Hawthorne Ethnicity and Clinical Trials Presentation
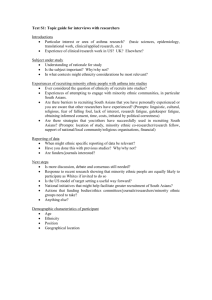
advertisement

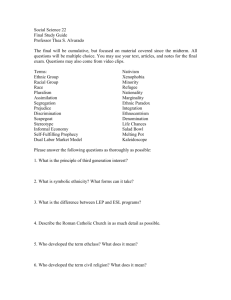
IDEA: IMPROVING THE DELIVERY OF ETHNICALLY APPROPRIATE RESEARCH, SERVICES AND POLICY THROUGH TRANS-DISCIPLINARY COLLABORATION Warwick University Institute of Advanced Study Incubation Award WHAT ARE WE ABOUT? • CURRENT RESEARCH IN ETHNICITY AND HEALTH TENDS TO BE SMALL -SCALE, SHORT-TERM, ‘ADD-ON’ THAT OFTEN ISN’T LINKED TO OTHER PARTS OF THE UK • RESEARCH FINDINGS DON’T GET INTO MAINSTREAM HEALTH SERVICES PROVISION • EACH RESEARCH CENTRE DEVELOPS ITS OWN TERMINOLOGY, OR RESEARCH OUTCOMES, SO COMPARABILITY AND COMBINATION IS DIFFICULT • HAVEN’T DISCOVERED THE ADDED DIMENSION OF WORKING ACROSS BOUNDARIES AND DISCIPLINES THIS FORUM • 3 WORKSHOPS, Clinical Trials, Diabetes and Obesity • UNITING RESEARCHERS WITH WELL-PLACED RESEARCH USERS, SOME HERE IN PERSON, SOME HERE VIRTUALLY • SPEAK DIRECTLY TO PROBLEMS FACED IN LOCATING HIGH QUALITY DATA, AND IN TRANSLATING RESEARCH FINDINGS INTO ETHNICALLY APPROPRIATE PRACTICE, PROVISION AND POLICY • IDENTIFY THE BARRIERS THAT OBSTRUCT KNOWLEDGE TRANSFER AND HAMPER EFFORTS TO ADDRESS PERSISTENT HEALTH INEQUALITIES AND POOR HEALTH OUTCOMES IN ETHNIC MINORITY GROUPS WE WANT: • US TO WORK TOGETHER TO DEVELOP NEW MODELS FOR RESEARCH ON KEY ETHNICITY-LINKED ISSUES IN MEDICINE, PUBLIC HEALTH, THE SOCIAL SCIENCES AND THE HUMANITIES • THE BEST RESEARCH TO BE WIDELY AND IMMEDIATELY ACCESSIBLE TO RESEARCH USERS: PRACTITIONERS, POLICY MAKERS, PUBLISHERS, FUNDING BODIES AND TARGET COMMUNITIES • TO DO SO, WE ALL NEED TO BE TALKING THE SAME LANGUAGE... CLINICAL TRIALS - issues with systematic reviews • Systematic Review of RCTs on culturally appropriate health education for minority groups with Type 2 diabetes (2009) • Searched for RCTs which specified a health education intervention and a named ethnic minority group across the world • Found short and medium term improvements in glycaemic control and knowledge. • Unable to determine the key elements of interventions across countries, ethnic groups and health systems CLINICAL TRIALS - issues with systematic reviews • Is it possible/ methodologically correct to compare such diverse groups? • On balance we decided it was, as these communities have a common experience of socio-economic disadvantage, communication and cultural differences from mainstream patients, inequalities in health and access to quality healthcare services. • General premise that information and empowerment leads to patientcentred clinical improvements, regardless of the origin of the patient • Searching for common, generic or key principles that could be adapted for any community or minority group • NOT adopting a rigorous approach could be implied ‘cultural deficit’ CLINICAL TRIALS - issues with systematic reviews • Problems with definitions used to define groups and the intervention: • Ethnic minority groups • How about studies from New Zealand, South Africa? • Culturally appropriate health education • What are the boundaries of this definition? CLINICAL TRIALS - issues with systematic reviews • Few studies fitted the selection criteria - 12 RCTs in the world literature. Limited number of minority groups. • Only one long term follow up study, one study that measured cost effectiveness. • Studies difficult to compare due to heterogeneous methodologies in approaches to culturally specific health education, although most based on previous experience in target communities • Need for culturally appropriate patient-centred outcome measures - many studies had to design and validate their own. Then not comparable with other studies. • Ethics of control groups/ disadvantaged groups/ keeping study protocols rigorous while engaging communities • Methodological issues - randomisation, power calculations. Unable to perform some analyses due to lack of sufficient studies. CLINICAL TRIALS - issues with systematic reviews • Why are ethnic minority groups rarely included in RCTs? - cf diabetes education methods are very idiosyncratic and often not assessed for effectiveness in a controlled manner • Unable to identify generic principles or key aspects of an intervention that could be adapted and applied to any community - eg effects of group working versus 1:1, type of intervention, duration and intensity of intervention, what types of cultural adaptations work best. • ‘Challenge remains to design research that is rigorous AND in accord with the personal commitments research teams need to make with participants. Issues of funding long-term studies as minority communities are often seen as peripheral to mainstream community research’. ISSUES IN CONDUCTING CLINICAL TRIALS • Difficulties recruiting participants - For trials targeted specifically to ethnic group, and for trials in general • Minority groups seen as ‘hard to reach’, and reluctant to take part in research. Some feel ‘over researched’ with no tangible outcomes for the community. • Language and cultural barriers - consent issues, lack of trust in the researchers leads to more refusals • Availability of common measurement tools that have been adapted to be culturally specific • Additional costs in time, staff and materials needing adaptation. • Worries about transferability of outcomes across cultural groups BARRIERS TO ETHNIC MINORITY PARTICIPATION IN CLINICAL TRIALS • (Hussain-Gambles et al, Health and Social Care in the Community, 2004) • Fear and mistrust • Inappropriate exclusion criteria, poorly designed trials • Access • Costs associated with interpreter/ translator • Shortage of ethnic minority trial co-ordinators • Consent issues • Socio-cultural barriers, stereotypes and cultural myths. OUR EXPERIENCE - Manchester and Cardiff • Approach minority communities via their community/ religious leaders • Pick study researchers who are culturally competent, culturally safe. Some of the research team should be from the community itself and grounded within it. Language should be as similar as possible to the group being studied. • Consult with the community, and look for ways to ‘pay back’ - eg general health promotion days, bringing in ‘ health experts’ to community events • Link research events to community events • Keep communities involved, and ensure they see the research outputs. • Use local radio, newspapers etc to keep people informed. WHAT ELSE DOES THE LITERATURE SAY? • Systematic under representation of BEM groups • Key themes: • researchers’ own attitudes and priorities differ from patient groups • stereotypes and prejudices about difficulties in engaging with BEM groups • logistical challenges of costs of language/ cultural communication offset against value for money • poorly developed understanding amongst community leaders of what research entails. • National Institute of health policy insists minority groups are represented in study samples WHAT ELSE DOES THE LITERATURE SAY? • Some minority groups mistrust purpose of research (African Americans) OTHER QUESTIONS • Should we use the term ‘ethnicity’? What is it about ethnicity and health? Do similar problems arise in relation to other taxonomies: gender, disability, age etc • Can we generate standard tools for establishing population taxonomies, rather than trying to set them ourselves? Eg the key relevant questions to support good research, a structure that all researchers will have considered,e even if only to discount • eg definitions of ‘ethnic minority groups’, ‘culturally appropriate’ interventions. • Can we generate a toolkit for engaging minority groups in research? • How to USE evidence in policy/ practice