Hearing disorders
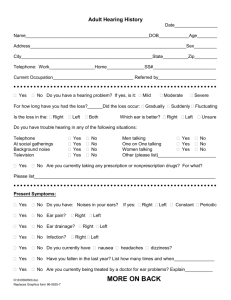
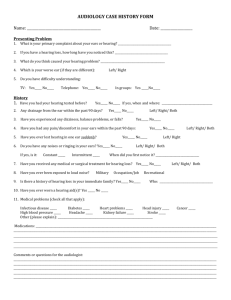
advertisement

Hearing Disorders The most common hearing disorders are those that affect hearing sensitivity. When a sound is presented to a listener with a hearing sensitivity disorder, one of two things may occur: 1. The listener with a HS disorder may be unable to detect the sound. 2. The sound will not be as loud to that listener as it would be to a listener with normal hearing. Note: Vision is different. The most common vision disorders affect acuity, not sensitivity to light. Acuity is the ability to resolve differences. Eyeglasses and contact lenses improve acuity, not sensitivity to light. Hearing aids are just the opposite – they improve sensitivity to sound by amplifying it – but do not improve acuity. Important: This sensitivity vs. acuity distinction is not quite so simple with hearing: hearing loss of any significance nearly always involves problems of both sensitivity and acuity – sounds are harder to hear (sensitivity) and they are nearly always distorted (acuity). More later. The Audiogram Most common way to measure hearing sensitivity is to measure pure-tone (sinusoid) thresholds. Threshold: Intensity required to barely detect a sound. 125 250 Audiogram of a Listener with Thresholds in the Normal Range 500 1000 2000 4000 8000 -10 0 Red: right ear 10 Intensity (dB HL) 20 (red, round, right) 30 40 50 60 70 80 90 100 110 Frequency (Hz) Mild high-frequency loss 125 250 Audiogram of a Listener with a Mild High-Frequency Hearing Loss 500 1000 2000 4000 8000 -10 0 10 Red: right ear Intensity (dB HL) 20 30 40 50 60 70 80 90 100 110 Frequency (Hz) Moderate-to-profound bilateral loss Severe Loss Left, Ear Moderate Loss Right Ear 125 250 500 1000 2000 4000 8000 -10 0 10 20 Intensity (dB HL) 30 40 50 60 70 80 90 100 110 Frequency (Hz) Pure Tone Average (PTA) Average thresholds at 500, 1000, 2000 Hz – the frequencies most important for speech understanding. From the audiogram above: Pure-tone Average, Left Ear: Pure-tone Average, Right Ear: 93 dB 50 dB Terminology Normal Hearing: PTAs < 25 dB Hearing Impairment: PTAs 25-92 dB Deaf: PTAs > 92 dB The term deafness is reserved for cases in which “ … the handicap for hearing everyday speech … [is] … total” (Davis & Silverman, 1979). Despite these conventions: (1) there is no sharp dividing line between hearing impairment and deafness, and (2) degrees of deafness are meaningful; e.g., there is an important difference between PTAs of 110 and 95. Types of Hearing Disorders Many ways to classify hearing disorders 1. Nature of the loss: Sensitivity vs. Acuity Dysacusia – Deficit in discrimination or interpretation of sound: “Don’t shout, I can hear you just fine. I just can’t understand what you’re saying.” Disacusia is a good term that isn’t in very common use. Acuity deficits sometimes due to disorders of the central auditory system. Disorders of sensitivity and acuity are not mutually exclusive. 2. Functional Classification Conductive – Disorders involving the conduction of sound to the cochlea. Sensori-neural – Disorders involving the cochlea (usually the hair cells) or 8th N. Central – Disorders affecting the brain stem or auditory cortex. Two related terms: Peripheral – Not central; i.e., conductive or sensorineural. Retrocochlear – Disorders involving anatomical structures beyond the cochlea; i.e., 8th N, brain stem, auditory cortex. 3. Cause or Etiology of the Disorder Hearing disorders can be classified on the basis of the cause of the disorder. Some examples: Ototoxic drugs Noise exposure Old age (presbycusis) Otitis media 8th N tumors Meniere’s Disease In this review, we will proceed by functional subsystem (conductive, sensori-neural, central), and by etiology within each subsystem. Conductive Hearing Disorders 1. External Ear Congenital malformations. There are many of these. Most serious is congenital atresia – collapse or closure of the EAM (ear canal). May occur in isolation, but typically associated congenital malformations of the middle ear as well. Impacted wax (cerumen) – results in mild hearing loss; easily treated by removal of the wax. 2. Middle Ear a. Otitis Media By far the most common cause of conductive hearing loss. By far the most common health problem in children. Otitis media means inflammation of the middle ear. Disease Process – OM involves a very specific chain of events revolving around the abnormal functioning of the Eustachian tube. Begins with an ordinary upper respiratory infection (head cold) involving, among other things, the nasopharynx. Nasal secretions infect the Eustachian tube. The Eustachian tube, which is normally closed, becomes inflamed and can no longer open upon swallowing, yawning, etc. This means that pressure can no longer be equalized between the middle ear and the ambient air. **** This is the key to the whole deal **** Oxygen in the ME cavity is consumed by ordinary metabolic processes. Ordinarily, this oxygen is re-supplied through the Eustachian tube. With a plugged ET, this cannot occur. The absorption of oxygen without re-supply results in a partial vacuum (i.e., lower than normal pressure) in the ME. The pressure drop sucks the TM inward into the ossicular chain, reducing its mobility. Consequences: hearing loss and pain – often quite intense. Partial vacuum creates another problem: Recall that the entire ME cavity is lined with mucous membrane. The pressure drop causes clear fluid to be sucked out of the mucosal lining of the ME. This accumulation of fluid contributes to the conductive hearing loss. Condition is called serous otitis media or nonsuppurative otitis media. Defining features: (1) clear, thin, watery fluid, (2) fluid is sterile (not infected). Suppurative or Purulent Otitis Media: As the disease progresses, the fluid can become infected and thickens into (eck) pus. Consequences The major consequences of OM are hearing loss and pain. The hearing loss is typically mild (usually 20-30 dB) and often fluctuating. The pain varies quite a bit but is often quite severe. It is not unusual for the pressure drop in the ME to become severe enough to cause the TM to rupture. Some Additional Terminology Acute vs. Chronic OM: A specific bout of OM with pain, accumulation of fluid, etc., is called acute otitis media. If OM lasts more than 2-3 months, the condition is known as chronic otitis media. Recurrent OM: Frequent bouts of OM: OM is treated successfully, then returns, then treated, then returns … This gets old after a while but is pretty common. Treatment of Otitis Media Most common treatment by far: Antibiotics (especially amoxicillin) Common treatment for recurrent or chronic OM: PE Tubes (PE = pressure equalization). This is a small plastic tube inserted into the TM. Why would such a tube be expected to treat OM? A Few Additional Terms Otitis Media with Effusion (OME): Otitis media characterized by the accumulation of fluid. This term refers to any kind of fluid -- sterile, infected, it doesn't matter. Mucoid or Mucous Otitis Media (“Glue Ear”): Fluid in middle ear is thick and gooey rather than thin and watery. Hearing loss is often more severe than serous OM. Seen in some cases of recurrent OM – purulent OM is treated, killing the infection, but fluid does not drain. Speech and Language Delay?? Evidence is mixed and controversial, but there is some research suggesting that frequent bouts of OM *may* result in delays in acquiring speech and language. Surprising to some since hearing loss is usually relatively mild and fluctuating, with significant periods of normal hearing in between bouts of OM for most kids. But, there is also clear evidence from other sources indicating that kids need higher sound levels to perceive speech with the same accuracy as adults. [Elliott et al. (1979). Children’s understanding of monosyllabic nouns in quiet and in noise. J. Acoust. Soc. Am. 66, 12-21.] b. Otosclerosis (note: topic here is still conductive HL, sorted by cause) Begins as a soft, spongy growth of new bone – may appear anywhere in the ME, but most often near oval window. Later hardens (i.e., becomes sclerotic) In 90% of cases: No symptoms In unlucky 10%: Growth reduces mobility of stapes, causing a conductive HL. Progressive. Beginning in childhood. For that unlucky 10%, HL typically begins in late teens, early 20s. Maximum HL seldom worse than ~50-60 dB. Treatment: Stapedectomy (removal of stapes and replacement with an artificial stapes) Stapedectomy incus prosthetic stapes c. Cholesteatoma Cyst that invades the ME; usually grows rapidly Can: (1) destroy the ossicular chain, (2) invade the cochlea, or (3) break through the thin shelf of bone that forms the superior surface of the ME cavity, invading the meninges. This is extremely not good. HL is usually mild and not really the major concern. From http://www.ohsu.edu/ent/ear/chol.html (read this on your own) Cholesteatomas are benign growths of skin in the middle ear and mastoid. These "skin cysts" can and do cause many problems in the ear. Cholesteatomas commonly cause hearing loss and infections. The only treatment available to cure a cholesteatoma is surgery. The surgery that is typically performed is tympanoplasty with or without mastoidectomy. Cholesteatomas left untreated can go on to cause serious and sometimes life threatening health problems, such as meningitis or brain abscess. Cholesteatomas can develop in both children and adults. Surgery is usually done as day surgery (outpatient). Sensorineural Hearing Loss General: By far the most common underlying cause of SN HL is damage to the hair cell transducers. In these most common cases, the auditory nerve and central auditory pathway are intact, but stimulation of the auditory nerve is abnormal due to damaged hair cells. There are many possible reasons for hair cell damage. The various etiologies of SN HL consist mainly of a catalog of different causes of HC damage. a.Presbycusis • Hearing loss associated with aging • Most common cause of SN HL – and most common cause of HL overall • Presbycusis begins in adolescence. Sad but true. This figure shows data for men (top) and women (bottom) at different ages. Not good. Men Note that high frequencies are more strongly affected than lows. (We’ll see this again when we talk about noise-induced HL.) Any guesses about why high-freqs are more vulnerable? (Answer: The traveling wave starts at the base [high freq] and heads to the apex [low freq]. So, low freq sound stimulates HCs at the low freq end and the high freq end, while high freq sound stimulates HCs at the high freq end only. And if you look back to the Rose et al. FRC data from the physiology lecture, the spread of excitation is especially large on the low freq side. So, for low freq sound HCs at both ends of the BM are vulnerable, but for high freq sound only HCs at the basal end are affected, preserving low freq HCs. Moral: If you’re a hair cell, you’re better off at the apex.) Women Moral: We all have a long, slow slide ahead of us. Don’t squander the hearing you have by needlessly exposing yourself to long periods of loud sound. Wear ear plugs or muffs when mowing the grass, snow-blowing, etc., and use some sense in listening to music. Once hair cells are damaged, they’re gone for good. One last point: Presbycusis is listed here under the SN category since it is clear that this is the dominant component. However: (1) The SN component may not be due exclusively to hair cell loss. Changes in the elasticity of the basilar membrane and metabolic changes in the stria vascularis may also play a role (Davis, H. and Silverman, S., 1978, Hearing and Deafness, New York: Holt, Rinehart & Winston ). (2) There may also be a conductive component due to age-related changes in the mobility of tissues in the middle ear. (3) There is sometimes a central component due to the loss of neurons in the CNS, (related primarily to arteriosclerosis). The result of this CNS damage is a reduction in acuity and speech perception abilities. The resulting deficit in speech perception ability is sometimes referred to as phonemic regression. In some cases it is this problem rather than a loss of hearing sensitivity that is the patient’s primary complaint. b. Noise-Induced Hearing Loss Exposure to high levels of noise can damage HCs and cause SN HL. Two types: Acoustic trauma: Injury due to brief exposure to very intense sounds such as gun shots, artillery fire, explosions, etc. HL may be severe and permanent, but substantial recovery is common. Long-term noise exposure (more common): Damage results from long-term exposure to high levels of noise. Common in some occupational settings – heavy manufacturing and agriculture being the most common. Amount of inner-ear damage depends on the combination of: Intensity of the noise Length of exposure Pretty simple: High levels x long exposures=Bad news Low levels x brief exposures=Not so bad news Audiometric Pattern is distinctive (audiogram on right shows more advanced progression than left) Image from http://www.aafp.org/afp/20000501/2749.html (American Academy of Family Physicians) Note: (1) Dip or “notch” at ~3-6 kHz (2) Typical progression shows the notch broadening (especially on the high frequency side) and deepening (3) High frequencies more affected than lows c. Ototoxic Drugs Certain drugs can cause SN HL. Toxicity effects vary from mild and temporary to severe and permanent. Some very common drugs such as aspirin (especially in large doses) can cause hearing loss (and/or tinnitus), but not in most people, and the loss is typically mild and temporary. An especially important group of antibiotics are notoriously ototoxic. Examples include neomycin, streptomycin, kanamycin. Since this is well known, why might these drugs ever be administered? (Answer: They’re used when death is the likely alternative.) ANTIBIOTICS WITH GOOD EVIDENCE FOR OTOTOXICITY Drug Vestibulotoxicity Erythromycin Hearing Toxicity Toxic Level yes High IV doses only Usually 2 weeks Gentamicin 8.6% minor Streptomycin very toxic minor dihydrostreptomicin minor toxic very toxic Tobramycin Yes minor in 6% Netilmicin 2.4% Amikacin not toxic 13.9% Neomycin minor very toxic Kanamycin minor very toxic Etiomycin moderate Vancomycin nontoxic none to moderate Metronidizole toxic (rarely) unknown Capreomycin Less toxic than Gentamicin In topical ear drops synergistic with gentamicin yes Table from: http://www.tchain.com/otoneurology/disorders/bilat/ototoxins.html See other classes of ototoxic drugs on the same web site. For your reference. The list below is from: www.lhh.org/hrq/22-2/ototoxic.htm A. Salicylates 1. aspirin and aspirin-containing products 2. salicylates & methyl-salicylates (linaments) B. Non-Steroidal Anti-Inflammatory Drugs (NSAIDS) 1. diclofenac (Voltaren) 2. etocolac (Lodine) 3. fenprofen (Nalfon) 4. ibuprofen (Motrin, Advil, Nuprin, etc.) 5. indomethacin (Indocin) 6. naproxen (Naprosyn, Anaprox, Alleve) 7. piroxicam (Feldene) 8. sulindac (Clinoril) (Toxic effects are dose related and are almost always reversible once medications are discontinued). C. Antibiotics 1. aminoglycosides a. amikacin (Amakin) b. gentamycin (Garamycin) c. kanamycin (Kantrex) d. neomycin (Found in many over-the-counter antibiotic ointments) e. netilmicin (Netromycin) f. streptomycin g. tobramycin (Nebcin) (Of particular interest is that topical ear drop medications containing gentamycin or neomycin do not appear to be ototoxic in humans unless the tympanic membrane (ear drum) is perforated. When a solution of an aminoglycoside antibiotic is used on the skin together with an aminoglycoside antibiotic used intravenously, there is a risk of an increase of the ototoxic effect, especially if the solution is used on a wound that is open or raw, or if the patient has underlying kidney damage. Neomycin is the drug that is most toxic to the structure involved in hearing, the cochlea, so it is recommended for topical use only. But even topical therapy has resulted in hearing loss when large areas were treated which allowed for large amounts of the drug to be absorbed into the body. Hearing loss caused by this class of antibiotics is usually permanent). 2. erythromycin a. EES b. E-mycin c. Ilosone d. Eryc e. Pediazole f. Biaxin g. Zithromax (Usually ototoxic when given in intravenous doses of 2-4 grams per 24 hours, especially if there is underlying kidney failure). 3. vancomycin (Vancocin) (Similar to aminoglycosides in that it may be ototoxic when used intravenously in life- threatening infections. To further exaggerate the problem is the fact that aminoglycosides and vancomycin are often used together intravenously when treating life-threatening infections). 4. minocycline (Minocin) (Similar to erythromycin). 5. polymixin B & amphotericin B (Antifungal preparations). 6. capreomycin (Capestat) (Anti-tuberculosis medication). D. Diuretics 1. bendroflumethazide (Corzide) 2. bumetadine (Bumex) 3. chlor-thalidone (Tenoretic) 4. ethacrynic acid (Edecrin) 5. furosemide (Lasix) (These are usually ototoxic when given intravenously for acute kidney failure, acute hypertensive crisis, or acute pulmonary edema/congestive heart failure. Rare cases of ototoxicity have been found when these medications are taken orally in high doses by people with chronic kidney disease). E. Chemotherapeutic Agents 1. bleomycine (Blenoxane) 2. bromocriptine (Parlodel) 3. carboplatinum (Carboplatin) 4. cisplatin (Platinol) 5. methotrexate (Rheumatrex) 6. nitrogen mustard (Mustargen) 7. vinblastin (Velban) 8. vincristine (Oncovin) (The ototoxic effects can be minimized by carefully monitoring blood levels). F. Quinine 1. chloroquine phosphate (Aralen) 2. quinacrine hydrochloride (Atabrine) 3. quinine sulfate (Quinam) (The ototoxic effects are very similar to those of aspirin). G. Mucosal Protectant 1. misoprostol (Cytotec) d. Meniere’s Disease Serious, often debilitating disease of hearing and balance of uncertain cause. MD affects a single ear in about 75% of cases. Four major symptoms: (1)Periodic episodes of rotary vertigo (the sensation of spinning) or dizziness (the “Meniere’s attack”) (2)Fluctuating, progressive, low-frequency hearing loss (3) Roaring or ringing tinnitus (4) A sensation of "fullness" or pressure in the ear (1) Rotary Vertigo This is often the most disruptive and debilitating symptom of Meniere’s. Similar to the mild vertigo you get from too many beers, or that you may remember as a kid from spinning around on a playground. Some major differences: Dramatically more severe Often accompanied by nausea, vomiting, sweating Onset is usually sudden Typically persists for hours or even days Patient has little or no ability to control it Condition often leaves the patient confined to a bed and as stationary as possible for long periods of time, until the symptoms subside. Even small head movements can greatly exacerbate the symptoms. (2) SN Hearing Loss Fluctuating Initially affects low-frequencies more than highs, but may spread to highs as the disease progresses Progressive (i.e., gets worse with time) Hearing may be completely lost in the affected ear Usually unilateral Sounds may appear “tinny” (due to low-freq loss) and distorted Loudness intolerance is common (abnormal sensitivity to intense Loudness intolerance is common (abnormal sensitivity to intense sounds) (3) Tinnitus Ringing, roaring, or buzzing sensation Fluctuates in intensity but does not abate Pretty annoying (4) Sensation of “fullness” Like the weird sensation you get on an airplane or elevator before your ears pop – except it can’t be cleared. (Cause of fullness sensation is unrelated to M.E. function) Cause of Meniere’s The proximate (i.e., immediate) cause of MD is thought by some to be excessive and fluctuating pressure in the endolymphatic fluid that courses through the membranous labyrinth of the cochlea and vestibular systems. This causes the membranous labyrinth to balloon or dilate. Condition is known as endolymphatic hydrops. Result is progressive damage to the hair cells responsible for both hearing and balance. Underlying cause of the fluid imbalance (if that actually is what’s going on) is not known. Likely suspects – viral infection or autoimmune disorder affecting production or absorption of endolymph (duh). Normal Ear Ear w/ Endolymphatic Hydrops Note bulging of membranous labyrinth (www.tchain.com/otoneurology/disorders/menieres/men_eti.html) Age and Sex Distribution: MD is an Equal-Opportunity Disease Moral: The disease strikes all ages and both sexes. Incidence (number of new cases diagnosed per year) Estimates vary, but probably somewhere between 100 and 200 new cases per year per million (see citations below). TJ Wilmot. Ménière's disorder. Clinical Otolaryngology 1979 4: 131-43. J Stahle, C Stahle, K Arenberg. Incidence of Ménière's disease. Archives of Otolaryngology 1978 104: 99-102. I Watanabe. Incidence of Ménière's disease, including some other epidemiological data. Ménière's Disease: A Comprehensive Appraisal, ed WJ Oosterveld. 1983 J Wiley & Sons. P Wladislavosky-Waserman, GW Facer, B Mokri, LT Kurland. Ménière's disease: a 30-year epidemiological and clinical study in Rochester MN, 1951-1980. Laryngoscope 1984 94: 1098-1102. D Celestino, G Ralli. Incidence of Ménière's disease in Italy. American Journal of Otology 1991 12: 135-8. Prevalence (number of cases present at any given time) 2,182 per million P Wladislavosky-Waserman, GW Facer, B Mokri, LT Kurland. Ménière's disease: a 30-year epidemiological and clinical study in Rochester MN, 1951-1980. Laryngoscope 1984 94: 1098-1102. Treatment Numerous: Everything from diet to medications (aimed at treating nausea and vertigo) to surgery. Considerable debate about the effectiveness of various treatments. A few surgical treatments deserve mention: (1) Endolymphatic shunt • Plastic tube installed to drain excessive fluid and reduce pressure • There is controversy about effectiveness – some have called it a “placebo” surgery. (2) Vestibular Nerve Resection • • Vestibular branch of 8th N is cut, leaving cochlear branch intact (therefore preserving residual hearing). Vertigo abates, but balance problems may persist. (3) Destruction of the Affected Ear (pray for no mix-ups) In some severe (always or nearly always unilateral) cases of MD that are unresponsive to other treatment, complete ablation of the labyrinth is recommended. (Surgeon goes in through the EAM, removes the incus and stapes, pokes a hole in the promontory, and removes the sensory tissue in the labyrinth. In some cases the 8th N is cut as well.) This surgery is pretty extreme – good indication of how debilitating MD can be. To my knowledge, there have been no randomized clinical trials of any surgical treatment for MD. For your reference – Drug Therapy: Betahistine There have been several well designed randomized clinical trials testing the effectiveness of a synthetic histamine call betahistine hydrochloride in treating vertigo/nausea. Results have been encouraging. Dark bars=No. of attacks/month Light bars=Duration of attacks TJ Wilmot, GE Menon. Betahistine in Ménière's disease. Journal of Laryngology and Otology 1976 90: 83340 IJC Frew, GE Menon. Betahistine hydrochloride in Ménière's disease. Postgraduate Medical Journal 1976 52: 501-3. Fischer & van Elferen (1985) A Fischer, L van Elfren. Betahistine in the treatment of paroxysmal attacks of vertigo. A double blind trial (transl.). TGO tijdschrift voor Therapie, Geneesmiddel en Onderzoek. 1985 10: 933-7. Prognosis • • • According to one source, vestibular symptoms can be controlled (not prevented) in about 70% of patients, meaning that attacks of vertigo will be prevented or will be reduced in severity/frequency. Tinnitus seldom disappears. If treatment is started while a patient's hearing is still fluctuating, it is sometimes improved by medical management. In some patients, however, hearing loss will continue to worsen. e. Infections Bacterial or viral infections that invade the inner ear can cause SN HL and disruptions of vestibular function. Generic term for infections that invade the inner ear: labyrinthitis. Meningitis can sometimes spread to the inner ear and result in labyrinthitis. Other infectious diseases: Mumps, measles, meningitis, encephalitis, chicken pox, influenza, and syphilis can also invade the inner ear and cause SN HL and/or vestibular symptoms. f. 8th N Tumors (acoustic neuroma) • • • • • • Benign (i.e., nonmalignant) tumor that exerts pressure on 8th N Almost always slow growing Most common symptom: hearing loss (mild initially), often accompanied by tinnitus Vestibular problems may also occur Cause is unknown Continued tumor growth can be life threatening f. 8th N Tumors (acoustic neuroma) • • • • Treatment: Surgical removal or radiation Early detection is really important: Small tumors can be removed with less risk of destroying the 8th N (and sometimes the 7th N as well). But, early detection is difficult – early-stage symptoms are not dramatic. Acoustic neuromas sometimes run in families (case in point to follow). g. Congenital Causes Congenital: Present at (or before) birth This is to be distinguished from acquired or adventitious hearing loss. Congenital etiologies may be hereditary or non-hereditary. (1) Non-Hereditary Causes (a) Maternal rubella (German measles) When an expectant mother is exposed to rubella, the mother is not in any great danger, but the fetus is – especially in the 1st trimester. Effects can include: Heart defects, brain damage, various visual impairments SN HL, often profound Less common now since the development of a rubella vaccine A rubella vaccine was not available when the last rubella epidemic occurred in 1964. A large proportion of the current population of congenitally deaf adults lost their hearing as a result of this epidemic. These folks are now in their mid-40s. The incidence of congenital deafness has been greatly reduced in recent years since maternal rubella has come under better control. (b) Anoxia (asphyxia) Insufficient oxygen during birth/delivery can cause all sorts of problems for the newborn. There’s hardly anything that’s not on the list of anoxia consequences. SN HL is on the list. (c) Many other etiologies that are less common (2) Hereditary Causes Genetic factors are thought to cause more than 50% of all incidents of congenital hearing loss in children (NIDCD, 1989). Two patterns: (a) autosomal dominant (autosome = not a sex chromosome) One parent has a dominant gene for SN HL (and typically has a hearing loss). There is at least a 50% probability that the child will also have a hearing loss. Probability is higher if both parents have the dominant gene. (b) autosomal recessive Both parents (typically with normal hearing) carry a recessive gene for SN HL. Each child will have a 1 in 4 chance of inheriting the bum gene. Approximately 80% of inherited hearing loss is autosomal recessive. This makes early detection tough since, with both parents hearing normally, the children are not considered at risk. (www.asha.org/hearing/disorders/causes.cfm) Syndromes: Inherited hearing loss can also be associated with a complex of inter-related symptoms in the form of a syndrome. A few examples include: Waardenburg Syndrome Treacher-Collins Syndrome Klippel-Feil Syndrome Waardenburg Syndrome Treacher-Collins Syndrome