ABO Reporting - Transplant Pro

Proposal to Modify ABO
Determination, Reporting, and
Verification Requirements
Operations and Safety Committee
Spring 2015
The Problem
Accidental ABO incompatible transplants – rare but devastating
Safety gaps and risk
Varying requirements and complex language:
Deceased and living donation
Candidate and donor
OPTN and CMS
Compliance issues
Goal of the Proposal
Reduce risk of accidental ABO incompatible transplants
Increase transplant safety
Improve policy consistency and clarity
Further align requirements with CMS
How the Proposal will Achieve its Goal
Address safety gaps
Provide clarity and consistency in policy
Further align policies with CMS
UNet sm changes enhance system safeguards for intentional ABOi transplants
Concerns noted in Public Comment
OPOs conducting verification at recovery when the intended recipient is not known
Requiring on-site recovering surgeon to participate in verification
Additional requirements not needed given infrequency of unintended ABOi transplants
Proposed policy too prescriptive
Entire process was redesigned
General Public Comment Themes
Requests for the following:
no differences from CMS requirements
updated templates and electronic solutions
postpone policy requirements until after ETT (TransNet sm ) implementation
Concerns about clarity of policy
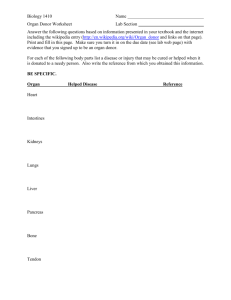
Substantive ABO Policy Changes
Requirement Current Proposed Align
CMS
Timing
Changes
Current
Practice
Expanded
Two ABO results must be obtained for deceased and living donors
Living donor recovery verification (time out) must be conducted
Deceased donor recovery verification (time out) must be conducted
Living donor recovery verification (time out) must be conducted
New
Conditional
Actions
Organ check-in
Pre-procedure ABO verification
• Prior to incision
• Prior to recovery
Prior to leaving
OR
• Prior to match run
• Prior to generation of donor ID
Prior to general anesthesia for donor
If organs remain in same OR suite
• Donor and organ info:
All cases
• Recipient info:
When intended recipient is known
If organs remain in same OR facility
All cases
Eliminates verification when leaving donor OR
None
None
If organ arrives from different OR suite
If recipient surgery starts prior to organ receipt no rule no rule
ABO Determination: Core Principles
Blood type and subtype results based on two laboratory tests
•Reduce chance of allocation being done on one erroneous lab result
Samples drawn on different occasions. With each collection, a separate patient identification and labeling procedure conducted prior to the blood draw
•Reduce chance of “wrong blood in tube” due to misidentification or label error
ABO Determination:
Changes from current policy
Remove OPO option to have one blood draw sent to two labs
Require protocol to have process when ABO primary types do not match
Exception clause for accelerated deceased donation cases
ABO Determination:
OPTN
Alignment with CMS
CMS
Deceased
Donor
Living
Donor
Candidate
2 Blood types on separate occasions
2 Blood types on separate occasions
2 Blood types on separate occasions
2 Blood types on separate occasions
Blood type must be done not specific
Blood type must be done not specific
ABO Reporting: Core Principles
Base reports on two lab results
Use source documents
Enter reports independently by two different users
Complete reports before becoming active in OPTN system
ABO Reporting:
Changes from current policy
“Qualified health care professional” must report
Safer timing
Exception clause for accelerated deceased donation cases
Addresses living donor VCA reporting
ABO Reporting: Timing Changes
Deceased
Donor
Living
Donor
Candidate
OPTN
Prior to
Match Run
Prior to
Incision
Prior to generate
Donor ID
Prior to
Active OPTN
Wait List
Before on tx hospital wait list
Before recovery
CMS
Before organ recovery
Medical eval prior to donation
ABO Verification (Time Out):
Core Principles
Confirmation of critical information includes surgeon
• Reduce chance of delayed or missed communication
Confirmation done at critical points of hand-off or introduction of risk
• Reduce chance of “wrong patient/wrong organ” and chance for accidental ABOi transplant
Changes will address
FMEA 1, 2, 4, 5, and 7
ABO Verification (Time Out):
Changes from current policy
Deceased donor: Donor and organ info (All cases)
Recipient info (When the intended recipient is known)
Living donor: All cases prior to general anesthesia
Timing and scope safer for all
ABO Verification (Time Out):
Changes from current policy
Organ Check In
New
Conditional: When organ received from outside OR suite
Pre-Transplant Verification
New
Conditional: When surgery starts before organ arrives
ABO Verification (Time Out):
Changes from current policy
All verification requirements now listed in responsible party policy
What must verified and what can be used as a verification source put in table format
Transplant surgeon and licensed health care professional included in pre-transplant verification
ABO Verification: Alignment with CMS
OPTN CMS
Deceased
Donor
Intended
Recipient is
Known: Prior to recovery
If organ in same suite: Before leave room and when enter recipient room
Intended
Recipient is
Known: Prior to recovery
Living
Donor
All: Prior to general anesthesia
If organ in same facility; Before leave room and when enter recipient room
All: Before removal donor organ
Candidate
After organ arrival, prior to transplant
After organ arrival, prior to transplant
Programming
Liver ABOi
Registrations
• Add warning
• Address FMEA
#3
Match Run
• Add candidate blood type on view
• Highlight ABO compatibility status with symbol !
!
• Human factors tool will assist with verifications
Subtype Second
User Verification
• Align programming with current policy
• Program subtype to verified by second user
• Same process as is currently done for primary type
What Members will Need to Do
OPOs and Transplant Hospitals :
Define “qualified health care professional” in protocols and process for resolving primary blood type conflicts
Be familiar with required verification information and acceptable sources
OPOs :
Assure two blood type determination and reports completed before match run
Conduct deceased donor organ recovery verification
Rerun match if organ not allocated on initial run or if data are updated/reported
What Members will Need to Do
Transplant hospitals :
Conduct living donor organ recovery verification before anesthesia
Conduct organ check-in when organs arrive from different OR suite
Conduct pre-procedure verification when surgery starts before organ arrives
Questions?
Theresa Daly, MS, FNP
Committee Chair thd9003@nyp.org
Regional Rep Name
Region X Representative email address
Susan Tlusty
Committee Liaison susan.tlusty@unos.org
Extras if needed
Near
Misses
Never Event
Death
Accidental
ABO
Transplant
Wrong Organ Arrived
Wrong Organ/Wrong
Patient
Not On Match Run
Labeling errors
ABO Testing issues
Communication issues
Changes to ABO data
Top Failure Modes
Number Failure Mode
1 OPO releases organ to recipient not on match run
2 Blood type verification does not occur prior to implantation
3 Candidate erroneously listed as accepting an ABO incompatible (pediatric heart, liver)
4 Wrong organ arrived-not checked at arrival to verify correct organ arrived for the correct potential recipient
5 If intended recipient surgery begins prior to arrival, no requirement for blood source documentation availability to confirm compatibility prior to anesthesia
6 Blood samples are mislabeled (candidate)
7 Verification occurs without both source documents for recipient and donor
8 One blood sample sent and tested twice
9 Only one sample drawn and tested prior to match (no ABO confirmation by second sample)
10 No pre-transfusion specimen is available for testing
11 Blood samples are mislabeled (donor)