The Digestive System
advertisement

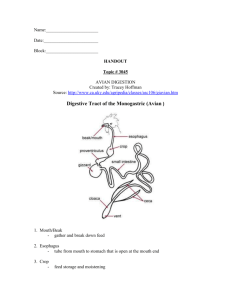
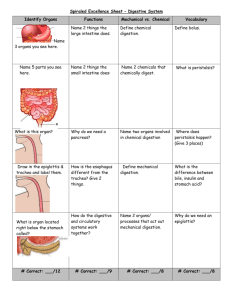
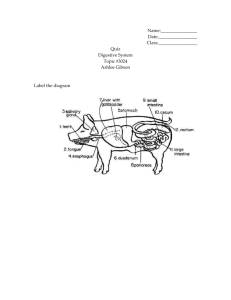
The Digestive System Digestive System: Overview • The alimentary canal or gastrointestinal (GI) tract digests and absorbs food. – Alimentary canal – mouth, pharynx, esophagus, stomach, small intestine, and large intestine. • Accessory digestive organs – teeth, tongue, gallbladder, salivary glands, liver, and pancreas. Greater Omentum • Greater - covers small intestines like an apron. • This is the visceral fat that may be detrimental to your health. Where does she carry most of her weight? Mesentery and Mesocolon • Mesentery of small intestines contain the nerves and the blood vessels • Mesocolon anchors colon to posterior body wall •Peritoneum – serous membrane of the abdominal cavity Visceral – covers external surface of most digestive organs Parietal – lines the body wall •Peritoneal cavity- small space between visceral and parietal peritoneum. Lubricates digestive organs Allows them to slide across one another Retroperitoneal structures are located behind the peritoneum. The Digestive System Process 1. Ingestion: intake of food. 2. Digestion: Mechanical and chemical breakdown of food. 3. Absorption: Uptake of nutrients from the digestive tract into the blood and lymph. 4. Compaction: Absorbing water and consolidating indigestible food to form feces. 5. Defecation: Elimination of the feces. Types of Digestion • Mechanical digestion – physical breakdown of food into smaller particles – teeth and churning action of stomach and intestines • Chemical digestion – series of hydrolysis reactions that break macromolecules into their monomers – enzymes from saliva, stomach, pancreas and intestines – Results • Polysaccharides into monosaccharides • Polypeptides into amino acids • Triglycerides into glycerol and fatty acids Motility in the Intestines • Segmentation ensures mechanical digestion in the SI. – Ensure enzymes mix with proper substrates for maximal absorption. Peristalsis Peristalsis moves contents steadily in one direction along the alimentary canal. Histology of the Alimentary Canal • From esophagus to the anal canal the walls of the GI tract have the same four layers (tunics) – From the lumen outward they are the mucosa, submucosa, muscularis externa, and serosa • Each tunic has a predominant tissue type and a specific digestive function Anatomy of the Alimentary Canal Diaphragm Serosa Mucosa Muscularis Submucosa Blood vessels Mucosa • The innermost layer epithelial layer that lines the lumen of the alimentary canal • Stomach and small intestine mucosa contain: – Enzyme-secreting cells that aid in the absorption of nutrients for of digestion – Mucus producing cells protects the lumen from hydrolytic enzymes while aiding the movement food through the alimentary canal • Has many lymphatic vessels that protection against infectious disease Other layers of the Alimentary Canal • Submucosa – – Dense connective tissue containing elastic fibers – Blood and lymphatic vessels – Nerves (Submucosal Nerve Plexus) • Muscularis externa – – Composed of involuntary smooth muscle innervated by the (Myenteric Nerve Plexus) – responsible for segmentation and peristalsis • Serosa – the protective visceral peritoneum – Outer most layer Enteric Nervous Control Myenteric Nerve Plexus Submucosal Nerve Plexus Enteric Nervous Control • Is often referred to the second brain because it can regulate digestive tract mobility, secretion and blood flow independently of CNS. – It is thought that there are more neurons in the ENS than the spinal cord. • Composed of two nerve networks – submucosal plexus • controls glandular secretion and muscular contraction of the mucosa – myenteric plexus • controls peristalsis • contractions of muscularis external Autonomic Function in Digestion • Parasympathetic nervous system has many neural connections to the ENS. • It stimulates digestive activities via the vagus nerve. • Sympathetic nervous system inhibits digestive activity by shunting blood away from the gut and to the heart and skeletal muscles. Phases of Digestion Cephalic phase • Prepares the digestive system before the ingestion of food. Stimulation of the senses (sight, smell and taste) or thought of food will activate the Parasympathetic Nervous System (PNS) via the vagus nerve. • The medulla will stimulate the both digestive organs and glands to increase their metabolic activity. • Excitatory events include: – Sight or thought of food – Stimulation of taste or smell receptors • Inhibitory events include: – Loss of appetite or depression – Decrease in stimulation of the parasympathetic division Digestive Processes in the Mouth • Mechanical digestion begins in the mouth (chewing) • Salivary amylase begins chemical breakdown of starch. – Mouth is at a fairly neutral ph. Ideal for amylase • Propulsion is initiated by swallowing • The pharynx and esophagus serve as a passage way for food from the mouth to the stomach. Salivary Glands Saliva • Functions of saliva – moisten, begin starch and fat digestion, cleanse teeth, inhibit bacteria, bind food together into bolus • Composed of 99.5% water and solutes – – – – – – salivary amylase, begins starch digestion lingual lipase, digests fat activated by stomach acid mucus, aids in swallowing lysozyme, enzyme kills bacteria immunoglobulin A, inhibits bacterial growth electrolytes = Na+, K+, Cl-, phosphate and bicarbonate • pH of 6.8 to 7.0 • • • • • Stomach Chemical breakdown of proteins and to a lesser extent fats begins and food (bolus) is converted to chyme. Cardiac region –connects the esophagus to stomach. Muscularis –Is composed of 3 muscular layers – Allows the stomach to churn, mix, and pummel food physically Rugae: folds in the stomach when empty stomach The pylorus is continuous with the duodenum through the pyloric sphincter – Regulates how rate that food enters into the small intestines. Digestion in the Stomach • The stomach: – Holds ingested food – Digests food both mechanically and chemically – Delivers chyme to the small intestine – Enzymatically digests proteins with pepsin • Lingual lipase activated. – Secretes intrinsic factor required for absorption of vitamin B12 • Vitamin B12 is necessary for the production of many different type of cells including nerve and red blood cells – Pernicious anemia can result from a lack of either Vitamin B12 or intrinsic factor. Glands of the Stomach • Gastric glands of the fundus and body have a variety of secretory cells – Mucous neck cells – secrete mucus to protect stomach from acid environment. – Parietal cells – secrete H+Cl- , intrinsic factor and ghrelin – Chief cells – produce pepsinogen and gastric lipase • Pepsinogen is activated to pepsin by H+Cl- in the stomach – Enteroendocrine cells – secrete hormones that regulate digestion and gastric motility. • G-cells secrete gastrin : hormone that increases secretory activity and gastric mobility Microscopic Anatomy of the Stomach Gastric Phase • Excitatory events include: Stimulate Gastrin release – Stomach distension (stomach expands as bolus enters) • Activation of stretch receptors stimulates the Vagus nerve – Activation of chemoreceptors: presences of proteins buffer stomach acid ↑pH • Inhibitory events include: – As food exits out the pylorus the pH may drop below 2 – There will be less distension. – Emotional upset that overrides the parasympathetic division and activate the sympathetic division Control of Gastric Secretion Stomach Acid Functions • Activate enzymes pepsin and lingual lipase. • Breakdown plant connective tissues and cell walls. • Denatures proteins and converts minerals to a more bioavailable form. • Contributes to immunity by destroying ingested pathogens. Healthy Mucosa and Peptic Ulcer • Gastric and Peptic ulcers are linked to the acid tolerant bacteria Helicobactor pylori and excessive use of NSAID’s. • Antibiotics function to kill the H pylori bacteria • Proton pump inhibitors block the H+K+ATPase pump thus reducing acid production in the stomach. Hiatal Hernia • Part of the esophagus and upper part of stomach get trapped in the thoracic cavity. • LES sphincter fails allowing acid in the esophagus. – mimic symptoms of a heart attack. • Over time it will erode the esophagus resulting in strictures, hemorrhage or even cancer. Hormones and Gastric Emptying • • • Once food (Chyme) enters the small intestines duodenal enteroendocrine cells secrete various hormones that inhibit gastric secretion : – CCK, (Cholecystokinin) VIP (Vasoactive Intestine Peptide ) GIP( Gastric inhibitory peptide) and Secretin These collectively inhibit stomach secretions of HCL and gastrin from the G-cells thus reducing stomach motility. Pyloric sphincter tightens limiting admission of more food into the duodenum. – Allows the duodenum time to work on the chyme that has already entered. Small Intestine – 3 Segments • Has three subdivisions: duodenum, jejunum, and ileum • Runs from pyloric sphincter to the ileocecal valve Small Intestine • Duodenum (10 in.) – Receives stomach contents through the pyloric sphincter. – Pancreatic juice and bile aid in chemical digestion of chyme. – Neutralizes stomach acids, emulsifies fats, pepsin inactivated by pH increase, pancreatic enzymes hydrolyze their specific substrate. – Mostly digestion with minimal absorption occurs here. • Jejunum - next 8 ft. (in upper abdomen) – has large tall circular folds; walls are thick, muscular – nutrient digestion and absorption occurs here • Ileum - last 12 ft. (in lower abdomen) – has peyer’s patches – clusters of lymphatic nodules – ends at ileocecal junction with large intestine – Primarily nutrient absorption occurs here Microscopic Anatomy of the Small Intestine Small Intestine: Histology • Lined simple columnar epithelium which functions in absorption and secretion. – Villi • fingerlike extensions of the mucosa containing blood and lymph vessels for the absorption of nutrients – Microvilli • tiny folds in the individual simple columnar epithelial cells that further increase digestive surface area. • Brush-border enzymes – hydrolytic enzymes responsible for chemical digestion of organic molecules and activation of pancreatic enzymes. • Pancreatic enzymes and bile enter the duodenum through for the sphincter of Oddi Liver: Functions • The largest gland in the body • Liver cells( Hepatocytes) functions include: – Production of bile (emulsification of fat) – Detoxification( removes or dilutes toxins in the body – Storage of fat-soluble vitamins ( ADEK) – Increases BGLs: gluconeogenesis and glycogenolysis. – Decreases BGL’s: Stores excess glucose as glycogen – Formation of cholesterol including HDL and LDL • Used to transport lipids throughout the circulatory system. Pancreas • Exocrine function – Acini (clusters of secretory cells) digestive enzymes – Secretes pancreatic juice which breaks down all categories of foodstuff • The pancreas also has an endocrine function – release of insulin and glucagon Acinus of the Pancreas Hormonal Control of the Intestinal Phase • Baroreceptor and Chemoreceptors detects distension chemical changes in the intestines results in enteroendocrine cells to secrete two hormones • Secretin causes the release of HCO3– from the pancreas neutralizing acid chyme • Alkaline pH provides an optimal environment for pancreatic enzymes • CCK stimulates the pancreas to release the following digestive enzymes: Amylase ,Lipase and Proteases : (trypsinogen, chymotrypsinogin, procarboxypeptidase) – contraction of the Gall bladder – Relaxes the Sphincter of Oddi into the duodenum. – Promotes short term satiety The Gallbladder • A green muscular sac on the ventral surface of the liver is palpable in the right upper quadrant. • Stores and concentrates bile that was produced in the liver • Bile is released in response to the hormone CCK. • Main role of bile is to emulsify fat (break into smaller pieces) • Emulsified fat droplets have a greater surface area for pancreatic lipase to work. Emulsification of Fats Fatty Acid Absorption Chemical Digestion: Fats • Absorption: bile salts and pancreatic lipase results in FFA and Glycerol • FFA diffuse into intestinal cells where they: – Combine with proteins and form chylomicrons – Large chylomicrons must enter lacteals and are transported to systemic circulation via lymphatic system. Carbohydrate Metabolism • Salivary amylase gets denatured in stomach (pH < 4.5) • Pancreatic amylase further hydrolyzes carbohydrates. • Brush border enzymes maltase, sucrase, lactase complete hydrolysis resulting in monosaccharides. – Maltase → Hydrolyzes maltose into 2 glucose molecules – Sucrase → hydrolyzes sucrose leaving fructose and glucose – Lactase → hydrolyzes lactose into Galactose and glucose • Absorption: via co-transport with Na+, and facilitated diffusion – Enter the capillary bed in the villi – Transported to the liver via the hepatic portal vein Carbohydrate Digestion - Small Intestine Protein Digestion Protein Digestion – Enzymes for protein digestion are released in inactive forms to avoid digesting the pancreas and associated ducts prior to reaching its appropriate substrates: – Enzymes include: • Trypsinogen is activated by brush border enzyme entrokinase to trypsin • Chymotrypsinogin is activated to Chymotrypsin by trypsin • Procarboxypeptidase is activated by trypsin to carboxypeptidase – Both break down proteins into A.A via hydrolysis reactions Alcohol metabolism Alcohol can be absorbed directly through the stomach. – Food acts as a buffer • Can cross the blood brain barrier of the brain – Impaired judgment cognitive and physical abilities. – DWI can result in sharing a cell with a guy named Bubba • Pound for pound females usually can’t tolerate as much alcohol as their male counterparts because they naturally produce less of the enzyme that breaks it down. (Alcohol dehydrogenase) – The heavier you can usually tolerate more alcohol. – Tolerance varies between different ethnicities. • With a lot of practice you will make more of the enzyme and be able to hold your liquor. Absorption of Polar Molecules • The absorption of water soluble polar molecules (carbohydrates, amino acids, nucleotides, electrolytes and water) is accomplished by specific transport proteins located on the cell membranes of the absorptive cells. Membrane proteins utilize – secondary active transport: Sodium dependant cotransport proteins is necessary for the absorption of glucose , Galactose, amino acids and many minerals • 95% of the water is absorbed in the SI via osmosis following the osmotic gradient established by the Na+,K+ATPase (pump – Digestion requires a lot of ATP! Should this influence the frequency of your meals if you’re trying to loss weight. Carbohydrate Absorption • Sodium-glucose transport proteins (SGLT) in membrane help absorb glucose and galactose Pancreas • Has both exocrine and endocrine cells and is located behind the stomach – Acinar cells produce an enzyme-rich juice used for digestion (98% of organ) (exocrine product) – Pancreatic islets (islets of Langerhans) produce hormones (endocrine products) • The islets contain two major cell types: – Alpha () cells that produce Glucagon – Beta () cells that produce insulin • Remember: If your diabetic you Beta () have your insulin. Pancreatic Islet Insulin • Insulin: – Lowers blood glucose levels by increasing membrane permeability to both glucose and amino acids. • Considered an anabolic hormone – Target organs include muscle, liver and adipose tissue – antagonizes Glucagon • Insulin uses a second messenger which allows more glucose to enter the cell. Once in the cell insulin: – Increased utilization of glucose for ATP production – Glycogen is formed when anabolic enzymes stimulate dehydration synthesis of glucose. – Converts extra glucose to fat particularly in adipose tissue and liver cells once glycogen stores are full. – Promotes cellular mitosis Glucagon • Hormone released when blood sugar levels drop • Its major target is the liver where it promotes: – Glycogenolysis – the breakdown of glycogen to glucose – Gluconeogenesis – synthesis of glucose from lactic acid and non-carbohydrates – Release of glucose to the blood from liver cells – All will elevate blood glucose levels during fasting periods. Large Intestine • Divided into 4 regions: – ascending colon: ascends up the right side of the abdominal cavity • cecum – Lies below the ileocecal valve – Contains a wormlike vermiform appendix » Acts as a reserve for good flora and other immune boosting cells following diarrhea. » Inflammation of appendix (appendicitis) – transverse colon: runs across the abdominal cavity – descending colon: descends down the left side of abdominal cavity. – sigmoid colon: S shaped leads to rectum where feces is stored until defecation occurs through the anal canal. Functions of the Large Intestine • 95% of water is absorbed in the small intestines following their osmotic gradient. • The remaining water is absorbed in the large intestine. • Other than digestion of enteric bacteria( probiotics), no further digestion takes place – Vitamins, and electrolytes are reclaimed • Its major function is propulsion of fecal material toward the anus Neural Control of Defecation Case Study 1 • 40-year-old male has chief complaints not being able to sleep throughout the night without making multiple trips to the bathroom. The patient is 5 foot four 260 pounds. Normally has difficulty sleeping because he’s been diagnosed with sleep apnea. He also reports that his wounds tend to heal very slowly. • What’s a possible diagnosis? Diabetes Mellitus (DM) • Chronically elevated blood glucose levels results from hyposecretion or hypoactivity of insulin • The three cardinal signs of DM are: – Polyuria – Frequent urination from excessive sugar levels spilling over in kidney filtrate. Water will follow the osmotic gradient to dilute the urine (filtrate). – Polydipsia – excessive thirst as a result if frequently urinating and dehydration. – Polyphagia – excessive hunger and food consumption because the body thinks its starving because the sugar is not able to get into the cell. • Hyperinsulinism – excessive insulin secretion, resulting in hypoglycemia Hyperinsulinism • From excess insulin injection or pancreatic islet tumor – Causes hypoglycemia, weakness and hunger – triggers secretion of epinephrine, GH and glucagon • side effects: anxiety, sweating and HR • Insulin shock – uncorrected hyperinsulinism with disorientation, convulsions or unconsciousness Types of Diabetes Mellitus • Type I (IDDM) - 10% of cases – some cases have autoimmune destruction of cells, diagnosed about age 12 – treated with diet, exercise, monitoring of blood glucose and periodic injections of insulin • Type II (NIDDM) - 90% – insulin resistance • failure of target cells to respond to insulin • Excessive weight gain increases intramyocellular lipids which turns down mitochondria. • Excessive accumulation of lipids in the liver contribute to inflammation and insulin resistance Fatty Liver/ Myocellular Lipids Major Risk Factors – 3 major risk factors are heredity, age (40+) and obesity • treated with weight loss program of diet and exercise • oral medications improve insulin secretion or target cell sensitivity –Gastric bypass surgery has been shown to cure DM in 60-80% of cases. What’s they key? Obesity Trends* Among U.S. Adults BRFSS, 1990, 1999, 2009 (*BMI 30, or about 30 lbs. overweight ) 1999 1990 2009 No Data <10% 10%–14% 15%–19% 20%–24% 25%–29% ≥30% Who is part of the Pepsi generation? Have a Coke and a smile! Anti-inflammatory Pyramid Food Labels • Is it really low fat? – 1% milk = 18% and 2% =36%fat calories • Whole milk is more then 50 % fat calories – Meat 75% lean has 225 calories which 14 grams come from fat which equals 126 total fat calories = 57% fat by calories – 93% ground lean = 45% fat calories • because labeled by weight not % calories The diet and conditions your meal lived in is important! • The food industry can make up the serving size. – 5 calories or less = non caloric. – ½ gram of fat or less = none fat. Watch the potions size! – Lite means ½ the amount of fat as the original. • Usually sugar is substituted. Food Labels • Organic means 95% organic products – Look for the USDA Organic food label • Made with organic must be 70% • Free range: in a chicken coup that the door must stay open 5 minutes a day. • Pastured means cage is on the grass. • Know your farmer! • Whole Grain= only has to be a little more then ½ to say it on the label. – Made with whole grain may almost have none. • Look for 100% Digestive System Screen • • • • • • • • • • • • • • • • Changes in appetite Abdominal and chest pain Nausea / Vomiting Fatigue/ Weakness Bowel movement changes such as constipation and Diarrhea Stool appearance( Color size and shape) Dehydration Psychological changes like depression and anxiety from nutritional deficiencies. (gas) flagalence Yellow skin, eyes and nails Pancreatitis Stones Ulcer history Hernias Rebound tenderness Hemorrhoids Case Study • A 33 y/o female goes to her doctor with c/o bloating and diarrhea (3 years). She now is feeling depressed and has trouble getting more than 6 hours of sleep a night. She also reports occasional numbness and tingling in her feet. Lab test reveal she has deficiencies in a variety of vitamins, minerals and amino acids. – What's going on with this patient?