HHV-6 or HHV-7
advertisement

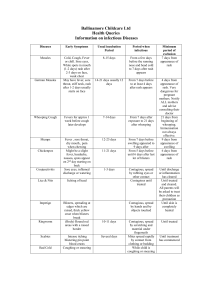
Pediatrics FEVER and RASH Lan-fang Tang Dept. Pediatric Pulmonology Rash appearance Skin lesions evolve over time, but the characteristic distribution and appearance provide important clues to the diagnosis Macular or Maculopapular Rash Diffuse Erythroderma Urticarial Rash Vesicular, Bullous, Pustular Petechial-Purpuric Erythema Nodosum Differential Diagnosis of Fever and Rash Macular or Maculopapular Rash -- virus: Measles Rubella Roseola (HHV-6 or HHV-7) Others: Erythema infectiosum (fifth disease, parvovirus B19), Epstein-Barr virus, Echoviruses, HBV, HIV Differential Diagnosis of Fever and Rash Macular or Maculopapular Rash--bacteria Scarlet fever (group A streptococcus) Others: Secondary syphilis, Leptospirosis, Pseudomonas, Meningococcal infection (early), Salmonella typhi (typhoid fever), Lyme disease (erythema migrans), Mycoplasma pneumoniae Measles Etiology Measles virus genus Morbillivirus family Paramyxoviridea Only one serotype Week vitality in vitro Measles virus Epidemiology Source of infection Route of transmission Susceptible population Source of infection patients as the main source infectivity from prodromal period to the time of 5~10 days after the rash appears respiratory secretions as the main media Route of transmission Direct respiratory transmission by droplet spray Indirect transmission by contact with the contaminated articles. Susceptible population Peak incidence: 8m~5yr Pathogenesis Virus inhalation incubation Local proliferation First viremia Proliferation in endoreticular system Second viremia prodromal All parts of the body eruption Clearance of virus convalescence Clinical Manifestation Typical measles Incubation stage Prodromal stage Eruptive stage Convalescent stage Stage 1: Incubation stage 6~18 days No symptoms or low fever, malaise Stage 2: Prodromal stage (Catarrhal stage) Lasts 3~4 days Low-grade to moderate fever Mucosal catarrh: conjunctivitis, coryza hacking cough Stimson line: transverse line of inflammation along the eyelid margin Koplik spots: a pathognomonic sign Koplik spots —a pathognomonic sign of measles Appear 2-3 days after fever develops Tend to occur over the buccal mucosa opposite the lower molars A grayish white dots(as small as grains of sands) with slight reddish areola Increase and disappear 1-2d after eruption Stage 3: Eruptive stage Lasts 3~4 days Characterized by the eruption of the rash The temperature rises abruptly as rash develops (usually >40℃) Exacerbated mucosal catarral symptoms: cough, vomitting and diarrhea, anorexia, a few rales on auscultation The order of eruption Usually starts on the upper lateral parts of the neck, behind ears, along the hairline and on the posterior parts of the cheek; Spreads rapidly over entire face, neck, upper arms and the upper parts of the chest within the first 24hr; Over the back, abdomen, entire arm and thighs during the succeeding 24hr; Finally reaches the feet on the 2nd~3rd day. The features of the rash Faint macules initially Pink maculopapular, 1-3mm in diameter Sparse to confluent or even fused with each other to form patches, but the normal skin can be found.in between. Begins to fade as the rash reaches the feet. Stage 4: Convalescent stage The symptoms resolve rapidly The rash fades downwards in the same sequence in which it appeared. Branny desquamation and brownish pigmentation occur and disappear within 710days Atypical Measles Atypical measles Mild measles (modified measles) Severe measles Measles without rash Hemorrhagic measles (black measles) Atypical measles syndrome Laboratory examination A laboratory confirmation is rarely needed Leukopenia , with a relative lymphocytosis Multinucleated giant cells in smear of nasal mucosa (Warthin-Finkeldey cells) Serum antibody(sIgM or double serum IgG) Virus isolation or virus antigen/RNA detection Complications Pneumonia ( fatal giant cell (Hecht) pneumonia in patients with impaired cell-mediated immunity) Laryngo-bronchitis Myocarditis Encephalitis Reactive tuberculosis Subacute sclerosing panencephalitis Basis of diagnosis Evidence of epidemiology Koplik spots The order and features of the rash Branny desquamation and brownish discoloration Therapy No specific antiviral therapy Supportive treatment antipyretics, bed rest, maintenance of an adequate fluid intake Management of complication Vitamine A supplement IVIG Vitamin A and measles: evidence Hyporetinemia is present in over 90% of measles cases in Africa and 22-70% in USA. There is an apparent inverse correlation between retinol concentration and the severity of measles. Oral Vitamin A supplement reduces the morbidity and mortality of severe cases. Indication for Vit A supplement (American Academy of Pediatrics) Hospitalized children 6mo~2yr of ages Children >6mo with immunodeficiency ophthalmologic evidence of Vit A deficiency impaired intestinal absorption moderate to severe malnutrition recent immigration from areas with a high mortality from measles Prevention Isolation Block the route of transmission Vaccine Post-exposure prophylaxis Prevention: Isolation Isolation precautions should be maintained from the 7th day after exposure until 5 days after the rash develops. Until 10 days after the rash develops for severe cases with pneumonia Contact with susceptibility be isolated for 21 days (28days for passive immunity receiver) Prevention: active immunization(Vaccine) Measles attenuated vaccine , or Measles- MumpsRubella vaccine(MMR) Initial immunization: 8mo A second immunization is recommended routinely(7y). Urgent vaccination for measles postexposure and outbreak prophylaxis Prevention: Passive immunization(post-exposure prophylaxis) Passive immunization with Ig within 5 days of exposure is effective for the prevention and attenuation of measles. Susceptible children <12mo should receive Ig (0.25ml/kg, <=15ml,IM) Differential Diagnosis of Fever and Rash Macular or Maculopapular Rash -- virus: Measles Rubella Roseola (HHV-6 or HHV-7) Others: Erythema infectiosum (fifth disease, parvovirus B19), Epstein-Barr virus, Echoviruses, HBV, HIV Rubella also known as German measles and 3-day measles; congenital rubella syndrome (infection in utero ) Etiology and epidemiology a single-stranded, positive-sense RNA virus ( a member of the togavirus family) Humans as the only host Spread either by oral droplet or transplacentally to fetus causing congenital infection Virus recovered from the nasopharynx 7d before exanthem and 7-8 d after its disappearance. Peak incidence in children 5~14 yr of age Clinical manifestations Incubation (14 to 21 d) Prodromal phase Mild catarrhal symptoms with shorter period Low-grade fever (1~3d) with meager systemic symptoms. About 2/3 are subclinical. Clinical manifestations The most characteristic sign: Enlarged post-occipital, retroauricular and posterior cervical lymph nodes with tender. Be evident 24h before rash and remain for 1 week or more Clinical manifestations Exanthem more variable even no rash first appear on face rapid evolution, usually cover the entire body in 24 h Usually clears by the 3rd day Discrete maculopapules with large flushing, or pinpoint appearance, or may be confluent on face Mild itching and minimal desquamation Clinical manifestations Enanthem in 20% patients Just before rash Discrete rose spots on the soft palate (Forchheimer spots) May coalesce into a red blush and extend over the fauces Slightly inflamed pharyngeal mucosa and conjunctivae without photophobia Clinical manifestations Congenital rubella (syndrome) Affects virtually all organ systems The most common manifestation is intrauterine growth retardation Other common findings: cataracts (microphthalmia, myocarditis, PDA); “blueberry muffin” skin lesions; hearing loss; meningoencephalitis. Diagnosis Apparent diagnosis based on clinical symptoms and signs Laboratory findings non-specific and generally do not aid in diagnosis confirmed by serology or virus culture Congenital rubella: serum sIgM or virus culture Prenatal diagnosis: cord blood sIgM or virus culture from amniotic fluid Treatment and prognosis There is no specific antiviral therapy Entirely supportive, and antipyretics The prognosis is excellent, but congenital rubella syndrome may have sequalae such as intrauterine growth retardation, cataracts, deafness, and a patent ductus arteriosus. Prevention Live rubella vaccine recommended as MMR for children( initial at 12-15m and second 4-6y) It is important for girls to have immunity before they reach childbearing age Differential Diagnosis of Fever and Rash Macular or Maculopapular Rash -- virus: Measles Rubella Roseola (HHV-6 or HHV-7) Others: Erythema infectiosum (fifth disease, parvovirus B19), Epstein-Barr virus, Echoviruses, HBV, HIV Etiology Roseola was first established as a distinct illness at the turn of 20th century; No causative pathogens were consistently identified until recent 10 years; It appears now that primary infection of human herpesvirus type 6 (HHV-6) and less frequently HHV-7 causes the majority of the cases of roseola. Epidemiology Primary HHV-6 infection occurs early in life with peak acquisition from 6-15 months of age. Rarely report contact with other infected children and outbreak uncommon. Most adults excrete HHV-6 and HHV-7 in saliva and may serve as primary sources for virus transmission. HHV-6 can be transmitted in utero. Cinical manifestations Incubation period: 5-10d Prodromal period: Usually asymptomatic Mild URT signs Mild cervical lymphadenopathy Cinical manifestations Clinical illness heralded by high fever 37.9~40.0 with an average of 39℃ Persists for 3-5 days and then resolves rather abruptly (crisis). Occasionally fever diminish over 24-36h gradually (lysis). May be irritable and anorexia but most behave normally Seizures in 5~10% Infrequent : rhinorrhea, sore throat, abdominal pain, vomiting and diarrhea. Cinical manifestations Eruption and fever A rash appears within 12~24 hours of fever resolution Eruption during defervescence or within a few hours of fever resolution Cinical manifestations Characteristic rash Rose colored rash ( discrete, small (2~5mm),slightly raised pink lesions) appears trunk , neck, behind ears, face and proximal extremities No pruritic, no vesicles Fade in 1~3 days Treatment and prevention There is no specific therapy HHV-6 is inhibited by ganciclovir but the benign nature preclude consideration of antiviral therapy. Excellent prognosis in majority no guidelines for prevention of roseola. Varicella Etiology Chickenpox (varicella) is the manifestation of primary infection of varicella-zoster virus (VZV). Zoster (shingles) is the manifestation of reactivated latent infection of endogenous VZV. Clinical manifestation Incubation period: 10~21d Subclinical varicella is rare Prodromal symptoms Usually moderate fever malaise, headache, anorexia and occasionally mild abdominal pain precede the rash by 24~48h Clinical manifestation The characteristic rash initially as small red papules rapidly progress to nonumbilicated, oval, "teardrop" vesicles on an erythematous base. The fluid progresses from clear to cloudy, and the vesicles ulcerate, crust, and heal. New crops appear for 3 to 4 days, usually beginning on the trunk followed by the head, the face, and, less commonly, the extremities. Clinical manifestation Pruritus, mucous membrane lesions, lymphadenopathy Hypopigmentation or hyperpigmentation persists for days to weeks in some Scarring unusual unless secondarily infected Clinical manifestation Progressive varicella usually in immunocompromised children Neonatal chickenpox delivery within 1 week before or after the onset of maternal varicella frequently results in severe varicella in neonates Congenital varicella when pregnant women (especially between 8-20 weeks) contract chickenpox, 25%of the fetuses may become infected. Complication Complications are common secondary infection of skin lesions by streptococci or staphylococci, Thrombocytopenia and hemorrhagic lesions or bleeding, pneumonia , myocarditis, pericarditis, orchitis, hepatitis, ulcerative gastritis, glomerulonephritis, and arthritis , Reye syndrome, encephalitis, cerebellar ataxia, nystagmus, and tremor Therapy Symptomatic therapy Antivirals (acyclovir, famciclovir, or valacyclovir ) are effective in preventing severe complications the routine oral administration of acyclovir is not recommended in otherwise healthy children because of the marginal therapeutic benefit, the lack of difference in complications, and the cost of acyclovir treatment. Thank you! Email: tanglanfangzju@163.com