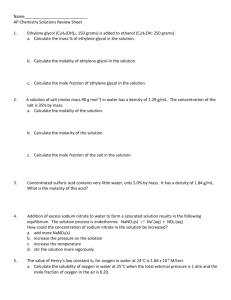
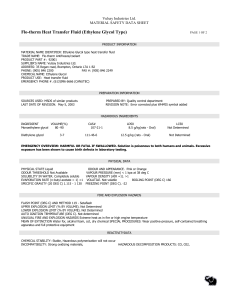
glycol
advertisement

Maurice Glenn Turner, a police officer in Cobb County, Georgia, went to the emergency room on March 2, 1995, complaining of flu-like symptoms. He was treated there, and when he felt better, he went home. The next morning, he was found dead. Dr. Brian Frist, the local medical examiner, found nothing abnormal except for left ventricular hypertrophy. He signed Glenn’s death out as “some complication related to an enlarged heart.” At this point, what is your differential diagnosis? Officer Glenn’s widow Lynn, a 911 dispatcher, collected around $153,000 in death benefits. Within a few days, she leased an apartment with her boyfriend, Forsyth county sheriff’s deputy Randy Thompson, who later also became a fireman. They did not marry, but they had a son in 1995 and a daughter in 1998. Fireman Randy insured himself for $200,000. The relationship ran into problems because of Lynn’s extravagant spending habits. Randy moved out and Lynn went into debt. However, he continued to visit her. On January 21, 2001, Randy went to the emergency room for a severe stomachache and vomiting. He was treated and released. Lynn made Randy some green Jell-O to help him settle his stomach. The next morning, he was found dead. Dr. Mark Koponen, the local medical examiner could find nothing wrong except for some crystals in the kidneys and some coronary artery atherosclerosis. He signed it out as sudden coronary death. At this point, what is your differential diagnosis? Fireman Randy’s girlfriend Lynn collected around $36,000 in death benefits. Officer Glenn’s mother read about Fireman Randy’s death in the newspaper. She contacted Fireman Randy’s mother. Both families felt that something was not right. They talked with Dr. Koponen, who sent blood and urine to forensic toxicologist Chris Tilson. Blood samples are routinely tested by several methods, including gas chromatography, which picks up voltaile acids and alcohols. Dr. Tilson found ethylene glycol, but not in quantities sufficient to cause death. He sent more samples to National Medical Services, a forensic reference lab. NMS found toxic levels of ethylene glycol. Dr. Koponen changed the cause of death to ethylene glycol poisoning. Dr. Frist exhumed Officer Glenn and found lethal levels of ethylene glycol as well. Julia Lynn Turner was indicted for Officer Glenn’s murder in 2001, and stood trial in May, 2004. A veterinary nurse described how Lynn had asked her in detail about the effects of antifreeze on cats. Other witnesses testified that she said she only cared about the insurance money, and that Officer Glenn had remarked that he was afraid she would try to kill him. The jury also heard about Fireman Randy’s cause of death. Toxicologist Chris Tilson explained his own error – a misplaced decimal point. Manufacturers testified that their embalming fluids did not contain ethylene glycol, thereby refuting the defense’s only real argument. Dr. Kris Sperry, the chief medical examiner for the Georgia Bureau of Investigation, made the clinical correlations. Dr. Frist, the original medical examiner, described some experiments that he had done. Lime Jell-O and Gator-Ade can be laced with ethylene glycol without significantly changing the look or taste. Lynn was found guilty of murdering Officer Glenn with malice. She got life in prison. Ethylene Glycol Because of its low molecular weight and the fact that it will not boil off, ethylene glycol is a superb antifreeze. It is odorless, colorless, and sweet-tasting. Fluorescein is added to antifreeze in the US, and it will appear in the urine if ethylene glycol has been ingested, alerting doctors. Around 90,000 animals and 4000 humans ingest ethylene glycol each year in the US. Here, Mark Trail’s dog Andy is shown discovering a pool of antifreeze. The problems develop when the molecule is metabolized to the three potent acids – glycolic acid, glyoxylic acid, and oxalic acid. Calcium oxalate crystals are familiar, and in ethylene glycol poisoning, they cause renal damage and appear in the urine. Here’s a touch prep from the kidney of a dog that died of ethylene glycol poisoning. The crystals are birefringent. It is probably these crystals that do the mechanical damage to brain and kidney. Always take a moment to calculate the anion gap. By custom, Na – Cl – HCO3 Normal range is 8-16 mEq/L Anion gap above 16 mEq/L? Remember: ketoacidosis lactic acidosis (shock / exertion) aspirin poisoning ethylene glycol poisoning uremia isopropanol, isoniazid, other Rx’s certain uncommon metabolic illnesses Treating ethylene glycol poisoning: Support Bicarbonate Ethanol (slows metabolism) Dialysis How do you do it? There have been other instances of criminal poisonings. On July 7, 2004, Maryann Neabor, an emergency medical technician, fatally poisoned her former brother-in-law with ethylene glycol in pineapple juice. James Keown, a Jefferson City, Missouri, radio personality, was arrested on the air in 2005. He is charged with chronically poisoning his wife, Julie, for her insurance money. In 2004, Maureen Plambeck was charged with poisoning her former sister-in-law with antifreeze in Margarita mix. The victim recovered. The defense was that she was trying to save the life of another family member. Scooby was a golden retriever in Albuquerque who was maliciously poisoned with ethylene glycol. Scooby got his due in April 2005, when New Mexico joined California and Oregon in mandating that a bitter-tasting compound be added to antifreeze. Two ethylene glycol molecules linked as an ether is diethylene glycol. This is a sweet, syrupy liquid that is somewhat less toxic than ethylene glycol, but still not good to ingest. Exactly how it does damage remains unknown. Diethylene glycol is the main ingredient in “Sterno.” It was the deadly ingredient in the 1938 sulfanilamide disaster in the US… Raspberry flavor Unfortunately, delicious … and the 1995-6 Haitian acetaminophen catastrophe. In 1985, some Austrian winemakers turned “dry” wine to “sweet” wine by adding diethylene glycol. One would have had to drink two bottles daily for a week to get sick, but this was still bad business. Regulations followed. This tale gave rise to the urban legend that the French had put antifreeze in wine. An 1990 episode of “The Simpsons” commemorated this. The Crepes of Wrath Bart became a hero for exposing a plot by French winemakers to add antifreeze to their wine. “Sierra” is propylene glycol. Much less toxic, but more expensive, it appeals to motorists who are concerned about animals. It’s also not quite so good an antifreeze. Why not? Okay. There’s more. Ryan Stallings: Three month old white male brought to Children’s Hospital, St. Louis, July 1989 1 day history of feeding intolerance followed by increased lethargy and tachypnea In the Cardinal Glennon Children’s ER, Ryan was found to have pH 7.02 Anion gap 26.3 Bicarb 3 mMol/L Ketonuria At this point, what is your differential diagnosis? On the second hospital day, St. Louis U’s toxicology lab reported: Serum Acetone 3700 umol/L = 215 mg/L Blood Ethylene Glycol 180 mg/L Smith Kline Beecham, an independent lab, confirmed the presence of deadly levels of ethylene glycol. Your lecturer led the College of American Pathologists’ team that did this lab’s inspection a few years ago. Ryan improved, but continued to be lethargic and to feed poorly. The physicians believed the child had been poisoned, and he was placed in a foster home. On September 1, Ryan’s mother Patricia was allowed a supervised visit, and fed him with a bottle. On September 4, Ryan was hospitalized again, with lethargy, muscle spasms, and hyperventilation. His pH was 6.9. He was treated with IV ethanol, but died soon afterwards. St. Louis Hospital’s lab found 119 mg/L of ethylene glycol in his blood. Smith-Kline confirmed this by gas chromatography. St. Louis also reported that “traces of ethylene glycol” were found on the bottle. Patricia Stallings was arrested for murder. Patricia Stallings spent the next seven months in jail, and then gave birth to a second son, David Jr., who was put in foster care. Within two weeks, David became acidotic and unresponsive, and was hospitalized. He was found almost at once to have vitamin B12-unresponsive methylmalonic acidemia. Methylmalonyl-CoA mutase is required to transform L-methylmalonyl-CoA into succinyl-CoA. If the enzyme is missing… Methylmalonic acid is elevated in the blood… … as is propionic acid (its decarboxylation product) and its various secondary metabolites. Of course, there was talk about a lab error and a death from a metabolic disorder. The state did its homework. Before the trial, the prosecutor actually asked Dr. Christopher Long to turn over a sample of Ryan’s blood to the local subspecialty lab. Dr. James Shoemaker, who ran the lab, found a large amount of methylmalonic acid, plus traces of ethylene glycol. Dr. Shoemaker presented this information at a conference. The team decided that little Ryan probably did indeed have methylmalonic acidemia. But they concluded that it was still ethylene glycol poisoning, because of the crystals in the brain and the presence of ethylene glycol in the bottle. They had the idea that the ethylene glycol in Ryan’s blood had “dissipated” in storage. Patricia Stalling’s lawyer did not attempt to obtain any expert support for the idea that Ryan’s death was not due to ethylene glycol poisoning. Patricia Stallings was convicted of murder. “Unsolved Mysteries” got ahold of the case. Dr. William Sly, chief of Biochemistry at SLU, watched the show and got together with Dr. Shoemaker. They went back to the specimens, and used a more sophisticated technique… … coupling a Hewlett-Packard 5890 gas chromatograph … … to a VG mass spectrometer. Gas chromatography…. Solid line is Ryan Stallings Dotted line is normal serum + 900 mg/L ethylene glycol Gas chromatography…. Solid line is Ryan Stallings spiked with ethylene glycol, no IS Dotted line is Ryan Stallings with internal standard Mass spectrum for ethylene glycol Mass spectrum for propionic acid The two fragmentation patterns are not at all similar. There was actually NO ethylene glycol in the blood. The old gas chromatograph technique mistook propionic acid for ethylene glycol. Huge amounts of propionic acid, plus methylmalonic, acetic, b-hydroxybutyric, and b-hydroxyisovaleric acids proved the diagnosis of methylmalonic acidemia. The prosecutor still could not explain the crystals in the brain. He contacted Yale’s Piero Rinaldo, who knew the answer. Everybody had overlooked the obvious. Babies metabolize big doses of ethanol into oxalic acid. The “ethylene glycol” on the bottle turned out to be residue from the ethylene oxide used to sterilize collection equipment. In an unprecedented move, the prosecutor asked the judge to declare trial counsel incompetent, and order a new trial. The prosecutor then dropped the charges, and Patricia Stallings was freed. Okay. There’s more. A previously healthy 6 month old girl was admitted to a community hospital. Mother had noted decreased activity, increased irritability, poor feeding, and decreased urination over 3 days. On the day of admission, the child had begun to vomit and become lethargic, pale, tachypneic, and hypotonic. Admitting labs: pH 7.12 pCO2 12 torr pO2 320 torr Bicarb 4 mmol/L Anion gap 24 UA: 100-120 rbc/hpf, 3-8 wbc/hpf Tox screen did not show ethylene glycol. At this point, what is your differential diagnosis? The community hospital sent the child to Mass General, where the anion gap and all the other abnormal labs were normal by the next day. All cultures were negative. The blood showed a very high level of glycine. Urine contained traces of three dicarboxylic acids (adipic, suberic, and octenedioic). The folks at Mass General were much too clever to fall into the trap of assuming this was ethylene glycol poisoning. They expected that with the Stallings fiasco, there would be no faulty reporting about ethylene glycol! They decided this must be another curious genetic disorder causing a metabolic acidosis, perhaps one that had never been reported. They decided to “wait and see.” Six days later, the child was back at the community hospital with the same symptoms. pH was 7.18, bicarbonate was 7, and anion gap was 28. The child was given bicarbonate and sent back to Mass General, where everything rapidly reverted to normal. Despite a lot of assays, all turning out normal, the Mass General team decided she had some disorder of fatty acid metabolism, and placed her on a low-fat diet. Two months later, she was back at the community hospital with the same abrupt onset of the same symptoms and lab findings. This time, she was transferred to Children’s in Boston. Children’s checked the urine for organic acids. It was loaded with glycolic acid and some unidentified peaks. Blood glycine was three times normal. Serum collected on the day of admission turned out to contain high levels of ethylene glycol. Really. It turned out that, unbeknownst to the community hospital and Mass General, the toxicology screens did not include ethylene glycol among the substances for which they searched. The district attorney and social services people investigated. The parents fired the baby-sitter “whose work schedule paralleled the onset of illness.” A bottle of infant formula in the refrigerator contained 220 mg/dL of ethylene glycol. There was none in the lot of formula from which this had been obtained. The child has had no sequelae. What did we learn?