physician order sheet STAT order Sheet Standing order Sheet
advertisement

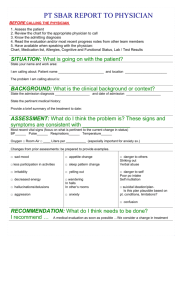
Chapter 16 Nursing Documentation medical and nursing documents A client's medical record client's record Temperature sheet Physician’s order sheet special nursing record chart , etc. Change-of-shift report (病室交班报告) Section 1 Record and Administration of medical and Nursing Documents Purpose of Records Principle of Records Administration of Medical and Nursing Documents Purpose of Records Providing Information Providing Data for Education and Research Providing Basis for Quality Review Providing Basis for Legal Purpose Principles of Records 1 2 3 4 5 Timely Objective and Accurate Complete Concise Legible 1 Timely • follow the hospital’s requirement to make documentation at regular intervals. •No recording should be done before providing nursing cares, and delaying or omitting the recording is not acceptable either. 2 Objective and Accurate Recording must be accurate and correct. Accurate recordings consist of facts or observations rather than opinions or interpretation. 3 Complete • The client's name, age, and bed number, should be written on each page of the record. •Leaving no blank lines on the client's chart. •the caregiver must sign his or her full name after recording. •a client's condition is critical. • a client insists on refusing a treatment or leaving the hospital against medical advice. •a client has inclination of committing suicide. these situations must be filled in the client's chart. 4 Concise Documentation must be concise, in a logical order, and lay stress on key points. 5 Legible • All entries must be legible and easy to read. • When a recording error is made, draw a line through it and write the corrector's name above it. • Do not erase, blot out, or use correction fluid. Administration of Medical and Nursing Documents Administration Requirements Arrangement Order of Medical Record Administration Requirements All medical and nursing documents should be placed according to organization guidelines. They should be replaced after being read or recorded. Medical and nursing documents must be kept neatly, orderly, completely and prevent them from being contaminated, mangled, disconnected and lost. The client or the client's family should not read the medical and nursing documents freely. No carrying the documents out of the ward without being permitted. If the documents need to be carried out of the ward for the purpose of medical activity or copy, it should be carried and kept well by hospital appointed staff. All the documents should be kept properly. When the client is discharged from the hospital, temperature sheet, physician’s order sheet and special nursing record chart will be kept permanently in Medical Recording Room of the hospital as parts of the client's casenotes. The change-of-shift report will be kept at least one year at the ward level. Arrangement Order of Medical Record Order of Admission Record Order of Discharge (transfer, death) Record Order of Admission Record • • • • • • • • • • • Temperature sheet Physician’s order sheet Admission sheet and record medical history and physical examination Physician's record Consultation record Diagnostic studies reports Special nursing record First page of client record Admission sheet Outpatient record Order of Discharge (transfer, death) Record • • • • • • • • • • • First page of client record Admission sheet (if client died, adding death report sheet) Discharge or death record Admission record medical history and physical examination Physician's record Consultation record Diagnostic studies reports special nursing record Physician’s order sheet Temperature sheet Outpatient record is given back to the client or the client's family. Section 2 Writing Nursing Documents Temperature Sheet Managing Physician’s Order Recording Special nursing Reporting Client’s Conditions 中国医疗信息化的发展 • 医院信息系 统(hospital information system, HIS) • 面向临床工作的医院临 床信息系统 ( clinical information system, CIS)将 成为HIS的重点发展方向。CIS包括电子病 历系统、医学影像处理系统、实验室数据 处理系统、临床专科数据分析系统等。 Temperature Sheet It is on the first page of client's hospitalization record. it provides the staff with a quick summary of all the client's condition and vital signs on the sheet. Filling in Top Part This part must be filled in with a blue-black inked or carbon inked pen . Client's name, sex, age, ward, admission date and hospitalization number must be filled in completely. year, month and day must be filled in the first day column of every page. the rest six days column only “Day” Filling in Between 40℃~42℃ Column of Temperature Sheet Time of admission, operation, childbirth, transfer,discharge or death is filled in the vertical line of corresponding time column with a red inked pen between 40 ℃~42℃ column. it is essential to specify the minute. If the time is not equal to the time at temperature sheet, fill in the proximal time column. Drawing Body Temperature Curve Drawing Sphygmogram Drawing Body Temperature Curve Oral temperature :“●”, Axillary temperature “×, Rectal temperature “○”. Two adjacent readings are connected by blue line. • A client with hyperpyrexia needs to have the body temperature taken again in half an hour after receiving physical therapy.The reading of measured temperature is drawn in the same longitudinal column of previous reading by red “○”, and connected with the reading before physical therapy by red dotted line. The reading of next measurement is still connected with the reading before physical therapy. a client's body temperature is below 35℃ 不 升 不 升 Reading of measured temperature is represented by blue “×”, and connected with the adjacent readings. Drawing Sphygmogram Pulse rate is drawn in red “ ● ”,Two corresponding readings of pulse rate are connected by red line. pulse deficit heart rate is in red “○”. Two corresponding readings of heart rate are connected by red line. filled in the area between the line of pulse rate and the line of heart rate in red line. If the reading of body temperature and pulse rate are at the same point, draw the temperature first in blue “×” , then draw a red circle( ○ ) outside the blue “ × ” to represent the pulse rate. Respiration Readings of respiration are recorded in corresponding time columns in Arabic number with blue pen and the numbers are written alternatively upward and downward. Filling in Bottom Part All this part is filled in by using a blue-black inked or carbon inked pen. Arabic number represents the readings. Calculation unit is omitted. Contents: Bowel Movement Document the bowel movement on the previous day. If there is no bowel movement, document "0"; fecal incontinence is documented as "※"; “ E” represents enema. (0/E ; 11/E) Document the number of times once a day 1 /E represents one time of defecation after enema. Fluid intake and output Fluid output Fluid Intake • Document the total amount of Fluid intake and output of the previous day (during a 24-hour period) according to the physician's order. • the amount of intake and output fluids are recorded in ml. Blood Pressure Readings of blood pressure are recorded in corresponding time columns. 110/75, 105/70 If more measuring is needed, the readings of measurement can be recorded in the nursing notes. Body Weight Fill it in the unit of kg. When a client is admitted, the nurse measures his or her body weight and documents it in the corresponding time column. During hospitalization, measure and document body weight once a week. days of operation (childbirth) The next day of operation (childbirth) is regarded as the first day of operation (childbirth) that has been charted continuously on the day column in Arabic number “1, 2, 3... ” until 10 days. If a second operation has been done within 10 days Days of hospitalization write in Arabic number“1, 2, 3...” from the day of admission to the day of discharge. Page Number • Fill the page numbers in sequence. Managing Physician’s Order physician order recording book( 医嘱本) physician order sheet(医嘱单) various types of forms that are necessary for implementation (各种执行单) ∨ ∨ ∨ physician order recording book 床号 姓名 时间 医嘱 医生 执行 护士 签名 时间 签名 2007-12-11 1-3 张利 8am 外科护理常规 马良 李 玲 Ⅱ级护理 流质饮食 青霉素皮试( )st 8am 黄华 10%GS500ml 青霉素640万u ivdrip qd 丁 胺卡那 0.2 im bid Vc 100mg tid 氧气吸入 p r n 李玲 2007-12-12 1-3 张利 4pm 停Vc 100mg tid 下午2点胸腔穿刺 安定 5mg hs 度冷丁 50mg im q6h 李玲 2pm 吕新 李玲 医 嘱 本 山东大学齐鲁医院 physician order sheet STAT order Sheet Standing order Sheet various types of forms that are necessary for implementation • • • • • nursing grade sheet diet sheet oral medication sheet injection sheet treatment sheet, etc. 口服药 1-3 张利 8 –12 – 4 Vc 100mg 土霉素 0.5 8pm 土霉素 0.5 Contents of Physician Order • Date, Time, • Bed No, Name • routine care • grade of nursing • diet • body position • physician's signature • nurse's signature • medication (name, dosage, routes of administration); • pre-operation preparation; • diagnostic Study and therapy, preparation for diagnostic test or surgery Types of Physician Order • • • • Standing Order STAT Order PRN Order SOS Order Standing Order • A standing order is valid until it is cancelled by the physician. Usually the valid time of a standing order exceeds 24 hours. STAT Order 安定 5mg hs. • The valid time limit of a STAT order is within 24 hours, usually only once. • Sometimes a STAT (ST) order signifies that a single dose of medication is to be given immediately. PRN Order • PRN order is a kind of standing order. • The physician may order a treatment on a PRN basis if the client's condition needs. • Often the physician sets minimal intervals between two times of administration. 度冷丁 50mg im q6h prn SOS Order • The valid time of the SOS order is within 12 hours. • It will be carried out only once as the state of an illness needs. • It becomes invalid if it exceeds the time limit. Managing Physician Order • Method of Handling •Principles of Managing Standing Order • transfers the orders onto various types of forms. • The standing orders transferred onto the implementation forms which are carried out in appointed time should be signed specific administered time. PRN order transfers them onto various types of forms. If the physician sets minimal intervals between two times of administration, each time the nurse carries out the PRN order, he or she has to document the exact time and sign full name. STAT Order • “st” means executing an order immediately. • After carrying out the order, the nurse has to sign his or her name in “executer” column and notes the time of executing. penicillin skin test penicillin positive (+) negative (-) SOS order • SOS order should be carried out only once as the state of an illness needs. • The person, who carries out the order, signs his or her name in “performer” column and notes the time of executing. • The order becomes invalid if it exceeds the time limit. The nurse writes the word “unexecuted”, documents the time and signs her name. Stop the Order • If a physician decides to stop an order for some reasons, the nurse cancels the order in related treatment sheet first. • write down the date and time in “stop” column in physician order sheet. Re-arranging the Order • draw a red line below the last row of physician orders, write “Rearranging” in the middle below the red line with a red pen, and transcribe original valid physician orders onto spaces below the red line. • Two nurses verify the rearranged orders and sign their names. • After the operation, childbirth or transferring, physician orders have to be rearranged too. Draw a red line below the last row of original orders, and write “post-operation order”, “post-childbirth order”, •Principles of Managing • Urgent Before Routine. When managing several physician orders, it is necessary to see which order is more important or urgent to the client, and give priority for carrying it out. •Principles of Managing STAT Order Before Standing Order. • It is routine to carry out a STAT order before a standing one. •Principles of Managing • The order could not be changed. If it is to be canceled, note “cancel” with a red pen and sign. •Principles of Managing • Generally speaking, the physician should not give oral orders. In the events of an emergency or during operation when the physician gives orders orally to nurses, the nurses have to repeat the order once again and make sure it is correct. • After the emergency has been allayed and the physician should record and sign all orders that were given. •Principles of Managing • If a STAT or SOS order is to be carried out on the next shift, the order should be written down in the nursing notes. •Principles of Managing • The physician orders must be checked in every shift and totally once every week. clinical information system, CIS 医嘱处理 医生登录医生工作站系统,将医嘱按照长期医嘱、 临时医嘱、辅助检查、化验等分类 录入系统, 护士 登录护士工作站系统进行处理: • 审核医嘱 • 执行医嘱 • 打印表单和医嘱单 Recording Fluid Intake and Output • Contents • Methods for Recording Contents fluid intake 出入液量记录单 •oral fluid intake •food intake •intravenous fluid infusions fluid output urine, stool, vomit, bleeding, sputum, gastric suction, and drainage from postsurgical drainage tubes. Methods for Recording • Daytime's fluid intake and output are recorded with a blue-black inked or carbon inked pen; • nighttime's fluid intake and output are recorded with a red pen. • intake and output are summarized at the end of each 12-hour and 24-hour period. Sum of intake and output of 24-hour period is filled in corresponding column of the temperature sheet. Recording Special Nursing • Contents of record • Methods and Recommendations for Recording Contents of record • • • • • • • vital signs level of consciousness fluid intake and output state of illness nursing intervention response to medication signature Methods and Recommendations 特别护理记录单 Change-of-shift report Components of Report Recommendations Components of Report • • • • • Discharge, Transfer-out, and Death Report Admission, Transfer-in Report Severely Ill Clients' Report Postoperative Clients' Report Pre-operation, pre-diagnostic Studies Preparation Report Ward Top Part date time total number of clients number of client admission discharge transfer Operation childbirth clients in critical state death. discharge, transfer-out, death admission, transfer-in Order of Writing operative clients, clients who gives birth, critically ill clients, and clients of unusual condition 病人情况日夜报告 护士长签字: 日期—年—月—日 姓名 床号 诊断 入院 出院 转出 病重 手术 死亡 同左 3床 杜鹃 甲状腺瘤住院10天治愈于9am出院 5床 许威 胃癌住院14天于4pm转普外科 19 床 T P R at 4pm 庞月 患者 上消化道穿 孔并腹膜炎 新 31床 吴军 肺癌 手术 T P R T P 患者 同左 R at T P 患者 R at at 护理要点:1、 护士签名 护士签名 护士签名 Recommendations • Record is on the basis of sound observation. • The report should be concise, accurate and objective, and highlight important points. • The report should be neat and legible. Do not erase. • Daytime's conditions are recorded with a blue pen, and nighttime's conditions are recorded with a red pen. • Entries are filled in the following orders: write down the bed number name and diagnosis vital signs and the time of measuring the clients' conditions, treatment and nursing care provided • For clients newly admitted, transferred-in, having operation or childbirth, write down the word “New”, “Transfer”, “Operation”, and “Childbirth” in red under the words of diagnosis. For severely ill clients, it is highlighted by the symbol “※”, or the word “critically ill” in red. • After finishing the recording, write down the number of pages and sign full name. • The head nurse should check the client's condition report of each shift and make sure it meets the nursing quality criteria, then sign her full name.