First Aid and Emergency Procedures
advertisement

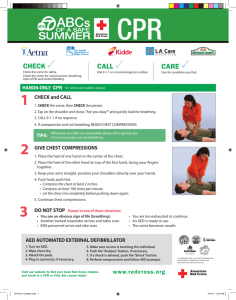
Date ECE 1B Objectives Teach ( WB = workbook) guppies Teach 2yo starfish 10 9 Birth – 2 Day 18 10/14 12/19 WB : st 3 objective 1b Pg: 7-8 Emergency procedures *Make a 1st Aid kit Preschool #1 Dolphins (3yo) & Whales (4yo) 8 Preschool #2 Lesson Plan Review and Prep Observe and Class Work Class Work assigned What is Due Today? 11, *13, Unit 5 12, 14 #1-5 13, 14 observe *Unit #4 Dolphins (3yo) & Whales (4yo) 7 #5 Unit 4 due Today 1st / 3rd QT sign up for support group Infant/Toddler Guppies (4) 2 year old Starfish (4) 3 year old Dolphins (3) 4 year old Whales (3) Emergency procedures WB : st 3 objective 1b Pg: 7-9 Emergency procedures *Make a 1st Aid kit Child Care Licensing Rule Interpretation Manual R430-100-10: EMERGENCY PREPAREDNESS (1) The provider shall post the center's street address and emergency numbers, including ambulance, fire, police, and poison control, near each telephone in the center. (2) At least one person at the facility at all times when children are in care shall have a current Red Cross, American Heart Association, or equivalent first aid and infant and child CPR certification. (3) The licensee shall maintain first-aid supplies in the center, including at least antiseptic, band-aids, and tweezers. Child Care Licensing Rule Interpretation Manual R430-100-10: EMERGENCY PREPAREDNESS (4) The provider shall have a written emergency and disaster plan which shall include at least the following: (a) procedures for responding to medical emergencies and serious injuries that require treatment by a health care provider; (b) procedures for responding to fire, earthquake, intruder, flood, power failure, and water failure; (c) the location of and procedure for emergency shut off of gas, electricity, and water; (d) an emergency relocation site where children may be housed if the center is uninhabitable; (e) a means of posting the relocation site address in a conspicuous location that can be seen even if the center is closed; (f) the transportation route and means of getting staff and children to the emergency relocation site; Child Care Licensing Rule Interpretation Manual R430-100-10: EMERGENCY PREPAREDNESS (4) The provider shall have a written emergency and disaster plan which shall include at least the following: (g) a means of accounting for each child's presence in route to and at the relocation site; (h) a means of accessing children's emergency contact information and emergency releases; including contact information for an out of area/state emergency contact person for the child, if available; (i) provisions for emergency supplies, including at least food, water, a first aid kit, diapers if the center cares for diapered children, and a cell phone; (j) procedures for ensuring adequate supervision of children during emergency situations, including while at the center's emergency relocation site; and (k) staff assignments for specific tasks during an emergency. Preparation for emergency Provides • The knowledge and skill needed to handle emergency medical care. With proper training, you will know how and when to treat illnesses and injuries. • Power, strength, and control. It will remove a lot of the fear when injuries happen. Believe me that they will happen! Our Center’s FIRE Procedure: • We will gather up the children and take them to the Seminary Building. Our Center’s Earthquake • Earthquake drill: Children take cover under desks, tables, or in doorways. • Students and teacher under larger tables, against walls covering head, or in doorways. • Do not leave building. Our Center’s Intruder alert • Lockdown- lock doors, take cover away from doors. – Infants stay in the infant room in the sleeping area. – Toddlers and preschoolers go into the observation booth. – Cindy, Julie, and Terry will lock doors while the students take the children to the safe locations. First Aid Kit and procedures • Keep a first aid kit handy and well stocked. –What items to include? • Store all items in one area. • Take the first aid kit with you on field trips. • Children with special needs should be accounted for when putting your first aid kit together. – Diabetes, Bee Sting kit – Have the parents put an emergency bag together for their child.) POISON • Symptoms: Vomiting, diarrhea, burns on mouth, convulsions. • Keep Poison Control Center phone number next to the phone. 801-581-2151 1-800-456-7707 • Determine what & how much the child ingested. Poison control will tell you the next steps to take. Wait to induce vomiting until poison control says to do so. Minor cuts, Abrasions, puncture wounds, and insect bites or stings 1. Wash your hands well, then take a look. 2. If the wound is bleeding, apply direct pressure with a clean bandage or towel until the bleeding stops. (If the bleeding doesn't stop after 10-20 minutes of direct pressure, take your child to the emergency room.) 3. After the bleeding stops, check for glass, dirt, or other foreign materials in the wound. If you see anything, try to flush it out with cool running water. If that doesn't work, use tweezers to carefully lift out the debris. 4. Then gently wash the wound well with soap and warm water, and carefully pat it dry. If your child strenuously objects to washing, try having him soak the wounded area in the bathtub. 5. It's not crucial, but applying an antibiotic ointment such as Polysporin after washing and drying the area can help reduce the risk of infection. Don't use rubbing alcohol, hydrogen peroxide, iodine, or Mercurochrome. Not only will they cause your baby more pain — they may actually slow healing. 6. Small cuts and scrapes heal faster when left open to the air, so unless the cut is in a spot that's likely to get dirty or rub against your baby's clothing, you can skip the bandage. Closed Wound Bumps • Diagnosis: Pain, redness, and swelling in the area. • Treatment: Cold Cloth or pack. (A frozen bag of peas works great) and elevation of the wounded area. • Applying ice directly on the area could damage skin tissue. and bruises Choking • Avoid foods that might cause choking in young toddlers and infants (nuts, popcorn, raw carrot slices, or grapes). • If choking occurs, encourage them to cough. • Never pound on the back or stick your finger down their throat to find the lodged item. • If there is no sound or breathing, use abdominal thrust / Heimlich Maneuver as many times as needed. – (Note: Some first aid training programs recommend alternating 5 back blows and 5 abdominal thrusts until either the item is dislodged or the victim becomes unconscious.) • If they pass out, lay them down and call 911. Begin CPR assessment CPR Assessment (ages 9-adult) • • Check for consciousness. Tilt the person’s forehead back and chin up to check for breathing. To do this tilt the head back and put your ear to the victims mouth. Your face should be pointing down the victims body. – • If the person isn't breathing normally, begin mouth-to-mouth breathing. – – – • With the airway open (using the head-tilt, chin-lift maneuver), pinch the nostrils shut for mouth-to-mouth breathing and cover the person's mouth with yours, making a seal. Prepare to give two rescue breaths. Give the first rescue breath — lasting one second — and watch to see if the chest rises. If it does rise, give the second breath. If the chest doesn't rise, repeat the head-tilt, chin-lift maneuver and then give the second breath. If the chest still doesn't rise the victim is choking and unconscious choking steps will need to be followed Check for pulse. To do this place your ear over the mouth like before but position two fingers in the groove of the neck closest to you. This is for children and adults. For infants place finger in between the shoulder and elbow on the inside of the arm. – • Look for chest motion, listen for normal breath sounds, and feel for the person's breath on your cheek and ear. Gasping is not considered to be normal breathing. If there is no pulse the victim is in serious danger and you will need to start CPR after doing the next step. Adult CPR – – Do 2 rescue breaths with your pocket mask into the victim. Do 30 chest compressions. You want to do chest compressions at a rate of 100 per minute. You do not do 100 but that is how fast you would go. • • • • • – – Put the person on his or her back on a firm surface. Kneel next to the person's neck and shoulders. Place the heel of one hand over the center of the person's chest, between the nipples. Place your other hand on top of the first hand. Keep your elbows straight and position your shoulders directly above your hands. Use your upper body weight (not just your arms) as you push straight down on (compress) the chest at least 2 inches (approximately 5 centimeters). Push hard at a rate of about 100 compressions a minute. You use the same two fingers in the chest on infants you do for unconscious choking also. Check for breathing Continue rotating between the rescue breaths and compressions until someone else can take over, medical help arrives, and AED arrives, or the person begins to breathe. To perform CPR on a child (ages 1-8) • The procedure for giving CPR to a child age 1 through 8 is essentially the same as that for an adult. The differences are as follows: • If you're alone, perform five cycles of compressions and breaths on the child — this should take about two minutes — before calling 911 or your local emergency number or using an AED. • Use only one hand to perform heart compressions. • Breathe more gently. • Use the same compression-breath rate as is used for adults: 30 compressions followed by two breaths. This is one cycle. Following the two breaths, immediately begin the next cycle of compressions and breaths. To perform CPR on a baby • • • • • • • • • • • • • • • • • • • • Most cardiac arrests in babies occur from lack of oxygen, such as from drowning or choking. If you know the baby has an airway obstruction, perform first aid for choking. If you don't know why the baby isn't breathing, perform CPR. To begin, examine the situation. Stroke the baby and watch for a response, such as movement, but don't shake the baby. If there's no response, follow the CAB procedures below and time the call for help as follows: If you're the only rescuer and CPR is needed, do CPR for two minutes — about five cycles — before calling 911 or your local emergency number. If another person is available, have that person call for help immediately while you attend to the baby. Circulation: Restore blood circulation Place the baby on his or her back on a firm, flat surface, such as a table. The floor or ground also will do. Imagine a horizontal line drawn between the baby's nipples. Place two fingers of one hand just below this line, in the center of the chest. Gently compress the chest about 1.5 inches (about 4 cm). Count aloud as you pump in a fairly rapid rhythm. You should pump at a rate of 100 compressions a minute. Airway: Clear the airway After 30 compressions, gently tip the head back by lifting the chin with one hand and pushing down on the forehead with the other hand. In no more than 10 seconds, put your ear near the baby's mouth and check for breathing: Look for chest motion, listen for breath sounds, and feel for breath on your cheek and ear. Breathing: Breathe for the infant Cover the baby's mouth and nose with your mouth. Prepare to give two rescue breaths. Use the strength of your cheeks to deliver gentle puffs of air (instead of deep breaths from your lungs) to slowly breathe into the baby's mouth one time, taking one second for the breath. Watch to see if the baby's chest rises. If it does, give a second rescue breath. If the chest does not rise, repeat the head-tilt, chin-lift maneuver and then give the second breath. If the baby's chest still doesn't rise, examine the mouth to make sure no foreign material is inside. If the object is seen, sweep it out with your finger. If the airway seems blocked, perform first aid for a choking baby. Give two breaths after every 30 chest compressions. Perform CPR for about two minutes before calling for help unless someone else can make the call while you attend to the baby. Continue CPR until you see signs of life or until medical personnel arrive. Minor (1st degree)Burn • These burns are much like typical sunburns and are cared for in a similar way. • You should immerse the burn in cool water (do not use ice it could harm the tissue!) and then blot it gently and apply burn cream and then cover with a dry, clean, non-stick pad. • These burns usually leave the skin red, mildly swollen, and painful to the touch. Second Degree: Second degree burns are more serious and should be seen by a medical professional. If the burn seems very severe report to an emergency room or call 911. Although second degree burns often look like first degree burns, in the sense that they are red, the damage goes deeper. With these burns, the pain is more intense and blistering may occur. The burns may also be wet, or weeping and may have a shiny surface. It is advised that these burns are not touched or covered. Bloody Nose • First, stay calm and reassure your child. Nosebleeds are very common and are rarely a cause for concern. • With your child upright in a chair, in your lap, or standing over the sink, tilt his or her head slightly forwards. – Have them spit out any blood in their mouth . • Using a tissue or a clean, soft washcloth, gently pinch the soft part of his nose (just below the bony ridge) shut. Keep pressure on the nose for about 10 minutes; if you stop too soon, bleeding may start again. – Do not have your child lean back. This may cause blood to flow down the back of the throat, which tastes bad and may cause gagging, coughing, or vomiting. – Don't pack his nose with cotton during or after a nosebleed. Bleeding can start right back up again when you remove the cotton and disrupt any clots that have formed. • During this time, remind your child to breathe through his mouth and continue to reassure him, if necessary. You might distract him by looking at a book together or watching a video. • After ten minutes, release the pressure and see if the bleeding has stopped. If it hasn't, pinch your toddler's nose closed for another ten minutes. – You can also apply a cold compress to the bridge of his nose.