Anaphylaxis - Jacobi Emergency Medicine
advertisement

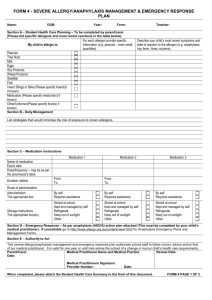
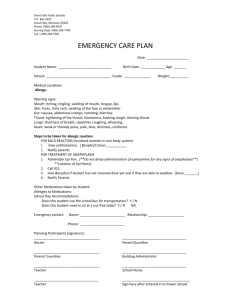
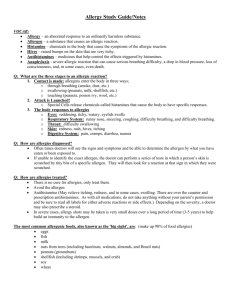
Anaphylaxis Anaphylaxis J Allergy Clin Immunol 2007;120:506-15 http://www.youtube.com/watch?v=VcxdqIPLyK8&list=PL7C80B961F004CBB8 Anaphylaxis Road Map Definition Pathophysiology Epidemiology Etiology Morbidity and Mortality Evaluation Treatment Dispo Ana- -phylaxis Ana- = again, up, back -phylaxis = protection, immunity, guarding 1902 + = 1902 + a few days + = Definition Clinically Meaningless: acute, severe, life-threatening, potentially fatal, multi-organ, systemic reaction caused by the release of chemical mediators from mast cells and basophils Definition Clinically Meaningful: When 1 of the following 3 criteria are fulfilled: 1. Acute onset of mucocutaneous signs AND 1 of the following: respiratory compromise (wheezing-bronchospasm, dyspnea, stridor, hypoxemia), hypotension (syncope), or hypotonia. 2. Rapid onset of 2 of the following after exposure to likely allergen: mucocutaneous signs, respiratory compromise, hypotension, or persistent gastrointestinal symptoms. 3. Hypotension after exposure to a known allergen. Pathophysiology Pathophysiology… for the ED doc Pathophysiology Type I Hypersensitivity Phases Pathophysiology Type I Hypersensitivity Phases Step 1: Sensitization “fool me once…” The allergen exposure allergen uptake by dendritic cells broken down into antigenic peptides peptides presented on T-lymphocytes cytokines are secreted from the T-lymphocytes -> B lymphocytes then directly interact with the Ts Bs produce antigen specific IgE which is packaged on the surface of mast cells (cell surfaces) and basophils (circulating) Pathophysiology Type I Hypersensitivity Phases Step 2: early-phase reaction Allergen re-exposure IgE on mast cell and basophil surfaces “recognizes” allergen degranulation releases histamine, tryptase, heparin) immediate symptoms at target organs (vasculature, skin, smooth muscle etc.) Step 3: late-phase reaction about 6 hours later, allergen stimulates T-cells to produce additional inflammatory mediators (ie. leukotrienes) resulting in inflammatory cell influx etc. etc. etc. Why me? Hypersensitivities are to substances – some people are predisposed to make IgE when exposed to these substances whereas “normals” make IgG (the activation of which would not result in hypersensitivity cascade) Or… Anaphylactoid reaction is an immediate systemic reaction that mimics anaphylaxis in end-point (mast cell and basophil degranulation) but lacks IgE’s involvement. Therefore, it can happen on first exposure. Typically “dose” dependant. Clinically indistinguishable from anaphylaxis. Epidemiology Very likely under-reported 1% of serious anaphylactic reactions result in death, or about 500-1000 deaths/year in the US Foods 100 -200 fatalities / year Beta Lactams (parenteral) 400 - 800 fatalities / year Radiocontrast 900 fatalities / year Insect stings 40 – 100 fatalities / year Latex 3 fatalities / year Desensitization injections about 3.4 fatalities / year Allergen testing 1 fatality reported between 1990-2001 Etiology #1: Food #2: Drugs – allergic reactions make up somewhere between 5-25% of all adverse drug reactions #3: Stinging insects Hymenoptera Apid (honeybee, bumblebee) Vespid (yellow jacket, hornet, wasp) Formicid (fire ant) #4: Latex #5: others (ie. exercise, idiopathic etc) Adverse Drug Reactions WHO definition: All nontherapeutic consequences, with the exception of treatment failures, purposeful or accidental poisonings, and drug abuse. All allergic reactions are ADRs, but not all ADRs (nausea, diarrhea, malaise) are allergic reactions, so clarify with your patient what their “allergy” really is. Adverse Drug Reactions Immediate hypersensitivity (IgE) Nonimmediate allergic reactions (not IgE, typically) SJS TEN Nonimmunological reactions Anaphylactoid Nonspecific histamine release (morphine itch, vanco red man) Bradykinin accumulation (ACE-I angioedema) Complement activation (radiocontrast) Leukotrienes (NSAIDs) DDx Anaphylaxis / Anaphylactoid Neurocardiac reaction (fancy pants for Vasovagal) Other Shock classes (cardiogenic, hemorrhagic, septic) “Flush” syndromes (carcinoid, medullary thyroid carcinoma) “Restaurant” syndromes (Scrombroid, MSG) Excess endogenous histamine production (things with big names) Nonorganic (nuts, the psych kind) Other (ACE-I, C1 esterase difficiency, pheos) Symptoms Definition J Allergy Clin Immunol 2006 ;117 : 391-7 Clinically Meaningful: When 1 of the following 3 criteria are fulfilled: 1. Acute onset of mucocutaneous signs AND 1 of the following: respiratory compromise (wheezing-bronchospasm, dyspnea, stridor, hypoxemia), hypotension (syncope), or hypotonia. 2. Rapid onset of 2 of the following after exposure to likely allergen: mucocutaneous signs, respiratory compromise, hypotension, or persistent gastrointestinal symptoms. 3. Hypotension after exposure to a known allergen. Criteria 1 : skin lesions and/or mucosa lesions (urticaria, itching or erythema, lip edema or tongue-uvula edema). With one or more or following signs : Respiratory troubles (dyspnea, bronchospasm, stridor, decreased of peak flow, hypoxia) Systolic BP<90 mmHg) or organ dysfunction (hypotonia, syncope, incontinence) Criteria 2 : 2 or more signs after exposition to a probable allergen: skin lesions and/or mucosa lesions (urticaria, itching or erythema, lips edema or tongue-uvula edema). With one or more of the following signs : Respiratory troubles (dyspnea, bronchospasm, stridor, decreased of peak flow, hypoxia) Systolic BP<90 mmHg) or organ dysfunction (hypotonia, syncope, incontinence) Persistent gastrointestinal troubles (abdominal pain, vomiting) Criteria 3: hypotension, know exposure Decrease of SBP< 90mmHg or more than 30% compared to basal in adults* after exposition to known allergen. *In child decrease of SBP is defined as: SBP < 70 mmHg from 1 month to 1 year, below (70 mmHg + [2 x age]) from 1 to 10 years, <90mmHg from 11 to 17 years. Symptoms Up to 35% of circulating volume can be displaced extravascularly within just 10 MINUTES of symptom onset Most cases have cutaneous findings A few cases do not Cutaneous 90% Respiratory 50% +/- 10% Cardiovascular (dizzy, syncope, low BP) 33% GI 25-30% Other Sxs (HA, chest pain, Sz) <8% Diagnostic Tests Yeaaaaah… For the inpatient team, you could send serum tryptase levels (which obviously peak between 60-90 minutes) Treatment Which of the following are first line agents for the treatment of anaphylaxis (select all that apply)? a. IV Corticosteroids b. PO Corticosteroids c. Parenteral Epinephrine d. Nebulized Beta agonists e. Oral Antihistamines f. IV Antihistamines Treatment Treatment Treatment AIRWAY Control it early (waaaaay easier to explain to an alive patient why they maybe didn’t need it then to explain to the family why the deceased, in retrospect, did) Standard of care is NOT to call ENT to look at larynx. You either look at the larynx yourself or you make a call based on symptoms (Voice change, respiratory distress, etc. One day, ultrasound) Many difficult airway devices will not work LMA – nope Combitube – eh eh Things to have: Bougie Tubes many sizes smaller than you typically use Fiberoptics (but Bougie + Glidescope pretty good too) ½ dose Etomidate without paralytic for “awake” intubation Crich tray or kit (seldinger) ENT, Anesthesiology (time permitting, don’t be proud, be smart) Treatment CIRCULATION (and A and B) Be vigilant for tachycardia (brady and other dysrhythmias can sometimes also happen), hypotension, etc. IV fluids – lots of them Epinephrine – Dr. House says, “Don’t be a….” Treatment - Epinephrine Study #1: 13 fatal or near-fatal cases of anaphylaxis of 6 who died, only 2 received epi within 1 hour of sx onset of 7 who survived, 6 received epi within 30 minutes Study #2: there were others, but I lost them, so here we are…. Delay in epi administration also associated with higher rate of biphasic reactions No placebo controlled allowed, so keep all your snooty journal club whining to yourselves Treatment - Epinephrine Treatment - Epinephrine BEST ROUTE = IM to the anterolateral middle third of the thigh with a needle long enough to reach MUSCLE SubQ unreliable absorption IV unless you need it, that sh$&% will kill you (virtually ALL adverse outcomes resulted from IV administration) Epi Dosing Adults IM 0.2 – 0.5mg Literature suggests that you go big (0.5 -1mg) or go home Peds IM 0.01mg / kg up to a max of 0.3mg IM solution is the 1:1000 one (which means 1gm /1000mL 1000mg / 1000mL 1mg in 1mL 0.5mg = 0.5mL Do this once. In five minutes, if necessary, do it again. Then draw up a third and mix up the IV epi for when the third fails. IV dosing is not well established Want to hear something scary? Multicenter study found: fewer than 25% of “serious reactions” received epi fewer than 16% discharged with Rx for epi-pens but.. 72% received antihistamines 48% systemic steroids 33% Nebs Another study: only 5% of housestaff new appropriate route and dosage Who SHOULDN’T get Epi? ABSOLUTELY NO ABSOLUTE CONTRAINDICATIONS! It IS safe (IM, anyway)…. A study of epi used in asthma exacerbations demonstrated safety in patients ages 15-96 years HOWEVER… … in patients using beta blocker, may get unopposed alpha, so some advise half-dose epi Take away the beta… Antihistamines H1 Blockers SECOND LINE, NEVER THE SOLE TX OF ANAPHYLAXIS SLOW ONSET (effects take 30 – 45 min to start) WORK TO PROHIBIT FURTHER DEGRANULATIONS, NOT TREAT THAT WHICH HAS ALREADY OCCURRED! H2 Blockers SECOND LINE Sound data to support use (randomized, double blind, placebo controlled) Corticosteroids SECOND LINE JOINT TASK FORCE IN ALLERGY blah blah and blah says, “systemic corticosteroids have no role in the acute management of anaphylaxis because they might have no effect for 4 to 6 hours, even when administered intravenously.” Never validated in placebo controlled trials, nor have standard dose, route, or type been proven superior But, duh European recs: 200 mg hydrocortisone IM or IV “following the initial resuscitation of the patient” Glucagon For either refractory or Beta-blocked patients Stimulate cAMP production (like Epi does) but via a different nonbeta-blocked receptor 1 – 5 mg IV over 5 minutes (peds = 20-30 microg / kg, max 1mg), then IV infusion of 5 – 15 microg / min titrated to response Other Nebs Terbutaline Vasopressin – evidence supports Other vasopressors Disposition DISPO Observe for at least 6 hours (8 appears better) from the time of symptom IMPROVEMENT, not onset Biphasic reactions occur in 5 – 20% of cases Latency period highly variable but nearly always within 72 hours Retrospective study of 164 cases of fatal anaphylaxis showed that vast majority of deaths occurred within 4 hours, all within 6 Dispo Extend observation and consider admission for: Asthmatic component of reaction History of biphasic reactions Continuing absorption of allergen Poor access to emergency care Overnight or alone at home Severe reactions with slow onset Unable to use epi-pen Admit Anyone not cardiorespitorily perfect after 8 hours BEFORE DISCHARGE, ALWAYS Clear instructions to return PRN and what constitutes PRN Rx for 3 days (72 hours for a reason) of antihistamine and steroids EPI-PEN x2 (either in their hand or RX able to be filled immediately Instructions how to use the epi-pen Follow up appointment / plan Among MDs who commonly rx epi-pens, only 25% correctly demonstrated the proper technique for use, only 24% knew it was available in 2 dosage forms ACE-Inhibitor Angioedema 0.1%- 0.5% of users (more so in A-As, ACE-I cough more so in Asians) Likely inhibition of ACE breakdown of bradykinin, a potent vasodilator Usually localized to head, neck Lacks cutaneous features of true allergy Anaphylaxis Tx never proven effective (epi, roids, H1&2s), but airway control has FFP replenishes ACE levels (class II) Icatibant (not likely available) specific bradykinin B2 receptor inhibitor (Class II, off-label use) ACE-Inhibitor Angioedema In one retrospective study of angioedema, ACE-I were responsible for 1/3 of events. Of those: Nearly half warranted ICU admission One-third required definitive airway So, they recommended outpt or obs for sxs limited to face, lips, soft palate Inpt for lingual edema, ICU for posterior lingual or laryngeal edema (whether visualized or based on sxs of stridor, dyspnea, voice change) C1 Esterase Inhibitor Deficiency 2 Forms Autosomal dominant Acquired (often associated with lymphoproliferative and autoimmune dzs) also De Novo mutations C1EI modulates complement activation, but it also helps regulate bradykinin formation Lack of Inhibitor means more bradykinin (ACE-I = inability to breakdown brady) (C1EI def = inability to slow creation) Recurrent episodes of well-circumscribed, nonpruritic angioedema May involve Gi and respiratory tracts (unexplained, recurrent abd pain) FFP, C1EI concentrate (both Class II) Penicillin and Cephs Shared beta-lactam structure “10% cross-reactivity” = from 1970s, 1st gen cephs which later were found to have trace amounts of PCN in them! (derived from same mold) New data suggest side chains may be more important than beta-lactam ring AAP recently endorsed use of 2nd gen and 3rd gen Cephs for otitis in PCN allergic peds as long as prior reaction was not hypersensitivity type 1 (fewer than 10% of those claiming PCN allergy have Type 1) All in all, risks of serious reaction to 2nd or 3rd Ceph in a pt with a selfreported / non-skin tested PCN allergy are low (perhaps <1% but realistically type 1 reaction to any given abx is 1-3% Radiographic Contrast Materials ANAPHYLACTOID (and therefore dose dependent, no IgE) Maybe some IgE cases Related to the osmolarity of the solution, now everyone uses safer “low osmolarity” (3.1% adverse rx, 0.04% severe) some using even safer “isoosmolar” No absolute contraindication History of Iodine-containing food allergy is NOT predictive (another 1970s study gone awry) RFs = hx of one, atopy / asthma, Beta blockade, CAD Tx Sxs like any other allergic / anaphylactic reaction Pretreatment appears to reduce event likelihood by 10-fold