62 - Viện y tế công cộng
advertisement

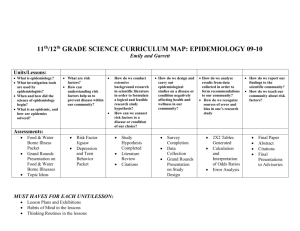
Điều Tra Vụ bùng phát bệnh từ thực phẩm GS, Ts Lê Hoàng Ninh Bùng phát là gì ?(outbreak) Dịch ( epidemic) hay còn gọi là bùng phát ( outbreak)khi số ca bệnh cao hơn số dự kiến xảy ra ( trị số bình thường) tại một địa phương, khu vực nào đó, hay trên một nhóm dân số nào đó trong một thời khoảng nhất định Epidemiology (Schneider) Số ca bệnh Bệnh lưu hành địa phương (endemic)và dịch ( epidemic) Lưu hành Thời gian Epidemiology (Schneider) Dịch Tại sao phải điều tra bùng phát/ dịch? Kiểm soát và phòng ngừa Sự ác tính và nguy cơ lây truyền cho người khác Cơ hội nghiên cứu để hiểu biết tốt hơn Cơ hội đào tạo Xem xét chương trình y tế Cab quan ngại khác: luật, chính trị, công cộng… Epidemiology (Schneider) Step 1: Verify the outbreak Determine whether there is an outbreak – an excess number of cases from what would be expected Establish a case definition Non-ambiguous Clinical / diagnostic verification Person / place / time descriptions Identify and count cases of illness Epidemiology (Schneider) Step 2: Plot an Epidemic Curve Graph of the number of cases (y-axis) by their date or time of onset (x-axis) Interpreting an epidemic curve Epidemiology (Schneider) Overall pattern: increase, peak, decrease Type of epidemic? Incubation period? Outliers: Unrelated? Early or late exposure? Index case? Secondary cases? Vector-borne Disease • Starts slowly • Time between the first case and the peak is comparable to the incubation period. • Slow tail Point Source Transmission • This is the most common form of transmission in foodborne disease, in which a large population is exposed for a short period of time. Continuing Common Source or Intermittent Exposure • In this case, there are several peaks, and the incubation period cannot be identified. Salmonellosis in passengers on a flight from London to the United States, by time of onset, March 13--14, 1984 Source: Investigating an Outbreak, CDC Legionnaires' Disease By date of onset, Philadelphia, July 1-August 18, 1976 Source: Investigating an Outbreak, CDC Foodborne Outbreak (Propagated) Source: CDC, unpublished data, 1978 Step 3: Calculate attack rates Attack rate = (ill / ill + well) x 100 during a time period If there is an obvious commonality for the outbreak, calculate attack rates based on exposure status (a community picnic) If there is no obvious commonality for the outbreak, calculate attack rates based on specific demographic variables (hepatitis cases in a community) Epidemiology (Schneider) Step 4: Determine the source of the epidemic If there is an obvious commonality for the outbreak, identify the most likely cause and investigate the source to prevent future outbreaks If there is no obvious commonality for the outbreak, plot the geographic distribution of cases by residence/ work/school/location and seek common exposures Epidemiology (Schneider) Step 5: Recommend control measures Control of present outbreak Prevention of future similar outbreaks Epidemiology (Schneider) The vast majority of outbreaks are food-borne Foodborne Disease Outbreak An incident in which (1) two or more persons experience a similar illness after ingestion of a common food, and (2) epidemiologic analysis implicates the food as the source of the illness Intoxication – ingestion of foods with Toxicants found in tissues of certain plants (Jimpson Weed) and animals (seal liver) Metabolic products (toxins) formed and excreted by microorganisms while they multiply (botulinum toxin) Poisonous substances introduced during production, processing, transportation or storage (chemicals, pesticides) Foodborne Disease Outbreak (cont.) Infections – Caused by the entrance of pathogenic microorganisms into the body and the reaction of the body tissues to their presence or to toxins they generate within the body Rule of thumb – but not law Intoxicants are rapid onset, no fever Toxins in the stomach produce vomiting Toxins in the intestines produce diarrhea Infections produce fever Types of Foodborne Contamination Physical Chemical Glass, metal fragments, tacks, dirt, bone, etc. Pesticides, cleaning compounds, poisonous metals, additives and preservatives Biological Bacteria, viruses, fungi, yeast, molds, parasites, poisonous fish and plants, insect and rodents Epidemiology (Schneider) Bacterial Requirements Food: Most bacteria require what is known as potentially hazardous food Milk or milk products, eggs, meat, poultry, fish, shellfish, crustaceans, raw seed sprouts, heat treated vegetables and vegetable products (fruits?) Generally high protein, moist foods Epidemiology (Schneider) Bacterial Requirements (cont.) Water: Bacteria require moisture to thrive The water activity (Aw) is the amount of water available in food The lowest Aw at which bacteria will grow is 0.85 Most potentially hazardous foods have a water activity of 0.97 to 0.99 pH: Best growth at neutral or slightly acidic pH Potentially hazardous foods have a pH of 4.6 – 7.0 Epidemiology (Schneider) Bacterial Requirements (cont.) Temperature: The danger zone for potentially hazardous foods is 45 to 140 degrees Fahrenheit This is the zone where most bacterial growth occurs Time: Potentially hazardous foods must not be allowed to remain in the danger zone for more than 4 hours Oxygen: Some bacteria require oxygen while others are anaerobic and others are facultative Epidemiology (Schneider) Major Causes of Foodborne Disease Improper cooling of foods Improper cooking of foods Improper reheating of foods Improper holding temperature of foods Cross contamination Infected food handlers, poor employee hygiene Epidemiology (Schneider) 0F 250 240 Temperature and Bacteria Control Canning temperatures for low-acid vegetables, meat, and poultry in pressure canner Canning temperatures for fruits, tomatoes, and pickles in waterbath canner 212 Water boils Most bacteria destroyed 165 No growth, but survival of some bacteria DANGER ZONE 140 Some bacterial growth; many bacteria survive 125 120 Hottest temperature hands can stand Extreme DANGER ZONE. Rapid growth of bacteria and production of poisons by some bacteria 98.6 60 45 40 32 Body temperature – ideal for bacterial growth Some growth of food poisoning bacteria may occur Slow growth of some bacteria that cause spoilage Water freezes Growth of bacteria is stopped, but bacteria level before freezing remains constant and not reduced 0 - 20 Keep frozen foods in this range Source: Keeping Food Safe to Eat, USDA Bacterial Growth Curve Stationary Phase Number of Cells Log Phase Lag Phase Time Epidemiology (Schneider) Decline Phase Number of Salmonella per gram Effect of Temperature in Salmonella Growth 50oF (10o C) 95oF (35o C) 44oF (6.7o C) 42oF (5.5o C) 1 2 3 Days Epidemiology (Schneider) 4 5 Incubation Periods 2-4 hours Staphylococcus aureus 12 hours Clostridium perfringens Cooked meats, gravy 12-36 hours Salmonella* Meat, poultry, eggs 12-36 hours Clostridium botulinum 12 hours Vibrio parahemolyticus* 24-48 hours Shigella* * Fever Cooked ham, meat, eggs, sauces and gravies Canned foods, smoked fish Raw fish, shellfish Contaminated by carrier, not foodborne National Data on Etiology of Foodborne Illness Agent Bacteria (40 agents) 68.7% Salmonella 25.0% Staph. aureus 12.7% Clostridium perfringens 10.0% Clostridium botulinum 9.5% Viral (11 agents) 9.4% Parasites (31 agents) 0.5% Fungal (16 agents) 1.8% Plants (36 agents) - Fish (28 agents) 12.3% Chemicals (28 agents) 7.3% Investigating an Epidemic: Oswego, NY On April 19, 1940, the local health officer in the village of Lycoming, Oswego County, New York, reported the occurrence of an outbreak of acute gastrointestinal illness to the District Health Officer in Syracuse. Dr. A. M. Rubin, epidemiologist-in-training, was assigned to conduct an investigation. When Dr. Rubin arrived in the field, he learned from the health officer that all persons known to be ill had attended a church supper the previous evening, April 18. Family members who had not attended the church supper had not become ill. Accordingly, the investigation was focused on the circumstances related to the supper. Source: CDC Interviews regarding the presence of symptoms, including the day and hour of onset, and the food consumed at the church supper, were completed on 75 of the 80 persons known to have been present. A total of 46 persons who had experienced gastrointestinal illness were identified. Q: Is this an Epidemic? Endemic for the region? Due to seasonal variation? Due to random variation? Epidemiology (Schneider) Select the correct case definition and find the error in the others: 1. All participants in the Oswego church supper held in the basement of the church in Lycoming, Oswego County, New York, on April 18, 1940, between 6:00 PM and 11:00 PM; whether they attended church or not; whether they participated in food preparation, transport, or distribution or not; whether they ate or not. 2. Persons who developed acute gastrointestinal symptoms within 72 hours of eating supper on April 18, 1940, and who were among attendees of the Lycoming, Oswego Church supper. 3. Church members who developed acute gastrointestinal symptoms within 72 hours of the church supper held in Lycoming, Oswego on April 18, 1940. Select the correct case definition and find the error in the others: 1. All participants in the Oswego church supper held in the basement of the church in Lycoming, Oswego County, New York, on April 18, 1940, between 6:00 PM and 11:00 PM; whether they attended church or not; whether they participated in food preparation, transport, or distribution or not; whether they ate or not. 2. Persons who developed acute gastrointestinal symptoms within 72 hours of eating supper on April 18, 1940, and who were among attendees of the Lycoming, Oswego Church supper. 3. Church members who developed acute gastrointestinal symptoms within 72 hours of the church supper held in Lycoming, Oswego on April 18, 1940. Select the correct case definition and find the error in the others: 1. All participants in the Oswego church supper held in the basement of the church in Lycoming, Oswego County, New York, on April 18, 1940, between 6:00 PM and 11:00 PM; whether they attended church or not; whether they participated in food preparation, transport, or distribution or not; whether they ate or not. Missing definition of sickness 2. Persons who developed acute gastrointestinal symptoms within 72 hours of eating supper on April 18, 1940, and who were among attendees of the Lycoming, Oswego Church supper. CORRECT 3. Church members who developed acute gastrointestinal symptoms within 72 hours of the church supper held in Lycoming, Oswego on April 18, 1940. Did not specify that they went to the dinner Incidence of Cases of Diarrhea Among People Attending Lycoming,Oswego Church Supper, June 1940 The supper was held in the basement of the village church. Foods were contributed by numerous members of the congregation. The supper began at 6:00 PM and continued until 11:00 PM. Food was spread out upon a table and consumed over a period of several hours. Epidemiology (Schneider) Church Supper Menu Main Dishes • • • • • Baked ham Spinach Mashed potatoes Cabbage salad Fruit Salad Side Dishes • • • Jello Rolls Brown Bread Desserts • • • Cakes Vanilla Ice Cream Chocolate Ice Cream Beverages • • • Milk Coffee Water Epidemiology (Schneider) Which menu item(s) is the potential culprit? To find out, calculate attack rates. The foods that have the greatest difference in attack rates may be the foods that were responsible for the illness. Epidemiology (Schneider) Attack Rates by Items Served: Church Supper, Oswego, New York; April 1940 Number of persons who ate specified item Well Total Attack rate (%) 17 46 Number of persons who did not eat specified item Baked ham Ill 29 Spinach 26 17 43 20 12 32 Mashed potato 23 14 37 23 14 37 Cabbage salad 18 10 28 28 19 47 Jello 16 7 23 30 22 52 Rolls 21 16 37 25 13 38 Brown bread 18 9 27 28 20 48 Milk 2 2 4 44 27 71 Coffee 19 12 31 27 17 44 Water 13 11 24 33 18 51 Cakes 27 13 40 19 16 35 Ice cream (van) 43 11 54 3 18 21 Ice cream (choc) 25 22 47 20 7 27 Fruit salad 4 2 6 42 27 69 Epidemiology (Schneider) Ill 17 Well 12 Total 29 Attack rate % Attack Rates by Items Served: Church Supper, Oswego, New York; April 1940 Number of persons who ate specified item Number of persons who did not eat specified item Baked ham Ill 29 Well 17 Total 46 Attack rate (%) 63 Ill 17 Well 12 Total 29 Attack rate % 59 Spinach 26 17 43 60 20 12 32 62 Mashed potato 23 14 37 62 23 14 37 62 Cabbage salad 18 10 28 64 28 19 47 60 Jello 16 7 23 70 30 22 52 58 Rolls 21 16 37 57 25 13 38 66 Brown bread 18 9 27 67 28 20 48 58 Milk 2 2 4 50 44 27 71 62 Coffee 19 12 31 61 27 17 44 61 Water 13 11 24 54 33 18 51 65 Cakes 27 13 40 67 19 16 35 54 Ice cream (van) 43 11 54 80 3 18 21 14 Ice cream (choc) 25 22 47 53 20 7 27 74 Fruit salad 4 2 6 67 42 27 69 61 Attack Rates by Items Served: Church Supper, Oswego, New York; April 1940 Number of persons who ate Ill specified item Well Total Attack rate (%) Number of persons who did not eat specified item Ill Well Total Attack rate % Baked ham 29 17 46 63 17 12 29 59 Spinach 26 17 43 60 20 12 32 62 Mashed potato 23 14 37 62 23 14 37 62 Cabbage salad 18 10 28 64 28 19 47 60 Jello 16 7 23 70 30 22 52 58 Rolls 21 16 37 57 25 13 38 66 Brown bread 18 9 27 67 28 20 48 58 Milk 2 2 4 50 44 27 71 62 Coffee 19 12 31 61 27 17 44 61 Water 13 11 24 54 33 18 51 65 Cakes 27 13 40 67 19 16 35 54 Ice cream (van) 43 11 54 80 3 18 21 14 Ice cream (choc) 25 22 47 53 20 7 27 74 Fruit salad 4 2 6 67 42 27 69 61 Highlighted row indicates largest difference between attack rates Attack Rate by Consumption of Vanilla Ice Cream, Oswego, New York; April 1940 Ate vanilla ice cream? Ill Well Total Attack Rate (%) Yes 43 11 54 79.6 No 3 18 21 14.3 Total 46 29 75 61.3 • The relative risk is calculated as 79.6/14.3 or 5.6 • The relative risk indicates that persons who ate vanilla ice cream were 5.6 times more likely to become ill than those who did not eat vanilla ice cream Conclusion An attack of gastroenteritis occurred following a church supper at Lycoming The cause of the outbreak was most likely contaminated vanilla ice cream Epidemiology (Schneider) Surveillance Ongoing systematic collection, collation, analysis and interpretation of data; and the dissemination of information to those who need to know in order that action may be taken. World Health Organization Epidemiology (Schneider) Purposes of Public Health Surveillance Estimate magnitude of the problem Determine geographic distribution of illnesses Portraying the natural history of disease Detect epidemic / Define a problem Generate hypotheses and stimulate research Evaluate control measures Monitor changes in infectious agents Detect changes in health practice Facilitate planning CDC Epidemiology (Schneider) Passive Surveillance Physicians, laboratories, and hospitals are given forms to complete and submit with the expectation that they will report all of the cases of reportable disease that come to their attention Advantages: Inexpensive Disadvantages: Data are provided by busy health professionals. Thus, the data are more likely to be incomplete and underestimate the presence of disease in the population Epidemiology (Schneider) Active Surveillance Involves regular periodic collection of case reports by telephone or personal visits to the reporting individuals to obtain the data Advantages: More accurate because it is conducted by individuals specifically employed to carry out the responsibility Disadvantages: Expensive Epidemiology (Schneider) Sentinel Surveillance Monitoring of key health events, through sentinel sites, events, providers, vectors/animals Case report indicates a failure of the health care system or indicates that special problems are emerging Advantages: Very inexpensive Disadvantages: Applicable only for a select group of diseases Epidemiology (Schneider) Some Surveillance Programs National Notifiable Diseases Surveillance System http://www.cdc.gov/epo/dphsi/nndsshis.htm Morbidity and Mortality Weekly Report (MMWR) http://www.cdc.gov Cancer Surveillance, Epidemiology and End Result (SEER) http://www.seer.cancer.gov/ Epidemiology (Schneider) “Good surveillance does not necessarily ensure the making of right decisions, but it reduces the chances of wrong ones.” Alexander D. Langmuir NEJM 1963;268:182-191 Epidemiology (Schneider)