Analgesics. Anesthetic and Neuromuscular Blocking Agents
advertisement

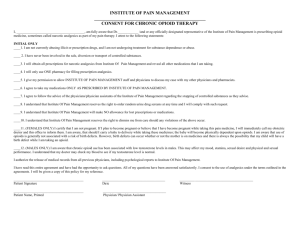
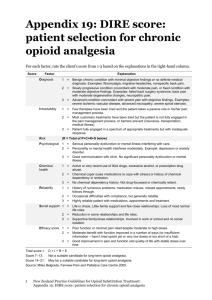
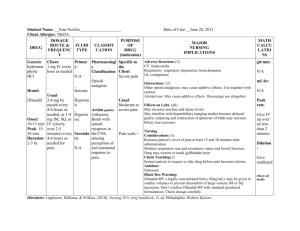
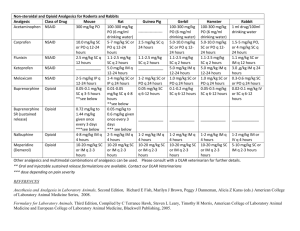
Pain Management What is pain? A protective mechanism to warn of damage or the presence of disease Part of the normal healing process Managing pain can be a challenge. Discussion What are the classifications of pain? Discussion What are the classifications of pain? Answer Acute Chronic Nonmalignant Malignant Pain Management Acute Pain Associated with trauma or surgery Easier to manage by treating the cause Has a beginning and an end Pain Management Chronic Pain No end to the pain Patients may have a sense of helplessness and hopelessness Affects different aspects of life Physical Psychological Social Spiritual Pain Management Chronic Nonmalignant Pain Cause may be diagnosed or undiagnosed Pain lasts for more than 3 months Patients may have signs and symptoms of depression Pain Management Chronic Malignant Pain Accompanies malignant disease Often increases in severity with disease progression Major Sources of Pain Source Area Involved Characteristics Treatment Somatic body framework throbbing, stabbing narcotics, NSAIDS Visceral kidneys, intestines, liver Nerves aching, throbbing, sharp, crampy burning, numbing, tingling narcotics, NSAIDS Neuropathic antidepressants, anticonvulsants Sympathetically overactive no pain should nerve blockers Mediated sympathetic be felt system Pain Transmission Tissue injury causes the release of: Bradykinin Histamine Potassium Prostaglandins Serotonin These substances stimulate nerve endings, starting the pain process. Pain Transmission There are two types of nerves stimulated: “A” fibers and “C” fibers Pain Transmission “A” Fibers “C” Fibers Myelin sheath Large fiber size Conduct fast Inhibit pain No myelin sheath Small fiber size Conduct slowly Facilitate pain transmission transmission Dull and nonlocalized Sharp and well-localized Pain Transmission Types of pain related to proportion of “A” to “C” fibers in the damaged areas Pain Transmission These pain fibers enter the spinal cord and travel up to the brain. The point of spinal cord entry is the DORSAL HORN. The DORSAL HORN is the location of the “GATE.” Pain Transmission This gate regulates the flow of sensory impulses to the brain. Closing the gate stops the impulses. If no impulses are transmitted to higher centers in the brain, there is NO pain perception. Pain Transmission Activation of large “A” fibers CLOSES gate Inhibits transmission to brain Limits perception of pain Pain Transmission Activation of small “B” fibers OPENS gate Allows impulse transmission to brain Pain perception Pain Transmission Gate innervated by nerve fibers from brain, allowing the brain some control over gate Allows brain to: Evaluate, identify, and localize the pain Control the gate before the gate is open Pain Transmission “T” cells Cells that control the gate have a threshold Impulses must overcome threshold to be sent to the brain Pain Transmission Body has endogenous neurotransmitters Enkephalins Endorphins Produced by body to fight pain Bind to opioid receptors Inhibit transmission of pain by closing gate Pain Transmission Rubbing a painful area with massage or liniment stimulates large sensory fibers Result: GATE closed, recognition of pain REDUCED Same pathway used by opiates Pain Management Narcotic Pain-modulating chemical derived from opium or is synthetically produced Also called opioid Causes insensibility or stupor Mainly effects on CNS and GI tract Lesser effects on peripheral tissues Pain Management Natural Opioids Endorphins, enkephalins, and dynorphins Produced by the brain in response to pain stimuli When receptors are activated causes decreased nerve transmission sensation of pain is diminished Opioids bind to these same receptors Discussion What are the three effects of narcotics? Discussion What are the three effects of narcotics? Answer Analgesia Sedation Euphoria and Dysphoria Opioid Analgesics Pain relievers that contain opium, derived from the opium poppy or chemically related to opium Narcotics: very strong pain relievers Poppy Papaver rhoeas L. 1. 2. Papaver somniferum L. 1 2 Opioid drugs are used primarily for the treatment of pain. Some of the CNS mechanisms that reduce the perception of pain also produce a state of well-being or euphoria. Thus, opioid drugs also are taken outside of medical channels for the purpose of obtaining the effects on mood. This potential for abuse has generated much research on separating the mechanism of analgesia from that of euphoria in the hope of eventually developing a potent analgesic that does not produce euphoria. The major risk for abuse or addiction occurs in patients complaining of pain with no clear physical explanation or with evidence of a chronic disorder that is not life threatening. Examples are chronic headaches, backaches, abdominal pain, or peripheral neuropathy. Even in these cases, an opioid might be considered as a brief emergency treatment, but longterm treatment with opioids is not advisable. In those relatively rare patients who develop abuse, the transition from legitimate use to abuse often begins with patients returning to their physician earlier than scheduled to get a new prescription or visiting emergency rooms of different hospitals complaining of acute pain and asking for an opioid injection. Opioid Analgesics codeine sulfate meperidine HCl (Demerol) methadone HCl (Dolophine) morphine sulfate propoxyphene HCl Opioid Analgesics Three classifications based on their actions: Agonist Agonist-antagonist Partial agonist Opioid Analgesics: Site of action Large “A” fibers Dorsal horn of spinal cord Opioid Analgesics: Mechanism of Action Bind to receptors on inhibitory fibers, stimulating them Prevent stimulation of the GATE Prevent pain impulse transmission to the brain Mechanism of action Opioids act at the Mesolimbic Dopaminergic System => Reward Center of the Brain. Inhibit the release of GABA at the VTA Inhibition of inhibition of Dopamine neurons DA activity Opiates concentrate in the VTA, nucleus accumbens, caudate nucleus and thalamus. The opiates bind to opiate receptors that are concentrated in areas within the reward system. The action of opiates in the thalamus contributes to their ability to produce analgesia Opioid Analgesics: Mechanism of Action Three types of opioid receptors: Mu Kappa Delta Opioid Analgesics: Therapeutic Uses Main use: to alleviate moderate to severe pain Opioids are also used for: Cough center suppression Treatment of constipation Subtypes of opioid receptors mu Analgesia, depression of breathing, euphoria, addiction development, sedative effect, depression of contents mocing through digestive tract, miosis kappa Analgesia, sedative eefect, psychotomimetic action delta Analgesia, euphoria, behaviour chnages sigma Mania, increasing of breathing frequency, hallucinations, midriasis Opioid Analgesics: Side Effects Euphoria Nausea and vomiting Respiratory depression Urinary retention Diaphoresis and flushing Pupil constriction (miosis) Constipation Opiate Antagonists naloxone (Narcan) naltrexone (Revia) Opiate antagonists Bind to opiate receptors and prevent a response Used for complete or partial reversal of opioid-induced respiratory depression Opiates: Opioid Tolerance A common physiologic result of chronic opioid treatment Result: larger dose of opioids are required to maintain the same level of analgesia Opiates: Physical Dependence The physiologic adaptation of the body to the presence of an opioid Opiates: Psychological Dependence (addiction) A pattern of compulsive drug use characterized by a continued craving for an opioid and the need to use the opioid for effects other than pain relief Opiates Opioid tolerance and physical dependence are expected with longterm opioid treatment and should not be confused with psychological dependence (addiction). Opiates Misunderstanding of these terms leads to ineffective pain management and contributes to the problem of undertreatment. Opiates Physical dependence on opioids is seen when the opioid is abruptly discontinued or when an opioid antagonist is administered. Narcotic withdrawal Opioid abstinence syndrome Opiates Narcotic Withdrawal Opioid Abstinence Syndrome Manifested as: anxiety, irritability, chills and hot flashes, joint pain, lacrimation, rhinorrhea, diaphoresis, nausea, vomiting, abdominal cramps, diarrhea Opioid Analgesics: Nursing Implications Before beginning therapy, perform a thorough history regarding allergies, use of other medications,health history, and medical history. Obtain baseline vital signs and I & O. Assess for potential contraindications and drug interactions. Opioid Analgesics: Nursing Implications Perform a thorough pain assessment, including nature and type of pain, precipitating and relieving factors, remedies, and other pain treatments. Assessment of pain is now being considered a “fifth vital sign.” Opioid Analgesics: Nursing Implications Be sure to medicate patients before the pain becomes severe as to provide adequate analgesia and pain control. Pain management includes pharmacologic and nonpharmacologic approaches. Be sure to include other interventions as indicated. Opioid Analgesics: Nursing Implications Oral forms should be taken with food to minimize gastric upset. Ensure safety measures, such as keeping side rails up, to prevent injury. Withhold dose and contact physician if there is a decline in the patient’s condition or if VS are abnormal— especially if respiratory rate is below 12 breaths/minute. Opioid Analgesics: Nursing Implications Follow proper administration guidelines for IM injections, including site rotation. Follow proper guidelines for IV administration, including dilution, rate of administration, and so forth. CHECK DOSAGES CAREFULLY OPIOIDS or NARCOTICS B. Acute Toxicity/Overdose 1.Disruption of central sympathetic activity. control of peripheral Brainstem Respiratory depression DEATH Circulatory depression BP Pupils constricted (miosis), (may be dilated with meperidine or severe hypoxia) Nausea and Vomiting Pulmonary edema Reflexes OPIOIDS or NARCOTICS 2. CNS depression Drowsiness Sedation Coma 3. CNS abnormal neuronal activity Convulsions -- with propoxyphene or meperidine OPIOIDS or NARCOTICS Treatment of overdose: acute toxicity and Naloxone. Opioid antagonist, used to block the actions of opioids in a life-threatening situation of opioid overdose. Given IV. Short half-life (1-2hrs). It precipitates withdrawal. Methadone. Used in the detoxification process. It causes a less pronounced euphoria and less severe withdrawal. OPIOIDS or NARCOTICS C. Withdrawal Most severe withdrawal of all drugs of abuse. Onset related to time-effect curve and t½ of narcotic. Not life threatening, no convulsions, no delirium, no disorientation. Opiate Withdrawal 6-8 hr =>drug seeking behavior, restless, anxious. 8-12 hr => Pupils dilated (mydriasis), reactive to light; increased pulse rate; blood pressure; yawning; chills; rhinorrhea; lacrimation; piloerection/ gooseflesh; sweating; restless sleep. 48-72 hrs (peak) => All of the above plus muscular weakness, aches (cramps) and twitches; nausea, vomiting and diarrhea; temperature; respiratory rate; heart rate and blood pressure; dehydration. Treatment of Sympathetic effects during withdrawal. ANS EFFECTS Clonidine 2-AR NA NE SN DA LC VTA VTA Motivational: Pleasure Reward Euphoria Used to block autonomic signs and symptoms of withdrawal: cramps nausea vomiting tachycardia sweating hypertension D. Treatment of Addiction Medical Detoxification A process whereby individuals are systematically withdrawn from addicting drugs in an inpatient or outpatient setting, typically under the care of a physician. Detoxification is sometimes called a distinct treatment modality but is more appropriately considered a precursor of treatment, because it is designed to treat the acute physiological effects of stopping drug use. OPIOIDS or NARCOTICS Severity of Withdrawal Heroin Methadone Naltrexone TIME OPIOIDS or NARCOTICS Detoxification or Maintenance treatment a. Methadone Used for the sequential detoxification and maintenance treatment of opiate dependence. b. LAAM (L--acetyl methadol, methadyl acetate). Structurally similar to methadone. Longer-acting opiate. Taken orally in liquid form, lasts 72 hrs (visits 3 X a week). “Take home" medication. c. Buprenorphine Partial opioid agonist which substitutes for low doses of opioids but antagonizes at high doses. Can be administered sublingually every 24-48 hrs as an alternative to methadone OPIOIDS or NARCOTICS d. Naltrexone Opiate Antagonist Causes precipitated abstinence. Use only for long-term maintenance of abstinence. Long half-life, oral, 3 times a week. Major problem in detoxification and maintenance of abstinence is the motivational component of the CNS effect, which is responsible for the “drug craving” sensations, also conditional dependence and social factors play an important role. Opioid Analgesics: Nursing Implications Constipation is a common side effect and may be prevented with adequate fluid and fiber intake. Instruct patients to follow directions for administration carefully, and to keep a record of their pain experience and response to treatments. Patients should be instructed to Opioid Analgesics: Nursing Implications Patients should not take other medications or OTC preparations without checking with their physician. Instruct patients to notify physician for signs of allergic reaction or adverse effects. Opioid Analgesics: Nursing Implications Monitor for side effects: Should VS change, patient’s condition decline, or pain continue, contact physician immediately. Respiratory depression may be manifested by respiratory rate of less than 12/min, dyspnea, diminished breath sounds, or shallow breathing. Opioid Analgesics: Nursing Implications Monitor for therapeutic effects: Decreased complaints of pain Increased periods of comfort With improved activities of daily living, appetite, and sense of well-being Pain Management Effects of Narcotics Analgesia Reduce pain from most sources Pain Management Effects of Narcotics Analgesia Reduce pain from most sources Sedation Decrease anxiety and cause drowsiness Pain Management Effects of Narcotics Analgesia Reduce pain from most sources Sedation Decrease anxiety and cause drowsiness Euphoria and Dysphoria Can cause feelings of well-being and disquiet or restlessness Potential for tolerance and dependence Pain Management Patient-Controlled Analgesia Pump Patient controls (within limits) when and how often medication is administered Allows for better pain control Pain Management Analgesic Ladder 1. Onset of mild to moderate pain Administer acetaminophen (APAP) or an NSAID Pain Management Analgesic Ladder 1. Onset of mild to moderate pain Administer acetaminophen (APAP) or an NSAID 2. Adequate relief is not achieved in Step 1 Administer NSAID plus a “weak” opioid (codeine) Pain Management Analgesic Ladder 1. Onset of mild to moderate pain Administer acetaminophen (APAP) or an NSAID 2. Adequate relief is not achieved in Step 1 Administer NSAID plus a “weak” opioid (codeine) 3. Adequate relief is not achieved in Step 2 Administer a strong opioid (morphine) Pain Management Chronic opioid therapy has a low risk of addiction when used appropriately. Discussion What is the difference between addiction and dependence? Pain Management Dependence Physical and emotional reliance on a drug Addiction Compulsive disorder Pain Management Symptoms of Addiction Preoccupation with drugs Refusal of medication tapers Strong preference for a specific opioid Decrease in ability to function Medication is typically not taken as prescribed Have a tendency to visit many different doctors and pharmacies in order to get the drug(s) Narcotic Dispensing Issues Warning! Pharmacy technicians have a legal and moral responsibility to alert pharmacist of suspected abuse and addiction. Pain Management Patients are more successful overcoming addiction if withdrawal symptoms are handled appropriately. Drug List Addiction Treatment buprenorphine (Buprenex, Subutex) buprenorphine-naloxone (Suboxone) methadone (Dolophine) methadone (Dolophine) Uses Detoxification Maintenance of narcotic addiction Dispensed in clinics or in hospitals Binds to opiate receptors without giving a euphoric feeling Pain Management Combinations of narcotics and nonnarcotics is common. Enhances relief Facilitates use of lower doses Decreases side effects Narcotic Analgesics Varying dose requirements due to Severity of pain Individual response to pain Patient’s age and weight Presence of concomitant disease NON-NARCOTIC ANALGESICS Types of action of non-narcotic analgesics Analgesic Antipyretic Anti-inflammatory (except paracetamol) Mechanism of action of non-narcotic analgesics depression of cyclooxygenases activity decreasing of prostaglnadins synthesis in peripheral tissues and in central nervous system decreasing of sensitivity of nervous endings and depression of transduction of nociceptive impulses on the level of CNS structures pain-relieving action of non-narcotic analgesics is partly connected with their anti-inflammatory activity Indications for administration of non-narcotic analgesics headache toothache radiculitis neuritis, neuralgias myositits, myalgia arthritis, arthralgia pain, connected with pelvic organs (dysmenorrhea) for potentiation of their action – combinations paracetamol with codein, analgin with dimedrol, analgin with codein Acetylsalicylic acid Blocks cyclooxygenase irreversably As a pyrolytic and analgesic drug – 0,25 and 0,5 g per time As an antiinflammatory – 3-4 g per day (for arthritis, myocarditis, подагрі, pleuritis, bronchitis For prophylaxis of thrombus-formation (in case of ischemic heart disease, thrombophlebitis etc.) – day dose – 80-100 mg Analgin (metamizol-sodium) Baralgin (maxigan, spazgan, spazmalgon, trigan) analgin+pitophenon hydrochloride+pheniverinium bromide Ampoules tablets suppositories Analgesic and spasmolytic activity Acetaminophen analgesic and pyrolytic drug maximal effect if the drug is introduced orally – after 2 hours, lasts approximately for 4 hours in case of durable administration of big doses – damaging of liver and kidneys, production of methemoglobin Acetaminophen Tablets Suppositories Syrups Soluble tablets Capsules Acetaminophen Panadol (Acetaminophen) Ketorolak (ketanov) according to analgesic activity it prevails over effect of acetylsalicylic acid, indometacin and equals to opioid analgesics moderate anti-inflammatory, pyrolytic and anti-aggregant effects high effectiveness in case of pain in postoperative period, in oncology, during child delivery, traumas, colics intramuscular introduction NOT indicated for chronic pain syndrome Ketoprophen (ketonal) strong analgesic, antiinflammatory and pyrolytic agent administered in case of arthroses and arthritis, ancilizing spondilitis, pain of different genesis (after surgeries, in case of traumas, painful menstruations etc.) administered orally, intramuscularly, in forms of suppositories and ointments TRAMADOL Analgesic activity is not weaker than activity of morphine In case of intravenous administration effect develops after 5-10 min, if administered orally – after 30-40 min, action lasts for 3-5 hours. ADMINISTRATION OF TRAMADOL surgery, traumatology, gynecology, neurology, urology, oncology For all kinds of acute and chronic pain of moderate and considerable intensity, including postoperative, traumatic pain neuralgias diagnostic and therapeutic interventions oncologic pathology Anesthesia Goals of Balanced Anesthesia Amnesia Anesthesia Goals of Balanced Anesthesia Amnesia Adequate Muscle Relaxation Anesthesia Goals of Balanced Anesthesia Amnesia Adequate Muscle Relaxation Adequate Ventilation Anesthesia Goals of Balanced Anesthesia Amnesia Adequate Muscle Relaxation Adequate Ventilation Pain Control Types of Anesthesia General Local Types of Anesthesia General Local Discussion What are some of the indicators used to assess general anesthesia? Discussion What are some of the indicators used to access general anesthesia? Answer: Blood pressure, hypervolemia, oxygen level, pulse, respiratory rate, tissue perfusion, urinary output General Anesthesia Preanesthetic Medications Control sedation Reduce postoperative pain Provide amnesia Decrease anxiety General Anesthesia Malignant Hyperthermia Side effect of anesthesia Fever of 110°F or more Life threatening Treatment: dantrolene (Dantrium) Warning! Always check expiration date. Drug List Inhalant Anesthetics desflurane (Suprane) enflurane (Ethrane) halothane isoflurane (Forane) nitrous oxide Inhalant Anesthesia Side Effects Causes reduction in blood pressure May cause nausea and vomiting nitrous oxide Causes analgesia only; no amnesia or relaxation May be given alone or may be given with more powerful anesthetics to hasten the uptake of the other agent(s) Commonly used for dental procedures Rapidly eliminated desflurane (Suprane) Has rapid onset and recovery Often used in ambulatory surgery General Anesthesia Often dispensed by IV drip Very lipid soluble Drug List Injectable Anesthetics etomidate (Amidate) fentanyl (Duragesic, Sublimaze) fentanyl-droperidol ketamine (Ketalar) morphine propofol (Diprivan) sufentanil (Sufenta) Drug List Injectable Anesthetics Barbituates methohexital (Brevital) thiopental (Pentothal) Benzodiazepines diazepam (Valium) lorazepam (Ativan) midazolam (Versed) propofol (Diprivan) Used for maintenance of anesthesia, sedation, or treatment of agitation Has antiemetic properties Drowsiness Respiratory depression Motor restlessness Increased blood pressure Injectable Anesthesia Dispensing Issues Warning! Diprivan (anesthetic) and Diflucan (antifungal) may be confused. This mix-up could be life-threatening. fentanyl Dosage Forms IV (Sublimaze) patch (Duragesic) lozenge (Actiq) for children Used extensively for open-heart surgery due to lack of cardiac depression Benzodiazepines Used for induction, short procedures, and dental procedures Useful in controlling and preventing seizures induced by local anesthetics midozolam (Versed) fastest onset of action greatest potency most rapid elimination Antagonist Agents Antagonist agents reverse benzodiazepine and narcotic overdose. Drug List Antagonist Agents flumazenil (Romazicon) nalmefene (Revex) naloxone (Narcan) flumazenil (Romazicon) Antagonizes benzodiazepines by competing for receptor site Used for complete or partial reversal naloxone (Narcan) Competes for opiate receptor sites Has a shorter duration of action than narcotics, so it must be given repeatedly Neuromuscular Blocking Agents Causes immediate skeletal muscle relaxation. Short Duration Intermediate Duration Extended Duration Used to facilitate endotracheal intubation. Allows for easier insertion of endotracheal tube. Keeps airway open. Drug List Neuromuscular Blocking Agents atracurium (Tracrium) cisatracurium (Nimbex) mivacurium (Mivacron) pancuronium rocuronium (Zemuron) succinylcholine (Quelicin) vecuronium (Norcuron) Neuromuscular Blocking Agents Dispensing Issues Warning! Very expensive Be conscious of storage requirements Store away from look-alike and drugs succinylcholine (Quelicin) Often called “sux.” Only depolarizing agent. All others work as competitive antagonists to ACh receptors. Persistent depolarization at motor endplate. Causes sustained, brief period of flaccid skeletal muscle paralysis. Reversal of Neuromuscular Blocking Agents Increases the action of acetylcholine by inhibiting acetylcholinesterase Used for reversal of nonpolarizing agents Drug List Anticholinesterase Agents edrophonium (Enlon) neostigmine (Prostigmin) pyridostigmine (Mestinon) Types of Anesthesia General Local Local Anesthesia Relieves pain without altering alertness or mental function. Local Anesthesia Variety of Dosage Forms Topical Superficial injection (infiltration) Nerve block IV Epidural Spinal Discussion Local anesthetics are classified by their chemistry into two classes. What are they? Discussion Local anesthetics are classified by their chemistry into two classes. What are they? Answer Esters Amides Local Anesthesia Esters Short acting Metabolized in the plasma and tissue fluids Excreted in urine Local Anesthesia Amides Longer acting Metabolized by liver enzymes Excreted in urine Drug List Local Anesthesia Esters benzocaine (Americaine) chloroprocaine (Nesacaine) dyclonine (Cēpacol Maximum Strength) procaine (Novocain) tetracaine (Cēpacol Viractin, Pontocaine) Drug List Local Anesthesia Amides bupivacaine (Marcaine) levobupivacaine (Chirocaine) lidocaine (L-M-X, Solarcaine, Xylocaine) lidocaine-epinephrine (Xylocaine w/ Epinephrine) lidocaine-prilocaine (EMLA) mepivacaine (Carbocaine) Discussion What functions are lost with local anesthetics? Discussion What functions are lost with local anesthetics? Answer Pain perception Temperature Touch sensation Proprioception Skeletal muscle tone Discussion Under what conditions would a local anesthetic be used over a general anesthetic? Discussion Under what conditions would a local anesthetic be used over a general anesthetic? Answer: It is chosen when a well-defined area of the body is targeted.