Dr. Fiona Miller - Canadian Agency for Drugs and Technologies in
advertisement

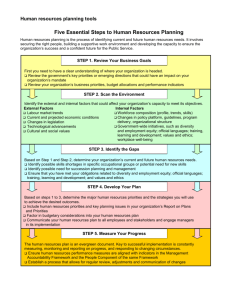
Improving the Appraisal of Non-Drug Technologies: Revising the Ontario Decision Framework Ethics & Social Values: Patient Centred Care Fiona A. Miller, PhD Associate Professor, IHPME Division of Health Policy & Ethics, THETA CADTH, Saskatoon April 14, 2015 Addressing Ethics & Social Values at OHTAC Decision determinants Public engagement PE #1 (2007-8) PE #2 (2012-2014) 2 Addressing Ethics & Social Values at OHTAC Decision determinants DD #1 (2007-8) • Johnson et al, Decision Determinants Committee #1: 2007-2008/9 - Nancy Sikich, Gerald Evans, William Evans, Mita Giacomini, Les Levin, Murray Krahn, Murray Glendinning, Paul Oh, Charmaine Perera 3 Ontario Health Technology Advisory Committee (OHTAC) Decision Determinants Addressing Ethics & Social Values at OHTAC Decision determinants DD #1 (2007-8) Subcommittee on social values & ethics (2011-2012) • Giacomini et al, Subcommittee on Social Values & Ethics Evaluation: Identification of core values relevant to OHTAC decision making (2011-2012) – Frank Wagner, Murray Krahn, Julia Abelson, Nancy Sickich, Kellee Kaulback 5 Giacomini et al, 2012Evidence-informed Quality policy Solidarity Resource sufficiency Resource stewardship Effectiveness Equity Economic Overarching Clinical Traditional in HTA Population health NOT Patient-centred care Traditional in HTA Collaboration Human rights, rule of law, etc. Canadian Health System • Canada Health Act • Romanow Commission • First Ministers’ Accord on Health Care Renewal • Health Council of Canada Ontario Health System • (No MOHLTC strategic plan) • Excellent Health Care for All Act • Ontario Health Plan for an Infuenza Epidemic • Ontario Health Quality Council Grounded in: Established values frameworks relevant to OHTAC’s jurisdiction Shared responsibility for health HTA (international ethics fwks) • EUNetHTA Core Model • INAHTA Working Group • (“Hoffman’s list”, IJTAHC) OHTAC • Mission Statement • Terms of Reference • Decision Determinants Framework • Public Engagement Subcommittee, 2007 • External reviews, 2005, 2008 • Citizen’s Reference Panel, 2010 Social values Six domains of social value 20 social values statements EQUITY#1: Access to health care should be universal among Canadians, and based on individual need. EQUITY #2: Individuals should not face discrimination on the basis of factors other than need. These include but are not limited to: ability to pay, wealth, province of residence, geographic location, origin, gender, or age. SOLIDARITY #1: The principle of solidarity recognizes the importance of relationships and interdependence for individual and societal flourishing. SOLIDARITY #2 Solidarity is related to other values such as equity, justice, collaboration, and shared responsibility for health. It also resonates with the familiar values of non-abandonment and compassion in clinical bioethics. SOLIDARITY #3: Solidarity entails sustaining strong, trusting, and compassionate relationships in the health system. These include relationships between patients and providers, between citizens and their government agencies, and others. SOLIDARITY #4: Solidarity also implies that conflicts of interest and externalities should be transparent and COLLABORATION #1: Health care is complex. Success depends on addressed. constructive collaboration between many providers, agencies, organizations, professionals, patients, and their caregivers. COLLABORATION #2: Mechanisms to support collaboration – whether legal frameworks, economic incentives, organizational structures, support technology, or others – should be regarded as integral and important aspects of health services. COLLABORATION #3: Health technologies should be analyzed in context, including attention to both their integral components and how they integrate with other aspects of health care. COLLABORATION #4: Policy makers should understand and consider health services’ (and technologies’) potential organizational, economic, and social impacts, and how these affect constructive 7 collaborations. Social values Six domains of social value 20 social values statements PATIENT-CENTRED CARE #1: Processes of care and positive patient experiences matter, in addition to health outcomes. PATIENT-CENTRED CARE #2: Patient burdens should be minimized and kept in proportion with benefits. PATIENT-CENTRED CARE #3: Health care services should be responsive to patients’ needs, values, and preferences. PATIENT-CENTRED CARE #4: Diversity in patient values should be expected, and accommodated within legal and pragmatic bounds PATIENT-CENTRED CARE #5: The dignity, rights, liberty, autonomy, and privacy of patients must be respected throughout the health care process. PATIENT-CENTRED CARE #6: Patient-centred care also entails respect and support for the roles of family members and other informal caregivers in generating the patient’s well-being. POPULATION HEALTH #1: The health system should serve the health of the population as well as the health of individuals. POPULATION HEALTH #2: Policy makers should consider implications of decisions for population health, prevention, and protection of the public from harm. SHARED RESPONSIBILITY FOR HEALTH #1: The health system holds partial responsibility for individual and population health. Additional responsibility rests on social factors, the environment, occupational settings, individual behaviours and lifestyle. SHARED RESPONSIBILITY FOR HEALTH #2: Consideration should be given to the role of not only the personal, but also the social determinants of health. 8 Addressing Ethics & Social Values at OHTAC Decision determinants DD #1 (2007-8) Subcommittee on social values & ethics (2011-2012) E&SV Working Group Economic Clinical DD #2 (2012-2014) • Krahn et al, Decision Determinants Committee #2: Revise decision determinants framework (2012-2014) - Mita Giacomini, Shawn Winsor, Frank Wagner, Fiona Miller, Ahmed Bayoumi, Ba Pham, Gabrielle Van Der Velde, Holger Schunemann, Ron Goeree, Nancy Sikich • Giacomini et al; Miller et al, Ethics & Social Values Working Group: Operationalize core values - Frank Wagner, Shawn Winsor, Juliana Yi, Celine Cressman (2014) 9 Operationalizing values as evaluative questions 1 Equity Interests Relationships Patient-centred care Population health Operationalizing values as evaluative questions 2 Equity Context-sensitive care Patient-centred care Evaluative questions Evaluative category Evaluative questions Equity Are there differences among equity-relevant groups* with regard to disease burden or access to care? Patient-centred care Describe patient experiences and preferences regarding the condition, as well as processes and outcomes of care? Have particular issues been identified relevant to ethical principles and rights in health care: autonomy and independence, vulnerability and dignity, privacy and confidentiality? Context-sensitive care Describe, if warranted, the potential effects on other health services or systems, in the short or long term - Setting precedents, establishing or diminishing clinical or organizational capacity, requiring new standards of practice for regulated health professionals, etc? Are there social or cultural pressures that affect the use of the technology - Tensions between the individual and their community, social stigma, or judgments of personal or social responsibility for poor or improved health? * Groups identified by MOHLTC HEIA Tool for equity considerations: Aboriginal peoples, Age-related groups, Disability, Ethno-racial communities, Francophone, Homeless, Linguistic communities, Low income, Religious/faith communities, Rural/remote or inner-urban populations, Sex/gender, Sexual orientation, “Other” 12 Test case for evidence-based E&SV analysis • Uterine fibroids – Benign tumors of the smooth muscle cells of the myometrium – Common • prevalence of 70% among white women in late 40s; 80% for black women, though are asymptomatic in most women. – Prevalence of clinically relevant tumors increases with age • 10-15% of white women in their 30’s and 35% of white women in their late 40’s. • 2-3 fold higher incidence rates for black women; earlier age of onset, over a greater age span; more severe disease at presentation and at surgery 13 Test case for evidence-based E&SV analysis • A range of treatment alternatives – Invasive • surgical interventions (myomectomy and hysterectomy) – Minimally invasive • various embolic and ablative therapies (embolization, radiofrequency, laser, microwave and cryoblation) – Non-invasive thermal ablation technology - MRgHIFU • magnetic resonance imaging (MR) for targeting and monitoring • high-intensity focused ultrasound (HIFU) for treatment Test case for evidence-based E&SV analysis • Research questions – What are patient values, preferences and expressed needs related to uterine fibroids and treatments for it? – What challenges exist in the provision of patient-centred care for uterine fibroids and how might these be affected by the availability of MRgHIFU? • Evidence review – Comprehensive review of relevant literature – systematic scoping review – 47 studies included in evidence synthesis • Primary studies of patients and providers – qualitative & quantitative • Epidemiologic and service utilization data (e.g., billing data, chart review, disease registry) • Findings across 4 thematic areas – – – – The burden of uterine fibroids The importance of values and preferences in treatment selection Challenges in delivering patient-centred care Challenges for health equity 15 Reorganizing evaluative questions Patient-centred care Equity Context-sensitive care Patientcentred care Patient-centred care Patient-Centred Care* Patient & public values Equitable & integrated care systems *Entwistle, V. A., & Watt, I. S. (2013). Treating patients as persons: A capabilities approach to support delivery of person-centered care. The American Journal of Bioethics, 13(8), 29-39. Patient-centred care Patient-Centred Care* Treating patients as persons, recognizing the relational nature of our autonomy Patient & • public values • • Not disease-centred Respectful and responsive to considered preferences, needs and values A positive and supportive respect, recognizing the social resources involved in formulating and achieving valued ends Equitable & integrated care systems *Entwistle, V. A., & Watt, I. S. (2013). Treating patients as persons: A capabilities approach to support delivery of person-centered care. The American Journal of Bioethics, 13(8), 29-39. Patient-centred care Patient-Centred Care* Treating patients as persons, recognizing the relational nature of our autonomy Patient & • public values • • Not disease-centred Respectful and responsive to considered preferences, needs and values A positive and supportive respect, recognizing the social resources involved in formulating and achieving valued ends Ensuring that health systems work to fairly serve the needs of populations of patients Equitable & integrated care systems • • • • Not staff or system-centred Integrated systems of responsive and respectful care Ensuring non-discrimination (not unfairly treating likes differently in the delivery of healthcare services) Seeking to overcome health inequities (remediating, where possible, avoidable, unfair and unjust differences in health outcomes) *Entwistle, V. A., & Watt, I. S. (2013). Treating patients as persons: A capabilities approach to support delivery of person-centered care. The American Journal of Bioethics, 13(8), 29-39. Ethics & Social Values at OHTAC AN EMERGING APPROACH 20 OHTAC Evidence Review Process 21 The stages of an HTA Vignette: Topic selection & scoping Ethics & Social Values Evidence based analysis Ethics & Social Values Appraisal: OHTAC Recommendations Ethics & Social Values Priority setting for HTA – Approach to E&SV Domain Patientcentred care Criteria Patient & public values Equitable & integrated care systems Ranking Unknown A B C Consistent with patient values & preferences Limited impact related to patient values/preferen ces Contrary to patient values and preferences Has the potential to improve the delivery of equitable and integrated care Limited impact on the delivery of equitable and integrated care May worsen the delivery of equitable and integrated care RANK • Incorporate the 2 main criteria proposed for the patient-centred care domain • Set at highest rank those technologies that promise to significantly improve patient-centred care 23 Scoping – Triggering evidence-based E&SV analysis • All mega-analyses should be accompanied by an evidence-based E&SV analysis • Review of a network of technologies provides excellent opportunity for considering patient-centred system of care • Evidence-based E&SV analysis to be triggered for other HTAs (e.g., single technology appraisals) on a case by case basis • Informed by: Institute of Health Economics, Edmonton, AB Report: Assessing the Need for and Quality of Ethics Analyses in HTA, October 18-26, 2013: 1-38. 24c Trigger checklist • Where use of priority setting tool identifies opportunities or challenges in addressing patient-centred care • Where treatments or outcomes are sensitive to patient preferences, values or needs • Where the patient population is vulnerable or marginalized – For example, ill children, individuals with impaired cognitive capacity, institutionalized persons, etc. – Marginalized by unfair or unjust health differences • Where the technology is proposed for use in healthy populations – Population screening; prophylactic interventions • Where the technology is ‘disruptive’ of existing services or systems – Changing health care delivery and disease management processes – Changing job prospects for health care providers – Requiring new capital equipment and infrastructure • Where the technology challenges legal or ethical commitments to patient autonomy, privacy or confidentiality 25 The stages of an HTA Vignette: Topic selection & scoping Ethics & Social Values Evidence based analysis Ethics & Social Values Appraisal: OHTAC Recommendations Ethics & Social Values Evidence-based E&SV analysis • Evidence-based E&SV analysis should involve a systematic review of research evidence • A consistent evidence-based approach to all relevant decision criteria • As appropriate, primary data collection or public engagement • PE Subcommittee 27 Suggested methodology • Suggested methodology for evidence review – Scoping review • Comprehensive and systematic search and selection • Not specific to any one research methodology (i.e., including qualitative studies but not only qualitative studies) • Quality assessment through assessment of relevance; use of quality prompts and exclusion for studies deemed critically flawed – Addressing multiple domains of interest to E&SV analysis - drawing on 3 non traditional approaches to research synthesis • Qualitative research – To illuminate social phenomena commonly captured by studies using qualitative methodologies: Patient (and other stakeholder) values, preferences and experiences; also social and cultural beliefs, perceptions of treatments and outcomes, implementation-relevant considerations • Health equity – To identify “differences in health outcomes that are avoidable, unfair and unjust.” (Welch et al, 2013, p2) • Health ethics – To identify the moral issues arising in technologies, technology appraisal, or technology use – Search strategy – PICo - intermediate level of sensitivity/specificity • Population, the phenomena of Interest, and the Context – Data extraction and analysis using criteria for E&SV appraisal 28 The stages of an HTA Vignette: Topic selection & scoping Ethics & Social Values Evidence based analysis Ethics & Social Values Appraisal: OHTAC Recommendations Ethics & Social Values Appraisal – Integrating E&SV • “Patient centred care” domain • Not to be completed unless evidence-based E&SV analysis undertaken • Summative judgment includes consideration of relevance and consistency of the evidence • Role of evaluative criteria • Influence decisions • Give reason for favouring/ disfavouring adoption • Inform implementation • Give guidance related to education, training, service design 30 Patient Centred Care Patient-Centred Care ✓ Check mark ("✓") indicates formal analysis completed. X mark ("✗") indicates no formal analysis completed. Do patients have specific values, preferences or needs related to the condition, treatment or life impact that are Aligned with patient values & relevant to this assessment? (NB. Values and preferences of preferences Patients: family, informal caregivers or the public to be considered, Values & as appropriate) Preferences Consistent with commitments Are there concerns regarding accepted ethical or legal to autonomy, privacy, standards related to patient autonomy, privacy or confidentiality confidentiality that are relevant to this assessment? Populations: Equity & Coordinated Care Enhances equity in access or outcomes Coordinates care SUMMARY Taking account of these considerations, select the degree to which the evidence supports the use of the technology(ies)/ intervention. Are there disadvantaged populations or populations in need whose access to care or health outcomes might be improved (or not worsened) that are relevant to this assessment? Are there challenges in the coordination of care for patients that might be improved (or not worsened) that are relevant to this assessment? Strongly supports Somewhat Neutral/ Does not Strongly supports Unknown support discourages Conclusion, 1 • At OHTAC, many efforts to to integrate ethics & social values into HTA: – Public engagement subcommittees – Decision Determinants subcommittees • Ethics & Social Values Working Group • Proposed methodology – Across stages of HTA – Based in set of social values – Involving clear conceptual framework & evidence review 32 Conclusion, 2 • Many questions remain – Evidence review • Have we asked the right questions? • Have we fairly and appropriately called attention to both – The preferences and values of individual patients? – The needs of populations of patients? – Evidence review relative to direct engagement • What is the value add? – Technology appraisal • What role does/ should these considerations play in HTA decisions? – Conducting evidence-based ethics & social values analysis • Is this the right methodology? • When should these reviews be done? 33 Acknowledgements E&SV Evidence review team Juliana Yi Celine Cressman Carolyn Barg Sarah Patton E&SV Working Group of DD Mita Giacomini (20122013) Shawn Windsor Frank Wagner Juliana Yi Celine Cressman (2014) • Decision Determinants Subcommittee – Murray Krahn, Chair – Ahmed Bayoumi – Ba Pham – Gabrielle Van Der Velde – Holger Schunemann – Ron Goeree – Nancy Sikich – Mita Giacomini – Frank Wagner – Shawn Windsor • Key HQO supports – Corinne Holubowich – Caroline Higgins – Gaylene Pron – Stephen Petersen