirst and increased secretion of antidiuretic hormone (ADH), also known as vasopressin.
How does ADH affect renal function?
𖹭 ADH increases renal water reabsorption, leading to decreased urine volume and increased urine osmolality.
What happens in the physiological response to an increase in water intake?
𖹭 There is an increase in water absorption through the gastrointestinal tract (GIT), leading to a decrease in plasma osmolality.
What are the responses to decreased plasma osmolality?
𖹭 The responses include decreased thirst and reduced secretion of antidiuretic hormone (ADH).
What are the results of reduced ADH secretion?
𖹭 Reduced ADH secretion leads to an increase in urine volume and a decrease in urine osmolality.
Picture demonstrating The kidney, ADH and renal waterexcretion:
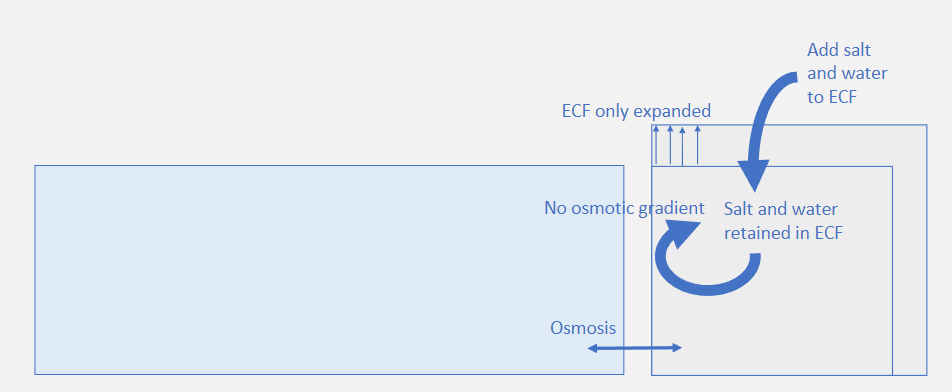
What determines the extracellular fluid (ECF) volume?
𖹭 The ECF volume is determined by the amount of sodium in this compartment.
What is necessary to maintain a constant ECF volume?
𖹭 Sodium intake and excretion must be balanced to maintain a constant ECF volume.
How is a fall in blood volume opposed?
𖹭 A fall in blood volume is opposed by hormonal signals promoting sodium retention, causing water to follow osmotically and restoring volume.
Where are the main volume sensors located?
𖹭 The main volume sensors are in the cardiovascular system.
Picture demonstrating The total amount of sodium in the ECFdetermines its volume:
Picture demonstrating how Sodium balance is required to maintainthe ECF volume:
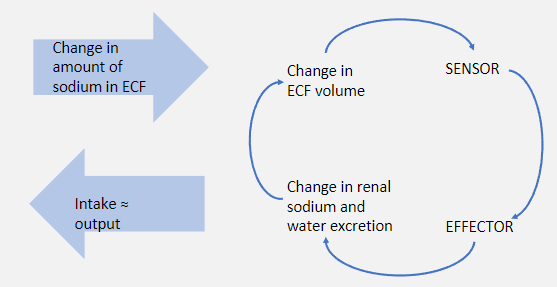
What is the role of the renin-angiotensin-aldosterone system (RAAS) in sodium balance?
The RAAS increases renal sodium reabsorption and increases extracellular fluid (ECF) volume.
What is the role of cardiac natriuretic peptides (ANP) in sodium balance?
𖹭 Cardiac natriuretic peptides (ANP) decrease renal sodium reabsorption and decrease extracellular fluid (ECF) volume.